Abstract
Background:
The group of passive prostheses consists of prosthetic hands and prosthetic tools. These can either be static or adjustable. Limited research and development on passive prostheses has been performed although many people use these prosthesis types. Although some publications describe passive prostheses, no recent review of the peer-reviewed literature on passive prostheses is available.
Objective:
Review the peer-reviewed literature on passive prostheses for replacement of the hand.
Study design:
Literature review.
Methods:
Four electronic databases were searched using a Boolean combination of relevant keywords. English-language articles relevant to the objective were selected.
Results:
In all, 38 papers were included in the review. Publications on passive prosthetic hands describe their users, usage, functionality, and problems in activities of daily living. Publications on prosthetic tools mostly focus on sport, recreation, and vehicle driving.
Conclusion:
Passive hand prostheses receive little attention in prosthetic research and literature. Yet one out of three people with a limb deficiency uses this type of prosthesis. Literature indicates that passive prostheses can be improved on pulling and grasping functions. In the literature, ambiguous names are used for different types of passive prostheses. This causes confusion. We present a new and clear classification of passive prostheses.
Clinical relevance
This review provides information on the users of passive prosthetic hands and tools, their usage and the functionality. Passive prostheses receive very little attention and low appreciation in literature. Passive prosthetic hands and tools show to be useful to many unilateral amputees and should receive more attention and higher acceptance.
Keywords: Upper limb, prosthesis, passive, cosmetic, hand, tool, adaptation, static, adjustable
Background
Classification of passive prostheses
The wide range of prostheses for replacement of the hand can be divided into active and passive prostheses. The force to control the grasping mechanism of active prostheses is applied to this mechanism internally, for example, by an electric actuator or a body-powered cable. In passive prosthesis, the force to adjust the grasping mechanism is applied externally, for example, by the sound hand.
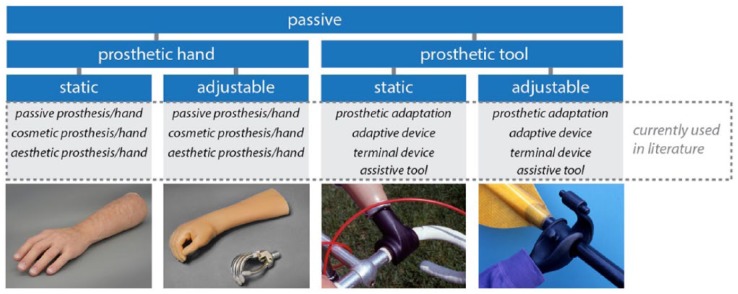
There are various types of passive prostheses. In the current literature, different terms are used for the same type of device, and often the same name is used for different types of passive devices. As a result, it is often unclear which type of device is discussed. To avoid any confusion in this literature review, we present a new and clear classification for passive prosthetic devices in Figure 1. The group of passive prostheses for replacement of the hand consists of prosthetic hands and prosthetic tools. Prosthetic hands offer a lifelike appearance and are used for a variety of activities.5 Prosthetic tools have a mechanical appearance and are mostly designed for one specific activity which needs to be performed two-handedly.6 Some prosthetic tools, such as a passive prosthetic hook, can be used for a variety of activities.2
Figure 1.
New classification of passive prostheses for replacement of the hand, along with their multiple different names used in current literature.
Source: Adapted from APC Prosthetics,3 Plettenburg,1 Myrdal Orthopedics,4 TRS Prosthetics.2
Both passive prosthetic types can either be static or adjustable. Static prostheses cannot be moved at all.7 Adjustable prostheses feature an adjustable grasping mechanism or parts of the prosthesis can be adjusted to multiple orientations (not taking into account the orientation of the wrist). Adjusting of the prosthesis is performed by the sound hand or by pushing the prosthesis against the environment.1 Using this classification, we can make a clear distinction between different passive devices, for example, between a static (passive) prosthetic hand or tool and an adjustable (passive) prosthetic hand or tool.
Problem statement
Very limited research has been dedicated to passive prostheses.8 The working principle of most of the available devices has not changed for half a century. The current available passive prostheses therefore seem to be underdeveloped relative to active prostheses. Many people though use passive prostheses.5,9–13 Passive prostheses have proved to be useful for many people with an upper limb deficiency.7 The limited research and developments on passive prostheses are therefore very remarkable and more research on these prostheses is required. Clear directions for improvement need to be identified.
Although some publications and books, such as the Atlas of Limb Prosthetics14 and Otto Bock prothesen-kompendium,15 describe passive prostheses, no recent review of the peer-reviewed literature on passive prostheses is available.
Objective
The objective of this literature research is to review the peer-reviewed literature on passive prostheses for replacement of the hand and to identify future research directions for the development of new technologies for passive prostheses.
Methods
Search query
In February 2016, a literature search was performed through a search of OvidSP (Inspec and Ovid MEDLINE), PubMed, Scopus, and Web of Science (WoS) using the following Boolean combination of keywords: (prosthesis OR prostheses) AND ((upper limb) OR (upper extremity)) AND ((function AND cosmetic) OR passive OR assistive OR adaptations OR appearance). This search query is visualized in Figure 2. Search results were limited to the English language and no time restrictions were imposed.
Figure 2.
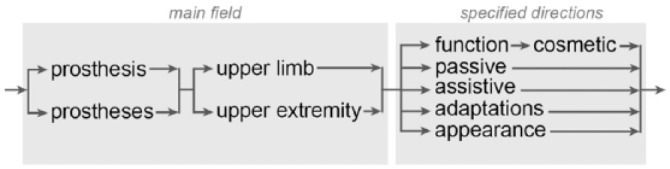
Search query visualization.
Selection criteria
Inclusion criteria
Articles focusing on one of the following topics were included in the review process: design, use, or satisfaction of (1) passive prosthetic hands, (2) passive prosthetic tools, or (3) the appearance of prostheses for replacement of the hand.
Criteria application
The selection criteria were applied to the titles and abstracts of the articles. In a few cases, the discussed type of prosthesis was not clearly stated in the title or abstract. In order to apply the selection criteria, the main text was scanned to obtain this information. No additional quality check was performed as only studies appearing in peer-review journals were included.
Results
Search results
Execution of the search query resulted in 655 articles distributed among the four databases. Removal of the overlap between databases resulted in approximately 360 unique articles. Application of the selection criteria decreased the number of articles to 30. The citations of these 30 articles, which were available in the aforementioned databases, were examined similarly. This resulted in eight more articles. In total, 38 articles were selected for inclusion in the review process as depicted in Figure 3.
Figure 3.
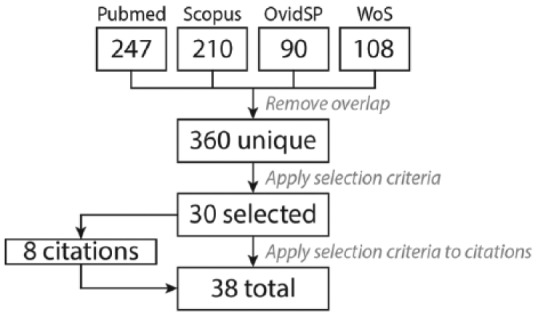
Search method flow chart: number of articles.
In the selected literature, prosthetic hands and prosthetic tools are not subdivided in static and adjustable prostheses. Inevitably, the results in this review do not present the information on static and adjustable prostheses separately.
The 38 selected articles are based on multiple methods and study designs: 17 articles are based on user studies (n = 2367 total) of which the majority is performed using a questionnaire. Three articles7,16,17 are based on the experience of the authors and their evaluation of the fitting of prostheses to patients (n = 7847 total). Two articles1,18 describe the design of a specific prosthesis and six articles8,19–23 are reviews which include passive prostheses. These six articles are either dated, do not provide a clear review of the peer-reviewed literature on passive hand prostheses, or do not indicate clear directions for improvement of passive devices. The remaining 10 articles range from general descriptions of prostheses to evaluations of prosthetic appearance.
Passive prosthetic hands
User aspects
Prosthetic users choose either an active or a passive prosthesis. Table 1 shows the percentage of users who use a passive prosthetic hand in multiple unique studies. The value for the “potential prosthetic hand users” is the sum of all respondents who use, or could use, a prosthetic hand. From these respondents, the number and percentage of passive prosthetic hand users are determined. Table 1 does not include review studies. The percentage of users of passive hands ranges from 13% up to 64%. On average, about one out of three potential prosthetic hand users uses a passive prosthesis.
Table 1.
Number of respondents who primarily use a passive prosthetic hand in multiple studies.
| Article (authors, year) | Method | Potential prosthetic hand users | Passive prosthetic hand users | Percentage |
|---|---|---|---|---|
| Kejlaa,24 1993 | Visit, questionnaire | 66 | 16 | 24 |
| Burger and Marinček,9 1994 | Questionnaire | 266 | 169 | 64 |
| Gaine et al.,12 1997 | Questionnaire | 55 | 16 | 29 |
| Fraser,5 1998 | Video analysis | 66 | 38 | 58 |
| Crandall and Tomhave,13 2002 | Questionnaire | 34 | 15 | 44 |
| Datta et al.,11 2004 | Questionnaire, medical records | 60 | 38 | 63 |
| Shida-Tokeshi et al.,25 2005 | Hospital chart review | 298 | 38 | 13 |
| Biddiss et al.,26 2007 | Questionnaire | 242 | 51 | 21 |
| Kyberd et al.,10 2007 | Questionnaire | 117 | 68 | 58 |
| Østlie et al.,27 2012 | Questionnaire, clinical tests, survey | 224 | 40 | 18 |
| Total | 1428 | 489 | 34 | |
| Ratio potential/passive users | 2.9 | 1.0 |
In this table, only original studies are presented, no reviews were included in the table.
Active prostheses generally provide more functional features than passive prostheses.24 Active prostheses are therefore often seen as a better solution for people with an upper limb deficiency. These prostheses are however harder to control.28 Young children and recent amputees are often prescribed a passive prosthetic hand which is relatively easy to use.17 After a period of familiarization, these people are expected to adopt an active prosthesis.3,26,29,30
Users of passive prostheses are, however, not merely young people or recent amputees. Kejlaa24 (16 passive users) and Burger and Marinček9 (169 passive users) found that the users of passive prostheses are older persons with a longer time-lapse since amputation. Kejlaa24 thereby states that with time people change from active to passive prostheses.
Biddiss et al.26 conclude that gender is not statistically associated with the type of prosthesis worn, based on a study which included users of both active and passive prostheses.
User motivations
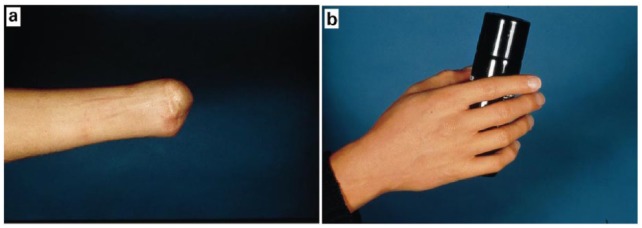
Users of passive prosthetic hands mostly rank appearance and comfort at the forefront.2,26,31 An example of a passive prosthetic hand which provides a natural appearance is shown in Figure 4. People with an upper limb deficiency often see both active and passive prostheses primarily as a cosmetic aid.9 As passive hand prostheses are prescribed primarily with a lifelike appearance and higher comfort than active prostheses, these may be preferable to active prostheses.9,11,27 Passive prosthetic hands are mostly used in social occasions17,28 as they enhance self-image and self-confidence.29,31 Passive prosthetic hands offer psychological and functional advantages.16,23 A passive prosthetic hand also enhances the rehabilitation of the user as it helps to forget the handicap and permits the user to have a professional and social life.20
Figure 4.
Traumatic amputation of the whole hand, a proximal amputation (a) without and (b) with passive prosthetic hand.
Source: Adapted from Pillet and Didierjean-Pillet.17
Usage
Biddiss et al.26 rank the importance of functional roles according to users of passive prosthetic hands: appearance, steadying, manipulating, gripping, and body language. The function of passive prostheses may be perceived as an additional passive support or as an instrument of social function and an aid to the patient.17,27 The studies of Fraser5 and Van Lunteren et al.32 reveal that the grasping function of adjustable hand prostheses is sometimes used by the user. The study of Fraser5 shows that the number of actions made for each non-manipulative activity with passive hands did not differ significantly from active hands, with exception of pull actions which were found to be difficult with a passive hand.
Views in literature on functionality
The reviewed literature describes two views on the functionality of passive prosthetic hands. The first view describes these passive prostheses as non-functional prostheses. Kejlaa24 states that users of active prosthetic hands have a superior performance over users of passive prosthetic hands in activities of daily living (ADLs). The fitting of active prostheses therefore is a “worthy effort.” The use of passive prostheses is sometimes even considered a “prosthetic failure”12 or the user may be classed as an “unsuccessful prosthetic user.”33 On the contrary, the second view describes passive prostheses as functional prostheses. Pillet,7 Fraser,5 and Crandall and Tomhave13 conclude that passive prosthetic hands are used functionally in multiple activities. Kyberd et al.10 argue that the frequency of need for repair and the failures that occur with passive prosthetic hands are an indication of the devices being actively used.
According to Beasley and colleagues,19,34 there is a tremendous overestimation of the physical impairment of people with an upper limb deficiency while the total impact on the individual is often neglected. They state that about 90% of the ADLs can be accomplished using the sound hand and the other 10% with a little extra effort. This statement is, however, not based on any presented data or evidence and seems to be based on an estimation made by the authors. Multiple statements and findings of others may though support this estimation. Crandall and Tomhave13 state that it has been said that prosthetic fitting on a person with one sound limb is unnecessary as we are all born with an “abundance” of arms. Neither of the statements is supported by evidence. Østlie et al.27 (n = 224) and Vasluian et al.6 (n = 218) report that people with an upper limb deficiency often prefer the use of both the unaffected and the affected body parts instead of prostheses. For some ADLs, such as tying shoelaces, external help is preferred.4 People with an upper limb deficiency may demonstrate a high level of prosthetic skill during clinical tests according to Fraser5 (n = 121). In performing ADLs, most are however likely to use their sound hand and prefer a compensatory pattern of behavior or two-handed behavior. People also use their teeth, chin, and lower limbs to compensate for the loss of hand function.35 Burger and Marinč;ek9 state from a study of 414 subjects that people with a unilateral upper limb loss quickly learn to compensate the loss using the sound limb. As this compensation is so efficient, people often find the prosthesis encumbering and are reluctant to accept it. This compensation is also found in children with unilateral full hand loss who experience little problems with the loss themselves.19,25 The aforementioned studies of Østlie et al.,27 Fraser,5 and Burger and Marinč;ek9 are based on user studies with many subjects (n = 759 total). The results show that people with a unilateral upper limb loss often prefer the use of their sound hand and only need limited prosthetic functions for the performance of ADLs. Use of the sound hand or a compensatory behavior however leads to a risk of overuse or wrong use of sound body parts.11
Indicated problems and future research
Literature often indicates generalized problems and future research for both active and passive prostheses. Biddiss29 states that prosthesis design in general should first focus on maximizing comfort, particularly by reducing the weight and improving the thermal properties of current models. Pillet and Didierjean-Pillet17 describe that a prosthesis must have two qualities: first it must allow the user to pass unnoticed and second it must be sufficiently comfortable to be worn and forgotten. The role of a prosthetic hand in supporting, stabilizing, pushing, pulling, holding, and facilitating balance in everyday life situations should be valued to be of more use than that of manipulating small objects in the clinic situation.3 Kejlaa24 indicates that problems are concentrated on activities of daily necessity which make a person an independent individual.
Besides indicating research areas for improvement for all types of prostheses, the literature also indicates areas for potential improvement specifically for passive prostheses. Biddiss et al.26 (n = 38) define the main prioritized design priorities as follows: first, comfort; second, appearance; and third, function. The main prioritized improvements according to Kyberd et al.10 (n = 68) are given as follows: first, appearance; second, fit of socket; and third, movement and grip function. Kyberd et al. also describe that users who occasionally use a passive prosthetic hand (n = 4) gave especially low ratings to the fit of the socket and aspects of their prostheses’ functionality.
Passive prosthetic tools
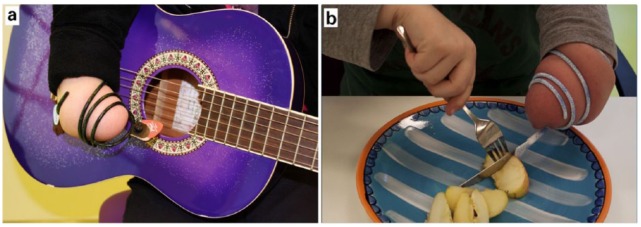
Usage
Publications on prosthetic tools primarily focus on sport, recreation, and vehicle driving. Prosthetic tools are, however, also very useful for ADLs such as using cutlery or riding a bicycle.4 Several examples of prosthetic tools are shown in Figure 5.
Figure 5.
Examples of prosthetic tools used for (a) playing a musical instrument and (b) eating.
Source: Adapted from De Hoogstraat Revalidatie.36
Prosthetic tools are commercially available for most common sports and recreational activities. This includes devices for holding and releasing hockey sticks, rackets, golf clubs, bowling balls, fishing poles, baseball bats, ski poles, kayak and canoe paddles, pistols, and cameras.18,37–40 Webster et al.20 denote that for many sports not all prostheses or equipment are allowed or have specific classifications. Walker et al.41 (n = 11) found that most children with upper limb amputations play baseball or basketball without a prosthesis at all. The available prosthetic tools actually rarely helped them in these activities.41 The major improvement of the use of prosthetic tools is found in activities where bimanual activity is obligatory, such as lifting barbells or playing the violin.6
For musicians also, multiple prosthetic tools are available. These include devices for holding a drumstick, violin bow, or flat pick.38,40,42 Woldendorp and van Gils43 and Charles et al.44 describe that musicians and caregivers do not always know the possibilities and have difficulties finding specific professional help. People with an upper limb deficiency may therefore unnecessarily stop their hobby or career. If special devices are required but not available, these can almost always be created.45 Successful performance of the desired activities is, however, always dependent on the motivation and proficiency of the prosthesis user, surgeon, prosthetist, and therapist.46
Fernández et al.47 (n = 236) found that the use of a prosthesis does not influence driving capability. Adaptations of the vehicle may, however, improve driving capability. This suggestion was supported by Burger and Marinč;ek48 (n = 37) who conclude that most people with an upper limb deficiency need at least one car adaptation for safe driving. They also found that for car driving a knob on the steering wheel was more frequently suggested to people with a left upper limb deficiency (in left steering cars). Verrall and Kulkarni49 found that automatic or electronically operated transmission and a knob on the steering wheel are the most frequent car adaptations requested by people with an upper limb deficiency. The steering ball can be operated by the sound hand, prosthetic hand, or prosthetic tool for driving.49 These adaptations are reported to be more frequently suggested to subjects following trans-humeral or more proximal amputation than to those following trans-radial or more distal amputation.48,49 The type of prosthesis does not influence the number of car adaptations.48
Views in literature on functionality
Although many prosthetic tools for various activities are available, it is not always clear how effective and safe they are in improving performance of the user.41,48 Prosthetic tools may be of use for learning new specific skills and supporting bimanual dexterity even if a prosthetic hand is rejected.6,20,41 The use of a prosthetic tool may even be preferred over the use of a prosthetic hand as it provides more function for a specific task and may have less disadvantages.6 A large variety of commercially available prosthetic components have become available over the last years.20,41,46 These have resulted in tremendously increased opportunities for persons with upper limb deficiency to participate in sport and recreational activities.
Some activities can be performed without a prosthesis or with a regular prosthesis which is not specifically adapted or designed for the activity. Many activities, however, require special prostheses or even custom or homemade devices developed according to personal needs.6,20,21,43 These special devices lead to a more effective task performance.50 Webster et al.20 state that it is important that the exact demands of the desired activity and the environment are considered. Exchange of prostheses for different activities can be performed relatively simply with the use of a quick-release wrist unit.20 Walker et al.41 state that, especially for children, interest in an activity may not be long-lived and prosthetic tools may subsequently be rejected. Prosthetic tools are especially useful when new skills are learned and may be unnecessary if the skills become more common and easy.6
Indicated problems and future research
According to Bragaru et al.,21 future research should focus on the technical characteristics and performance of sport prostheses. Bragaru et al. argue that data concerning sport prostheses are scarce and mostly descriptive in nature. Vasluian et al.6 indicate that users want more information about different prosthetic tools. The important main characteristics of prosthetic tools are secure suspension, durability, optimal weight, and simplicity.20 Information on these characteristics will ultimately lead to an increase in participation in sports and physical activities of people with an upper limb deficiency.21
Next to the provision of clear characteristics, the costs are important. The costs for the user strongly depend on regulations which differ per country.6 Many prosthetic tools are expensive.6,41 Therefore, people critically weigh the costs of the prosthesis against its advantages.
Discussion
Remarks on the reviewed literature on passive prostheses
Implementing a clear classification of passive prostheses
Literature uses similar names for different types of passive prostheses. This complicates the understanding of the literature and causes confusion. Most of the reviewed literature does not make a distinction between static and adjustable passive prostheses. This distinction is, however, required as it has a major influence on prosthesis functionality and it is expected that this difference in functionality influences the usage and acceptance of the different types of devices. In order to prevent the aforementioned problems and in order to gain new data on the differences between the devices, future studies should make a clear distinction between static and adjustable devices. We propose to use the prosthetic classification presented in the “Background” section and in Figure 1 as a standard classification for passive devices.
Providing characteristics
In the selected literature, scarce information is found on the characteristics of passive prostheses, for example, hand opening, hand mass, and force required to open the hand. The literature primarily discusses passive prostheses in a general and qualitative manner. These general descriptions hardly give direction to future research, as more specific information on the characteristics is required.
Neither is a clear overview and comparison of the available passive prostheses available. Literature presents little information on characteristics of specific passive prostheses. These characteristics are, however, very interesting and useful for rehabilitation specialists and patients.
Passive prosthetic hands
Static and dynamic appearance
Appearance can be divided into static and dynamic appearance. Static appearance relates to the shape, color, and finishing of the hand. Dynamic appearance relates to the movement of the artificial limb and the manner in which activities are performed in relation to a sound hand.22,31 Scarce information on the dynamic appearance of prostheses is found. This is very remarkable since the appearance is valued as a major prosthetic function and research direction.
Over the past decades, manual labor has become less important. This also influenced the field of upper limb prosthetics.19 The functions of hand prostheses have become less important and the major requirements shifted to lifelike appearance.
People with a unilateral upper limb deficiency need limited prosthetic functions
Multiple publications5,9,13,19,27,34 state that many ADLs can be performed one-handed. People with a unilateral upper limb deficiency therefore need limited prosthetic functions to perform the ADLs. So instead of focusing on the increase in functionality, future research should focus on the development of prostheses which only offer limited although sufficient functionality for most ADLs. Limiting the prosthetic functionality increases the design space for the enhancement of cosmesis, comfort, and control. This future research may result in prostheses which are useful for people currently not using a prosthesis, as well as for those using an active or a passive prosthesis.
Views in literature on functionality
Literature presents two views on the functionality of passive prosthetic hands. The first view states that these prostheses offer very little functionality and mainly improve appearance.12,24,33 This view is mainly based on statements and visions of authors. The second view states that passive prosthetic hands are used as a functional support in many ADLs. This second view is strengthened by numerous studies which are based on user studies and profound research and therefore more reliable.5,10,13 Passive prosthetic hands are thus functional in many ADLs. Passive prosthetic hands should therefore be offered as a serious first and ultimate option of choice, along with active devices, and not mainly as a stepping stone to an active prosthesis, as a last resort or just for improving appearance.
The functional value of passive prostheses is accepted by most people involved, including therapist, patient, prosthetist, and manufacturer. It seems, however, that active prostheses remain the standard and are mostly the prime subject of research. The general focus on active prostheses might have two causes: (1) the physical impairment of people with a unilateral upper limb deficiency is overestimated and (2) the associated people have expectations and interests not directly related to the patients’ individual needs. These may be personal desires or financial motives.
Future research
Literature indicates various research areas for improvement of passive devices. This might be caused by the individual needs of different users. The most reported prioritized improvement areas are appearance, comfort, and function.10,24,26,29 Current research is, however, limited to appearance and comfort, as similar problems are experienced for active prostheses.8,22 The functions of passive prosthetic hands are not researched nor have they been improved.
Users of passive prosthetic hands have functional difficulties with the performance of pulling, gripping, holding, and releasing objects in ADLs.5,10,24,26 This is especially the case in bimanual tasks when these activities have to be performed with the prosthesis. Static prosthetic hands can hardly be improved in functions. Adjustable prosthetic hands, however, offer a high potential to be improved in the performance of difficult bimanual activities. More specifically, the fingers of passive adjustable prosthetic hands could be made articulating, the grip force could be made adjustable, and the control of the opening and closing of the hand could be made faster and easier.
Passive prosthetic tools
Usage
Prosthetic tools are primarily described for sport and recreation. Literature does not present devices for activities relating to independent living and work. This is remarkable since independent living is very important to people. On average, people spend about 35% of their day on work-related activities.51 Prosthetic tools can be very useful for these activities since work-related activities often require bimanual performance and repetitive activities.
For vehicle driving, prosthetic tools as well as vehicle adaptations are discussed. Adaptations made to the patients’ environment could also be useful for multiple other activities as they may enhance and ease the performance of these activities. In order to prevent users from often changing their prosthetic tool, it is desired that the prosthetic tool (or hand) can be used for multiple activities.
Future research
As different types of prostheses offer different advantages, multiple prostheses may be used by an individual. Therefore, a well-founded compromise between prosthetic hands, prosthetic tools, and environmental adaptations has to be selected per individual. To ease this selection, clear characteristics have to be provided per prosthesis.
Prosthetic hands are used for a variety of activities. Prosthetic tools are, however, mostly optimized for one predefined activity. This results in a wide range of available tools for numerous activities. Multiple prosthetic tools can be combined as they may offer similar characteristics, such as the cylindrical grasp tool18 for kayak paddling and lifting an exercise weight. However, a passive adjustable hand which could grasp and hold a wide range of objects and handlebars and which can be used for most ADLs would make these prosthetic tools unnecessary.
Conclusion
Passive prostheses have received very little attention in prosthetic research and in the literature. Often little functional value is attributed to passive hand prostheses when compared to active prostheses. Yet, user studies show that as much as one out of three prosthetic hand users uses a passive prosthesis. People with a unilateral upper limb deficiency often need only limited prosthetic function. Passive hand prostheses have been shown to be useful for many people and should therefore receive more attention in current research and literature.
The current literature clearly indicates potential improvements for current passive prostheses. The ability of pulling and grasping objects should be improved. Of all different types of passive devices, future research should focus on passive adjustable prosthetic hands, as these devices offer the most potential for improvement. The fingers of passive adjustable prosthetic hands could be made articulating, the grip force could be made adjustable, and the control of the opening and closing of the hand could be made faster and easier.
Current literature uses ambiguous names for different types of passive prostheses. This complicates the understanding of the literature and causes confusion. In order to avoid these problems, we present a new classification of passive prostheses which makes a clear distinction between the different types of devices. Particularly, we advise to make a clear distinction between static passive devices and adjustable passive devices in future user studies.
Footnotes
Author contribution: All authors contributed equally in the preparation of this manuscript.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Plettenburg DH. The WILMER passive hand prosthesis for toddlers. J Prosthet Orthot 2009; 21(2): 97–99. [Google Scholar]
- 2. TRS Prosthetics. Innovative, high performance body powered prosthetic technology, http://www.trsprosthetics.com/ (accessed March 2015).
- 3. APC Prosthetics. Upper limb prostheses, http://www.apcprosthetics.com.au/upper-limb-prostheses/ (accessed March 2015).
- 4. Myrdal Orthopedics. Criterium bicycle handlebar adapters, http://www.myrdalorthopedics.com/ (accessed March 2015).
- 5. Fraser CM. An evaluation of the use made of cosmetic and functional prostheses by unilateral upper limb amputees. Prosthet Orthot Int 1998; 22(3): 216–223. [DOI] [PubMed] [Google Scholar]
- 6. Vasluian E, van Wijk I, Dijkstra PU, et al. Adaptive devices in young people with upper limb reduction deficiencies: use and satisfaction. J Rehab Med 2015; 47: 1–10. [DOI] [PubMed] [Google Scholar]
- 7. Pillet J. The aesthetic hand prosthesis. Orthop Clin North Am 1981; 12(4): 961–969. [PubMed] [Google Scholar]
- 8. Biddiss E, Chau T. Upper limb prosthesis use and abandonment: a survey of the last 25 years. Prosthet Orthot Int 2007; 31(3): 236–257. [DOI] [PubMed] [Google Scholar]
- 9. Burger H, Marinč;ek C. Upper limb prosthetic use in Slovenia. Prosthet Orthot Int 1994; 18(1): 25–33. [DOI] [PubMed] [Google Scholar]
- 10. Kyberd PJ, Wartenberg C, Sandsjo L, et al. Survey of upper-extremity prosthesis users in Sweden and the United Kingdom. J Prosthet Orthot 2007; 19(2): 55–62. [DOI] [PubMed] [Google Scholar]
- 11. Datta D, Selvarajah K, Davey N. Functional outcome of patients with proximal upper limb deficiency-acquired and congenital. Clin Rehabil 2004; 18(2): 172–177. [DOI] [PubMed] [Google Scholar]
- 12. Gaine WJ, Smart C, Bransby-Zachary M. Upper limb traumatic amputees. Review of prosthetic use. J Hand Surg 1997; 22(1): 73–76. [DOI] [PubMed] [Google Scholar]
- 13. Crandall RC, Tomhave W. Pediatric unilateral below-elbow amputees: retrospective analysis of 34 patients given multiple prosthetic options. J Pediatr Orthop 2002; 22(3): 380–383. [PubMed] [Google Scholar]
- 14. Michael JW, Bowker JH. Atlas of amputations and limb deficiencies: surgical, prosthetic, and rehabilitation principles. 3rd ed. Rosemont, IL: American Academy of Orthopedic Surgeons, 2004. [Google Scholar]
- 15. Näder HG. Otto Bock Prothesen-Kompendium: Prothesen für die obere Extremität. Duderstadt: Otto Bock HealthCare GmbH, 2011. [Google Scholar]
- 16. Pillet J. Esthetic hand prostheses. J Hand Surg 1983; 8(5 Pt 2): 778–781. [DOI] [PubMed] [Google Scholar]
- 17. Pillet J, Didierjean-Pillet A. Aesthetic hand prosthesis: gadget or therapy? Presentation of a new classification. J Hand Surg 2001; 26(6): 523–528. [DOI] [PubMed] [Google Scholar]
- 18. Highsmith MJ, Carey SL, Koelsch KW, et al. Design and fabrication of a passive-function, cylindrical grasp terminal device. Prosthet Orthot Int 2009; 33(4): 391–398. [DOI] [PubMed] [Google Scholar]
- 19. Beasley RW. Hand and finger prostheses. J Hand Surg 1987; 12(1): 144–147. [DOI] [PubMed] [Google Scholar]
- 20. Webster JB, Levy CE, Bryant PR, et al. Sports and recreation for persons with limb deficiency. Arch Phys Med Rehabil 2001; 82(3): S38–S44. [PubMed] [Google Scholar]
- 21. Bragaru M, Dekker R, Geertzen JH. Sport prostheses and prosthetic adaptations for the upper and lower limb amputees: an overview of peer reviewed literature. Prosthet Orthot Int 2012; 36(3): 290–296. [DOI] [PubMed] [Google Scholar]
- 22. Ritchie S, Wiggins S, Sanford A. Perceptions of cosmesis and function in adults with upper limb prostheses: a systematic literature review. Prosthet Orthot Int 2011; 35(4): 332–341. [DOI] [PubMed] [Google Scholar]
- 23. Thurston AJ. Paré and prosthetics: the early history of artificial limbs. ANZ J Surg 2007; 77(12): 1114–1119. [DOI] [PubMed] [Google Scholar]
- 24. Kejlaa GH. Consumer concerns and the functional value of prostheses to upper limb amputees. Prosthet Orthot Int 1993; 17(3): 157–163. [DOI] [PubMed] [Google Scholar]
- 25. Shida-Tokeshi J, Bagley A, Molitor F, et al. Predictors of continued prosthetic wear in children with upper extremity prostheses. J Prosthet Orthot 2005; 17(4): 119–124. [Google Scholar]
- 26. Biddiss E, Beaton D, Chau T. Consumer design priorities for upper limb prosthetics. Disabil Rehabil Assist Technol 2007; 2(6): 346–357. [DOI] [PubMed] [Google Scholar]
- 27. Østlie K, Lesjo IM, Franklin RJ, et al. Prosthesis use in adult acquired major upper-limb amputees: patterns of wear, prosthetic skills and the actual use of prostheses in activities of daily life. Disabil Rehabil Assist Technol 2012; 7(6): 479–493. [DOI] [PubMed] [Google Scholar]
- 28. Silcox DH, Rooks MD, Vogel RR, et al. Myoelectric prostheses. A long-term follow-up and a study of the use of alternate prostheses. J Bone Joint Surg Am 1993; 75(12): 1781–1789. [DOI] [PubMed] [Google Scholar]
- 29. Biddiss E. Need-directed design of prostheses and enabling resources. In: Murray C. (ed.) Amputation, prosthesis use, and phantom limb pain: an interdisciplinary perspective. New York: Springer, 2010, pp. 7–21. [Google Scholar]
- 30. Shaperman JLS, Setoguchi Y. Early upper limb prosthesis fitting: when and what do we fit. J Prosthet Orthot 2003; 15(1): 11–17. [Google Scholar]
- 31. Soltanian H, de Bese G, Beasley RW. Passive hand prostheses. Hand Clin 2003; 19(1): 177–183. [DOI] [PubMed] [Google Scholar]
- 32. Van Lunteren A, van Lunteren-Gerritsen GHM, Stassen HG, et al. A field evaluation of arm prostheses for unilateral amputees. Prosthet Orthot Int 1983; 7(3): 141–151. [DOI] [PubMed] [Google Scholar]
- 33. Roeschlein RA, Domholdt E. Factors related to successful upper extremity prosthetic use. Prosthet Orthot Int 1989; 13(1): 14–18. [DOI] [PubMed] [Google Scholar]
- 34. Beasley RW, de Bese GM. Upper limb amputations and prostheses. Orthop Clin North Am 1986; 17(3): 395–405. [PubMed] [Google Scholar]
- 35. Østlie K, Franklin RJ, Skjeldal OH, et al. Musculoskeletal pain and overuse syndromes in adult acquired major upper-limb amputees. Arch Phys Med Rehabil 2011; 92(12): 1967–1973. [DOI] [PubMed] [Google Scholar]
- 36. De Hoogstraat Revalidatie. Amputatie of aanlegstoornis van de arm, http://www.dehoogstraat.nl/home (accessed March 2015).
- 37. Dillingham TR. Rehabilitation of the upper limb amputee. In: Dillingham TR, Belandres P. (eds) Rehabilitation of the injured combatant. Washington: Office of the Surgeon General, 1998, pp. 33–77. [Google Scholar]
- 38. Radocy B. Upper-extremity prosthetics: considerations and designs for sports and recreation. Clin Prosthet Orthot 1987; 11(3): 131–153. [Google Scholar]
- 39. Truong XT, Erickson R, Galbreath R. Baseball adaptation for below-elbow prosthesis. Arch Phys Med Rehabil 1986; 67(6): 418. [PubMed] [Google Scholar]
- 40. Radocy B. Special considerations: upper-limb prosthetic adaptations for sports and recreation. In: Bowker HK, Michael JW. (eds) Atlas of limb prosthetics: surgical, prosthetic, and rehabilitation principles. 2nd ed. Rosemont, IL: American Academy of Orthopedic Surgeons, 1992. [Google Scholar]
- 41. Walker JL, Coburn TR, Cottle W, et al. Recreational terminal devices for children with upper extremity amputations. J Pediatr Orthop 2008; 28(2): 271–273. [DOI] [PubMed] [Google Scholar]
- 42. Norris RN. Applied ergonomics: adaptive equipment and instrument modification for musicians. Md Med J 1993; 42(3): 271–275. [PubMed] [Google Scholar]
- 43. Woldendorp KH, van Gils W. One-handed musicians—more than a gimmick. Med Probl Perform Art 2012; 27(4): 231–237. [PubMed] [Google Scholar]
- 44. Charles D, James KB, Stein RB. Rehabilitation of musicians with upper limb amputations. J Rehabil Res Dev 1988; 25(3): 25–32. [PubMed] [Google Scholar]
- 45. Rubin G, Fleiss D. Devices to enable persons with amputation to participate in sports. Arch Phys Med Rehabil 1983; 64(1): 37–40. [PubMed] [Google Scholar]
- 46. Michael JW, Gailey RS, Bowker JH. New developments in recreational prostheses and adaptive devices for the amputee. Clin Orthop Relat Res 1990; 256: 64–75. [PubMed] [Google Scholar]
- 47. Fernandez A, Lopez MJ, Navarro R. Performance of persons with juvenile-onset amputation in driving motor vehicles. Arch Phys Med Rehabil 2000; 81(3): 288–291. [DOI] [PubMed] [Google Scholar]
- 48. Burger H, Marinč;ek C. Driving ability following upper limb amputation. Prosthet Orthot Int 2013; 37(5): 391–395. [DOI] [PubMed] [Google Scholar]
- 49. Verrall T, Kulkarni JR. Driving appliances for upper limb amputees. Prosthet Orthot Int 1995; 19(2): 124–127. [DOI] [PubMed] [Google Scholar]
- 50. Yoneyama K, Nakashima M. Development of swimming prosthetic for physically disabled. In: Moritz EF, Haake SJ. (eds) The engineering of sport 6. New York: Springer, 2006, pp. 431–436. [Google Scholar]
- 51. Bureau of Labor Statistics. Charts from the American Time Use Survey, http://www.bls.gov/tus/charts/ (accessed March 2015).