Summary:
Infection of the temporomandibular joint (TMJ) is a rare pediatric condition resulting from the introduction of pathogens into the joint by hematogenous seeding, local extension, or trauma. Early recognition of the typical signs and symptoms including fever, trismus, preauricular swelling, and TMJ region tenderness are critical in order to initiate further evaluation and prevent feared complications of fibrosis, ankylosis, abnormal facial structure, or persistence of symptoms. Contrast-enhanced computed tomography with ancillary laboratory analysis including erythrocyte sedimentation rate, C-reactive protein, and white blood cell count are beneficial in confirming the suspected diagnosis and monitoring response to therapy. Initial intervention should include empiric parenteral antibiotics, early mandibular mobilization, and joint decompression to provide synovial fluid for analysis including cultures. This report describes a case of TMJ bacterial arthritis in a healthy 6-year-old male who was promptly treated nonsurgically with intravenous antibiotics and localized needle joint decompression with return to normal function after completion of oral antibiotics and physical therapy.
CASE REPORT
A 6-year-old healthy male with 3 days of fever, right-sided facial swelling, and trismus, presented as a transfer after outside hospital computed tomography (CT) demonstrated a 16 × 16 × 10 mm rim-enhancing collection consistent with an intraarticular right TMJ abscess and adjacent parotitis, temporalis myositis, and cellulitis (Fig. 1). Outside hospital records indicated the patient initially presented with a temperature of 102.4°F and neutrophilic leukocytosis (18,000/mm3). The patient had blood cultures drawn before transfer, which were serially followed and consistently negative until final culture confirmed no growth at 5 days. On initial consultation, physical examination was significant for right facial swelling, tenderness to palpation of right preauricular and temporal regions, and decreased maximal incisal opening (MIO) of 15 mm restricted by pain. Laboratory values showed C-reactive protein (CRP) of 4.2 mg/L and erythrocyte sedimentation rate (ESR) of 1 mm/h. After initiation of empiric intravenous antibiotics (clindamycin 10 mg/kg 3 times daily), ultrasound-guided needle aspiration under general anesthesia returned 2 milliliters of purulent fluid. MIO improved to 22 mm following aspiration, and the patient immediately started range of motion (ROM) mandibular exercises. After aspirate culture grew Streptococcus pyogenes, antibiotics were changed to parenteral ampicillin (200 mg/ kg / daily divided into 4 doses). Following a 4-day hospitalization, the patient was discharged with a 14-day course of oral amoxicillin (85 mg/kg/daily) and instructions to continue ROM exercises. At discharge, MIO was 30 mm. At 13-day follow-up, the patient reported tenderness at the right TMJ, with painless MIO of 32 mm. Mandibular radiographs showed symmetric, normal appearing condyles bilaterally. Due to persistent tenderness of the right TMJ and elevated ESR of 45 mm/h, amoxicillin was extended for another 14 days despite a decreased CRP of 0.7 mg/L. At 5-week follow-up, the patient had no abnormal physical examination findings and MIO increased to 39 mm. At 12-week follow-up, the patient reported no symptoms with MIO of 40 mm.
Fig. 1.
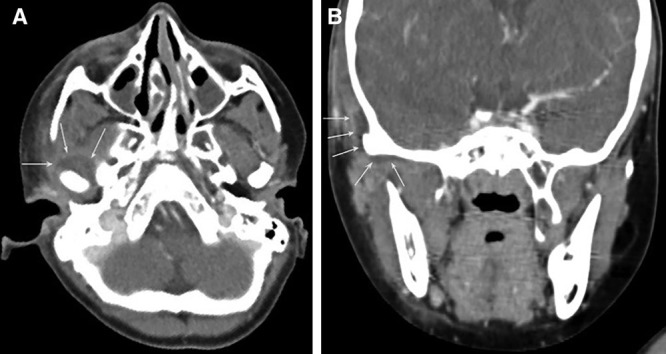
Axial (A) and coronal (B) CT images: arrows demonstrate low-density rim-enhancing collection arising from right TMJ extending anteriorly from the mandibular condyle into the masticator space along the deep surface of the temporalis.
DISCUSSION
TMJ infectious arthritis is caused by hematogenous seeding or direct contiguous spread of pathogens into the joint.1,2 Early diagnosis and treatment are critical to prevent complications including destruction of synovium, fibrotic adhesions, bony ankylosis, or osteomyelitis.3,4 In pediatric patients, an additional feared complication includes injury to the growth plate located under the fibrocartilage covering the condylar head, which may result in deficient mandibular growth and potential permanent facial asymmetry.5–7 Characteristic signs and symptoms of TMJ infectious arthritis include fever, trismus, preauricular swelling, and TMJ region tenderness, all present in this case.8 The similarity in physical examination findings to other pediatric disorders involving the TMJ, such as juvenile rheumatoid arthritis, trauma-related injury, or dental malocclusion–related joint derangement, makes diagnosis challenging without laboratory and radiographic studies.9–11
Contrast-enhanced CT is the superior imaging method in the assessment of the TMJ.12,13 Alternatively, cone-beam CT provides a similar evaluation while delivering less radiation.14 CT allows visualization of inflamed soft tissues and increased intracapsular fluid while also permitting evaluation of adjacent structures to determine the presence of concomitant myositis or osteomyelitis.8,12 If initial CT imaging is negative and clinical suspicion remains high, magnetic resonance imaging should be performed.15
Although typical laboratory values such as WBC, ESR, and CRP are helpful, they lack specificity and sensitivity to make a diagnosis without clinical signs and synovial fluid analysis.16 CRP levels are helpful in determining the resolution of infection after aspiration and antibiotic therapy.17,18 In this case, the CRP level was initially 4.2 mg/L, and diagnosis was made based on history, physical, and imaging.
There is insufficient evidence to support a definitive algorithm for the surgical management of pediatric TMJ septic arthritis, initial interventions described have included aspiration only, aspiration with arthroscopic joint lavage, or arthrotomy.19,20 In general, initial intervention for any infected joint should include antibiotics, joint decompression with fluid analysis, and early mobilization.18 Antibiotics should be started urgently, then tailored based on synovial fluid cultures.16,18 Causative organisms in TMJ septic arthritis include Staphylococcus aureus, Streptococcus species, Pseudomonas aeruginosa, E. coli, Neisseria, and Haemophilus influenza.21–23 Aspiration of intrasynovial fluid is essential for decompression, elimination of inflammatory contents, and to facilitate synovial fluid analysis to guide antibiotic therapy.24 Additional options of arthroscopy and arthrotomy allow direct joint visualization and additional lavage, lysis of adhesions, or debridement.19,24 A randomized, multicenter prospective trial including 130 children with culture-positive bacterial arthritis showed that a combination of antibiotics and a single aspiration are sufficient for treatment if physical examination improves and CRP normalizes; however, no case involved the TMJ.25
No specific data exists supporting the initiation, duration, or type of physiotherapy, but other reviews of TMJ septic arthritis advocate early mandibular ROM exercises.10,26 Similar to closed treatment of pediatric condylar fractures, early initiation of mandibular ROM exercises are recommended to improve condyle excursion and prevent fibrotic adhesions.27 In this case, active opening and bite exercises helped improve MIO to 40 mm (normal for age group) by 12-weeks follow-up.28
CONCLUSIONS
TMJ septic arthritis is uncommon but potentially devastating in the pediatric population. Often presenting with generalized symptoms, it may be confused with other TMJ disorders. Infectious arthritis of the TMJ should be considered in a patient presenting with fever, preauricular swelling, and impaired TMJ function such as decreased maximal incisal opening. Physical examination, contrast-enhanced CT, and laboratory analysis should determine the need for diagnostic and potentially therapeutic TMJ arthrocentesis and joint decompression. Although no gold standard exists for management, one can maximize patient outcomes by recognizing clinical and radiologic findings to initiate early joint decompression with synovial fluid analysis, antibiotic therapy, and joint mobilization with monitoring of maximal incisal opening.
Footnotes
The article was created in accordance without violation of ethical standards.
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Yang SW, Cho JY, Kim HM. Septic arthritis of the temporomandibular joint: a case report. J Korean Assoc Oral Maxillofac Surg. 2016;42:227–230.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Klüppel LE, Bernabé FB, Primo BT, et al. Septic arthritis of the temporomandibular joint. J Craniofac Surg. 2012;23:1752–1754.. [DOI] [PubMed] [Google Scholar]
- 3.Yew CC, Rahman SA, Alam MK. Temporomandibular joint ankylosis in a child: an unusual case with delayed surgical intervention. BMC Pediatr. 2015;15:169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Amos MJ, Patterson AR, Worrall SF. Septic arthritis of the temporomandibular joint in a 6-year-old child. Br J Oral Maxillofac Surg. 2008;46:242–243.. [DOI] [PubMed] [Google Scholar]
- 5.Allori AC, Chang CC, Fariña R, et al. Current concepts in pediatric temporomandibular joint disorders: Part 1. Etiology, epidemiology, and classification. Plast Reconstr Surg. 2010;126:1263–1275.. [DOI] [PubMed] [Google Scholar]
- 6.Ringold S, Cron RQ. The temporomandibular joint in juvenile idiopathic arthritis: frequently used and frequently arthritic. Pediatr Rheumatol Online J. 2009;7:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wadhwa S, Kapila S. TMJ disorders: future innovations in diagnostics and therapeutics. J Dent Educ. 2008;72:930–947.. [PMC free article] [PubMed] [Google Scholar]
- 8.Cai XY, Yang C, Zhang ZY, et al. Septic arthritis of the temporomandibular joint: a retrospective review of 40 cases. J Oral Maxillofac Surg. 2010;68:731–738.. [DOI] [PubMed] [Google Scholar]
- 9.Hammoudi K, Manceau A, Cazeneuve N, et al. [Childhood septic temporomandibular arthritis]. Ann Otolaryngol Chir Cervicofac. 2009;126:18–21.. [DOI] [PubMed] [Google Scholar]
- 10.Gayle EA, Young SM, McKenna SJ, et al. Septic arthritis of the temporomandibular joint: case reports and review of the literature. J Emerg Med. 2013;45:674–678.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Niibo P, Pruunsild C, Voog-Oras Ü, et al. Contemporary management of TMJ involvement in JIA patients and its orofacial consequences. EPMA J. 2016;7:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Larheim TA, Abrahamsson AK, Kristensen M, et al. Temporomandibular joint diagnostics using CBCT. Dentomaxillofac Radiol. 2015;44:20140235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Morales H, Cornelius R. Imaging approach to temporomandibular joint disorders. Clin Neuroradiol. 2016;26:5–22.. [DOI] [PubMed] [Google Scholar]
- 14.Barghan S, Tetradis S, Mallya S. Application of cone beam computed tomography for assessment of the temporomandibular joints. Aust Dent J. 2012;57:109–118.. [DOI] [PubMed] [Google Scholar]
- 15.Al-Khalisy HM, Nikiforov I, Mansoora Q, et al. Septic arthritis in the temporomandibular joint. N Am J Med Sci. 2015;7:480–482.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Margaretten ME, Kohlwes J, Moore D, et al. Does this adult patient have septic arthritis? JAMA. 2007;297:1478–1488.. [DOI] [PubMed] [Google Scholar]
- 17.Muhayidina AD, Said MS. Septic arthritis in rheumatology: review of five cases. J Clin Med Res. 2009;1:173–177.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mathews CJ, Kingsley G, Field M, et al. Management of septic arthritis: a systematic review. Ann Rheum Dis. 2007;66:440–445.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sembronio S, Albiero AM, Robiony M, et al. Septic arthritis of the temporomandibular joint successfully treated with arthroscopic lysis and lavage: case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:e1–e6.. [DOI] [PubMed] [Google Scholar]
- 20.Cai XY, Yang C, Chen MJ, et al. Arthroscopic management of septic arthritis of temporomandibular joint. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:24–30.. [DOI] [PubMed] [Google Scholar]
- 21.Chaves Netto HD, Nascimento FF, Chaves Md, et al. TMJ ankylosis after neonatal septic arthritis: literature review and two case reports. Oral Maxillofac Surg. 2011;15:113–119.. [DOI] [PubMed] [Google Scholar]
- 22.Goldschmidt MJ, Butterfield KJ, Goracy ES, et al. Streptococcal infection of the temporomandibular joint of hematogenous origin: a case report and contemporary therapy. J Oral Maxillofac Surg. 2002;60:1347–1353.. [DOI] [PubMed] [Google Scholar]
- 23.Broy SB, Schmid FR. A comparison of medical drainage (needle aspiration) and surgical drainage (arthrotomy or arthroscopy) in the initial treatment of infected joints. Clin Rheum Dis. 1986;12:501–522.. [PubMed] [Google Scholar]
- 24.Goldenberg DL, Brandt KD, Cohen AS, et al. Treatment of septic arthritis: comparison of needle aspiration and surgery as initial modes of joint drainage. Arthritis Rheum. 1975;18:83–90.. [DOI] [PubMed] [Google Scholar]
- 25.Peltola H, Pääkkönen M, Kallio P, et al. ; Osteomyelitis-Septic Arthritis (OM-SA) Study Group. Prospective, randomized trial of 10 days versus 30 days of antimicrobial treatment, including a short-term course of parenteral therapy, for childhood septic arthritis. Clin Infect Dis. 2009;48:1201–1210.. [DOI] [PubMed] [Google Scholar]
- 26.Dickerson SM, Weaver JM, Boyson AN, et al. The effectiveness of exercise therapy for temporomandibular dysfunction: a systematic review and meta-analysis. Clin Rehabil. 2017;31:1039–1048.. [DOI] [PubMed] [Google Scholar]
- 27.Ghasemzadeh A, Mundinger GS, Swanson EW, et al. Treatment of pediatric condylar fractures: a 20-year experience. Plast Reconstr Surg. 2015;136:1279–1288.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fatima J, Kaul R, Jain P, et al. Clinical measurement of maximum mouth opening in children of Kolkata and its relation with different facial types. J Clin Diagn Res. 2016;10:ZC01–ZC05.. [DOI] [PMC free article] [PubMed] [Google Scholar]


