Supplemental Digital Content is available in the text.
Abstract
Background:
When tissue expansion is necessary in breast reconstruction, a single-stage approach is possible using adjustable expander/implants, with or without the use of acellular dermal matrix. We aimed to present the senior author’s single-stage experience over a period of 12 years using combined expander/implants in breast reconstruction.
Methods:
This is a Single-institution, retrospective review of breast reconstruction with combined expander/implants from 2002 to 2014. Logistic regression was performed to evaluate the impact of multiple variables on long-term outcomes.
Results:
A total of 162 implants in 105 patients were included in this study. Mean follow-up time was 81.7 months (SD, ± 39.2; range, 15–151). Complication rates were as follows: 0.62% extrusion, 1.2% mastectomy flap necrosis, 1.2% hematoma, 1.9% dehiscence, 2.5% seroma, 4.9% infection, and 15.4% deflation. The following associations were identified by logistic regression: adjuvant radiotherapy and capsular contracture (P = 0.034), tumor size and deflation (P = 0014), and smoking history and infection (P = 0.013).
Conclusions:
Overall, 81% of breasts were successfully reconstructed in a single stage. Single-stage reconstruction using all-in-one expander/implants reduces costs by eliminating the need for a second procedure under general anesthesia and can achieve results comparable with other alloplastic reconstructions reported in the literature.
INTRODUCTION
Breast cancer remains the most commonly diagnosed and the second leading cause of death from cancer in women in North America.1 Given the increasing trend in both prophylactic (BRCA gene carriers) and curative mastectomies, along with the accomplishments of breast reconstruction awareness events, there is an increasing demand for breast reconstruction. Before 2002, autologous reconstruction was the most popular method of reconstruction in the United States.2 However, after 2008, implant-based reconstruction outnumbered autologous reconstruction by a ratio of 2:1 (258 versus 120 per 1,000 mastectomies), a ratio that is even higher today. According to the American Society of Plastic Surgeons, 2-stage implant-based breast reconstruction accounts for 72.6% of all breast reconstruction.3 The single-stage approach has been gaining popularity recently due to improved techniques, use of acellular dermal matrix, and improved patient selection.4,5 With proper patient selection, direct-to-implant reconstruction can have similar complication rates when compared with a 2-stage approach.6 In cases where tissue expansion is necessary or when asymmetry is significant, a single-stage approach with all-in-one adjustable expander/implants is a possibility. Spectrum is a single lumen saline-filled implant with a removable external port allowing adjustability postoperatively, with the patient’s input. These implants have a remote fill-tube, similar to a subcutaneous port-a-cath, for optional postoperative saline expansion. Once the desired breast size is achieved, the fill-tube and valve are removed under local anesthesia and the expander becomes a permanent implant, eliminating the need for a second procedure under general anesthesia. The primary objective of this study was to present this alternative approach of single-stage breast reconstruction using Spectrum (Mentor Worldwide LLC, Santa Barbara, Calif.), which has been the reconstructive modality of choice of the senior author for the past 12 years.
METHODS
After approval from the institutional Research Ethics Board, we performed a retrospective review of all patients who underwent alloplastic breast reconstruction with a senior breast surgeon at our institution (senior author). A total of 120 patients underwent reconstruction with Spectrum expander/implants between January 2002 and January 2014. Data were collected from both electronic and paper medical records by 2 independent reviewers. Patients with congenital breast deformities were excluded. All procedures were performed by the senior author in a single center (McGill University Health Centre). An inframammary fold incision (IMF) was used for the subpectoral implant placement in all delayed reconstructions, despite the mastectomy scar. Initially, the senior author used anatomical textured expander/implants; however, the shell thickness was palpable in many patients. Moreover, due to recent concerns of anaplastic large cell lymphoma, only smooth expander/implants have been used in the past 18 months. Consistent use of acellular dermal matrix began in 2012 in immediate reconstruction. All implants underwent irrigation with triple antibiotic solution before insertion. All valves are placed below the IMF at the anterior axillary line. Valve location can be appreciated in Figure 1. Figure 2 is an example of a long-term result, postvalve removal under local anesthesia. Details of our surgical technique are demonstrated in video, Supplemental Digital Content 1, which displays the all-in-one adjustable expander/implant technique. This video is available in the “Related Videos” section of PRSGlobalOpen.com or at http://links.lww.com/PRSGO/A631. Nipple-areolar complex reconstruction and fat grafting procedures that are performed at the same time by the senior author were not recorded. The following outcomes were recorded: hematoma, seroma, infection, necrosis, dehiscence, capsular contracture, deflation, and extrusion. Patient, cancer- and treatment-related variables were also recorded (Table 1). Logistic regression was performed to study the association between all variables and postoperative outcomes. Means and frequencies were calculated for continuous variables and categorical data, respectively. Statistical significance was set at a P value of 0.05. All analyses were carried out using the statistical program SPSS (SPSS Inc., Chicago, IL).
Fig. 1.
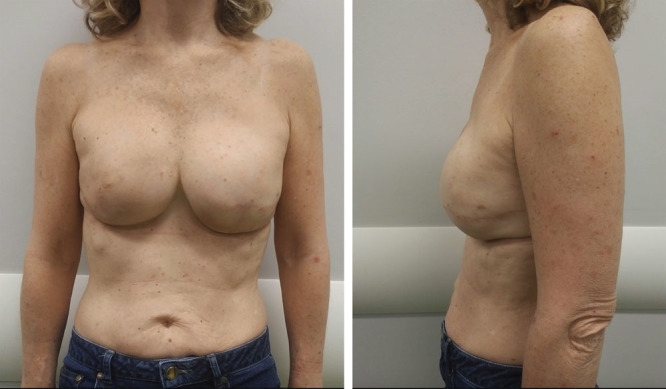
A 56-year-old female 6 months post bilateral skin-sparing mastectomy with immediate Spectrum expander/implant reconstruction. The external port is visible below the inframammary folds.
Fig. 2.
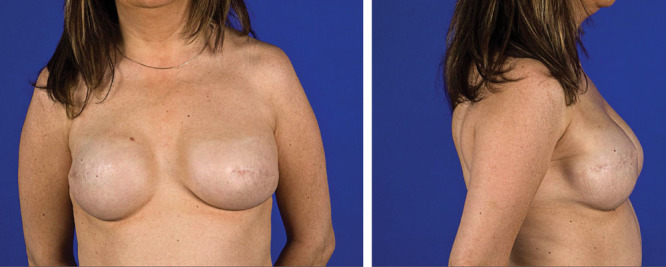
A 55-year-old female, 10 years post bilateral delayed breast reconstruction with Spectrum expander/implants.
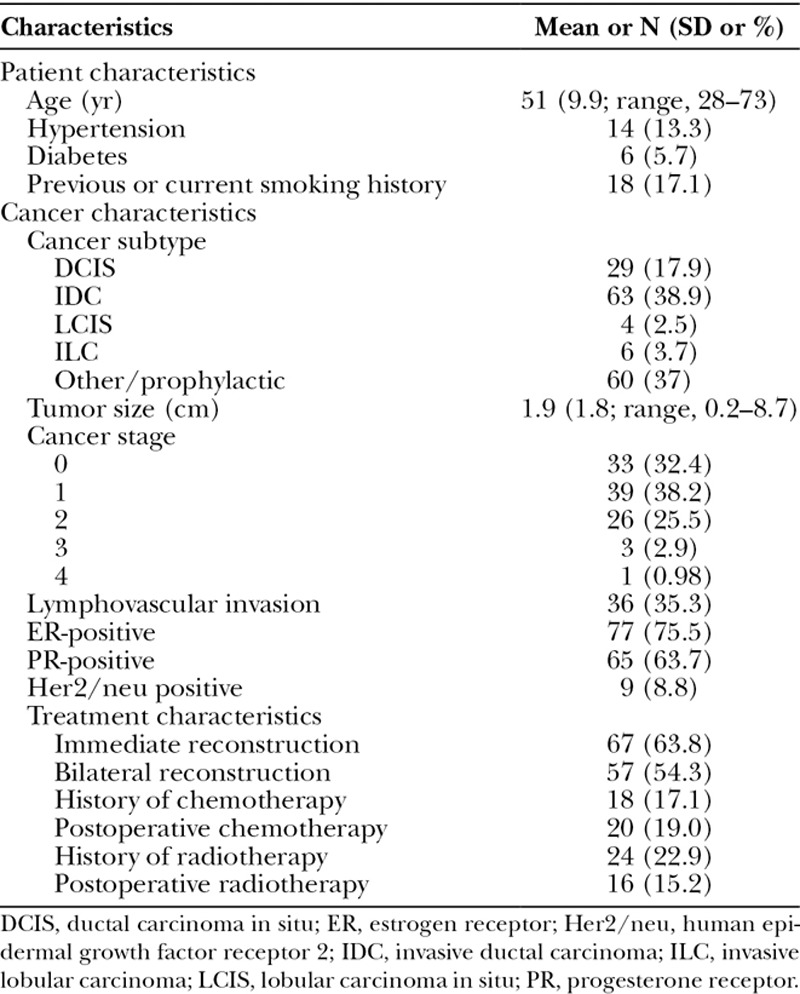
Table 1.
Patient Demographics
Video Graphic 1.

See video, Supplemental Digital Content 1, which displays the all-in-one adjustable expander/implant technique. This video is available in the “Related Videos” section of PRSGlobalOpen.com or at http://links.lww.com/PRSGO/A631.
RESULTS
Mean patient age was 51 years (SD, ±9.9; range, 28–73). Mean follow-up was 81.7 months (SD, ±39.2; range, 15–151). Ten patients were lost to follow-up and excluded. Five patients with congenital breast deformities were also excluded. A total of 162 implants in 105 patients were included in this study. Immediate reconstruction was performed in 63.8% of cases. Patient, cancer, and treatment characteristics are listed in Table 1. Complication rates were as follows: 0.62% extrusion, 1.2% partial mastectomy flap necrosis, 1.2% hematoma, 1.9% dehiscence, 2.5% seroma, 4.9% infection, and 15.4% deflation (Table 2). Five patients had capsular contracture requiring reoperation.
Table 2.
Primary Outcomes
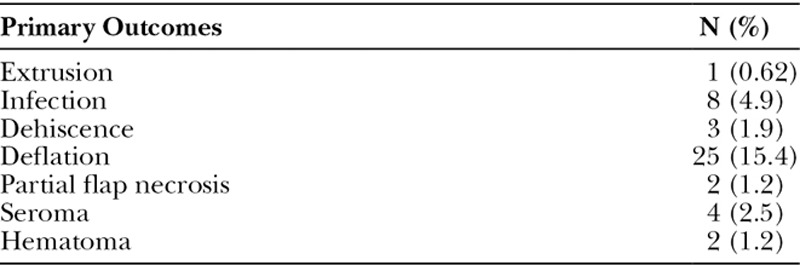
The following associations were identified by logistic regression: adjuvant radiotherapy and capsular contracture (P = 0.034), tumor size and deflation (P = 0014), and smoking history and infection (P = 0.013). Of the 162 implants, 31 (19.1%) were replaced for the following reasons: extrusion (1 patient), capsular contracture (5 patients), and deflation (25 patients). Overall, 81% of breasts were successfully reconstructed using a single stage with the expander/implant approach.
DISCUSSION
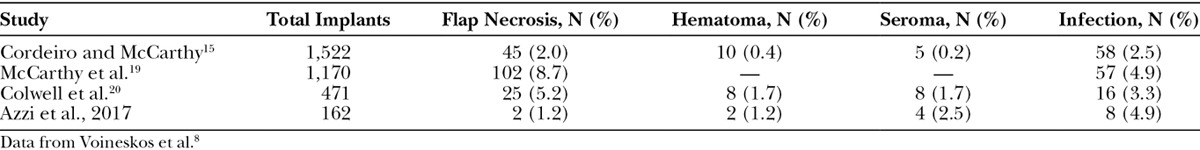
In 2015, a total of 77,219 procedures were performed by a 2-stage alloplastic approach (expander/implant), representing 73% of the overall reconstructive breast procedures in the United States.3 Single-stage reconstruction (implant alone) was performed 8,794 times, approximately 8% of the overall procedures, a new trend that has recently gained popularity. The complication rates of the 2 procedures were found comparable in a recent systematic review, 35% for single-stage reconstruction and 34% for 2-stage expander-implant reconstruction.7 Voineskos et al.8 performed a review of complication rates in expander/implant reconstruction. Their findings are compared with those in this study in Table 3. Hematoma, infection, and mastectomy flap necrosis rates using Spectrum all-in-one expander/implants are comparable with 2-stage reconstruction rates. However, with only 1 surgical procedure, the patient is subjected to anesthesia-related complications only once.
Table 3.
Comparison between 2-Stage Alloplastic Reconstruction Versus This Review’s All-in-One Expander/Implants
Capsular contracture rates in 2-stage alloplastic procedures vary significantly in the literature. Cordeiro et al.9 reported that 68% of irradiated patients developed capsular contracture, compared with 40% in the nonirradiated group (P = 0.025). Another study evaluated the long-term outcomes of 2-stage expander/implant reconstruction and postmastectomy radiation therapy.10 Over a period of 7 years, they reported that 17 patients (11.2%) underwent replacement of implant for grade 3 or 4 capsular contractures. Despite the advantage of performing capsulotomy/capsulectomy during expander/implant exchange in the 2-stage approach, our outcomes of capsular contracture are comparable with the reported rates in the literature. In our review, 3 of the 16 patients (18.8%) who underwent postmastectomy radiation required an exchange of implant due to capsular contracture.
Initially, when the implant first came to market, Mentor11 conducted a study on 416 patients and reported a deflation rate of 18.0% within 5 years of breast reconstruction using Spectrum, 26.9% within 7 years, and 33.2% within 10 years. Deflation was the most common reason for reoperation in our study. There were 25 (15.4%) deflated implants, all of which were replaced. Although our deflation rate is lower than the aforementioned study, it remains higher than the reported deflation rates of permanent implants in the literature. Long-term saline implant deflation rates range from 0.01% to 6.8% in the literature.12–15 Companies often report valves as frequent sites of implant failure. In our experience, most deflations occur shortly after the removal of the fill tube. Failure at the site of the self-sealing T-shaped valve tubing appeared to be at the origin of deflation. Before reviewing this series, the senior author contacted the company to inquire about a defect possibility after a few implants deflated immediately after valve removal. A specific technical information became available to us regarding the importance of the direction of extraction during the simple local procedure of valve removal. The angle of removal must be perpendicular to the inframammary crease in a straight vertical downward pull maneuver (video, Supplemental Digital Content 1). As a result of this new information, our deflation rates have drastically decreased in more recent years, which we hope to demonstrate in a follow-up study.
In a population-based study over a 25-year period consisting of 3,495 implants, the authors report a reoperation rate of 35.5% after breast reconstruction.12 They did not perform a subgroup analysis to compare the rates between single and two-stage alloplastic reconstruction. In a retrospective review of 582 breasts over an 8-year period, Susarla et al.16 found that 32.3% of patients required additional operative interventions after single-stage reconstruction. They also report additional operative interventions in 21.5% of patients who underwent 2-stage reconstruction. Some of the arguments against single-stage reconstruction are that a revision procedure is often required. Due to improved techniques, the use of acellular dermal matrix, and better patient selection, reoperation rates of single-stage alloplastic reconstruction has declined.4,5 In our experience, an attempt at avoiding a second surgery under general anesthesia is appealing to patients and their family, even with a high deflation rate. The additional benefit of postoperative adjustments renders the all-in-one expander/implant even more appealing to patients. Moreover, due to recent concerns of anaplastic large cell lymphoma, the option of a smooth surfaced expander/implant is also appealing to patients, a safe addition to the armamentarium of breast reconstruction.
The cost of bilateral implant-based reconstruction is an estimated $75,013 (USD), compared with $94,065 with bilateral DIEP reconstruction.17 In the event that a complication occurs, the total cost can be upward of $100,000 (USD). Spectrum implants were introduced at our institution by the senior author as part of a strategy aimed at more efficient use of limited OR resources, in the context of increasing breast reconstruction demand. Krishnan et al.7 performed a cost-utility analysis comparing direct-to-implant breast reconstruction relative to 2-stage reconstruction. Their comparative economic analysis compared the cost, outcomes, and quality of life for patients undergoing either method of reconstruction. The authors found a cost decrease of US$4,492.66 and a clinical benefit of 0.89 quality-adjusted life-year with the direct-to-implant approach, yielding a dominant incremental cost-utility ratio of US$5,047.93 Grover et al.18 also found that immediate implant placement was more cost-effective than expanders with implant exchange (2 stages), and patients had superior quality measure parameters.
We acknowledge that our results are subject to the forms of bias associated with retrospective reviews, such as inferring causality. Several confounding factors may affect the results such as variation in mastectomy approach, type, and incision. Mastectomies were not all performed by the same general surgeon, and procedures varied from total mastectomies to skin and nipple-sparing mastectomies. In addition, there has been evolution in radiation and chemotherapy in the past decade, including the type of drugs, dose of radiation, and timing of treatment. These variables could not be accounted for in this study but could potentially be confounding factors.
CONCLUSIONS
Overall, 81% of breasts in this series were successfully reconstructed in a single surgical procedure. Single-stage reconstruction using all-in-one adjustable expander/implants is cost effective, eliminates the necessity for a second procedure under general anesthesia, and can achieve results comparable with other alloplastic approaches reported in the literature.
Supplementary Material
Footnotes
We have received ethical approval by our institution’s ethics committee. We have followed the World Medical Association’s Declaration of Helsinki.
Presented at the Canadian Society of Plastic and Reconstructive Surgeons (CSPS) Annual Meeting, June 2016, Ottawa, ON; L’Association des Spécialistes en Chirurgie Plastique et Esthétique du Québec (ASCPEQ) annual meeting, February 2017, Montreal, QC; Fraser Gurd Surgical Research Forum, McGill University, May 2016, Montreal, QC; American Society of Plastic Surgeons (ASPS) Annual Meeting, October 2017, Orlando, FL.
Disclosure: The video was financed by Mentor. The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid by the authors.
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
REFERENCES
- 1.Canadian Cancer Society’s Advisory Committee on Cancer Statistics. Canadian Cancer Statistics 2016. 2016Toronto, ON: Canadian Cancer Society. [Google Scholar]
- 2.Albornoz CR, Bach PB, Mehrara BJ, et al. A paradigm shift in U.S. breast reconstruction: increasing implant rates. Plast Reconstr Surg. 2013;131:15–23.. [DOI] [PubMed] [Google Scholar]
- 3.American Society of Plastic Surgeons. Plastic surgery procedural statistics. Available at: http://www.plasticsurgery.org/news/plastic-surgery-statistics.html. Accessed October 14, 2016.
- 4.Cordeiro PG. Breast reconstruction after surgery for breast cancer. N Engl J Med. 2008;359:1590–1601.. [DOI] [PubMed] [Google Scholar]
- 5.Colwell AS, Damjanovic B, Zahedi B, et al. Retrospective review of 331 consecutive immediate single-stage implant reconstructions with acellular dermal matrix: indications, complications, trends, and costs. Plast Reconstr Surg. 2011;128:1170–1178.. [DOI] [PubMed] [Google Scholar]
- 6.Salzberg CA, Ashikari AY, Koch RM, et al. An 8-year experience of direct-to-implant immediate breast reconstruction using human acellular dermal matrix (AlloDerm). Plast Reconstr Surg. 2011;127:514–524.. [DOI] [PubMed] [Google Scholar]
- 7.Krishnan NM, Fischer JP, Basta MN, et al. Is single-stage prosthetic reconstruction cost effective? A cost-utility analysis for the use of direct-to-implant breast reconstruction relative to expander-implant reconstruction in postmastectomy patients. Plast Reconstr Surg. 2016;138:537–547.. [DOI] [PubMed] [Google Scholar]
- 8.Voineskos SH, Frank SG, Cordeiro PG. Breast reconstruction following conservative mastectomies: predictors of complications and outcomes. Gland Surg. 2015;4:484–496.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cordeiro PG, Pusic AL, Disa JJ, et al. Irradiation after immediate tissue expander/implant breast reconstruction: outcomes, complications, aesthetic results, and satisfaction among 156 patients. Plast Reconstr Surg. 2004;113:877–881.. [DOI] [PubMed] [Google Scholar]
- 10.Ho A, Cordeiro P, Disa J, et al. Long-term outcomes in breast cancer patients undergoing immediate 2-stage expander/implant reconstruction and postmastectomy radiation. Cancer. 2012;118:2552–2559.. [DOI] [PubMed] [Google Scholar]
- 11.Mentor: saline-filled and spectrum breast implants. Product data sheet. Available at: http://www.mentorwwllc.com/Documents/saline_spectrum_ppi.pdf. Accessed October 14, 2016.
- 12.Handel N, Cordray T, Gutierrez J, et al. A long-term study of outcomes, complications, and patient satisfaction with breast implants. Plast Reconstr Surg. 2006;117:757–767.; discussion 768. [DOI] [PubMed] [Google Scholar]
- 13.Levi B, Rademaker AW, Fine NA, et al. Comparison of breast implant deflation for mentor anterior and posterior valve designs in aesthetic and reconstructive patients. Plast Reconstr Surg. 2008;122:685–692.. [DOI] [PubMed] [Google Scholar]
- 14.Spear SL, Majidian A. Immediate breast reconstruction in two stages using textured, integrated-valve tissue expanders and breast implants: a retrospective review of 171 consecutive breast reconstructions from 1989 to 1996. Plast Reconstr Surg. 1998;101:53–63.. [DOI] [PubMed] [Google Scholar]
- 15.Cordeiro PG, McCarthy CM. A single surgeon’s 12-year experience with tissue expander/implant breast reconstruction: part I. A prospective analysis of early complications. Plast Reconstr Surg. 2006;118:825–831.. [DOI] [PubMed] [Google Scholar]
- 16.Susarla SM, Ganske I, Helliwell L, et al. Comparison of clinical outcomes and patient satisfaction in immediate single-stage versus two-stage implant-based breast reconstruction. Plast Reconstr Surg. 2015;135:1e–8e.. [DOI] [PubMed] [Google Scholar]
- 17.Matros E, Albornoz CR, Razdan SN, et al. Cost-effectiveness analysis of implants versus autologous perforator flaps using the BREAST-Q. Plast Reconstr Surg. 2015;135:937–946.. [DOI] [PubMed] [Google Scholar]
- 18.Grover R, Padula WV, Van Vliet M, et al. Comparing five alternative methods of breast reconstruction surgery: a cost-effectiveness analysis. Plast Reconstr Surg. 2013;132:709e–723e.. [DOI] [PubMed] [Google Scholar]
- 19.McCarthy CM, Mehrara BJ, Riedel E, et al. Predicting complications following expander/implant breast reconstruction: an outcomes analysis based on preoperative clinical risk. Plast Reconstr Surg. 2008;121:1886–1892.. [DOI] [PubMed] [Google Scholar]
- 20.Colwell AS, Tessler O, Lin AM, et al. Breast reconstruction following nipple-sparing mastectomy: predictors of complications, reconstruction outcomes, and 5-year trends. Plast Reconstr Surg. 2014;133:496–506.. [DOI] [PubMed] [Google Scholar]


