Abstract
Fibrinolysis is a physiologic component of hemostasis that functions to limit clot formation. However, following trauma or surgery excessive fibrinolysis may contribute to coagulopathy, bleeding, and inflammatory responses. Antifibrinolytic agents are increasingly used to reduce bleeding and allogeneic blood administration, and adverse clinical outcomes. Tranexamic acid is the agent most extensively studied and used in most countries. This review will explore the role of fibrinolysis as a pathologic mechanism, review the different pharmacologic agents used to inhibit fibrinolysis, and focus on the role of tranexamic acid as a therapeutic agent to reduce bleeding in patients following surgery and trauma.
Introduction
Fibrinolysis is a physiologic component of hemostasis that functions to limit clot formation.1 However, following tissue injury associated with trauma or surgery, ischemia and reperfusion, blood contact with large non-endothelial surfaces such as cardiopulmonary bypass (CPB) circuits or as a contributing factor in other hemostatic disorders, excessive fibrinolysis may contribute to coagulopathy, bleeding, and inflammatory responses. As a result, growing data have reported the efficacy of antifibrinolytic agents to reduce bleeding, allogeneic blood administration, and adverse clinical outcomes. Of all the pharmacologic agents, tranexamic acid is the agent most extensively studied in the literature and used in most countries. This commentary will review the role of fibrinolysis as a pathologic mechanism, review the different pharmacologic agents used to inhibit fibrinolysis, and focus on the role of tranexamic acidas a therapeutic agent to reduce bleeding in patients.
Fibrinolysis
Fibrinolysis regulates the extent of fibrin formation and vascular obstruction during hemostasis. Following tissue and vascular injury, multiple hemostatic mechanisms are initiated as shown in figure 1, resulting in thrombin generation, platelet adhesion, cross-linking of platelets, and fibrin formation.1,2 As part of the hemostatic response to limit clot formation, fibrinolysis is initiated. Fibrin, the end product of coagulation activation, becomes the co-factor for plasminogen activation by tissue plasminogen activator. Plasmin, the enzymatic actor in fibrinolysis, then lyses fibrin, but as a promiscuous enzyme with respect to substrate specificity, it can also mediate the proteolytic (in)activation of multiple hemostatic and inflammatory components when present at conentrations that exceed the local and systemic inhibitors (most notably alpha2-antiplasmin), as shown in figures 1 and 2.1,3,4 Overall, when regulated, fibrinolysis can be considered a protective physiologic response that appropriately limits clot size. However, following major tissue damage that occurs during surgical and traumatic injury, inhibiting fibrinolysis may potentially inhibit other responses that contribute to bleeding.2,5 Fibrinolysis also contributes to coagulopathy by additional mechanisms beyond cleavage of fibrinogen and fibrin but also cleaving glycoprotein Ib and IIb/IIIa receptors on platelets reducing platelet adhesion and agrregation.6–8
Figure 1.
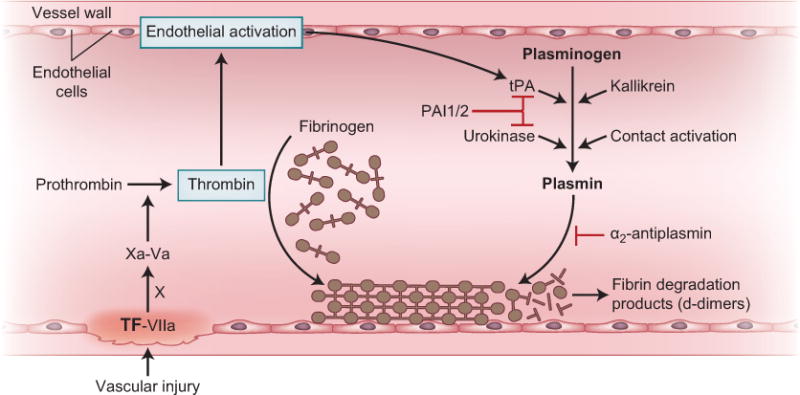
Simplified fibrinolysis pathway.
For clot formation, the principal event is fibrin formation following vascular injury, tissue factor binding to factor VIIa and activation of the Xase complex for hemostatic activation and thrombin generation. Thrombin stimulates endothelial release of tissue plasminogen activator (tPA), but also increased vascular flow, kinins, and other factors will release tissue plasminogen activator. Plasmin is released by formation of a plasminogen-tissue plasminogen activator complex that assembles on fibrin and binds to lysine sites on fibrin clot. Once assembled, tissue plasminogen activator cleaves plasminogen to its active form plasmin. Plasmin can also be generated by other mechanisms including urokinase, contact activation, and kallikrein mediated protease activation. Fibrinolysis is inhibited by plasminogen activator inhibitors (PAI 1 and PAI 2), and by thrombin binding to thrombomodulin to release and activate thrombin-activatable fibrinolysis inhibitor (not shown).
Abbreviations: TF—tissue factor, VIIa-factor VIIa, X- factor X, Va-factor Va, tPA—tissue plasminogen activator, PAI—plasminogen activator inhibitor
Figure 2.
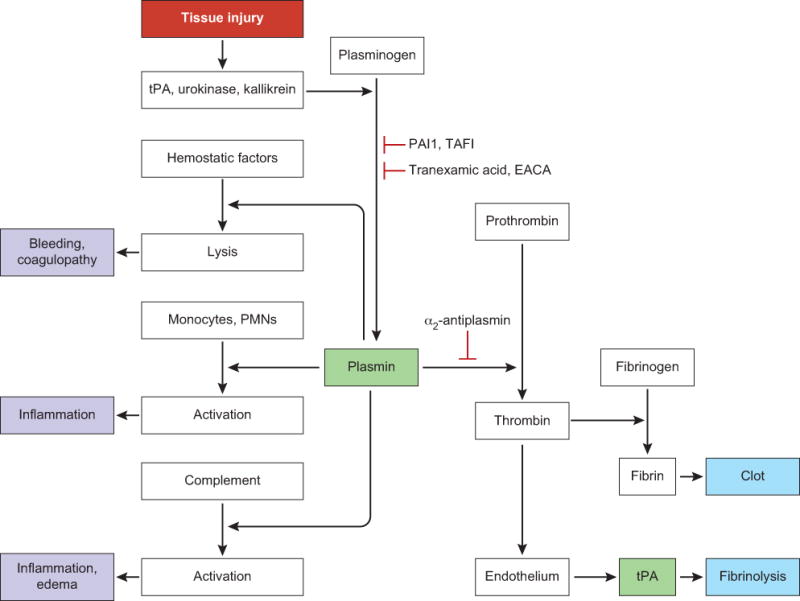
Multiple pathways are responsible for generation of plasmin, including endothelial activation and release of tissue plasminogen activator (tPA), contact activation, and kallikrein-mediated plasmin activation. Plasmin generation and activity are also inhibited by plasminogen activator inhibitor1 (PAI1), thrombin-activatable fibrinolysis inhibitor (TAFI), lysine analogues (tranexamic acid and ε-aminocaproic acid [EACA]), and α2-antiplasmin. Plasmin generation after tissue injury can induce many other responses, including thrombin generation and cleavage of fibrinogen to fibrin. Plasmin also binds and activates monocytes, neutrophils, platelets, and endothelial cells, to increase proinflammatory responses and multiorgan system-failure. Attenuation of these pathophysiological responses with tranexamic acid might provide additional mechanisms to restore hemostatic balance and control of plasmin generation and fibrinolysis, as shown in CRASH–2.PMNs=polymorphonuclear leucocytes. After trauma, tissue injury shifts the complex balance of fibrinolysis to additional plasmin generation, and activation that increases coagulopathy, inflammatory responses, and bleeding. (from Levy JH Lancet reference 5)
Thus, plasmin may exhibit multiple proinflammatory responses that could stimulate pathophysiologic responses and multi-organ system failure. These adverse outcomes may be attenuated with antifibrinolytic agents, and reports suggest that antifibrinolytic therapy may improve mortality in high-risk patients undergoing cardiac surgery.9,10,11
Molecular regulation of fibrinolysis
The molecular activators of plasminogen are primarily tissue-plasminogen activator but also urokinase-plasminogen activator.2,6 Endothelial activation by a variety of agonists releases tissue plasminogen activator from vascular endothelial cells where it binds to fibrin and activates plasminogen to promote fibrinolysis at the site of clot formation. Activation of fibrinolysis is facilitated by sites in the plasminogen molecule that bind to fibrin’s lysine residues.2,6 Tranexamic acid, a synthetic derivative of lysine, interferes with this step by occupying the lysine binding sites in plasminogen.
The molecular inhibitors of fibrinolysis include plasminogen activator inhibitor 1 that inhibits tissue plasminogen activator and plasminogen activator inhibitor 2 that inhibits urokinase-plasminogen activator.2 The physiologic inhibitor of plasmin is alpha2-antiplasmin but currently called plasmin inhibitor. Also, α2-macroglobulin functions as a plasmin inhibitor. Factor XIIIa, a transglutaminase, crosslinks fibrin to increase clot strength and render it more resistant to fibrinolysis.12 Thrombin activatable fibrinolysis inhibitor, when activated by the thrombin-thrombomodulin complex, removes lysine residues on fibrin, eliminating binding sites for plasminogen, and may play an important role in regulating crosstalk between inflammation and coagulation.13
With normal physiology and that includes an intact vascular and endothelial system, hemostatic balance is well preserved. However, following massive trauma, surgery, or extracorporeal circulation, the ability to locally regulate fibrinolysis is exceeded, such that plasmin generation and ensuing fibrinolysis becomes systemic, and coagulopathy ensues. This is the basis of pharmacologic administration of tranexamic acid that will be reviewed. Although increasing data suggest the critical role of hyperfibrinolysis as a pathologic cause of bleeding, there is individual variability of fibrinolysis in all pathologic states. This has led to potential concerns for an increase of plasminogen activator inhibitor -1 and a decrease of tissue plasminogen activator activity in some patients, a scenario that has been termed fibrinolytic shutdown.14,15 The theory is that patients with fibrinolytic shutdown would not be expected to benefit from an antifibrinolytic such as tranexamic acid, and may develop potential thrombotic effects. However, the clinical relevance of fibrinolytic shutdown is the subject of ongoing debate and research.15–17
Laboratory measurement of fibrinolysis
Over the years, multiple methods to assess fibrinolytic activity in blood have been reported, however, there is no “gold standard” test.4 Available assays vary depending on whether whole blood, plasma, or the euglobulin fraction of plasma is used for the assessment of fibrinolysis. Point-of-care testing using whole blood in a perioperative setting has the benefit of evaluating all plasma and cellular components including red blood cells, platelets, mononuclear, and polymorphonuclear leukocytes.
The most extensively used tools for measuring fibrinolysis in a perioperative setting are thromboelastography and rotational thromboelastometry that use different activators, including kaolin, tissue factor, or ellagic acid to measure viscoelastic changes in whole blood over time. Fibrinolysis is measured by the rapidity of tapering of the clot over time and is expressed as maximal lysis for rotational thromboelastometry. Maximal lysis >3% is the critical value for initiation of antifibrinolytic therapy in trauma, while a value of >15% suggests hyperfibrinolysis.4,18,19 Thromboelastography/thromboelastometry is the test most often used clinically to determine fibrinolysis in trauma patients.20 With the increasing use of pre-emptive antifibrinolytic therapy to reduce bleeding in trauma and surgery, there is some debate regarding the need for assessment of fibrinolysis. However, based on concerns regarding fibrinolytic shutdown in a subset of patients, there is growing interest in monitoring fibrinolysis in trauma.16 thromboelastography and rotational thromboelastometry are frequently used to assess fibrinolytic activation in trauma patients. However, they are not sensitive enough to detect minor degrees of fibrinolytic activation.15,18,21,22 There is ongoing debate about their utility to detect fibrinolytic activation and guide antifibrinolytic agent administration.19
Other methods of evaluating fibrinolysis include plasma turbidity methods based on measuring optical density changes that reflect fibrin formation and lysis.4 The classic test for fibrinolysis is the euglobulin clot lysis time developed in the 1950s that acidifies citrated platelet-poor plasma to selectively precipitate certain factors including fibrin(ogen), plasminogen, and tissue plasminogen activator, while largely excluding the principal inhibitors of fibrinolysis (plasminogen activator inhibitor -1, alpha2-antiplasmin and alpha2-macroglobulin). This ‘re-balancing’ of plasma components within the precipitate (the euglobulin fraction) allows the measurement of endogenous fibrinolysis, which is normally inhibited by the large excess of fibrinolytic inhibitors. The clot within the euglobulin fraction can be visually evaluated until complete lysis occurs.4 Although there is no single gold standard assay for global measurement of fibrinolysis, thromboelastography and rotational thromboelastometry are the assays that are most often used in practice.
Pharmacology of antifibrinolytic agents
The two mainstay anti-fibrinolytic agents are the synthetic lysine analogs tranexamic acid and epsilon aminocaproic acid that inhibit fibrinolysis by attaching to the lysine-binding site of the plasmin (ogen) molecule, thereby displacing plasminogen from fibrin. Both tranexamic acid and were developed and approved for use by regulatory agencies over 50 years ago when it was found that some amino acids such as lysine and its analogs inhibited the activation of plasminogen in vitro.23 Aprotinin, another fibrinolytic inhibitor, is a broad-spectrum naturally occurring protease inhibitor that is only available in certain countries. Other molecular entities have been studied as potential fibrinolytic inhibitors, but are not approved for use, and include nafamostat, MDCO-2010, and textilinins from Pseudonaja textilis.24–26 The three clinically available agents will be reviewed as follows.
Aprotinin
Aprotinin is a protease inhibitor isolated from bovine lung and is comprised of 58 amino acids with a molecular weight of 6512 Daltons. The molecular structure with its three kringles is structurally similar to tissue factor pathway inhibitor. Aprotinin dosing is calculated in “kallikrein inhibiting units” and protocols usually follow a “full-dose” (2×106 kallikrein inhibiting units bolus followed by 5×10 5 / h continuous infusion) or a “half-dose” protocol. The agent is predominantly eliminated via proteolysis and only to a minor extend via the kidneys. The initial plasma half-life is 150 min, with a terminal half-life of approximately 10 hours.27
Aprotinin is a broad-spectrum protease inhibitor that reversibly complexes with the active serine residue in various proteases in plasma, and reversibly inhibits trypsin, kallikrein, plasmin, elastase, and is the most potent antifibrinolytic agent.28 The propagation of fibrinolysis through Factor XIIa-mediated kallikrein activation (contact activation) and plasmin generation through tissue plasminogen activator -mediated plasminogen activation is inhibited by ~4 μmol/l of aprotinin.28 However, apart from these direct effects on the plasmatic coagulation system, aprotinin also inhibits the protease-activated receptor-1 thrombin receptor involved in both coagulation and inflammation.29 Aprotinin’s inhibition of – protease-activated receptor -1 has been postulated to be a mechanism for stroke reduction following aprotinin administration for cardiac surgery.28,30,31
Despite multiple studies reporting its efficacy, several reports questioned its safety, leading to its temporary removal from the United States market. Following a re-analysis of the data, the European Medicines Agency recommended in 2012 that its suspension in the European Union be lifted and is currently being re-introduced in Europe. However, the European Medicines Agency noted that aprotinin should only be given for “prophylactic use to reduce blood loss and blood transfusion in adult patients who are at high risk of major blood loss undergoing isolated cardiopulmonary bypass graft surgery (i.e. coronary artery bypass graft surgery that is not combined with other cardiovascular surgery” and “only after careful consideration of the benefits and risks, and the consideration that alternative treatments are available” (http://www.ema.europa.eu/docs/en_GB/document_library/Referrals_document/Antifibrinolytic_medicines/WC500153601.pdf). Additionally the European Medicines Agency required the establishment of a European registry for aprotinin use (http://www.ema.europa.eu/docs/en_GB/document_library/Press_release/2012/02/WC500122914.pdf). The European Society of Anaesthesiology task force reported on aprotinin use in a perioperative setting and has current suggestions for its use.32
Epsilon aminocaproic acid
Epsilon-aminocaproic acid is a synthetic inhibitor of plasminogen activation with a molecular weight of ~131 daltons. Pharmacokinetic studies evaluating intravenous epsilon aminocaproic acid of 10 g or 100 mg/kg in volunteers produced an initial concentration of about 1.5 g/L that decreased to 35 mg/L within 3-4 h and 80-100% was eliminated in the urine by filtration.33–35 In vitro experiments and clinical studies report that a plasma epsilon aminocaproic acid concentration of ~130 mcg/ml is required to inhibit systemic fibrinolytic activity.33–35 Since epsilon aminocaproic acid is rapidly excreted in the urine it must be administered intravenously as an infusion to maintain therapeutic levels. Nilsson et al recommended a dose of 0.1 g/kg bodyweight every 3-4 h, whereas McNicol et al recommended an initial loading dose of 10 g followed by a continuous i.v. infusion of 1 g/h to maintain a plasma concentration of ~130mcg/ml.33,35,36
After intravenous administration, the volume of distribution is reported to be 30.0 ± 8.2 L and is primarily eliminated by the kidneys, with 65% recovered unchanged, and 11% appearing as adipic acid.33–35 The total body clearance is 169 mL/min with a terminal elimination half-life of ~2 hours.33–35 (http://www.accessdata.fda.gov/drugsatfda_docs/label/2004/15197scm036,scf037,scp038,scm039_amicar_lbl.pdf) The concentration of epsilon aminocaproic acid required to inhibit fibrinolysis is ~1 mMol/L or 0.13 mg/mL that is achieved with a 5 g load followed by 1 to 1.25 g/hr, which should maintain plasma levels of 0.13 mg/mL.
Epsilon aminocaproic acid is most extensively used in the United States compared to most countries that use tranexamic acid. This may be related to costs and that it was the first agent that was widely available. Side effects reported from epsilon aminocaproic acid include hypotension, cardiac arrhythmias, rhabdomyolysis, and renal dysfunction.37,38
Tranexamic acid
Tranexamic acid is a lysine analog with a molecular weight of ~157 Daltons that reversibly binds to the lysine-binding sites on plasminogen to inhibit its affinity to bind to multiple proteins including fibrin. After a 10 mg/kg intravenous dose of tranexamic acid, the half-life is ~80 minutes with 30% renal elimination within the first hour, while after oral administration of 10 to 15 mg/kg, peak plasma concentrations occur within 3 hours.39 Andersson et al. reported 98-100% reduction of fibrinolytic activity required concentrations of ~100 mg/L.40
After intravenous administration of 10 mg tranexamic acid /kg bodyweight, 30% was recovered in the urine by one hour, 55% by three hours and 90% within 24 hours. Further studies indicated that tranexamic acid, like epsilon aminocaproic acid, is eliminated by glomerular filtration.39 Also similar to epsilon aminocaproic acid, tranexamic acid is distributed throughout the intracellular and extracellular compartments.36 On molar basis tranexamic acid is 7-10 times more potent than epsilon aminocaproic acid and has more sustained antifibrinolytic activity in tissues.36,40
Intravenous dosing ranges from ~0.5 to 25 g depending on the types of patients and procedures. In one of the largest studies to date of tranexamic acid, the Clinical Randomization of an Antifibrinolytic in Significant Hemorrhage trial (CRASH-2 trial) conducted in patients with post traumatic bleeding, tranexamic acidwas administered as a loading dose of 1 g intravenously followed by an infusion of 1 g over 8 hours. In orthopedic surgery, tranexamic acid doses usually range from 0.5 to 2 g. Recent studies have utilized a loading dose of 4 g intravenously over 1 hour followed by infusion of 1 g/hour over 6 hours.41,42 For excessive menstrual bleeding, based on the United States prescribing information tranexamic acid is given orally (Lysteda®) at doses of 1.3 g every 8 hours for up to 5 days.
Despite the potential toxicity concerns, side effects are uncommon, as noted in patients with heavy menstrual bleeding receiving oral doses of 1.3 g three times daily for 4-5 days.43 Oral tranexamic acid is currently approved by the FDA and in other countries, with an impressive safety record, for reducing bleeding in women with idiopathic menorrhagia. Its efficacy is thought to be explained by inhibition of increased fibrinolytic activity in the endometrium during the initial days of menstruation. However, macroscopic hematuria with bleeding from the upper renal tract is considered a contraindication to tranexamic acid due to concerns for clot obstruction in the ureters, and reports of acute renal cortical necrosis with renal failure.23
Antifibrinolytic therapy and risk of thrombosis
The potential role of antifibrinolytic therapy producing hypercoagulability is a potential concern among clinicians.44 There may be a prothrombotic effect of plasmin during therapeutic fibrinolysis that is explained by plasmin-mediated prothrombin and platelet activation.45 Multiple studies have reported that fibrinolysis and fibrinolytic therapy activates platelets and/or the plasma coagulation components both in vitro and in vivo.46–48 Despite concerns about the potential for a prothrombotic effect of fibrinolytic inhibitors, thrombosis has not been a significant clinical issue. In randomized controlled trials of antifibrinolytics in major orthopedic surgery, cardiac surgery, or trauma (CRASH-2 trial), there were no increased in thrombotic complications compared to controls.49 Of note is that meta-analyses of tranexamic acid in orthopedic surgical patients, who are at particularly high risk for venous thromboembolism, no increased incidence of venous thromboembolism was observed compared to controls.50–52 Moreover, one analysis reviewed thrombotic events as an outcome in 5,049 subjects from 57 studies of patients treated with tranexamic acid, epsilon aminocaproic acid, or aprotinin for various types of bleeding not related to trauma or surgery.53 A total of 3,616 (72%) had subarachnoid hemorrhages of which 3,414 (68%) patients received tranexamic acid and 1,635 (32%) received epsilon aminocaproic acid. The frequencies of limb ischemia and myocardial infarction were <1% for tranexamic acid and epsilon aminocaproic acid. The frequency of deep vein thrombosis or pulmonary embolism was 1.9% for tranexamic acid and 3.0% for epsilon aminocaproic acid.53
In orthopedic surgical patients undergoing total hip replacement or total knee arthroplasty, randomized controlled trials have compared the effect of tranexamic acid, epsilon aminocaproic acid, or aprotinin with placebo on bleeding, transfusion or venous thromboembolic events. Tranexamic acid was used in the majority of trials, where patients also received routine mechanical and/or pharmacological prophylaxis for deep vein thrombosis.54 The mean age of patients ranged from 55-76 years. The analyses showed no significant difference in risk of venous thromboembolism in patients receiving antifibrinolytic therapy compared to those receiving placebo in 1,637 patients. Additional subgroup analyses according to the antifibrinolytic therapy reported no significant differences in venous thromboembolic events between the treated and control groups.
In liver transplantation, from 23 studies involving 1,407 patients who received tranexamic acid or aprotinin, despite reduced bleeding and the need for transfusion, there was no increased risk for hepatic artery thrombosis, venous thromboembolic events or perioperative mortality.55
Anti-inflammatory effects of inhibiting fibrinolysis
One of the proposed benefits of inhibiting fibrinolysis is that plasmin and plasminogen have broad-spectrum inflammatory effects due to cellular binding, proteolytic activity, and generation of inflammatory mediators as shown in figure1.56 Plasmin, particularly when bound to the surface of macrophages, plays a critical role in monocyte activation and inflammation including exit from circulation into injured or infected tissue, cytokine production, and proteolytic activation of matrix-metalloproteases with subsequent degradation and remodeling of extracellular matrix. Activated plasmin elicits chemotaxis and actin polymerization in monocytes including the release of cytokines downstream of the transcription factors nuclear factor-κB, activator protein 1, and signal transducer and activator of transcription.57,58
Much of the data that demonstrate the role of plasmin and plasminogen in inflammation have been generated in experimental animal models that have included plasminogen knock out mice. Plasminogen null mice were found to have reduced macrophage infiltration into sites of inflammation following peritoneal thioglycollate injection as well as reduced abdominal aortic aneurysm formation after calcium chloride injection.59 Reduction in macrophage infiltration and abdominal aortic aneurysm were associated with reduced matrix-metalloproteases -9 activity. In this model, macrophage infiltration, matrix-metalloproteases -9 activity, and vascular remodeling leading to abdominal aortic aneurysm could be restored by injecting plasminogen knock-out animals with activated plasmin. The dependence of these murine models of inflammation and vascular remodeling on the proteolytic activity of plasmin highlights its importance to innate immunity and inflammation.
The relationship between plasmin activity and inflammation has been studied in humans primarily during the use of antifibrinolytic drugs (tranexamic acid, epsilon aminocaproic acid, and aprotinin) to inhibit plasmin and decrease bleeding. In cardiac surgery, the effects of tranexamic acid and aprotinin were studied using whole blood mRNA expression profiling of inflammatory genes.60 Of the 114 genes studied, eight produced less transcript in the presence of aprotinin, while three genes were inhibited by tranexamic acid and aprotinin, the broader spectrum of aprotinin most likely owing to its broader inhibitory activity against serine proteases and its effects on the protease actived receptor-1/thrombin receptor of platelets.
Apart from cardiac surgery, inflammation secondary to bacterial infection and exposure to lipopolysaccharide results in plasmin generation which may contribute to disseminated intravascular coagulation in septic shock. Macrophages and dendritic cells have several receptors for binding and activating plasminogen to plasmin11 that in turn activates other proteases, digests extracellular matrix, and initiates an inflammatory response needed to fight infection. One study in humans has attempted to address the ability of systemically administered anti-fibrinolytic drugs to counteract the inflammation associated with lipopolysaccharide exposure. Healthy volunteers were given an intravenous bolus of E. coli derived lipopolysaccharide 4 ng/kg, preceded either by a 30-minute infusion of tranexamic acid (2g) or placebo.61 In normal humans, LPS induces rapid increases in plasma of levels d-dimers and plasmin-α2-antiplasmin complexes. Pretreatment with tranexamic acid prior to lipopolysaccharide administration greatly attenuates d-dimer and plasmin-α2-antiplasmin complexes, indicating a reduction in the activity of free plasmin and protection against fibrinolysis. However, tranexamic acid pretreatment did not affect LPS-induced thrombin generation; expression of lipopolysaccharide -induced markers of leukocyte activation CD11b and CD66b on leukocytes; lipopolysaccharide -induced release of von Willebrand factor and E-selectin from endothelial cells; or lipopolysaccharide -induced production of tumor necrosis factor α, interleukin-6, interleukin-8, and interleukin-10. Taken together, these results seem to suggest that tranexamic acid can inhibit the activity of free plasmin and fibrinolysis; however, many of the inflammatory effects are mediated by plasmin bound to the surface of leukocytes where it is relatively protected from antifibrinolytic drugs. Plasmin’s importance in initiating inflammation, leukocyte chemotaxis, and extracellular matrix remodeling is indisputable given the dramatic phenotype induced in plasminogen knock-out mice. What is not fully clear is the degree to which anti-fibrinolytic drugs can modulate inflammation by limiting plasmin’s proteolytic activity. Expression of several inflammatory genes is altered by the administration of anti-fibrinolytic drugs in the setting of cardiac surgery. However, several lipopolysaccharide -induced aspects of plasmin activation are not affected by pretreatment with antifibrinolytics.
Clinical Uses
Cardiac Surgery
Cardiac surgery including cardiopulmonary bypass (CPB) but also off-pump is arguably one of the most studied scenarios of antifibrinolytic use. Treated patients consistently demonstrate reduced bleeding and allogeneic transfusion requirements. We have previously reviewed the use of antifibrinolytic agents in cardiac surgery in this journal, as shown in Table 1, and have noted that these drugs are an important part of perioperative blood conservation management.27
Table 1.
Antifibrinolytic agents: drugs description, doses, and mechanisms of action.
| Drug | Composition | Mechanism of Action | Elimination | Pharmaco-dynamics | Suggested Dosing in Adults | Approval |
|---|---|---|---|---|---|---|
| Aprotinin | Protein, isolated from bovine lung tissue | protease inhibitor Reversibly complexes with the active sites of plasmin, kallikrein, and trypsin Inhibition of: fibrinolysis, factor XIIa induced contact activation, thrombin induced platelet activation inflammatory response |
predominantly proteolysis, ~60% % renal |
initial plasmaT½ 150 min, terminal T½ life 10 h |
“Full Dose”: 2× 106 KIU bolus patient, 2× 106 KIU bolus CPB, continuous infusion of 5×105 KIU “Half Dose”: 1×106 KIU bolus patient, 1×106 KIU bolus CPB, continuous infusion of 2.5×105 KIU |
suspended since 2008; suspension lifted in Canada in 2011 and Europe in 2012 In the US still suspended |
| Tranexamic Acid | synthetic lysine analogue | antifibrinolytic; competitive inhibition of the activation of plasminogen to plasmin | renal | plasma ½ life 3 h | “High Dose”: 30 mg/kg bolus patient, 2 mg/kg CPB, continuous infusion of 16mg/kg “Low Dose”: 10 mg/kg bolus patient, 1-2 mg CPB, continuous infusion of 1 mg/kg |
US, Canada, Europe |
| Epsilon Aminocaproic Acid | synthetic lysine analogue | antifibrinolytic: competitive inhibition of the activation of plasminogen to plasmin | renal | plasma T½ life 2 h | 100 mg/kg bolus patient, 5 mg/kg CPB, continuous infusion of 30 mg/kg |
US, Canada |
From reference 5 (Anesthesiology. 2015;123(1):214-21).
Despite this, the optimal dose of tranexamic acid is still not established. In a prospective, blinded dosing study, 148 patients were randomized to placebo, while five groups received intravenous tranexamic acid as loading doses that ranged from 2.5 to 40 mg/kg before incision, followed by an infusion of one-tenth the loading dose for 12 hours.62 The authors reported that patients receiving an initial 10 mg/kg loading dose followed by an infusion had significantly less chest tube drainage than with lower doses, but did not alter transfusions, and higher doses did not provide additional reductions in bleeding. Fiechtner et al. reported that a bolus 10 mg/kg dose with an infusion of 1 mg/kg/h was provided a tranexamic acid plasma concentration that inhibited fibrinolytic activity in vitro.63 Dowd et al. calculated a loading dose of 30 mg/kg followed by 16 mg/kg/hour for 6 hours and 2 mg/kg added to the pump prime to achieve 100% inhibition of fibrinolytic activity.64 (see Table 1). Using this dosing strategy, Sharma et al. found mean plasma tranexamic acid concentration was consistently higher than the previously suggested threshold.65
With the increasing use of tranexamic acid in cardiac surgery and at higher doses, reports emerged about generalized convulsive seizures in the absence of new ischemic lesions on brain imaging, often in patients receiving higher tranexamic acid doses of 100 mg/kg intravenously followed by 20–50 mg/kg/hour with a total dose up to 259 mg/kg.66 Experimental models noted that hyperexcitability and seizures appeared in a dose-dependent fashion when tranexamic acid was applied topically onto central nervous system tissue. However, these concentrations are unlikely to be achieved in clinical practice.67
In the largest randomized clinical trial of tranexamic acid in cardiac surgery, Myles et al randomized 4631coronary-artery surgical patients to receive aspirin or placebo and tranexamic acid or placebo with a primary composite outcome of death and thrombotic complications that included nonfatal myocardial infarction, pulmonary embolism, stroke, renal failure, or bowel infarction) within 30 days after surgery.68 A total of 2311 patient received tranexamic acid and 2320 placebo. The primary outcome event occurred in 386 tranexamic acid patients (16.7%) and 420 patients (18.1%) placebo. tranexamic acid reduced transfusion during hospitalization from 7,994 total units in placebo to 4,331 in the tranexamic acid group. Adverse events including hemorrhage or cardiac tamponade requiring reoperation occurred in 2.8% of placebo and 1.4% of tranexamic acid, and seizures occurred in 0.1% of placebo and 0.7% of tranexamic acid treated patients.69
Seizures and tranexamic acid
In 2010, clinicians began to report convulsive seizures following cardiac surgery with CPB using high-dose tranexamic acid initially, and from retrospective evaluations at lower doses.70 In a recent meta-analysis of randomized controlled trials and retrospective studies, the use of tranexamic acid was associated with a 4.1-fold increased risk of clinical seizures.71 Suggested mechanisms for tranexamic acid -induced seizures include increased neuronal excitation mediated by antagonizing inhibitory γ-aminobutyric acid (GABA) neurotransmission and neural glycine receptors.67 As shown in figure 2, tranexamic acid, γ-aminobutyric acid, and glycine have similar molecular structures. However, despite the similarities, epsilon aminocaproic acid, another lysine analog antifibrinolytic agent, has not been reported to produce seizures. tranexamic acid’s structure is similar to glycine that functions as an inhibitory neurotransmitter in the brain and spinal cord. In cardiac surgical patients, seizures are primarily observed in older patients after CPB for open heart surgery, where multiple other mechanisms including cerebral emboli may be responsible. With emboli, vascular injury may cause local disturbances of the blood brain barrier, increase tranexamic acid concentrations at the site of injury in the brain and potentially promote seizures as we have previously speculated in an editorial in the journal.70 Therefore, additional mechanisms may be responsible for producing seizures. This is particularly important because the risk of seizures seems insignificant in women receiving approximately 4 g a day of tranexamic acid for menstrual bleeding, in trauma patients in the large CRASH-2 trial who received 2 g of tranexamic acid, and in non-cardiac surgical patients.
However, the impact of tranexamic acid associated seizures after cardiac surgery on clinical outcomes is not well understood. Assuming a transient pharmacological mechanism, one would expect only a minor effect on clinical outcomes, presumably with the exception of some critically ill patients where weaning from mechanical ventilation may be delayed. This consideration is consistent with an analysis of a large national database of over 11,000 pediatric patients undergoing surgery for congenital heart disease.72 The propensity matching resulted in more than 3,700 pairs of patients and reported the incidence of seizures was 8-fold increased (1.6% vs 0.2%) in patients who received tranexamic acid, while all other clinical outcomes were comparable between groups. In contrast, in the aforementioned large randomized clinical trial in coronary artery bypass patients, the seizure rate in the tranexamic acid group was 7-fold increased (15 patients [0.7%] vs. 2 patients [0.1%]) and seizures were associated with a 9.52-fold risk of 30 day mortality.68 However, in these patients the relative risk for stroke was nearly 22-fold. Patient numbers are too small to draw any definitive conclusions. However, these data suggest that besides temporal pharmacological effects, other mechanisms contributed to the seizures and persisting neurological damage.
Liver Surgery
Bleeding and coagulopathy in patients undergoing liver surgery or transplantation is common. In patients with hepatic dysfunction, complex alterations in hemostatic function are common due to multiple causes, and excessive bleeding is common during these procedures. Hyperfibrinolysis is also common during liver transplantation.73 During the early development of liver surgery and transplantation, hyperfibrinolysis was reported using thromboelastography, and empiric antifibrinolytics were initially used by transplant pioneer Dr. Thomas Starzl to reduce bleeding. Several years later, when further evaluating coagulopathy associated with liver transplantation, potential concerns regarding venous thromboembolism and increased mortality were reported. The routine use of tranexamic acid and antifibrinolytic agents overall is variable. During hepatic transplantation, tissue plasminogen activator levels may be increased during the anhepatic phase of transplantation due to vascular injury and reduced clearance. Following reperfusion of the transplanted liver, tissue plasminogen activator clearance and plasminogen activator inhibitor -1 release often corrects the hyperfibrinolysis. Most liver transplant centers use viscoelastic monitoring with rotational thromboelastometry or thromboelastography as a guide for the use of tranexamic acid for hyperfibrinolysis.
Molenaar reported a meta-analysis of safety and efficacy in randomized clinical trials of antifibrinolytics used in liver transplantation up to 2007 that included tranexamic acid, aprotinin, and epsilon aminocaproic acid. A total of 23 studies with 1,407 patients were analyzed and found that both aprotinin and tranexamic acid reduced the need for allogeneic transfusions, without safety concerns that included hepatic artery thrombosis, venous thromboembolic events or perioperative mortality.55
Additional studies include a randomized multicenter evaluation of primary liver transplantation in 137 patients with high and low dose aprotinin published in 2000. Blood loss was reduced in the aprotinin-treated patients by 44 – 60%, transfusion requirements were 20 – 37% lower, and there were no differences in mortality or thromboembolic events among the groups.74 In another trial of 132 patients undergoing hepatic transplantation, patients were randomized to tranexamic acid, epsilon aminocaproic acid, or placebo. Transfusions were reduced in the tranexamic acid treated patients, and there was no benefit of epsilon aminocaproic acid, and no intergroup difference with regard to transfusion requirements, thromboembolic events, and mortality.75
There are less data for antifibrinolytic use in patients undergoing hepatic resection. In a prospective randomized trial for hepatic tumor resections, tranexamic acid was compared to placebo in 214 hepatectomies with continuation of therapy every 6 hours for 3 days. The authors noted lower blood losses, transfusions, shorter operative times, and lower hospital costs in the tranexamic acid treated patients. There were no differences in adverse outcomes including thromboembolic events or mortality.76
Orthopedic surgery
Multiple clinical trials have reported the efficacy of antifibrinolytic therapy in reducing bleeding and transfusion requirements in orthopedic surgery. Zufferey reported a meta-analysis examining both efficacy for reducing perioperative allogeneic red blood cell transfusion from 43 randomized controlled trials in total hip and knee arthroplasty, spine fusion, musculoskeletal sepsis, or tumor surgery performed prior to July 2005.77 The report included 23 trials with 1,268 patients receiving aprotinin, 20 trials with 1,084 patients receiving tranexamic acid, and 4 trials with 171 patients receiving epsilon aminocaproic acid. Both aprotinin and tranexamic acid significantly reduced patient need for red blood cell transfusions with an odds ratio of 0.43 for aprotinin and 0.17 for tranexamic acid.77
Additional randomized clinical trials in patients undergoing primary total hip arthroplasty using only tranexamic acid at doses of 0.5-2 g reported on 505 patients from 11 studies for total hip arthroplasty. tranexamic acid significantly reduced perioperative bleeding and allogeneic transfusion requirements compared to the control group with no differences in venous thromboembolism or other adverse events using dosing strategies of ~1g before incision (10–15 mg/kg), with or without additional dosing by continuous infusion or repeat dosing.50
For primary total knee arthroplasty, a meta-analysis up to 2012 reported 1,114 patients from 19 randomized clinical trialsand noted tranexamic acid reduced postoperative bleeding and transfusion requirements without differences in venous thromboembolism or other adverse events in the immediate postoperative period.78 In a meta-analysis of 411 patients from six randomized clinical trials, tranexamic acid at doses of ≥ 15 mg/kg reduced bleeding and the need for transfusion without safety concerns includingvenous thromboembolism.79
Multiple studies have reported that tranexamic acid reduces blood loss and transfusions in patients undergoing total knee arthroplasty. tranexamic acid is routinely used for total knee arthroplasty, whereas epsilon aminocaproic acid is less frequently used. As a result, a multicenter retrospective chart review of elective unilateral total knee arthroplasty from April 2012 through December 2014 was performed that included 5 hospitals within a health care system.80 The authors collected age, severity of illness score, gender, use of antifibrinolytic agent and dose, red blood cell transfusions, and pre-admission and discharge hemoglobin. epsilon aminocaproic acid dosing was 5 or 10 g and based on weight, compared to 1 g for tranexamic acid included 2,922 primary unilateral total knee arthroplasty cases, 820 patients received, 610 patients received tranexamic acid, and 1,492 patients received no antifibrinolytic therapy (control group). The proportion of patients transfused with epsilon aminocaproic acid was 2.8%, tranexamic acid 3.2%, and controls 10.8% with lower mean red blood cell units transfused per patient. However, there were no differences between the epsilon aminocaproic acid and tranexamic acid groups in the number red blood cell units transfused per patient, percentage of patients transfused, or discharge Hb levels.81
The same investigators similarly evaluated antifibrinolytic use in total hip arthroplasty in a retrospective chart review of 1,799 primary unilateral total hip arthroplasty cases from April 2012 through December 2014, of whom 711 received epsilon aminocaproic acid, 445 received tranexamic acid, and 643 received no antifibrinolytic agent. RBC transfusions were 6.8% in the epsilon aminocaproic acid treated patients, 9.7% in the tranexamic acid group, and 24.7% in the patient is receiving no therapy, although no differences were noted in mean red blood cell units per patient and percentage of patients transfused between the antifibrinolytic treated patient groups.
Antifibrinolytic therapy in most surgical procedures including orthopedic surgery is limited to intraoperative use. In a recent study, Zufferey et al examined whether additional postoperative tranexamic acid infusion could further reduce blood loss and need for allogeneic transfusions in a randomized, blinded, prospective study of 168 patients for primary hip arthroplasty.82 A 1 gram tranexamic acid loading dose was initially administered followed by a continuous infusion of 1 gram or placebo for 8 hours along with a restrictive transfusion algorithm. There were no differences between the groups, and the authors also performed a meta-analysis combining this study with five other similar trials and found no differences in bleeding or transfusion rates.
Postpartum hemorrhage
Postpartum hemorrhage is a leading cause of maternal morbidity and mortality worldwide. Hematologic changes in pregnancy at the time of delivery include decreased plasminogen activator inhibitor -2 synthesis and tissue plasminogen activator release and hyperfibrinogenemia at levels of 500-600 mg/dL. Multiple studies in different patient populations have evaluated tranexamic acid as a therapeutic agent to reduce bleeding and improve outcomes. In two initial randomized clinical trials, tranexamic acid was given as 1 g or 0.5 g intravenously 2–3 minutes after vaginal delivery, or 1 g intravenously prior to incision for cesarean section.83 The authors reported blood loss was reduced with tranexamic acid but there were no differences between the chosen doses.83 In an analysis of over 1,000 women from five randomized clinical trials undergoing elective cesarean section, tranexamic acid at doses of 1 g intravenously prior to incision reduced bleeding.84
For a more definitive answer, the recently reported World Maternal Antifibrinolytic(WOMAN) trial was a randomized, double-blind, placebo-controlled trial evaluating early administration of tranexamic acid on mortality, hysterectomy, and other relevant outcomes with post-partum hemorrhage. Recruitment was from March, 2010 to April, 2016 in 20,060 women after vaginal delivery or caesarean section from 193 hospitals in 21 countries.85 tranexamic acid was administered as a 1 g intravenous dose, but if bleeding persisted or restarted within 24 h of the first dose, a second 1 g dose could be given. The composite primary endpoint was death from all-causes or hysterectomy within 42 days and was analyzed on an intention-to-treat basis. Death due to bleeding was reduced in tranexamic acid treated women (1.5%-155/10,036 patients) compared to [1.9% 191 of 9985) in the placebo group, risk ratio [RR] 0·81; p=0·045). When tranexamic acid was given within 3 h of delivery mortality was 1.2% compared to 1.7% in placebo, RR 0·69; p=0·008), and there were no differences in hysterectomy in tranexamic acid treated patients versus controls [3.6% vs 3·5%]. The composite primary endpoint of all-cause mortality or hysterectomy was not reduced with tranexamic acid [5.3% vs 5.5%], and there were no differences in adverse events between the groups.85
Traumatic injury
Despite the extensive use of antifibrinolytic therapy and tranexamic acid for multiple other indications, its use in trauma has significantly increased only in recent years. Fibrinolysis follows tissue injury as initially noted. However, multiple studies have helped better define fibrinolysis following trauma. In a study of 303 trauma patients, rotational thromboelastometry, d-dimer and plasmin-antiplasmin (PAP) complexes were used to better define implications of traumatic injury. 57% had “moderate” hyperfibrinolysis detected by the biomarker levels but not rotational thromboelastometry, while 5% had severe hyperfibrinolysis, detected by the biomarkers and rotational thromboelastometry. The combined hyperfibrinolysis groups had increased 28-day mortality compared to patients without hyperfibrinolysis (12% vs. 1%; p<0.001).21
In the CRASH-2 trial (Clinical Randomization of an Antifibrinolytic in Significant Hemorrhage), adult trauma patients were randomized within 8 hours of injury to a 1 g intravenous loading dose of tranexamic acid followed by a 1 g infusion over 8 hours compared to placebo. The primary outcome was in-hospital 28-day mortality. From 10,060 patients randomized to receive tranexamic acid compared to 10,067 receiving placebo, mortality was reduced with tranexamic acid (14.5 vs. 16.0%; p = 0.0035), and the risk of death due to bleeding was also significantly reduced. Additional analyses of the 35% of patients who died from bleeding reported that the benefit from tranexamic acid was greatest when administered within the first hour of injury, but if given more than 3 hours after injury, mortality was paradoxically increased. Despite the novelty and the results of CRASH-2, the mortality difference of 1.5% was rather small, and statistically significant due to a large number of patient studied. The performance and results of this large trial have been the subject of an intensive controversial debate.86 Only approximately 5% of patients died because of bleeding, and only 50% of patients received blood transfusions. Most of the patients were studied in countries where rapid access to blood products, damage-control surgery, angiography, laboratory testing, and advanced critical care were not available. As there was no difference in the amount of blood transfused between groups, the mechanism of the effect of tranexamic acid on outcomes remains undetermined. Additional trials are underway including Pre-hospital Anti-fibrinolytics for Traumatic Coagulopathy and Hemorrhage (PATCH), a prospective, randomized, placebo-controlled multicenter study that will include 1,200 patients in Australia and New Zealand. Modern trauma care, examination of coagulation, fibrinolysis, transfusion requirements, and incidence of vascular occlusive complications as well as effects on inflammation, immune function and sepsis will be examined to advance knowledge regarding the role of tranexamic acid in trauma. (https://clinicaltrials.gov/ct2/show/NCT02187120)
A post hoc evaluation of CRASH-2, (CRASH-2 IBS) evaluated outcomes in 270 participants with intracranial bleeding. Although either benefits or harmful effects could not be excluded, the results suggested tranexamic acid warranted further research [125]. The ongoing study in the UK (Tranexamic acid in IntraCerebral Hemorrhage – TICH) will include 2,000 participants with a closure date of 2018. The protocol for tranexamic acid /placebo is the same as in CRASH-2. (www.controlled-trial.com/ISRCTN50867461). Another trial in progress is CRASH-3 – tranexamic acid for the treatment of significant traumatic brain injury: (https://clinicaltrials.gov/ct2/show/NCT01402882?term=crash+3&rank=1). Ten thousand patients within 8 h of injury with any intracranial bleeding on computerized tomography will be recruited. Finally, a trial of pre-hospital tranexamic acid treatment in moderate to severe traumatic brain injury is expected to enroll 967 patients (NCT01990768). The trial will randomize patients to three groups dosed by ambulance crews with 1g tranexamic acid, 2g tranexamic acid or placebo.
Fibrinolytic shutdown in trauma
One of the major arguments surrounding the routine use of antifibrinolytic agents in trauma is the concern about fibrinolytic shutdown. As previously mentioned, although hyperfibrinolysis in an important pathologic cause of bleeding, considerable individual variability in the fibrinolytic profile at baseline has been noted. This includes a sub-group with increased circulating plasminogen activator inhibitor -1 and decreased tissue plasminogen activator activity, a profile that is termed fibrinolytic shutdown.14,15
As a result of the recent widespread use of thromboelastography and rotational thromboelastometry in trauma, hyperfibrinolysis has been identified in a subgroup of severely injured patients, and this has been proposed as a contributing cause of bleeding in trauma-induced coagulopathy.87 Acutely injured patients with severe hyperfibrinolysis after 30 minutes based on thromboelastography findings are reported to have mortality rates exceeding 70%.18,22,88 Based on the CRASH-2 trial, many trauma centers throughout the world use tranexamic acid for all major trauma patients. However, among patients with trauma-induced coagulopathy, phenotypic distinction between those with global factor deficiency versus those with hyperfibrinolysis is apparent.14,15 Moore and colleagues hypothesize that tissue injury and hemorrhagic shock produce distinct and opposing phenotypic effects on fibrinolysis, such that untimely inhibition of fibrinolysis in those with fibrinolytic shutdown may result in increased mortality.15 Despite these concerns, we believe the overwhelming safety of antifibrinolytic therapy, the variability of fibrinolytic phenotype at different times after tissue injury for a given individual, and the potential for clotting factor and blood product administration to worsen hypercoagulability continue to make this perspective controversial.
Intracranial Hemorrhage and Neurosurgery
In patients with intracranial hemorrhage, continued bleeding or expansion of the hematoma is a major cause of morbidity and mortality. After a subarachnoid hemorrhage, a recurrence of bleeding within the first 24 hours is reported to occur in 9–17% of patients and is associated with a mortality of ~60%.89,90 Antifibrinolytic therapy after subarachnoid hemorrhage is reported to reduce rebleeding by 35-40%, although outcomes are not improved due to delayed cerebral ischemia following injury, and overall due to adverse effects of intracranial hemorrhage.91,92
A Cochrane review of nine studies between 1973 and 2000 reported that with antifibrinolytic therapy, outcomes were not improved because of cerebral ischemia.91 However, eight of the nine trials were published before 1990, and current standard therapies including calcium channel blockers, and other interventions including triple-H-therapy (hypertension, hypervolemia, and hemodilution) for vasospasm prophylaxis were not used, which might account for the higher number of ischemic events. However, even with current therapies for vasospasm, studies suggest rebleeding is reduced but without benefit on neurologic outcomes.93
In a study from three Swedish hospitals published in 2002 not included in the mentioned Cochrane review, Hillman studied 596 patients with subarachnoid hemorrhage randomized to receive tranexamic acid at 1 g every 6 hours until the aneurysm was clipped, coiled, or secured.94 A total of 70% of aneurysms were treated within 24 hours of admission. Although the study was not blinded, the tranexamic acid treated patients had a lower re-bleeding rate within the first 24 hours of 2.4% vs. 10.8% for controls. Also, re-bleeding occurred in 30 of the 33 patients within the first 8 hours. However, there were only non-significant trends of improved mortality (16.3 vs. 12.9%) and outcomes (Glasgow outcome score 4 or 5: 70.5 vs 74.8%) in the tranexamic acid treated patients, albeit without other concerns for adverse events.94
Starke reported a similar study but with epsilon aminocaproic acid95 in 248 patients with subarachnoid hemorrhage who received a 4 g loading dose followed by a 1 g /hour infusion. A total of 73 patients received epsilon aminocaproic acidwith a lower re-bleeding rate in treated patients of 2.7% compared to 11.4% in controls but with an increased incidence of lower extremity deep vein thrombosis.95
Harrigan retrospectively analyzed 356 patients with subarachnoid hemorrhage treated with epsilon aminocaproic acid on intensive care unit admission.96 Treatment of the ruptured aneurysm occurred an average of 47.4 hours after hospital admission and patients received an average epsilon aminocaproic acid dose of 40.6 g over 35.6 hours. The overall re-bleeding rate was low, 1.4%, and the rate of re-hemorrhage per 24-hour period was 0.71%. Vasospasm occurred in 11.5% of patients, and permanent neurological deficits from ischemic stroke were seen in 7.2%.96
Overall, with the administration of antifibrinolytic therapy to prevent early re-bleeding in subarachnoid hemorrhage, there appears to be no increased risk of ischemic events or adverse outcomes. Despite reduced re-bleeding rates, additional improvement of outcomes with antifibrinolytic agents has not been established, likely due to the complexity of the original bleeding event, neurologic injury, and location of the bleed. Further complicating outcomes are concerns about optimal times to re-start venous thromboembolic prophylaxis in these immobile patients.
Topical administration of tranexamic acid
A recent Cochrane review addressed the topical application of tranexamic acid in a large variety of clinical settings such as cardiac surgery, knee arthroplasty, and spinal surgery.97 The authors concluded that topically administered tranexamic acid may reduce bleeding and transfusions, but expressed concern that safety data, particularly with regard to thromboembolic complications, are unknown. Topical administration of tranexamic acid may lead to lower plasma levels but variability depending on the dose used, the application site, local re-adsorption, and may achieve plasma levels that effectively inhibit systemic hyperfibrinolysis.97
Summary
The use of antifibrinolytic therapy in the perioperative setting has been extensively studied. Most studies report that tranexamic acid and aprotinin are consistently associated with a reduction in bleeding and need for allogeneic transfusions. Despite the extensive use of epsilon aminocaproic acid primarily in the United States, there are far less safety and efficacy data regarding this agent. Although theoretical concerns about the potential for hypercoagulable effects of antifibrinolytic agents remain, the scientific data and clinical experience suggests the relative safety of these agents regarding thromboembolic complications. However, again most of the available data are related to tranexamic acid. In patients undergoing cardiac surgery, the efficacy of tranexamic acid and aprotinin to reduce blood loss and transfusion is established. Although tranexamic acid -associated seizures occur only in cardiac surgical patients, their impact on clinical outcomes needs further investigation. The re-introduction of aprotinin in Europe will be accompanied by a large registry that hopefully will provide more data regarding previously raised safety concerns. In trauma patients, the extensive use of tranexamic acid is based on the CRASH2 study that reported a reduced mortality with early tranexamic acid administration. Controversy regarding fibrinolytic shutdown in a subset of patients with traumatic injury and potential adverse effects of antifibrinolytics has limited routine administration of tranexamic acid in the United States. For orthopedic surgery, antifibrinolytic treatment is associated with clear reductions in bleeding, and variable effects on reduction of allogeneic blood transfusions. There is good evidence for a reduction in transfusion requirements in liver transplantation for both aprotinin and tranexamic acid with no indication of an increased risk of thrombotic complications. The recently published data for the prevention of post-partum hemorrhage with antifibrinolytics are also further supported from the WOMAN study.
Summary Statement.
Fibrinolysis is important for hemostatic balance, but following trauma or surgery may contribute to coagulopathy and bleeding. Antifibrinolytic agents reduce bleeding and transfusions, and tranexamic acid is the agent most extensively studied and administered.
Acknowledgments
Support was provided from institutional and/or departmental sources and NIGMS T32 GM08600, Duke University Medical Center (QQ).
Footnotes
Conflicts of interest:
JHL- serves on steering committees for Boehringer Ingelheim, CSL Behring, Grifols, Instrumentation Labs, and on advisory committees for Leading Biosciences, Octapharma, Pfizer, and Portola
AK- none
QJK- none
TJM- steering committee Portola, consultant CSL Behring
NSK- consultant Bayer, CSL Behring; research support: Baxalta US Inc
References
- 1.Chapin JC, Hajjar KA. Fibrinolysis and the control of blood coagulation. Blood Rev. 2015;29:17–24. doi: 10.1016/j.blre.2014.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Longstaff C, Kolev K. Basic mechanisms and regulation of fibrinolysis. J Thromb Haemost. 2015;13(Suppl 1):S98–105. doi: 10.1111/jth.12935. [DOI] [PubMed] [Google Scholar]
- 3.Wiman B, Collen D. Molecular mechanism of physiological fibrinolysis. Nature. 1978;272:549–50. doi: 10.1038/272549a0. [DOI] [PubMed] [Google Scholar]
- 4.Ilich A, Bokarev I, Key NS. Global assays of fibrinolysis. Int J Lab Hematol. 2017 doi: 10.1111/ijlh.12750. [DOI] [PubMed] [Google Scholar]
- 5.Levy JH. Antifibrinolytic therapy: new data and new concepts. Lancet. 2010;376:3–4. doi: 10.1016/S0140-6736(10)60939-7. [DOI] [PubMed] [Google Scholar]
- 6.Cesarman-Maus G, Hajjar KA. Molecular mechanisms of fibrinolysis. Br J Haematol. 2005;129:307–21. doi: 10.1111/j.1365-2141.2005.05444.x. [DOI] [PubMed] [Google Scholar]
- 7.Chandler WL. The human fibrinolytic system. Crit Rev Oncol Hematol. 1996;24:27–45. doi: 10.1016/1040-8428(96)00206-5. [DOI] [PubMed] [Google Scholar]
- 8.Pasche B, Ouimet H, Francis S, Loscalzo J. Structural changes in platelet glycoprotein IIb/IIIa by plasmin: determinants and functional consequences. Blood. 1994;83:404–14. [PubMed] [Google Scholar]
- 9.Karkouti K, Wijeysundera DN, Yau TM, McCluskey SA, Tait G, Beattie WS. The risk-benefit profile of aprotinin versus tranexamic acid in cardiac surgery. Anesth Analg. 2010;110:21–9. doi: 10.1213/ANE.0b013e3181c0ea6d. [DOI] [PubMed] [Google Scholar]
- 10.Medcalf RL. Fibrinolysis, inflammation, and regulation of the plasminogen activating system. J Thromb Haemost. 2007;5(Suppl 1):132–42. doi: 10.1111/j.1538-7836.2007.02464.x. [DOI] [PubMed] [Google Scholar]
- 11.Syrovets T, Simmet T. Novel aspects and new roles for the serine protease plasmin. Cell Mol Life Sci. 2004;61:873–85. doi: 10.1007/s00018-003-3348-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Levy JH, Greenberg C. Biology of Factor XIII and clinical manifestations of Factor XIII deficiency. Transfusion. 2013;53:1120–31. doi: 10.1111/j.1537-2995.2012.03865.x. [DOI] [PubMed] [Google Scholar]
- 13.Bajzar L, Jain N, Wang P, Walker JB. Thrombin activatable fibrinolysis inhibitor: not just an inhibitor of fibrinolysis. Crit Care Med. 2004;32:S320–4. doi: 10.1097/01.ccm.0000126361.00450.b1. [DOI] [PubMed] [Google Scholar]
- 14.Kluft C, Verheijen JH, Jie AF, Rijken DC, Preston FE, Sue-Ling HM, Jespersen J, Aasen AO. The postoperative fibrinolytic shutdown: a rapidly reverting acute phase pattern for the fast-acting inhibitor of tissue-type plasminogen activator after trauma. Scand J Clin Lab Invest. 1985;45:605–10. doi: 10.3109/00365518509155267. [DOI] [PubMed] [Google Scholar]
- 15.Moore HB, Moore EE, Gonzalez E, Chapman MP, Chin TL, Silliman CC, Banerjee A, Sauaia A. Hyperfibrinolysis, physiologic fibrinolysis, and fibrinolysis shutdown: the spectrum of postinjury fibrinolysis and relevance to antifibrinolytic therapy. J Trauma Acute Care Surg. 2014;77:811–7. doi: 10.1097/TA.0000000000000341. discussion 817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moore EE, Moore HB, Gonzalez E, Chapman MP, Hansen KC, Sauaia A, Silliman CC, Banerjee A. Postinjury fibrinolysis shutdown: Rationale for selective tranexamic acid. J Trauma Acute Care Surg. 2015;78:S65–9. doi: 10.1097/TA.0000000000000634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moore EE, Moore HB, Gonzalez E, Sauaia A, Banerjee A, Silliman CC. Rationale for the selective administration of tranexamic acid to inhibit fibrinolysis in the severely injured patient. Transfusion. 2016;56(Suppl 2):S110–4. doi: 10.1111/trf.13486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schochl H, Frietsch T, Pavelka M, Jambor C. Hyperfibrinolysis after major trauma: differential diagnosis of lysis patterns and prognostic value of thrombelastometry. J Trauma. 2009;67:125–31. doi: 10.1097/TA.0b013e31818b2483. [DOI] [PubMed] [Google Scholar]
- 19.Chapman MP, Moore EE, Ramos CR, Ghasabyan A, Harr JN, Chin TL, Stringham JR, Sauaia A, Silliman CC, Banerjee A. Fibrinolysis greater than 3% is the critical value for initiation of antifibrinolytic therapy. J Trauma Acute Care Surg. 2013;75:961–7. doi: 10.1097/TA.0b013e3182aa9c9f. discussion 967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Theusinger OM, Levy JH. Point of care devices for assessing bleeding and coagulation in the trauma patient. Anesthesiol Clin. 2013;31:55–65. doi: 10.1016/j.anclin.2012.10.006. [DOI] [PubMed] [Google Scholar]
- 21.Raza I, Davenport R, Rourke C, Platton S, Manson J, Spoors C, Khan S, De’Ath HD, Allard S, Hart DP, Pasi KJ, Hunt BJ, Stanworth S, MacCallum PK, Brohi K. The incidence and magnitude of fibrinolytic activation in trauma patients. J Thromb Haemost. 2013;11:307–14. doi: 10.1111/jth.12078. [DOI] [PubMed] [Google Scholar]
- 22.Cotton BA, Harvin JA, Kostousouv V, Minei KM, Radwan ZA, Schochl H, Wade CE, Holcomb JB, Matijevic N. Hyperfibrinolysis at admission is an uncommon but highly lethal event associated with shock and prehospital fluid administration. J Trauma Acute Care Surg. 2012;73:365–70. doi: 10.1097/TA.0b013e31825c1234. discussion 370. [DOI] [PubMed] [Google Scholar]
- 23.Tengborn L, Blomback M, Berntorp E. Tranexamic acid–an old drug still going strong and making a revival. Thromb Res. 2015;135:231–42. doi: 10.1016/j.thromres.2014.11.012. [DOI] [PubMed] [Google Scholar]
- 24.Kim H, Szlam F, Tanaka KA, van de Locht A, Ogawa S, Levy JH. The Effects of MDCO-2010, a Serine Protease Inhibitor, on Activated Clotting Time in Blood Obtained from Volunteers and Cardiac Surgical Patients. Anesth Analg. 115:244–52. doi: 10.1213/ANE.0b013e3182576a5a. [DOI] [PubMed] [Google Scholar]
- 25.Sundaram S, Gikakis N, Hack CE, Niewiarowski S, Edmunds LH, Jr, Koneti Rao A, Sun L, Cooper SL, Colman RW. Nafamostat mesilate, a broad spectrum protease inhibitor, modulates platelet, neutrophil and contact activation in simulated extracorporeal circulation. Thromb Haemost. 1996;75:76–82. [PubMed] [Google Scholar]
- 26.Flight SM, Johnson LA, Du QS, Warner RL, Trabi M, Gaffney PJ, Lavin MF, de Jersey J, Masci PP. Textilinin-1, an alternative anti-bleeding agent to aprotinin: Importance of plasmin inhibition in controlling blood loss. Br J Haematol. 2009;145:207–11. doi: 10.1111/j.1365-2141.2009.07605.x. [DOI] [PubMed] [Google Scholar]
- 27.Koster A, Faraoni D, Levy JH. Antifibrinolytic Therapy for Cardiac Surgery: An Update. Anesthesiology. 2015;123:214–21. doi: 10.1097/ALN.0000000000000688. [DOI] [PubMed] [Google Scholar]
- 28.Mojcik CF, Levy JH. Aprotinin and the systemic inflammatory response after cardiopulmonary bypass. Ann Thorac Surg. 2001;71:745–54. doi: 10.1016/s0003-4975(00)02218-9. [DOI] [PubMed] [Google Scholar]
- 29.Day JR, Punjabi PP, Randi AM, Haskard DO, Landis RC, Taylor KM. Clinical inhibition of the seven-transmembrane thrombin receptor (PAR1) by intravenous aprotinin during cardiothoracic surgery. Circulation. 2004;110:2597–600. doi: 10.1161/01.CIR.0000138027.80056.31. [DOI] [PubMed] [Google Scholar]
- 30.Levy JH, Pifarre R, Schaff HV, Horrow JC, Albus R, Spiess B, Rosengart TK, Murray J, Clark RE, Smith P. A multicenter, double-blind, placebo-controlled trial of aprotinin for reducing blood loss and the requirement for donor-blood transfusion in patients undergoing repeat coronary artery bypass grafting. Circulation. 1995;92:2236–44. doi: 10.1161/01.cir.92.8.2236. [DOI] [PubMed] [Google Scholar]
- 31.Spiess BD, Royston D, Levy JH, Fitch J, Dietrich W, Body S, Murkin J, Nadel A. Platelet transfusions during coronary artery bypass graft surgery are associated with serious adverse outcomes. Transfusion. 2004;44:1143–8. doi: 10.1111/j.1537-2995.2004.03322.x. [DOI] [PubMed] [Google Scholar]
- 32.anaesthesia TESoAtfrotpoaic. Aprotinin: is it time to reconsider? European Journal of Anaesthesiology (EJA) 2015;32:591–595. doi: 10.1097/EJA.0000000000000284. [DOI] [PubMed] [Google Scholar]
- 33.Nilsson IM, Andersson L, Bjorkman SE. Epsilon-aminocaproic acid (E-ACA) as a therapeutic agent based on 5 year’s clinical experience. Acta Med Scand Suppl. 1966;448:1–46. [PubMed] [Google Scholar]
- 34.Nilsson IM, Sjoerdsma A, Waldenstrom J. Antifibrinolytic activity and metabolism of 6-aminocaproic acid in man. Lancet. 1960;1:1322–6. doi: 10.1016/s0140-6736(60)92305-9. [DOI] [PubMed] [Google Scholar]
- 35.McNicol GP, Douglas AS. Epsilon-Aminocaproic Acid and Other Inhibitors of Fibrinolysis. Br Med Bull. 1964;20:233–9. doi: 10.1093/oxfordjournals.bmb.a070338. [DOI] [PubMed] [Google Scholar]
- 36.Nilsson IM. Clinical pharmacology of aminocaproic and tranexamic acids. J Clin Pathol Suppl (R Coll Pathol) 1980;14:41–7. [PMC free article] [PubMed] [Google Scholar]
- 37.Seymour BD, Rubinger M. Rhabdomyolysis induced by epsilon-aminocaproic acid. Ann Pharmacother. 1997;31:56–8. doi: 10.1177/106002809703100109. [DOI] [PubMed] [Google Scholar]
- 38.Vanneste JA, van Wijngaarden GK. Epsilon-aminocaproic acid myopathy. Report of a case and literature review. Eur Neurol. 1982;21:242–8. doi: 10.1159/000115487. [DOI] [PubMed] [Google Scholar]
- 39.Eriksson O, Kjellman H, Pilbrant A, Schannong M. Pharmacokinetics of tranexamic acid after intravenous administration to normal volunteers. Eur J Clin Pharmacol. 1974;7:375–80. doi: 10.1007/BF00558210. [DOI] [PubMed] [Google Scholar]
- 40.Andersson L, Nilsoon IM, Colleen S, Granstrand B, Melander B. Role of urokinase and tissue activator in sustaining bleeding and the management thereof with EACA and AMCA. Ann N Y Acad Sci. 1968;146:642–58. doi: 10.1111/j.1749-6632.1968.tb20322.x. [DOI] [PubMed] [Google Scholar]
- 41.Ducloy-Bouthors AS, Jude B, Duhamel A, Broisin F, Huissoud C, Keita-Meyer H, Mandelbrot L, Tillouche N, Fontaine S, Le Goueff F, Depret-Mosser S, Vallet B, Group ES. Susen S. High-dose tranexamic acid reduces blood loss in postpartum haemorrhage. Crit Care. 2011;15:R117. doi: 10.1186/cc10143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Faraoni D, Carlier C, Samama CM, Levy JH, Ducloy-Bouthors AS. Efficacy and safety of tranexamic acid administration for the prevention and/or the treatment of post-partum haemorrhage: a systematic review with meta-analysis. Ann Fr Anesth Reanim. 2014;33:563–71. doi: 10.1016/j.annfar.2014.07.748. [DOI] [PubMed] [Google Scholar]
- 43.Preston JT, Cameron IT, Adams EJ, Smith SK. Comparative study of tranexamic acid and norethisterone in the treatment of ovulatory menorrhagia. Br J Obstet Gynaecol. 1995;102:401–6. doi: 10.1111/j.1471-0528.1995.tb11293.x. [DOI] [PubMed] [Google Scholar]
- 44.Berntorp E, Follrud C, Lethagen S. No increased risk of venous thrombosis in women taking tranexamic acid. Thromb Haemost. 2001;86:714–5. [PubMed] [Google Scholar]
- 45.Aronson DL, Chang P, Kessler CM. Platelet-dependent thrombin generation after in vitro fibrinolytic treatment. Circulation. 1992;85:1706–12. doi: 10.1161/01.cir.85.5.1706. [DOI] [PubMed] [Google Scholar]
- 46.Eisenberg PR, Miletich JP. Induction of marked thrombin activity by pharmacologic concentrations of plasminogen activators in nonanticoagulated whole blood. Thromb Res. 1989;55:635–43. doi: 10.1016/0049-3848(89)90396-4. [DOI] [PubMed] [Google Scholar]
- 47.Eisenberg PR, Miletich JP, Sobel BE, Jaffe AS. Differential effects of activation of prothrombin by streptokinase compared with urokinase and tissue-type plasminogen activator (t-PA) Thromb Res. 1988;50:707–17. doi: 10.1016/0049-3848(88)90329-5. [DOI] [PubMed] [Google Scholar]
- 48.Winters KJ, Santoro SA, Miletich JP, Eisenberg PR. Relative importance of thrombin compared with plasmin-mediated platelet activation in response to plasminogen activation with streptokinase. Circulation. 1991;84:1552–60. doi: 10.1161/01.cir.84.4.1552. [DOI] [PubMed] [Google Scholar]
- 49.Shakur H, Roberts I, Bautista R, Caballero J, Coats T, Dewan Y, El-Sayed H, Gogichaishvili T, Gupta S, Herrera J, Hunt B, Iribhogbe P, Izurieta M, Khamis H, Komolafe E, Marrero MA, Mejia-Mantilla J, Miranda J, Morales C, Olaomi O, Olldashi F, Perel P, Peto R, Ramana PV, Ravi RR, Yutthakasemsunt S. Effects of tranexamic acid on death, vascular occlusive events, and blood transfusion in trauma patients with significant haemorrhage (CRASH-2): a randomised, placebo-controlled trial. Lancet. 2010;376:23–32. doi: 10.1016/S0140-6736(10)60835-5. [DOI] [PubMed] [Google Scholar]
- 50.Sukeik M, Alshryda S, Haddad FS, Mason JM. Systematic review and meta-analysis of the use of tranexamic acid in total hip replacement. J Bone Joint Surg Br. 2011;93:39–46. doi: 10.1302/0301-620X.93B1.24984. [DOI] [PubMed] [Google Scholar]
- 51.Alshryda S, Sarda P, Sukeik M, Nargol A, Blenkinsopp J, Mason JM. Tranexamic acid in total knee replacement: a systematic review and meta-analysis. J Bone Joint Surg Br. 2011;93:1577–85. doi: 10.1302/0301-620X.93B12.26989. [DOI] [PubMed] [Google Scholar]
- 52.Alshryda S, Sukeik M, Sarda P, Blenkinsopp J, Haddad FS, Mason JM. A systematic review and meta-analysis of the topical administration of tranexamic acid in total hip and knee replacement. Bone Joint J. 2014;96-B:1005–15. doi: 10.1302/0301-620X.96B8.33745. [DOI] [PubMed] [Google Scholar]
- 53.Ross J, Al-Shahi Salman R. The frequency of thrombotic events among adults given antifibrinolytic drugs for spontaneous bleeding: systematic review and meta-analysis of observational studies and randomized trials. Curr Drug Saf. 2012;7:44–54. doi: 10.2174/157488612800492744. [DOI] [PubMed] [Google Scholar]
- 54.Kagoma YK, Crowther MA, Douketis J, Bhandari M, Eikelboom J, Lim W. Use of antifibrinolytic therapy to reduce transfusion in patients undergoing orthopedic surgery: a systematic review of randomized trials. Thromb Res. 2009;123:687–96. doi: 10.1016/j.thromres.2008.09.015. [DOI] [PubMed] [Google Scholar]
- 55.Molenaar IQ, Warnaar N, Groen H, Tenvergert EM, Slooff MJ, Porte RJ. Efficacy and safety of antifibrinolytic drugs in liver transplantation: a systematic review and meta-analysis. Am J Transplant. 2007;7:185–94. doi: 10.1111/j.1600-6143.2006.01591.x. [DOI] [PubMed] [Google Scholar]
- 56.Foley JH. Plasmin(ogen) at the Nexus of Fibrinolysis, Inflammation, and Complement. Semin Thromb Hemost. 2017;43:135–142. doi: 10.1055/s-0036-1592302. [DOI] [PubMed] [Google Scholar]
- 57.Syrovets T, Jendrach M, Rohwedder A, Schule A, Simmet T. Plasmin-induced expression of cytokines and tissue factor in human monocytes involves AP-1 and IKKbeta-mediated NF-kappaB activation. Blood. 2001;97:3941–50. doi: 10.1182/blood.v97.12.3941. [DOI] [PubMed] [Google Scholar]
- 58.Burysek L, Syrovets T, Simmet T. The serine protease plasmin triggers expression of MCP-1 and CD40 in human primary monocytes via activation of p38 MAPK and janus kinase (JAK)/STAT signaling pathways. J Biol Chem. 2002;277:33509–17. doi: 10.1074/jbc.M201941200. [DOI] [PubMed] [Google Scholar]
- 59.Gong Y, Hart E, Shchurin A, Hoover-Plow J. Inflammatory macrophage migration requires MMP-9 activation by plasminogen in mice. J Clin Invest. 2008;118:3012–24. doi: 10.1172/JCI32750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Later AF, Sitniakowsky LS, van Hilten JA, van de Watering L, Brand A, Smit NP, Klautz RJ. Antifibrinolytics attenuate inflammatory gene expression after cardiac surgery. J Thorac Cardiovasc Surg. 2013;145:1611–6. 1616 e1–4. doi: 10.1016/j.jtcvs.2012.11.042. [DOI] [PubMed] [Google Scholar]
- 61.Renckens R, Weijer S, de Vos AF, Pater JM, Meijers JC, Hack CE, Levi M, van der Poll T. Inhibition of plasmin activity by tranexamic acid does not influence inflammatory pathways during human endotoxemia. Arterioscler Thromb Vasc Biol. 2004;24:483–8. doi: 10.1161/01.ATV.0000118280.95422.48. [DOI] [PubMed] [Google Scholar]
- 62.Horrow JC, Van Riper DF, Strong MD, Grunewald KE, Parmet JL. The dose-response relationship of tranexamic acid. Anesthesiology. 1995;82:383–92. doi: 10.1097/00000542-199502000-00009. [DOI] [PubMed] [Google Scholar]
- 63.Fiechtner BK, Nuttall GA, Johnson ME, Dong Y, Sujirattanawimol N, Oliver WC, Jr, Sarpal RS, Oyen LJ, Ereth MH. Plasma tranexamic acid concentrations during cardiopulmonary bypass. Anesth Analg. 2001;92:1131–6. doi: 10.1097/00000539-200105000-00010. [DOI] [PubMed] [Google Scholar]
- 64.Dowd NP, Karski JM, Cheng DC, Carroll JA, Lin Y, James RL, Butterworth J. Pharmacokinetics of tranexamic acid during cardiopulmonary bypass. Anesthesiology. 2002;97:390–9. doi: 10.1097/00000542-200208000-00016. [DOI] [PubMed] [Google Scholar]
- 65.Sharma V, Fan J, Jerath A, Pang KS, Bojko B, Pawliszyn J, Karski JM, Yau T, McCluskey S, Wasowicz M. Pharmacokinetics of tranexamic acid in patients undergoing cardiac surgery with use of cardiopulmonary bypass. Anaesthesia. 2012;67:1242–50. doi: 10.1111/j.1365-2044.2012.07266.x. [DOI] [PubMed] [Google Scholar]
- 66.Murkin JM, Falter F, Granton J, Young B, Burt C, Chu M. High-dose tranexamic acid is associated with nonischemic clinical seizures in cardiac surgical patients. Anesth Analg. 2009;110:350–3. doi: 10.1213/ANE.0b013e3181c92b23. [DOI] [PubMed] [Google Scholar]
- 67.Lecker I, Wang DS, Romaschin AD, Peterson M, Mazer CD, Orser BA. Tranexamic acid concentrations associated with human seizures inhibit glycine receptors. J Clin Invest. 2012;122:4654–66. doi: 10.1172/JCI63375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Myles PS, Smith JA, Forbes A, Silbert B, Jayarajah M, Painter T, Cooper DJ, Marasco S, McNeil J, Bussieres JS, McGuinness S, Byrne K, Chan MT, Landoni G, Wallace S, Network AIotACT Tranexamic Acid in Patients Undergoing Coronary-Artery Surgery. N Engl J Med. 2017;376:136–148. doi: 10.1056/NEJMoa1606424. [DOI] [PubMed] [Google Scholar]
- 69.Myles PS, Smith JA, Forbes A, Silbert B, Jayarajah M, Painter T, Cooper DJ, Marasco S, McNeil J, Bussieres JS, McGuinness S, Byrne K, Chan MT, Landoni G, Wallace S, Network AIotACT Tranexamic Acid in Patients Undergoing Coronary-Artery Surgery. N Engl J Med. 2016 [Google Scholar]
- 70.Koster A, Levy JH. Understanding potential drug side effects: can we translate molecular mechanisms to clinical applications? Anesthesiology. 2017;127:6–8. doi: 10.1097/ALN.0000000000001666. [DOI] [PubMed] [Google Scholar]
- 71.Takagi H, Ando T, Umemoto T, All-Literature Investigation of Cardiovascular Evidence g Seizures associated with tranexamic acid for cardiac surgery: a meta-analysis of randomized and non-randomized studies. J Cardiovasc Surg (Torino) 2017;58:633–641. doi: 10.23736/S0021-9509.17.09877-9. [DOI] [PubMed] [Google Scholar]
- 72.Maeda T, Sasabuchi Y, Matsui H, Ohnishi Y, Miyata S, Yasunaga H. Safety of Tranexamic Acid in Pediatric Cardiac Surgery: A Nationwide Database Study. J Cardiothorac Vasc Anesth. 2017;31:549–553. doi: 10.1053/j.jvca.2016.10.001. [DOI] [PubMed] [Google Scholar]
- 73.Roullet S, Pillot J, Freyburger G, Biais M, Quinart A, Rault A, Revel P, Sztark F. Rotation thromboelastometry detects thrombocytopenia and hypofibrinogenaemia during orthotopic liver transplantation. Br J Anaesth. 2010;104:422–8. doi: 10.1093/bja/aeq022. [DOI] [PubMed] [Google Scholar]
- 74.Porte RJ, Molenaar IQ, Begliomini B, Groenland TH, Januszkiewicz A, Lindgren L, Palareti G, Hermans J, Terpstra OT. Aprotinin and transfusion requirements in orthotopic liver transplantation: a multicentre randomised double-blind study. EMSALT Study Group. Lancet. 2000;355:1303–9. doi: 10.1016/s0140-6736(00)02111-5. [DOI] [PubMed] [Google Scholar]
- 75.Dalmau A, Sabate A, Acosta F, Garcia-Huete L, Koo M, Sansano T, Rafecas A, Figueras J, Jaurrieta E, Parrilla P. Tranexamic acid reduces red cell transfusion better than epsilon-aminocaproic acid or placebo in liver transplantation. Anesth Analg. 2000;91:29–34. doi: 10.1097/00000539-200007000-00006. [DOI] [PubMed] [Google Scholar]
- 76.Wu CC, Ho WM, Cheng SB, Yeh DC, Wen MC, Liu TJ, P’Eng FK. Perioperative parenteral tranexamic acid in liver tumor resection: a prospective randomized trial toward a “blood transfusion”-free hepatectomy. Ann Surg. 2006;243:173–80. doi: 10.1097/01.sla.0000197561.70972.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Zufferey P, Merquiol F, Laporte S, Decousus H, Mismetti P, Auboyer C, Samama CM, Molliex S. Do antifibrinolytics reduce allogeneic blood transfusion in orthopedic surgery? Anesthesiology. 2006;105:1034–46. doi: 10.1097/00000542-200611000-00026. [DOI] [PubMed] [Google Scholar]
- 78.Tan J, Chen H, Liu Q, Chen C, Huang W. A meta-analysis of the effectiveness and safety of using tranexamic acid in primary unilateral total knee arthroplasty. J Surg Res. 2013;184:880–7. doi: 10.1016/j.jss.2013.03.099. [DOI] [PubMed] [Google Scholar]
- 79.Li ZJ, Fu X, Xing D, Zhang HF, Zang JC, Ma XL. Is tranexamic acid effective and safe in spinal surgery? A meta-analysis of randomized controlled trials. Eur Spine J. 2013;22:1950–7. doi: 10.1007/s00586-013-2774-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Churchill JL, Puca KE, Meyer ES, Carleton MC, Truchan SL, Anderson MJ. Comparison of epsilon-Aminocaproic Acid and Tranexamic Acid in Reducing Postoperative Transfusions in Total Hip Arthroplasty. J Arthroplasty. 2016;31:2795–2799 e1. doi: 10.1016/j.arth.2016.05.011. [DOI] [PubMed] [Google Scholar]
- 81.Churchill JL, Puca KE, Meyer E, Carleton M, Truchan SL, Anderson MJ. Comparing epsilon-Aminocaproic Acid and Tranexamic Acid in Reducing Postoperative Transfusions in Total Knee Arthroplasty. J Knee Surg. 2016 doi: 10.1055/s-0036-1593362. [DOI] [PubMed] [Google Scholar]
- 82.Zufferey PJ, Lanoiselee J, Chapelle C, Borisov DB, Bien JY, Lambert P, Philippot R, Molliex S, Delavenne X, investigators of the PeriOpeRative Tranexamic acid in hip arthrOplasty S Intravenous Tranexamic Acid Bolus plus Infusion Is Not More Effective than a Single Bolus in Primary Hip Arthroplasty: A Randomized Controlled Trial. Anesthesiology. 2017;127:413–422. doi: 10.1097/ALN.0000000000001787. [DOI] [PubMed] [Google Scholar]
- 83.Novikova N, Hofmeyr GJ. Tranexamic acid for preventing postpartum haemorrhage. Cochrane Database Syst Rev. 2010:CD007872. doi: 10.1002/14651858.CD007872.pub2. [DOI] [PubMed] [Google Scholar]
- 84.Roberts I, Ker K. Tranexamic acid for postpartum bleeding. Int J Gynaecol Obstet. 2011;115:220–1. doi: 10.1016/j.ijgo.2011.09.001. [DOI] [PubMed] [Google Scholar]
- 85.Collaborators WT. Effect of early tranexamic acid administration on mortality, hysterectomy, and other morbidities in women with post-partum haemorrhage (WOMAN): an international, randomised, double-blind, placebo-controlled trial. Lancet. 2017;389:2105–2116. doi: 10.1016/S0140-6736(17)30638-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Binz S, McCollester J, Thomas S, Miller J, Pohlman T, Waxman D, Shariff F, Tracy R, Walsh M. CRASH-2 Study of Tranexamic Acid to Treat Bleeding in Trauma Patients: A Controversy Fueled by Science and Social Media. J Blood Transfus. 2015;2015:874920. doi: 10.1155/2015/874920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Chang R, Cardenas JC, Wade CE, Holcomb JB. Advances in the understanding of trauma-induced coagulopathy. Blood. 2016;128:1043–9. doi: 10.1182/blood-2016-01-636423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ives C, Inaba K, Branco BC, Okoye O, Schochl H, Talving P, Lam L, Shulman I, Nelson J, Demetriades D. Hyperfibrinolysis elicited via thromboelastography predicts mortality in trauma. J Am Coll Surg. 2012;215:496–502. doi: 10.1016/j.jamcollsurg.2012.06.005. [DOI] [PubMed] [Google Scholar]
- 89.Starke RM, Connolly ES, Jr, Participants in the International Multi-Disciplinary Consensus Conference on the Critical Care Management of Subarachnoid H Rebleeding after aneurysmal subarachnoid hemorrhage. Neurocrit Care. 2011;15:241–6. doi: 10.1007/s12028-011-9581-0. [DOI] [PubMed] [Google Scholar]
- 90.Rosenorn J, Eskesen V, Schmidt K, Ronde F. The risk of rebleeding from ruptured intracranial aneurysms. J Neurosurg. 1987;67:329–32. doi: 10.3171/jns.1987.67.3.0329. [DOI] [PubMed] [Google Scholar]
- 91.Roos Y, Rinkel G, Vermeulen M, Algra A, van Gijn J. Antifibrinolytic therapy for aneurysmal subarachnoid hemorrhage: a major update of a cochrane review. Stroke. 2003;34:2308–9. doi: 10.1161/01.STR.0000089030.04120.0E. [DOI] [PubMed] [Google Scholar]
- 92.Baharoglu MI, Germans MR, Rinkel GJ, Algra A, Vermeulen M, van Gijn J, Roos YB. Antifibrinolytic therapy for aneurysmal subarachnoid haemorrhage. Cochrane Database Syst Rev. 2013:CD001245. doi: 10.1002/14651858.CD001245.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Roos Y. Antifibrinolytic treatment in subarachnoid hemorrhage: a randomized placebo-controlled trial. STAR Study Group. Neurology. 2000;54:77–82. doi: 10.1212/wnl.54.1.77. [DOI] [PubMed] [Google Scholar]
- 94.Hillman J, Fridriksson S, Nilsson O, Yu Z, Saveland H, Jakobsson KE. Immediate administration of tranexamic acid and reduced incidence of early rebleeding after aneurysmal subarachnoid hemorrhage: a prospective randomized study. J Neurosurg. 2002;97:771–8. doi: 10.3171/jns.2002.97.4.0771. [DOI] [PubMed] [Google Scholar]
- 95.Starke RM, Kim GH, Fernandez A, Komotar RJ, Hickman ZL, Otten ML, Ducruet AF, Kellner CP, Hahn DK, Chwajol M, Mayer SA, Connolly ES., Jr Impact of a protocol for acute antifibrinolytic therapy on aneurysm rebleeding after subarachnoid hemorrhage. Stroke. 2008;39:2617–21. doi: 10.1161/STROKEAHA.107.506097. [DOI] [PubMed] [Google Scholar]
- 96.Harrigan MR, Rajneesh KF, Ardelt AA, Fisher WS., 3rd Short-term antifibrinolytic therapy before early aneurysm treatment in subarachnoid hemorrhage: effects on rehemorrhage, cerebral ischemia, and hydrocephalus. Neurosurgery. 2010;67:935–9. doi: 10.1227/NEU.0b013e3181ebaa36. discussion 939-40. [DOI] [PubMed] [Google Scholar]
- 97.Ker K, Beecher D, Roberts I. Topical application of tranexamic acid for the reduction of bleeding. Cochrane Database Syst Rev. 2013:CD010562. doi: 10.1002/14651858.CD010562.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]


