Supplemental Digital Content is available in the text.
Summary:
Most cases of severely contracted nose require revision rhinoplasty and septoplasty, wherein preoperative and/or intraoperative expansion of nasal soft tissue is necessary for tension-free revision surgery. The present study aimed to evaluate the efficacy and safety of pre- and postoperative adjuvant therapy using polydeoxyribonucleotide (PDRN) and invasive, pulsed-type, bipolar, alternating current radiofrequency (RF) for revision surgery of a contracted nose. In total, 30 patients were treated with 16 sessions (8 preoperative sessions and 8 postoperative sessions) of intralesional injection of PDRN and invasive RF treatment using microneedle electrodes at 1-week intervals. One week after the final combined pretreatment using PDRN and invasive bipolar RF, the skin of contracted noses was sufficiently softened, and nasal skin mobility was notably improved in all the patients. During revision rhinoplasty and septoplasty, the contracted nasal skin in each patient was adequately released for proper covering of the nasal tip without tension. Postoperatively, 8 sessions of adjuvant therapy elicited marked clinical improvements in persistent nasal tip dimpling and contracture, septal deviation, and warping from the incomplete recovery of nasal contracture after revision surgery. In conclusion, our pre- and postoperative adjuvant therapies using PDRN and invasive bipolar RF remarkably improved the therapeutic outcomes of revision rhinoplasty and septoplasty for contracted skin of the nose without major side effects.
INTRODUCTION
Many cases of severely contracted nose result from regional infections on and around nasal implants, including silicone products.1 Subsequent inflammatory reactions and excessive fibrosis can elicit the formation of extensive scar tissue over the dermis and subcutaneous fat layers, with or without distorting the underlying nasal cartilage framework.1 Most patients with contracted nose require revision rhinoplasty and septoplasty, for which preoperative and/or intraoperative expansion of nasal soft tissue is necessary.1–6 Scar tissue formed along the nose, however, limits the expansion of nasal tissue needed for tension-free revision surgery. In the present report, we describe the use of polydeoxyribonucleotide (PDRN) injections in combination with invasive bipolar radiofrequency (RF) treatment to soften nasal skin and improve skin mobility for improved outcomes in revision rhinoplasty and septoplasty.
PATIENTS AND METHODS
Thirty Korean patients (12 males and 18 females with a mean age of 37.7 years, ranging from 23 to 62 years) with contracted nose agreed to undergo adjuvant therapy for revision rhinoplasty and septoplasty using PDRN and invasive, pulsed-type, bipolar, alternating current RF treatment. After obtaining written informed consent, the patients were treated with 16 sessions (8 preoperative sessions and 8 postoperative sessions) of intralesional PDRN (Polydien; Han Wha Pharma Co., Ltd., Seoul, Korea) injection and invasive RF treatment using microneedle electrodes (SYLFIRM; Viol, Kyunggi, Korea) at 1-week intervals. The skin along the nose was first cleansed with 70% ethanol, after which PDRN was injected into the contracted nose at 3 points at a total amount of 0.3 mL using a 31-gauge, 1-mL insulin syringe. Then, invasive RF treatment was delivered at a power level of 3 and a microneedle penetration depth of 1.5 mm over 2–3 passes. All shots were delivered after firmly pressing the disposable tip on the skin for the precise penetration of microneedle electrodes into the target area. Immediately after combined treatment, the treatment area was cooled with icepacks without prophylactic systemic or topical antibiotics and corticosteroids.
At 1 week after the final session of pretreatment, revision rhinoplasty and septoplasty were performed in all 30 patients. Briefly, the nasal skin was separated from the cartilage via an open rhinoplasty incision method and widely dissected through the surgical plane below the softened capsule. For effective septal extension from an insufficient tip projection and septal cartilage, rib cartilage, which was harvested from the eighth or ninth rib, was grafted as a columellar strut. The harvested rib cartilage was sculpted, according to the size of the expected tip projection, and fixed to the septal base. Then, the lower lateral cartilages were sutured to the columellar strut after caudal and upward mobilization. Any side effects of revision surgery and pre- and postoperative adjuvant therapies were evaluated during the follow-up period after revision surgery of more than 18 months.
RESULTS
One week after combined pretreatment using PDRN and invasive bipolar RF, the skin of contracted noses was remarkably softened, and nasal skin mobility was notably improved in all patients. Among the 30 patients, 18 patients (60%) exhibited marked to complete resolution of nasal tip dimpling and contracture 1 week after completing the 8 sessions of pretreatment. Meanwhile, 12 patients (40%) presented mild-to-moderate clinical improvement in nasal tip dimpling and contracture.
Thereby, all the 30 patients were able to undergo revision rhinoplasty and septoplasty as the contracted nasal skin in each patient was adequately released for sufficient covering of the nasal tip without tension. Dorsal augmentation of the contracted noses was performed using dermal fat graft in 22 patients (73.3%) and carved rib cartilage in 8 patients (26.7%). One week after the revision surgery, 8 sessions of postoperative adjuvant therapy were delivered using PDRN and invasive bipolar RF at 1-week intervals. During the follow-up period after the revision surgery of over 18 months, we noted persistent nasal tip dimpling and contracture in 6 patients (20%), prolonged erythema or dyspigmentation in 3 patients (10%), wound infection in 3 patients (10%), nasal tip absorption in 2 patients (6.7%), septal deviation in 2 patients (6.7%), and warping in 1 patient (3.3%). Nonetheless, most of the cases with persisted nasal tip dimpling and contracture, septal deviation, and warping resulting from incomplete recovery of the nasal contracture were further improved or resolved with postoperative adjuvant therapy [Figs. 1, 2; see figure, Supplementary Digital Content 1, which displays a contracted nose in a 62-year-old female patient. Clinical photographs (a and c) at baseline and (b and d) at 18 months after revision surgery with 8 sessions of preoperative and 8 sessions of postoperative adjuvant therapy using PDRN and invasive, pulsed-type, bipolar, alternating current RF, http://links.lww.com/PRSGO/A653; see figure, Supplementary Digital Content 2, which displays contracted nose in a 52-year-old female patient. Clinical photographs (a and c) at baseline and (b and d) at 18 months after revision surgery with 8 sessions of preoperative and 8 sessions of postoperative adjuvant therapy using PDRN and invasive bipolar RF, http://links.lww.com/PRSGO/A654; see figure, Supplementary Digital Content 3, which displays a contracted nose in a 31-year-old female patient. Clinical photographs (a and c) at baseline and (b and d) at 7 months after revision surgery with 8 sessions of preoperative and 8 sessions of postoperative adjuvant therapy using PDRN and invasive bipolar RF, http://links.lww.com/PRSGO/A655; see figure, Supplementary Digital Content 4, which displays a contracted nose in a 56-year-old male patient. Clinical photographs (a and c) at baseline and (b and d) at 7 months after revision surgery with 8 sessions of preoperative and 8 sessions of postoperative adjuvant therapy using PDRN and invasive bipolar RF, http://links.lww.com/PRSGO/A656; see figure, Supplementary Digital Content 5, which displays a contracted nose in a 25-year-old male patient. Clinical photographs (a and c) at baseline and (b and d) at 7 months after revision surgery with 8 sessions of preoperative and 8 sessions of postoperative adjuvant therapy using PDRN and invasive bipolar RF, http://links.lww.com/PRSGO/A657].
Fig. 1.
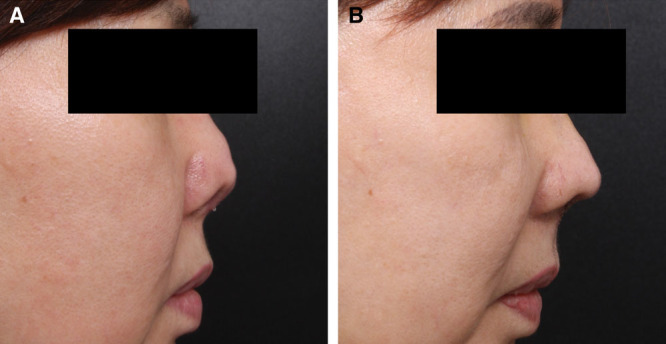
Contracted nose in a 62-year-old female patient. Clinical photographs at baseline (A) and at 18 months after revision surgery (B) with 8 sessions of preoperative and 8 sessions of postoperative adjuvant therapy using PDRN and invasive, pulsed-type, bipolar, alternating current RF.
Fig. 2.
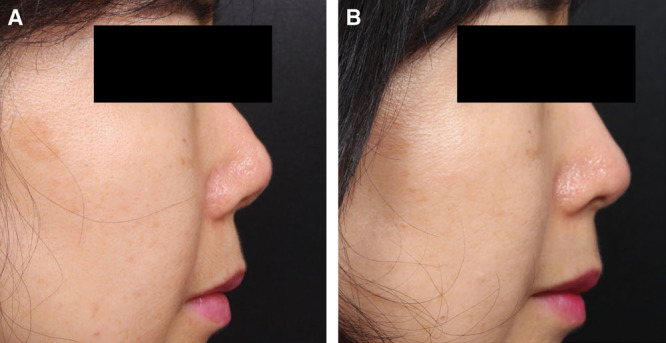
Contracted nose in a 52-year-old female patient. Clinical photographs at baseline (A) and at 18 months after revision surgery (B) with 8 sessions of preoperative and 8 sessions of postoperative adjuvant therapy using PDRN and invasive bipolar RF.
During the course of pre- and postoperative adjuvant therapies, no remarkable side effects, including excessive oozing or bleeding; secondary infection; prolonged posttherapy erythema or dyschromia; or worsening of the contracture or scarring, were reported. As well, pain during the combined treatment was transient and well tolerated. Most of the patients were very satisfied or satisfied with the postoperative results, and none reported cosmetic dissatisfaction.
DISCUSSION
Invasive bipolar AC RF devices deliver high-frequency energy via penetrating microneedle electrodes.7 Continuous delivery thereof generates a larger area of tissue coagulation over time, which appears from the tips of individual microneedles.7 Thereby, invasive bipolar RF technology has been used for treating atrophic scars, inflammatory acne lesions, wrinkles, and skin laxity by inducing wound repair and neocollagenesis.7,8 In the present study, a pulsed-type, invasive bipolar AC RF device was utilized to deliver gated RF oscillations. Our data demonstrated that the pre- and postoperative adjuvant treatment therewith at the microneedle penetration depth of 1.5 mm in combination with PDRN injections effectively softened contracted nasal skin, providing greater mobility, and improved postoperative outcomes. We suggest that the gating of RF oscillations could have reduced the risk of excessive thermal coagulation and further tissue scarring in the contracted nasal skin of our patients.
PDRN activates the adenosine A2A receptor that stimulates fibroblast differentiation and maturation and the release of vascular endothelial cell growth factor for neovascularization.9,10 Thereby, PDRN treatment has been found to effectively enhance the survival of skin flaps, promote hair restoration, and promote wound repair without significant side effects.9–11 In this study, PDRN was injected into the contracted nose at a dose of 0.3 mL/session at 1-week intervals, followed by invasive bipolar RF treatments. We noted that PDRN-induced angiogenesis and invasive bipolar RF-induced wound repair seemed to remarkably soften the contracted skin and improve skin mobility. Furthermore, the repetitive generation of tissue wounding with minimal thermal coagulation by pulsed-type RF significantly maximized the utilization of PDRN in the contracted nasal skin. In our experience, preoperative adjuvant therapy noticeably shortens the preparatory period for revision surgery, and postoperative adjuvant therapy prevents further tissue contracture by the revision surgery.
In conclusion, our pre- and postoperative adjuvant treatments using PDRN and invasive bipolar RF remarkably improved the therapeutic outcomes of revision rhinoplasty and septoplasty for contracted skin of the nose without major side effects. Nevertheless, further prospective, controlled investigations are required to confirm our findings and optimize the pre- and postrevision surgery adjuvant therapies in patients with severely contracted nose for better postoperative results.
ACKNOWLEDGMENTS
The authors thank Anthony Thomas Milliken, ELS (Editing Synthase, Seoul, Korea) for his help with the editing of this article.
Supplementary Material
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
REFERENCES
- 1.Oh YH, Seo JW, Oh SJ, et al. Correction of severely contracted nose. Plast Reconstr Surg. 2016;138:571–582.. [DOI] [PubMed] [Google Scholar]
- 2.Park JH, Jin HR. Use of autologous costal cartilage in Asian rhinoplasty. Plast Reconstr Surg. 2012;130:1338–1348.. [DOI] [PubMed] [Google Scholar]
- 3.Jung DH, Moon HJ, Choi SH, et al. Secondary rhinoplasty of the Asian nose: correction of the contracted nose. Aesthetic Plast Surg. 2004;28:1–7.. [DOI] [PubMed] [Google Scholar]
- 4.Kridel RW, Ashoori F, Liu ES, et al. Long-term use and follow-up of irradiated homologous costal cartilage grafts in the nose. Arch Facial Plast Surg. 2009;11:378–394.. [DOI] [PubMed] [Google Scholar]
- 5.Kim SK, Kim HS. Secondary Asian rhinoplasty: lengthening the short nose. Aesthet Surg J. 2013;33:353–362.. [DOI] [PubMed] [Google Scholar]
- 6.Suh MK, Ahn ES, Kim HR, et al. A 2-year follow-up of irradiated homologous costal cartilage used as a septal extension graft for the correction of contracted nose in Asians. Ann Plast Surg. 2013;71:45–49.. [DOI] [PubMed] [Google Scholar]
- 7.Na J, Zheng Z, Dannaker C, et al. Electromagnetic initiation and propagation of bipolar radiofrequency tissue reactions via invasive non-insulated microneedle electrodes. Sci Rep. 2015;5:16735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Taheri A, Mansoori P, Sandoval LF, et al. Electrosurgery: part II. Technology, applications, and safety of electrosurgical devices. J Am Acad Dermatol. 2014;70:607.e1–12.; quiz 619. [DOI] [PubMed] [Google Scholar]
- 9.Chung KI, Kim HK, Kim WS, et al. The effects of polydeoxyribonucleotide on the survival of random pattern skin flaps in rats. Arch Plast Surg. 2013;40:181–186.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Galeano M, Bitto A, Altavilla D, et al. Polydeoxyribonucleotide stimulates angiogenesis and wound healing in the genetically diabetic mouse. Wound Repair Regen. 2008;16:208–217.. [DOI] [PubMed] [Google Scholar]
- 11.Lee SH, Zheng Z, Kang JS, et al. Therapeutic efficacy of autologous platelet-rich plasma and polydeoxyribonucleotide on female pattern hair loss. Wound Repair Regen. 2015;23:30–36.. [DOI] [PubMed] [Google Scholar]


