Supplemental Digital Content is available in the text.
Keywords: atherosclerosis, coronary disease, disease progression, risk assessment, tomography, vascular calcification
Abstract
Background:
Computed tomography (CT) allows estimation of coronary artery calcium (CAC) progression. We evaluated several progression algorithms in our unselected, population-based cohort for risk prediction of coronary and cardiovascular events.
Methods:
In 3281 participants (45–74 years of age), free from cardiovascular disease until the second visit, risk factors, and CTs at baseline (b) and after a mean of 5.1 years (5y) were measured. Hard coronary and cardiovascular events, and total cardiovascular events including revascularization, as well, were recorded during a follow-up time of 7.8±2.2 years after the second CT. The added predictive value of 10 CAC progression algorithms on top of risk factors including baseline CAC was evaluated by using survival analysis, C-statistics, net reclassification improvement, and integrated discrimination index. A subgroup analysis of risk in CAC categories was performed.
Results:
We observed 85 (2.6%) hard coronary, 161 (4.9%) hard cardiovascular, and 241 (7.3%) total cardiovascular events. Absolute CAC progression was higher with versus without subsequent coronary events (median, 115 [Q1–Q3, 23–360] versus 8 [0–83], P<0.0001; similar for hard/total cardiovascular events). Some progression algorithms added to the predictive value of baseline CT and risk assessment in terms of C-statistic or integrated discrimination index, especially for total cardiovascular events. However, CAC progression did not improve models including CAC5y and 5-year risk factors. An excellent prognosis was found for 921 participants with double-zero CACb=CAC5y=0 (10-year coronary and hard/total cardiovascular risk: 1.4%, 2.0%, and 2.8%), which was for participants with incident CAC 1.8%, 3.8%, and 6.6%, respectively. When CACb progressed from 1 to 399 to CAC5y≥400, coronary and total cardiovascular risk were nearly 2-fold in comparison with subjects who remained below CAC5y=400. Participants with CACb≥400 had high rates of hard coronary and hard/total cardiovascular events (10-year risk: 12.0%, 13.5%, and 30.9%, respectively).
Conclusions:
CAC progression is associated with coronary and cardiovascular event rates, but adds only weakly to risk prediction. What counts is the most recent CAC value and risk factor assessment. Therefore, a repeat scan >5 years after the first scan may be of additional value, except when a double-zero CT scan is present or when the subjects are already at high risk.
Editorial, see p 680
Clinical Perspective.
What Is New?
For the first time, the predictive value of coronary artery calcification (CAC) progression for coronary and cardiovascular events was assessed in a population-based study with a prespecified 5-year interval between computed tomography scans.
CAC progression added some predictive value to baseline computed tomography and risk assessment, even when 5-year risk factors were taken into account.
However, CAC progression yielded no additional benefit, when, instead of the baseline CAC, the 5-year CAC results were taken into account.
Double-zero CAC scans in a 5-year interval mean an excellent prognosis, which was better than the prognosis for incident CAC after 5 years.
What Are the Clinical Implications?
Sophisticated CAC progression algorithms are unnecessary; clinicians can rely on the most recent risk and CAC assessment.
Patients with zero CAC may benefit from a follow-up scan to reinsure the excellent prognosis for coronary or cardiovascular events.
Patients with double-zero CAC during follow-up do not need another computed tomography scan in the near future because of the excellent prognosis.
For CAC>0 and <400, repeat computed tomography scans after 5 years will provide individual risk readjustment attributable to the increased risk when CAC≥400 is reached.
In the case of CAC≥400, a high coronary and cardiovascular risk is present; additional CAC scoring is not required.
Computed tomography (CT) provides unique features in atherosclerotic coronary artery disease imaging. Coronary artery calcification (CAC) can be detected, localized, and quantified, enabling studies on CAC progression or even regression.1–5 Raggi et al6 were the first to show that CAC progression was very common and significantly greater in patients with than without a clinical coronary event. This was confirmed in MESA (Multi-Ethnic Study on Atherosclerosis).7 In addition, CAC progression yielded incremental values in predicting all-cause mortality.8 In contrast, the CCLS trial (Cooper Center Longitudinal Study) reported only a modest association with cardiovascular outcome, although no additional prognostic information was provided in comparison with the latest single CAC value.9 Various algorithms of CAC progression have been reported,6,8,10,11 which resulted in divergent subject classification in ≤30% of individuals.12 Our own analyses favor a log scale for single CAC measurements, log(CAC+1), and differences between logarithms for determining CAC progression.11 We calculated quantile regression on the baseline log(CAC+1) value and confirmed the hypothesis that the individual’s CAC progresses exponentially with time, similar to CAC percentiles with age.3,11 Therefore, we used this and other published algorithms to estimate (1) the benefit of CAC progression over CAC at baseline or after a prespecified interval of 5 years by using survival analyses, C-statistics (Harrell C), net reclassification improvement (NRI), and integrated discrimination index (IDI); (2) the value of a final CAC score in comparison with the progression rate; and (3) the need for a repeat CT scan in subgroups of CAC categories. We evaluated the predictive power for risk assessment of coronary and cardiovascular events in our population-based cohort of the Heinz Nixdorf Recall study in a prospective and observational manner.
Methods
All data, methods used in the analysis, and materials are available for purposes of reproducing the results by contacting the corresponding author.
Study Participants
In 2000, the Heinz Nixdorf Recall (HNR) study drew simple random samples of residents of the cities of Essen, Mülheim, and Bochum, aged 45 to 74 years, from mandatory lists of residents as previously described.13 Subjects with prior coronary artery disease, defined as coronary artery bypass surgery and interventional revascularization procedures and history of prior myocardial infarction, were excluded. At baseline, 4275 (95.3%) of 4487 participants (2027 men, 2248 women) received an electron beam CT examination and were followed for a mean of 5.1±0.3 years (4.2–7.5 years), when a second electron beam CT scan was performed. Subjects free of cardiovascular event at the second scan (n=3281, 53.6% women) were followed for a further mean of 7.8±2.2 years (prospective phase), and coronary and cardiovascular events were recorded. The overall observation period thus was 12.9±2.2 years (Figure 1). Current risk factors were measured and medication was listed. All participants provided written informed consent and the study was approved by the ethical committee at the University Clinic Essen, Germany. The study was certified and recertified according to DIN EN ISO 9001:2000/2008.
Figure 1.
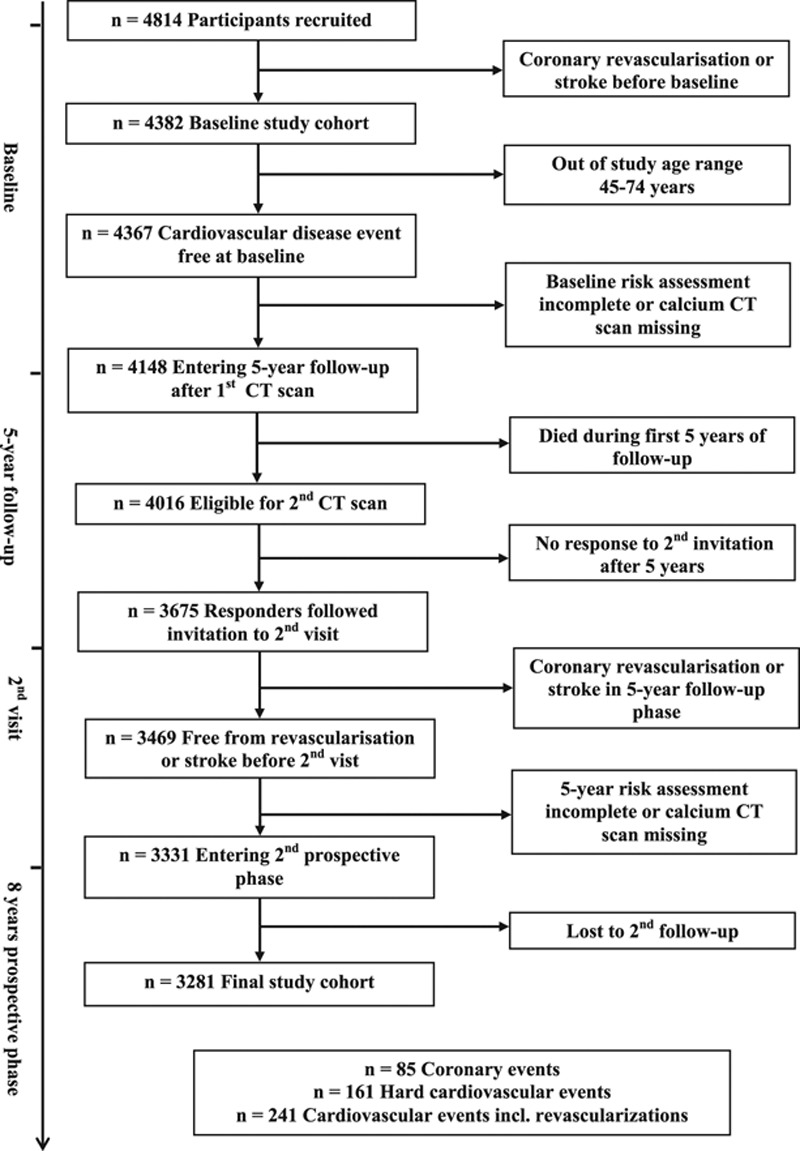
Flowchart of Heinz Nixdorf Recall study population. CT indicates computed tomography.
Electron Beam CT
At baseline, 2 radiological institutions performed the scans with C-100 and C-150 scanners (GE, Imatron).14 For the 5-year follow-up, only a C-150 scanner in the radiology department of the Alfried-Krupp-Hospital, Essen, Germany, was used.3 The electron beam CT scanners were operated in the single-slice mode with an image acquisition time of 100 ms; a slice thickness of 3 mm was used with a prospective ECG triggering at 80% of the R–R interval.14 Contiguous slices from the base of the heart down to the apex were obtained. The Agatston algorithm was used for CAC quantification, including at least 4 contiguous pixels with a CT density ≥130 Hounsfield units as a single area of CAC.15 The total CAC score was computed, comprising all calcified lesions in the coronary system. Analyses were performed using a Virtuoso workstation (Siemens Medical Solutions). We implemented a reassessment of CAC scoring as quality control when extreme progression or regression from baseline (CACb) to 5-year (CAC5Y) examination was found (CACb≤10 to CAC5Y>50, CACb>20 to CAC5Y≤10, or, otherwise, >30% or <–7% annual change, accounting for the reproducibility by given correction factors.16 In these cases (n=244), a reader with several years of experience in evaluation of cardiac CT (A.A.M.), who was blinded to the results of the initial reading, and the risk factor profile of the participants, as well, performed a second reading of the CAC score. To that end, the images of both CT examinations were reevaluated off-line using the same workstation (Aquarius, TerraRecon).17 CAC scores were not made available to the participants or their physicians at baseline, but were reported after the second CT scan.3 The rate of revascularizations at first cardiovascular event was 1.7% in the 5-year time span between first and second scan and 2.4% in the 5-year span after the second scan, which is partly because of the ageing of the cohort. Thus, reporting the results did not lead to a dramatic increase in revascularization procedures in our cohort.
Risk Factor Analyses
Cardiovascular risk factors were recorded at baseline and after 5 years. The methodology has recently been published.17 Smoking behavior was assessed in detail.18 Body mass index (kg/m2) was calculated from measured height and weight. Total cholesterol, high-density lipoprotein cholesterol, and triglycerides, and low-density lipoprotein cholesterol, as well, were measured with standard enzymatic methods.17 The use of lipid-lowering drugs, and antihypertensive and antidiabetic medication, as well, was documented. With the use of an oscillometric method (Omron), blood pressure was measured and the mean value of the second and third of 3 measurements taken at least 2 minutes apart were used.19 Hypertension was defined as systolic or diastolic blood pressure ≥140 mm Hg or ≥90 mm Hg, respectively, or use of antihypertensive medication.20 Blood glucose was measured after overnight fasting with a mean of 9.7±4.9 hours (median 12 hours).21 Participants were classified as diabetic when fasting glucose exceeded 126 mg/dL or nonfasting glucose exceeded 200 mg/dL, or the use of insulin or oral hypoglycemic agents was reported.21 The Framingham risk equation was used to predict the 10-year probability of CHD (10-year CHD risk) at baseline and follow-up.22 Serum creatinine was measured (Advia Clinical Chemistry Analyzer, Siemens HealthCare Diagnostics) and glomerular filtration rate (milliliters per minute per 1.73 m2 of body surface area) was estimated using the modification of diet in renal disease equation. High sensitive C-reactive protein was determined by BN-II, Siemens HealthCare Diagnostics.20 Homocysteine was measured using a fluorescence polarization immunoassay (IMx, Abbott Laboratories). All analyses were done within 12 hours after sampling at 1 central laboratory (D.F.).17
Follow-Up Data Collection
Because an observational design was selected, no intervention was proposed; medical treatment of participants was left to the discretion of the treating physicians. An annual postal questionnaire assessed the morbidity status during follow-up, ie, hospital admissions, outpatient diagnoses of cardiovascular disease. After 5 and 10 years, a second medical examination in the study center was arranged.11 Participants were followed for a total time of 12.9±2.2 years, 7.8±2.2 years after the second CT (median [Q1–Q3]: 8.5 [6.7–9.3] years). As reported, we excluded subjects with coronary or cardiovascular events before the first and second CT. Thus, 3281 participants (53.6% women) form the basis for the present analysis.
Study End Points and Verification of Study End Points
Primary end points for this study were based on unequivocally documented incidental coronary events that met predefined study criteria.14 Hard coronary events were nonfatal acute myocardial infarction and coronary death defined as clinical symptoms, signs on ECG, increased enzymes (levels of creatinine kinase), and troponin T or I, as well, and necropsy changes.14,17 Hard cardiovascular events were hard coronary events or stroke, defined as focal neurological deficits over a period of >24 hours of presumed cerebrovascular origin, or an independently International Classification of Diseases, 10thRevision–coded death cause in chapter 9: Diseases of the Circulatory System.20 Revascularizations during follow-up after the second CT scan were listed in addition and, together with hard cardiovascular events, defined total cardiovascular events. For all primary study end points, hospital and nursing home records including ECGs, laboratory values, and pathology reports were collected. Death certificates were collected and interviews with general practitioners, relatives, and eyewitnesses were undertaken, if possible, in those who died. Medical records were obtained for all reported end points.17,20 An external end point committee blinded for risk factor status and CAC scores reviewed all documents and classified the end points at separate regular meetings twice a year. For the end point stroke, an additional expert panel consisting of 4 neurologists was created.
Statistical Analysis
General Statistics
Continuous parameters are represented as mean±SD or median (25th percentile, Q1; 75th percentile, Q3). Accordingly, tests for group differences in continuous parameters are performed using the Student t test or Mann-Whitney U test. Nominal or ordinal parameters are given as n (percentage, %); group differences are evaluated by using the χ2 or Fisher exact test or Cochran-Armitage trend test. Annualized progression parameters (absolute [untransformed] CAC change [Absolute], square root CAC change [Root], log(CAC+1) change [Log]) were defined, eg, as follows:
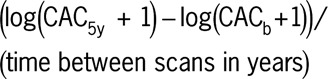 |
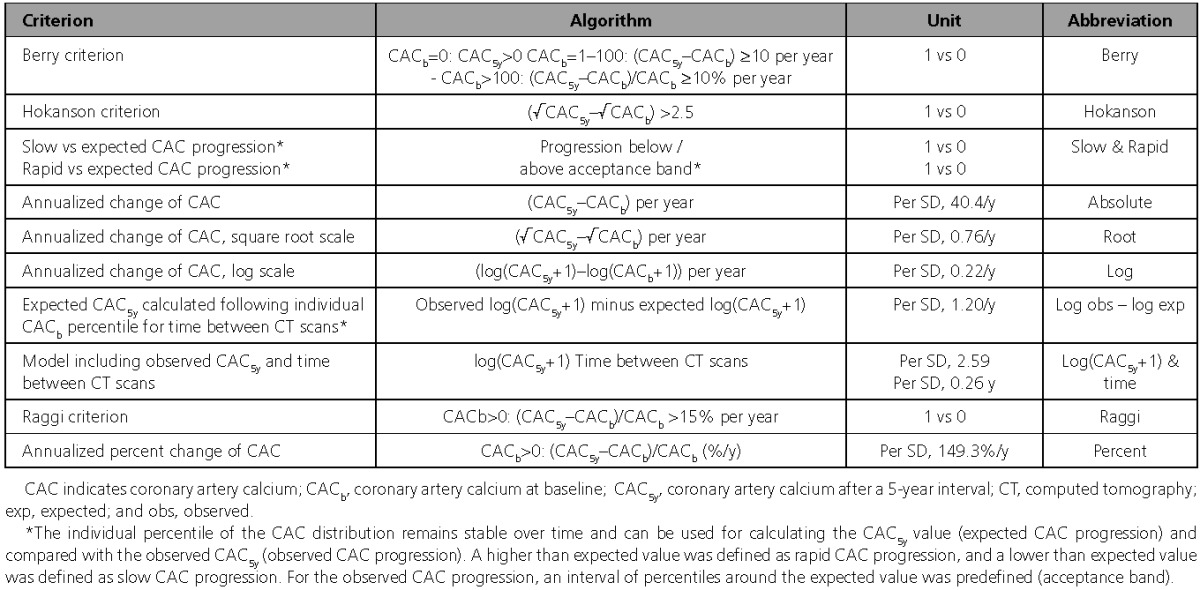
Another continuous measure contains 2 parameters, log(CAC5y+1) and time between scans (log(CAC5y+1) and time). We also use the percentage per year (Percent) as continuous measure, which is of course only defined in the group with CACb >0, which holds for the categorical measure defined by Raggi as well. An overview of progression measures is given in Table 1. Continuous parameters enter survival (time-to-event) analysis per SD as given in Table 1.
Table 1.
Criteria Used for Estimating Coronary Artery Calcification Progression Calculated from Baseline and 5-Year CT Scans
Expected CAC5y and Rated Progression
We calculated CAC percentiles as a function of age for each sex at baseline. The individual percentile of the CAC distribution, CAC remains stable over time and can be used for calculating the CAC value after 5 years (expected CAC progression) and compared with the observed CAC after 5 years.3 A higher than predicted value was regarded as rapid, and a lower than predicted value was regarded as slow CAC progression in comparison with those who progressed within the predicted range (acceptance range).23,24 Statistically, this involves quantile regression on the log-scale (log(CAC+1)), and a dedicated approximation scheme, and the definition of vicinity to the percentile (acceptance band), as well.11,23,24 The definition of the acceptable range D, within which an individual’s percentile P may vary, is as follows:
with δ=0.2, such that D nominally covers 20%. Note that the range is in general skew, especially for P/100>0.5, deviations from P to higher percentiles are penalized earlier than deviations to lower values. An illustration is given in Figure I in the online-only Data Supplement.
Another (continuous) measure of progression is the difference observed log(CAC5y+1) minus expected log(CAC+1) at the second visit, following the individual’s log(CACb+1) percentile for the time between scans (Log obs – log exp).
Time-to-Event Analyses
Kaplan-Meier estimates of event-free survival probabilities were calculated in strata defined by rated CAC progression categories and evaluated with a log-rank test of trend. We used multivariable Cox proportional hazards regression to calculate adjusted hazard ratios and corresponding 95% confidence intervals. Analysis of Schoenfeld residuals and a Kolmogorov-type supremum test confirmed validity of the proportional hazards assumption.
Added Predictive Value Analysis
Cox regression also forms the base of added predictive value analyses in terms of (change in) the Harrell C-statistics25 (Δ C), which is evaluated using SAS macros available at Harvard University26 based on 1000 bootstrap replicates of the original sample. Furthermore, we calculate NRI27 and IDI27 after estimating the 10-year probability of events from Cox regression (maximal observation time after second scan in our data: 10.9 years). For NRI we chose, following the risk definitions of the Framingham score, 0 to <6%; 6% to 20%, >20% as the risk limits for coronary events,22 and, for cardiovascular events, the end point categories <5%, 5% to 7.5%, >7.5% per the American College of Cardiology/American Heart Association 2013 risk/cholesterol guidelines.28 For calculation, we used the SAS macro “%add_predictive”.28a NRI, IDI, and their 95% confidence limits were estimated using a bootstrap sample with 1000 replicates drawn from the original data.
In addition to added predictive value analysis, we also compared C-statistics (standard receiver-operating-characteristic analysis) for models involving 5-year risk profile (including CAC) with models involving baseline risk factor profile (including CAC). Regarding the number of parameters involved and the smaller number of coronary events, this is feasible only for cardiovascular events.
Subgroup Analysis
Incidences of coronary and cardiovascular events are reported as 10-year risk, referring to the mean observation period after the second scan, 7.8 years, and extrapolating to 10 years. Incidence rates per 1000 person-years with 95% confidence limits are also reported, for the full study cohort, and in subgroups by CAC categories and sex, as well.
Results
Demographic Characteristics
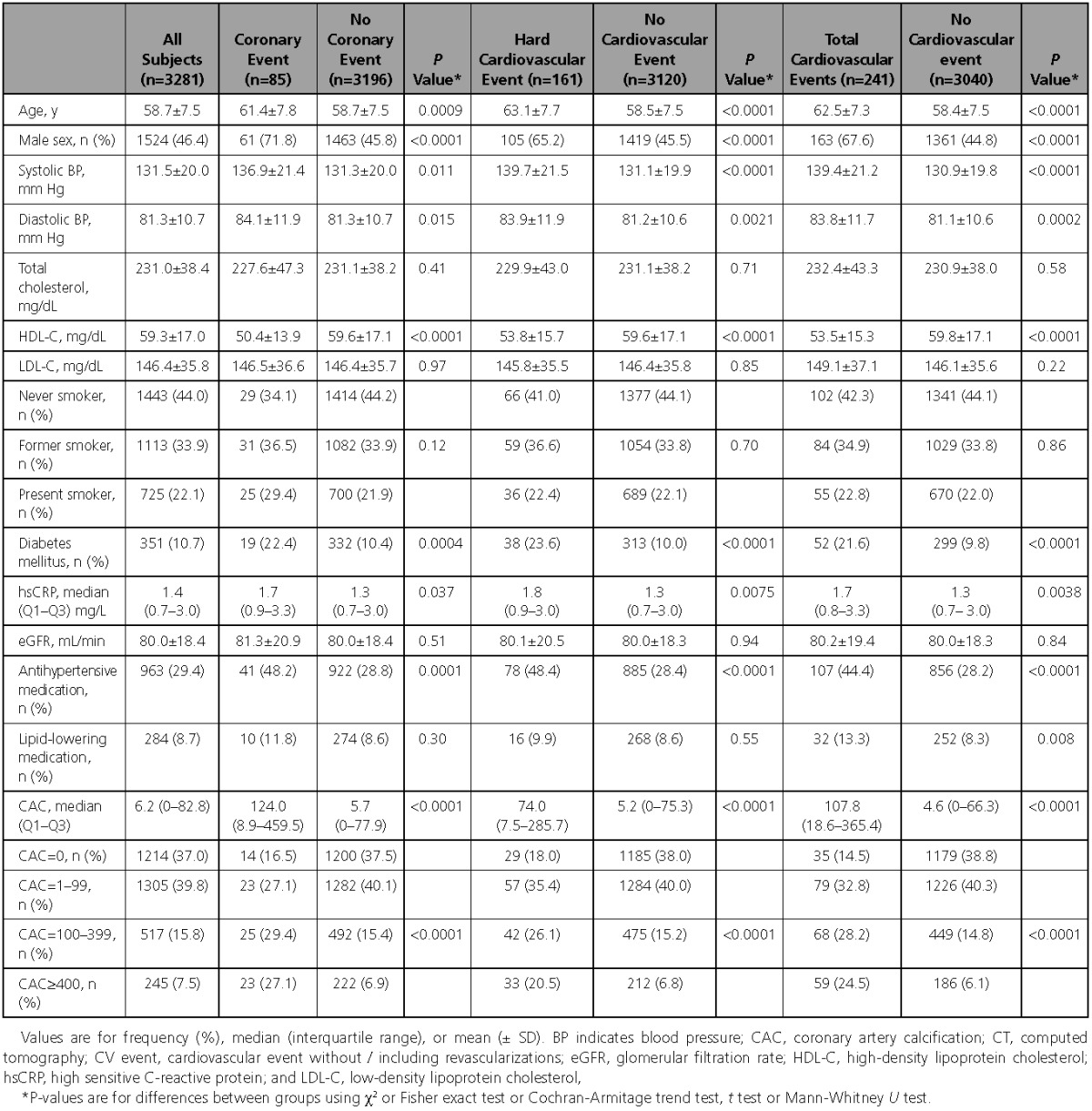
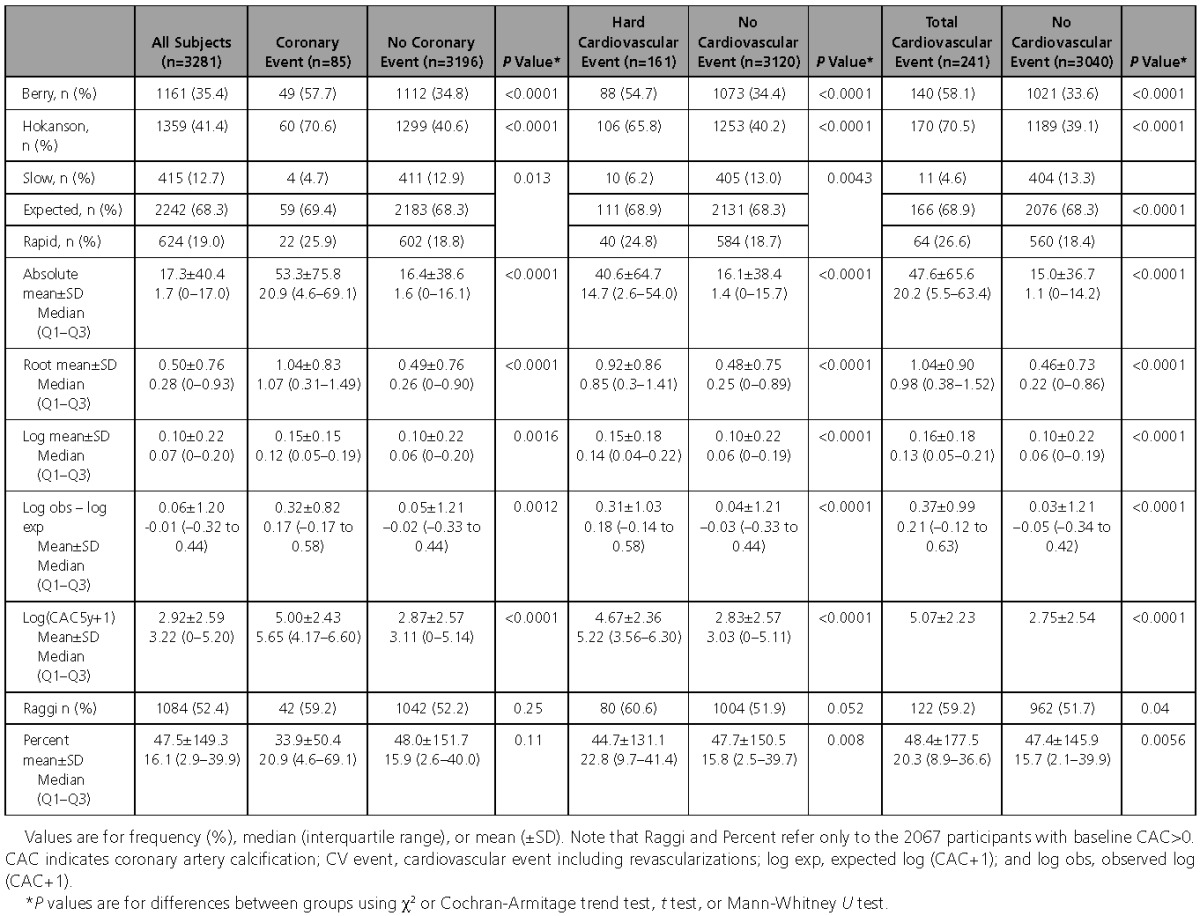
Our cohort of 3281 participants (Figure 1), who had 2 CT scans with a 5 (5.1±0.3) year time interval and no coronary or cardiovascular events including revascularization before the first and second scan, was followed for 7.8±2.2 years after the second scan. During follow-up, 85 subjects (2.6%) developed hard coronary events, 161 (4.9%) experienced hard cardiovascular events, and 241 (7.3%) had cardiovascular events including revascularization (total cardiovascular events). Substantial risk factor differences were found between those with and without events at baseline (Table 2), and after 5 years (Table I in the online-only Data Supplement), as well. But changes of the risk factor profiles in the 5-year interval did not discriminate between those with and without events (data not shown). However, CAC progression was higher in those with than without coronary events, Δ CAC median 115 (Q1–Q3, 23–360) versus 8 (0–83), with and without hard cardiovascular events, Δ CAC 75 (13–272) versus 7 (0–81), and total cardiovascular events, Δ CAC 106 (28–314) versus 6 (0–73), all P<0.0001. CAC=0 was found at baseline in 1214 (37%) and after 5 years in 1179 (36%) participants, CAC≥400 was found in 245 (7.5%) and 465 (14.2%) participants, respectively (Table 2 and Table I in the online-only Data Supplement).
Table 2.
Baseline Characteristics of the Heinz Nixdorf Recall Cohort (n=3281) With 2 CT Scans, the Second After a Time Interval Without Events of 5 Years, According to Coronary (n=85), Hard Cardiovascular (n=161), and Cardiovascular Events Including Revascularizations (n=241) During a Follow-Up Time of 7.8±2.2 Years After the Last CT Scan
Receiver-operating-characteristic analysis showed that 5-year risk factors and CAC5y were superior to baseline risk factors and CACb in predicting cardiovascular events (hard cardiovascular events: AUC5y=0.769 versus AUCb=0.753, Δ=0.016 (0.001–0.031), P=0.043; total cardiovascular events: AUC5y=0.785 versus AUCb=0.767, Δ=0.018 (0.007–0.030), P=0.0013).
Evaluating Algorithms for Calculating CAC Progression
Detailed analysis of CAC progression, defined by 10 different algorithms, demonstrated significant differences between participants with and without coronary, and cardiovascular events (hard or total), as well (Table 3). Only 2 algorithms, the Raggi criterion and the annualized percent change of CAC, showed no significant differences for coronary events, which became significant, however, when differences were classified regarding cardiovascular events.
Table 3.
CAC Progression Measures, Stratified by Coronary and Cardiovascular Event Status
Using log (CACb+1) and the baseline risk factor profile as reference model, the added predictive values of CAC progression for hard coronary events using different algorithms are illustrated in Figure 2A. The survival analysis detected hazard ratios per SD of up to 1.91 (95% confidence interval, 1.02–3.59) for log(CAC5y+1), P=0.043, and 1.29 (1.09–1.53), P=0.003 for time. An effect of slow versus expected and rapid versus expected progression can be detected in the Kaplan-Meier survival curves, when the nonadjusted data were used (Figure IIA in the online-only Data Supplement; for an illustration of the definition of slow, expected, and rapid progression see Figure I in the online-only Data Supplement). Positive effects were lost in the Harrell C-statistics and for NRI. Minor, but positive results were seen in the IDI analysis for the absolute differences, log, and log obs–log exp in the range of 0.006 and 0.002.
Figure 2.
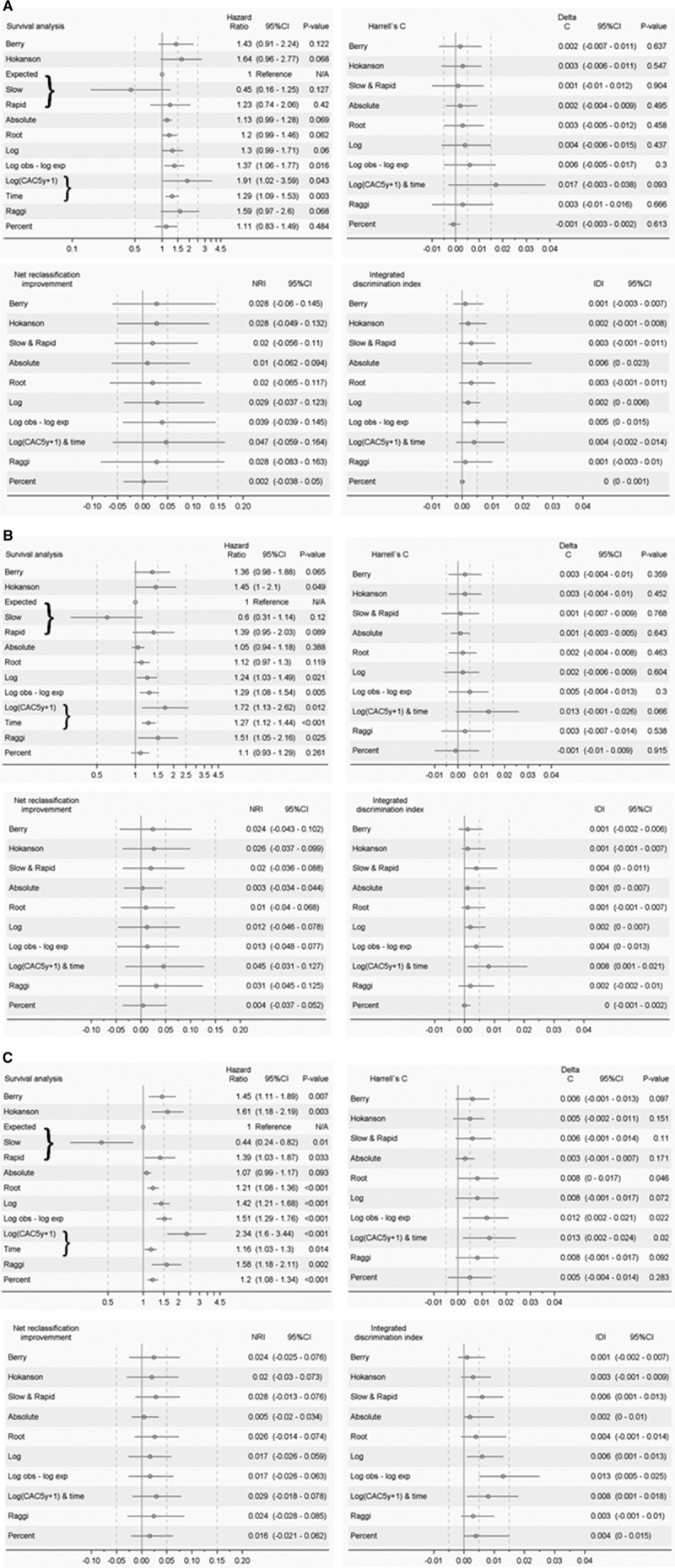
Added predictive value analyses for hard coronary, hard cardiovascular, and total cardiovascular events. A, Added predictive value analysis for hard coronary events (for different CAC progression algorithms, with respect to baseline risk assessment and baseline CAC). Upper left, hazard ratios; upper right, change in C-statistics; lower left, NRI; lower right, IDI. Base model: log(CAC+1) at baseline and, evaluated at baseline examination, age, sex, LDL, HDL, diabetes mellitus, present smoking, systolic blood pressure, intake of cholesterol-lowering or antihypertensive medications. Base model C-statistics: for the cohort with baseline CAC>0 (Raggi and Percent) C=0.728, all other C=0.750. For definition of progression algorithms, see Table 1. Hazard ratios for continuous measures are given per SD, see Table 1. B, Added predictive value analysis as in Figure 2A, but for hard cardiovascular events. Base model C-statistics: for the cohort with baseline CAC>0 (Raggi and Percent) C=0.705, all other C=0.747. For definition of progression algorithms, see Table 1. Hazard ratios for continuous measures are given per SD, see Table 1. C, Added predictive value analysis as in Figure 2A, but for total cardiovascular events. Base model C-statistics: for the cohort with baseline CAC>0 (Raggi and Percent) C=0.723, all other C=0.764. For definition of progression algorithms, see Table 1. Hazard ratios for continuous measures are given per SD, see Table 1. CAC indicates coronary artery calcium; CI, confidence interval; exp, expected; HDL, high-density lipoprotein; IDI, integrated discrimination index; LDL, low-density lipoprotein; NRI, net reclassification improvement; obs, observed.
For hard cardiovascular events, the survival analysis reached the highest hazard ratio of 1.72 (1.13–2.62), P=0.012 for log(CAC5y+1). Only 4 other parameters were significant as well (Figure 2B). For risk prediction of total cardiovascular events, the survival analysis reached a hazard ratio of 2.34 (1.6–3.44), P<0.001 for log(CAC5y+1) (Figure 2C). The Harrell C-statistic revealed for log(CAC5y+1) and time an improvement by 0.013 (0.002–0.024), P=0.02. In the NRI analysis, these positive effects could not be seen; the improvements over baseline risk assessment and baseline CAC were not significant at all. However, for IDI log obs–log exp showed an improvement of 0.013 (0.005–0.025), while for log(CAC5y+1) and time the IDI amounted to 0.008 (0.001–0.018). In addition, Slow and Rapid was positive with an IDI of 0.006 (0.001–0.013). The Kaplan-Meier curves for hard and total cardiovascular events showed a nice separation for the unadjusted values stratified by slow, expected, and rapid progression (Figure IIB and IIC in the online-only Data Supplement).
To test the influence of the 5-year risk factor distribution, the analyses were repeated, taking into account the 5-year risk assessment, and, as before, the baseline CAC values, as well (Figure IIIA in the online-only Data Supplement for coronary events). In the survival analysis, the coronary event rate prediction showed only minor differences in comparison with the analysis using the baseline risk assessment (Figure 2A). The same holds true for the Harrell C-statistics, the NRI and IDI results.
For hard cardiovascular events, and for cardiovascular events, as well, including revascularization, the use of the 5-year risk assessment resulted in a minor reduction of the predictive values in comparison with the use of the baseline risk assessment (Figure IIIB and IIIC in the online-only Data Supplement).
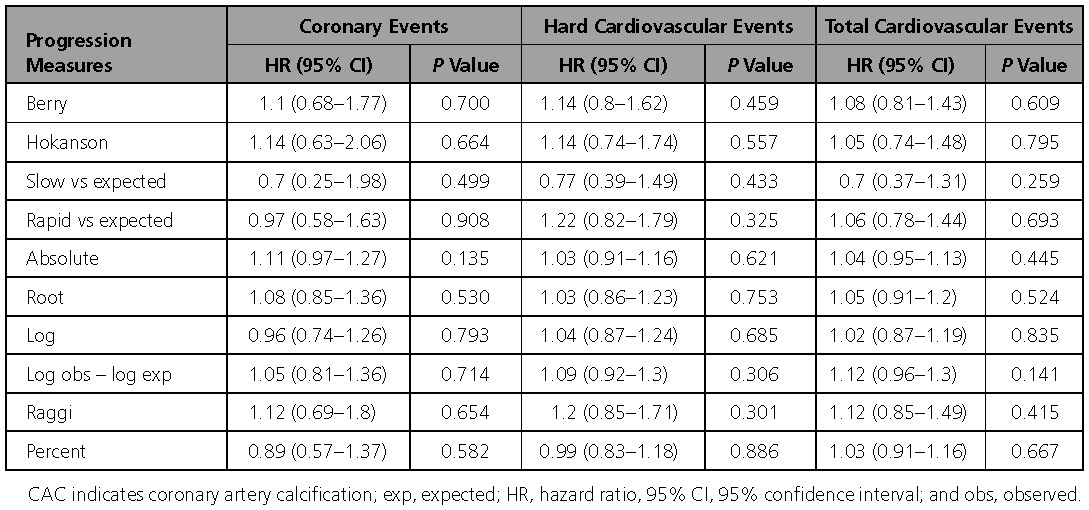
The lack of effect of CAC progression on the prediction of coronary and cardiovascular events is shown in Table 4: when log(CAC5y+1) is already included in the respective model and the 5-year risk factors and medication, as well. No significant improvement or even tendency could be found for any of the 10 algorithms studied.
Table 4.
Lack of Effect of Progression Measures on Development of Coronary and Cardiovascular Events When log(CAC5y+1) Is Already Included in the Respective Model, in Addition to 5-Year Risk Factors and Medication
Evaluating Subgroups of CAC
When we had shown the negative results for the total group, we tested whether or not different CAC categories could provide a different perspective (Table 5). We analyzed participants with CAC=0, CAC=1 to 399, and CAC ≥400 in men and women.
Table 5.
Event Risk Profile in Different Categories of Baseline and 5-Year CAC
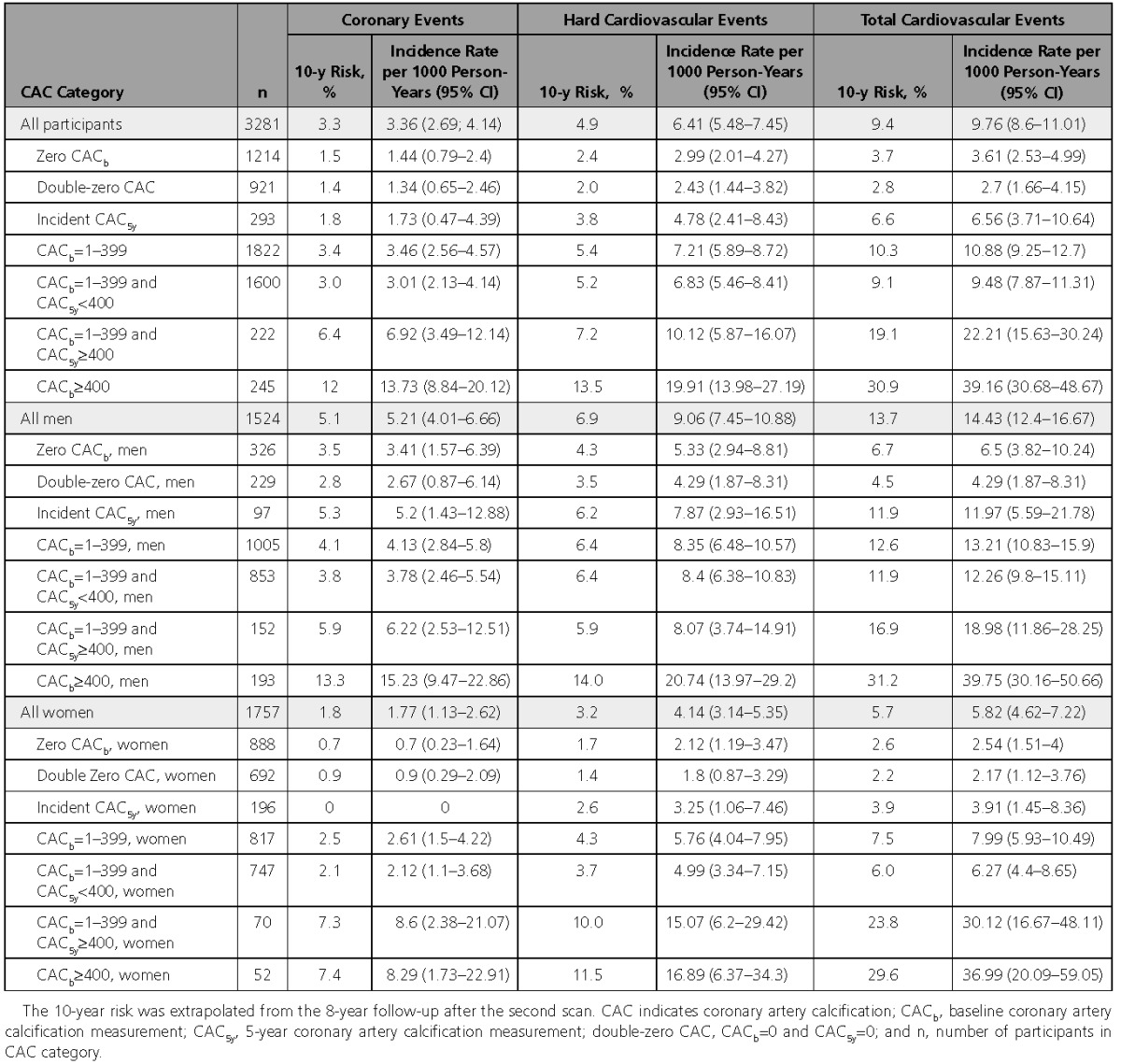
Participants with CAC=0 had low event rates, which were found for both sexes. Those with CACb=0 and CAC5y=0 showed an even lower incidence rate of coronary events per 1000 person-years (95% confidence interval), 1.34 (0.65–2.46), than incident CAC 1.73 (0.47–4.39) (Table 5). CAC5y ≥400 indicated highest risk with 13.73 (8.84–20.12) in comparison with CAC5y 1 to 399 with a rate of 3.46 (2.56–4.57). Similar results were found for cardiovascular events (Table 5).
Discussion
The high predictive value of CAC regarding coronary and cardiovascular events, and all-cause mortality, as well, has been established. Our prospective observational study with a prespecified time interval between 2 CT scans of 5 years and exclusion of events before the follow-up CT scan adds a strong body of evidence to current knowledge of the predictive value of CAC progression using 10 different algorithms for the calculation of CAC progression, testing for their predictive value not only on coronary, but also on cardiovascular event rates using survival analysis, C-statistics, NRI, and IDI calculations, as well. (1) Risk factor profiles were significantly different between those with and without hard coronary and cardiovascular events. (2) Changes of the risk factor profiles in the 5-year interval did not discriminate between those with and without events. (3) CAC progression was higher for those with than without hard coronary and hard cardiovascular events. (4) CAC progression added predictive value when added to CACb and risk factor profile data. (5) This also holds when CAC progression was added to CACb and 5-year risk factor profiles. (6) The repeat CT scan after 5 years overrided any algorithm used for the calculation CAC progression rate. (7) In a subgroup analysis, those with double-zero CT scan had the best prognosis, better than those with incident CAC. (8) Participants who exceeded CAC5y≥400 had a higher event rate than those who had a CAC5y<400
Rate of Progression and Risk for Cardiovascular Events
Angiographic progression of coronary artery disease has been shown to be associated with the development of myocardial infarction.29,30 With the use of CT, progression of CAC can be assessed and quantified. Previous studies have provided evidence that the assessment of CAC progression could yield some additional benefit related to CAC alone.6–8 A review of published reports, however, came to the conclusion that quantification of CAC progression cannot be recommended in clinical practice.10 A more recent analysis of the MESA study showed that CAC progression is a risk marker for future hard and total CHD events.7 In our study, however, CAC progression did not yield better prediction than CAC5y, ie, the most recent scan and risk factor analysis. As opposed to the previous work,7 we only included events occurring after the follow-up CAC scan, and this may, in part, explain the different results. In addition, imputation algorithms had not been used for replacing missing values.7 A more recent report in 5933 subjects with a follow-up time of 3.5 years showed only a modest association of CAC progression with cardiovascular outcome.9 When the authors used follow-up CAC instead of baseline CAC, CAC progression was no longer associated with total incidence of cardiovascular events.9
Different algorithms have been used to report CAC progression. It seems to be difficult to find the ideal algorithm because of the exponential curvature of the age- and sex-related CAC distribution. We included recent published algorithms.3,10–12,31,32 Our analysis demonstrates that neither categorized nor continuous algorithms are helpful for better risk prediction. Even our previously reported rated CAC progression11 showed only minor improvements when adjusted for the 5-year risk profile and CACb score; overshadowed using CAC5y.
Zero CAC and CAC Onset
Recent studies could demonstrate that zero CAC predicted a low cardiovascular event rate, which was close to 1% in the 10-year risk assessment.24,31–33 In 106 (25.1%) of 621 individuals with zero CAC, incident conversion to CAC>0 was observed within a time of 4.1±0.9 years.31 The rate of progression was nonlinear and highest in the fifth year, and risk factor predictors were age, diabetes mellitus, and smoking. In a previous analysis, 1184 (36.1%) of 3276 participants without events and CT at baseline and after 5 years had zero CAC. Of those, 107 (31.3%) men and 210 (22.9%) women showed incident CAC.24 The probability of CAC onset increased with age. In Framingham risk factor–adjusted multivariable analysis, odds ratios for CAC onset showed similar values for men and women with significant values for age in men and for age, systolic blood pressure, low-density lipoprotein cholesterol, and current smoking in women, as well. In an adolescent group, both low-density lipoprotein cholesterol and systolic blood pressure were identified as independent markers of incident CAC 20 years later.34 In 4609 individuals, the lowest event rate and CAC progression was found in those with zero CAC.8 In the MESA study, 5682 persons had a follow-up scan ≈2.5±0.8 years apart and 535 (15.8%) of 3494 persons with zero CAC showed incident CAC.7 The median follow-up from baseline was 7.6 years with an event rate of myocardial infarction and fatal coronary heart disease ≈2% in comparison with ≈1% for those without incident CAC. Hecht et al35 previously suggested using a 4-year time interval in subjects with zero CAC rather than a shorter interval. In addition, we could now demonstrate that those with double-zero CACb and CAC5y, as well, had the best prognosis. Only 10 (1.1%) had a hard coronary and 18 (2.0%) of 921 subjects had a hard cardiovascular event within an 8-year follow-up after the CAC5y CT scan. However, it has to be taken into account that coronary events may still occur in persons with zero CAC based on other pathophysiological mechanisms, but with a very low prevalence in comparison with atherosclerotic diseases.36
Practical Consequences
Physicians often will be confronted with the question of additional CT scans during follow-up. So far, few reports have addressed this topic. Based on our results, we propose the following decision tree based on the most recent CT scan. People with double-zero CAC do not need an additional scan, however, those with a first zero CAC result may profit from a second scan after 5 or more years due to the higher incidence of events in this cohort compared to the double zero cases. Both men and women with CAC>0 to 399 may be sent for a new CT scan to detect who has reached higher-risk thresholds of CAC≥400, which seems to be more likely for those with CAC>100 than those with incident CAC or CAC<100 at baseline. Men and women with CAC≥400 are at high risk and may not need another CT scan. These assumptions are supported by recent reports,37,38 demonstrating that individual high-risk levels mean a quite aggressive strategy for prevention. Implementing the American College of Cardiology/American Heart Association 2013 Cholesterol Guideline in all untreated, statin-eligible adults attained the best results in individuals with a 10-year atherosclerotic cardiovascular disease risk ≥7.5%, meaning high risk for cardiovascular events.28 With the use of American College of Cardiology/American Heart Association, and European Society of Cardiology guidelines, as well, CAC scores >400 indicated high risk independently on eligibility for statin therapy.38
Limitations
In general, plaque composition consists of ≈10% CAC, 10% lipids, 70% fibrotic tissue, and 10% other substances.39 Therefore, progression in CAC may not accurately reflect progression in total plaque volume. Higher rates of antihypertensive and lipid-lowering medication were found in subjects with enhanced CAC progression.40,41 Therefore, we adjusted for these parameters to exclude any bias. In addition, the 5-year changes of the risk factor profile were not associated with coronary or cardiovascular events rates, contrary to CAC progression.
It cannot be excluded that a more detailed analysis of the calcification process would yield different results, as assumed previously.10,42 We used the well-established Agatston score, taking into account the area and density of the CAC plaques. Because a slice thickness of 3 mm was selected, the Agatston scoring scale was used, knowing that the calcium volume score is less dependent on changes in slice thickness of different scanners.43 We also used absolute values of CAC, because they represent the plaque load using the electron beam CT scanner. In addition, age-sex-race/ethnicity–adjusted percentile CAC scores have been proposed,44 which entered our analysis in terms of rated CAC progression. To increase the accuracy, the calcium (mineral) mass score had been proposed,45 but has not yet been validated in large cohorts during follow-up. In addition, CAC progression seems to be largely restricted to known predilection sites of coronary arteriosclerosis.46 Recently, an analysis of the calcium coverage of all 3 major arteries was proposed to estimate the percentage of coronary arteries loaded with calcified plaques.47 The same authors presented the spatial weighted calcium score based on the MESA data, providing the advantage of being independent on threshold values like the Agatston score to detect CAC, and may provide a new useful research tool.48 Noncalcified lesions were not depicted, thus leaving large parts of coronary atherosclerosis in the dark. Modern CT technology is lowering the x-ray exposure to a great extent, so that, even for asymptomatic subjects, contrast CT may become an option in the future.
The interval between scans was prospectively limited to 5 years. However, this time interval was realized in the whole study group with only a small variation, which can be regarded as a major advantage. No imputation of missing data was necessary, because we included in the study only those who had 2 consecutive CT scans, and excluded those with events within the first and second CT scan to avoid any misinterpretation attributable to coronary bypass surgery or stent implantation. Of course, a longer follow-up time interval after the second CT scan would be desirable related to the number of events. Already, the time interval between the first CT and follow-up has reached 13 years, and the impact of CAC progression could be assessed by using CACb and CAC5y data. A larger number of events might have increased the precision of estimates, especially regarding our results for cardiovascular events.
Whereas the baseline CAC result were not open to the participants, the physicians and study center, the 5-year results had to be presented, because, meanwhile, multiple studies have had demonstrated the high predictive value of CAC.16,17,49,50 In addition, recent analyses have not shown that the number of revascularizations is increased by adding information about risk factors to CAC results.
Predictive value added by CAC progression was overwritten by the most recent CT scan result. Categorical NRI depends on the risk limits chosen, so our a priori choice of 6% and 20% for hard coronary events may not be the most sensitive. However, because no numeric association was observed in the model including follow-up CAC, it is unlikely that any sophisticated CAC progression algorithm or added predictive value computation would have any large impact on risk prediction once accounting for the most recent CT scan.
Our findings demonstrate that the progression of CAC, measured by using CT, is associated with coronary and cardiovascular events. As opposed to CAC progression, coronary and cardiovascular events were independent of changes in the risk factor profile within 5 years. CAC progression can be predicted based on newly developed algorithms, thereby also allowing estimation of the time until a critical CAC burden (eg, CAC=400) is reached.3,37,38 However, a higher CAC progression was no longer associated with cardiovascular events once accounting for the most recent CAC scan, and the absolute baseline and follow-up scores were the major predictors of cardiovascular events. Accordingly, serial CAC scans may only offer additional prognostic benefit in a subgroup of asymptomatic subjects. Zero CAC and, in particular, double-zero CAC confer a superb prognosis. Incident CAC has a good prognosis, but 2-fold higher event rates than double-zero CAC. In the presence of CAC>0, a second CAC scan after ≥5 years may be helpful to check if and when CAC scores tend to reach the high-risk threshold of CAC≥400. The most recent CAC score, assessed at 1 time during ageing, represents a measure of the cumulative effects of risk factor exposure during life based on genetic and epigenetic predisposition.
Acknowledgments
The authors acknowledge the support of the SarstedtAG&Co. (Nümbrecht, Germany) concerning laboratory equipment. We thank Prof. K. Lauterbach (Adjunct Professor, Harvard School of Public Health, Boston, MA) for his valuable contributions in an earlier phase of the study. The authors are indebted to all study participants and to the dedicated personnel of both the study center of the HNR study and the EBT-scanner facilities, and to the investigative group, in particular, to U. Slomiany, E.M. Beck, A. Öffner, S. Münkel, M. Bauer, S. Schrader, R. Peter, and H. Hirche.
Sources of Funding
The authors thank the Heinz Nixdorf Foundation [Chairman: Martin Nixdorf; Past Chairman: Dr jur. Gerhard Schmidt (deceased)], for their generous support of this study. This study is also supported by the German Ministry of Education and Science (BMBF), and the German Aero-space Center [Deutsches Zentrum für Luft- und Raumfahrt (DLR)], Bonn, Germany. The German Research Council Assessment supported the study (DFG project: ER 155/6-2) and funded the study of psychosocial factors and neighbourhood level information (DFG project SI 236/8-1 and SI 236/9-1). The sponsor of the study transferred the monitoring of the study to the German Ministry of Education and Science, Bonn using an international advisory board and quality control, and event committee, as well, but had no role concerning the study design, data collection, analysis, interpretation, or writing the report. The corresponding authors had full access to all data in the study and final responsibility for the submission of the article for publication. Funding to pay the Open Access publication charges for this article was provided by the Heinz Nixdorf Recall Investigative Group.
Disclosures
None.
Supplementary Material
Appendix
Advisory Board
T. Meinertz, Hamburg, Germany (Chair); C. Bode, Freiburg, Germany; P.J. de Feyter, Rotterdam, Netherlands; B. Güntert, Hall LT, Austria; F. Gutzwiller, Bern, Switzerland; H. Heinen, Bonn, Germany; O. Hess, Bern, Switzerland; B. Klein (†), Essen, Germany; H. Löwel, Neuherberg, Germany; M. Reiser, Munich, Germany; G. Schmidt (†), Essen, Germany; M. Schwaiger, Munich, Germany; C. Steinmüller, Bonn, Germany; T. Theorell, Stockholm, Sweden; S.N. Willich, Berlin, Germany.
Criteria and End Point Committee
C. Bode, Freiburg, Germany (Chair); K. Berger, Münster, Germany; H.R. Figulla, Jena, Germany; C. Hamm, Bad Nauheim, Germany; P. Hanrath, Aachen, Germany; W. Köpcke, Münster, Germany; B. Ringelstein, Münster, Germany; M. Dichgans, München, C. Weimar, Essen, Germany; A. Zeiher, Frankfurt, Germany.
Footnotes
Drs Lehmann and Erbel contributed equally.
Continuing medical education (CME) credit is available for this article. Go to http://cme.ahajournals.org to take the quiz.
The online-only Data Supplement is available with this article at http://circ.ahajournals.org/lookup/suppl/doi:10.1161/CIRCULATIONAHA.116.027034/-/DC1.
Contributor Information
T. Meinertz, Hamburg, Germany (Chair)
C. Bode, Freiburg, Germany
P.J. de Feyter, Rotterdam, Netherlands
B. Güntert, Hall LT, Austria
F. Gutzwiller, Bern, Switzerland
H. Heinen, Bonn, Germany
O. Hess, Bern, Switzerland
B. Klein, (†), Essen, Germany
H. Löwel, Neuherberg, Germany
M. Reiser, Munich, Germany
G. Schmidt, (†), Essen, Germany
M. Schwaiger, Munich, Germany
C. Steinmüller, Bonn, Germany
T. Theorell, Stockholm, Sweden
S.N. Willich, Berlin, Germany
C. Bode, Freiburg, Germany (Chair)
K. Berger, Münster, Germany
H.R. Figulla, Jena, Germany
C. Hamm, Bad Nauheim, Germany
P. Hanrath, Aachen, Germany
W. Köpcke, Münster, Germany
B. Ringelstein, Münster, Germany
M. Dichgans, München
A. Zeiher, Frankfurt, Germany
Collaborators: T. Meinertz, C. Bode, P.J. de Feyter, B. Güntert, F. Gutzwiller, H. Heinen, O. Hess, B. Klein, H. Löwel, M. Reiser, G. Schmidt, M. Schwaiger, C. Steinmüller, T. Theorell, S.N. Willich, C. Bode, K. Berger, H.R. Figulla, C. Hamm, P. Hanrath, W. Köpcke, B. Ringelstein, M. Dichgans, and A. Zeiher
References
- 1.Budoff MJ, Raggi P. Coronary artery disease progression assessed by electron-beam computed tomography. Am J Cardiol. 2001;88(2A):46E–50E. doi: 10.1016/s0002-9149(01)01767-2. [DOI] [PubMed] [Google Scholar]
- 2.Kronmal RA, McClelland RL, Detrano R, Shea S, Lima JA, Cushman M, Bild DE, Burke GL. Risk factors for the progression of coronary artery calcification in asymptomatic subjects: results from the Multi-Ethnic Study of Atherosclerosis (MESA). Circulation. 2007;115:2722–2730. doi: 10.1161/CIRCULATIONAHA.106.674143. doi: 10.1161/CIRCULATIONAHA.106.674143. [DOI] [PubMed] [Google Scholar]
- 3.Erbel R, Lehmann N, Churzidse S, Rauwolf M, Mahabadi AA, Möhlenkamp S, Moebus S, Bauer M, Kälsch H, Budde T, Montag M, Schmermund A, Stang A, Führer-Sakel D, Weimar C, Roggenbuck U, Dragano N, Jöckel KH Heinz Nixdorf Recall Study Investigators. Progression of coronary artery calcification seems to be inevitable, but predictable: results of the Heinz Nixdorf Recall (HNR) study. Eur Heart J. 2014;35:2960–2971. doi: 10.1093/eurheartj/ehu288. doi: 10.1093/eurheartj/ehu288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gassett AJ, Sheppard L, McClelland RL, Olives C, Kronmal R, Blaha MJ, Budoff M, Kaufman JD. Risk factors for long-term coronary artery calcium progression in the Multi-Ethnic Study of Atherosclerosis. J Am Heart Assoc. 2015;4:e001726. doi: 10.1161/JAHA.114.001726. doi: 10.1161/JAHA.114.001726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schindler TH, Cadenas J, Facta AD, Li Y, Olschewski M, Sayre J, Goldin J, Schelbert HR. Improvement in coronary endothelial function is independently associated with a slowed progression of coronary artery calcification in type 2 diabetes mellitus. Eur Heart J. 2009;30:3064–3073. doi: 10.1093/eurheartj/ehp482. doi: 10.1093/eurheartj/ehp482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Raggi P, Callister TQ, Shaw LJ. Progression of coronary artery calcium and risk of first myocardial infarction in patients receiving cholesterol-lowering therapy. Arterioscler Thromb Vasc Biol. 2004;24:1272–1277. doi: 10.1161/01.ATV.0000127024.40516.ef. doi: 10.1161/01.ATV.0000127024.40516.ef. [DOI] [PubMed] [Google Scholar]
- 7.Budoff MJ, Young R, Lopez VA, Kronmal RA, Nasir K, Blumenthal RS, Detrano RC, Bild DE, Guerci AD, Liu K, Shea S, Szklo M, Post W, Lima J, Bertoni A, Wong ND. Progression of coronary calcium and incident coronary heart disease events: MESA (Multi-Ethnic Study of Atherosclerosis). J Am Coll Cardiol. 2013;61:1231–1239. doi: 10.1016/j.jacc.2012.12.035. doi: 10.1016/j.jacc.2012.12.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Budoff MJ, Hokanson JE, Nasir K, Shaw LJ, Kinney GL, Chow D, Demoss D, Nuguri V, Nabavi V, Ratakonda R, Berman DS, Raggi P. Progression of coronary artery calcium predicts all-cause mortality. JACC Cardiovasc Imaging. 2010;3:1229–1236. doi: 10.1016/j.jcmg.2010.08.018. doi: 10.1016/j.jcmg.2010.08.018. [DOI] [PubMed] [Google Scholar]
- 9.Radford NB, DeFina LF, Barlow CE, Lakoski SG, Leonard D, Paixao AR, Khera A, Levine BD. Progression of CAC Score and Risk of Incident CVD. JACC Cardiovasc Imaging. 2016;9:1420–1429. doi: 10.1016/j.jcmg.2016.03.010. doi: 10.1016/j.jcmg.2016.03.010. [DOI] [PubMed] [Google Scholar]
- 10.McEvoy JW, Blaha MJ, Defilippis AP, Budoff MJ, Nasir K, Blumenthal RS, Jones SR. Coronary artery calcium progression: an important clinical measurement? A review of published reports. J Am Coll Cardiol. 2010;56:1613–1622. doi: 10.1016/j.jacc.2010.06.038. doi: 10.1016/j.jacc.2010.06.038. [DOI] [PubMed] [Google Scholar]
- 11.Lehmann N, Erbel R, Mahabadi AA, Kälsch H, Möhlenkamp S, Moebus S, Stang A, Roggenbuck U, Strucksberg KH, Führer-Sakel D, Dragano N, Budde T, Seibel R, Grönemeyer D, Jöckel KH Heinz Nixdorf Recall Study Investigators. Accelerated progression of coronary artery calcification in hypertension but also prehypertension. J Hypertens. 2016;4:2233–2242. doi: 10.1097/HJH.0000000000001080. doi: 10.1097/HJH.0000000000001080. [DOI] [PubMed] [Google Scholar]
- 12.Paixao ARM, Chakravorty R, Khera A, Leonard D, DeFina LF, Barlow CE, Radford NB, Levine BD. Disagreement between different definitions of coronary artery calcium progression. JACC Cardiovasc Imaging. 2015;10:743–745. doi: 10.1016/j.jcmg.2014.07.019. doi: 10.1016/j.jcmg.2014.07.019. [DOI] [PubMed] [Google Scholar]
- 13.Stang A, Moebus S, Dragano N, Beck EM, Möhlenkamp S, Schmermund A, Siegrist J, Erbel R, Jöckel KH Heinz Nixdorf Recall Study Investigation Group. Baseline recruitment and analyses of nonresponse of the Heinz Nixdorf Recall Study: identifiability of phone numbers as the major determinant of response. Eur J Epidemiol. 2005;20:489–496. doi: 10.1007/s10654-005-5529-z. [DOI] [PubMed] [Google Scholar]
- 14.Schmermund A, Möhlenkamp S, Berenbein S, Pump H, Moebus S, Roggenbuck U, Stang A, Seibel R, Grönemeyer D, Jöckel KH, Erbel R. Population-based assessment of subclinical coronary atherosclerosis using electron-beam computed tomography. Atherosclerosis. 2006;185:177–182. doi: 10.1016/j.atherosclerosis.2005.06.003. doi: 10.1016/j.atherosclerosis.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 15.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15:827–832. doi: 10.1016/0735-1097(90)90282-t. [DOI] [PubMed] [Google Scholar]
- 16.Detrano RC, Anderson M, Nelson J, Wong ND, Carr JJ, McNitt-Gray M, Bild DE. Coronary calcium measurements: effect of CT scanner type and calcium measure on rescan reproducibility–MESA study. Radiology. 2005;236:477–484. doi: 10.1148/radiol.2362040513. doi: 10.1148/radiol.2362040513. [DOI] [PubMed] [Google Scholar]
- 17.Erbel R, Möhlenkamp S, Moebus S, Schmermund A, Lehmann N, Stang A, Dragano N, Grönemeyer D, Seibel R, Kälsch H, Bröcker-Preuss M, Mann K, Siegrist J, Jöckel KH Heinz Nixdorf Recall Study Investigative Group. Coronary risk stratification, discrimination, and reclassification improvement based on quantification of subclinical coronary atherosclerosis: the Heinz Nixdorf Recall study. J Am Coll Cardiol. 2010;56:1397–1406. doi: 10.1016/j.jacc.2010.06.030. doi: 10.1016/j.jacc.2010.06.030. [DOI] [PubMed] [Google Scholar]
- 18.Jöckel KH, Lehmann N, Jaeger BR, Moebus S, Möhlenkamp S, Schmermund A, Dragano N, Stang A, Grönemeyer D, Seibel R, Mann K, Volbracht L, Siegrist J, Erbel R. Smoking cessation and subclinical atherosclerosis–results from the Heinz Nixdorf Recall Study. Atherosclerosis. 2009;203:221–227. doi: 10.1016/j.atherosclerosis.2008.05.041. doi: 10.1016/j.atherosclerosis.2008.05.041. [DOI] [PubMed] [Google Scholar]
- 19.Stang A, Moebus S, Möhlenkamp S, Dragano N, Schmermund A, Beck EM, Siegrist J, Erbel R, Jöckel KH Heinz Nixdorf Recall Study Investigative Group. Algorithms for converting random-zero to automated oscillometric blood pressure values, and vice versa. Am J Epidemiol. 2006;164:85–94. doi: 10.1093/aje/kwj160. doi: 10.1093/aje/kwj160. [DOI] [PubMed] [Google Scholar]
- 20.Erbel R, Lehmann N, Möhlenkamp S, Churzidse S, Bauer M, Kälsch H, Schmermund A, Moebus S, Stang A, Roggenbuck U, Bröcker-Preuss M, Dragano N, Weimar C, Siegrist J, Jöckel KH Heinz Nixdorf Recall Study Investigators. Subclinical coronary atherosclerosis predicts cardiovascular risk in different stages of hypertension: result of the Heinz Nixdorf Recall Study. Hypertension. 2012;59:44–53. doi: 10.1161/HYPERTENSIONAHA.111.180489. doi: 10.1161/HYPERTENSIONAHA.111.180489. [DOI] [PubMed] [Google Scholar]
- 21.Moebus S, Stang A, Möhlenkamp S, Dragano N, Schmermund A, Slomiany U, Hoffmann B, Bauer M, Broecker-Preuss M, Mann K, Siegrist J, Erbel R, Jöckel KH Heinz Nixdorf Recall Study Group. Association of impaired fasting glucose and coronary artery calcification as a marker of subclinical atherosclerosis in a population-based cohort–results of the Heinz Nixdorf Recall Study. Diabetologia. 2009;52:81–89. doi: 10.1007/s00125-008-1173-y. doi: 10.1007/s00125-008-1173-y. [DOI] [PubMed] [Google Scholar]
- 22.Wilson PW, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–1847. doi: 10.1161/01.cir.97.18.1837. [DOI] [PubMed] [Google Scholar]
- 23.Kowall B, Lehmann N, Mahabadi AA, Moebus S, Budde T, Seibel R, Grönemeyer D, Erbel R, Jöckel KH, Stang A. Progression of coronary artery calcification is stronger in poorly than in well controlled diabetes: Results from the Heinz Nixdorf Recall Study. J Diabetes Complications. 2017;31:234–240. doi: 10.1016/j.jdiacomp.2016.08.011. doi: 10.1016/j.jdiacomp.2016.08.011. [DOI] [PubMed] [Google Scholar]
- 24.Lehmann N, Möhlenkamp S, Mahabadi AA, Schmermund A, Roggenbuck U, Seibel R, Grönemeyer D, Budde T, Dragano N, Stang A, Mann K, Moebus S, Erbel R, Jöckel KH. Effect of smoking and other traditional risk factors on the onset of coronary artery calcification: results of the Heinz Nixdorf Recall study. Atherosclerosis. 2014;232:339–345. doi: 10.1016/j.atherosclerosis.2013.11.045. doi: 10.1016/j.atherosclerosis.2013.11.045. [DOI] [PubMed] [Google Scholar]
- 25.Harrell FE, Jr, Lee KL, Mark DB. Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med. 1996;15:361–387. doi: 10.1002/(SICI)1097-0258(19960229)15:4<361::AID-SIM168>3.0.CO;2-4. doi: 10.1002/(SICI)1097-0258(19960229)15:4<361::AID-SIM168>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 26.Risk Prediction Modeling: SAS Macros. http://ncook.bwh.harvard.edu/sas-macros.html. Accessed July 19, 2017.
- 27.Pencina MJ, D’Agostino RB, Sr, D’Agostino RB, Jr, Vasan RS. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med. 2008;27:157–172. doi: 10.1002/sim.2929. discussion 207. doi: 10.1002/sim.2929. [DOI] [PubMed] [Google Scholar]
- 28.Goff DC, Jr, Lloyd-Jones DM, Bennett G, Coady S, D’Agostino RB, Gibbons R, Greenland P, Lackland DT, Levy D, O’Donnell CJ, Robinson JG, Schwartz JS, Shero ST, Smith SC, Jr, Sorlie P, Stone NJ, Wilson PW, Jordan HS, Nevo L, Wnek J, Anderson JL, Halperin JL, Albert NM, Bozkurt B, Brindis RG, Curtis LH, DeMets D, Hochman JS, Kovacs RJ, Ohman EM, Pressler SJ, Sellke FW, Shen WK, Smith SC, Jr, Tomaselli GF American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 suppl 2):S49–S73. doi: 10.1161/01.cir.0000437741.48606.98. doi: 10.1161/01.cir.0000437741.48606.98. Erratum in: Circulation. 2014;129(25 suppl 2):S74–S75. [DOI] [PubMed] [Google Scholar]
- 28a.Kennedy KF, Pencina MJ. A SAS Macro to Compute Added Predictive Ability of New Markers Predicting a Dichotomous Outcome. 2010. http://www.analytics.ncsu.edu/sesug/2010/SDA07.Kennedy.pdf. Accessed January 23, 2018.
- 29.Ambrose JA, Tannenbaum MA, Alexopoulos D, Hjemdahl-Monsen CE, Leavy J, Weiss M, Borrico S, Gorlin R, Fuster V. Angiographic progression of coronary artery disease and the development of myocardial infarction. J Am Coll Cardiol. 1988;12:56–62. doi: 10.1016/0735-1097(88)90356-7. [DOI] [PubMed] [Google Scholar]
- 30.Little WC, Constantinescu M, Applegate RJ, Kutcher MA, Burrows MT, Kahl FR, Santamore WP. Can coronary angiography predict the site of a subsequent myocardial infarction in patients with mild-to-moderate coronary artery disease? Circulation. 1988;78(5 pt 1):1157–1166. doi: 10.1161/01.cir.78.5.1157. [DOI] [PubMed] [Google Scholar]
- 31.Budoff MJ, McClelland RL, Nasir K, Greenland P, Kronmal RA, Kondos GT, Shea S, Lima JA, Blumenthal RS. Cardiovascular events with absent or minimal coronary calcification: the Multi-Ethnic Study of Atherosclerosis (MESA). Am Heart J. 2009;158:554–561. doi: 10.1016/j.ahj.2009.08.007. doi: 10.1016/j.ahj.2009.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Min JK, Lin FY, Gidseg DS, Weinsaft JW, Berman DS, Shaw LJ, Rozanski A, Callister TQ. Determinants of coronary calcium conversion among patients with a normal coronary calcium scan: what is the “warranty period” for remaining normal? J Am Coll Cardiol. 2010;55:1110–1117. doi: 10.1016/j.jacc.2009.08.088. doi: 10.1016/j.jacc.2009.08.088. [DOI] [PubMed] [Google Scholar]
- 33.Blaha MJ, Cainzos-Achirica M, Greenland P, McEvoy JW, Blankstein R, Budoff MJ, Dardari Z, Sibley CT, Burke GL, Kronmal RA, Szklo M, Blumenthal RS, Nasir K. Role of coronary artery calcium score of zero and other negative risk markers for cardiovascular disease: the Multi-Ethnic Study of Atherosclerosis (MESA). Circulation. 2016;133:849–858. doi: 10.1161/CIRCULATIONAHA.115.018524. doi: 10.1161/CIRCULATIONAHA.115.018524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hartiala O, Magnussen CG, Kajander S, Knuuti J, Ukkonen H, Saraste A, Rinta-Kiikka I, Kainulainen S, Kähönen M, Hutri-Kähönen N, Laitinen T, Lehtimäki T, Viikari JS, Hartiala J, Juonala M, Raitakari OT. Adolescence risk factors are predictive of coronary artery calcification at middle age: the cardiovascular risk in young Finns study. J Am Coll Cardiol. 2012;60:1364–1370. doi: 10.1016/j.jacc.2012.05.045. doi: 10.1016/j.jacc.2012.05.045. [DOI] [PubMed] [Google Scholar]
- 35.Hecht HS. A zero coronary artery calcium score: priceless. J Am Coll Cardiol. 2010;55:1118–1120. doi: 10.1016/j.jacc.2009.09.064. doi: 10.1016/j.jacc.2009.09.064. [DOI] [PubMed] [Google Scholar]
- 36.Schmermund A, Erbel R. Unstable coronary plaque and its relation to coronary calcium. Circulation. 2001;104:1682–1687. doi: 10.1161/hc3901.093339. [DOI] [PubMed] [Google Scholar]
- 37.Egan BM, Li J, White K, Fleming DO, Connell K, Hernandez GT, Jones DW7, Ferdinand KC, Sinopoli A. 2013 ACC/AHA Cholesterol Guideline and Implications for Healthy People 2020 Cardiovascular Disease Prevention Goals. J Am Heart Assoc. 2016;5(8):e003558. doi: 10.1161/JAHA.116.003558. doi: 10.1161/JAHA.116.003558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mahabadi AA, Möhlenkamp S, Lehmann N, Kälsch H, Dykun I, Pundt N, Moebus S, Jöckel KH, Erbel R Heinz Nixdorf Recall Study Investigators. CAC score improves coronary and CV risk assessment above statin indication by ESC and AHA/ACC primary prevention guidelines. JACC Cardiovasc Imaging. 2017;10:143–153. doi: 10.1016/j.jcmg.2016.03.022. doi: 10.1016/j.jcmg.2016.03.022. [DOI] [PubMed] [Google Scholar]
- 39.Puri R, Nicholls SJ, Shao M, Kataoka Y, Uno K, Kapadia SR, Tuzcu EM, Nissen SE. Impact of statins on serial coronary calcification during atheroma progression and regression. J Am Coll Cardiol. 2015;65:1273–1282. doi: 10.1016/j.jacc.2015.01.036. doi: 10.1016/j.jacc.2015.01.036. [DOI] [PubMed] [Google Scholar]
- 40.Dykun I, Lehmann N, Kälsch H, Möhlenkamp S, Moebus S, Budde T, Seibel R, Grönemeyer D, Jöckel KH, Erbel R, Mahabadi AA. Statin medication enhances progression of coronary artery calcification: the Heinz Nixdorf Recall Study. J Am Coll Cardiol. 2016;68:2123–2125. doi: 10.1016/j.jacc.2016.08.040. doi: 10.1016/j.jacc.2016.08.040. [DOI] [PubMed] [Google Scholar]
- 41.Friedewald VE, Ambrose JA, Stone GW, Roberts WC, Willerson JT. The editor’s roundtable: the vulnerable plaque. Am J Cardiol. 2008;102:1644–1653. doi: 10.1016/j.amjcard.2008.09.001. doi: 10.1016/j.amjcard.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 42.Rodriguez-Granillo GA, Carrascosa P, Bruining N. Progression of coronary artery calcification at the crossroads: sign of progression or stabilization of coronary atherosclerosis? Cardiovasc Diagn Ther. 2016;6:250–258. doi: 10.21037/cdt.2016.03.03. doi: 10.21037/cdt.2016.03.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Budoff MJ, Achenbach S, Blumenthal RS, Carr JJ, Goldin JG, Greenland P, Guerci AD, Lima JA, Rader DJ, Rubin GD, Shaw LJ, Wiegers SE American Heart Association Committee on Cardiovascular Imaging and Intervention; American Heart Association Council on Cardiovascular Radiology and Intervention; American Heart Association Committee on Cardiac Imaging, Council on Clinical Cardiology. Assessment of coronary artery disease by cardiac computed tomography: a scientific statement from the American Heart Association Committee on Cardiovascular Imaging and Intervention, Council on Cardiovascular Radiology and Intervention, and Committee on Cardiac Imaging, Council on Clinical Cardiology. Circulation. 2006;114:1761–1791. doi: 10.1161/CIRCULATIONAHA.106.178458. doi: 10.1161/CIRCULATIONAHA.106.178458. [DOI] [PubMed] [Google Scholar]
- 44.Budoff MJ, Nasir K, McClelland RL, Detrano R, Wong N, Blumenthal RS, Kondos G, Kronmal RA. Coronary calcium predicts events better with absolute calcium scores than age-sex-race/ethnicity percentiles: MESA (Multi-Ethnic Study of Atherosclerosis). J Am Coll Cardiol. 2009;53:345–352. doi: 10.1016/j.jacc.2008.07.072. doi: 10.1016/j.jacc.2008.07.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ferencik M, Ferullo A, Achenbach S, Abbara S, Chan RC, Booth SL, Brady TJ, Hoffmann U. Coronary calcium quantification using various calibration phantoms and scoring thresholds. Invest Radiol. 2003;38:559–566. doi: 10.1097/01.RLI.0000073449.90302.75. doi: 10.1097/01.RLI.0000073449.90302.75. [DOI] [PubMed] [Google Scholar]
- 46.Schmermund A, Baumgart D, Möhlenkamp S, Kriener P, Pump H, Grönemeyer D, Seibel R, Erbel R. Natural history and topographic pattern of progression of coronary calcification in symptomatic patients: an electron-beam CT study. Arterioscler Thromb Vasc Biol. 2001;21:421–426. doi: 10.1161/01.atv.21.3.421. [DOI] [PubMed] [Google Scholar]
- 47.Brown ER, Kronmal RA, Bluemke DA, Guerci AD, Carr JJ, Goldin J, Detrano R. Coronary calcium coverage score: determination, correlates, and predictive accuracy in the Multi-Ethnic Study of Atherosclerosis. Radiology. 2008;247:669–675. doi: 10.1148/radiol.2473071469. doi: 10.1148/radiol.2473071469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Liang CJ, Budoff MJ, Kaufman JD, Kronmal RA, Brown ER. An alternative method for quantifying coronary artery calcification: the multi-ethnic study of atherosclerosis (MESA). BMC Med Imaging. 2012;12:14. doi: 10.1186/1471-2342-12-14. doi: 10.1186/1471-2342-12-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Becker A, Leber A, Becker C, Knez A. Predictive value of coronary calcifications for future cardiac events in asymptomatic individuals. Am Heart J. 2008;155:154–160. doi: 10.1016/j.ahj.2007.08.024. doi: 10.1016/j.ahj.2007.08.024. [DOI] [PubMed] [Google Scholar]
- 50.McClelland RL, Chung H, Detrano R, Post W, Kronmal RA. Distribution of coronary artery calcium by race, gender, and age: results from the Multi-Ethnic Study of Atherosclerosis (MESA). Circulation. 2006;113:30–37. doi: 10.1161/CIRCULATIONAHA.105.580696. doi: 10.1161/CIRCULATIONAHA.105.580696. [DOI] [PubMed] [Google Scholar]


