Supplemental digital content is available in the text.
Abstract
Background
Few studies have examined the association between individual-level socioeconomic status and access to kidney transplantation. This study aims to investigate the association between predialysis income and education, and access to (i) the kidney waitlist (first listing), and (ii) kidney transplantation conditional on waitlist placement. Adjustment will be made for a number of medical and nonmedical factors.
Methods
The Swedish Renal Register was linked to national registers for adult patients in Sweden who started dialysis during 1995 to 2013. We employed Cox proportional hazards models.
Results
Nineteen per cent of patients were placed on the waitlist. Once on the waitlist, 80% received kidney transplantation. After adjusting for covariates, patients in the highest income quintile were found to have higher access to both the waitlist (hazard ratio [HR], 1.73; 95% confidence interval [CI], 1.53-1.96) and kidney transplantation (HR, 1.33; 95% CI, 1.16-1.53) compared with patients in the lowest income quintile. Patients with higher education also had better access to the waitlist and kidney transplantation (HR, 2.16; 95% CI, 1.94-2.40; and HR, 1.16; 95% CI, 1.03-1.30, respectively) compared with patients with mandatory education.
Conclusions
Socioeconomic status-related inequalities exist with regard to both access to the waitlist, and kidney transplantation conditional on listing. However, the former inequality is substantially larger and is therefore expected to contribute more to societal inequalities. Further studies are needed to explore the potential mechanisms and strategies to reduce these inequalities.
Renal replacement therapy (RRT) includes kidney transplantation (KTx) and dialysis. Compared with dialysis, KTx generally offers lower morbidity and mortality, increased quality of life, and decreased costs to the family and society.1-4
Ensuring equity in access to the waitlist is an important part of, and key intermediate step in, the effort to ensure equity in access to KTx. It is considered important that patients in equal need of KTx have equal access. Previous international studies have found that age, sex, race,5,6 education,5,7 and marital status7 are associated with access to the waitlist. Socioeconomic status (SES), typically measured through income, education and occupation,5,6,8 appears to play a complex role.5
The results of studies on access to the waitlist that use residential postcodes as a proxy for SES are contradictory. Kihal-Talantikite et al9 report that, in France, living in disadvantaged neighborhoods did not affect the chance of access to the waitlist compared with living in advantaged neighborhoods, whereas studies from the United States and the United Kingdom have shown a negative effect of living in disadvantaged neighborhoods.6,8,10 Two studies from the United States, investigating the effect of individual-level education, found that patients with higher education had a greater chance to be put on the waitlist compared with patients with lower education.5,7
Previous studies have also shown inconsistent associations between SES and access to KTx conditional on waitlisting. Studies from the United Kingdom8 and France9 found that patients living in disadvantaged neighborhoods had an equal chance of KTx compared with patients living in advantaged neighborhoods. However, Schold et al6 found a negative effect of living in disadvantaged neighborhoods in the United States. Regarding education, studies from the US report that higher individual-level education was associated with a higher chance of KTx.5,7
Despite the increase in evidence of SES-related inequalities in access to the waitlist and KTx, the relative influence of individual-level SES remains poorly understood. The most important limitations of previous studies are: (i) income was measured at area-level (postal code or neighborhood poverty),6,10 rather than an individual-level and this introduced measurement error which may lead to bias estimation of the effect of income; (ii) they included only a single measure of SES; and (iii) they included only a subsample of the relevant population9 or lacked potentially important confounders such as blood type6 and comorbidities,5,6 which may lead to overestimation of the SES effects.
Sweden has a publicly funded healthcare system and access to the waitlist and KTx should not depend on SES after adjusting for need and/or capacity to benefit.11 However, individual-level SES-related inequalities in access to KTx have been shown to exist in Sweden.12 There is a paucity of studies on this topic worldwide, not to mention within the context of the Nordic healthcare systems, investigating individual-level SES and access to the waitlist and KTx conditional on waitlist placement. Therefore, using a Swedish population sample and register data, this study will investigate whether there are SES-related inequalities in KTx, by studying 2 specific questions: (i) Are predialysis income and education associated with access to the kidney waitlist? (ii) Are predialysis income and education associated with access to KTx conditional on waitlist placement?
The main contribution of the current registry-based study, with extensive adjustment for predialysis medical, nonmedical factors and individual-level SES measures, is to divide SES-related inequality into inequality of waitlisting and inequality of kidney allocation. Moreover, this study will consider the research gaps regarding individual-level SES inequality within RRT.
MATERIALS AND METHODS
Data Source
All data come from 4 databases: the Swedish Renal Register (SRR)13 the Register of the Total Population,14 the Longitudinal Integration Database for Health Insurance and Labour Market Studies (LISA by Swedish acronym),15 and the Scandia transplant database.16 The detailed information of the databases has previously been described in Zhang et al.12 The SRR, with almost 100% coverage and a data reporting incidence of 95%,17 includes data on all Swedish RRT patients. The Register of the Total Population includes marital status and citizenship information while the LISA includes SES-related data (eg, income and education) up to 10 years before and after dialysis start. Information regarding waitlist placement is derived from the Scandia transplant database.
In Sweden, there are 4 independent transplant centers with (slightly) different policies of allocation of transplants. However, all 4 centers mainly consider blood group compatibility and time on waitlist and should not consider SES. Because some patients have multiple listings/retransplantations, only the first listing/KTx is considered in the current analysis.
Study Population
The study included all adult end-stage renal disease (ESRD) patients who started dialysis between 1 January 1995 and 31 December 2013, as recorded in the SRR (16 943 patients excluding those listed for multiorgan transplantation). Each patient was followed to deceased-donor KTx, death, or the end of the study (June 1, 2015). Patients who met the following criteria were excluded: (i) the current treatment modality was unknown (6 patients, 0.04%); or the patient: (ii) recovered or died within 91 days of start of dialysis (1819 patients, 10.74%), (iii) received preemptive transplantation or living donor transplants after being placed on the waitlist (173 patients, 1.02%), and (iv) was placed on the waitlist before starting dialysis (261 patients, 1.54%). In addition, 1019 observations were excluded due to missing information for other important factors (ie, income [259 patients, 1.53%], education [357 patients, 2.11%], marital status [86 patients, 0.51%]). Therefore, the final sample included 13 982 adult patients on dialysis.
(i) SES indicators
SES indicators included predialysis income and education 1 year (or 5 years, in the sensitivity analysis) before dialysis start. Income was defined as individual (after-tax) disposable income (including income from work and benefits) derived from the household disposable income adjusted for consumption weights.18 The income variable was adjusted to the 2012 price level using the Consumer Price Index from Statistics Sweden19 and was exchanged from Swedish krona (SEK) to Euro (€) using 2012 average exchange rate (€1 = SEK8.7053).20 Income was divided into 5 income quintiles, from quintile 1, the most disadvantaged quintile (income range: €-39 494-11 377), to quintile 5, the most advantaged quintile (income range: €20 992-1.24 × 106). Negative income can occur if a person, for example, is running a business at a loss in a particular year (16 patients; 0.1% of the sample). Education was categorized, according to the Swedish educational system, into mandatory education (≤9 years), secondary education (>9-12 years), and higher education (>12 years).
(ii) Confounding factors
Confounding factors included demographic variables and clinical features at start of dialysis. Demographic variables included age, sex, year of first dialysis, marital status, citizenship, and whether the home county had a KTx center. There are 4 KTx centers in Sweden, located in the 4 largest cities (Stockholm, Gothenburg, Malmö, and Uppsala). A binary variable of home county was created to capture any potential advantage of living in an administrative area where KTx was being performed and/or living close to the performing hospital. Clinical features included primary renal diseases and comorbidities. Comorbidities included blood malignancy, skin malignancy, other malignancy, hypertension, diabetes mellitus, ischemic heart disease, cerebrovascular disease, and peripheral vascular disease. For patients on the waitlist, data also included ABO blood type information.
Statistical Analysis
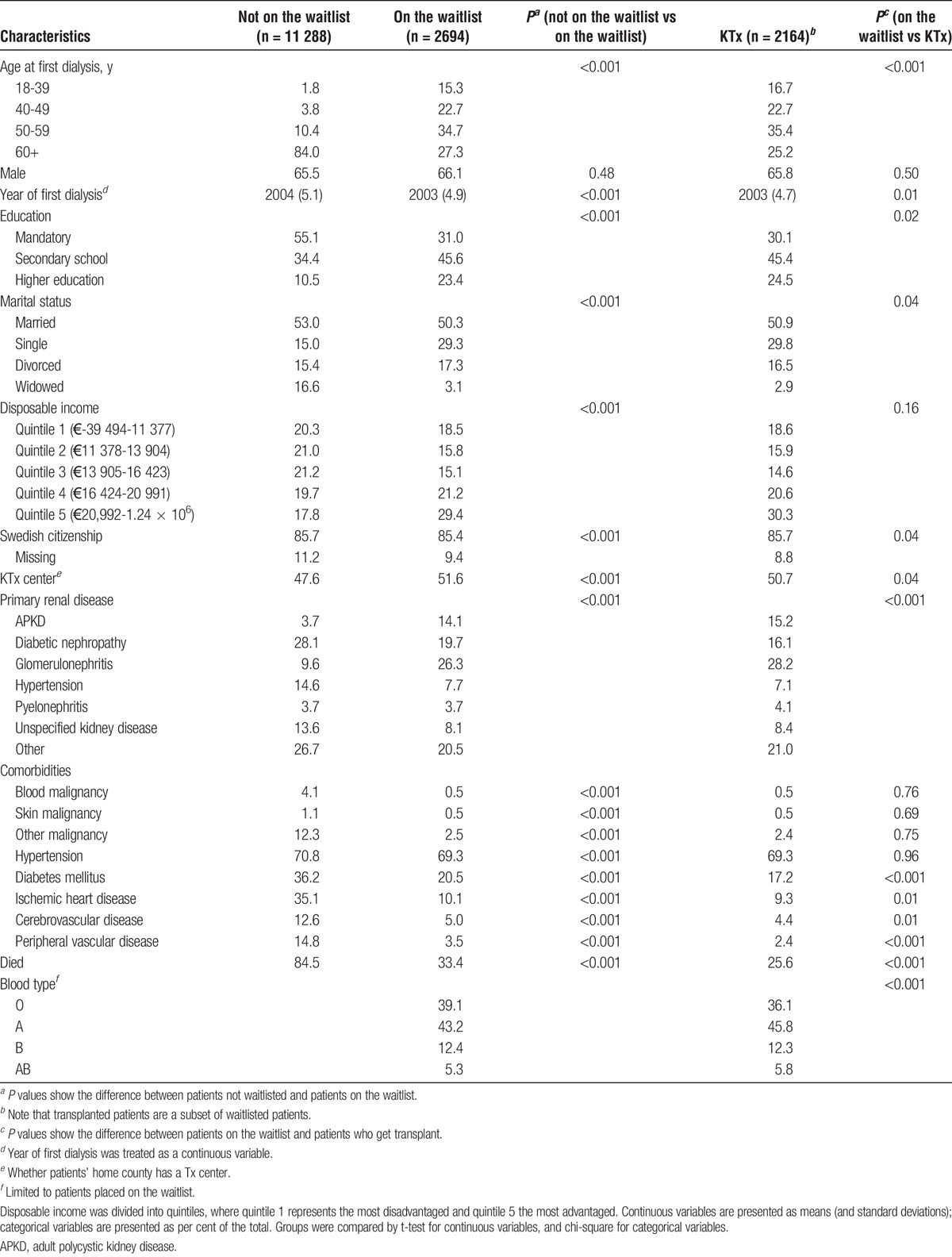
The characteristics of patients, together and separately, based on waitlist/transplantation status, are shown in Table 1. It should be noted that the transplanted patients are a subset of waitlisted patients. The continuous variables are expressed as means and SDs and the categorical variables are expressed as percentages. Between-group comparisons of continuous and categorical variables were done using t and χ2 statistics, respectively.
TABLE 1.
Characteristics of all patients, not waitlisted as well as waitlisted patients, and patients receiving a kidney transplant
Time to waitlisting was calculated as the time from the start of dialysis to the date of placement on the waitlist. Patients not waitlisted were censored at the time of death or at the end of the study. Time to KTx was calculated as the time from placement on the waitlist to the date of the KTx. Patients taken off the waitlist (temporary or permanently), or remaining on the waitlist but not transplanted, were censored at the time of death or at the end of the study.
First, univariate Cox models were used to study the association between income/education and access to the waitlist and KTx, respectively (model 1, Tables 2-5).Then, for income, 3-step multivariate Cox models (models 2-4, Tables 2 and 4) were estimated stepwise adjusting for education (model 2), demographic variables (model 3), and clinical variables (model 4). Income and education were included simultaneously because education can be seen as a factor underlying the association between income and access to KTx. Moreover, we can also explore which was the stronger independent factor that could inform inferences about mechanisms. For education, we performed a similar analysis as for income but without adjusting for income in a 2-step multivariate Cox model (models 2-3, Tables 3 and 5).
TABLE 2.
Association between income and access to the waitlist, by Cox proportional hazard regression (n = 13,982)
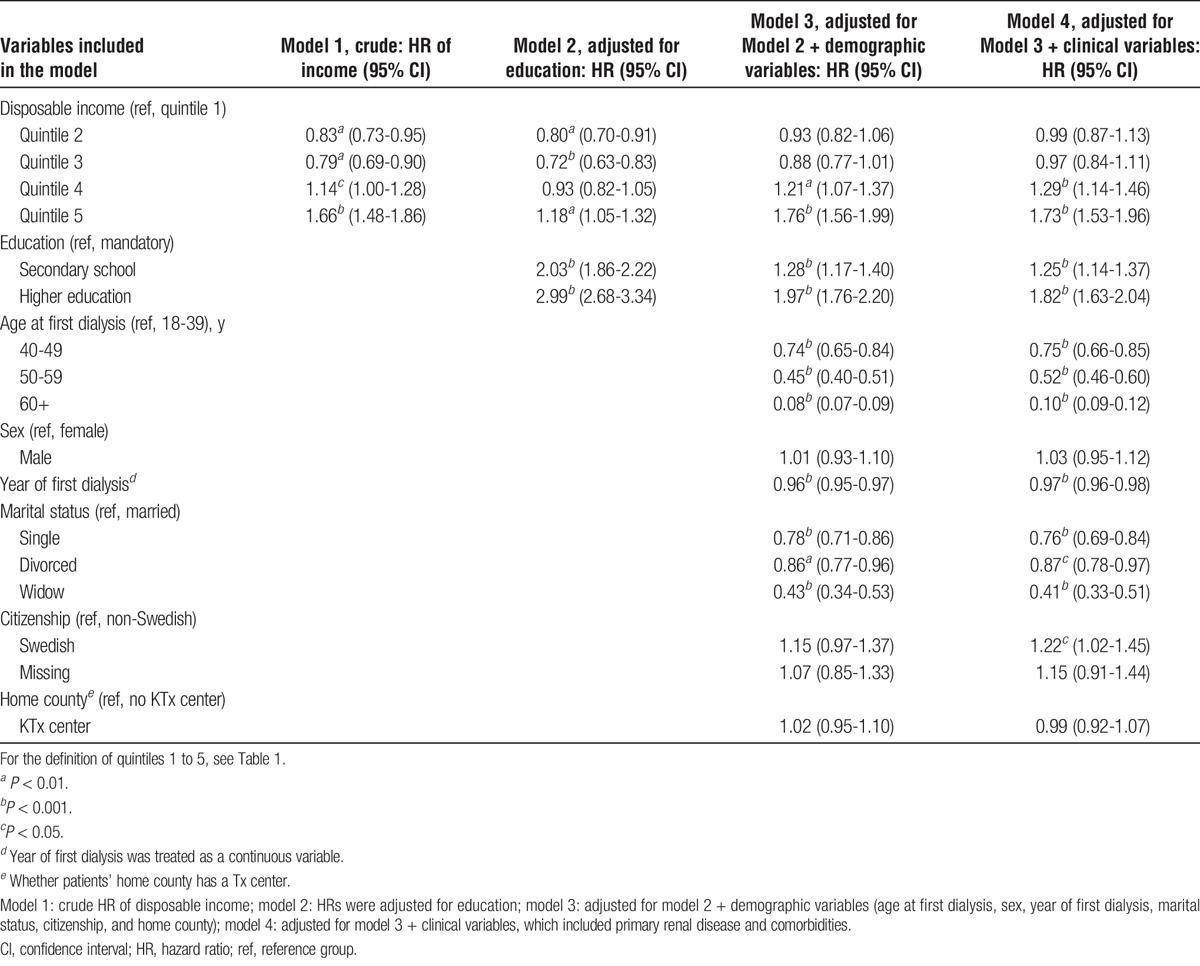
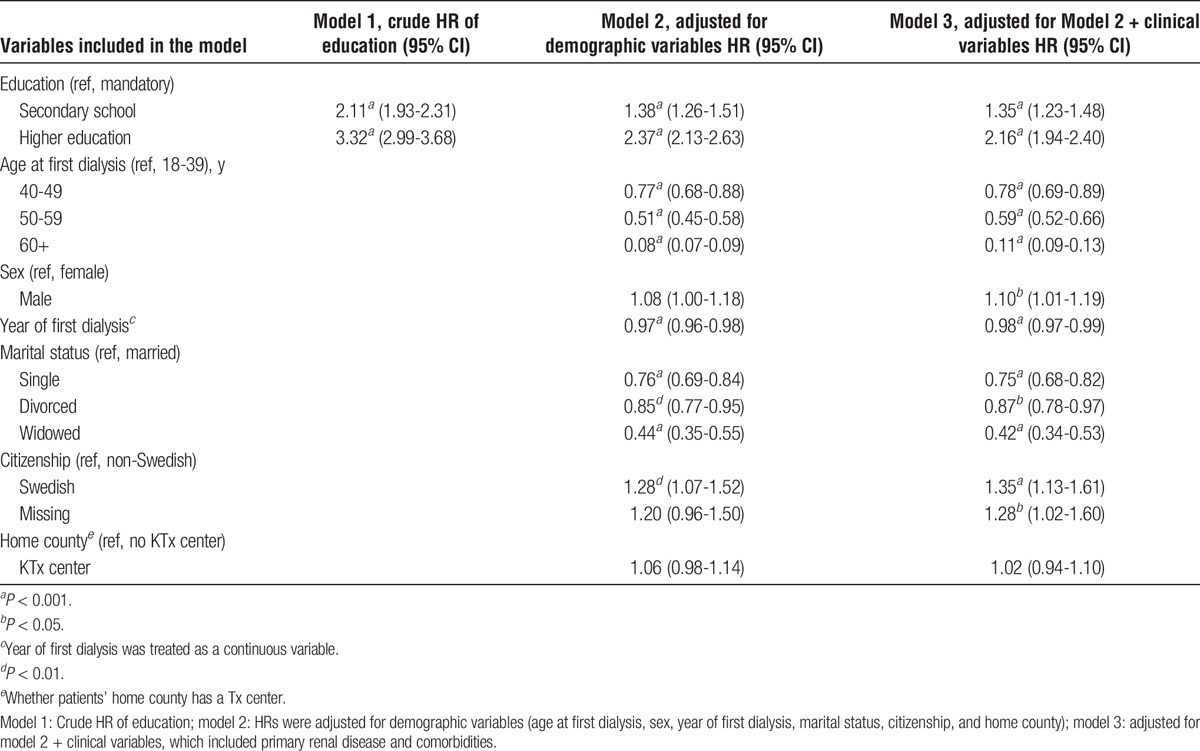
TABLE 5.
Association between education and access to KTx for patients on the waitlist (n = 2,694), by Cox proportional hazard regression
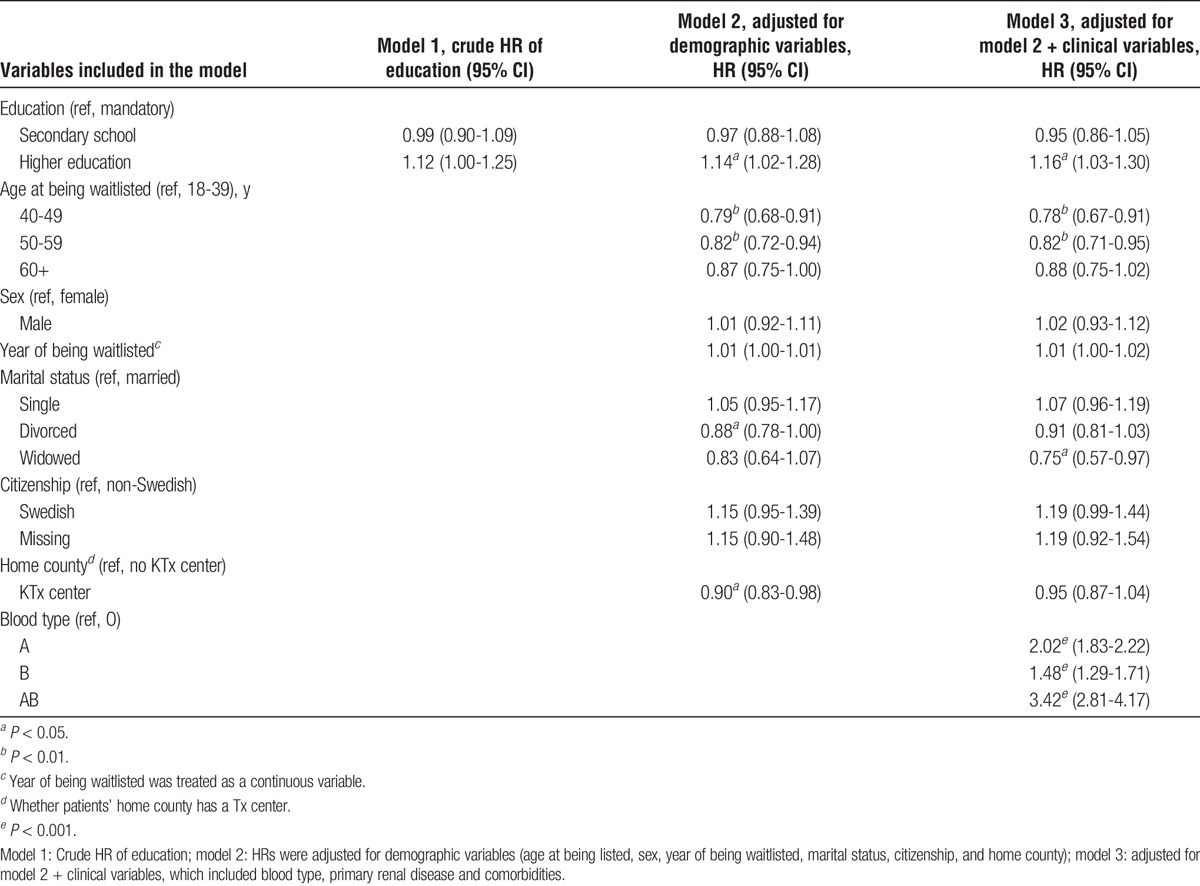
TABLE 4.
Association between income and access to KTx for patients on the waitlist (n = 2,694), by Cox proportional hazard regression
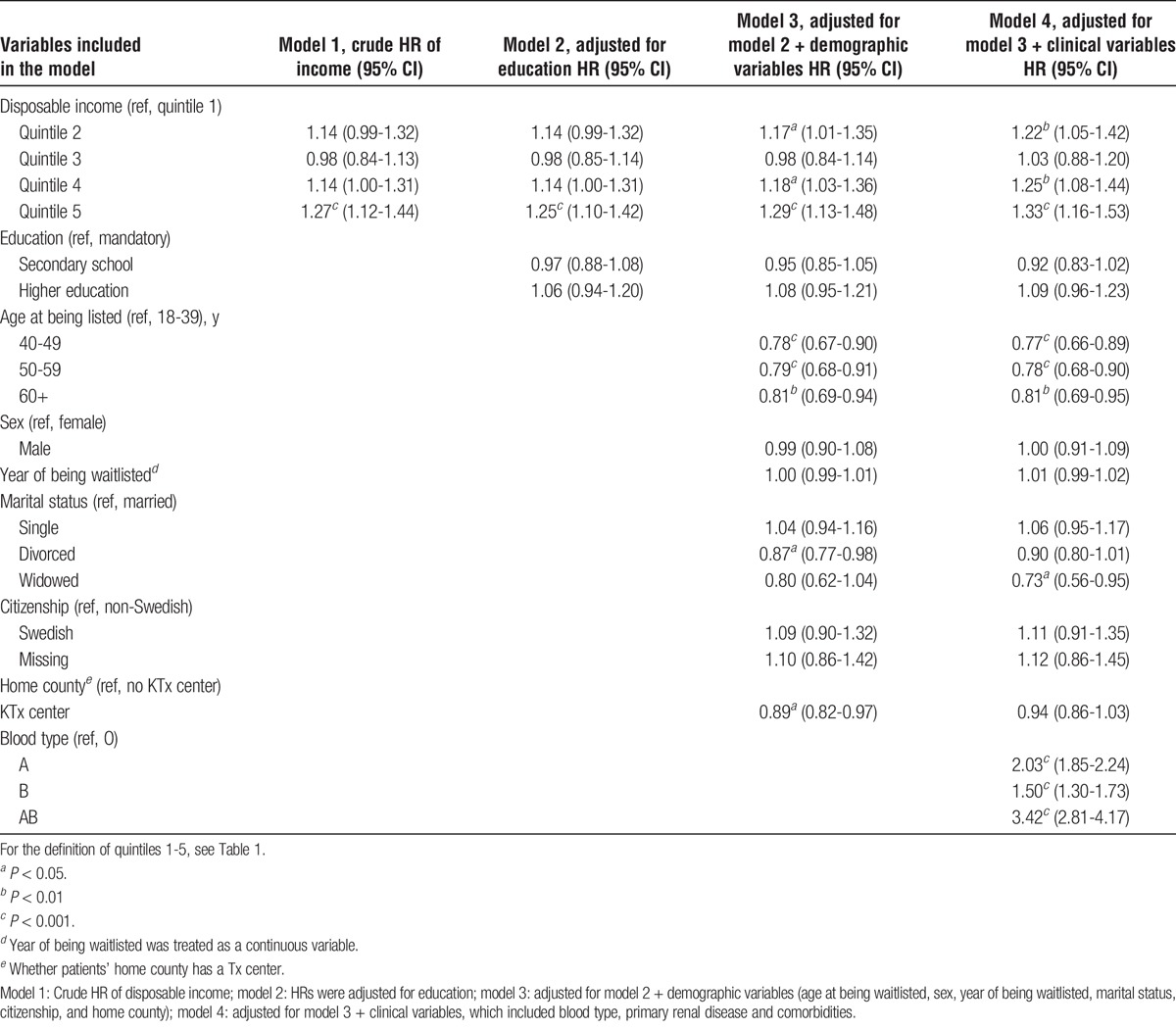
TABLE 3.
Association between education and access to the waitlist, by Cox proportional hazard regression (n = 13,982)
Sensitivity analyses were conducted estimating the association between income 5 years before dialysis and the average income over 5 years before dialysis compared with 1 year before dialysis in the main estimates (models 1-4, supplemental digital content [SDC], Table S1, http://links.lww.com/TXD/A60). We also ran the full models for men and women separately to investigate whether the effects of income and education differ by sex. Moreover, we reran our analysis excluding patients with negative as well as very low disposable income (cutoff, < SEK 70 000) to study if potential misclassification of income threatens to affect the results.
Statistical significance was assumed for P values less than 0.05. All statistical analyses were performed using STATA software, version 14.0 (Stata Corporation, College Station, TX). The study has been approved by Lund Regional Ethical Review Board (Dnr: 2014/144).
RESULTS
Baseline Characteristics
The final sample included 13 982 adult patients on dialysis, 2694 (19.3%) of whom were placed on the waitlist. Among patients on the waitlist, 2164 (80.3%) received a KTx during the study period. Patient characteristics are shown in Table 1. The mean age at starting dialysis was 63.7 years (SD, 15.1), 65.6% was males. According to the univariate analysis, patients on the waitlist were younger, more educated, had higher income, fewer comorbidities, and were more likely to live closer to a transplantation centre compared with patients not on the waitlist (ie, dialysis patients) (P < 0.001). However, there was no sex difference between patients on the waitlist and not on the waitlist (P = 0.48).
Effect of SES on Access to the Kidney Waitlist
Table 2 shows the association between income and access to the waitlist in 4 Cox models. The results from model 1 found a U-shaped relationship between income and access to the waitlist while also showing that patients in quintile 5 had 1.66 times higher likelihood of accessing the waitlist compared with patients in quintile 1 (reference group). The effect of high income decreased substantially when simultaneously adjusting for education (model 2) although remaining positive and significant. Adjusting for demographic variables (model 3) dramatically increased the effect of income while further adjusting for clinical factors (model 4) did not influence the effect of income. The full model (model 4) showed a clear positive association between income and access to the waitlist, as well as removing the U-shaped relationship.
Table 3 shows the association between education and access to the waitlist in 3 Cox models. The results from model 1 found that patients with higher education had more than 3 times the likelihood of placement on the waitlist compared with patients with mandatory education. Although adjusting for other covariates reduced the effect, education was still significantly positively associated with the likelihood of placement on the waitlist in the fully adjusted model (model 3).
Younger age, being married, and having Swedish citizenship was found to increase the likelihood of placement on the waitlist. In the income model, neither sex nor living in the county where the transplantation centre was located was found to have any effect although a small positive effect of male sex was noted in the education model.
Effect of SES on Access to KTx Conditional on Waitlist Placement
Table 4 shows the association between income and access to KTx for waitlisted patients in 4 Cox models. The results from model 1 found that patients in quintile 5 had 1.27 times higher likelihood of receiving KTx compared with patients in quintile 1 (reference group). The effect of high income decreased marginally when simultaneously adjusting for education (model 2). Adjusting also for demographic variables (model 3) and clinical factors (model 4) slightly increased the effect size and showed a clear significant positive association between income and access to KTx. However, the effect seemed to be mostly isolated to the lowest income quintile.
Table 5 shows the association between education and access to KTx in 3 Cox models. The results from model 1 found that higher education had no effect on access to KTx compared with mandatory education. However, after adjusting for demographic variables (model 2) and clinical factors (model 3), a small, significantly positive association between education and access to KTx could be noted.
A positive effect on the likelihood of receiving KTx given waitlist was found for younger age, being married (versus being widowed), and having A, B, or AB blood type. Sex, living in the county in which the transplantation centre was located, and having Swedish citizenship were not found to have an effect on access to KTx.
Sensitivity Analysis
Access to the Kidney Waitlist
When using income 5 years before dialysis, the effect of income decreased compared with the main estimates (model 1 in SDC, Table S1, http://links.lww.com/TXD/A60). The effect of high income increased when using the average income over 5 years before dialysis (model 2, SDC, Table S1, http://links.lww.com/TXD/A60). Both changes were relatively small.
Access to KTx Conditional on Waitlisting
When using income 5 years before dialysis, the effect of income decreased and became nonsignificant compared with the main estimates (model 3, SDC, Table S1, http://links.lww.com/TXD/A60). Using the average income over 5 years before dialysis, the effect of high income decreased compared with the main estimates but remained significant (model 4, SDC, Table S1, http://links.lww.com/TXD/A60).
Men and Women Separately
For both men and women, the effects of income and education on access to the waitlist/KTx were similar to the main estimates (SDC, Table S2 and S3, http://links.lww.com/TXD/A60), as were the effects of other factors (eg, citizenship).
Excluding Patients With Negative and Very Low Disposable Income
Excluding patients with negative and very low disposable income (< SEK 70,000) (SDC, Table S4, http://links.lww.com/TXD/A60), did not change the results compared to the main analysis in any meaningful way.
DISCUSSION
This study indicates that, in Sweden, differences linked to patients' SES exist in the likelihood of being placed on the kidney waitlist and getting a KTx. After multivariate adjustment, patients in the highest income group had a more than 1.7 times and 1.3 times increased chance of access to the waitlist and KTx, respectively, compared with patients in the lowest income group. Patients with higher education had more than 2 times and 1.15 times higher chance of access to the waitlist and KTx, respectively, compared with patients with only mandatory education.
Separate Cox models were constructed, using different groups of covariates to assess their relative contribution on the likelihood to be waitlisted/get a transplant, especially how the effect of income and education changed when adding more covariates. When income was used as the measure of SES, education seemed to be a modifier especially for the difference between the highest and lowest income group in the probability to be waitlist. In particular, the likelihood of listing for the highest income group was reduced, but still statistically significant, after adjustment for education. However, education did not have much effect on the difference between the highest and lowest income group as to access to KTx. Retrospectively, when education was used as a measure of SES, the likelihood of waitlisting for the higher education group decreased, whereas the likelihood of getting a transplant slightly increased when adding covariates gradually.
The socioeconomic gradient was found to be stronger for placement on the waitlist compared with receiving a transplant once on the waitlist. The decision to put a patient on the waitlist is probably more subjective and more vulnerable to inequality because this entails a closer relationship between the treating physician and the patient. The transplantation decision once on the waitlist is more objectively based on medical factors without the patient necessarily meeting the transplantation surgeon.
Moreover, the association between education and access to waitlist is stronger than the association between income and access to waitlist. Because of the more subjective decision to waitlist compared with KTx, this could be explained by education potentially capturing other aspects, such as knowledge and attitudes to disease and treatment, compliance and/or communication skills. Education could therefore be expected to be more related to the likelihood of being waitlisted compared to income, even when income potentially captures aspects of general health (see below).
Income 1 year before dialysis runs the risk of capturing patients’ general health status as a result of the kidney disease as well as their SES status. We therefore conducted sensitivity analyses using both income 5 years and the average income over the 5 years before dialysis. These measures should be less influenced by the patients’ kidney-related health status and should therefore be purer SES measures. The downside of using them is that income levels may have changed over the period and that the income 5 years before dialysis may not be a good indicator of current SES. The results of the sensitivity analysis using average income over 5 years before dialysis were similar but somewhat lower compared with the main analysis on access to KTx given on the waitlist. When income 5 years before dialysis was used as income measurement, the effect of income was further reduced (hazard ratio, 1.15) and only significant on the 5% level. This indicates that income 1 year before dialysis captures aspects of general health, and given a positive effect of health on likelihood of access to KTx, that the estimated association of SES on access to KTx is potentially overestimated. This could also explain why the association between income and KTx is stronger compared with the association between education and KTx, given that education is not affected by current health status. However, to disentangle the health and income (SES) effects, we would need to adjust further for general health, which unfortunately is not available in the current data set.
The data include patients with negative or very low disposable income, who accordingly are categorized in income quintile 1. There are several potential reasons for such low income level despite that the Swedish social insurance systems should guarantee everyone a certain “liveable” income level. The main concern is that these individuals might belong to very rich households that, for example, evade tax or live on savings during a particular year. This potential misclassification could introduce an underestimation of the effect of income. However, excluding patients with a disposable income below SEK 70, 000 resulted only in a very small reduction of the association between income and likelihood of getting a transplant compared with the baseline results. This indicates that the results are not sensitive to potential misclassification of rich individuals as poor due to negative or very low disposable income during a particular year.
We could also show that A, B, and AB blood types were all associated with a higher probability of receiving KTx compared with O blood type, whereas 1 study found the positive association only for A and AB blood types.9 This discrepancy could potentially be explained by the relative proportion of different blood types in different countries.21 In addition, a small positive effect of male sex was shown when estimating the effect of education on access to the waitlist. The possible reason for this may be that disposable income is lower for women than men, which is captured by the sex variable when income is not adjusted for.
The current results are consistent with studies from the United States,5,7 showing that higher education was associated with greater likelihood of being placed on the waitlist and undergoing KTx and the International Dialysis Outcomes and Practice Patterns Study,22 which found that education was not associated with access to KTx when adjusting for income. The current results regarding income are also consistent with studies from the United States,6,10 showing an association between living in lower SES neighborhoods and decreased likelihood to complete steps to KTx. Contrary to this, other studies from France9 and the United Kingdom8 found no effect of SES neighborhoods on likelihood of being waitlisted or receiving KTx. In the current study, though the effect size of SES was lower for getting a transplant compared with being placed on the waitlist, it was still significant. These conflicting results between the current study and prior studies may be due to use of different SES measures: individual-level versus area-level SES (eg, neighborhood deprivation, degree of urbanization,9 and Carstairs score to assess social deprivation8). In addition, differences in healthcare systems between countries might be another possible reason for these conflicting results.
Potential reasons for SES discrepancies in access to KTx lie with both the patients and the healthcare provider. From the healthcare provider side, studies have found bias in identifying potential transplant candidates.23 From the patient side, SES-disadvantaged patients may have more, and more severe, comorbidities and worse adherence compared with SES-advantaged patients.5,24 Lower education is associated with factors, such as smoking, less exercise, and overweight, by themselves relative contraindications to transplantation or factors with impact on comorbidities that are contraindications.25 Differences in knowledge, attitudes to disease and treatment, and preference for transplantation may lead to different treatment choices by SES-disadvantaged patients compared to SES-advantaged patients.8 Hence, SES may have both a direct effect on access to KTx process (eg, through discrimination) and an indirect effect (operating through patients’ preference).26 The SES inequalities shown above are therefore not necessarily due to discrimination. However, they will still contribute to societal inequalities in health and wealth, and as such, it is of interest to mitigate them.
A limitation of this study is that although we controlled for many important confounding factors, we lack information on other unobserved factors (eg, more measures of general health, adherence, race/ethnicity, patients’ preference, and physician bias) and other biochemical data (eg, serum albumin level and other measures of inflammation; levels of parathyroid hormone) which also are associated with access to KTx.9 Additionally, we have information on comorbidities but not about their severity, nor about changes during follow-up.
In addition to the limitations above, there are important strengths. Instead of geographically defined SES, 2 classic individual-level SES indicators, education and income, were used and were expected to better capture the SES and thereby give more accurate effect estimates. In addition, population based national register data with almost 100% coverage and a data reporting incidence of 95%17 gives the study high power and excellent generalizability to ESRD patients in Sweden.
CONCLUSION
Individual-level low income and education both are associated with a reduced chance of access to the waitlist and KTx among Swedish ESRD patients. However, the factors behind the observed SES inequalities in Swedish Health Care System, which aims to provide good and equal healthcare for all Swedish citizens, are unknown. To this end, further studies are needed to identify the mechanisms behind these inequalities to construct interventions to reduce SES barriers and to assess if these inequalities are unfair inequalities.
Supplementary Material
ACKNOWLEDGMENTS
This study was based on data and received (nonfinancial) support from the Swedish Renal Registry, which is gratefully acknowledged.
Footnotes
Published online 24 January, 2018.
Y.Z. received funds from the China Scholarship Council (CSC) to perform this research as a part of her PhD thesis. Financial support from the Swedish Research Council (Dnr 2014-646) is gratefully acknowledged. The Health Economics Programme (HEP) at Lund University receives core funding from the Government Grant for Clinical Research (“ALF”) and the Region Skåne (Gerdtham).
The authors declare no conflicts of interest.
Y.Z. is the first author and conducted the data analysis, interpretation and write-up of the article. J.J. and U.-G.G. contributed in study design, interpretation of the results and the writing of the article. H.R. contributed with clinical consultation, interpretation of the results and writing.
Supplemental digital content (SDC) is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal’s Web site (www.transplantationdirect.com).
REFERENCES
- 1.Wolfe RA, Ashby VB, Milford EL, et al. Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. N Engl J Med. 1999;341:1725–1730. [DOI] [PubMed] [Google Scholar]
- 2.Neipp M, Karavul B, Jackobs S, et al. Quality of life in adult transplant recipients more than 15 years after kidney transplantation. Transplantation. 2006;81:1640–1644. [DOI] [PubMed] [Google Scholar]
- 3.Eggers P. Comparison of treatment costs between dialysis and transplantation. Semin Nephrol. 1992;12:284–289. [PubMed] [Google Scholar]
- 4.Jarl J, Desatnik P, Peetz Hansson U, et al. Do kidney transplantations save money? A study using a before–after design and multiple register-based data from Sweden. [published online August 7, 2017]. Clin Kidney J. doi.org/10.1093/ckj/sfx088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schaeffner ES, Mehta J, Winkelmayer WC. Educational level as a determinant of access to and outcomes after kidney transplantation in the United States. Am J Kidney Dis. 2008;51:811–818. [DOI] [PubMed] [Google Scholar]
- 6.Schold JD, Gregg JA, Harman JS, et al. Barriers to evaluation and wait listing for kidney transplantation. Clin J Am Soc Nephrol. 2011;6:1760–1767. [DOI] [PubMed] [Google Scholar]
- 7.Khattak MW, Sandhu GS, Woodward R, et al. Association of marital status with access to renal transplantation. Am J Transplant. 2010;10:2624–2631. [DOI] [PubMed] [Google Scholar]
- 8.Oniscu GC, Schalkwijk AA, Johnson RJ, et al. Equity of access to renal transplant waiting list and renal transplantation in Scotland: cohort study. BMJ. 2003;327:1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kihal-Talantikite W, Vigneau C, Deguen S, et al. Influence of socio-economic inequalities on access to renal transplantation and survival of patients with end-stage renal disease. PLoS One. 2016;11:e0153431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Saunders MR, Cagney KA, Ross LF, et al. Neighborhood poverty, racial composition and renal transplant waitlist. Am J Transplant. 2010;10:1912–1917. [DOI] [PubMed] [Google Scholar]
- 11.Qureshi AR, Evans M, Stendahl M, et al. The increase in renal replacement therapy (RRT) incidence has come to an end in Sweden-analysis of variations by region over the period 1991-2010. Clin Kidney J. 2013;6:352–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang Y, Jarl J, Gerdtham UG. Are there inequities in treatment of end-stage renal disease in Sweden? A longitudinal register-based study on socioeconomic status-related access to kidney transplantation. Int J Environ Res Public Health. 2017;14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.SNR. Swedish Renal Registry. http://www.medscinet.net/snr. Accessed Sep 15, 2017.
- 14.Statistics Sweden. Register of the Total Population (RTB). https://www.scb.se/sv_/Vara-tjanster/Bestalla-mikrodata/Vilka-mikrodata-finns/Registret-over-totalbefolkningen-RTB/. Accessed Oct 19, 2017.
- 15.Statistics Sweden (SCB). LISA database. Secondary LISA database. http://www.scb.se/en_/Services/Guidance-for-researchers-and-universities/SCB-Data/Longitudinal integration-database-for-health-insurance-and-labour-market-studies-LISA-by-Swedish-acronym/.eng; http://www.scb.se/lisa/swedish. Accessed September 15, 2017.
- 16.Scandia transplant database. http://www.scandiatransplant.org/. Accessed Oct 19, 2017.
- 17.Schon S, Ekberg H, Wikstrom B, et al. Renal replacement therapy in Sweden. Scand J Urol Nephrol. 2004;38:332–339. [DOI] [PubMed] [Google Scholar]
- 18.Longitudinell integrationsdatabas för Sjukförsäkrings—och Arbetsmark nadsstudier (LISA) 1990–2013. http://www.scb.se/Statistik/AM/AM9901/_dokument/AM9901_1990I13_BR_AM76BR1601.pdf. Accessed Sep 15, 2016.
- 19.Statistics Sweden (SCB). http://www.scb.se/en_/Finding-statistics/Statistics-by-subject-area/Prices-and-Consumption/Consumer-Price-Index/Consumer-Price-Index-CPI/Aktuell-Pong/33779/Consumer-Price-Index-CPI/272151/. Accessed September 15, 2016.
- 20.The Swedish Central Bank Annual average exchange rates. http://www.riksbank.se/sv/Rantor-och-valutakurser/Sok-rantor-och-valutakurser/?g130-SEKEURPMI=on&from=2012-01-02&to=2012-12-28&f=Year&cAverage=Average&s=Comma#search. Accessed June 09, 2016.
- 21.Christian Baudelot YC, Olivier Godechot, Sylvie Mercier. Renal diseases and social inequalities in access to transplantation in France. Population (Engl Ed). 2016;71:023–052. [Google Scholar]
- 22.Satayathum S, Pisoni RL, McCullough KP, et al. Kidney transplantation and wait-listing rates from the international Dialysis Outcomes and Practice Patterns Study (DOPPS). Kidney Int. 2005;68:330–337. [DOI] [PubMed] [Google Scholar]
- 23.Kasiske BL, London W, Ellison MD. Race and socioeconomic factors influencing early placement on the kidney transplant waiting list. J Am Soc Nephrol. 1998;9:2142–2147. [DOI] [PubMed] [Google Scholar]
- 24.Kasiske BL, Ramos EL, Gaston RS, et al. The evaluation of renal transplant candidates: clinical practice guidelines. Patient Care and Education Committee of the American Society of Transplant Physicians. J Am Soc Nephrol. 1995;6:1–34. [DOI] [PubMed] [Google Scholar]
- 25.Cowell AJ. The relationship between education and health behavior: some empirical evidence. Health Econ. 2006;15:125–146. [DOI] [PubMed] [Google Scholar]
- 26.Moscelli G, Siciliani L, Gutacker N, et al. Socioeconomic inequality of access to healthcare: does choice explain the gradient? [published online June 23 2017]. J Health Econ. 2017; doi: 10.1016/j.jhealeco.2017.06.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


