Abstract
Purpose
To determine the long-term outcomes of same-site revision of failed filtering blebs with mitomycin C application.
Patients and methods
Noncomparative retrospective case series of 45 eyes of 39 patients. Main outcome measures were surgical success (≤21, ≤18, and ≤16 mm Hg reduction in intraocular pressure (IOP)). Other outcome measures included best-corrected visual acuity (VA), visual field loss, number of glaucoma medications, need for further interventions, time from surgery to recommencement of medications or interventions, and complications.
Results
Mean follow-up was 126±59.6 months (range 16–227 months). The overall success proportion at last follow-up was 96% for IOP ≤21 mm Hg (criterion 1), 91% for IOP ≤18 mm Hg (criterion 2), and 84% for IOP ≤16 mm Hg (criterion 3). Absolute success at last follow-up was 64%, 38%, and 33% for criteria 1, 2, and 3, respectively. Mean baseline IOP was reduced from 24.2±5.5 to 12.4±5.5 mm Hg at last follow-up. Ten eyes (22%) had early and 3 (7%) eyes had late complications. None of these complications resulted in visual loss or surgery failure. Nine eyes (20%) required further glaucoma surgery. Nine eyes (20%) required further glaucoma laser.
Conclusions
Same-site, augmented, bleb revision is a safe and effective technique to control IOP and prevent further visual loss in patients with failed trabeculectomies.
Introduction
Trabeculectomy has been the glaucoma surgery of choice for over 40 years.1 Despite high initial success, there is a steady rate of failure of the procedure, owing to progressive subconjunctival scarring, with subsequent increase of intraocular pressure (IOP).2, 3 Surgical innovation, including usage of releasable or adjustable scleral flap sutures and modification of wound healing by intraoperative and postoperative application of antimetabolites and bleb needling has improved outcomes.4 However, reports of randomized controlled studies and case series suggest that despite surgical inventions and highly proactive postoperative care, the success remains high initially, but gradually declines, by ~10% per year.2, 5, 6
Currently there is lack of consensus with regards to management of a failed trabeculectomy bleb and the decision depends largely on the surgeon’s expertise and patient-specific factors. Reinstitution of medical therapy is usually the initial approach. If the trabeculectomy bleb is perceived as salvageable, then it may be revived by either needling or same-site revision of the bleb. Adjunctive wound-healing-modifying agents, such as 5-fluorouracil (5FU) and mitomycin C (MMC) are used intraoperatively for the majority of these cases.7, 8, 9 If these interventions fail, alternative approaches include laser trabeculoplasty, new augmented trabeculectomy, aqueous shunt implantation, or cyclodiode laser.6, 10, 11, 12
Revision of the trabeculectomy bleb involves exploration of the previous surgical site, opening the scleral flap, and ensuring a functional fistula, usually with the concomitant use of an antimetabolite.9, 13 It presents significant potential advantages compared to other surgical approaches. It utilizes the optimal position for a trabeculectomy bleb, minimizes intraocular manipulation, by not repeating a peripheral iridectomy, and does not traumatize new areas of conjunctiva and underlying tissues.
The purpose of this study is to describe the surgical technique and outcomes of same-site, augmented, anterior bleb revision.
Materials and methods
This study was approved by the audit department of Moorfields Eye Hospital. The medical records of all patients who underwent augmented bleb revision surgery by a single surgeon (IM), between July 1994 and January 2012, were identified and reviewed. At each postoperative visit the following information was documented: logmar VA, Goldman IOP, bleb morphology, anterior and posterior segment findings, complications, and laser or surgical interventions. The main indication for this surgical intervention was glaucomatous progression (defined by ongoing visual field deterioration, optic disc changes, and/or disc hemorrhages), or a raised IOP to a level previously known to be associated with glaucoma progression, in the presence of a flat or encapsulated bleb. Choice of surgical approach was decided according to patient preferences, ocular examination findings, details of previous surgery, and risk factors for failure.
Surgical procedure
Surgery was performed either by local or general anesthesia, according to patient’s characteristics and preferences. The technique had common principles, but varied according to intraoperative findings. In all cases a fornix-based conjunctival flap was created in the superior quadrant, with blunt dissection of the subconjunctival space to a distance of over 15 mm behind the limbus and the sclera was exposed. Excessively thickened Tenon’s capsule was excised selectively. Polyvinyl acetal sponges (Visitec, Abingdon, Oxfordshire, UK) soaked in MMC were placed between the conjunctiva and the sclera over the determined filtration area. The MMC concentration varied from 0.1 to 0.5 mg/ml according to each patient’s risk factors, and duration of application was 5 min for all cases. The pre-existing scleral flap was then identified and reopened (Figure 1). In all but one instance a surrounding area was dissected to include the original flap. In one event of a very large original flap, a smaller one was made within the pre-existing one. In eyes with a full-thickness scleral flap defect, the defect was covered with Tenon’s capsule, donor scleral patch graft, or a reflected host scleral flap. Enlargement of the osteum was performed when no free-flow post-scleral flap dissection was observed. The scleral flap was sutured with a combination of 10-0 nylon fixed and releasable sutures. The conjunctiva was closed with interrupted 10-0 nylon mattress sutures. Subconjunctival cefuroxime 125 mg/ml and dexamethasone 3.3 mg/ml were administered at the end of the procedure.
Figure 1.
Schematic diagram of same-site trabeculectomy revision.
Postoperative care
All patients were discharged on topical drops of dexamethasone 0.1% preservative-free 2 hourly and chloramphenicol 0.5% 4 times daily. The antibiotics were discontinued when all conjunctival sutures were removed. The steroids were tapered according to individual bleb findings. All patients were reviewed the following day and at 1 week. Subsequent visits were scheduled as necessitated. During follow-up, if the filtering bleb showed signs of significant subconjunctival scarring or impending failure (increased vascularity, reduction of extend, flattening, and encapsulation), a slit-lamp subconjunctival injection of dexamethasone with or without 5FU was administered.
Outcome measures
Demographic data, including age, sex, ethnicity, glaucoma subtype, ocular history, and number of medications were collected for all patients. Primary outcome measure was IOP. For the purpose of Kaplan–Meier survival analysis success was defined according to the following three criteria.
Criterion 1: IOP ≤21 mm Hg.
Criterion 2: IOP ≤18 mm Hg.
Criterion 3: IOP ≤16 mm Hg.
Absolute success for each criterion was defined as maintaining the desirable IOP without any topical medications, further laser or surgical interventions. Qualified success comprised maintenance of the desirable IOP with topical medication.
Secondary outcomes were change in best-corrected VA, visual field loss, number of glaucoma medications, time from index surgery to revision, need for further laser or surgical intervention, time from surgery to commencement of medications, laser or surgical intervention, complications, and registration as visually impaired.
Statistical analysis
Statistical analysis was undertaken using SPSS v21.0 (SPSS, Chicago, IL, USA). Tests for statistical significance were performed using the χ2 or Fisher’s exact test for discrete variables, Student’s t-test for parametric data, and the Mann–Whitney U-test for non-parametric data. Kaplan–Meier plots were constructed to estimate the probability of IOP survival over time with respect to the set levels of ≤21, ≤18, and ≤16 mm Hg. All data are resented as mean±SD unless otherwise indicated. A P-value of <0.05 was considered statistically significant for the purpose of our analysis.
Results
Demographics and clinical characteristics
A total of 49 patients were identified who had undergone same-site trabeculectomy revision with adjunctive MMC. Forty-five eyes of 39 patients (21 female) were included in the study. One patient lived abroad and follow-up details were not available, as the care had been transferred locally. One patient died 2 months post surgery. Two patients had incomplete note retrieval. The average age of the population was 66.2±13.1 years (range 18–87 years). The majority were Caucasians (31), with 7 African or Caribbean, 2 Asian, and 5 of unknown origin. Of the 45 eyes, 26 were right. Time from initial trabeculectomy to revision was 91.7±79.3 months (range 9–437 months). The mean follow-up was 126±60 months (range 16–227 months). The preoperative VA was 0.25±0.28 (range 0–1.25) and the MD of Humphrey field analysis was −15.8±8.3 (range −31.7 to −0.24). The average preoperative IOP was 24.2±5.5 mm Hg (range 14–38) and the cup-to-disc ration 0.9±0.1 (range 0.6–1.0).
The baseline ocular characteristics are detailed in Table 1. The predominant diagnosis was primary open-angle glaucoma (69%). Twenty-one patients (47%) had coexisting pathology. The primary surgery was augmented with an antimetabolite in 22 cases and non-augmented in 19 cases (45%). Three patients had the initial trabeculectomy elsewhere and intraoperative details were unknown. Thirty-one patients had undergone ocular surgery in addition to primary trabeculectomy. Before surgery, 43 eyes were on topical glaucoma treatment, amongst which 12 eyes were also on systemic acetazolamide.
Table 1. Baseline preoperative ocular characteristics.
| Total number of eyes | 45 |
| Diagnosis | |
| Primary open-angle glaucoma | 31 (69%) |
| Chronic angle-closure glaucoma | 8 (18%) |
| Uveitic glaucoma | 5 (11%) |
| Pseudoexfoliative glaucoma | 1 (2%) |
| Coexisting ocular pathology | |
| Corneal pathology (herpetic endotheliitis, Fuchs endothelial dystrophy) | 2 (4%) |
| Posterior segment pathology (DR, AMD, high myopia) | 10 (22%) |
| Inflammation (uveitis, episcleritis) | 6 (13%) |
| Aqueous misdirection | 1 (2%) |
| Significant cataract | 1 (2%) |
| Previous surgery | |
| One trabeculectomy | 45 (100%) |
| Two trabeculectomies | 1 (2%) |
| Bleb revision | 3 (7%) |
| Bleb needling with 5FU | 2 (4%) |
| Cataract extraction and intraocular lens implantation (phako, extracapsular cataract extraction) | 21 (47%) |
| Surgical iridectomy | 1 (2%) |
| Penetrating keratoplasty | 1 (2%) |
| Antimetabolite at initial trabeculectomy | |
| MMC | 7 (16%) |
| 5FU | 15 (33%) |
| Unknown | 3 (7%) |
| Nil | 21 (57%) |
| B-irradiation | 1 (2%) |
| Preoperative drops | |
| 0 | 2 (4%) |
| 1 | 9 (20%) |
| 2 | 19 (42%) |
| 3 | 11 (24%) |
| 4 | 4 (9%) |
| Preoperative acetazolamide (yes/no) | 12/33 |
Surgical technique, postoperative course, and complications
All patients underwent same-site anterior revision of bleb as described above. In five eyes the sclerostomy was enlarged and in one eye a smaller flap was created inside the old scleral flap. High doses of intraoperative MMC (0.4–0.5 mg/ml) were used in 35/45 eyes. Postoperatively, releasable sutures were removed in 27/45 eyes. Postoperative subconjunctival 5FU 50 mg/ml or dexamethasone 3.3 mg/ml was administered in 35/45 eyes within 8 weeks from surgery. Fifteen eyes (33%) required 1–8 subconjunctival injections of dexamethasone and 20 eyes (44%) required 1–8 subconjunctival injections of 5FU.
Ten eyes suffered early complications (within 2 months from surgery). Five had hypotony, which resolved spontaneously. One case developed hyphema that resolved spontaneously. Three had a conjunctival leak, one of which required suturing twice. The final case was a combined trabeculectomy revision with phacoemulsification. Posterior capsular tear occurred during surgery, which resulted in sulcus implantation of the intraocular lens (IOL). The IOL displayed a mild inferior dislocation immediately postoperatively.
Late complications were noted in three patients. One eye required vitrectomy and repositioning of the dislocated IOL, 25 months post-bleb revision. One case developed malignant glaucoma requiring pars plana vitrectomy and cataract extraction with phacoemulsification, 20 months post index surgery. One case developed endophthalmitis 6 months post surgery. This responded well to therapy.
None of the early or late complications resulted in loss of vision or failure of surgery. None of these eyes required further glaucoma surgery.
Table 2 shows the overall findings at the preoperative visit at 1 year and at final follow-up.
Table 2. Key findings at preoperative visit, year 1 and final follow-up.
|
Preoperative |
1 year |
Last follow-up |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Range | Mean | SD | Range | Mean | SD | Range | |
| LogMAR VA | 0.25 | 0.28 | 0–1.25 | 0.42 | 0.55 | 0–3 | 0.81 | 1.26 | 0–4 |
| IOP (mmHg) | 24.2 | 5.5 | 14–38 | 13.6 | 5.3 | 6–22 | 12.4 | 5.52 | 6–40 |
| No. of drops | 2.1 | 1.05 | 0–4 | 0.2 | 1.21 | 0–3 | 1.1 | 1.23 | 0–4 |
| MD (db) | −15.8 | 8.3 | −31.68– (−0.24) | −15.72 | 8.98 | −34.28– (+1.00) | |||
Abbreviations: db, decibel; IOP, intraocular pressure; MD, mean deviation; SD, standard deviation; VA, visual acuity.
IOP outcomes
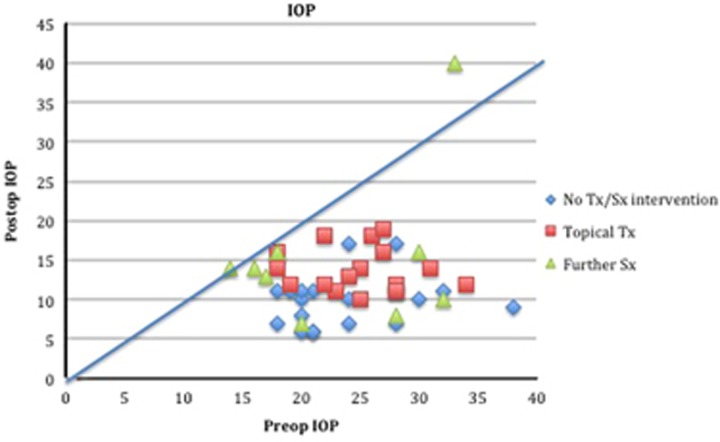
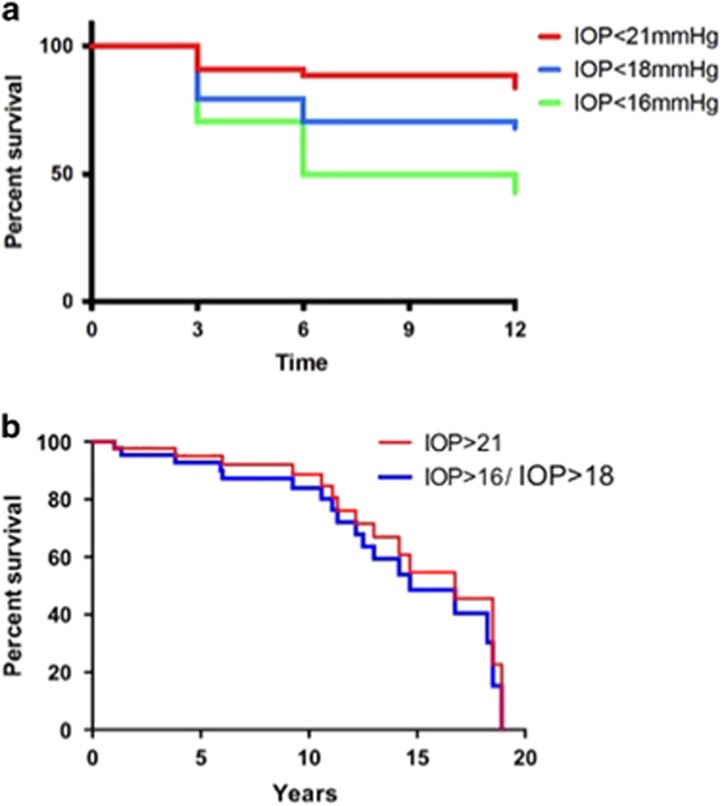
A scatter plot indicating how preoperative IOP compared with postoperative IOP is shown in Figure 2. Kaplan–Meier survival curves, for the first year and last follow-up, are shown in Figure 3.
Figure 2.
Scattergram of preoperative vs postoperative IOP during follow-up period. Each point represents one eye showing the preoperative IOP value on the abscissa and the postoperative IOP values on the ordinate, respectively. Rhombuses represent patients who did not require any further medical or surgical intervention. Rectangles represent patients who were on topical medications. Triangles represent patients who underwent further surgical treatment.
Figure 3.
(a) Kaplan–Meier survival curves of the cumulative probability of success until 12 months, defining failure as IOP >21, >18, and >16 mm Hg. (b) Kaplan–Meier survival curves of the cumulative probability of success at last follow-up, defining failure as IOP >21, >18, and >16 mm Hg.
There was a significant decrease in IOP after surgery at all measured time intervals (P<0.001). At 12 months, mean IOP was 13.6±5.10 mm Hg (range 6–22 mm Hg) and at last follow-up mean IOP was 12.4±5.45 mm Hg (range 6–40 mm Hg). Requirement for topical medications dropped from a mean of 2.1 (range 0–4 drops) to 0.2 (range 0–3 drops) the first year (P<0.001) and to 1.1 (range 0–4 drops) at last follow-up (P<0.001; Table 2).
Success proportions for the first year and last follow-up, according to our predefined criteria, are provided in Table 3. Absolute success was higher at year 1 and at last follow-up for all three criteria. One case failed according to all success criteria at year 1 and at last follow-up. This patient was Caribbean in origin, suffered from both uveitis and proliferative diabetic retinopathy, with recurrent vitreous hemorrhages, and underwent a second redo-trabeculectomy 52 months post index surgery, which also failed. Nine cases (20%) underwent further glaucoma surgery during the follow-up period. All of those eyes achieved a final IOP ≤16 mm Hg with (eight eyes) or without (one eye) topical treatment during the last follow-up.
Table 3. Success proportions for the first year and the last follow-up, according to the three IOP criteria.
| Success proportion | ≤21 mm Hg (criterion 1) | ≤18 mm Hg (criterion 2) | ≤16 mm Hg (criterion 3) |
|---|---|---|---|
| 1 year | |||
| Overall | 40 (89%) | 35 (78%) | 29 (65%) |
| Absolute | 35 (78%) | 31 (69%) | 26 (58%) |
| Qualified | 5 (11%) | 4 (9%) | 3 (7%) |
| Last follow-up | |||
| Overall | 43 (96%) | 41 (91%) | 38 (84%) |
| Absolute | 17 (38%) | 17 (38%) | 15 (33%) |
| Qualified | 26 (58%) | 24 (53%) | 23 (51%) |
VA outcomes
VA changes after the revision of surgery are shown in Table 3. The visual field MD did not change to any major extent. The same cannot be said however for VA which dropped by 0.3 logMAR in 11 eyes (23%). Four eyes had macular degeneration, two had diabetic ischemic maculopathy, and two pseudophakic eyes developed decompensated corneas post cataract extraction. The final three eyes had advanced glaucoma and the loss of vision was attributed to this. The eye that developed malignant glaucoma and underwent pars plana vitrectomy and cataract extraction also lost significant vision.
Other outcomes
Contingency tables were constructed and risk factors for failure explored (Pearson’s χ2). Ethnicity (χ2 P=0.191), age (<70 years old or above; χ2 P=0.309), previous surgery (χ2 P=0.29), coexisting pathology (χ2 P=0.32), and number of preoperative drops (x2 P=0.783) did not have an influence on survival. If ethnicity is made binary Caucasian/non-Caucasian, the second group appeared more likely to fail (P=0.046).
Time from revision to recommencement of glaucoma medication was 42.03±44.79 (range 0–141 months). Twenty-six patients (54%) were on topical glaucoma treatment at last follow-up (1–4 drops). Time from revision to new surgery or laser intervention was 40.7±37.5 (range 1–136 months). Nine eyes (19%) required further glaucoma surgery. The latter involved further trabeculectomy surgery in five, bleb needling in one, and aqueous shunt insertion in three eyes. Nine eyes (24%) required further glaucoma laser surgery by means of cyclodiode ciliary body ablation. Fifteen eyes (33%) underwent other ocular surgery. Eleven eyes (23%) had cataract extraction with phacoemulsification and IOL implantation. Four eyes (9%) underwent surgery as a result of early or late complications, as mentioned in the complications section above. At last follow-up 11 patients (24%) were registered sight impaired.
Discussion
Trabeculectomy outcomes have improved over the years, with a trend for highly proactive postoperative care, achieving better IOP control with lower numbers of complications.2 However, multiple risk factors may lead to failure and a previously failed trabeculectomy increases this risk further.14, 15
Trabeculectomy bleb failure is a result of increased aqueous resistance at one of the three following levels: the internal sclerostomy; the scleral flap; or the subconjunctival space. The latter is recognized as the most common area of resistance.3, 16 Same-site bleb revision may act on any of these levels. It can enlarge an inadequately sized or blocked sclerostomy, re-open and correct the scleral flap size, and inhibit postoperative scarring with the adjunctive application of an antimetabolite. It preserves the optimum bleb position with superior filtration, preserves conjunctiva and underlying tissues for further surgery, and minimizes intraocular inflammation, by not repeating peripheral iridectomy. Operating in a previously used surgical field has also disadvantages though. Dissecting tissues may prove challenging due to excessive scarring or bleeding. The underlying tissues may reveal atrophic areas or full-thickness scleral defects that make closure difficult or require additional patch grafts. Dissection outside the original flap area provides sound tissue for securing the flap and frequently the dissection can go beneath the original scared flap allowing a complete new flap to be raised for suturing and postoperative management as in a primary trabeculectomy. Titration of intraoperative MMC dose is also a challenge, so as to achieve optimum antiscarring effect, but prevent the complications of avascular blebs and late leaks.17 Postoperative management remains an art rather than a science, when deciding on the optimum timing for suture removal and subconjunctival injections or needling procedures. Therefore, this method requires an experienced surgeon.
This study presents the long-term outcomes of this surgical technique. We chose three different criteria to report success. Criterion 1 (IOP <21 mm Hg) was chosen to facilitate comparison with other studies, as it has been the commonest cutoff point of success. Criterion 2 was based on the Advanced Glaucoma Intervention Study outcome that IOP <18 mm Hg may prevent visual filed loss over a 10-year period in eyes with advanced glaucoma.11 The third and most stringent criterion was chosen because a significant number of patients in this study had advanced glaucoma (mean baseline MD: −15.27) and required low IOP levels.
Same-site surgical revision of failed bleb has been described in a small number of studies, amongst which only two have used MMC augmentation.13, 18, 19, 20 It is difficult to compare the results in view of the significant diversity in the surgical techniques, success criteria, and postoperative management. The first study by Hara et al20 has been reported in the Japanese language literature. For a follow-up period of on average 39.8 months, they report absolute and overall success proportions of 53.4% and 60.2%, respectively, for IOP<21 mm Hg. These appear to be different to ours, which were 43% and 98%, respectively, at last follow-up and for the same success criterion. However, surgical and postoperative details are not available to explore possible causes.
Anand and Arora13 have published the only study in the English language literature that reports outcomes of reopening the scleral flap in failed filtration surgery, with MMC 0.2 mg/ml enhancement. They presented a retrospective review of 54 eyes that underwent a surgical procedure very similar to the one performed in our study. Follow-up was 39±10 months and population had very similar baseline clinical characteristics to our study. They defined success as an IOP <18 mm Hg and 20% decrease from preoperative IOP, and absolute and qualified success were 38% and 64%, respectively, 3 years post index surgery. These results appear to be comparable to our success rates of 43% and 53%, without or with treatment, respectively, using a similar definition of success at last follow-up. However, in the aforementioned study 51.8% of the population underwent further glaucoma surgery (42.5 needling and 9.3% other glaucoma procedures) to achieve this level of success. Conversely, in our study only 19% required further glaucoma operations. We propose that using intraoperatively high doses of MMC (0.4–0.5 mg/ml in 78% of cases), in combination with highly proactive postoperative care, including subconjunctival injections of dexamethasone (30%) and/or 5FU (43%), contributed to the reduced need for further glaucoma surgery. Anand et al report higher proportions of postsurgical complications, such as hyphema (20 vs 2%), choroidal effusions (17 vs 4%), and conjunctival leak (22 vs 6%). A possible explanation could lie in the technique of scleral flap and conjunctival suturing. In both studies complications did not result in significant loss of vision. In our study none of these compilations led to further glaucoma surgery. In the tube vs trabeculectomy study, eligible eyes had undergone either cataract surgery or failed trabeculectomy, and were subsequently randomized to either second trabeculectomy or glaucoma tube surgery. Overall complications were again more frequently reported, 57% in the trabeculectomy group and 34% in the tube group. In addition to possible variations in surgical technique, the recoding of complications may be more accurate in a randomized controlled trial than in retrospective case series.
In the case series described by Coote and associates, bleb revision has been described through a posterior approach. Surgery involved fornix incision with opening of the scleral flap posteriorly at the same site of previous trabeculectomy and application of 0.2–0.4 mg/ml MMC. The probability of maintaining IOP ≤15 mmg without treatment at 5 years was 84%. This success proportion is significantly higher than any previously reported case series. Detailed clinical characteristics and ophthalmic history are not reported, however the cohort of patients included a significant proportion of elderly Caucasian patients at a lower risk for failure.9
It is important to note that a quarter of the eyes, in our case series, lost 0.3 logMAR or more vision over the period of follow-up. Despite many eyes having severe glaucoma, in three quarters of these instances this was due to non-glaucomatous pathology.
The limitations of this study are intrinsic to the retrospective nature of case series. The index surgery was performed by more than one surgeon, and the intraoperative technique and antimetabolite differed amongst cases. Time from index surgery to revision varied significantly from 9 to 437 months. There was a noticeable variation in the nature and number of previous surgeries. The surgical technique of revision, despite common principles, differed according to findings. These factors may have influenced clinical outcomes. Unfortunately, adjustments for these factors by statistical techniques are limited by the small number of these case series.
To date this study represents one of the largest reported series, with the longest follow-up, of patients who have undergone same-site bleb revision for trabeculectomy failure. Although multiple methods exist for managing failed blebs, our surgical technique, described above, was proven to be a safe and effective method for reviving filtering blebs and controlling IOP long term. In an era of worldwide austerity, where aqueous shunts are not always available in National Health Systems, it would be very useful for ophthalmic surgeons to be aware of outcomes of a technique that could be used for a proportion of patients requiring tube surgery.
Acknowledgments
Author contributions
Conception and design of the study: EN and IM; conduct of the study: EN; analysis and interpretation of data: EN and IM; writing of the article: EN and IM; critical revision of the article: EN and IM; final approval of the article: EN and IM.
Footnotes
The authors declare no conflict of interest.
References
- Cairns JE. Trabeculectomy. Preliminary report of a surgical method of reducing intra-ocular pressure in chronic simple glaucoma without sub-conjunctival drainage of aqueous humor. Bibl Ophthalmol 1970; 81: 143–153. [PubMed] [Google Scholar]
- Kirwan JF, Lockwood AJ, Shah P, Macleod A, Broadway DC, King AJ et al. Trabeculectomy in the 21st century: a multicenter analysis. Ophthalmology 2013; 120(12): 2532–2539. [DOI] [PubMed] [Google Scholar]
- Skuta GL, Parrish RK 2nd. Wound healing in glaucoma filtering surgery. Surv Ophthalmol 1987; 32(3): 149–170. [DOI] [PubMed] [Google Scholar]
- Khaw PT, Chiang M, Shah P, Sii F, Lockwood A, Khalili A. Enhanced trabeculectomy: the Moorfields Safer Surgery System. Dev Ophthalmol 2012; 50: 1–28. [DOI] [PubMed] [Google Scholar]
- Five-year follow-up of the Fluorouracil Filtering Surgery Study. The Fluorouracil Filtering Surgery Study Group. Am J Ophthalmol 1996; 121(4): 349–366. [DOI] [PubMed] [Google Scholar]
- Gedde SJ, Schiffman JC, Feuer WJ, Herndon LW, Brandt JD, Budenz DL et al. Treatment outcomes in the Tube Versus Trabeculectomy (TVT) study after five years of follow-up. Am J Ophthalmol 2012; 153(5): 789–803. e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broadway DC, Bloom PA, Bunce C, Thiagarajan M, Khaw PT. Needle revision of failing and failed trabeculectomy blebs with adjunctive 5-fluorouracil: survival analysis. Ophthalmology 2004; 111(4): 665–673. [DOI] [PubMed] [Google Scholar]
- Maestrini HA, Cronemberger S, Matoso HD, Reis JR, Merula RV, Filho AD et al. Late needling of flat filtering blebs with adjunctive mitomycin C: efficacy and safety for the corneal endothelium. Ophthalmology 2011; 118(4): 755–762. [DOI] [PubMed] [Google Scholar]
- Coote MA, Gupta V, Vasudevan S, Crowston JG. Posterior revision for failed blebs: long-term outcomes. J Glaucoma 2011; 20(6): 377–382. [DOI] [PubMed] [Google Scholar]
- Olali C, Rotchford AP, King AJ. Outcome of repeat trabeculectomies. Clin Exp Ophthalmol 2011; 39(7): 658–664. [DOI] [PubMed] [Google Scholar]
- Ederer F, Gaasterland DA, Dally LG, Kim J, VanVeldhuisen PC, Blackwell B et al. The Advanced Glaucoma Intervention Study (AGIS): 13. Comparison of treatment outcomes within race: 10-year results. Ophthalmology 2004; 111(4): 651–664. [DOI] [PubMed] [Google Scholar]
- You YA, Gu YS, Fang CT, Ma XQ. Long-term effects of simultaneous subconjunctival and subscleral mitomycin C application in repeat trabeculectomy. J Glaucoma 2002; 11(2): 110–118. [DOI] [PubMed] [Google Scholar]
- Anand N, Arora S. Surgical revision of failed filtration surgery with mitomycin C augmentation. J Glaucoma 2007; 16(5): 456–461. [DOI] [PubMed] [Google Scholar]
- Broadway DC, Chang LP. Trabeculectomy, risk factors for failure and the preoperative state of the conjunctiva. J Glaucoma 2001; 10(3): 237–249. [DOI] [PubMed] [Google Scholar]
- Law SK, Shih K, Tran DH, Coleman AL, Caprioli J. Long-term outcomes of repeat vs initial trabeculectomy in open-angle glaucoma. Am J Ophthalmol 2009; 148(5): 685–95 e1. [DOI] [PubMed] [Google Scholar]
- Khaw PT, Chang L, Wong TT, Mead A, Daniels JT, Cordeiro MF. Modulation of wound healing after glaucoma surgery. Curr Opin Ophthalmol 2001; 12(2): 143–148. [DOI] [PubMed] [Google Scholar]
- Anand N, Khan A. Long-term outcomes of needle revision of trabeculectomy blebs with mitomycin C and 5-fluorouracil: a comparative safety and efficacy report. J Glaucoma 2009; 18(7): 513–520. [DOI] [PubMed] [Google Scholar]
- Cohen JS, Shaffer RN, Hetherington J Jr, Hoskins D. Revision of filtration surgery. Arch Ophthalmol 1977; 95(9): 1612–1615. [DOI] [PubMed] [Google Scholar]
- Swan K. Reopening of nonfunctioning filters—simplified surgical techniques. Trans Sect Ophthalmol Am Acad Ophthalmol Otolaryngol 1975; 79(2): OP342–OP348. [PubMed] [Google Scholar]
- Hara T, Shirato S. [Surgical revision of failed filtering bleb with mitomycin C]. Nippon Ganka Gakkai Zasshi 1997; 101(6): 516–519. [PubMed] [Google Scholar]