Abstract
Squamous cell carcinoma (SCC) of the head and neck affects a significant number of people around the world every year. Treatment generally entails surgical resection, radiotherapy, chemotherapy, or some combination of the three. Following resection, microsurgical reconstruction can provide definitive coverage, replace many tissue types simultaneously, and bring healthy tissue to irradiated wound beds. Microsurgical engineering, the manipulation and reorganization of native vascular tissue, can further augment the adaptability of free tissue transfer to complex, compromised wound beds. We present one such case. The patient described in the following report was treated for a recurrent SCC of the left face, which required extensive resection resulting in a complex, composite tissue defect with compromised vascular supply. Using the principals of microsurgical engineering, definitive coverage of the defect, with accept- able aesthetic result, was achieved via bipedicle, DIEP flap with flow-through intraflap anastomosis.
Squamous cell carcinoma (SCC) represents 95% of head and neck cancers (HNCs) and was forecast to cost the United States health care system 3.6 billion dollars in 2014.1 Treatment entails a combination of surgical resection, radiation therapy, and chemotherapy. Initial tumor resection typically involves straightforward conventional or microsurgical reconstruction. Following tumor extirpation, microsurgical reconstruction provides definitive wound coverage, can replace multiple tissue types, and brings healthy tissue into complicated wounds where radiation has reduced local tissue regenerative capacity.2,3 Challenges arise in recurrent disease resulting in postresection composite defects in irradiated surgical fields with limited microsurgical recipient vessel options. This report describes a bipedicle, flow-through deep inferior epigastric artery perforator (DIEP) flap for the reconstruction of a large defect secondary to extensive resection of HNC and introduces the concept of microsurgical engineering for management of complex, composite tissue defects.
CASE DESCRIPTION
A 52-year-old Caucasian male with a 10-year history of recurrent skin cancer presented with a large recurrence of previously resected SCC of the left conchal bowl. He previously underwent resection of a contralateral facial SCC, which was reconstructed with an anterolateral thigh flap with postoperative radiation therapy.
Resection included removal of the left ear, parotid gland, facial nerve, mandibular condyle, and distal external carotid artery, which was ligated at the glenoid fossa. The left temporal bone was also partially resected, and a left-sided radical neck dissection was performed. The bony defect had no intracranial extension. The resultant defect measured 18 × 18 cm (Fig. 1). Adequate recipient vessels were limited. A branch of the internal jugular vein and take-off of the facial artery remained and were suitable for microsurgical recipient vessel anastomosis.
Fig. 1.
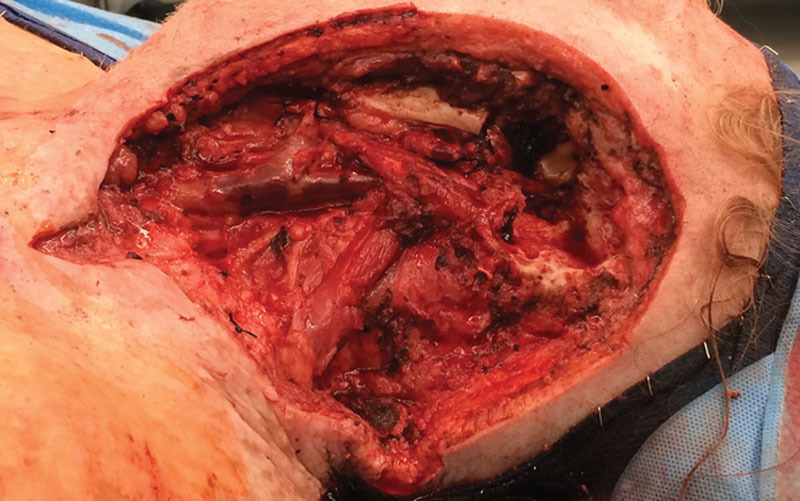
Defect following resection.
Given the size of the defect, planned postoperative radiation, and the patient’s body habitus, the abdomen was chosen as the donor site. A 30 × 18 cm bipedicle, DIEP flap with flow-through intraflap anastomosis was designed (Fig. 2). The bipedicle DIEP flap was raised in standard fashion with a single medial row perforator perfusing each hemiabdomen.
Fig. 2.
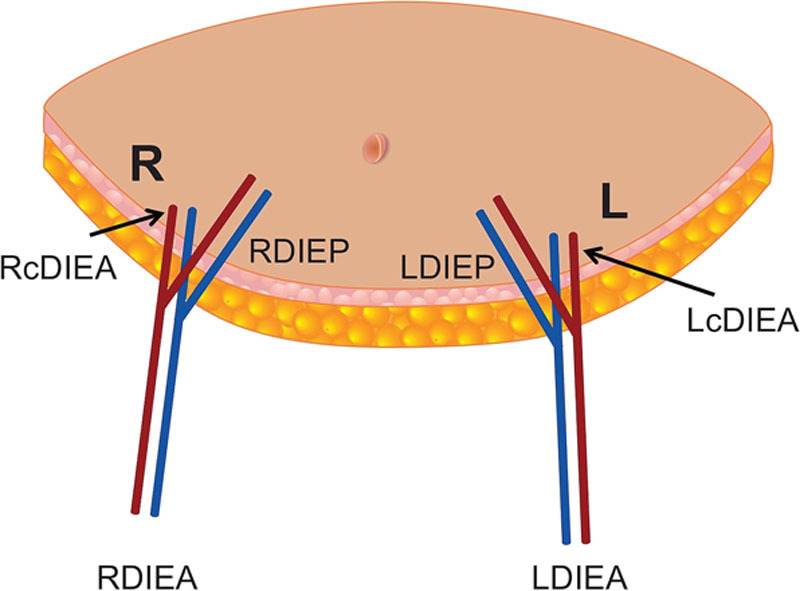
Flap anatomy before harvest. LcDIEA, left cephalad deep inferior epigastric artery/vein; LDIEA, left deep inferior epigastric artery/vein; LDIEP, left deep inferior epigastric artery perforator; RcDIEA, right cephalad deep inferior epigastric artery/vein; RDIEA, right deep inferior epigastric artery/vein; RDIEP, right deep inferior epigastric artery perforator.
The flap was oriented to cover the defect such that the left hemiabdomen was cephalad and the right hemiabdomen was caudal. The caudal venous anastomosis was accomplished by coupling the right deep inferior epigastric vein to a ligated branch of the internal jugular vein. The right deep inferior epigastric artery was anastomosed to the facial artery using 9-0 nylon suture. The caudal left DIEP vessels were anastomosed to the cephalic continuation of the right DIEP vessels (Fig. 3). The lateral zone was trimmed off both hemiabdominal flaps and inset to fit the defect (Fig. 4). The postoperative course was uneventful, and the patient was discharged on postoperative day 6. At 5-month follow-up, the patient continues radiation therapy with a viable flap and stable reconstruction.
Fig. 3.
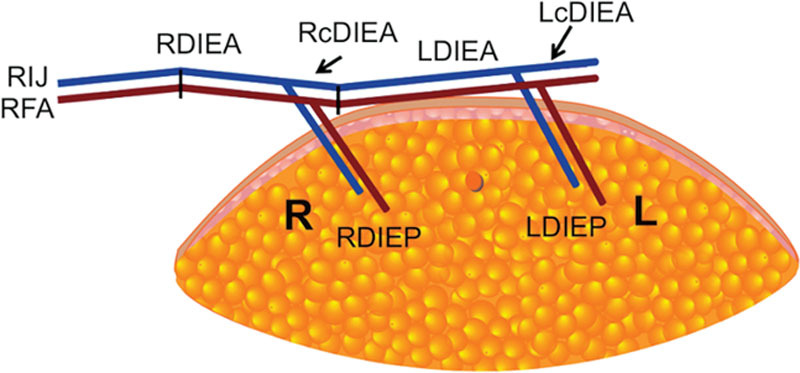
Microsurgically engineered bilateral DIEP flap with intra-flap flow-through anastomosis. LcDIEA, left cephalad deep inferior epigastric artery/vein; LDIEA, left deep inferior epigastric artery/vein; LDIEP, left deep inferior epigastric artery perforator; RcDIEA, right cephalad deep inferior epigastric artery/vein; RDIEA, right deep inferior epigastric artery/vein; RDIEP, right deep inferior epigastric artery perforator. RIJ, right internal jugular vein; RFA, right facial artery.
Fig. 4.
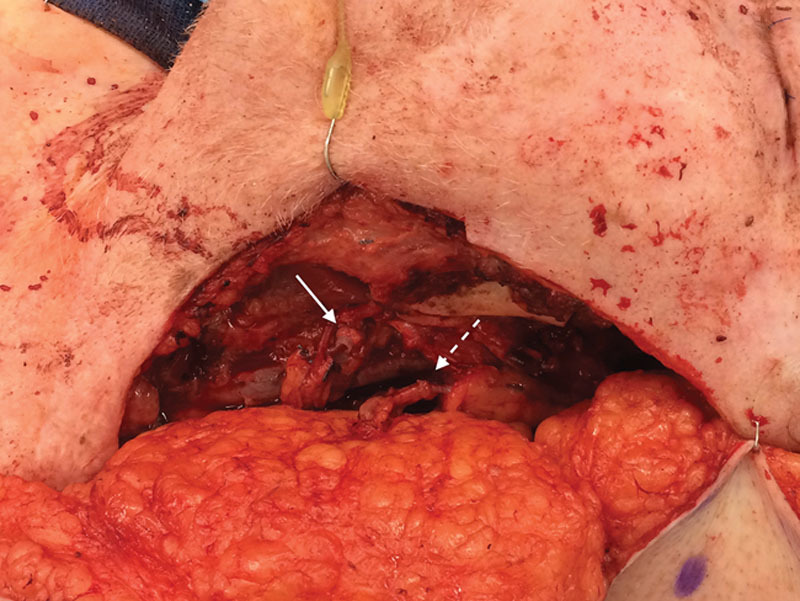
Flap anatomy at inset. Donor/recipient arterial and venous anastomoses (solid arrow), intra-flap right cephalad deep inferior epigastric artery/vein to left deep inferior epigastric artery/vein anastomoses (dashed arrow).
DISCUSSION
In large, complicated head and neck reconstructions where regional pedicle flaps, such as the pectoralis major flap, would not provide sufficient coverage, free tissue transfer delivers predictable defect coverage. Flaps commonly used for reconstruction of large defects include anterolateral thigh flaps, thoracodorsal artery perforator flaps, and DIEP flaps, to name a few.2 In the era of modern microsurgery, DIEP flaps are gaining support for reconstruction of HNC-related defects by virtue of their versatility, reliable vascular supply, and high flap survival rate (97.1%).4,5 This discussion presents evidence that demonstrates the suitability of DIEP flaps for coverage of large head and neck defects and additionally highlights the versatility of the bilateral DIEP systems for use in engineering microsurgical solutions to complex reconstructive problems.
The vessel-depleted neck is often an unintended consequence of HNC tumor extirpation and cannot be adequately planned for using preoperative imaging. Microsurgical engineering—the manipulation and reorganization of native vascular tissue—is requisite for efficient coverage in such cases. Boasting a mean perforator length of 10 cm, perforator diameter of 2.16 mm, vascular territory of 296 cm2, and reliable vascular anatomy the DIEP pedicle is a superb candidate for microsurgical engineering by merit of its versatility and pliability.6,7 Additionally, outflow may be augmented via the superficial inferior epigastric vessels, which can easily be identified intraoperatively.8 In this case, manipulation of the pedicle and recipient site vasculature allowed for creation of a viable intraflap flow-through anastomosis, complete with an identified superficial inferior epigastric vessel lifeboat—an uncommon pattern for DIEP vessel anastomosis to be sure, but one that ultimately proved dependable in our patient.
Head and neck defects present a challenge to reconstructive surgeons as they balance effective coverage with aesthetic, functional long-term results. For this reason, adipocutaneous flaps, such as the DIEP flap, are advantageous. The subcutaneous fat of the DIEP flap is easily contoured via liposuction and has proven to maintain superior bulk and form relative to muscular flaps, which decrease in total volume as denervation and atrophy occur.5 Furthermore, the DIEP flap is favorable for allowing vascularized bone transfer, potentially via fibula-derived free flap, for bony reconstruction of the jaw during a subsequent operation.9 In addition to volume maintenance and superior secondary contouring, vascularized fat facilitates disease surveillance by creating a distinct plane on postoperative imaging, most notably T1-weighted Magnetic Resonance Imaging, to aid in recurrence detection.2
A final consideration in this discussion is morbidity. DIEP flaps spare vital donor-site structures, resulting in decreased postoperative pain and minimal loss of function.2 Decreased donor-site morbidity and increased total quality-adjusted life years, relative to other muscle-sparing abdominal flaps, have propelled DIEP flaps to the forefront of autologous breast reconstruction.10 DIEP flap reconstruction can be applied to complicated head and neck defects while maintaining the standard of low donor-site morbidity, which is a mainstay of contemporary microsurgery.5
CONCLUSIONS
We believe that flow-through, bipedicle DIEP free flaps present a viable, safe method for closing large defects of the head and neck secondary to resection of recurrent HNC. DIEP flaps merit consideration in such instances due to demands of the vessel-depleted neck, superior benefits of an adipocutaneous flap, and minimal associated donor-site morbidity. Application of the principals of microsurgical engineering to a robust, versatile substrate allowed for satisfactory closure of this large facial defect by means of a bipedicle flow-through DIEP flap.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.A snapshot of head and neck cancer. National Cancer Institute. Available at http://www.cancer.gov/research/progress/snapshots/head-and-neck. 2014. Accessed December 16, 2016.
- 2.Guerra AB, Lyons GD, Dupin CL, et al. Advantages of perforator flaps in reconstruction of complex defects of the head and neck. Ear Nose Throat J. 2005;84:441–447.. [PubMed] [Google Scholar]
- 3.Urken ML, Weinberg H, Buchbinder D, et al. Microvascular free flaps in head and neck reconstruction. Report of 200 cases and review of complications. Arch Otolaryngol Head Neck Surg. 1994;120:633–640.. [DOI] [PubMed] [Google Scholar]
- 4.Masià J, Sommario M, Cervelli D, et al. Extended deep inferior epigastric artery perforator flap for head and neck reconstruction: a clinical experience with 100 patients. Head Neck. 2011;33:1328–1334.. [DOI] [PubMed] [Google Scholar]
- 5.Clemens MW, Davison SP. Buried deep inferior epigastric perforator flaps for complex head and neck contour defects. J Reconstr Microsurg. 2009;25:81–88.. [DOI] [PubMed] [Google Scholar]
- 6.Wong C, Saint-Cyr M, Mojallal A, et al. Perforasomes of the DIEP flap: vascular anatomy of the lateral versus medial row perforators and clinical implications. Plast Reconstr Surg. 2010;125:772–782.. [DOI] [PubMed] [Google Scholar]
- 7.Ireton JE, Lakhiani C, Saint-Cyr M. Vascular anatomy of the deep inferior epigastric artery perforator flap: a systematic review. Plast Reconstr Surg. 2014;134:810e–821e.. [DOI] [PubMed] [Google Scholar]
- 8.Rothenberger J, Amr A, Schiefer J, et al. A quantitative analysis of the venous outflow of the deep inferior epigastric flap (DIEP) based on the perforator veins and the efficiency of superficial inferior epigastric vein (SIEV) supercharging. J Plast Reconstr Aesthet Surg. 2013;66:67–72.. [DOI] [PubMed] [Google Scholar]
- 9.Taylor GI, Corlett RJ, Ashton MW. The evolution of free vascularized bone transfer: a 40-year experience. Plast Reconstr Surg. 2016;137:1292–1305.. [DOI] [PubMed] [Google Scholar]
- 10.Zoghbi Y, Gerth DJ, Tashiro J, et al. Deep inferior epigastric perforator versus free transverse rectus abdominis myocutaneous flap: complications and resource utilization. Ann Plast Surg. 2017;78:516–520.. [DOI] [PubMed] [Google Scholar]


