Summary:
Natural and synthetic fillers have revolutionized aesthetic facial rejuvenation and soft-tissue augmentation. We present a case highlighting the dangers of filler self-injection. A 37-year-old woman self-injected a dermal filler around both temples. She immediately experienced left--side hearing loss, blanching over the left face, and pain. Prompt treatment with hyaluronidase, topical nitro paste, and warm compresses ensued. An emergency computed tomography angiogram showed occlusion of a superficial temporal artery branch. We treated her with enoxaparin, aspirin, dexamethasone, piperacillin-tazobactam, and intradermal lidocaine. After 6 hyperbaric oxygen therapy (HBO2) treatments in 3 days, the patient showed improvement in appearance with markedly decreased ischemic discoloration and her hearing returned to baseline. Algorithms for treating such injuries generally neglect HBO2. HBO2 is thought to be efficacious in these situations by a variety of mechanisms: oxygenation of ischemic tissues, reduction of edema, amelioration of ischemic/reperfusion injury, promotion of angiogenesis and collagen maturation. Her resolved hearing highlights the utility of HBO2 in sudden hearing loss as well. Injectors should have guidelines for using product, not only on patients but staff as well. Filler courses should include handling complications and include HBO2 in their guidelines. Clinicians should remind patients to seek treatment from qualified clinicians. The goal of a bargain price using self-injection may quickly become expensive and disfiguring.
INTRODUCTION
Natural and synthetic fillers have revolutionized aesthetic facial rejuvenation and soft-tissue augmentation to treat volume loss, dermatological diseases, age-related changes such as tear troughs, wrinkles, depressed scars, and also for lip, cheek, and chin augmentation.1 We present the case of a patient who self-injected with a hyaluronic acid filler and required intervention for complications including hyperbaric oxygen therapy (HBO2). We will discuss the utility of HBO2 and the ease of obtaining product, and the need for regulations and self-governance.
CASE
A 37-year-old woman self-injected Juvederm Voluma XC (a hyaluronic acid gel, Allergan, Irvine, CA) on both sides of her face around the proximal temple. Immediately after injection, she experienced hearing loss in her left ear, blanching over the left side of her face, and severe pain. Prompt treatment with hyaluronidase, topical nitro paste, and warm compresses ensued. With no improvement 9 hours after the injection, she presented to an outside emergency department with signs of ischemic changes to her left face and postauricular area and also hearing loss but no other vestibular symptoms. A computed tomography angiography of the head showed occlusion of a branch of the left superficial temporal artery. They treated her with enoxaparin, aspirin, dexamethasone 10 mg IV, piperacillin/tazobactam, and intradermal 1% lidocaine (0.1 ml per site). Our facility accepted her in transfer for hyperbaric oxygen treatments for vascular insufficiency. Beginning 15 hours after the initial insult, she received 6 total treatments, done twice daily, the initial 2 at 3.0 atmospheres absolute for 90 minutes followed by 4 treatments at 2.4 ATA × 90 minutes, all with air breaks every 30 minutes. After 3 days, the patient showed improvement in appearance with markedly decreased ischemic discoloration and her hearing returned to baseline (subjectively, audiograms were not performed). She chose to follow-up with her personal dermatologist in her hometown. She reports that she developed increased erythema over the next few days after discharge, prompting treatment with platelet-rich plasma. She notes good resolution thereafter. By 4 months after treatment, she had an acceptable cosmetic outcome, and 1 year later, she reports that the residual is unnoticeable except by herself. Unfortunately, the patient was unwilling to share photographs or other details that would have further illustrated the case and issues at hand (but did send photographs to supplement her 4- and 12-month self-assessments; Fig. 1).
Fig. 1.
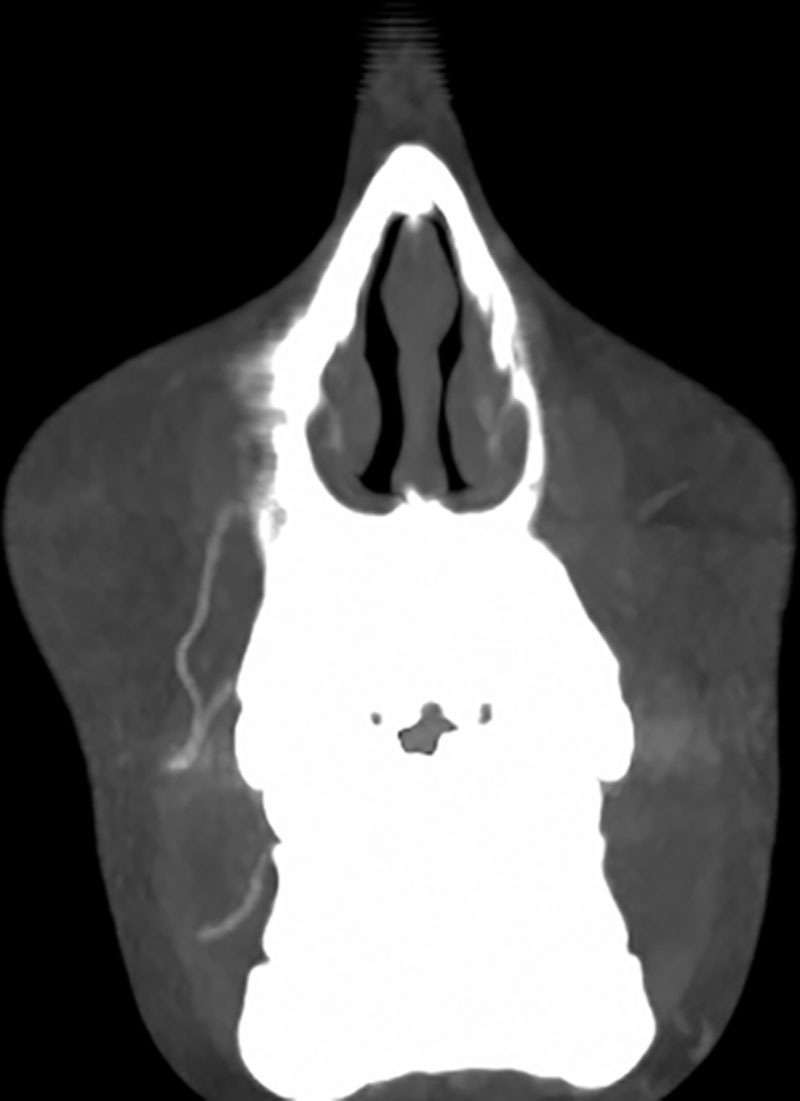
Computed tomography angiogram (maximum intensity projection) demonstrating loss of left temporal artery branches.
The patient did not give us permission to use her photos or identifying information. We have complied with this wish and in all other ways are in compliance with the Declaration of Helsinki.
DISCUSSION
Acute peripheral arterial ischemia is an indication for prompt HBO2 promulgated by multiple medical societies involved in hyperbaric medicine and accepted by the Centers for Medicare & Medicaid Services and numerous third-party payors. However, only a few reported cases exist similar to ours raising the question of efficacy in this specific scenario.2,3 Algorithms for treating such injection injuries generally do not include HBO2.4,5 Hyperbaric oxygen is thought to be an efficacious adjunct in these situations by a variety of mechanisms including oxygenation of ischemic tissues, reduction of edema, amelioration of ischemic/reperfusion injury, and promotion of angiogenesis and collagen maturation.6 A comprehensive treatment approach may include hyaluronidase (if a hyaluronic acid filler), topical nitroglycerin paste, warm compresses, steroids, aspirin or low molecular weight heparin, phosphodiesterase inhibitor, HBO2, consideration of prophylactic antibiotic and antiviral therapy, and plastic surgery, ophthalmology, and neurology consultation.7
Not having performed an audiology examination, the etiology of her hearing loss remains unclear. An embolism is unlikely given the cochlea’s basilar supply. We conjecture that the injection effected the tympanic and deep auricular arteries coming off the external carotid next to superficial temporal artery. These supply the middle ear and the tympanic membrane. It is conceivable that ischemia there caused stiffness in the tympanum resulting in conductive, rather than sensorineural, hearing loss.
This case highlights the use of HBO2 for both peripheral arterial ischemia and also for sudden hearing loss.8 Both of these problems resolved well with the emergent application of HBO2 although other interventions including “tincture of time” were at play as well.
This case also highlights the dangers of the rising trend of filler self-injection. Although few cases exist in the literature, this is likely due to under reporting.
Many patients are able to obtain fillers from unregulated sources online and internationally. This coupled with the wide availability of online videos and diagrams, illustrating injection techniques by qualified clinicians and unqualified laypersons make it easy for patients to acquire and attempt self-injection of fillers.9
How do we combat the rising trend of patients self-injecting products such as fillers? Some have suggested an injunction on all websites selling do-it-yourself fillers and showing self-injection techniques. Others encourage tighter governmental regulations. Offices should have guidelines for injectors using product on not only patients but also other staff and themselves. Filler courses should include thorough instructions on handling complications.
SUMMARY
Providers should know their limits and when to seek assistance from other clinicians.10 A comprehensive treatment algorithm, including HBO2 and hyaluronidase, should be in place. Clinicians should educate their patients and thoroughly explain the risks during patient consultations. Clinicians should also remind patients to seek treatment from a well-trained, qualified clinician. The goal of a bargain price using self-injection can become quickly expensive, dangerous, and disfiguring in the event of a complication.
Footnotes
Abstract presented as poster at Undersea and Hyperbaric Medicine Society, Annual Scientific Meeting 2017, Naples, FL.
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the Department of Emergency Medicine, University of Nebraska Medical Center, Omaha, Neb.
REFERENCES
- 1.Ballin AC, Brandt FS, Cazzaniga A. Dermal fillers: an update. Am J Clin Dermatol. 2015;16:271–283.. [DOI] [PubMed] [Google Scholar]
- 2.Adir Y, Halpern P, Nachum Z, et al. Hyperbaric oxygen therapy for ischaemia of the hand due to intra-arterial injection of methadone and flunitrazepam. Eur J Vasc Surg. 1991;5:677–679.. [DOI] [PubMed] [Google Scholar]
- 3.Darling MD, Peterson JD, Fabi SG. Impending necrosis after injection of hyaluronic acid and calcium hydroxylapatite fillers: report of 2 cases treated with hyperbaric oxygen therapy. Dermatol Surg. 2014;40:1049–1052.. [DOI] [PubMed] [Google Scholar]
- 4.Glaich A, Cohen J, Goldberg L. Injection necrosis of the glabella: protocol for prevention and treatment after use of dermal fillers. Dermatol Surg. 2006;32:276–281.. [DOI] [PubMed] [Google Scholar]
- 5.Hirsch RJ, Cohen JL, Carruthers J. Successful management of an unusual presentation of impending necrosis following a hyaluronic acid injection embolus and a proposed algorithm for management with hyaluronidase. Dermatol Surg. 2007;33:357–360.. [DOI] [PubMed] [Google Scholar]
- 6.Thom SR. Hyperbaric oxygen: its mechanisms and efficacy. Plast Reconstr Surg. 2011;127 Suppl 1:131S–141S.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dominguez S, Moshrefi S, Dobke M. Treatment protocol for acute arterial occlusion secondary to facial revolumization procedures. Emerg Med. 2017;49:221–229.. [Google Scholar]
- 8.Bennett M, Kertesz T, Perleth M, et al. Hyperbaric oxygen for idiopathic sudden sensorineural hearing loss and tinnitus. Cochrane Database Syst Rev. 2012;10:CD004739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ono S, Hyakusoku H. Complications after self-injection of hyaluronic acid and phosphatidylcholine for aesthetic purposes. Aesthet Surg J. 2010;30:442–445.. [DOI] [PubMed] [Google Scholar]
- 10.Funt D, Pavicic T. Dermal fillers in aesthetics: an overview of adverse events and treatment approaches. Clin Cosmet Investig Dermatol. 2013;6:295–316.. [DOI] [PMC free article] [PubMed] [Google Scholar]


