Abstract
Study Design:
Secondary analysis of prospective, multicenter data.
Objective:
To evaluate impact of sagittal parameters on health-related quality of life (HRQoL) in adults with lumbosacral spondylolisthesis.
Methods:
Adults with unoperated lumbosacral spondylolisthesis were identified in the Spinal Deformity Study Group database. Pearson’s correlations were calculated between SF-12 (Short Form–12)/Scoliosis Research Society–30 (SRS-30) scores and radiographic parameters (C7 sagittal vertical axis [SVA] deviation, T1 pelvic angle, pelvic tilt [PT], pelvic incidence, sacral slope, slip angle, Meyerding slip grade, Labelle classification). Main effects linear regression models measured association between individual health status measures and individual radiographic predictor variables.
Results:
Forty-five patients were analyzed (male, 15; female, 30; average age 40.5 ± 18.7 years; 14 low-grade, 31 high-grade). For low-grade slips, SVA had strong negative correlations with SF-12 mental component score (MCS), SRS-30 appearance, mental, and satisfaction domains (r = −0.57, r = −0.60, r = −0.58, r = −0.53, respectively; P < .05). For high-grade slips, slip angle had a moderate negative correlation with SF-12 MCS (r = −0.36; P = .05) and SVA had strong negative correlations with SF-12 physical component score (PCS), SRS-30 appearance and activity domains (r = −0.48, r = −0.48, r = −0.45; P < .05) and a moderate negative correlation with SRS-30 total (r = −0.37; P < .05). T1 pelvic angle had a moderate negative correlation with SF-12 PCS and SRS-30 appearance (r = −0.37, r = −0.36; P ≤ .05). For every 1° increase in PT, there was a 0.04-point decrease in SRS appearance, 0.05-point decrease in SRS activity, 0.06-point decrease in SRS satisfaction, and 0.04-point decrease in SRS total score (P < .05).
Conclusion:
Lumbosacral spondylolisthesis in adults negatively affects HRQoL. Multiple radiographic sagittal parameters negatively affect HRQoLs for patients with low- and high-grade slips. Improvement of sagittal parameters is an important goal of surgery for adults with lumbosacral spondylolisthesis.
Keywords: lumbosacral spondylolisthesis, health-related quality of life, sagittal, balance, lumbopelvic parameters, slip angle
Introduction
Lumbosacral isthmic spondylolisthesis is a heterogeneous developmental disorder that often manifests clinically in childhood and adolescence.1–3 Pain, hamstring tightness, neurologic symptoms, cosmetic deformity, and sagittal malalignment are common accompanying symptoms that may result in varying degrees of functional and psychological disability.4 Associated disability and health-related quality of life (HRQoL) scores are consistently correlated with severity of global sagittal malalignment and abnormal lumbopelvic alignment in children and adolescents.5–7 While abnormalities in sagittal profile have proven to be important determinants of disability in adults with spinal deformity,8–12 the relationship between radiographic parameters of sagittal alignment and HRQoL scores in adults with lumbosacral isthmic spondylolisthesis is yet to be evaluated. As such, the objective of this study is to evaluate the impact of sagittal alignment and lumbosacral parameters on health status in adults with lumbosacral spondylolisthesis.
Methods
Data for this study was obtained from the Spinal Deformity Study Group (SDSG). The SDSG is a prospective, multicenter, consecutive clinical series of which the principal goal was to evaluate surgical treatment of adolescents with idiopathic scoliosis and spondylolisthesis. Members of SDSG were either full-time academic surgeons or affiliated with a major academic medical center principally in the United States, but also in France, Japan, and South Korea.
Approval was obtained from the Committees for Human Research at participating centers, as well as from the Research Committee of the SDSG. Adults with lumbosacral (L5-S1) spondylolisthesis were retrospectively reviewed. Only patients with spondylolisthesis were evaluated. No patients had other spinal pathology, including adolescent idiopathic scoliosis. No patient had previous surgery. Health-related quality of life outcome measurements included: Short Form–12 version 2 (SF-12v2) and the Scoliosis Research Society–30 (SRS-30) surveys. The SF-12v2 contains 2 subscores: the mental component score (MCS) and the physical component score (PCS). The SRS-30 has a total score and component subscores based on function/activity, pain, self-image/appearance, mental health, and satisfaction with management.
Preoperative radiographic analyses were obtained from full-length anteroposterior (AP) and lateral spine radiographs. Radiographic measurements were performed using Surgimap, (Nemaris, Inc, New York, NY, USA). Measured parameters included C7 sagittal vertical axis deviation (SVA: distance from the posterior-superior corner of S1 to the C7 plumb line), T1 pelvic angle (T1PA: angle subtended by a line from the femoral heads to the center of the T1 vertebral body and a line from the femoral heads to the center of the superior sacral end plate),10 thoracic kyphosis (TK: angle between T5’s superior and T12’s inferior endplates), lumbar lordosis (LL: angle between S1’s endplate and T12’s inferior endplate), pelvic tilt (PT: angle between a vertical line and a line through the midpoint of the sacral endplate to the axis of femoral heads), pelvic incidence (PI: angle between a line perpendicular to the midpoint of the sacral endplate and a line through the midpoint of the sacral endplate to the axis of femoral heads), sacral slope (SS: angle made between a horizontal line and S1’s endplate), slip angle (angle between a line along the inferior endplate of L5 and a line perpendicular to the posterior aspect of the S1 body), and Meyerding slip grades (percent of anterolisthesis of L5 on S1; ie, grade 1, 0%-25%; grade 2, 25%-50%; grade 3, 50%-75%; grade 4, 75%-100%; grade 5, >100%).13 The Labelle classification for each patient was also defined.14,15
Statistical Analysis
Secondary analysis using linear regression was performed to determine the association between spondylolisthesis grade and HRQoL. Because of sample size restrictions, only main effects models were considered, with no covariates included. Furthermore, Pearson’s correlation coefficients were also calculated to assess linear correlation between spondylolisthesis grade (low, Meydering ≤2; high, Meydering ≥3) and HRQoL scores. A P value <.05 defined statistical significance. Statistics were conducted using STATA 13 (, StataCorp LP, College Station, TX, USA).
Results
Forty-five patients were analyzed (male 15, female 30; average age 40.5 ± 18.7 years; 14 low-grade, 31 high-grade). Patient demographics, radiographic measurements, and HRQoL scores are presented in Table 1. Patients with high-grade slips were significantly younger and had significantly greater slip angles and less thoracic kyphosis than patients with low-grade slips (Table 1). In both groups, average lumbopelvic parameters were abnormal, as average PI was 80°, average PT = 30°, and average LL was >60°. Average SVAs for the entire cohort and for each group were <3 cm. For patients with low-grade and high-grade slips, general health status (average PCS 36.4, average MCS 47.9) was on average below the national mean.16 SF-12 PCS scores were on average 11 points lower than SF-12 MCS scores for the entire cohort and for both groups. Average SRS-30 scores were ≤3 for all SRS-30 domains, except for the mental domain (3.4 ± 0.9). Average scores for the SF-12 PCS/MCS scores and all SRS-30 domains were not statistically different between patients with low- and high-grade slips.
Table 1.
Patient Demographics, Deformity Classification, and Radiographic Sagittal Parameters for Adults With Low-Grade and High-Grade Lumbosacral Spondylolisthesis.
| Total | Low Grade (Meyerding ≤2) | High Grade (Meyerding ≥3) | P | |
|---|---|---|---|---|
| N | 45 | 14 | 31 | n/a |
| Age, years | 40.5 ± 18.7 | 51.9 ± 17.6 | 35.3 ± 16.9 | <.01 |
| Gender | ||||
| Male | 15 | 5 | 10 | |
| Female | 30 | 9 | 21 | |
| Meydering grade | ||||
| 1 | 0 | 0 | n/a | n/a |
| 2 | 14 | 14 | n/a | n/a |
| 3 | 20 | n/a | 20 | n/a |
| 4 | 9 | n/a | 9 | n/a |
| 5 | 2 | n/a | 2 | n/a |
| Labellea | ||||
| 1 | 0 | 0 | n/a | n/a |
| 2 | 1 | 1 | n/a | n/a |
| 3 | 12 | 12 | n/a | n/a |
| 4 | 16 | n/a | 16 | n/a |
| 5 | 13 | n/a | 13 | n/a |
| 6 | 1 | n/a | 1 | n/a |
| Radiographic | ||||
| PI | 79.6 ± 10.7 | 79.4 ± 11.0 | 79.7 ± 10.7 | .94 |
| SS | 50.7 ± 10.3 | 49.5 ± 9.2 | 51.2 ± 10.9 | .63 |
| PT | 29.5 ± 6.2 | 29.9 ± 6.6 | 29.2 ± 6.2 | .74 |
| LL | 66.6 ± 16.0 | 62.2 ± 16.9 | 68.7 ± 15.4 | .21 |
| TK | 44.5 ± 11.0 | 49.5 ± 8.2 | 42.2 ± 11.4 | .04 |
| SVA | 26.0 ± 51.4 | 20.2 ± 55.3 | 28.7 ± 50.4 | .61 |
| Slip angle | 5.5 ± 14.5 | −4.26 ± 7.8 | 9.8 ± 14.7 | <.01 |
| T1PA | −5.7 ± 3.9 | −5.9 ± 4.4 | −5.6 ± 3.7 | .83 |
| Outcomes | ||||
| SF-12 | ||||
| PCS | 36.4 ± 8.1 | 34.4 ± 8.8 | 37.3 ± 7.6 | .28 |
| MCS | 47.9 ± 11.5 | 46.5 ± 10.4 | 48.5 ± 24.4 | .58 |
| SRS-30 | ||||
| Pain | 2.5 ± 0.8 | 2.2 ± 0.6 | 2.6 ± 0.8 | .08 |
| Appearance | 2.9 ± 0.7 | 3.0 ± 0.9 | 2.8 ± 0.6 | .55 |
| Activity | 2.9 ± 0.8 | 2.7 ± 0.9 | 3.0 ± 0.8 | .19 |
| Mental health | 3.4 ± 0.9 | 3.3 ± 0.9 | 3.5 ± 0.9 | .46 |
| Subscore | 2.9 ± 0.6 | 2.8 ± 0.7 | 3.0 ± 0.6 | .29 |
| Satisfaction | 3.0 ± 1.3 | 3.0 ± 1.5 | 3.0 ± 1.3 | .84 |
| Total | 2.9 ± 0.6 | 2.8 ± 0.7 | 3.0 ± 0.6 | .37 |
Abbreviations: n/a, not applicable; PI, pelvic incidence; SS, sacral slope; PT, pelvic tilt; LL, lumbar lordosis; TK, thoracic kyphosis; SVA, C7 sagittal vertical axis deviation; T1PA, T1 pelvic angle; SF-12 PCS, Short Form–12 physical component score; SF-12 MCS, Short Form–12 mental component score.
aTwo patients without Labelle classification.
For low-grade slips, SVA had strong negative correlations with SF-12 MCS (r = −0.57; P < .05), SRS-30 appearance (r = −0.60; P < .05), SRS-30 mental (r = −0.58; P < .05), and SRS-30 satisfaction (r = −0.53; P < .05). PI had strong negative correlations with SRS-30 total (r = −0.57; P < .05), SRS-30 mental (r = −0.53; P < .05), and SRS-30 total (r = −0.57; P < .05). SS also had a strong negative correlation with SF-12 MCS (r = −0.61; P = .02), while thoracic kyphosis had a strong positive correlation with SRS-activity (r = 0.62; P = .02).
For high-grade slips, the slip angle had a moderate negative correlation with SF-12 MCS (r = −0.36; P = .05). SVA had strong negative correlations with SF-12 PCS (r = −0.48; P < .05), SRS-30 appearance (r = −0.48; P < .05), SRS-30 activity domains (r = −0.45; p < .05) and a moderate negative correlation with SRS-30 total (r = −0.37; P < .05). T1PA had a moderate negative correlation with SF-12 PCS (r = −0.37; P < .05) and SRS-30 appearance (r = −0.36; P < .05). SS had a negative moderate correlation with SRS-mental (r = −0.36; P = .05). Thoracic kyphosis had negative correlations with SF-12 PCS (r = −0.35, P = .01) and SRS satisfaction (r = −0.49; P = .01).
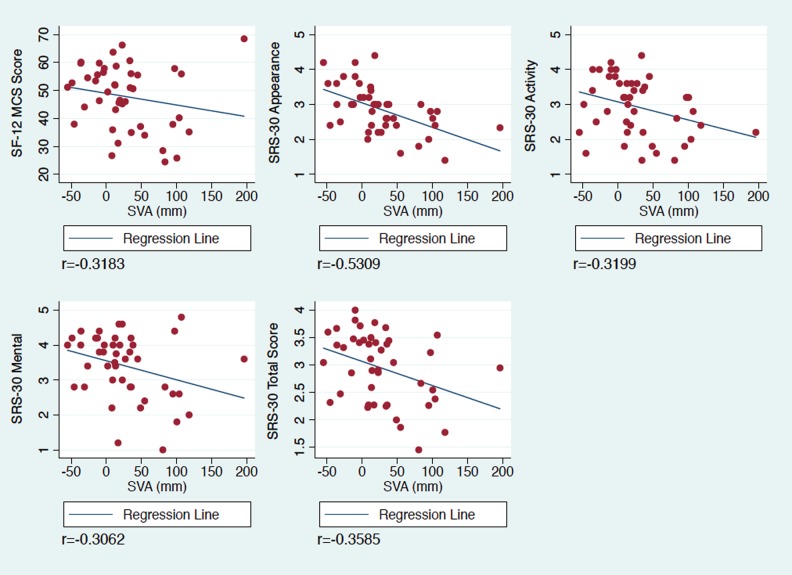
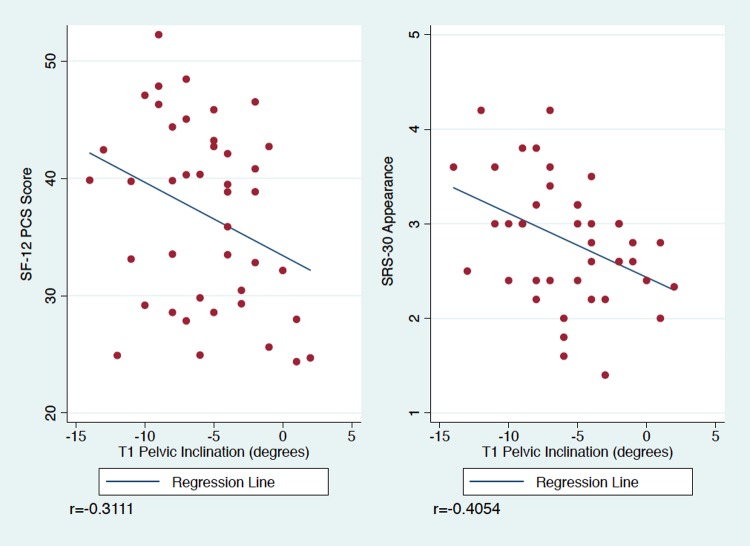
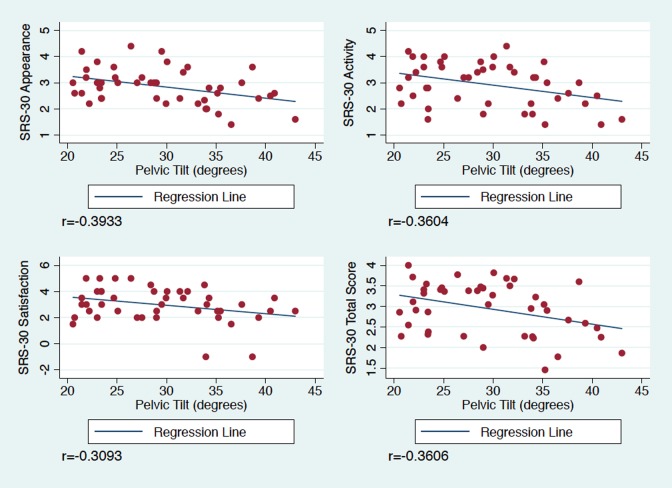
Linear regression analyses are presented in Tables 2 and 3 and Figures 1, 2, and 3. For every 1-cm increase in SVA, there was a 0.5-point decrease in SF-12 PCS, 0.07-point decrease in SRS appearance, 0.05-point decrease in SRS activity, 0.05-point decrease in SRS Mental, 0.04-point decrease in SRS total scores (P < .05 for all) (Figure 1). For every 1° increase in the T1 pelvic angle, there was a 0.63-point decrease in SF-12 PCS and 0.07-point decrease in SRS appearance (P < .05) (Figure 2). For every 1° increase in PT, there was a 0.04-point decrease in SRS appearance, 0.05-point decrease in SRS activity, 0.06-point decrease in SRS satisfaction, and 0.04-point decrease in SRS total score (P < .05) (Figure 3). There were no significant associations between slip angle or slip grade and the SF-12 and SRS-30 domain scores.
Table 2.
Main Effects Linear Regression Analysis Between SF-12 Scores and Radiographic Parameters and Labelle Classification Types.
| SF-12 | ||||
|---|---|---|---|---|
| MCS | P | PCS | P | |
| Labelle 2-4 vs 5-6 | 0.199 | .957 | 3.09 | .229 |
| Labelle 2-3 vs 5-6 | Failed due to collinearity | |||
| PT | −0.362 | .195 | −0.194 | .329 |
| SVA | −0.042 | .221 | −0.05 | .035 |
| T1PA | 0.004 | .994 | −0.625 | .045 |
| Slip angle | −0.195 | .118 | 0.029 | .732 |
| Slip grade | −0.271 | .897 | 0.334 | .822 |
Abbreviations: PT, pelvic tilt; SVA, C7 sagittal vertical axis deviation; T1PA, T1 pelvic angle; SF-12, Short Form–12; PCS, physical component score; MCS, mental component score.
Table 3.
Main Effects Linear Regression Analysis Between SRS-30 Domains and Radiographic Parameters and Labelle Classification Types.
| SRS-30 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pain | P | Appearance | P | Activity | P | Mental | P | Satisfaction | P | Total Score | P | |
| Labelle 2-4 vs 5-6 | 0.327 | .189 | 0.185 | .394 | 0.349 | .185 | 0.443 | .126 | −0.161 | .702 | 0.296 | .138 |
| Labelle 2-3 vs 5-6 | Failed due to collinearity | |||||||||||
| PT | −0.02 | .297 | −0.042 | .008 | −0.048 | .016 | −0.038 | .087 | −0.064 | .041 | −0.036 | .016 |
| SVA | −0.002 | .496 | −0.007 | <.0001 | −0.005 | .034 | −0.005 | .043 | 0.0001 | .98 | −0.004 | .017 |
| T1PA | −0.018 | .58 | −0.068 | .008 | −0.038 | .271 | −0.037 | .315 | 0.008 | .879 | −0.038 | .132 |
| Slip angle | 0.003 | .69 | −0.005 | .503 | −0.005 | .552 | −0.007 | .494 | −0.001 | .926 | −0.004 | .595 |
| Slip grade | 0.039 | .788 | −0.063 | .614 | 0.088 | .562 | 0.005 | .976 | 0.032 | .896 | 0.009 | .939 |
Abbreviations: PT, pelvic tilt; SVA, C7 sagittal vertical axis deviation; T1PA, T1 pelvic angle; SRS, Scoliosis Research Society.
Figure 1.
Significant linear regression analyses for sagittal vertical axis (SVA) and health-related quality of life outcome scores in adults with lumbosacral spondylolisthesis. SVA = sagittal vertical axis; MCS = mental component score; SRS = Scoliosis Research Society.
Figure 2.
Significant linear regression analyses for T1 pelvic angle/inclination and health-related quality of life outcome scores in adults with lumbosacral spondylolisthesis. PCS = physical component score; SRS = Scoliosis Research Society.
Figure 3.
Significant linear regression analyses for pelvic tilt and health-related quality of life outcome scores in adults with lumbosacral spondylolisthesis. PCS = physical component score; SRS = Scoliosis Research Society.
Discussion
We present the first study to assess the impact of global sagittal alignment and lumbosacral parameters on functional health status in unoperated adults with lumbosacral (L5-S1) isthmic spondylolisthesis. Noteworthy findings of this investigation are that adults with low- and high-grade isthmic spondylolisthesis have abnormal lumbopelvic parameters and sagittal alignment as well as compromised general health (SF-12) and SRS-30 scores. Additionally, several radiographic parameters of sagittal malalignment (ie, C7 SVA, T1PA) are negatively correlated with SF-12 MCS scores and multiple domains of the SRS-30 survey. Furthermore, progressively more severe sagittal malalignment is associated with worse physical and psychological disability. While our findings are unique, they are consistent with previous literature regarding the relationship between the sagittal profile and HRQoL scores in children and adolescents with isthmic spondylolisthesis.5–7,17
Sacral sagittal malalignment is a hallmark of lumbosacral spondylolisthesis that has been proposed to directly influence the development and progression of the disorder.1–4 In a retrospective study of 214 subjects with L5-S1 spondylolisthesis, Labelle et al1 found that average PI (71.6° ± 7.7°) was significantly greater in subjects with spondylolisthesis than the control subjects. Additionally, Roussouly et al2 demonstrated that patients with lumbosacral spondylolysis/low-grade spondylolisthesis had significantly higher PI (average 65.5°) than the control population (average 51.9°). Our cohort was no exception, as the average value for PI was 80°, although there were no statistical differences in average values between patients with low- and high-grade slips.
As sagittal malalignment is an inevitable phenomenon of increased PI, patients with lumbosacral spondylolisthesis attempt to maintain an acceptable upright posture by increasing lumbar lordosis, decreasing thoracic kyphosis, and retroverting the pelvis.1,2,18–20 In the aforementioned study by Labelle et al,1 the average SS (49.4° ± 5.9°), PT (22.2° ± 6.3°), and LL (42.7° ± 5.4°) were significantly greater in the subjects with spondylolisthesis than the control subjects and that the differences noted between the 2 groups increased linearly as spondylolisthesis severity increased. In the study by Roussouly et al,2 the patients with lumbosacral spondylolysis/low-grade spondylolisthesis had significantly higher LL (70.8°) than the control population (average 61.4°). In our cohort, abnormal lumbopelvic parameters were also present (SS 20°; PT 30°; LL > 60°). As these compensatory mechanisms to maintain sagittal alignment require significant energy expenditure, they may cause notable disability. In our cohort, average SF-12 scores (PCS 36.4, MCS 47.9) were below the national mean16 and average SRS-30 scores were ≤3 in all domains, except for the mental domain (3.4 ± 0.9). Interestingly, our linear regression analysis demonstrated that for every 1° increase in PT, there was a 0.04-point decrease in SRS appearance, 0.05-point decrease in SRS activity, 0.06-point decrease in SRS satisfaction, and 0.04-point decrease in the SRS total scores (P < .05).
Lumbosacral kyphosis also contributes to lumbopelvic mismatch in patients with lumbosacral spondylolisthesis. Previous studies on children and adolescents with lumbosacral spondylolisthesis have demonstrated that the slip angle is correlated with worse functional outcome scores.6,7,17 In patients treated nonoperatively and operatively for high-grade lumbosacral spondylolisthesis, Lundine et al17 reported that a more kyphotic slip angle was associated with worse SRS-30 scores. In a retrospective study of adolescents with lumbosacral spondylolisthesis (67 low-grade, 29 high-grade), Tanguay et al6 found that slip angle was significantly correlated with SF-12 PCS scores (r = −0.55) and that correlations were even stronger (r = −0.62) for patients with high-grade slips. In our study, we found that slip angle had a moderate negative correlation with SF-12 MCS (r = −0.36) in patients with high-grade slips. There were no significant correlations between the slip angle and HRQoL scores of low-grade slip or SRS-scores in either group. This difference may be a result of our average slip angle of 9.8° in patients with a high-grade slip, while a value of 30° was associated with an increased proportion of subjects with poor SF-12 PCS scores in the study by Tanguay et al.6
When sagittal balance cannot be maintained by compensatory mechanisms, sagittal decompensation ensues. In adults with spinal deformity and children and adolescents with spinal lumbosacral spondylolisthesis, sagittal imbalance has consistently been associated with poor HRQoL scores.5,8,9,12 In a retrospective study of 149 children and adolescents with lumbosacral spondylolisthesis, Harroud et al5 reported that the SRS-22 total score was significantly correlated (r = −0.35) with C7 SVA deviation in patients with high-grade slips. We too found that in patients with high-grade slips C7 SVA deviation correlated with worse HRQoL scores, including SF-12 PCS and 3 domains of SRS-30 (appearance, activity, total). Our linear regression analysis of C7 SVA demonstrated that for every 1-cm increase in SVA, there was a 0.5 point decrease in SF12-PCS, 0.07 decrease in SRS appearance, 0.05 decrease in SRS activity, 0.05 decrease in SRS mental, and 0.04 decrease in SRS total scores. In contrast to Harroud et al,5 we found that C7 SVA negatively correlated with SF-12 MCS and SRS-30 appearance, mental, and satisfaction domains in patients with low-grade slips. This difference may be attributable to the fact that different SRS surveys were evaluated (SRS-22 vs SRS-30) or that deformity-specific scores in our adult cohort with low-grade slips were worse (average SRS-30 scores ≤3.4) than in their children with low-grade slips (average SRS-22 scores ≥3.89).5 It should be noted that these associations between SVA and HRQoL are from relatively young patient populations (average age 41 years in our study). As such, our data does not provide insight into the unclear relationship between SVA and HRQoL scores in more elderly patients (ie, >70 years).
In addition to the C7 SVA, the T1 pelvic angle has been correlated with HRQoL scores in patients with adult spinal deformity.10 In our study, the T1PA was found to have a moderate negative correlation with SF-12 PCS and SRS-30 appearance scores. Our linear regression also demonstrated that for every 1° increase in T1PA, there was a 0.63-point decrease in SF-12 PCS and a 0.07-point decrease in SRS appearance (P < .05).
As surgical correction of slip angle and lumbopelvic and global sagittal malalignment in children with high-grade lumbosacral isthmic spondylolisthesis has been recommended,21–25 our correlations between impaired HRQoL scores and sagittal malalignment (C7 SVA, T1PA) and pelvic retroversion suggest that surgical correction of lumbopelvic deformity in adults with lumbopelvic isthmic spondylolisthesis may also be beneficial. However, as we do not present data regarding clinical or radiographic outcomes after surgical intervention in our cohorts, this theoretical speculation should be confirmed by future multicenter, prospective investigations.
Our findings should also be considered in the context of the study’s limitations. It is a retrospective analysis of a heterogeneous multicenter database that introduces variability for which we are unable to control. For example, the type of previous nonoperative management each patient received is not known and may have influenced how patients responded to the SRS-30 questionnaire. We are also unable to ascertain other patient demographic information (ie, medical and psychiatric comorbidities) that may have influenced survey responses. Another limitation is the use of an older version of the SRS questionnaire (SRS-30), which includes several questions that require recall and have been subsequently removed. Furthermore, our small sample sizes, particularly Labelle 6, precluded more robust statistical analyses and impeded us from drawing stronger conclusions. The use of main effect linear regression models may overestimate the true effects found in this study due to inability to adjust for potential confounding factors. Nevertheless, the results of this study provide a unique new framework that may facilitate a more accurate preoperative shared decision making process with adults with lumbosacral spondylolisthesis.
Conclusion
Lumbosacral isthmic spondylolisthesis in adults negatively impacts mental and physical HRQoL. While HRQoL are similar between patients with low- and high-grade slips, multiple global and local radiographic sagittal parameters negatively affect HRQoLs for both groups. Thus, improvement of sagittal parameters, particularly global sagittal alignment, is an important goal of surgery for adults with lumbosacral spondylolisthesis.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Labelle H, Roussouly P, Berthonnaud E, et al. Spondylolisthesis, pelvic incidence, and spinopelvic balance: a correlation study. Spine (Phila Pa 1976). 2004;29:2049–2054. [DOI] [PubMed] [Google Scholar]
- 2. Roussouly P, Gollogly S, Berthonnaud E, Labelle H, Weidenbaum M. Sagittal alignment of the spine and pelvis in the presence of L5-S1 isthmic lysis and low-grade spondylolisthesis. Spine (Phila Pa 1976). 2006;31:2484–2490. [DOI] [PubMed] [Google Scholar]
- 3. Jackson RP, Phipps T, Hales C, Surber J. Pelvic lordosis and alignment in spondylolisthesis. Spine (Phila Pa 1976). 2003;28:151–160. [DOI] [PubMed] [Google Scholar]
- 4. Hu SS, Tribus CB, Diab M, Ghanayem AJ. Spondylolisthesis and spondylolysis. Instr Course Lect. 2008;57:431–445. [PubMed] [Google Scholar]
- 5. Harroud A, Labelle H, Joncas J, Mac-Thiong J. Global sagittal alignment and health-related quality of life in lumbosacral spondylolisthesis. Eur Spine J. 2013;22:849–856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Tanguay F, Labelle H, Wang Z, Joncas J, de Guise JA, Mac-Thiong JM. Clinical significance of lumbosacral kyphosis in adolescent spondylolisthesis. Spine (Phila Pa 1976). 2012;37:304–308. [DOI] [PubMed] [Google Scholar]
- 7. Tanguay F, Mac-Thiong JM, Wang Z, Joncas J, De Guise JA, Labelle H. Developmental spondylolisthesis: is slip angle related to quality of life? Stud Health Technol Inform. 2010;158:182–185. [PubMed] [Google Scholar]
- 8. Glassman SD, Berven S, Bridwell K, Horton W, Dimar JR. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine (Phila Pa 1976). 2005;30:682–688. [DOI] [PubMed] [Google Scholar]
- 9. Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F. The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976). 2005;30:2024–2029. [DOI] [PubMed] [Google Scholar]
- 10. Protopsaltis T, Schwab F, Bronsard N, et al. The T1 pelvic angle, a novel radiographic measure of global sagittal deformity, accounts for both spinal inclination and pelvic tilt and correlates with health-related quality of life. J Bone Joint Surg Am. 2014;96:1631–1640. [DOI] [PubMed] [Google Scholar]
- 11. Takemoto M, Boissière L, Novoa F, et al. Sagittal malalignment has a significant association with postoperative leg pain in adult spinal deformity patients. Eur Spine J. 2016;25:2442–2451. [DOI] [PubMed] [Google Scholar]
- 12. Mac-Thiong JM, Transfeldt EE, Mehbod AA, et al. Can C7 plumbline and gravity line predict health-related quality of life in adult scoliosis? Spine (Phila Pa 1976). 2009;34:E519–E527. [DOI] [PubMed] [Google Scholar]
- 13. Meyerding H. Spondylolisthesis. Surg Gynecol Obstet. 1932;54:371–377. [Google Scholar]
- 14. Labelle H, Mac-Thiong JM, Roussouly P. Spino-pelvic sagittal balance of spondylolisthesis: a review and classification. Eur Spine J. 2011;20(suppl 5):641–646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mac-Thiong JM, Labelle H. A proposal for a surgical classification of pediatric lumbosacral spondylolisthesis based on current literature. Eur Spine J. 2006;15:1425–1435. [DOI] [PubMed] [Google Scholar]
- 16. The SF-12 Health Survey–PCS and MCS scores. http://www.outcomes-umassmed.org/ALS/sf12.aspx. Accessed April 14, 2015.
- 17. Lundine K, Lewis S, Al-Aubaidi Z, Alman B, Howard A. Patient outcomes in the operative and nonoperative management of high-grade spondylolisthesis in children. J Pediatr Orthop. 2014;34:483–489. [DOI] [PubMed] [Google Scholar]
- 18. Barrey C, Roussouly P, Le Huec J, D’Acunzi G, Perrin G. Compensatory mechanisms contributing to keep the sagittal balance of the spine. Eur Spine J. 2013;22(suppl 6):S834–S841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lafage V, Schwab F, Patel A, Hawkinson N, Farcy J. Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine (Phila Pa 1976). 2009;34:E599–E606. [DOI] [PubMed] [Google Scholar]
- 20. Kobayashi T, Atsuta Y, Matsuno T, Takeda N. A longitudinal study of congruent sagittal spinal alignment in an adult cohort. Spine (Phila Pa 1976). 2004;29:671–676. [DOI] [PubMed] [Google Scholar]
- 21. Boachie-Adjei O, Do T, Rawlins BA. Partial lumbosacral kyphosis reduction, decompression, and posterior lumbosacral transfixation in high-grade isthmic spondylolisthesis: clinical and radiographic results in six patients. Spine (Phila Pa 1976). 2002;27:E161–E168. [DOI] [PubMed] [Google Scholar]
- 22. Mac-Thiong JM, Wang Z, de Guise JA, Labelle H. Postural model of sagittal spino-pelvic alignment and its relevance for lumbosacral developmental spondylolisthesis. Spine (Phila Pa 1976). 2008;33:2316–2325. [DOI] [PubMed] [Google Scholar]
- 23. Labelle H, Roussouly P, Chopin D, Berthonnaud E, Hresko T, O’Brien M. Spino-pelvic alignment after surgical correction for developmental spondylolisthesis. Eur Spine J. 2008;17:1170–1176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hresko M, Labelle H, Roussouly P, Berthonnaud E. Classification of high-grade spondylolistheses based on pelvic version and spine balance: possible rationale for reduction. Spine (Phila Pa 1976). 2007;32:2208–2213. [DOI] [PubMed] [Google Scholar]
- 25. Longo U, Loppini M, Romeo G, Maffulli N, Denaro V. Evidence-based surgical management of spondylolisthesis: reduction or arthrodesis in situ. J Bone Joint Surg Am. 2014;96:53–58. [DOI] [PubMed] [Google Scholar]