Abstract
Breast cancer (BC) is a highly heterogeneous disease associated with metabolic reprogramming. The shifts in the metabolome caused by BC still lack data from Latin populations of Hispanic origin. In this pilot study, metabolomic and lipidomic approaches were performed to establish a plasma metabolic fingerprint of Colombian Hispanic women with BC. Data from 1H-NMR, GC-MS and LC-MS were combined and compared. Statistics showed discrimination between breast cancer and healthy subjects on all analytical platforms. The differentiating metabolites were involved in glycerolipid, glycerophospholipid, amino acid and fatty acid metabolism. This study demonstrates the usefulness of multiplatform approaches in metabolic/lipid fingerprinting studies to broaden the outlook of possible shifts in metabolism. Our findings propose relevant plasma metabolites that could contribute to a better understanding of underlying metabolic shifts driven by BC in women of Colombian Hispanic origin. Particularly, the understanding of the up-regulation of long chain fatty acyl carnitines and the down-regulation of cyclic phosphatidic acid (cPA). In addition, the mapped metabolic signatures in breast cancer were similar but not identical to those reported for non-Hispanic women, despite racial differences.
Introduction
Breast cancer (BC) remains the most frequent type of cancer and the main cause of cancer deaths among women worldwide [1]. According to GLOBOCAN, breast cancer mortality rates in developed countries have declined in the last years, but the incidence rates continues to rise, especially in Latin America and other developing regions [1, 2]. Mortality reduction has been associated with the advances in medical diagnostic methods and the development of new therapies; however, the high heterogeneity of breast cancer still poses challenges to the understanding of its characteristic phenotype. Reported findings of breast cancer have suggested prognosis and predictive biomarkers based on alterations in genes (e.g. BRCA1 and BRCA2) [3, 4] and protein expression (e.g. mTOR, ras, PKC) [5–7]. In the past few years, metabolites have been proposed as BC markers, along with genes and proteins.
Metabolomics is a consolidated field that has enabled to observe differences in metabolic signatures generated by a pathological state such as cancer. These differences allow to postulate molecular mechanisms involved in cancer, proposing and evaluating promissory treatment targets and diagnosis tools [8–10]. Although the identification of breast cancer biomarkers by metabolomics is still at an early stage, exploratory studies have allowed highlighting alterations in aerobic glycolysis, de novo lipogenesis, glutaminolysis, glycerolipid, glycerophospholipid and amino acid metabolism [11–15]. These alterations have been used to identify metabolic changes associated with advanced metastatic breast cancer in cell lines [16, 17] and serum [18], as well as breast cancer subtypes in plasma [13, 19] and tissue [13, 19–21]. Moreover, the identification of suitable targets for drug development in cell lines [22–24] and therapy selection in cell lines [25] and serum [26] have also been achieved.
High-throughput analytical chemical techniques such as chromatography coupled to mass spectrometry (MS) and nuclear magnetic resonance (NMR) spectroscopy [27, 28] have been used in metabolomics, along with univariate and multivariate statistics [29, 30], in order to provide information on a large number of metabolites, in particular those with altered levels between healthy subjects and cancer patients [9, 31–34]. Metabolomics in BC has been mainly performed by NMR and MS, according to the purpose of the study and the characteristics of measured metabolites [35]. NMR has proven useful to determine significant differences in serum samples, allowing a discrimination between early and metastatic BC, regarding to amino acid, small organic molecules and general lipid content [26, 36, 37], and also to predict BC recurrence using amino acid, fatty acid and choline levels [38]. Both GC-MS and LC-MS have detected alterations that have been proposed for several biomarkers, including amino acids [38–41], small organic acids [13, 38] and fatty acids [26, 38], whereas lysophospholipid [42, 43] and carnitine [13] alterations have been found only by LC-MS. In addition, alterations in less polar lipids, such as glycerophospholipids [42, 44, 45] and glycerolipids [43, 46] have been reported by LC-MS using a lipidomics approach.
In last decades, extensive research in breast cancer has been conducted in order to understand its heterogeneity, however a comprehensive metabolic profile is still required to identify promising underlying metabolic signatures that can be used to improve breast cancer diagnosis and treatment. Besides, most studies of metabolic alterations in BC have been performed on Asian, European and North American women, little is known about the metabolic signature of BC in women from developing regions. In the present pilot study, a multiplatform metabolomic and lipidomic approach based on NMR, GC-MS and LC-MS was performed towards mapping breast cancer metabolic perturbations in Colombian Hispanic women. To our present knowledge, this is the first report of the metabolic fingerprint of BC in the Colombian population.
Materials and methods
Characterization of studied subjects and sample collection
Fifty-eight women between 35 and 65 years were selected for the study with the following characterization of individual groups. Control patient (CP) group: 29 healthy women with an average age of 51 ± 8 years (where ± is standard deviation) and a body mass index (BMI) with a mean value of 27 ± 3 kg/m2. Breast cancer patient (BCP) group: 29 women diagnosed with breast cancer, mostly invasive ductal carcinoma between stage I and III (Table 1). The average age was 50 ± 7 years and BMI mean value of 26 ± 3 kg/m2. All participants were non-smokers, not taking hormonal contraception, and had undergone the last dose of cancer-related treatment between three to six months before sampling, allowing at least a three month period of wash-out before sampling. The study was approved by the ethics committee of the Universidad de Los Andes and Liga contra el Cancer- Seccional Bogotá, Colombia. All participants signed the written informed consent form. Sample collection took place at Liga contra el Cancer—Seccional Bogotá, Colombia from December 2015 to January 2016. Venous blood samples were taken in the morning after overnight fasting and were collected using K3EDTA and Heparin Vacuette blood collection tubes for MS and NMR analysis, respectively. Once collected, the blood was centrifuged at room temperature (19°C) for 15 min at 3000 x g. The harvested plasma was fractionated into 100 μL aliquots in micro centrifuge tubes and stored at -80°C until analysis.
Table 1. Characteristics of studied subjects.
| Characteristic | BCP | CP | |
|---|---|---|---|
| n = 29 | n = 29 | ||
| Age Group, years (Average ± SD) | 51 ± 8 | 50 ± 7 | |
| BMI, Kg/m2(Average ± SD) | 26 ± 3 | 27 ± 3 | |
| Diagnosis | IDC | 19 (65.5%) | NA |
| ILC | 10 (34.5%) | NA | |
| Stage | I | 3 (10.3%) | NA |
| II | 15 (51.7%) | NA | |
| III | 11 (37.9%) | NA | |
| ER status | pos | 19 (65.5%) | NA |
| neg | 10 (34.5%) | NA | |
| PR status | pos | 12 (41.4%) | NA |
| neg | 17 (58.6%) | NA | |
| HER2 status | pos | 6 (20.7%) | NA |
| neg | 23 (79.3%) | NA | |
| Surgery | Yes | 24 (82.8%) | NA |
| No | 5 (17.2%) | NA | |
| Chemotherapy | Yes | 27 (93.1%) | NA |
| No | 2 (6.9%) | NA | |
| Radiotherapy | Yes | 22 (75.9%) | NA |
| No | 7 (24.1%) | NA | |
| Hormonal Therapy | Yes | 15 (51.7%) | NA |
| no | 14 (48.1%) | NA | |
IDC: Invasive ductal carcinoma; ILC: Invasive lobular carcinoma; ER: Estrogen receptor; PR: Progesterone receptor; HER2: Human epidermal growth factor receptor 2; NA: not applicable.
Metabolic fingerprinting by GC-MS analysis
Plasma sample preparation and metabolite analysis by GC-MS were performed as previously reported by Garcia et al. [47]. Briefly, the plasma (40 μL) was deproteinized with cold acetonitrile (1:3, −20°C), followed by a two-step derivatization: (i) methoximation with O-Methoxyamine hydrochloride in pyridine (15 mg/mL, room temperature, 16 h) followed by (ii) silylation with BSTFA containing 1% TMCS (70°C, 1 h). Metabolic fingerprinting (MF) was performed using an HP 6890 Series GC system equipped with an HP 6890 autosampler and an Agilent Mass Selective Detector 5973 (Agilent technologies, Palo Alto, CA, USA). Two microliters of the derivatized plasma samples were injected onto a Zebron ZB-5MSi capillary GC column (30 m x 0.25 mm x 0.25 μm) using helium as carrier gas at a constant gas flow of 1.0 mL/min. The injector temperature was set at 250°C and the split ratio to 1:10. The temperature gradient program started at 60°C held for 1 min, followed by a subsequent increase in temperature to 320°C at a rate of 10°C/min. The GC-MS transfer line, filament source and the quadrupole temperature were set at 280, 230 and 150°C, respectively. The electron ionization (EI) source was set at 70 eV and the mass spectrometer was operated in full scan mode applying a mass range from m/z 50 to 600 at a scan rate of 1.38 scan/s.
Metabolic fingerprinting by LC-MS analysis
Plasma deproteinization and metabolite extraction were performed using the protocol published by Ciborowski et al. [48]. The plasma (40 μL) was mixed with a cold mixture of methanol/ethanol (1:1, −20°C) in a ratio of 1:3. MF by LC-MS was performed using an HPLC system 1200 series coupled to Q-TOF 6520 (Agilent Technologies, Santa Clara, CA, USA). Ten microliter of sample extract were injected onto a C18 column (Kinetex C18 150 mm x 2.1 mm, 2.6 μm; Phenomenex) with a guard column (Kinetex C18 20 mm x 2.1 mm, 2.6 μm; Phenomenex). LC separation was performed at 40°C using a mobile phase that consisted of 0.1% (v/v) formic acid in water (A) and 0.1% (v/v) formic acid in acetonitrile (B) at a flow rate of 0.3 mL/min. The applied gradient elution program started at 25% B increased then to 95% B in 35 min, returned to initial conditions in 1 min and was kept constant for 9 min to ensure re-equilibration of the column. Data were collected in both positive and negative electrospray ionization (ESI) modes in separate runs, using the conditions previously described [48]. During all analysis, two reference masses were continuously injected for mass correction: m/z 121.0509 (C5H4N4) and m/z 922.0098 (C18H18O6N3P3F24) for positive ionization mode and m/z 112.9856 (C2O2F3(NH4)) and m/z 1033.9881 (C18H18O6N3P3F24) for negative ionization mode.
Metabolic fingerprinting by NMR analysis
Plasma samples for NMR analysis were prepared according to the procedure published by Dona et al [49]. In short, D2O phosphate buffer pH 7.4 (0.075M Na2HPO4·7H2O) with 3-trimethylsilyl propionic acid (TSP) (350 μL) was added to heparin containing plasma samples (350 μL). The mixture was centrifuged and transferred into NMR tubes. 1H-NMR spectra were acquired using a Bruker UltraShield 400 MHz spectrometer (Bruker Biospin, Karlsruhe, Germany). Samples were measured at 300 K employing two NMR experiments. First, a water suppression using pre-saturation pulses (zgpr, 25Hz) was carried out using the standard pulse sequence [RD—P(90°)–AQ]. Thereafter, a Carr-Purcell-Miboom-Gill (CPMG) pulse sequence was applied with a receiver gain of 90.5, a total mixing time of 78 ms (126 loops), 4 dummy scans and 64 free induction decay (FID). FIDs were multiplied by a 0.3 Hz exponential function prior to Fourier transform and only zero-order phase correction was allowed [50].
Lipid fingerprinting by LC-MS analysis
Plasma lipids were extracted using methyl tert-butyl ether (MTBE) as previously reported by Whiley et al. [51]. In short, plasma (20 μL) was vortex-mixed with MTBE/methanol (10:2) mixture, deionized water (250 μL) was added and the upper phase containing the plasma lipid fraction was transferred into vials for LC-MS analysis. Lipid fingerprinting (LF) was performed employing the same instrumentation used for MF analysis by LC-MS. Five microliter of the lipid extract were injected onto a C8 column (Phenomenex-Luna C8 150mm x 2.0 mm, 3um). Chromatographic analysis were carried out at 60°C using a gradient elution applying 10 mM ammonium formate in Milli-Q water (A) and 10 mM ammonium formate in methanol (B) at a constant flow of 0.5 mL/min. The eluent gradient ranged from 75% to 96% B in 23 min, and was then held for 22 min at 96%B. The gradient was then increased to 100% B in 1 min and kept constant for 4 min before the gradient could return to its initial conditions in 1 min and held there for 14 min to enable column re-equilibration. Mass spectrometric detection was performed in both positive and negative ionization mode as previously described by Whiley et al. [51]. Throughout the analysis, the same reference masses were used as described in the section on MF analysis.
Quality control samples
Quality control (QC) samples were prepared by mixing equal volumes of plasma from each BCP and CP sample. Subsequently, profiles from the QC samples were recorded following the same procedures as described above for each technique. To determine the reproducibility of plasma sample preparation and the stability of the analytical platforms used, several QC runs were performed prior to the analysis of all plasma samples until system equilibration was achieved. QC plasma samples were also analyzed after every five randomized plasma samples [52].
Data treatment
GC-MS data treatment consisted in data deconvolution and metabolite identification using Agilent MassHunter Unknowns Analysis B.07.00, Fiehn version 2008 and NIST 14 libraries. Thereafter, retention time alignment was performed using Agilent Mass Profiler Professional B.12.1 software, and the results were exported to Agilent MassHunter Quantitative B.07.00 in order to perform the integration of each metabolite. Raw LC-MS data was treated with Agilent MassHunter Profinder Software B.06.00 using Molecular Feature Extraction (MFE) and subsequent Recursive Feature Extraction (RFE) algorithms for noise reduction, feature deconvolution and alignment. Finally, alignment and integration of the features by GC-MS and LC-MS were manually inspected and exported to Excel (Microsoft) to filter by presence and reproducibility, keeping only the metabolites detected in at least 80% of all plasma samples and a coefficient of variation (CV %) of less than 30% of the same metabolite detected in the QC samples [53].
For NMR data treatment, the spectral range was set 0.5 to 8.5, in which the spectral regions of water (4.7 to 4.9 ppm) and TSP (-0.20 to 0.20ppm) were excluded. Data were segmented and reduced by binning method with a window of 0.04 ppm and stored as a data matrix.
Statistical analysis
Significant differences between plasma samples fingerprints from BCP and CP obtained within each technique, were evaluated by multivariate (MVA) and univariate (UVA) statistical analysis. MVA were performed using SIMCA-P+ 12.0 (Umetrics, Umea, Sweden). Unsupervised principal component analysis (PCA) was first used to evaluate the quality of the analytical system performance using the QC samples. Then, a supervised method, orthogonal partial least squares regression (OPLS-DA) was performed to maximize differences between BCP and CP, and for the selection of the variables responsible for the separation between the two different groups. Pareto scaling and logarithmic transformation were used before the statistical analysis. The accuracy of the classification was assessed by means of a double cross-validation scheme. The original data set was split into a training, test and external set before any step of statistical analysis. The number of OPLS components were chosen on the basis of a 7-fold cross-validation that was performed on the training set only, and the best model was used to predict the samples in the test set. The whole procedure was repeated 50 times with a 7 cross-validation scheme, and the results were averaged [54].
UVA was performed employing MatLab (7.10.0 Mathworks, Inc., Natick). Data normality was verified by evaluation of the Kolmogorov-Smirnov-Lillefors and Shapiro—Wilk tests and variance ratio by the Levene’s test. The p-value was determined by parametric (unpaired t-test) or non-parametric (Mann—Whitney U test) tests with a Benjamini—Hochberg False Discovery Rate post hoc correction (FDR).
For both LC-MS and GC-MS data, the significant variables were selected by keeping only the variables that fulfilled: 1) UVA (p-value <0.05 from hypothesis testing) and 2) MVA criteria (variance important in projection (VIP) with Jack-knife confident interval (JK) not including 0), while in NMR significant chemical shifts were selected only by MVA.
Metabolite identification
Metabolites obtained by GC-MS analysis were identified using the Fiehn version 2008 and NIST 14 libraries, while significant features obtained by LC-MS were putatively identified by matching the observed accurate mass of each compound with the m/z values available online using following databases: METLIN (http://metlin.scripps.edu), KEGG (http://genome.jp/kegg), lipid MAPS (http://lipidMAPS.org), and HMDB (http://hmdb.ca) with the CEU Mass Mediator tool (http://ceumass.eps.uspceu.es/mediator/). Finally, some LC-MS significant metabolites were further analyzed by MS/MS analysis, in order to confirm the metabolite’s identity. For NMR, metabolites were identified by their 1H-NMR spectra by comparison of observed chemical shifts and signal multiplicities reported previously in the literature [55, 56].
Pathway mapping of metabolites
Metabolic pathway analysis was performed using MetaboAnalyst 3.0 tool (http://www.metaboanalyst.ca/), which integrates two pathways analysis approaches, enrichment and topology pathway analysis. A list of compound names from identified significant metabolites was uploaded and processed using “homo sapiens” library [57].
Results
Multiplatform metabolic and lipid fingerprinting analysis of BCP and CP plasma samples were conducted using four different approaches aiming at detecting the largest possible number of metabolites. The total coverage of plasma metabolites from the MS-based platforms consisted of 1428 identified metabolites, 77 by GC-MS, 298 by MF/LC-MS(+), 313 by MF/LC-MS(-), 532 by LF/LC-MS(+) and238 by LF/LC-MS(-). Furthermore, 1757 chemical shifts were detected by 1H NMR analysis. A comparison between the number of detected metabolites during data processing across the different analytical techniques used is presented in S1 Table, and a typical metabolic fingerprint from each platform is presented in S1–S3 Figs.
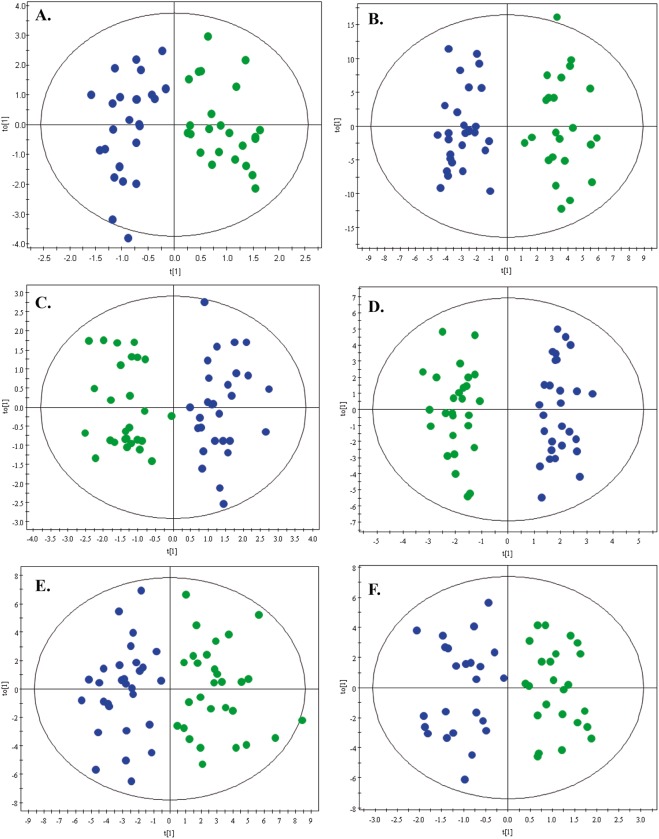
The performance of the different analytical platforms was assessed by clustering of the QC samples in the PCA models (S4 Fig), assuring the acquired data quality and the conservation of biological variation over experimental bias. Using this approach, further statistical comparisons across the samples were allowed. The discrimination between BCP and CP was achieved using an OPLS-DA model for each platform, as shown in Fig 1. A clear group separation was observed in the score plots for all models, with acceptable values of predicted variance (R2) and predictive ability (Q2). Double cross-validation of the models showed that these correctly discriminated the groups correctly above 70% of classification accuracy for NMR (71%), MF/LC-MS(+) (81%), MF/LC-MS(-) (79%) and GC-MS (71%), while only above 60% for LF/LC-MS(+) (68%) and LF/LC-MS(-) (60%). Individual differentiating metabolites were determined by a combination of MVA (VIP > 1 with JK) and UVA (percentage of change > 30% and p < 0.05) criteria, obtaining 16 significant metabolites by GC-MS, 31 by MF/LC-MS(+), 50 by MF/LC-MS(-), 50 by LF/LC-MS(+) and 41 by LF/LC-MS(-) analysis.
Fig 1. OPLS-DA models.
OPLS-DA models with Log transformation and Pareto scaling for metabolic and lipid fingerprinting of breast cancer (green dots) and control (blue dots) groups. Panels: A. MF by GC-MS: R2 = 0.827. Q2 = 0.514. B. MF by NMR: R2 = 0.921. Q2 = 0.614. C. MF by LC-MS(+):R2 = 0.858. Q2 = 0.665. D. MF by LC-MS(-): R2 = 0.930. Q2 = 0.681. E. LF by LC-MS(+): R2 = 0.779. Q2 = 0.535. F. LF by LC-MS(-):R2 = 0.829. Q2 = 0.501.
For GC-MS analysis, the significant metabolites corresponded to the chemical classes of fatty acids, organic acids and amino acids (Table 2). All identified metabolites were up-regulated in the BCP group, except for one metabolite; pyruvic acid. MF/LC-MS(±) analysis resulted in the identification of altered lipids in the plasma of BCP (Table 3), in particular, fatty acylcarnitines, fatty acids, lysophosphatidylethanolamines (LPE), lysophosphatidylcholines (LPC), phosphatidic acids (PA) and phosphatidylglycerol (PG). In addition, LF/LC-MS(±) determined significant differences in non-polar lipids such as phosphatidylcholines (PC), sphingolipids (SM) and mono, di-and triacylglycerides (MG, DG and TG) (Table 4). The number of statistical significant metabolites across MS platforms are compared in Fig 2.
Table 2. Compounds with statistical significance identified by GC-MS.
| Compound | Molecular formula | RT (min) | Target ion | Qualifier ion (Q) m/z | CV for QC (%) | Change (%) | p-value | VIPb |
|---|---|---|---|---|---|---|---|---|
| Amino acids and derivatives | ||||||||
| Valine | C5H11NO2 | 7.146 | 72 | 55 | 5 | + 36 | 0.012 | 1.83 |
| Alanine | C3H7NO2 | 7.413 | 116 | 73 | 6 | + 25 | 0.045 | 1.34 |
| Isoleucine | C6H13NO2 | 8.480 | 86 | 79 | 7 | + 21 | 0.035 | 1.15 |
| Serine | C3H7NO3 | 9.682 | 132 | 8 | + 110 | 0.019a | 2.65 | |
| Glutamic acid | C5H9NO4 | 14.390 | 246 | 73 | 8 | + 27 | 0.047 | 1.26 |
| 4-Hydroxyproline | C5H9NO3 | 13.306 | 230 | 73 | 11 | + 55 | 0.042a | 2.18 |
| Organic acids | ||||||||
| Pyruvic acid | C3H4O3 | 6.587 | 174 | 89 | 6 | - 22 | 0.014 | 1.35 |
| 2-Hydroxybutyric acid | C4H8O3 | 7.788 | 131 | 147 | 6 | + 31 | 0.029a | 1.62 |
| 3-Hydroxybutyric acid | C4H8O3 | 8.350 | 147 | 73 | 9 | + 26 | 0.045 | 1.62 |
| Sugar alcohol | ||||||||
| Glycerol | C3H8O3 | 9.959 | 205 | 147 | 4 | + 21 | 0.048 | 1.05 |
| Fatty acids | ||||||||
| Myristic acid | C14H28O2 | 16.797 | 117 | 285 | 13 | + 20 | 0.047 | 1.03 |
| Palmitoleic acid | C16H30O2 | 18.577 | 311 | 75 | 17 | + 60 | 0.017a | 2.32 |
| Palmitic acid | C16H32O2 | 18.757 | 313 | 117 | 8 | + 29 | 0.041a | 1.28 |
| Linoleic acid | C18H32O2 | 20.304 | 75 | 67 | 8 | + 41 | 0.032a | 1.68 |
| Oleic acid | C18H34O2 | 20.346 | 339 | 117 | 11 | + 39 | 0.021a | 1.87 |
| Arachidonic acid | C20H32O2 | 21.684 | 91 | 73 | 12 | + 43 | 0.021 | 1.41 |
a p values corrected by Benjamin Hochberg (FDR correction),
bVIP values with Jack-Knife confidence intervals estimative not including 0, 95% confidence level, RT: retention time; CV for QC (%): CV obtained for the same feature within the set of quality control samples.; Change: percentage of change of the abundances, calculated as (Breast cancer-control)/control, the sign indicates the direction of change in BCP group.
Table 3. Compounds with statistical significance identified by metabolic fingerprinting using LC-MS(±).
| Compound name | Molecular formula | Molecular weight (DB) g/mol | RT (min) | Mass error (ppm) | CV for QC (%) | Change (%) | p-value | VIPb | DET | CON |
|---|---|---|---|---|---|---|---|---|---|---|
| Fatty acyl carnitines | ||||||||||
| Decanoylcarnitine | C17H33NO4 | 315.2409 | 11.085 | 0 | 8 | + 35 | 0.0091 | 1.75 | ESI+ | MS/MS |
| Decenoylcarnitine | C17H31NO4 | 313.2253 | 9.079 | 0 | 7 | + 22 | 0.079 | 1.18 | ESI+ | MS/MS |
| Dodecenoylcarnitine | C19H35NO4 | 341.2566 | 12.982 | 2 | 9 | + 48 | 0.011a | 2.12 | ESI+ | MS/MS |
| Laurylcarnitine | C19H37NO4 | 343.2722 | 14.813 | 1 | 9 | + 45 | 0.011a | 2.06 | ESI+ | MS/MS |
| Linoleyl carnitine | C25H45NO4 | 423.3348 | 20.040 | 1 | 10 | + 20 | 0.010 | 0.97 | ESI+ | Putative |
| Myristoylcarnitine | C21H41NO4 | 371.3035 | 18.065 | 0 | 12 | + 36 | 0.011a | 1.82 | ESI+ | MS/MS |
| Oleoylcarnitine | C25H47NO4 | 425.3505 | 21.912 | 1 | 9 | + 29 | 0.0083 | 1.48 | ESI+ | Putative |
| Palmitoylcarnitine | C23H45NO4 | 399.3348 | 21.154 | 0 | 9 | + 21 | 0.0077 | 1.26 | ESI+ | MS/MS |
| Tetradecadiencarnitine | C21H37NO4 | 367.2722 | 14.597 | 2 | 9 | + 46 | 0.021a | 2.01 | ESI+ | MS/MS |
| Tetradecenoylcarnitine | C21H39NO4 | 369.2879 | 16.351 | 0 | 26 | + 54 | 0.0044a | 2.42 | ESI+ | MS/MS |
| Glycerophospholipids | ||||||||||
| cPA(18:0) | C21H41O6P | 420.2641 | 11.383 | 6 | 24 | - 45 | 0.040a | 1.68 | ESI- | Putative |
| LPC(16:1) | C24H48NO7P | 493.3168 | 18.548 | 1 | 11 | + 26 | 0.0064a | 1.73 | ESI+ | MS/MS |
| LPC(18:1) | C26H52NO7P | 521.3481 | 22.415 | 0 | 11 | + 27 | 0.017a | 2.07 | ESI+ | MS/MS |
| LPC(18:4) | C26H46NO7P | 515.3012 | 20.066 | 5 | 19 | + 29 | 0.014a | 1.33 | ESI- | Putative |
| LPC(20:4) | C28H48NO8P | 557.3118 | 19.477 | 4 | 17 | + 24 | 0.033a | 1.21 | ESI- | Putative |
| LPE(18:0) | C23H48NO7P | 481.3168 | 21.090 | 17 | 22 | + 49 | 0.017b | 1.90 | ESI- | Putative |
| LPE(18:1) | C23H46NO7P | 479.3012 | 19.473 | 16 | 19 | + 29 | 0.015a | 1.39 | ESI- | Putative |
| PA(32:0) | C35H69O8P | 648.4730 | 31.822 | 4 | 8 | + 35 | 0.00067a | 1.74 | ESI- | Putative |
| PA(P-31:1) | C34H65O7P | 616.4468 | 28.111 | 8 | 19 | + 52 | 0.011a | 1.95 | ESI- | Putative |
| PG(22:0) | C28H57O9P | 568.3740 | 10.833 | 1 | 24 | + 50 | 0.014 | 1.52 | ESI- | Putative |
| Fatty Acids | ||||||||||
| 11’-Carboxy-γ-tocotrienol | C25H36O4 | 400.2614 | 31.615 | 14 | 24 | + 70 | 0.000059a | 2.37 | ESI- | Putative |
| 9’-Carboxy-γ-tocotrienol | C23H32O4 | 372.2301 | 28.888 | 13 | 16 | + 41 | 0.0030a | 1.74 | ESI- | Putative |
| γ-Homolinolenic acid | C20H34O2 | 306.2550 | 31.203 | 12 | 25 | + 76 | 9.7E-07a | 2.68 | ESI- | Putative |
| Adrenic acid | C22H36O2 | 332.2710 | 31.616 | 17 | 14 | + 62 | 0.00074a | 2.15 | ESI- | Putative |
| Arachidonic acid | C20H32O2 | 304.2402 | 28.976 | 2 | 10 | + 45 | 0.014 | 2.28 | ESI± | MS/MS |
| Docosapentaenoic acid | C22H34O2 | 330.2559 | 29.592 | 17 | 20 | + 49 | 0.0045a | 1.73 | ESI- | Putative |
| 12-HETE | C20H32O3 | 320.2351 | 26.800 | 14 | 16 | + 35 | 0.017 | 1.35 | ESI- | Putative |
| Linoleic acid | C18H32O2 | 280.2400 | 29.349 | 2 | 22 | + 50 | 0.00019 | 2.65 | ESI± | MS/MS |
| Oleic acid | C18H34O2 | 282.2550 | 31.955 | 6 | 5 | + 43 | 0.0019a | 2.29 | ESI± | MS/MS |
| Palmitic acid | C16H32O2 | 256.2400 | 31.255 | 2 | 17 | + 34 | 0.0044a | 2.04 | ESI± | MS/MS |
a p values corrected by Benjamin Hochberg (FDR correction),
b VIP values with Jack-Knife confidence intervals estimative not including 0, 95% confidence level, RT: retention time; CV for QC (%): CV obtained for the same feature within the set of quality control samples; Change: percentage of change of the abundances, calculated as (Breast cancer-control)/control, the sign indicates the direction of change in BCP group; DET: detection mode; CON: confirmation.
Table 4. Compounds with statistical significance identified by lipid fingerprinting using LC-MS(±).
| Compound name | Molecular formula | Mass (Da) | RT | Mass error (ppm) | CV for QC (%) | Change (%) | p-value | VIPb | DET | CON | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Oleic acid | C18H36O2 | 356.2927 | 5.77 | 2 | 21 | + | 34 | 0.026 | 1.85 | ESI+ | MS/MS |
| Stearic acid | C18H36O2 | 284.4772 | 7.35 | 0 | 15 | + | 35 | 0.007 | 2.25 | ESI- | MS/MS |
| Monoacylglycerides | |||||||||||
| MG(18:1) | C21H40O4 | 356.2927 | 22.940 | 2 | 30 | + | 95 | 0.0027a | 1.98 | ESI+ | Putative |
| MG(18:2) | C21H38O4 | 354.2770 | 22.520 | 3 | 27 | + | 80 | 0.000057a | 2.24 | ESI+ | MS/MS |
| Diacylglycerides | |||||||||||
| DG(32:1) | C35H66O5 | 566.4910 | 21.550 | 3 | 24 | + | 77 | 0.012a | 1.62 | ESI+ | Putative |
| DG(34:1) | C37H70O5 | 594.5223 | 22.980 | 1 | 25 | + | 77 | 0.0019a | 1.85 | ESI+ | Putative |
| DG(34:2) | C37H68O5 | 592.5067 | 22.050 | 1 | 21 | + | 88 | 0.000049a | 2.28 | ESI+ | Putative |
| DG(34:3) | C37H66O5 | 590.4910 | 21.080 | 0 | 19 | + | 84 | 0.000076a | 2.32 | ESI+ | MS/MS |
| DG(36:2) | C37H72O5 | 620.5380 | 23.420 | 0 | 24 | + | 68 | 0.00035a | 1.94 | ESI+ | Putative |
| DG(36:4) | C39H68O5 | 616.5067 | 17.560 | 2 | 28 | + | 46 | 0.0039a | 1.51 | ESI+ | Putative |
| DG(38:3) | C41H74O5 | 646.5536 | 19.740 | 0 | 21 | + | 32 | 0.0062a | 1.35 | ESI+ | Putative |
| DG(40:4) | C39H68O5 | 616.5067 | 21.600 | 1 | 22 | + | 75 | 0.00033b | 2.09 | ESI+ | Putative |
| Triacylglycerides | |||||||||||
| TG(48:0) | C51H98O6 | 806.7363 | 31.700 | 1 | 10 | + | 41 | 0.00072a | 1.56 | ESI+ | MS/MS |
| TG(48:1) | C51H96O6 | 804.7207 | 30.380 | 3 | 13 | + | 56 | 0.00019a | 1.92 | ESI+ | MS/MS |
| TG(48:2) | C51H96O6 | 802.7050 | 31.090 | 1 | 24 | + | 63 | 0.028a | 1.59 | ESI+ | MS/MS |
| TG(48:3) | C51H92O6 | 800.6894 | 29.890 | 1 | 28 | + | 56 | 0.023a | 1.58 | ESI+ | MS/MS |
| TG(50:0) | C53H102O6 | 834.7676 | 33.980 | 3 | 12 | + | 36 | 0.00025a | 1.61 | ESI+ | Putative |
| TG(50:1) | C53H100O6 | 832.7520 | 33.260 | 8 | 21 | + | 70 | 0.0019a | 1.88 | ESI+ | Putative |
| TG(50:2) | C53H98O6 | 830.7363 | 31.700 | 15 | 18 | + | 87 | 0.0013a | 2.27 | ESI+ | Putative |
| TG(50:3) | C53H96O6 | 828.7207 | 31.690 | 1 | 17 | + | 89 | 0.00015a | 2.28 | ESI+ | MS/MS |
| TG(50:4) | C53H94O6 | 844.7389 | 30.380 | 3 | 27 | + | 99 | 0.000053a | 2.43 | ESI+ | MS/MS |
| TG(52:0) | C55H106O6 | 862.7989 | 37.050 | 2 | 26 | + | 71 | 0.00083a | 1.94 | ESI+ | MS/MS |
| TG(52:1) | C55H104O6 | 860.7833 | 34.890 | 5 | 16 | + | 52 | 0.00027a | 1.85 | ESI+ | MS/MS |
| TG(52:2) | C55H102O6 | 858.7676 | 34.000 | 10 | 14 | + | 45 | 0.00019a | 1.80 | ESI+ | MS/MS |
| TG(52:3) | C55H100O6 | 856.7520 | 32.360 | 9 | 15 | + | 66 | 0.000071a | 2.05 | ESI+ | MS/MS |
| TG(52:4) | C55H98O6 | 854.7363 | 32.360 | 1 | 14 | + | 66 | 0.00019a | 2.02 | ESI+ | MS/MS |
| TG(52:5) | C55H96O6 | 852.7207 | 30.990 | 0 | 21 | + | 79 | 0.0012a | 2.17 | ESI+ | MS/MS |
| TG(54:2) | C57H106O6 | 886.7989 | 36.840 | 9 | 18 | + | 64 | 0.000076a | 2.08 | ESI+ | MS/MS |
| TG(54:3) | C57H104O6 | 884.7833 | 37.070 | 1 | 30 | + | 90 | 0.00077a | 2.13 | ESI+ | MS/MS |
| TG(54:4) | C57H102O6 | 882.7676 | 34.900 | 1 | 19 | + | 63 | 0.00022a | 2.02 | ESI+ | MS/MS |
| TG(54:5) | C57H100O6 | 880.7520 | 33.890 | 1 | 20 | + | 69 | 0.00053a | 1.97 | ESI+ | Putative |
| TG(54:6) | C57H98O6 | 878.7363 | 31.590 | 2 | 10 | + | 77 | 0.00063a | 2.08 | ESI+ | MS/MS |
| TG(56:5) | C59H104O6 | 908.7833 | 36.100 | 0 | 16 | + | 77 | 0.0053a | 2.17 | ESI+ | MS/MS |
| TG(56:6) | C59H102O6 | 906.7676 | 34.790 | 0 | 23 | + | 96 | 0.000014a | 2.60 | ESI+ | MS/MS |
| TG(56:7) | C59H100O6 | 904.7520 | 33.300 | 0 | 19 | + | 87 | 0.0000093a | 2.39 | ESI+ | MS/MS |
| TG(56:8) | C59H98O6 | 902.7363 | 31.730 | 3 | 16 | + | 115 | 0.0000052a | 2.65 | ESI+ | MS/MS |
| TG(58:9) | C61H100O6 | 928.7520 | 32.450 | 0 | 9 | + | 72 | 0.0000093a | 2.22 | ESI+ | Putative |
| Phosphatidylcholines | |||||||||||
| PC(P-31:1) | C39H76NO7P | 701.5359 | 20.740 | 4 | 16 | + | 33 | 0.0036a | 1.35 | ESI+ | MS/MS |
| PC(32:1) | C40H78NO8P | 731.5465 | 20.680 | 0 | 18 | + | 40 | 0.0027a | 1.49 | ESI+ | MS/MS |
| PC(36:0) | C44H88NO8P | 789.6248 | 21.810 | 6 | 23 | + | 44 | 0.0019a | 1.60 | ESI+ | MS/MS |
| PC(36:1) | C44H86NO8P | 787.6091 | 21.790 | 0 | 23 | + | 49 | 0.0018a | 1.68 | ESI+ | MS/MS |
| PC(O-36:4) | C44H82NO7P | 765.5672 | 21.330 | 1 | 21 | + | 40 | 0.000058a | 1.76 | ESI+ | MS/MS |
| PC(38:4) | C46H84NO8P | 809.5935 | 21.810 | 10 | 23 | + | 41 | 0.0021a | 1.54 | ESI+ | MS/MS |
| PC(P-38:4) | C46H84NO7P | 793.5985 | 22.130 | 2 | 28 | + | 34 | 0.0066a | 1.36 | ESI+ | MS/MS |
| PC(38:6) | C46H80NO8P | 805.5622 | 19.520 | 0 | 13 | + | 36 | 0.0000014a | 1.68 | ESI+ | MS/MS |
| PC(38:7) | C46H78NO8P | 803.5465 | 19.540 | 0 | 13 | + | 35 | 0.00016a | 1.67 | ESI+ | MS/MS |
| PC(40:5) | C48H86NO8P | 835.6091 | 21.980 | 0 | 23 | + | 43 | 0.00017a | 1.65 | ESI+ | MS/MS |
| PC(40:6) | C48H84NO8P | 833.5935 | 21.120 | 0 | 18 | + | 43 | 0.000014a | 1.80 | ESI+ | MS/MS |
| Sphingolipid | |||||||||||
| SM(d41:2) | C46H91N2O6P | 798.6615 | 22.740 | 1 | 26 | + | 34 | 0.0099a | 1.29 | ESI+ | MS/MS |
| SM(d42:2) | C47H93N2O6P | 812.6771 | 23.340 | 0 | 27 | + | 32 | 0.014a | 1.15 | ESI+ | MS/MS |
a p values corrected by Benjamin Hochberg (FDR correction),
bVIP values with Jack-Knife confidence intervals estimative not including 0, 95% confidence level, RT: retention time; CV for QC (%): CV obtained for the same feature within the set of quality control samples; Change: percentage of change of the abundances, calculated as (Breast cancer-control)/control, the sign indicates the direction of change in BCP group; DET: detection mode; CON: confirmation.
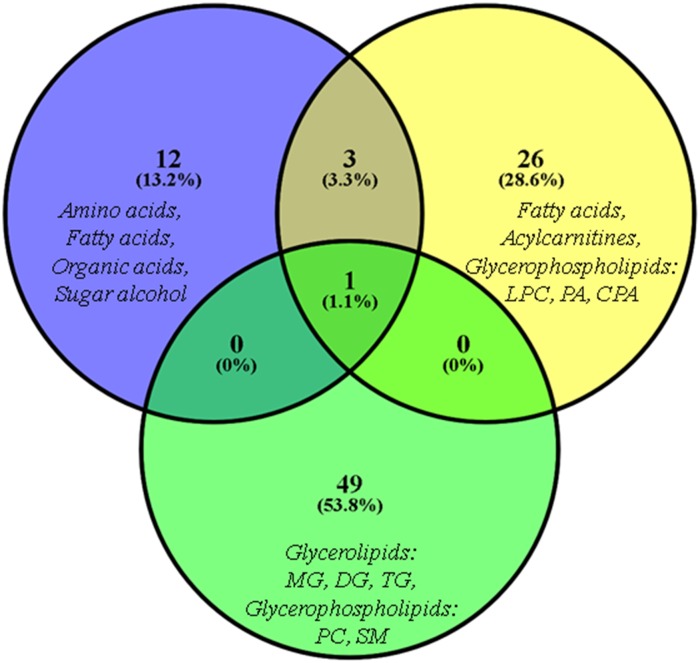
Fig 2. Venn diagram.
Venn diagram for the number of differentiating metabolites in BCP group identified in each chromatographic technique coupled to mass spectrometry (blue circle: MF/GC-MS, yellow circle: MF/LC-MS(±), green circle: LF/LC-MS(±).
For 1H-NMR analysis, a total of 519 chemical shifts in the spectral range were found statistically significant for group differentiation. These chemical shifts correspond to the region of lipids, lactate and the amino acid valine (Table 5). These regions were integrated and evaluated by UVA, and the data allows to conclude that lactate, valine and lipids were statistically significant with a p-value < 0.05.
Table 5. Chemical shifts of compounds with statistical significance identified by 1H-NMR.
| Metabolite | Assignment 1H (δ) | Multiplicity | Trend | p-value | VIP |
|---|---|---|---|---|---|
| Valine | 1.02 | d | ↑ | 0.019a | 1.41 |
| 1.07 | d | ↑ | 0.022a | 1.95 | |
| 2.31 | m | ↑ | 0.031a | 1.96 | |
| Alanine | 1.49 | d | ↑ | 0.025a | 2.18 |
| Lactate | 1.33 | d | ↑ | 0.0014a | 2.88 |
| 4.11 | q | ↑ | 0.0040a | 1.18 | |
| Lipids | 0.8 | m | ↑ | 0.014a | 2.25 |
| 1.28 | m | ↑ | 0.014 a | 1.27 | |
| 2.04 | m | ↑ | - | 1.16 | |
| 5.26–5.33 | m | ↑ | - | 1.64 |
a p values corrected by Benjamin Hochberg (FDR correction), Trend: Regulation in BCP group: ↑ Up regulated, ↓ Down regulated, VIP: variance important in projection from OPLS-DA model with Jack-Knife confidence intervals estimative not including 0, 95% confidence level.
Discussion
Our results show that a multiplatform approach for metabolic and lipid fingerprinting allows a wide coverage of different metabolite classes in plasma. The combination of these approaches enabled the detection of 1450 metabolites in total, of which 95 were significantly altered in BCP, including amino acids (7), organic acids (3), sugar alcohols (1), fatty acyls (15), fatty acylcarnitines (10), glycerophospholipids (24) and glycerolipids (35). Fig 2 compares the number of altered metabolites identified by MS-based platforms, where 13%, 27% and 49% of the alterations were determined exclusively by GC, MF/LC(±) and LF/LC(±), respectively. Only oleic acid was common on all platforms.
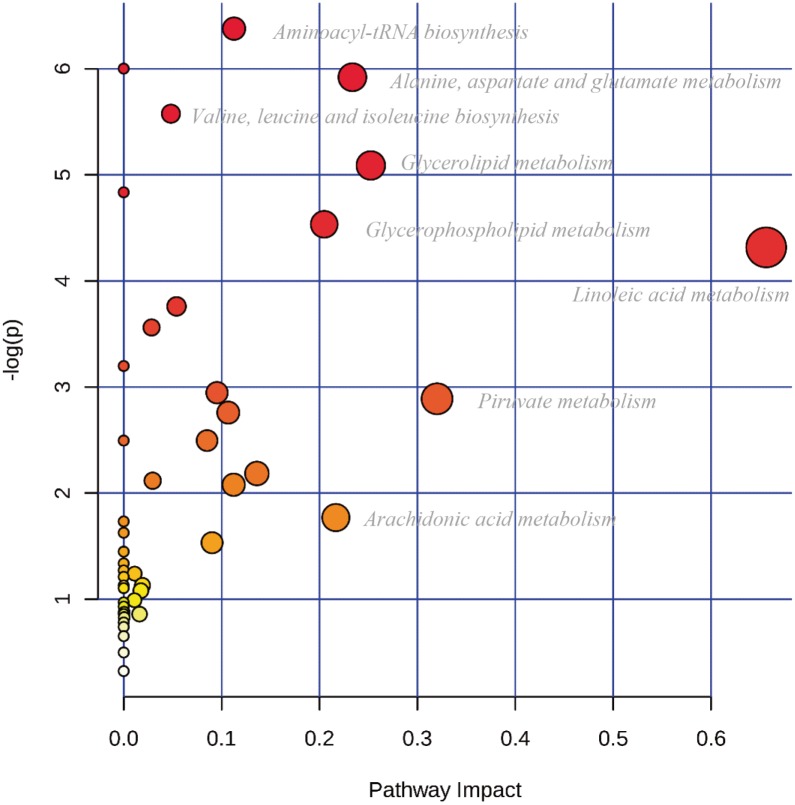
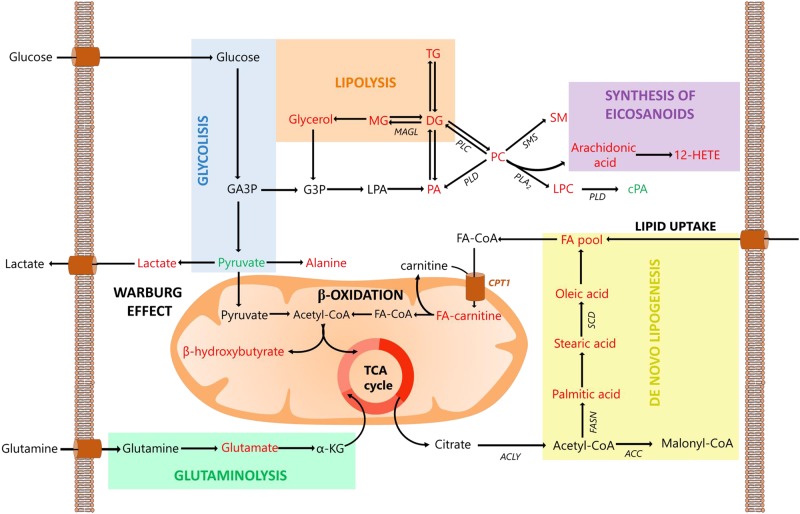
The pathway analysis shows perturbations in the biosynthesis of aminoacyl-tRNA and several amino acids, as well as in the metabolism of fatty acids, glycerolipids and glycerophospholipids (Fig 3 and S3 Table). GC-MS and NMR both identify shifts in the glycolytic pathway [14]. The observed down-regulation of pyruvic acid and the up-regulation of lactic acid and alanine (Tables 1 and 4) are in accordance with the Warburg effect [58]. In cancer cells, energy metabolism shifts occur in order to generate energy, mainly by pyruvate to lactate conversion, regardless of oxygen concentration [59]. This generates a decrease in pyruvate and an increase in lactate. The depletion of pyruvate also affects the tricarboxylic acid (TCA) cycle. Cancer cells promote the conversion of glutamine to glutamic acid via glutaminolysis in order to maintain the TCA cycle [12, 60–62] and to provide amino groups for serine biosynthesis. Both glutamic acid and serine were detected as significantly upregulated (Table 2).
Fig 3. Pathway analysis.
Pathway analysis displaying metabolic pathways arranged by scores from pathway enrichment (y axis) and from topology analysis (x axis) using MetaboAnalyst 3.0 tool. The color and size of each circle is based on p-values and pathway impact values, respectively [57].
All three analytical platforms were consistent in indicating an overall upregulation of fatty acyls (FA) (Tables 1–4). This is expected considering that FA can be used as signalling molecules and an energy source in themselves, and also as building blocks for the synthesis of complex lipids. For that reason, FA are crucial to maintaining cancer cell proliferation, migration, survival and tissue invasion [13]. In breast cancer, a high demand of FA from de novo synthesis has been reported [63] as a response to the overexpression of several enzymes, such as fatty acid synthase (FASN) [23, 64], acetyl-CoA carboxylase (ACC) and ATP citrate lyase (ACLY) [65]. The differentiating FA included palmitic (16:0), oleic (18:1), linoleic (18:2) and arachidonic acids (20:4), as well as 12-HETE, which have been proposed as potential biomarkers in breast cancer [62, 66]. For instance, linoleic acid can modulate BRCA1 gene expression and increase 12-HETE and 15-HETE production in BC [67], thereby promoting proliferation, angiogenesis and immunomodulation in tumors [68].
FA can also be consumed through β-oxidation, producing key substituents to providing the energy needed for cancer cell survival [69]. For this purpose, carnitines are used as shuttle system to transport long chain FA inside the mitochondria. Carnitine palmitoyltransferase 1 (CPT1), which catalyzes the transfer of the fatty acid moiety from acyl-coenzyme A (CoA) to a long-chain acylcarnitine, has been reported as overexpressed in breast cancer [70, 71]. Moreover, increased levels of several carnitines in BC were reported by Shen et al., including hexanoylcarnitine, octanoylcarnitine and cis-4-decenoylcarnitine [13]. Therefore, the up-regulation of (16:0), (18:1) and (18:2) fatty acyl carnitines shown in Table 3, suggest transport of de novo synthetized FA to mitochondria, where they are used to energy production via β-oxidation. This is also supported by the up-regulation of the 3-hydroxybutyric acid (a ketone body), observed by GC-MS. An overview of the basic relationships between the pathways described is presented in Fig 4.
Fig 4. Significant altered pathways in breast cancer.
Significant altered pathways in breast cancer according to multiplatform findings in blood plasma. In red up-regulated and in green down-regulated metabolites. Abbreviations: 12-HETE, 12-hydroxyeicosatrienoic acid; α-KG, α-ketoglutarate; ACC, acetyl-CoA carboxylase; ACLY, acetyl-CoA lyase; cPA, cyclic phosphatidic acid; CPT1, carnitine palmitoyltransferase I; DG, diacylglycerides; FA, fatty acid; FA-CoA, fatty acyl-CoA; FA-carnitine, fatty acyl-carnitine; FASN, fatty acid synthase; GA3P, glyceraldehyde 3-phosphate; G3P, glycerol 3-phosphate; LPA, lysophosphatidic acid; LPC, lysophosphatidylcholine; MAGL, monoacylglycerol lipase; MG, monoacyl glycerides; PA, phosphatidic acid; PC, phosphatidylcholine; PLA2, phospholipase A2; PLC, phospholipase C; PLD, phospholipase D; SCD, stearoyl-CoA desaturase; SM, sphingomyelin; SMS, sphingomyelin synthase; TCA cycle, tricarboxylic acid cycle; TG, triacylglycerides.
A comprehensive understanding of the perturbations in glycerophospolipid metabolism was established both by metabolic and lipid approaches based on LC-MS. While LF/LC-MS(±) analysis found alterations in phosphatidylcholines (PC), MF/LC-MS(±) analysis found changes in phosphatidic acid (PA), lysophosphatidylcholines (LPC) and lysophosphatidylethanolamines (LPE). PC are the most common glycerophospholipids because of their structural roles and since they serve as a precursor of signalling molecules such as arachidonic acid, diacylglycerol (DG) and PA [72–74]. The relevance of PC has been examined in several studies which have determined alterations in BC samples [75–77]. As shown in Table 4, all differentiating PC species were found up-regulated in the BCP group, including some already reported as PC(32:1) [78–81], PC(36:0) [45], PC(36:1) [78–80], PC(38:4) [78] [79], PC(40:5) [17], and PC(40:6) [17, 79]. It has been suggested that PC accumulation in BC is caused by an unbalance between a high activity of the enzyme choline kinase in the anabolic pathway [73, 82, 83] and the activity of the enzymes phospholipases A2 (PLA2), phospholipase C (PLC) and phospholipase D (PLD) in the catabolic pathway [73, 84–87].
Lysophospholipids can be produced by PLA2 activity over PC and others glycerophospholipids. Lyso-type lipids have specific actions in cancer cells, such as activation of specific G-protein coupled receptors by LPC [88] or the increase of intracellular Ca2+ by LPE [89]. Therefore, the observed up-regulation of LPC and LPE species are suggested to play a role in cancer cell signaling, in agreement with previous published studies that found alterations in LPC (16:1), LPC (18:1) [17, 90, 91], LPC (20:4) [45, 92], LPE (18:0) [91], LPE (18:1) [91]. PC cleavage can also be performed by PLD to generate PA, such as the PA (32:0) and PA(P-31:1) found in this study. These acids can act as messengers that directly binds to the mammalian target of rapamycin (mTOR) to activate this anti-apoptotic pathway [93].
Nevertheless, a structural analogue of lysophosphatidic acid (LPA), the cyclic phosphatidic acid cPA (18:0) was found to be down-regulated (Table 3), which is consistent with its activity to inhibit cell proliferation, platelet aggregation, and metastasis in cancer [94]. To our present knowledge, it is the first report of cPA alterations in breast cancer plasma samples.
Finally, lipid fingerprinting by LC-MS(±) was the only analytical platform able to detect glycerolipids as differential metabolites (S2 Table). As shown in Table 4, several MG, DG and TG species were found up-regulated in the BCP group, which is consistent with previous reports in breast cancer [46, 91, 95–97]. MG can be used as a source of FA in cancer cells in order to maintain an FA pool always available, given the overexpression of monoacylglycerol lipase (MAGL) as reported by Nomura et al [98]. DG are important intermediates of the lipid metabolism and cellular signalling. Several studies have reported alterations in DG concentrations in diseases like breast cancer [46] and various other cancer types [99], by affecting the protein kinase C (PKC) [86, 100, 101]. TG are central to energy storage and as a source of building blocks for complex lipids; therefore, high TG levels have been associated with breast cancer progression and aggressiveness [102–106]. Raised TG production has been suggested as a cell strategy to decrease the cytotoxicity generated by the high amount of free FA in the cytoplasm [107, 108]. Although TG upregulation also could be related to the dietary fat, a direct link to BC has not been proven [95, 96].
Previous studies on BC in Colombian women of Hispanic origin have been focused on genomics. These studies have revealed several disparities in the gene mutations spectra when compared to other Hispanic families in United States [109] or other Central/South America countries [110, 111]. Considering that genotypic differences can be related with phenotypic ones, the present study provides an insight into the alterations of plasma metabolites in Colombian women, which is helpful for further personalized and population-based medicine approaches. A comprehensive view of all the alterations found in this multiplatform study are in accordance with the general plasma metabolic signatures associated with BC for other populations, including the glycolytic pathway, amino acid and lipid metabolism. However, some of the differentiating metabolites have not yet been reported for BC, such as cPA and several FAcyl-carnitines, which might be reflecting genotype and environmental disparities of BC in Latin woman of Hispanic origin. Although this pilot study allowed the exploration of metabolic perturbations in Colombian Hispanic women with BC, it will be important to consider for further targeted studies and/or biomarker validation a much larger cohort of women with BC in early stage, without any previously treatment.
Conclusion
Through metabolic and lipid fingerprinting, a comprehensive characterization of metabolite alterations of breast cancer in Colombian Hispanic women was achieved. This multiplatform study demonstrated the complementarity of the different analytical technologies in non-target approaches, allowing to observe modifications in a wide range of metabolite levels. Altered metabolites belonging to glutaminolysis, amino acids, fatty acids, glycerolipid and glycerophospholipid metabolism were observed. Most of the alterations found agreed with the metabolic signatures reported previously for BC; nevertheless, in this study, new metabolites were observed that had not yet been reported, such as the down-regulation of cyclic phosphatidic acid cPA (18:0) or the up-regulation of several long fatty acylcarnitines. These findings not only provided a map of metabolic perturbations in BC, but also demonstrated that the metabolic signature of BC in Hispanic women is comparable to the metabolic signature reported for Asian, European and North American women, regardless of the large variations in this heterogeneous disease. Determining metabolic disturbances in specific populations may be promising for patient stratification, regarding the selection of an appropriate therapy or the development of new therapeutic targets.
Supporting information
Comparison of GC-MS chromatograms (truncated at 30 minutes) for breast cancer (green) and control (blue). Identified metabolites: 1. N-Ethylglycine I. 2. Pyruvic acid. 3. Lactic acid. 4. Glycolic acid. 5. Valine I. 6. Alanine I. 7. 2-Ketoisocaproic acid I. 8. Acetoacetate I. 9. Glycine I. 10. 2-Hydroxybutyric acid I. 11. Sarcosine. 12. Acetoacetate II. 13. Oxalic acid. 14. p-Cresol. 15. Leucine I. 16. 3-Hydroxybutyric acid. 17. 2-etoisocaproic acid I. 18. N-methylalanine. 19. Proline I. 20. Isoleucine I. 21. 2-Ketoisocaproic acid II. 22. Malonic acid I. 23. Valine II. 24. Glyceraldehyde II. 25. Benzoic acid. 26. Urea. 27. Serine I. 28. Caprylic acid. 29. Leucine II. 30. Glycerol. 31. Phosphoric acid. 32. Threonine I. 33. Isoleucine II. 34. Proline II. 35. Glycine. 36. Glyceric acid. 37. Fumaric acid. 38. Serine II. 39. Pipecolic acid II. 40. Threonine II. 41. Aspartic acid I. 42. 3-Aminoisobutyric acid II. 43. Iminodiacetic acid I. 44. Threose II. 45. Aminomalonic acid. 46. Threitol. 47. Methionine II. 48. Pyroglutamic acid. 49. trans-4-Hydroxy-L-proline II. 50. Iminodiacetic acid II. 51. Phenylalanine I. 52. Creatinine. 53. Glutamic acid II. 54. Phenylalanine II. 55. Lauric acid. 56. Asparagine II. 57. Pyrophosphate. 58. Arabitol. 59. Xylitol. 60. Glutamine III. 61. Shikimic acid. 62. Hypoxanthine I. 63. OrnithineII. 64. Citric acid. 65. Myristic acid. 66. Galactopyranoside. 67. Pyranose (Glucose/Altrose/Galactose/Talose). 68. Furanose (Tagatose I). 69. p-Hydroxyphenyllactic acid. 70. Gluconic acid lactone I. 71. Tagatose II. 72. Fructose I. 73. Fructose II + Glucose. 74. Glucose. 75. Glucose. 76. Sorbitol. 77. Tyrosine II. 78. 3-Indoleacetic acid. 79. Galactopyranoside. 80. Palmitoleic acid. 81. Palmitic acid. 82. Uric acid I. 83. Methyl stearate (IS). 84. Tryptophan II. 85. Linoleic acid. 86. Oleic acid. 87. Arachidonic acid. 88. 1-Monomyristin. 89. Lactose II. 90. 5-Hydroxy-L-tryptophan I. 91. 2-Palmitoylglycerol. 92 1-Monopalmitin. 93. 2-Monostearin. 94. Glycerol monostearate. 95. Cholesterol.
(DOCX)
Comparison of LC-MS base peak chromatograms for breast cancer (green) and control (blue). Panel A. Metabolic fingerprinting by LC-MS. B. Lipid fingerprinting by LC-MS. The marked windows are according to the compound class and their elution time.
(DOCX)
Comparison of 1H-NMR spectra for breast cancer (green) and control (blue). Chemical shifts of compounds with statistical significance are expanded.
(DOCX)
PCA score plots for data set filtered by presence and reproducibility (green dots: breast cancer group; blue dots. control group; orange diamonds: quality control). Panel: A. MF by GC-MS. B. MF by NMR. C. MF by LC-MS(+)D. MF by LC-MS(-)E. LF by LC-MS(+). F. LF by LC-MS(-).
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Acknowledgments
The authors thank to the Centre of Metabolomics and Bioanalysis (CEMBIO) from the University of San Pablo Madrid, Spain for the technical support. The authors would like to thank all the voluntary participants of the study, Liga Contra el Cancer (Bogotá, Colombia) and CliniSalud Medical Center (Socorro, Colombia). We are grateful with Juan Sebastian Carreño for his assistance during the NMR analysis of plasma samples.
Data Availability
All relevant data are available from Metabolomics Workbench at the following URL: http://dx.doi.org/10.21228/M8QM3R.
Funding Statement
This study was financially supported by the Proyecto Semilla (Call for funding 2015-1, doctoral candidates) from the Faculty of Sciences of Universidad de los Andes, Bogotá D.C., Colombia to MPCM.
References
- 1.Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. International Journal of Cancer. 2015;136(5):E359–E86. 10.1002/ijc.29210 [DOI] [PubMed] [Google Scholar]
- 2.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA: A Cancer Journal for Clinicians. 2015;65(1):5–29. 10.3322/caac.21254 [DOI] [PubMed] [Google Scholar]
- 3.Welcsh PL, King M-C. BRCA1 and BRCA2 and the genetics of breast and ovarian cancer. Human Molecular Genetics. 2001;10(7):705–13. 10.1093/hmg/10.7.705 [DOI] [PubMed] [Google Scholar]
- 4.Marcus JN, Page DL, Watson P, Narod SA, Lenoir GM, Lynch HT. BRCA1 and BRCA2 hereditary breast carcinoma phenotypes. Cancer. 1997;80(S3):543–56. [DOI] [PubMed] [Google Scholar]
- 5.Mourtada-Maarabouni M, Hasan AM, Farzaneh F, Williams GT. Inhibition of human T-cell proliferation by mammalian target of rapamycin (mTOR) antagonists requires noncoding RNA growth-arrest-specific transcript 5 (GAS5). Mol Pharmacol. 2010;78(1):19–28. Epub 2010/04/28. 10.1124/mol.110.064055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morse-Gaudio M, Connolly JM, Rose DP. Protein kinase C and its isoforms in human breast cancer cells: relationship to the invasive phenotype. Int J Oncol. 1998;12(6):1349–54. Epub 1998/06/04. . [DOI] [PubMed] [Google Scholar]
- 7.von Lintig FC, Dreilinger AD, Varki NM, Wallace AM, Casteel DE, Boss GR. Ras activation in human breast cancer. Breast Cancer Res Treat. 2000;62(1):51–62. Epub 2000/09/16. . [DOI] [PubMed] [Google Scholar]
- 8.Wishart SD, Mandal R, Stanislaus A, Ramirez-Gaona M. Cancer Metabolomics and the Human Metabolome Database. Metabolites. 2016;6(1). 10.3390/metabo6010010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Spratlin JL, Serkova NJ, Gail Eckhardt S. Clinical Applications of Metabolomics in Oncology: A Review. Clinical cancer research: an official journal of the American Association for Cancer Research. 2009;15(2):431–40. 10.1158/1078-0432.CCR-08-1059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Armitage EG, Southam AD. Monitoring cancer prognosis, diagnosis and treatment efficacy using metabolomics and lipidomics. Metabolomics. 2016;12(9):146 10.1007/s11306-016-1093-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mishra P, Ambs S. Metabolic Signatures of Human Breast Cancer. LID—e992217. (2372–3556 (Linking)). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Geck RC, Toker A. Nonessential amino acid metabolism in breast cancer. Advances in Biological Regulation. 2016;62:11–7. 10.1016/j.jbior.2016.01.001. [DOI] [PubMed] [Google Scholar]
- 13.Shen J, Yan L, Liu S, Ambrosone CB, Zhao H. Plasma Metabolomic Profiles in Breast Cancer Patients and Healthy Controls: By Race and Tumor Receptor Subtypes. Translational Oncology. 2013;6(6):757–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Budczies J, Denkert C, Muller BM, Brockmoller SF, Klauschen F, Gyorffy B, et al. Remodeling of central metabolism in invasive breast cancer compared to normal breast tissue—a GC-TOFMS based metabolomics study. Bmc Genomics. 2012;13 10.1186/1471-2164-13-334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen XL, Chen HK, Dai MY, Ai JM, Li Y, Mahon B, et al. Plasma lipidomics profiling identified lipid biomarkers in distinguishing early-stage breast cancer from benign lesions. Oncotarget. 2016;7(24):36622–31. 10.18632/oncotarget.9124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim H-Y, Lee K-M, Kim S-H, Kwon Y-J, Chun Y-J, Choi H-K. Comparative metabolic and lipidomic profiling of human breast cancer cells with different metastatic potentials. Oncotarget. 2016;7(41). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.You JC, Yang J, Fang RP, Hu N, Zhang XD, Zhang WY, et al. Analysis of phosphatidylcholines (PCs) and lysophosphatidylcholines (LysoPCs) in metastasis of breast cancer cells. Progress in Biochemistry and Biophysics. 2015;42(6):563–73. [Google Scholar]
- 18.Tenori L, Oakman C, Claudino WM, Bernini P, Cappadona S, Nepi S, et al. Exploration of serum metabolomic profiles and outcomes in women with metastatic breast cancer: a pilot study. Mol Oncol. 2012;6(4):437–44. Epub 2012/06/13. 10.1016/j.molonc.2012.05.003 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fan Y, Zhou X, Xia TS, Chen Z, Li J, Liu Q, et al. Human plasma metabolomics for identifying differential metabolites and predicting molecular subtypes of breast cancer. Oncotarget. 2016;7(9):9925–38. 10.18632/oncotarget.7155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim IC, Lee JH, Bang G, Choi SH, Kim YH, Kim KP, et al. Lipid profiles for HER2-positive breast cancer. Anticancer Res. 2013;33(6):2467–72. Epub 2013/06/12. . [PubMed] [Google Scholar]
- 21.Foulkes WD, Smith IE, Reis-Filho JS. Triple-negative breast cancer. N Engl J Med. 2010;363(20):1938–48. Epub 2010/11/12. 10.1056/NEJMra1001389 . [DOI] [PubMed] [Google Scholar]
- 22.Shajahan-Haq AN, Cheema MS, Clarke R. Application of Metabolomics in Drug Resistant Breast Cancer Research. Metabolites. 2015;5(1):100–18. 10.3390/metabo5010100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liu H, Liu Y, Zhang JT. A new mechanism of drug resistance in breast cancer cells: fatty acid synthase overexpression-mediated palmitate overproduction. Mol Cancer Ther. 2008;7(2):263–70. Epub 2008/02/19. 10.1158/1535-7163.MCT-07-0445 . [DOI] [PubMed] [Google Scholar]
- 24.Stewart DA, Winnike J, McRitchie S, Pathmasiri W, Sumner S. Triple negative breast cancer: Metabolomics and flux analysis to identify targets for drug development. Cancer Research. 2015;75 10.1158/1538-7445.am2015-1836 [DOI] [Google Scholar]
- 25.Stewart DA, Winnike JH, McRitchie SL, Clark RF, Pathmasiri WW, Sumner SJ. Metabolomics Analysis of Hormone-Responsive and Triple-Negative Breast Cancer Cell Responses to Paclitaxel Identify Key Metabolic Differences. Journal of Proteome Research. 2016;15(9):3225–40. 10.1021/acs.jproteome.6b00430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wei SW, Liu LY, Zhang J, Bowers J, Gowda GAN, Seeger H, et al. Metabolomics approach for predicting response to neoadjuvant chemotherapy for breast cancer. Molecular Oncology. 2013;7(3):297–307. 10.1016/j.molonc.2012.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Alonso A, Marsal S, Julià A. Analytical Methods in Untargeted Metabolomics: State of the Art in 2015. Frontiers in Bioengineering and Biotechnology. 2015;3(23). 10.3389/fbioe.2015.00023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schrimpe-Rutledge AC, Codreanu SG, Sherrod SD, McLean JA. Untargeted Metabolomics Strategies—Challenges and Emerging Directions. Journal of The American Society for Mass Spectrometry. 2016;27(12):1897–905. 10.1007/s13361-016-1469-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Worley B, Powers R. Multivariate Analysis in Metabolomics. Current Metabolomics. 2013;1(1):92–107. 10.2174/2213235X11301010092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liland KH. Multivariate methods in metabolomics—from pre-processing to dimension reduction and statistical analysis. TrAC Trends in Analytical Chemistry. 2011;30(6):827–41. 10.1016/j.trac.2011.02.007. [DOI] [Google Scholar]
- 31.Yin P, Xu G. Current state-of-the-art of nontargeted metabolomics based on liquid chromatography—mass spectrometry with special emphasis in clinical applications. Journal of Chromatography A. 2014;1374:1–13. 10.1016/j.chroma.2014.11.050. [DOI] [PubMed] [Google Scholar]
- 32.Wishart DS. Emerging applications of metabolomics in drug discovery and precision medicine. Nat Rev Drug Discov. 2016;15(7):473–84. 10.1038/nrd.2016.32 [DOI] [PubMed] [Google Scholar]
- 33.Sethi S, Brietzke E. Recent advances in lipidomics: Analytical and clinical perspectives. Prostaglandins & Other Lipid Mediators. 2017;128–129:8–16. 10.1016/j.prostaglandins.2016.12.002. [DOI] [PubMed] [Google Scholar]
- 34.Armitage EG, Barbas C. Metabolomics in cancer biomarker discovery: current trends and future perspectives. (1873-264X (Electronic)). [DOI] [PubMed] [Google Scholar]
- 35.Gunther UL. Metabolomics Biomarkers for Breast Cancer. Pathobiology. 2015;82(3–4):153–65. 10.1159/000430844 [DOI] [PubMed] [Google Scholar]
- 36.Oakman C, Tenori L, Claudino WM, Cappadona S, Nepi S, Battaglia A, et al. Identification of a serum-detectable metabolomic fingerprint potentially correlated with the presence of micrometastatic disease in early breast cancer patients at varying risks of disease relapse by traditional prognostic methods. Ann Oncol. 2011;22(6):1295–301. Epub 2011/01/05. 10.1093/annonc/mdq606 . [DOI] [PubMed] [Google Scholar]
- 37.Jobard E, Pontoizeau C, Blaise BJ, Bachelot T, Elena-Herrmann B, Tredan O. A serum nuclear magnetic resonance-based metabolomic signature of advanced metastatic human breast cancer. Cancer Lett. 2014;343(1):33–41. Epub 2013/09/18. 10.1016/j.canlet.2013.09.011 . [DOI] [PubMed] [Google Scholar]
- 38.Asiago VM, Alvarado LZ, Shanaiah N, Gowda GAN, Owusu-Sarfo K, Ballas R, et al. Early Detection of Recurrent Breast Cancer Using Metabolite Profiling. Cancer research. 2010;70(21):8309–18. 10.1158/0008-5472.CAN-10-1319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Miyagi Y, Higashiyama M, Gochi A, Akaike M, Ishikawa T, Miura T. Plasma free amino acid profiling of five types of cancer patients and its application for early detection. PLoS One. 2011;6 10.1371/journal.pone.0024143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lai HS, Lee JC, Lee PH, Wang ST, Chen WJ. Plasma free amino acid profile in cancer patients. Semin Cancer Biol. 2005;15 10.1016/j.semcancer.2005.04.003 [DOI] [PubMed] [Google Scholar]
- 41.Gu Y, Chen T, Fu S, Sun X, Wang L, Wang J, et al. Perioperative dynamics and significance of amino acid profiles in patients with cancer. Journal of Translational Medicine. 2015;13(1):35 10.1186/s12967-015-0408-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Qiu YP, Zhou BS, Su MM, Baxter S, Zheng XJ, Zhao XQ, et al. Mass Spectrometry-Based Quantitative Metabolomics Revealed a Distinct Lipid Profile in Breast Cancer Patients. International Journal of Molecular Sciences. 2013;14(4):8047–61. 10.3390/ijms14048047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cui M, Wang QL, Chen G. Serum metabolomics analysis reveals changes in signaling lipids in breast cancer patients. Biomedical Chromatography. 2016;30(1):42–7. 10.1002/bmc.3556 [DOI] [PubMed] [Google Scholar]
- 44.Hammad LA, Wu GX, Saleh MM, Klouckova I, Dobrolecki LE, Hickey RJ, et al. Elevated levels of hydroxylated phosphocholine lipids in the blood serum of breast cancer patients. Rapid Communications in Mass Spectrometry. 2009;23(6):863–76. 10.1002/rcm.3947 [DOI] [PubMed] [Google Scholar]
- 45.More TH, Bagadi M, RoyChoudhury S, Dutta M, Uppal A, Mane A, et al. Comprehensive quantitative lipidomic approach to investigate serum phospholipid alterations in breast cancer. Metabolomics. 2016;13(1):3 10.1007/s11306-016-1138-y [DOI] [Google Scholar]
- 46.Yang L, Cui X, Zhang N, Li M, Bai Y, Han X, et al. Comprehensive lipid profiling of plasma in patients with benign breast tumor and breast cancer reveals novel biomarkers. Analytical and Bioanalytical Chemistry. 2015;407(17):5065–77. 10.1007/s00216-015-8484-x [DOI] [PubMed] [Google Scholar]
- 47.Garcia A, Barbas C. Gas Chromatography-Mass Spectrometry (GC-MS)-Based Metabolomics In: Metz OT, editor. Metabolic Profiling: Methods and Protocols. Totowa, NJ: Humana Press; 2011. p. 191–204. [DOI] [PubMed] [Google Scholar]
- 48.Ciborowski M, Javier Ruperez F, Paz Martinez-Alcazar M, Angulo S, Radziwon P, Olszanski R, et al. Metabolomic Approach with LC-MS Reveals Significant Effect of Pressure on Diver’s Plasma. Journal of Proteome Research. 2010;9(8):4131–7. 10.1021/pr100331j [DOI] [PubMed] [Google Scholar]
- 49.Dona AC, Jiménez B, Schäfer H, Humpfer E, Spraul M, Lewis MR, et al. Precision High-Throughput Proton NMR Spectroscopy of Human Urine, Serum, and Plasma for Large-Scale Metabolic Phenotyping. Analytical Chemistry. 2014;86(19):9887–94. 10.1021/ac5025039 [DOI] [PubMed] [Google Scholar]
- 50.Arana VA, Medina J, Alarcon R, Moreno E, Heintz L, Schäfer H, et al. Coffee’s country of origin determined by NMR: The Colombian case. Food Chemistry. 2015;175:500–6. 10.1016/j.foodchem.2014.11.160. [DOI] [PubMed] [Google Scholar]
- 51.Whiley L, Godzien J, Ruperez FJ, Legido-Quigley C, Barbas C. In-Vial Dual Extraction for Direct LC-MS Analysis of Plasma for Comprehensive and Highly Reproducible Metabolic Fingerprinting. Analytical Chemistry. 2012;84(14):5992–9. 10.1021/ac300716u [DOI] [PubMed] [Google Scholar]
- 52.Gika HG, Macpherson E, Theodoridis GA, Wilson ID. Evaluation of the repeatability of ultra-performance liquid chromatography—TOF-MS for global metabolic profiling of human urine samples. Journal of Chromatography B. 2008;871(2):299–305. 10.1016/j.jchromb.2008.05.048. [DOI] [PubMed] [Google Scholar]
- 53.Godzien J, Alonso-Herranz V, Barbas C, Armitage EG. Controlling the quality of metabolomics data: new strategies to get the best out of the QC sample. Metabolomics. 2015;11(3):518–28. 10.1007/s11306-014-0712-4 [DOI] [Google Scholar]
- 54.Rubingh CM, Bijlsma S, Derks EPPA, Bobeldijk I, Verheij ER, Kochhar S, et al. Assessing the performance of statistical validation tools for megavariate metabolomics data. Metabolomics. 2006;2(2):53–61. 10.1007/s11306-006-0022-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Nicholson JK, Foxall PJD, Spraul M, Farrant R, Duncan. Lindon JC. 750 MHz 1H and 1H-13C NMR Spectroscopy of Human Blood Plasma. Anal Chem. 1995;67(5):793–811. 10.1021/ac00101a004 [DOI] [PubMed] [Google Scholar]
- 56.Louis E, Bervoets L, Reekmans G, De Jonge E, Mesotten L, Thomeer M, et al. Phenotyping human blood plasma by 1H-NMR: a robust protocol based on metabolite spiking and its evaluation in breast cancer. Metabolomics. 2015;11(1):225–36. 10.1007/s11306-014-0690-6 [DOI] [Google Scholar]
- 57.Xia J, Wishart DS. Web-based inference of biological patterns, functions and pathways from metabolomic data using MetaboAnalyst. Nature protocols. 2011;6(6):743–60. Epub 2011/06/04. 10.1038/nprot.2011.319 [DOI] [PubMed] [Google Scholar]
- 58.Warburg O. On the origin of cancer cells. (0036–8075 (Print)). D—clml: 5630:6832 oto—nlm. [Google Scholar]
- 59.Gatenby RA, Smallbone K, Maini Pk, Rose F, Averill J, Nagle Rb, Worrall L, et al. Cellular adaptations to hypoxia and acidosis during somatic evolution of breast cancer. (0007–0920 (Print)). D—NLM: EDAT- 2007/08/10 09:00 MHDA- 2007/10/10 09:00 CRDT- 2007/08/10 09:00 AID—6603922 AID— PST—ppublish. 10.1038/sj.bjc.6603922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Erickson JW, Cerione RA. Glutaminase: A Hot Spot For Regulation Of Cancer Cell Metabolism? Oncotarget. 2010;1(8):734–40. 10.18632/oncotarget.208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Barnes T, Bell K, DiSebastiano Km, Vance V, Hanning R, Russell C Dubin JA, et al. Plasma amino acid profiles of breast cancer patients early in the trajectory of the disease differ from healthy comparison groups. (1715–5320 (Electronic)). [DOI] [PubMed] [Google Scholar]
- 62.Dowling P, Henry M, Meleady P, Clarke C, Gately K, O’Byrne K, et al. Metabolomic and proteomic analysis of breast cancer patient samples suggests that glutamate and 12-HETE in combination with CA15-3 may be useful biomarkers reflecting tumour burden. Metabolomics. 2015;11(3):620–35. 10.1007/s11306-014-0723-1 [DOI] [Google Scholar]
- 63.Cheng C-s, Wang Z, Chen J. Targeting FASN in Breast Cancer and the Discovery of Promising Inhibitors from Natural Products Derived from Traditional Chinese Medicine. Evidence-Based Complementary and Alternative Medicine. 2014;2014:16 10.1155/2014/232946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kuhajda FP, Pizer ES, Li JN, Mani NS, Frehywot GL, Townsend CA. Synthesis and antitumor activity of an inhibitor of fatty acid synthase. Proc Natl Acad Sci U S A. 2000;97(7):3450–4. Epub 2000/03/15. 10.1073/pnas.050582897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Yoon S, Lee MY, Park SW, Moon JS, Koh YK, Ahn YH, et al. Up-regulation of acetyl-CoA carboxylase alpha and fatty acid synthase by human epidermal growth factor receptor 2 at the translational level in breast cancer cells. J Biol Chem. 2007;282(36):26122–31. Epub 2007/07/17. 10.1074/jbc.M702854200 . [DOI] [PubMed] [Google Scholar]
- 66.Lv W, Yang T. Identification of possible biomarkers for breast cancer from free fatty acid profiles determined by GC—MS and multivariate statistical analysis. Clinical Biochemistry. 2012;45(1–2):127–33. 10.1016/j.clinbiochem.2011.10.011. [DOI] [PubMed] [Google Scholar]
- 67.Rose DP, Connolly JM. Omega-3 fatty acids as cancer chemopreventive agents. Pharmacology & Therapeutics. 1999;83(3):217–44. 10.1016/S0163-7258(99)00026-1. [DOI] [PubMed] [Google Scholar]
- 68.Furstenberger G, Krieg P, Muller-Decker K, Habenicht AJ. What are cyclooxygenases and lipoxygenases doing in the driver’s seat of carcinogenesis? (0020–7136 (Print)). [DOI] [PubMed] [Google Scholar]
- 69.Zhang F, Du G. Dysregulated lipid metabolism in cancer. World Journal of Biological Chemistry. 2012;3(8):167–74. 10.4331/wjbc.v3.i8.167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zaugg K, Yao Y, Reilly PT, Kannan K, Kiarash R, Mason J, et al. Carnitine palmitoyltransferase 1C promotes cell survival and tumor growth under conditions of metabolic stress. Genes & Development. 2011;25(10):1041–51. 10.1101/gad.1987211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Linher-Melville K, Zantinge S, Sanli T, Gerstein H, Tsakiridis T, Singh G. Establishing a relationship between prolactin and altered fatty acid beta-oxidation via carnitine palmitoyl transferase 1 in breast cancer cells. BMC Cancer. 2011;11:56 Epub 2011/02/08. 10.1186/1471-2407-11-56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ackerstaff E, Glunde K, Bhujwalla ZM. Choline phospholipid metabolism: A target in cancer cells? Journal of Cellular Biochemistry. 2003;90(3):525–33. 10.1002/jcb.10659 [DOI] [PubMed] [Google Scholar]
- 73.Glunde K, Jie C, Bhujwalla ZM. Molecular causes of the aberrant choline phospholipid metabolism in breast cancer. Cancer Res. 2004;64(12):4270–6. Epub 2004/06/19. 10.1158/0008-5472.CAN-03-3829 . [DOI] [PubMed] [Google Scholar]
- 74.Podo F. Tumour phospholipid metabolism. NMR in Biomedicine. 1999;12(7):413–39. [DOI] [PubMed] [Google Scholar]
- 75.Negendank W. Studies of human tumors by MRS: A review. NMR in Biomedicine. 1992;5(5):303–24. 10.1002/nbm.1940050518 [DOI] [PubMed] [Google Scholar]
- 76.Leach MO, Verrill M, Glaholm J, Smith TA, Collins DJ, Payne GS, et al. Measurements of human breast cancer using magnetic resonance spectroscopy: a review of clinical measurements and a report of localized 31P measurements of response to treatment. NMR Biomed. 1998;11(7):314–40. Epub 1998/12/22. . [DOI] [PubMed] [Google Scholar]
- 77.Ting YL, Sherr D, Degani H. Variations in energy and phospholipid metabolism in normal and cancer human mammary epithelial cells. Anticancer Res. 1996;16(3b):1381–8. Epub 1996/05/01. . [PubMed] [Google Scholar]
- 78.He M, Guo S, Li Z. In situ characterizing membrane lipid phenotype of breast cancer cells using mass spectrometry profiling. Scientific Reports. 2015;5:11298 10.1038/srep11298 http://www.nature.com/articles/srep11298#supplementary-information. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Hilvo M, Denkert C, Lehtinen L, Muller B, Brockmoller S, Seppanen-Laakso T, et al. Novel theranostic opportunities offered by characterization of altered membrane lipid metabolism in breast cancer progression. Cancer Res. 2011;71(9):3236–45. 10.1158/0008-5472.CAN-10-3894 . [DOI] [PubMed] [Google Scholar]
- 80.Ide Y, Waki M, Hayasaka T, Nishio T, Morita Y, Tanaka H, et al. Human Breast Cancer Tissues Contain Abundant Phosphatidylcholine(36:1) with High Stearoyl-CoA Desaturase-1 Expression. PLoS ONE. 2013;8(4):e61204 10.1371/journal.pone.0061204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kim H, Min H, Kong G, Moon M. Quantitative analysis of phosphatidylcholines and phosphatidylethanolamines in urine of patients with breast cancer by nanoflow liquid chromatography/tandem mass spectrometry. Analytical and Bioanalytical Chemistry. 2009;393(6–7):1649–56. 10.1007/s00216-009-2621-3 [DOI] [PubMed] [Google Scholar]
- 82.Katz-Brull R, Degani H. Kinetics of choline transport and phosphorylation in human breast cancer cells; NMR application of the zero trans method. Anticancer Res. 1996;16(3b):1375–80. Epub 1996/05/01. . [PubMed] [Google Scholar]
- 83.Ramirez de Molina A, Gutierrez R, Ramos MA, Silva JM, Silva J, Bonilla F, et al. Increased choline kinase activity in human breast carcinomas: clinical evidence for a potential novel antitumor strategy. Oncogene. 2002;21(27):4317–22. Epub 2002/06/26. 10.1038/sj.onc.1205556 . [DOI] [PubMed] [Google Scholar]
- 84.Abalsamo L, Spadaro F, Bozzuto G, Paris L, Cecchetti S, Lugini L, et al. Inhibition of phosphatidylcholine-specific phospholipase C results in loss of mesenchymal traits in metastatic breast cancer cells. Breast Cancer Res. 2012;14(2):R50 Epub 2012/03/21. 10.1186/bcr3151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Noh DY, Ahn SJ, Lee RA, Park IA, Kim JH, Suh PG, et al. Overexpression of phospholipase D1 in human breast cancer tissues. Cancer Lett. 2000;161(2):207–14. Epub 2000/11/25. . [DOI] [PubMed] [Google Scholar]
- 86.Noh DY, Kang HS, Kim YC, Youn YK, Oh SK, Choe KJ, et al. Expression of phospholipase C-gamma 1 and its transcriptional regulators in breast cancer tissues. Anticancer Res. 1998;18(4a):2643–8. Epub 1998/08/15. . [PubMed] [Google Scholar]
- 87.Yamashita S, Yamashita J, Ogawa M. Overexpression of group II phospholipase A2 in human breast cancer tissues is closely associated with their malignant potency. Br J Cancer. 1994;69(6):1166–70. Epub 1994/06/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Xu Y. Sphingosylphosphorylcholine and lysophosphatidylcholine: G protein-coupled receptors and receptor-mediated signal transduction. Biochimica et Biophysica Acta (BBA)—Molecular and Cell Biology of Lipids. 2002;1582(1–3):81–8. 10.1016/S1388-1981(02)00140-3. [DOI] [PubMed] [Google Scholar]
- 89.Park S-J, Lee K-P, Im D-S. Action and Signaling of Lysophosphatidylethanolamine in MDA-MB-231 Breast Cancer Cells. Biomolecules & Therapeutics. 2014;22(2):129–35. 10.4062/biomolther.2013.110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Dória ML, Cotrim CZ, Simões C, Macedo B, Domingues P, Domingues MR, et al. Lipidomic analysis of phospholipids from human mammary epithelial and breast cancer cell lines. Journal of Cellular Physiology. 2013;228(2):457–68. 10.1002/jcp.24152 [DOI] [PubMed] [Google Scholar]
- 91.Cui M, Wang Q, Chen G. Serum metabolomics analysis reveals changes in signaling lipids in breast cancer patients. Biomedical Chromatography. 2016;30(1):42–7. 10.1002/bmc.3556 [DOI] [PubMed] [Google Scholar]
- 92.Qiu Y, Zhou B, Su M, Baxter S, Zheng X, Zhao X, et al. Mass spectrometry-based quantitative metabolomics revealed a distinct lipid profile in breast cancer patients. Int J Mol Sci. 2013;14(4):8047–61. Epub 2013/04/16. 10.3390/ijms14048047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Fang Y, Vilella-Bach M, Bachmann R, Flanigan A, Chen J. Phosphatidic acid-mediated mitogenic activation of mTOR signaling. Science. 2001;294(5548):1942–5. Epub 2001/12/01. 10.1126/science.1066015 . [DOI] [PubMed] [Google Scholar]
- 94.Fujiwara Y. Cyclic Phosphatidic Acid—A Unique Bioactive Phospholipid. Biochimica et biophysica acta. 2008;1781(9):519–24. 10.1016/j.bbalip.2008.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Potischman N, McCulloch CE, Byers T, Houghton L, Nemoto T, Graham S, et al. Associations between breast cancer, plasma triglycerides, and cholesterol. Nutr Cancer. 1991;15(3–4):205–15. Epub 1991/01/01. 10.1080/01635589109514128 . [DOI] [PubMed] [Google Scholar]
- 96.Kapil U, Bhadoria AS, Sareen N, Singh P, Dwivedi SN. Total Cholesterol and Triglyceride Levels in Patients with Breast Cancer. Journal of Breast Cancer. 2013;16(1):129–30. 10.4048/jbc.2013.16.1.129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Zielinski CC, Stuller I, Rausch P, Müller C. Increased serum concentrations of cholesterol and triglycerides in the progression of breast cancer. Journal of Cancer Research and Clinical Oncology. 1988;114(5):514–8. 10.1007/bf00391503 [DOI] [PubMed] [Google Scholar]
- 98.Nomura DK, Lombardi DP, Chang JW, Niessen S, Ward AM, Long JZ, et al. Monoacylglycerol lipase exerts dual control over endocannabinoid and fatty acid pathways to support prostate cancer. Chem Biol. 2011;18(7):846–56. Epub 2011/08/02. 10.1016/j.chembiol.2011.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Li YL, Su X, Stahl PD, Gross ML. Quantification of diacylglycerol molecular species in biological samples by electrospray ionization mass spectrometry after one-step derivatization. Anal Chem. 2007;79(4):1569–74. Epub 2007/02/15. 10.1021/ac0615910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Nishizuka Y. Protein kinase C and lipid signaling for sustained cellular responses. Faseb j. 1995;9(7):484–96. Epub 1995/04/01. . [PubMed] [Google Scholar]
- 101.Bertagnolo V, Benedusi M, Brugnoli F, Lanuti P, Marchisio M, Querzoli P, et al. Phospholipase C-beta 2 promotes mitosis and migration of human breast cancer-derived cells. Carcinogenesis. 2007;28(8):1638–45. Epub 2007/04/13. 10.1093/carcin/bgm078 . [DOI] [PubMed] [Google Scholar]
- 102.Abu-Bedair FA, El-Gamal BA, Ibrahim NA, El-Aaser AA. Serum Lipids and Tissue DNA Content in Egyptian Female Breast Cancer Patients. Japanese Journal of Clinical Oncology. 2003;33(6):278–82. 10.1093/jjco/hyg059 [DOI] [PubMed] [Google Scholar]
- 103.Bhat SA, Mir MR, Majid S, Reshi AA, Husain I, Hassan T, et al. Serum Lipid Profile of Breast Cancer Patients in Kashmir. J Invest Biochem. 2013;2(1):26–31. [Google Scholar]
- 104.Gong Y, Dou LJ, Liang J. Link between obesity and cancer: role of triglyceride/free fatty acid cycling. European review for medical and pharmacological sciences. 2014;18(19):2808–20. [PubMed] [Google Scholar]
- 105.Kokoglu E, Karaarslan I, Karaarslan HM, Baloglu H. Alterations of serum lipids and lipoproteins in breast cancer. Cancer Lett. 1994;82(2):175–8. Epub 1994/07/29. . [DOI] [PubMed] [Google Scholar]
- 106.Ray G, Husain SA. Role of lipids, lipoproteins and vitamins in women with breast cancer. Clin Biochem. 2001;34(1):71–6. Epub 2001/03/10. . [DOI] [PubMed] [Google Scholar]
- 107.Listenberger LL, Han X, Lewis SE, Cases S, Farese RV Jr, Ory DS, et al. Triglyceride accumulation protects against fatty acid-induced lipotoxicity. Proc Natl Acad Sci U S A. 2003;100(6):3077–82. Epub 2003/03/12. 10.1073/pnas.0630588100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Schaffer JE. Lipotoxicity: when tissues overeat. Curr Opin Lipidol. 2003;14(3):281–7. Epub 2003/07/04. 10.1097/01.mol.0000073508.41685.7f . [DOI] [PubMed] [Google Scholar]
- 109.Torres D, Rashid MU, Gil F, Umana A, Ramelli G, Robledo JF, et al. High proportion of BRCA1/2 founder mutations in Hispanic breast/ovarian cancer families from Colombia. Breast Cancer Res Treat. 2007;103(2):225–32. Epub 2006/11/03. 10.1007/s10549-006-9370-1 . [DOI] [PubMed] [Google Scholar]
- 110.Hernandez JE, Llacuachaqui M, Palacio GV, Figueroa JD, Madrid J, Lema M, et al. Prevalence of BRCA1 and BRCA2 mutations in unselected breast cancer patients from medellin, Colombia. Hered Cancer Clin Pract. 2014;12(1):11 Epub 2014/04/20. 10.1186/1897-4287-12-11 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Sanabria MC, Muñoz G, Vargas CI. Análisis de las mutaciones más frecuentes del gen BRCA1 en mujeres con cáncer de mama en Bucaramanga, Colombia. Biomédica. 2009;29:61–72. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Comparison of GC-MS chromatograms (truncated at 30 minutes) for breast cancer (green) and control (blue). Identified metabolites: 1. N-Ethylglycine I. 2. Pyruvic acid. 3. Lactic acid. 4. Glycolic acid. 5. Valine I. 6. Alanine I. 7. 2-Ketoisocaproic acid I. 8. Acetoacetate I. 9. Glycine I. 10. 2-Hydroxybutyric acid I. 11. Sarcosine. 12. Acetoacetate II. 13. Oxalic acid. 14. p-Cresol. 15. Leucine I. 16. 3-Hydroxybutyric acid. 17. 2-etoisocaproic acid I. 18. N-methylalanine. 19. Proline I. 20. Isoleucine I. 21. 2-Ketoisocaproic acid II. 22. Malonic acid I. 23. Valine II. 24. Glyceraldehyde II. 25. Benzoic acid. 26. Urea. 27. Serine I. 28. Caprylic acid. 29. Leucine II. 30. Glycerol. 31. Phosphoric acid. 32. Threonine I. 33. Isoleucine II. 34. Proline II. 35. Glycine. 36. Glyceric acid. 37. Fumaric acid. 38. Serine II. 39. Pipecolic acid II. 40. Threonine II. 41. Aspartic acid I. 42. 3-Aminoisobutyric acid II. 43. Iminodiacetic acid I. 44. Threose II. 45. Aminomalonic acid. 46. Threitol. 47. Methionine II. 48. Pyroglutamic acid. 49. trans-4-Hydroxy-L-proline II. 50. Iminodiacetic acid II. 51. Phenylalanine I. 52. Creatinine. 53. Glutamic acid II. 54. Phenylalanine II. 55. Lauric acid. 56. Asparagine II. 57. Pyrophosphate. 58. Arabitol. 59. Xylitol. 60. Glutamine III. 61. Shikimic acid. 62. Hypoxanthine I. 63. OrnithineII. 64. Citric acid. 65. Myristic acid. 66. Galactopyranoside. 67. Pyranose (Glucose/Altrose/Galactose/Talose). 68. Furanose (Tagatose I). 69. p-Hydroxyphenyllactic acid. 70. Gluconic acid lactone I. 71. Tagatose II. 72. Fructose I. 73. Fructose II + Glucose. 74. Glucose. 75. Glucose. 76. Sorbitol. 77. Tyrosine II. 78. 3-Indoleacetic acid. 79. Galactopyranoside. 80. Palmitoleic acid. 81. Palmitic acid. 82. Uric acid I. 83. Methyl stearate (IS). 84. Tryptophan II. 85. Linoleic acid. 86. Oleic acid. 87. Arachidonic acid. 88. 1-Monomyristin. 89. Lactose II. 90. 5-Hydroxy-L-tryptophan I. 91. 2-Palmitoylglycerol. 92 1-Monopalmitin. 93. 2-Monostearin. 94. Glycerol monostearate. 95. Cholesterol.
(DOCX)
Comparison of LC-MS base peak chromatograms for breast cancer (green) and control (blue). Panel A. Metabolic fingerprinting by LC-MS. B. Lipid fingerprinting by LC-MS. The marked windows are according to the compound class and their elution time.
(DOCX)
Comparison of 1H-NMR spectra for breast cancer (green) and control (blue). Chemical shifts of compounds with statistical significance are expanded.
(DOCX)
PCA score plots for data set filtered by presence and reproducibility (green dots: breast cancer group; blue dots. control group; orange diamonds: quality control). Panel: A. MF by GC-MS. B. MF by NMR. C. MF by LC-MS(+)D. MF by LC-MS(-)E. LF by LC-MS(+). F. LF by LC-MS(-).
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Data Availability Statement
All relevant data are available from Metabolomics Workbench at the following URL: http://dx.doi.org/10.21228/M8QM3R.