Abstract
Introduction
Over 8,500 United States Coast Guard (USCG) personnel were deployed in response to the Deepwater Horizon (DWH) oil spill; however, human respiratory effects as a result of spill-related exposures are relatively unknown.
Methods
USCG personnel who responded to the DWH oil spill were queried via survey on exposures to crude oil and oil dispersant, and acute respiratory symptoms experienced during deployment. Adjusted log binomial regressions were used to calculate prevalence ratios (PRs) and 95% confidence intervals (CI), investigating the associations between oil spill exposures and respiratory symptoms.
Results
4,855 USCG personnel completed the survey. More than half (54.6%) and almost one-fourth (22.0%) of responders were exposed to crude oil and oil dispersants, respectively. Coughing was the most prevalent symptom (19.4%), followed by shortness of breath (5.5%), and wheezing (3.6%). Adjusted analyses showed an exposure-response relationship between increasing deployment duration and likelihood of coughing, shortness of breath, and wheezing in the pre-capping period. A similar pattern was observed in the post-capping period for coughing and wheezing. Adjusted analyses revealed increased PRs for coughing (PR=1.92), shortness of breath (PR=2.60), and wheezing (PR=2.68) for any oil exposure. Increasing frequency of inhalation of oil was associated with increased likelihood of all three respiratory symptoms. A similar pattern was observed for dermal contact with oil dispersants for coughing and shortness of breath. The combination of both oil and oil dispersants presented associations that were much greater in magnitude than oil alone for coughing (PR=2.72), shortness of breath (PR=4.65), and wheezing (PR=5.06).
Conclusions
Results from the present study suggested strong relationships between oil and oil dispersant exposures and acute respiratory symptoms among disaster responders. Future prospective studies will be needed to confirm these findings.
Keywords: crude oil, oil dispersants, respiratory symptoms, Deepwater Horizon, oil spill
Introduction
On April 20th, 2010, the Deepwater Horizon (DWH) drilling rig exploded, resulting in the release of approximately 200 million gallons of crude oil into the Gulf of Mexico over the next three months, making this the largest marine oil spill in U.S. history(United States Coast Guard 2011). Additionally, nearly 2 million gallons of oil dispersants (mainly Corexit 9500 and 9527A) were used in clean-up efforts. The United States Coast Guard (USCG) led the interagency response and coordinated clean-up activities, deploying over 8,500 USCG personnel as responders.
A Health Hazard Evaluation Report of the DWH oil spill carried out by the Centers for Disease Control and Prevention (CDC) concluded that responders faced chemical exposures from crude oil and its components, dispersants used to break down the crude oil in the water, and in situ burning of crude oil (King and Gibbins 2011). However, relatively little is understood about the human health effects from these exposures. Limited prior epidemiological studies have identified a number of acute physical, psychological, genotoxic, and endocrine effects in exposed populations (Aguilera et al. 2010; Laffon et al. 2016; Ordinioha and Sawyer 2010). These observed effects may be due to the range of chemical agents encountered during oil spills (Ha et al. 2012). For example, crude oil typically contains volatile organic compounds (VOCs) such as benzene, toluene, ethylbenzene, and xylenes, polycyclic aromatic hydrocarbons (PAHs), and heavy metals (Liu et al. 2012). Inhalation of VOCs, in particular, is associated with respiratory symptoms such as respiratory tract irritation and bronchitis (Hulin et al. 2012). Further, as inhalation is the major route of exposure for many of these chemicals in the context of an oil spill, it is not surprising that prior epidemiological studies have shown an increased prevalence of respiratory symptoms in residents and clean-up workers immediately after exposure to an oil spill (Janjua et al. 2006; S Meo et al. 2009; SA Meo et al. 2009; Peres et al. 2016), and that these effects may be prolonged after the spill (Rodriguez-Trigo et al. 2010; Zock et al. 2007; Zock et al. 2012).
Components of two primary dispersants used in the DWH response included propylene glycol and 2-butoxyethanol, which have been linked to respiratory irritation in both humans and animals (Agency for Toxic Substances and Disease Registry 1997, 1998; Wieslander et al. 2001). After treatment with the dispersants Corexit 9500 and 9572A alone or in combination with crude oil, studies in animal models have observed cell death and formation of reactive oxygen species in airway epithelial cells (Shi et al. 2013; Wang et al. 2012) and observed breathing difficulty (Roberts et al. 2011). A study recently published from the GuLF STUDY cohort (Kwok et al. 2017) found that potential exposure to either of these dispersants was significantly associated with respiratory symptoms (e.g., cough, wheeze, tightness of chest, and shortness of breath). (McGowan et al. 2017) In another recent study, Liu et al reported that Corexit 9527A appeared to act synergistically with crude oil in altering gene expression in human airway epithelial cells in vitro (Liu et al. 2016).
Though previous epidemiological studies have characterized respiratory health symptoms after oil spills, important gaps in our knowledge remain. Most of these previous studies have relied on proxies of exposure to crude oil, such as whether or not an individual participated in the cleanup, their duration of clean-up work, or proximity to the oil spill (Aguilera et al. 2010; Laffon et al. 2016; Ordinioha and Sawyer 2010). Also, these studies were limited in sample size, and were unable to identify vulnerable subgroups through stratification of relevant factors. Additionally, few studies have examined the impact of use of personal protective equipment (PPE) on respiratory effects among oil spill clean-up workers (Carrasco et al. 2006; Gwack et al. 2012; Lee et al. 2009; Sim et al. 2010; Suarez et al. 2005; Zock et al. 2007), which could provide valuable guidance on reducing risk among these disaster workers.
Considering the paucity of data on crude oil, oil dispersants in general, use of PPE in responders and their association with respiratory health symptoms, along with the increasing number of oil spills in recent decades (Aguilera et al. 2010), the present study is positioned to fill important gaps in knowledge. Using a cross-sectional design, this study aims to examine the association between specific exposures encountered during oil spill clean-up work (crude oil/oily water and oil dispersants) and acute respiratory symptoms.
Methods
Study Population
The current cross-sectional study was based on data from the DWH Oil Spill Responder Coast Guard cohort, which has been previously described (Rusiecki et al. 2017). Briefly, 8,696 USCG responders who worked at least one day on the DWH oil spill response were identified via USCG administrative databases. Among these responders, 4,855 (55.8%) completed an exit survey that queried information related to their deployment (timing, duration, missions), relevant exposures (crude oil, oil dispersants, exhaust fumes), health symptoms, PPE use, and lifestyle factors. All responders who completed this survey were included in the current analysis. This study was approved by the Institutional Review Boards of the Uniformed Services University, The United States Coast Guard, and The University of North Carolina, Chapel Hill.
Exposure Assessment
Responders reported the deployment dates and duration of their DWH oil spill response in the exit survey. Frequency of exposure to crude oil/oily water was assessed via a 5 point Likert scale for each of four specific routes of exposure: inhalation, direct skin contact, ingestion, and submersion (e.g., “How often were you exposed to crude oil/oily water via inhalation/direct skin contact/ingestion/submersion?”). The present analyses focused on exposure to crude oil/oily water via inhalation. Frequency of exposure to oil dispersants was assessed via a 5 point Likert scale based on the question: “How often did you personally handle, apply, or come in contact with oil dispersants?”
Assessment of Acute Respiratory Symptoms
The acute respiratory symptoms assessed in the exit survey- coughing, shortness of breath, spitting up of blood, and wheezing - were reported by participants on a three-point scale: “Most of the time,” “Sometimes,” and “Never.” The current study focused on coughing, shortness of breath, and wheezing; spitting up of blood was dropped from analyses because it was reported by a low number of responders (n = 11).
Statistical Analyses
Cross-sectional analyses of the exit survey exposure and health data were carried out in order to investigate the association between oil spill clean-up exposures of interest and acute respiratory symptoms. Responders with multiple deployments (n=292) represented a small proportion of the cross-sectional study; therefore, analyses were limited to individuals’ first deployment only.
The effect of deployment length on respiratory health symptoms was evaluated. Deployment length was categorized into a three-level variable: less than or equal to 30 days, more than 30 days and less than or equal to 60 days, and more than 60 days. Because the oil well was capped on July 15, 2010 and exposure to fresh oil and other cleanup-related stressors likely changed after this date, timing of response (April 20th 2010 – July 15th, 2010 vs. after July 15th, 2010) was examined jointly with duration of response in relation to respiratory health symptoms; thus models were stratified by period of response in relation to the capping of the well. Responders were classified as being deployed pre- or post-capping of the well according to the start date of their deployment. The post-capping period was truncated on September 30th, 2010 to exclude respiratory symptoms that might have been due to seasonal respiratory infections.
For exposure to crude oil/oily water exposure via inhalation and direct skin contact with oil dispersant exposures, a three-level variable was created: none, low, or high. The three-level categorical variables (none, low, high) for inhalation of crude oil exposure and oil dispersant were generated by combining “Rarely” and “Sometimes” into a “Low” category and “Most of the Time” and “All of the Time” into a “High” category. Finally, a general crude oil/oily water exposure variable, regardless of exposure route, was created as an ever/never variable, where indication of any exposure to oil via inhalation, direct skin contact, submersion, or ingestion was identified as “ever” exposed to oil. Respiratory health effects were analyzed by combining “Sometimes” and “Most of the Time” into an “Ever” category.
To avoid overestimation of effects due to non-rarity of the outcomes (Barros and Hirakata 2003), adjusted log binomial regression was used to investigate associations between exposures to crude oil/oily water and oil dispersants and respiratory health effects to yield prevalence ratios (PR) and corresponding 95% confidence intervals (CIs). In the event of non-convergence in the log-binomial model, the COPY method was used with 1,000,000 copies (Deddens and Petersen 2008).
To create the final adjusted models, a base model was constructed using the most frequently-reported respiratory health outcome (coughing) as the dependent variable, with the following variables selected a priori as potential confounders: age, gender, engine exhaust exposure, dispersant exposure, and smoking during deployment. If a potential confounder changed the estimate of association between the oil exposure index and coughing by greater than 10%, it was retained in the final model. Confounders identified in this method were retained for other models that examined the other respiratory health effects and other crude oil/oily water exposures. Final adjusted models for crude oil/oily water analyses included age, exhaust exposure, and smoking during deployment. Models for inhalation of crude oil/oily water were adjusted for these variables as well, additionally adjusting for direct skin contact with crude oil/oily water. A similar method was implemented when building adjusted models for oil dispersant exposure. Age, exhaust exposure, ever exposure to oil, and smoking during deployment were included in final adjusted models for oil dispersants. To test for trend, exposure frequency categories were modeled as a continuous variable.
Sensitivity analyses were carried out to examine the robustness of main findings. For oil analyses, responders who indicated that they were exposed to oil dispersants were excluded. For oil dispersant analyses, those who indicated that they were exposed to dispersant but not also to oil were excluded from analyses to reduce possible reporting error.
Stratified analyses were carried out for both oil exposures and for dispersant exposures, based on a priori factors. Models examining ever/never exposure to oil were stratified by individuals’ use of any oil exposure-reducing PPE (yes vs. no), use of respirators specifically (yes vs. no), smoking status (yes vs. no), timing of deployment (before vs. after well capping on July 15th, 2010), dispersant exposure, and combustion engine exhaust exposure. Models for ever/never dispersant contact were stratified by dispersant PPE use (yes vs. no), smoking status, and capping period.
Because we wanted to understand the effects of oil dispersants within the context of an oil spill setting, responders reported only being exposed to oil dispersants were excluded from further analyses (N = 95). Therefore, the combined effects of exposure to crude oil and dispersant on acute respiratory symptoms were examined by calculating PRs and 95% CIs for: 1) responders who reported only oil exposure compared to those who reported neither oil nor oil dispersant exposure, and 2) responders who reported both oil dispersant and any oil exposure compared to those who reported neither exposure.
All analyses were carried out using SAS Version 9.3 (SAS Institute 2012).
Results
A total of 4,855 responders were included in the present analyses. Table 1 provides the distribution of demographic characteristics, oil exposures, and acute respiratory symptoms. The majority of responders were active duty (n = 3,102; 63.9%), enlisted (n = 3,530; 72.7%), grade E1–E10 (n = 3,544; 73.0%), younger than 34 years of age (n = 2,955; 60.9%), male (n = 4,127; 85.0%, white (n = 3,741; 77.1%), and had a maximum educational attainment of graduating high school or equivalent (n = 2,715; 55.9%). Over half of responders reported ever exposure to oil (n = 2,651; 54.6%). Over half of responders reported exposure to crude oil via inhalation (n = 2,478; 51.0%), and over one-third reported direct skin contact with crude oil/oily water (n = 1,696; 34.9%). A total of 1,068 (22.0%) responders reported contact with oil dispersants. The most common acute respiratory symptom was coughing (n = 942; 19.4%), followed by shortness of breath (n = 265; 5.5%), and wheezing (n = 173; 3.6%).
Table 1.
Distribution of demographics, exposures, and respiratory symptoms of surveyed responders of the Deepwater Horizon oil spill
| Responders who took a survey N=4,855 |
||
|---|---|---|
| Characteristic | N | % |
| Employee Class | ||
| Active Duty | 3102 | 63.89 |
| Selected Reserve | 1753 | 36.11 |
| Employee Type | ||
| Enlisted | 3530 | 72.71 |
| Officer | 1311 | 27.00 |
| Other (Cadet/Unknown) | 14 | 0.29 |
| Grade | ||
| E1–E5 | 2233 | 45.99 |
| E6–E10 | 1311 | 27.00 |
| O1–O4, W2–W4 | 1128 | 23.23 |
| O5–O10 | 183 | 3.77 |
| Age Group | ||
| Less than 25 years old | 827 | 17.03 |
| 25 – 34 years old | 2128 | 43.83 |
| 35 – 50 years old | 1738 | 35.80 |
| Older than 50 | 162 | 3.34 |
| Gender | ||
| Male | 4127 | 85.01 |
| Female | 728 | 14.99 |
| Ethnic Group | ||
| White | 3741 | 77.05 |
| Black or African American | 203 | 4.18 |
| Asian/AI/AN/NH/PI | 182 | 3.75 |
| Other | 242 | 4.98 |
| Unknown | 487 | 10.03 |
| Educational Attainment | ||
| Less Than HS Graduate | 25 | 0.51 |
| HS Graduate or Equivalent | 2715 | 55.92 |
| Some College/Technical School | 870 | 17.92 |
| Bachelor’s Level Degree | 905 | 18.64 |
| Master’s Level Degree | 188 | 3.87 |
| Doctorate Level Degree | 26 | 0.54 |
| Other or Not Indicated | 126 | 2.60 |
| Any Oil Exposure | ||
| Ever | 2651 | 54.60 |
| Oil Inhalation | ||
| Ever | 2478 | 51.00 |
| Low | 2011 | 41.40 |
| High | 467 | 9.60 |
| Oil Contact | ||
| Ever | 1696 | 34.90 |
| Low | 1559 | 32.10 |
| High | 137 | 2.80 |
| Oil Dispersant Contact | ||
| Ever | 1068 | 22.00 |
| Low | 978 | 20.10 |
| High | 90 | 1.90 |
| Exhaust Inhalation | ||
| Ever | 3660 | 75.40 |
| Low | 2830 | 58.30 |
| High | 830 | 17.10 |
| Respiratory Symptoms | ||
| Coughing | 942 | 19.40 |
| Shortness of Breath | 265 | 5.50 |
| Wheezing | 173 | 3.60 |
Table 2 presents associations between deployment duration and coughing, shortness of breath, and wheezing, after adjustment for age and smoking during deployment and stratified by period of response. During the pre-capping period, an exposure-response relationship between increasing duration and coughing was observed, with ptrend <0.01, and with responders with the longest deployment duration (>60 days) having PR=2.12 (95% CI: 1.75, 2.56). A similar pattern was found for shortness of breath (ptrend: <0.01); again, responders with deployments longer than 60 days had a significantly elevated PR (PR=1.91; 95% CI: 1.34, 2.72). For wheezing, there was suggestion of a possible exposure-response relationship, with ptrend: 0.04, in the pre-capping period; responders with the longest duration had PR=1.69 (95% CI: 1.05, 2.50). There was also evidence of increasing risk of cough with increasing deployment duration in the post-capping period (ptrend: <0.01), with responders with the longest duration having a significantly elevated PR (PR: 2.53). Increased risk of shortness of breath and wheezing was observed among responders with the longest duration of deployment (PR=2.32 (95% CI: 1.09, 4.93) and PR=3.16 (95% CI: 1.38, 7.24), respectively), but with no apparent exposure-response relationship; however, the number of subjects in some exposure groups was small, resulting in imprecise risk estimates.
Table 2.
Adjusted associations between deployment duration and respiratory symptoms stratified by capping period among surveyed responders of the Deepwater Horizon oil spill
| Pre-Capping (N = 3353) | Post-Capping (N = 1258) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||||
| Deployment Duration | N | Prevalence Ratio | 95% CI | ptrend | Deployment Duration | N | Prevalence Ratio | 95% CI | ptrend | ||
|
|
|
||||||||||
| Coughing (N = 637) | <30 days | 146 | ref | -- | Coughing (N = 242) | <30 days | 47 | ref | -- | ||
| 31 to 60 days | 291 | 1.48 | 1.23 – 1.77 | 31 to 60 days | 157 | 1.65 | 1.22 – 2.23 | <0.01 | |||
| ≥60 days | 200 | 2.12 | 1.75 – 2.56 | <0.01 | ≥60 days | 38 | 2.53 | 1.74 – 3.68 | |||
|
|
|
||||||||||
| Shortness of Breath (N = 202) | <30 days | 51 | ref | -- | Shortness of Breath (N = 52) | <30 days | 15 | ref | -- | ||
| 31 to 60 days | 88 | 1.31 | 0.94 – 1.84 | 31 to 60 days | 26 | 0.86 | 0.46 – 1.61 | 0.11 | |||
| ≥60 days | 63 | 1.91 | 1.34 – 2.72 | <0.01 | ≥60 days | 11 | 2.32 | 1.09 – 4.93 | |||
|
|
|
||||||||||
| Wheezing (N = 130) | <30 days | 36 | ref | -- | Wheezing (N = 36) | <30 days | 10 | ref | -- | ||
| 31 to 60 days | 55 | 1.09 | 0.72 – 1.65 | 31 to 60 days | 15 | 0.73 | 0.33 – 1.62 | ||||
| ≥60 days | 39 | 1.61 | 1.04 – 2.50 | 0.04 | ≥60 days | 11 | 3.16 | 1.38 – 7.24 | 0.03 | ||
Note: Deployments that began after September 30, 2010 were excluded to rule out respiratory symptoms that might have been due to seasonal respiratory infections.
Adjusted for: age and smoking during deployment
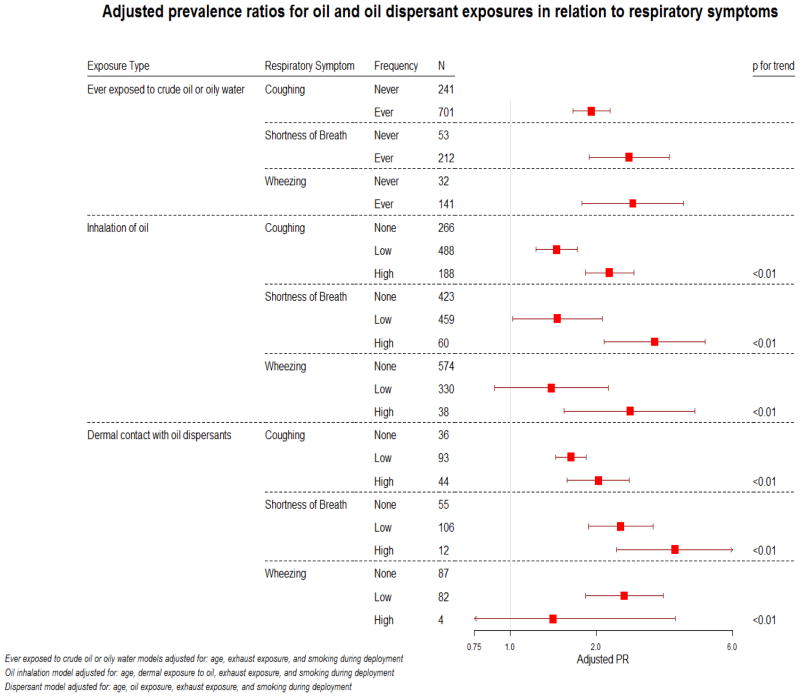
Figure 1 is a graphical representation of adjusted PRs and their corresponding 95% CIs for ever exposure to any crude oil/oily water, and frequencies of inhalation of crude oil/oily water and contact with oil dispersants in relation to the acute respiratory symptoms. Models were additionally adjusted for duration of deployment; however, estimates did not appreciably change (>10%) and thus were not included in the final models. Any oil exposure was associated with a significantly elevated PRs of 1.92 for coughing. Significantly elevated PRs of 2.60 and 2.68 were observed for shortness of breath and wheezing, respectively. For frequency of specific routes of exposures, statistically significant, elevated PRs were found for increasing frequency of oil inhalation exposure (Figure 1) in relation to coughing (PRlow: 1.48, PRhigh: 2.22), shortness of breath (PRlow: 1.46, PRhigh: 3.20), and wheezing (PRlow: 1.39, PRhigh: 2.62); all of which had apparent exposure-response relationships (ptrend < 0.01). Increased frequency of contact with oil dispersants was associated with statistically significant increased PRs for coughing (PRlow: 1.63, PRhigh: 2.03) and shortness of breath (PRlow: 2.43, PRhigh: 3.76), with apparent trends (ptrend < 0.01).
Figure 1.
Adjusted prevalence ratios for oil and oil dispersant exposure in relation to respiratory symptoms.
Sensitivity analyses were carried out for both oil and oil dispersant models. After removal of responders who reported dispersant exposure, the effect of crude oil/oily water on risk of respiratory symptoms was attenuated, but the associations remained significantly elevated (data not shown). Similarly, after removal of responders who did not report oil exposure, exposure to oil dispersants still showed increased PRs for all three respiratory health effects, although the number of exposed subjects was small (data not shown).
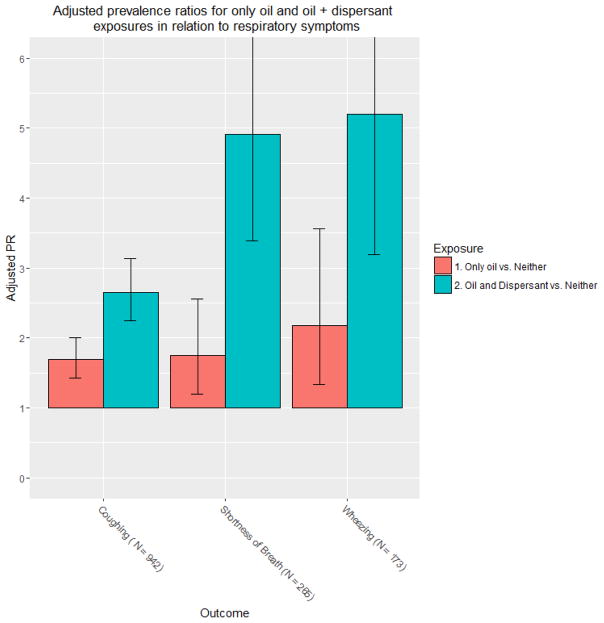
Figure 2 shows adjusted associations for responders exposed to (1) only oil and (2) to both oil and dispersant, compared to responders exposed to neither. Those who reported only oil exposure had elevated PRs for coughing (PR: 1.68; 95% CI: 1.42 – 1.98), shortness of breath (PR: 1.81; 95% CI: 1.24 – 2.64), and wheezing (PR: 2.22; 95% CI: 1.37 – 3.61). Responders with exposure to both oil and oil dispersant had substantially stronger PRs in relation to coughing (PR: 2.72; 95% CI: 2.31 – 3.21), shortness of breath (PR: 4.65; 95% CI: 3.25 – 6.64), and wheezing (PR: 5.06; 95% CI: 3.16 – 8.11).
Figure 2.
Adjusted prevalence ratios for only oil and oil plus dispersant exposure in relation to respiratory symptoms.
Results of stratified analyses of crude oil exposure (ever/never), can be found in Supplementary Table 1. When stratified by use of any oil-related PPE, PRs for all three acute respiratory symptoms were higher among responders who did not report PPE use compared to those who did report PPE use. In a related analysis, a similar pattern was found for responders reporting use of a respirator, in that those who did not report use had higher PRs for shortness of breath and wheezing (data not shown). The impact of smoking on these associations was less clear: the PR was higher among smokers for shortness of breath, but PRs were slightly lower among smokers for coughing and wheezing, compared to non-smokers. Also, the combined impacts of oil exposure and dispersant and exhaust exposures on acute respiratory symptoms were not entirely clear. Though there was a tendency for PRs to be higher among responders without dispersant exposure and without exhaust exposure, compared to responders with these exposures, the number of exposed individuals was small in some strata.
Adjusted dispersant models were similarly stratified by use of dispersant-related PPE, period of response in relation to the well capping, and smoking status (Supplementary Table 2). Use of dispersant-related PPE had inconsistent associations: higher PRs were detected for coughing and wheezing among those who did not use dispersant-related PPE; however, an elevated PR was found among responders who reported use of dispersant-related PPE for shortness of breath. Dispersant exposure was more strongly associated with presence of acute respiratory symptoms among individuals who were deployed after the well was capped than among those deployed before and among non-smokers compared to smokers.
Discussion
The present study has identified several exposures often encountered during oil spill clean-up work (crude oil/oily water, oil dispersants, and engine exhaust) that appear to be associated with acute respiratory symptoms in this cohort of USCG responders. In short, duration of a responder’s deployment in the period before the capping of the well, when exposures to oil, dispersant, and other stressors were likely to be at their highest, was associated with coughing, shortness of breath, and wheezing. Interestingly, these associations were also present in the post-capping period among responders whose self-report of respiratory symptoms were not likely to due to seasonal respiratory infections (i.e., those deployed after September 30, 2010), and were particularly strong among responders with the longest deployments (>60 days). The current study found that responders exposed to oil and oil dispersant exposures had at least twice the prevalence of coughing, shortness of breath, and wheezing, which generally followed an exposure-response relationship. Further, exposure to crude oil and oil dispersant together was associated with a substantially higher prevalence of each of these symptoms than was exposure to crude oil alone (approximately a five-fold increased prevalence for shortness of breath and wheezing). Finally, these associations were modified by several factors, including use of PPE, smoking, deployment timing, suggesting that some exposed responders may be particularly vulnerable to acute respiratory health effects.
Similar to the present study, Suarez et al found a higher frequency of throat and respiratory tract symptoms with increased duration in highly polluted areas among workers participating in the Prestige oil spill cleanup (Suarez et al. 2005). Several prior epidemiological studies have also detected associations between measures of oil spill exposure (e.g., duration of clean-up activities, proximity to oil spill) and elevated frequency of respiratory health symptoms (Aguilera et al. 2010; Laffon et al. 2016; Ordinioha and Sawyer 2010). With respect to oil exposure, Rusiecki et al reported associations between an oil exposure index and acute respiratory symptoms in the same population as the present study (Rusiecki et al. 2017). This oil exposure index incorporated self-report of oil exposure, timing of deployment, and length of deployment was associated with a doubling of prevalence of coughing, wheezing, and shortness of breath. This is consistent with the present study’s findings, which examined the effects of not only ever report of oil exposure, but also specific routes of exposure. Similar to the current study, environmental exposure to the DWH spill was associated with increased odds of self-reported coughing, shortness of breath, and wheezing among a cohort of women living in southern Louisiana (Peres et al. 2016).
Oil dispersants are commonly-used compounds in oil spill clean-up activities; however, little is known about human health effects related to exposure via dermal contact or inhalation. At the beginning of the DWH response, BP used Corexit 9527A, but soon switched to Corexit 9500 (United States Coast Guard 2011). Considering that these dispersants contain compounds such as 2-butoxyethanol and propylene glycol, which are considered respiratory irritants (Agency for Toxic Substances and Disease Registry 1997, 1998; Wieslander et al. 2001), their potential impact on respiratory health symptoms in humans warrants investigation. Though the effects of dispersant contact were not as strong as oil exposures in the present study, significant trends were found with increasing dispersant contact frequency, suggesting an exposure-response relationship between this agent(s) and coughing and shortness of breath. These corroborate the findings of the GuLF STUDY, which recently reported significant associations between direct dispersant exposure (compared to no exposure) and cough (PR=1.47), wheeze (PR=1.45), tightness of chest (PR=1.74), and shortness of breath (PR=1.63). (McGowan et al. 2017) A recent in vitro study of human airway epithelial cells by Liu et al identified 84 differentially expressed genes (including 38 upregulated and 46 downregulated genes) after treatment with Corexit 9500 (Liu et al. 2016). These genes are involved in cell junctions and airway angiogenesis, which are commonly altered in asthma patients. Taken together, these findings suggest that exposure to oil dispersants may independently affect respiratory health.
The current study also examined the effects of exposure to oil alone and to oil and oil dispersants combined. The combination of both oil and oil dispersants presented associations that were much greater in magnitude than oil alone. These findings corroborate findings by Liu et al, who looked at expression patterns of genes after treatment with either crude oil, oil dispersants (Corexit 9500 or 9527), or both in human airway epithelial cells (Liu et al. 2016). A synergistic effect was identified as there were a greater number of differentially expressed genes detected in cells that were treated with both Corexit 9527 and oil. In contrast, findings from Liu et al suggested that Corexit 9500 may attenuate the harmful effects of oil. However, the present study was unable to ascertain the type of oil dispersant to which responders were exposed (i.e., Corexit 9500 or 9527A).
Stratification on several factors suggested several subgroups may be more vulnerable to the respiratory impact of oil exposure. Most importantly, responders who did not report use of PPE had consistently higher relative risks for all three acute respiratory symptoms, which has been previously observed (Lee et al. 2009; Suarez et al. 2005; Zock et al. 2007). Other studies that have focused on intact PPE (e.g., worn and not torn) or education on use of PPE found an increased number of respiratory symptoms among those who had damaged PPE or were uninformed (Carrasco et al. 2006; Sim et al. 2010). However, Gwack et al have observed an association between correct use of specific PPE (masks) and the presence of respiratory symptoms (Gwack et al. 2012); type of activities during that oil spill clean-up effort was not captured, and thus propensity of those using PPE to be more highly exposed could not be assessed. While use of a respirator was captured in the present study, the small number of individuals who reported respirator use limited the ability to carry out analyses and draw conclusions for this subgroup. Furthermore, responders who used respirators may have been different from those who did not with regard to underlying exposures. Future studies will need to capture detailed information on PPE use together with exposure opportunity among oil cleanup responders. No consistent patterns were observed when stratified by smoking status with respect to oil exposure status, suggesting a complex relationship between smoking, oil exposure, and acute respiratory symptoms. When stratified by spill-related factors (capping period, exhaust exposure and dispersant exposure), again, no consistent patterns arose, suggesting a need to further investigate interactions with other exposures and the effect of oil exposures in these subgroups. Stratification of dispersant models showed stronger effects among those who did not report use of PPE, those who responded after the capping of the well, and among nonsmokers. No other study has examined use of PPE specifically used for dispersant-related work, and future studies should be carried out to confirm findings in the present study.
This study has a number of limitations. Assessment of exposure to crude oil, oil dispersants, and exhaust were based on self-report, and may be subject to reporting bias. Additionally, although Corexit 9527A and 9500 were widely used in the DWH oil spill response, the survey instrument did not explicitly ask for oil dispersant product names, many participants are unlikely to have known, and there was substantial temporal overlap of use of the two dispersants. Also, reporting of exposure to oil and oil dispersants was highly concordant; therefore, the effect of only oil dispersant exposure in the absence of oil could not be meaningfully assessed. Finally, this study is cross-sectional in nature; therefore, the timing of the exposure and health effects in relation to each other are unknown; however, there is a longitudinal component of this cohort and we plan to follow-up findings from this study in future analyses. Despite limitations, there are clear strengths to the study. First, the study population was large, allowing stratified analyses to be carried out based on factors not previously reported or understudied in the literature (e.g., use of PPE, specific type of PPE, other exposures). Second, USCG responders are generally very healthy, reducing the impact of comorbidities on the symptoms reported herein. Finally, recall of the deployment experience is likely to be accurate, as more than two-thirds of responders completed the exit survey within the month of their deployment, with the majority of the responders completing prior to or at the end of their deployment (57%).
In summary, responders of the DWH oil spill faced a variety of physical, environmental and chemical exposures that may have impacted their short-term and long-term health. Further investigation in populations that respond to such disasters is warranted, as the number of people affected by these ever-increasing disasters is large.
Supplementary Material
Highlights.
Cross sectional analyses of crude oil/dispersant exposures and acute respiratory symptoms in disaster responders
Elevated prevalence ratios for coughing, shortness of breath, and wheezing with crude oil exposure
Increasing crude oil inhalation and dermal contact showed increasing likelihood for respiratory symptoms
Combination of crude oil and dispersants showed associations greater in magnitude than oil alone
We found strong relationships between crude oil/dispersant exposures and acute respiratory symptoms
Acknowledgments
This study was supported by a National Institutes of Health grant (RO1ES020874). The authors would like to thank Renee Funk, CDC, for assistance with creating the survey upon which these results are based. Kate Christenbury and David Johndrow provided data management and data analysis.
Footnotes
Statement of Authors’ Contributions: Melannie Alexander led the analysis and wrote the manuscript. Jennifer Rusiecki (PI), conceived, designed, and executed the study and assisted writing the manuscript. Lawrence Engel (co-PI) designed and executed the study, worked closely with the PI in all aspects. Erica Schwartz (co-PI) assisted with making data available from the U.S. Coast Guard and helped execute the study. Nathan Olaiya and Li Wang assisted with data analyses. Laura Weems provided expertise/advice on Coast Guard personnel exposures. John Barrett provided expertise/advice on health effects. All co-authors provided assistance interpreting results and editing the manuscript.
Disclaimer: The Views expressed here are those of the authors and do not necessarily reflect the official views of the Uniformed Services University of the Health Sciences, the Department of Defense, the United States Coast Guard, The Department of Homeland Security, or the Centers for Disease Control and Prevention.
Conflict of Interest Statement: The authors declare no conflict of interest
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Agency for Toxic Substances and Disease Registry PHS, U.S. Department of Health and Human Services. Toxicological profile for propylene glycol. 1997 [PubMed] [Google Scholar]
- Agency for Toxic Substances and Disease Registry PHS, U.S. Department of Health and Human Services. Toxicological profile for 2-butoxyethanol and 2-butoxyethanol acetate. 1998 [PubMed] [Google Scholar]
- Aguilera F, Mendez J, Pasaro E, Laffon B. Review on the effects of exposure to spilled oils on human health. J Appl Toxicol. 2010;30:291–301. doi: 10.1002/jat.1521. [DOI] [PubMed] [Google Scholar]
- Barros AJ, Hirakata VN. Alternatives for logistic regression in cross-sectional studies: An empirical comparison of models that directly estimate the prevalence ratio. BMC Med Res Methodol. 2003;3:21. doi: 10.1186/1471-2288-3-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carrasco JM, Lope V, Perez-Gomez B, Aragones N, Suarez B, Lopez-Abente G, et al. Association between health information, use of protective devices and occurrence of acute health problems in the prestige oil spill clean-up in asturias and cantabria (spain): A cross-sectional study. BMC Public Health. 2006;6:1. doi: 10.1186/1471-2458-6-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deddens JA, Petersen MR. Approaches for estimating prevalence ratios. Occup Environ Med. 2008;65:481, 501–486. doi: 10.1136/oem.2007.034777. [DOI] [PubMed] [Google Scholar]
- Gwack J, Lee JH, Kang YA, Chang KJ, Lee MS, Hong JY. Acute health effects among military personnel participating in the cleanup of the hebei spirit oil spill, 2007, in taean county, korea. Osong Public Health Res Perspect. 2012;3:206–212. doi: 10.1016/j.phrp.2012.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ha M, Kwon H, Cheong HK, Lim S, Yoo SJ, Kim EJ, et al. Urinary metabolites before and after cleanup and subjective symptoms in volunteer participants in cleanup of the hebei spirit oil spill. Sci Total Environ. 2012;429:167–173. doi: 10.1016/j.scitotenv.2012.04.036. [DOI] [PubMed] [Google Scholar]
- Hulin M, Simoni M, Viegi G, Annesi-Maesano I. Respiratory health and indoor air pollutants based on quantitative exposure assessments. Eur Respir J. 2012;40:1033–1045. doi: 10.1183/09031936.00159011. [DOI] [PubMed] [Google Scholar]
- Janjua NZ, Kasi PM, Nawaz H, Farooqui SZ, Khuwaja UB, Najam ul H, et al. Acute health effects of the tasman spirit oil spill on residents of karachi, pakistan. BMC Public Health. 2006;6:84. doi: 10.1186/1471-2458-6-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King BS, Gibbins JD. Health hazard evaluation of deepwater horizon response workers. US Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, Health Hazard Evaluation Program; 2011. [Google Scholar]
- Kwok RK, Engel LS, Miller AK, Blair A, Curry MD, Jackson WB, et al. The gulf study: A prospective study of persons involved in the deepwater horizon oil spill response and clean-up. Environ Health Perspect. 2017;125:570–578. doi: 10.1289/EHP715. doi:510.1289/EHP1715. Epub 2017 Mar 1231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laffon B, Pasaro E, Valdiglesias V. Effects of exposure to oil spills on human health: Updated review. J Toxicol Environ Health B Crit Rev. 2016;19:105–128. doi: 10.1080/10937404.2016.1168730. [DOI] [PubMed] [Google Scholar]
- Lee SM, Ha M, Kim EJ, Jeong WC, Hur J, Park SG, et al. the effects of wearing protective devices among residents and volunteers participating in the cleanup of the hebei spirit oil spill. J Prev Med Public Health. 2009;42:89–95. doi: 10.3961/jpmph.2009.42.2.89. [DOI] [PubMed] [Google Scholar]
- Liu YZ, Roy-Engel AM, Baddoo MC, Flemington EK, Wang G, Wang H. The impact of oil spill to lung health--insights from an rna-seq study of human airway epithelial cells. Gene. 2016;578:38–51. doi: 10.1016/j.gene.2015.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Z, Liu J, Zhu Q, Wu W. The weathering of oil after the deepwater horizon oil spill: Insights from the chemical composition of the oil from the sea surface, salt marshes and sediments. Environmental Research Letters. 2012;7:035302. [Google Scholar]
- McGowan CJ, Kwok RK, Engel LS, Stenzel MR, Stewart PA, Sandler DP. Respiratory, dermal, and eye irritation symptoms associated with corexit ec9527a/ec9500a following the deepwater horizon oil spill: Findings from the gulf study. Environ Health Perspect. 2017;125:097015. doi: 10.1289/EHP1677. doi:097010.091289/EHP091677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meo S, Al-Drees A, Rasheed S, Meo I, Al-Saadi M, Ghani H, et al. “Health complaints among subjects involved in oil cleanup operations during oil spillage from a greek tanker” tasman spirit. Int J Occup Med Environ Health. 2009;22:143–148. doi: 10.2478/v10001-009-0011-x. [DOI] [PubMed] [Google Scholar]
- Meo SA, Al-Drees AM, Rasheed S, Meo IM, Khan MM, Al-Saadi MM, et al. Effect of duration of exposure to polluted air environment on lung function in subjects exposed to crude oil spill into sea water. Int J Occup Med Environ Health. 2009;22:35–41. doi: 10.2478/v10001-009-0007-6. [DOI] [PubMed] [Google Scholar]
- Ordinioha B, Sawyer W. Acute health effects of a crude oil spill in a rural community in bayelsa state, nigeria. Niger J Med. 2010;19:140–144. doi: 10.4314/njm.v19i2.56500. [DOI] [PubMed] [Google Scholar]
- Peres LC, Trapido E, Rung AL, Harrington DJ, Oral E, Fang Z, et al. The deepwater horizon oil spill and physical health among adult women in southern louisiana: The women and their children’s health (watch) study. Environ Health Perspect. 2016;124:1208–1213. doi: 10.1289/ehp.1510348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts JR, Reynolds JS, Thompson JA, Zaccone EJ, Shimko MJ, Goldsmith WT, et al. Pulmonary effects after acute inhalation of oil dispersant (corexit ec9500a) in rats. J Toxicol Environ Health A. 2011;74:1381–1396. doi: 10.1080/15287394.2011.606794. [DOI] [PubMed] [Google Scholar]
- Rodriguez-Trigo G, Zock JP, Pozo-Rodriguez F, Gomez FP, Monyarch G, Bouso L, et al. Health changes in fishermen 2 years after clean-up of the prestige oil spill. Ann Intern Med. 2010;153:489–498. doi: 10.7326/0003-4819-153-8-201010190-00279. [DOI] [PubMed] [Google Scholar]
- Rusiecki JA, Alexander M, Schwartz EG, Wang L, Weems L, Barrett J, et al. The deepwater horizon response coast guard cohort study. 2017 doi: 10.1136/oemed-2017-104343. Accepted to Occupational and Environmental Medicine. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAS Institute. The SAS system for Windows, Part 9.3. Cary, NC: SAS Institute; 2012. [Google Scholar]
- Shi Y, Roy-Engel AM, Wang H. Effects of corexit dispersants on cytotoxicity parameters in a cultured human bronchial airway cells, beas-2b. J Toxicol Environ Health A. 2013;76:827–835. doi: 10.1080/15287394.2013.821396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sim MS, Jo IJ, Song HG. Acute health problems related to the operation mounted to clean the hebei spirit oil spill in taean, korea. Mar Pollut Bull. 2010;60:51–57. doi: 10.1016/j.marpolbul.2009.09.003. [DOI] [PubMed] [Google Scholar]
- Suarez B, Lope V, Perez-Gomez B, Aragones N, Rodriguez-Artalejo F, Marques F, et al. Acute health problems among subjects involved in the cleanup operation following the prestige oil spill in asturias and cantabria (spain) Environ Res. 2005;99:413–424. doi: 10.1016/j.envres.2004.12.012. [DOI] [PubMed] [Google Scholar]
- United States Coast Guard. On scene coordinator report deepwater horizon oil spill: Submitted to the national response team 2011 [Google Scholar]
- Wang H, Shi Y, Major D, Yang Z. Lung epithelial cell death induced by oil-dispersant mixtures. Toxicol In Vitro. 2012;26:746–751. doi: 10.1016/j.tiv.2012.03.011. [DOI] [PubMed] [Google Scholar]
- Wieslander G, Norback D, Lindgren T. Experimental exposure to propylene glycol mist in aviation emergency training: Acute ocular and respiratory effects. Occup Environ Med. 2001;58:649–655. doi: 10.1136/oem.58.10.649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zock JP, Rodriguez-Trigo G, Pozo-Rodriguez F, Barbera JA, Bouso L, Torralba Y, et al. Prolonged respiratory symptoms in clean-up workers of the prestige oil spill. Am J Respir Crit Care Med. 2007;176:610–616. doi: 10.1164/rccm.200701-016OC. [DOI] [PubMed] [Google Scholar]
- Zock JP, Rodriguez-Trigo G, Rodriguez-Rodriguez E, Espinosa A, Pozo-Rodriguez F, Gomez F, et al. Persistent respiratory symptoms in clean-up workers 5 years after the prestige oil spill. Occup Environ Med. 2012;69:508–513. doi: 10.1136/oemed-2011-100614. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.