Abstract
Objectives
There is substantial variation in treatment intensity among children with autism spectrum disorder (ASD). This study asks whether policies that target health care utilization for ASD affect children differentially based on this variation. Specifically, we examine the impact of state-level insurance mandates that require commercial insurers to cover certain treatments for ASD for any fully-insured plan.
Methods
Using insurance claims between 2008 and 2012 from three national insurers, we used a difference-in-differences approach to compare children with ASD who were subject to mandates to children with ASD who were not. To allow for differential effects, we estimated quantile regressions that evaluate the impact of mandates across the spending distributions of three outcomes: (1) monthly spending on ASD-specific outpatient services, (2) monthly spending on ASD-specific inpatient services, and (3) quarterly spending on psychotropic medications.
Results
The change in spending on ASD-specific outpatient services attributable to mandates varied based on the child’s level of spending. For those children with ASD who were subject to the mandate, monthly spending for a child in the 95th percentile of the ASD-specific outpatient spending distribution increased by $1,460 (p<0.001). In contrast, the effect was only $2 per month for a child in the 5th percentile (p<0.001). Mandates did not significantly affect spending on ASD-specific inpatient services or psychotropic medications.
Conclusions
State-level insurance mandates have larger effects for those children with higher levels of spending. To the extent that spending approximates treatment intensity and the underlying severity of ASD, these results suggest that mandates target children with greater service needs.
INTRODUCTION
Autism spectrum disorder (ASD) is characterized by “persistent deficits in social communication and social interactions” and “restricted, repetitive patterns of behavior, interests, or activities.”1 The clinical presentation of ASD is remarkably heterogeneous, as some individuals have minor difficulties with social engagement while others face profound cognitive and behavioral impairments.2 The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition recently introduced a three-tiered categorization of mild, moderate, and severe ASD,1 although such categorizations only superficially capture the diversity of ASD.3
The breadth of service needs for ASD results in great variation in health care utilization.4,5 More-mildly affected individuals may benefit from psychosocial therapies designed to improve social ability and address ancillary speech or behavioral impairments.4 More-impaired individuals typically rely on intensive behavioral treatments combined with psychotropic medications.4,6 In some cases, especially among those children with ASD and an intellectual disability, self-injurious and aggressive behaviors can occur and may require one-to-one supports and, at times, psychiatric hospitalizations.7,8
Citing the financial burden and lack of evidentiary support for some ASD treatments, commercial insurers historically limited coverage for these services.9 Since 2001, most states have responded by introducing laws that require the coverage of many treatments for commercially-insured children with ASD.10 Mandates have annual expenditure caps on services ranging from $12,000 to $50,000 and generally target specific age groups.10
Insurers expressed concern that mandates would result in a dramatic increase in the number of children diagnosed with ASD.9 One study found that mandates led to an increase in the number of children diagnosed, but that the treated prevalence was still less than the community prevalence.10 Insurers also argued that mandates would lead to many children with ASD increasing their health care utilization.9,11 A second study found that, on average, mandates increased the use of and spending on outpatient services by children with ASD.12 However, the clinical heterogeneity of ASD begs the question – do mandates impact children with ASD similarly or do their effects depend on a child’s health care utilization?
Rather than focus on the average effects of state-level ASD policies already explored in previous research,10,12–17 this study examines the extent to which mandates affect children with ASD differentially based on their health care spending. Using insurance claims from three large national insurers and a quasi-experimental approach, we evaluate the impact of mandate implementation across the distributions of three outcomes: monthly spending on ASD-specific outpatient services, monthly spending on ASD-specific inpatient services, and quarterly spending on psychotropic medications.
METHODS
Insurance Mandates
To identify implementation dates and age eligibility criteria for mandates that took effect during our study period (2008 to 2012), we first obtained information on state initiatives from Autism Speaks.18 Because implementation dates for mandates were imprecise, we then reviewed the original legislation, which was compiled by the National Council of State Legislatures.19 During our study period, three states introduced mandates in 2008, six states introduced mandates in 2009, four states introduced mandates in 2010, eight states introduced mandates in 2011, and seven states introduced mandates in 2012.10
State-level policies like mandates affect roughly half of the commercially-insured population due to the Employee Retirement Income Security Act (ERISA) of 1974, which exempts self-insured firms that contract directly with health plans to administer their employees’ health benefits.20 Per ERISA, mandates apply to fully-insured firms with more than 50 employees unless otherwise specified.20 In our study, 22 of the 29 mandates also applied to fully-insured firms with 50 or fewer employees.10
Data
Our data included outpatient, inpatient, and pharmaceutical claims between January 1, 2008 and December 31, 2012 from the Health Care Cost Institute (HCCI), which included claims from Aetna, Humana, and UnitedHealthcare and indicated whether beneficiaries were enrolled in fully-insured plans and thus subject to state-level policies. Spending measures were the sum of insurance payments and out-of-pocket spending (including copays, coinsurance, and deductibles) and were inflated to 2012 dollars using the Personal Health Care Index from the CMS Office of the Actuary.21 Our study sample included children from birth through 21 years old with at least two claims on different days containing an International Classification of Diseases, Ninth Revision, Clinical Modification code 299.xx during the study period. We excluded children without mental health coverage, children in individually insured plans, and children in the top 0.1% of total spending. This study was exempted from review by the University of Pennsylvania’s Institutional Review Board.
The outcomes of interest were (1) monthly spending on ASD-specific outpatient services, including physical, occupational, and speech therapies and other behavioral services such as psychotherapy and medication management, (2) monthly spending on ASD-specific inpatient services, and (3) quarterly spending on psychotropic medications, including antipsychotics, antidepressants, mood stabilizers, anxiolytics, and stimulants. When analyzing psychotropic medications, we further excluded any children without prescription drug coverage and aggregated spending to the three-month level because prescriptions may extend beyond 30 days.
The primary independent variables were binary indicators of whether a child lived in a state subject to a mandate and whether the child was eligible for that mandate in a given month or quarter. Eligibility required that a child be enrolled in a fully-insured plan and meet the mandate’s age criteria. For states that did not pass a mandate during the study period, we considered children to be eligible if they had fully-insured coverage and were 21 years old or younger, which was the modal age range covered by mandates. Other covariates were gender, age, insurance product type, and month/quarter, state, and year fixed effects. Complete information on birthdate was not included in the data, so ages were estimated assuming a July 1 birthdate in the child’s birth year.
Statistical Analysis
To identify the effect of mandates on health care spending among children with ASD, we used a difference-in-differences approach.22–24 The treatment group included children living in states with active mandates who were eligible for that mandate and the comparison group included (1) children in states with an active mandate who were ineligible for that mandate, (2) children in states without an active mandate who would have been eligible given their insurance status and age, and (3) children in states without an active mandate who would not have been eligible if one were active.
Rather than use linear regressions that report the effect of mandates on the conditional mean of an outcome, we used quantile regressions that can estimate the effect of mandates in any quantile of the outcome’s distribution. The most commonly utilized quantile regression is the median regression, which minimizes the sum of absolute residuals.25 When analyzing other quantiles, residuals are weighted based on the quantile specification – for example, at the 90th percentile, the errors above receive a weight of 0.9, while errors below receive a weight of 0.1.25 Thus, the coefficient for a 90th percentile quantile regression refers to the specific change in monthly spending for the child in the 90th percentile of the spending distribution. Because quantiles are based on the distribution of the outcome variable in a given month/quarter, children move to different percentiles throughout the study period.
To illustrate the impact of mandates across the spending distribution, we estimated quantile regressions on every 5th percentile. Currently, there is no logistically-feasible method of clustering standard errors within a quantile regression framework.26 To account for the risk of type 1 errors, we assessed statistical significance at the 1 percent level.
RESULTS
The final study sample included 106,977 children. Between 2008 and 2012, 99 percent had at least one outpatient claim and 7 percent had at least one inpatient claim specifying ASD. For those children with prescription drug coverage, 61 percent had at least one prescription claim for a psychotropic medication (Table).
Table 1.
Descriptive Statistics of Monthly/Quarterly Health Care Use and Spending Among Children with ASD, 2008–2012
| Children with ASD | Children in Mandate States (29 states as of 2012) | Children in Non-Mandate States (22 states as of 2012) | |||
|---|---|---|---|---|---|
| Fully-Insured | Self-Insured | Fully-Insured | Self-Insured | ||
| Any ASD Outpatient Utilization (%) | 99.0 | 99.4 | 98.9 | 99.3 | 98.9 |
| conditional spending: 5th percentile | $55 | $55 | $55 | $55 | $55 |
| conditional spending: 50th percentile | $219 | $240 | $220 | $225 | $200 |
| conditional spending: 95th percentile | $2,125 | $3,839 | $2,146 | $5,753 | $1,766 |
| Any ASD Inpatient Utilization (%) | 7.1 | 7.2 | 7.0 | 6.9 | 7.2 |
| conditional spending: 5th percentile | $873 | $850 | $893 | $1,125 | $825 |
| conditional spending: 50th percentile | $6,082 | $6,011 | $5,926 | $6,799 | $6,340 |
| conditional spending: 95th percentile | $23,541 | $22,955 | $22,846 | $24,518 | $25,734 |
| Any Psychotropic Prescriptions (%) | 61.4 | 59.7 | 60.1 | 63.1 | 66.7 |
| conditional spending: 5th percentile | $21 | $23 | $21 | $19 | $20 |
| conditional spending: 50th percentile | $479 | $484 | $479 | $469 | $475 |
| conditional spending: 95th percentile | $2,835 | $2,840 | $2,905 | $2,721 | $2,735 |
| Number of Children | 106,977 | 23,105 | 55,511 | 7,985 | 20,376 |
Notes: Fully-insured children are subject to state-level mandates if they meet other eligibility criteria, but self-insured children are not due to ERISA. Subsamples are based on a child’s status in the first month/quarter they entered the dataset. Psychotropic measures exclude children without Rx coverage.
There was substantial heterogeneity in the distribution of each spending measure. For monthly spending on ASD-specific outpatient services, the 95th percentile was $2,520, the median was $219, and the 5th percentile was $55. For monthly spending on ASD-specific inpatient services, the 95th percentile was $23,541, the median was $6,082, and the 5th percentile was $873. For quarterly spending on psychotropic medications, the 95th percentile was $2,835, the median was $479, and the 5th percentile was $21.
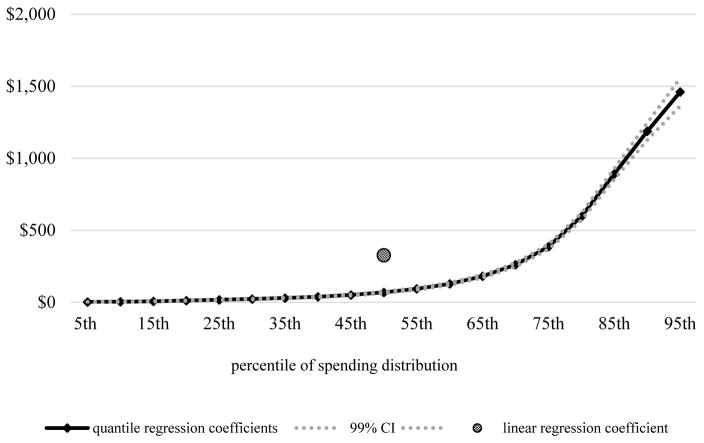
Mandates had differential effects on monthly spending on ASD-specific outpatient services, with larger effects occurring for children with higher levels of spending (Figure 1). Among eligible children, increases in spending attributable to the mandate were $1,460 per child-month at the 95th percentile (99% CI, $1,363–$1,557), $69 per child-month at the median (99% CI, $63–$74), and $2.32 per child-month at the 5th percentile (99% CI, $1.15–$3.49). By comparison, the average effect of the mandate as estimated by a linear regression was a $327 (99% CI, $308–$345) increase in monthly spending.
Figure 1. Adjusted Estimates of the Effects of State Mandates on Monthly Spending on ASD-Specific Outpatient Services using Quantile Regressions, 2008–2012.
Notes. ASD-specific outpatient service claims occurred in 853,355 child-months between 2008 and 2012. Confidence intervals are at the 1% level of significance. Covariates include age, gender, insurance type, and month, state, and year fixed effects.
Notably, the increase in spending on ASD-specific outpatient services was both absolutely and relatively larger among high spenders: at the 95th percentile, spending increased by 58 percent in mandate states relative to non-mandate states; at the 5th percentile, spending increased by only 4 percent.
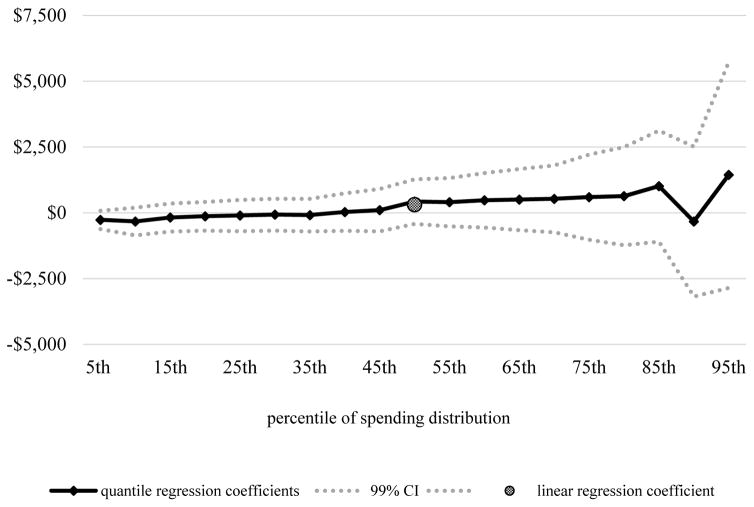
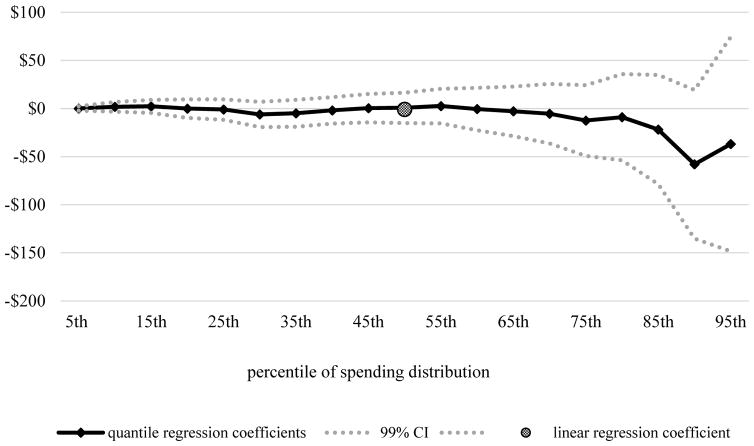
Mandates did not significantly impact ASD-specific inpatient services (Figure 2) or psychotropic medications (Figure 3).
Figure 2. Adjusted Estimates of the Effects of State Mandates on Monthly Spending on ASD-Specific Inpatient Services using Quantile Regressions, 2008–2012.
Notes. ASD-specific inpatient service claims occurred in 12,204 child-months between 2008 and 2012. Confidence intervals are at the 1% level of significance. Covariates include age, gender, insurance type, and month, state, and year fixed effects.
Figure 3. Adjusted Estimates of the Effects of State Mandates on Quarterly Spending on Psychotropic Medications using Quantile Regressions, 2008–2012.
Notes. Children without prescription drug coverage are excluded from the analysis. Psychotropic medication claims occurred in 299,158 child-quarters between 2008 and 2012. Confidence intervals are at the 1% level of significance. Covariates include age, gender, insurance type, and quarter, state, and year fixed effects.
DISCUSSION
This study asked whether insurance mandates affect children with ASD differentially based on how much they spend on services. While mandates increased monthly spending on ASD-specific outpatient services for children across the spending distribution, we found that the effects were larger for children with higher levels of spending. Addressing insurers’ concerns, it appears that mandates had a modest effect for many children with ASD: increases in monthly spending on ASD-specific outpatient services attributable to the mandate were less than $100 per child-month through the 55th percentile of the spending distribution.
It is encouraging to observe that, even among high spenders, the effect of the mandates was solely on outpatient services rather than inpatient services or psychotropic medication use. While some mandates were broad in the services they cover, they were written with the explicit intent to increase the use of community-based outpatient services that have been shown to improve outcomes for children with ASD.27,28
Several limitations should be noted. First, diagnoses of ASD in insurance claims cannot be verified through clinical interview, although prior research finds a high positive predictive value of this strategy.29 Second, pharmacy claims do not have an associated diagnosis that can identify them as ASD-specific, so we cannot be sure that medications were prescribed to address ASD symptoms. Third, insurance claims do not include other ASD-related expenditures, such as spending on school-based services or services paid for completely out-of-pocket. Fourth, we cannot control for the availability of approved providers, which varies substantially within and across states. Finally, we did not account for some of the policy nuances in mandates, including expenditure caps, coverage of specified services, and whether exemptions from state-level policies were granted to firms with fewer than 50 employees.
Despite these limitations, there are important implications of our findings. To the extent that health care spending can approximate the treatment intensity of a child, these results indicate that mandates have a larger impact on children with greater service needs. If health care spending correlates to the underlying severity of a child’s ASD, these findings also indicate that children with severe ASD are being disproportionately affected by mandates.
An alternative interpretation is less reassuring. Barriers to obtaining care, such as limited provider networks30 and uncertainty about which services are covered11, are well-documented among children with ASD. If some families are more adept at navigating these hurdles due to socio-demographics, location, or awareness, our results suggest that issues with access remain. However, these findings may be due to children with lower levels of spending already having their service needs met through the education system, so they do not turn to health care even in the presence of mandates.
Policies are rarely one-size-fits-all, yet studies typically report their average effects. Using a linear regression, we found that the average effect of mandates on monthly spending for ASD-specific outpatient services was $327. Using quantile regressions, we found that the effects of mandates on spending differed dramatically across the spending distribution, with spending increasing by $1,460 per month for children in the 95th percentile and only $2 per month for children in the 5th percentile. This study demonstrates the need for researchers to explore the differential effects of policies, especially when those polices target a clinically diverse condition like ASD.
Acknowledgments
Funding: NIMH R01MH096848 (PIs: Barry and Mandell)
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to report.
References
- 1.Association AP. Diagnostic and Statistical Manual of Mental Disorders. 5. Washington, DC: 2013. [Google Scholar]
- 2.Howlin P. Autism and Asperger Syndrome, Preparing for Adulthood. New York: Routledge; 2004. [Google Scholar]
- 3.Kanne SM, Abbachhi AM, Constantino JN. Multi-informant ratings of psychiatric symptom severity in children with autism spectrum disorders: The importance of environmental context. Journal of Autism and Developmental Disorders. 2009;39:856. doi: 10.1007/s10803-009-0694-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Myers S, Johnson C. American Academy of Pediatrics Council on Children with Disabilities. Management of children with autism spectrum disorders. Pediatrics. 2007;120:1,162–1,182. doi: 10.1542/peds.2007-2362. [DOI] [PubMed] [Google Scholar]
- 5.Horlin C, Falkmer M, Parsons R, Albrecht MA, Falkmer T. The Cost of Autism Spectrum Disorders. PLoS One. 2014;9(9):e106552. doi: 10.1371/journal.pone.0106552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shea S, Turgay A, Carroll A, Schulz M, Orlik H, Smith I, Dunbar F. Risperidone in the Treatment of Disruptive Behavioral Symptoms in Children with Autistic and Other Pervasive Developmental Disorders. Pediatrics. 2004;114(5):e634–e641. doi: 10.1542/peds.2003-0264-F. [DOI] [PubMed] [Google Scholar]
- 7.Matson JL, LoVullo SV. A review of behavioral treatments for self-injurious behaviors of persons with autism spectrum disorders. Behavior Modification. 2008;32(1):61–76. doi: 10.1177/0145445507304581. [DOI] [PubMed] [Google Scholar]
- 8.Stein D, Ring A, Shulman C, Meir D, Holan A, Weizman A, Barak Y. Brief report: Children with autism as they grow up – description of adult inpatients with severe autism. Journal of Autism and Developmental Disorders. 2001;31(3):355–360. doi: 10.1023/a:1010707622612. [DOI] [PubMed] [Google Scholar]
- 9.Bouder JN, Spielman S, Mandell DS. Brief Report: Quantifying the Impact of Autism Coverage on Private Insurance Premiums. Journal of Autism and Developmental Disorders. 2009;39(6):953–957. doi: 10.1007/s10803-009-0701-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mandell DS, Barry CL, Marcus SC, Xie M, Shea K, Mullan K, Epstein AJ. The Effects of Autism Insurance Mandates on the Treated Prevalence of Autism. JAMA Pediatrics. 2016;170(9):887–893. doi: 10.1001/jamapediatrics.2016.1049. [DOI] [PubMed] [Google Scholar]
- 11.Baller J, Barry C, Shea K, Walker M, Ouellette R, Mandell D. Assessing early implementation of state autism insurance mandates. Autism. 2016;20(8):796–807. doi: 10.1177/1362361315605972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barry CL, Epstein AJ, Marcus SC, Kennedy-Hendricks A, Candon M, Xie M, Mandell DS. Effects of State Insurance Mandates on Health Care Use and Spending. Health Affairs. 2017;36(10):1,754–1,761. doi: 10.1377/hlthaff.2017.0515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ganz ML. The lifetime distribution of the incremental societal costs of autism. Archives of Pediatric and Adolescent Medicine. 2007;161(4):343–349. doi: 10.1001/archpedi.161.4.343. [DOI] [PubMed] [Google Scholar]
- 14.Liptak GS, Stuart T, Auinger P. Health care utilization and expenditures for children with autism: Data from U.S. National Samples. Journal of Autism and Developmental Disorders. 2006;36:871–879. doi: 10.1007/s10803-006-0119-9. [DOI] [PubMed] [Google Scholar]
- 15.Lavelle TA, Weinstein MC, Newhouse JP, Munir K, Kuhlthau KA, Prosser LA. Economic Burden of Childhood Autism Spectrum Disorders. Pediatrics. 2014;133(3):e520–9. doi: 10.1542/peds.2013-0763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chatterji P, Decker SL, Markowitz S. The Effects of Mandated Health Insurance Benefits for Autism on Out-of-Pocket Costs and Access to Treatment. Journal of Policy Analysis and Management. 2015;34(2):328–53. doi: 10.1002/pam.21814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bilaver LA, Jordan N. Impact of State Mental Health Parity Laws on Access to Autism Services. Psychiatric Services. 2013;64(10):967–973. doi: 10.1176/appi.ps.201200411. [DOI] [PubMed] [Google Scholar]
- 18.Autism Speaks. State Initiatives. 2015 ( https://www.autismspeaks.org/state-initiatives)
- 19.National Conference of State Legislatures. Autism and Insurance Coverage. ( http://www.ncsl.org/research/health/autism-and-insurance-coverage-state-laws.aspx)
- 20.Buchmueller T, Cooper P, Jacobson M, Zuvekas S. Parity for whom? Exemptions and the extent of state mental health parity legislation. Health Affairs. 2007;26:w483–7. doi: 10.1377/hlthaff.26.4.w483. [DOI] [PubMed] [Google Scholar]
- 21.Centers for Medicare & Medicaid Services, Office of the Actuary, National Health Statistics Group. National Health Expenditure Accounts: Methodology Paper. 2014 ( https://www.cms.gov/research-statistics-data-and-systems/statistics-trends-and-reports/nationalhealthexpenddata/downloads/dsm-14.pdf)
- 22.Gruber J. State-mandated benefits and employer-provided health insurance. Journal of Public Economics. 1994;55:433–64. [Google Scholar]
- 23.Harris K, Carpenter C, Bao Y. The effects of state parity laws on the use of mental health care. Medical Care. 2006;44:499–505. doi: 10.1097/01.mlr.0000215813.16211.00. [DOI] [PubMed] [Google Scholar]
- 24.Schmidt L. Effects of infertility insurance mandates on fertility. Journal of Health Economics. 2007;26:431–46. doi: 10.1016/j.jhealeco.2006.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gujarati D. Econometrics by Example. 2. Palgrave: 2014. pp. 405–406. [Google Scholar]
- 26.Maclean JC, Webber DA, Marti J. An Application of Unconditional Quantile Regression to Cigarette Taxes. Journal of Policy Analysis and Management. 2014;33(1):188–210. [Google Scholar]
- 27.National Conference of State Legislatures. Autism and Insurance Coverage: State Laws. 2015. [Google Scholar]
- 28.Warren Z, McPheeters ML, Sathe N, Foss-Feid JH, Glasser A, Veenstra-VanderWeele J. A Systematic Review of Early Intensive Intervention for Autism Spectrum Disorders. Pediatrics. 2014;127(5):e1303–e1311. doi: 10.1542/peds.2011-0426. [DOI] [PubMed] [Google Scholar]
- 29.Burke JP, Jain A, Yang W, Kelly JP, Kaiser M, Becker L, Lawer L, Newschaffer CJ. Does a claims diagnosis of autism mean a true case? Autism. 2014;18(3):321–30. doi: 10.1177/1362361312467709. [DOI] [PubMed] [Google Scholar]
- 30.Gordon-Lipkin E, Foster J, Peacock G. Whittling Down the Wait Time: Exploring Models to Minimize the Delay from Initial Concern to Diagnosis and Treatment of Autism Spectrum Disorder. Pediatric Clinics of North America. 2016;63(5):851–859. doi: 10.1016/j.pcl.2016.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]