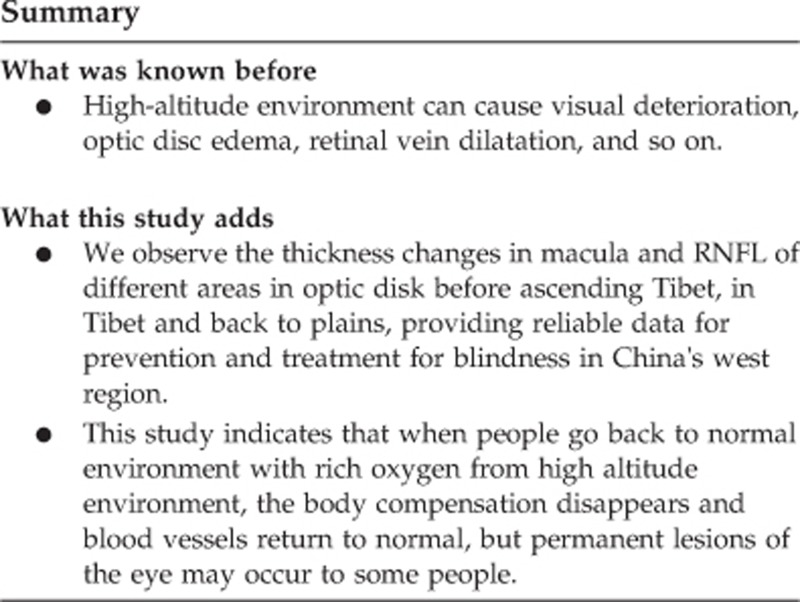
Abstract
Purpose
To determine what impact rapid ascension to a high-altitude environment has on the retina with the aim of preventing and treating high-altitude oculopathy.
Patients and methods
Participants in the study were members of the Chinese military assigned to the high-altitude environment of the Tibetan plateau. Ninety-one participants were enrolled in the study. Optical coherence tomography was used to measure the thickness of retina-related indicators. Measurements were taken before and after exposure to the high-altitude environment and upon return to the baseline altitude.
Results
Following exposure to the high-altitude environment in Tibet, there was a significant increase in retinal nerve fiber layer (RNFL) thickness in the temporal and nasal quadrants of the optic disc, whilst a significant decrease in RNFL thickness in the inferior optic disc was also observed. A significant increase in RNFL thickness in the superior and inferior macula was also evident, along with a significant increase in the ganglion cell layer thickness in the superior macula. Upon return to the baseline altitude, all measurements returned to baseline levels except for the RNFL of the inferior macula, which was significantly thicker. Pathological changes were also documented in the eyes of nine participants upon returning to baseline altitude, including ischemic optic neuropathy, myopia, and cortical amaurosis.
Conclusions
The high-altitude environment can have a negative impact on the health of the retina and may contribute to the incidence of various eye diseases. This study deepens the understanding of what impact a high-altitude environment has on retina and provides reliable data for blindness prevention and treatment.
Introduction
Tibet, with an average altitude above 4000 m, is often referred to as the ‘roof of the world’. As a consequence of its high altitude, environmental factors such as low atmospheric oxygen, low humidity, strong ultraviolet radiation, and low temperatures are prevalent. Given the current political climate surrounding Tibet and neighboring China, it is possible for members of the Chinese military to be assigned to the Tibetan plateau at short notice. However, when military personnel ascend to the Tibetan plateau, they are likely to suffer from a range of symptoms prompted by acute oxygen deficiency, of which ocular disorders are common.1, 2 The incidence of high-altitude oculopathy can be dependent or independent of other altitude-induced disorders and it is therefore imperative to study the epidemiological and pathogenic basis of these ocular manifestations to understand, and ultimately to prevent their occurrence. As there are few studies describing acute high-altitude oculopathy and its long-term prognosis, this study aimed to describe the effects on the retina from rapidly entering a high-altitude environment and returning to baseline altitude.
Materials and methods
Participants
Informed consent was obtained from all participants in the study. All procedures performed were in accordance with the ethical standards of the ethics committee of the 153rd Central Hospital of PLA (Zhengzhou, China) and with the 1964 declaration of Helsinki. Participants in the study were military personnel who set out from baseline altitude through mechanical delivery (at about 100 m above sea level) and based in a training facility (4600 m above sea level) in Tibet in 2015. One month after entering Tibet, optical coherence tomography (OCT) was used to evaluate the retinal structure of 156 military personnel. Exclusion criteria included participants with myopia, glaucoma, astigmatism, or any other condition which may be detrimental to ocular health. After excluding those who did not meet the inclusion criteria, 91 healthy participants were included in the study and their health reports (1 week before ascent to Tibet) were obtained. In addition, none of the 91 participants had altitude sickness or took any medication including acetazolamide during the research. The cohort consisted of 82 males and nine females, with an average age of 28.7±7.4 years (range 18–49 years). From this cohort, 23 participants were followed-up and underwent two retinal examinations at intervals of 1 month and 3 months after returning to baseline altitude (at about 100 m above sea level). This group consisted of 18 males and five females, with an average age of 32.0±5.9 years (range 20–45 years).
Methods
OCT is a non-invasive, non-contact micron resolution imaging technology which uses optical coherence to obtain internal tomographic structure. In this study, a three-dimensional (3D) OCT-2000 unit (Topcon Medical Systems, Tokyo, Japan) was employed to determine the thickness of the retinal nerve fiber layer (RNFL) and ganglion cell layer (GCL) in the macula and the RNFL of the optic disc. Two scanning modes were employed as follows: (1) macula: a 512 × 128 resolution 3D tomography scan was centered on the fovea to measure the thickness of the RNFL and GCL in the superior and inferior areas of the macula; (2) optic disc: a 3D tomography scan with a circular diameter of 3.4 mm (centered on the optic disc) was conducted to obtain RNFL thickness in the superior, inferior, nasal, and temporal quadrants of the optic disc. After scanning, image analysis was undertaken using software included within the 3D OCT-2000 system (version 8.0).
Statistical analysis
SPSS version 19.0 software (IBM, New York, USA) was used for all statistical analyses. A student’s t-test was used to compare the group means, with a P<0.05 accepted as statistically significant.
Results
In this study, we investigated the retina of the military personnel before, during and after their posting. As shown in Table 1, changes in the thickness of the RNFL and GCL in the participants were evident following their ascent to high altitude. In the macula, there was a significant increase in the thickness of the RNFL in the superior and inferior quadrants and of the GCL in the superior quadrant (P<0.05). However, the difference in thickness of the GCL in the inferior quadrant was not significant (P>0.05). In the optic disc, there was also a significant increase in the thickness of the RNFL in the nasal and temporal quadrants following ascent to high altitude (P<0.05), with an insignificant increase in mean RNFL and RNFL thickness in the superior quadrant also documented (P>0.05). Intriguingly, the thickness of the RNFL in the inferior quadrant decreased significantly (P<0.05).
Table 1. Retinal nerve fiber layer and ganglion cell layer thickness before and after ascension into Tibet (x±s, μm).
| Checkpoint | Parameters | Before ascent to Tibet (N=91) | After ascent to Tibet (N=91) | t | P |
|---|---|---|---|---|---|
| Macular area | Superior nerve fiber layer | 32.05±2.83 | 36.81±5.31 | −4.516 | 0.000 |
| Inferior nerve fiber layer | 32.55±1.95 | 39.49±6.00 | −7.883 | 0.000 | |
| Superior ganglion cell layer | 70.60±2.14 | 73.54±6.48 | −3.066 | 0.004 | |
| Inferior ganglion cell layer | 70.00±3.26 | 71.59±6.22 | −1.307 | 0.208 | |
| Optic disc | Superior area | 123.70±10.93 | 124.38±12.46 | −0.184 | 0.857 |
| Inferior area | 127.35±13.60 | 115.96±14.18 | 2.503 | 0.029 | |
| Nasal area | 70.10±7.07 | 82.49±10.82 | −4.941 | 0.000 | |
| Temporal area | 69.60±5.53 | 80.20±11.02 | −5.062 | 0.000 | |
| Mean thickness | 97.69±5.59 | 100.76±8.67 | −1.546 | 0.144 |
P<0.05 indicates significant difference.
Two follow-up examinations were performed on 23 participants following their return to baseline altitude, with the results shown in Table 2. After returning from the high-altitude environment, the thickness of the RNFL in the inferior quadrant of the optic disc increased, whereas it decreased in the remaining areas of the optic disc and macula. The only measurements to not experience a significant change in the two examinations were those for the thickness of the GCL in the superior and inferior areas of the macula, the RNFL thickness in the superior and inferior areas and the mean RNFL thickness of the optic disc (P>0.05).
Table 2. Results of two examinations upon return to the baseline altitude (x±s, μm).
| Checkpoint | Parameters | After ascent to Tibet (N=23) | The first examination (N=23) | The second examination (N=23) |
Comparison of the two examinations |
|
|---|---|---|---|---|---|---|
| t | P | |||||
| Macular area | Superior nerve fiber layer | 35.65±4.21 | 35.52±3.98 | 33.02±3.22 | 2.340 | 0.024 |
| Inferior nerve fiber layer | 38.50±5.06 | 37.37±5.20 | 34.48±3.94 | 2.125 | 0.040 | |
| Superior ganglion cell layer | 71.48±5.66 | 71.59±6.12 | 70.48±7.07 | 0.569 | 0.573 | |
| Inferior ganglion cell layer | 69.41±5.92 | 69.85±6.20 | 69.63±7.09 | 0.111 | 0.912 | |
| Optic disc | Superior area | 123.47±10.50 | 125.09±9.71 | 119.61±13.37 | 1.590 | 0.120 |
| Inferior area | 113.83±11.52 | 117.98±11.68 | 124.73±12.83 | −1.869 | 0.068 | |
| Nasal area | 80.57±9.97 | 79.15±8.00 | 72.91±8.09 | 2.630 | 0.012 | |
| Temporal area | 78.43±11.48 | 80.54±10.91 | 73.21±8.65 | 2.524 | 0.016 | |
| Mean thickness | 99.08±7.23 | 100.69±7.02 | 97.62±6.90 | 1.496 | 0.142 | |
P<0.05 indicates significant difference.
Comparison of the RNFL and GCL thickness readings taken before ascent to high altitude and from the second examination upon return to baseline altitude are shown in Table 3. All of the measurement areas showed no significant change in RNFL or GCL thickness (P>0.05) except for the inferior quadrant of the macula, where the RNFL became significantly thicker (P<0.05). Consequently, it could be concluded that after the participants returned to baseline altitude, their retinal anatomy generally recovered to normal without pathological changes. Results also showed one participant did develop ischemic optic neuropathy, two developed cortical amaurosis and six demonstrated signs of permanent myopia (200–300°), which subsequently recovered to ~150°.
Table 3. Retinal nerve fiber layer and ganglion cell layer thickness at baseline altitude before and after the ascension into Tibet (x±s, μm).
| Check point | Parameters | Before ascent to Tibet (N=23) | The second examination upon return to baseline altitude (N=23) | t | P |
|---|---|---|---|---|---|
| Macular area | Superior nerve fiber layer | 31.66±3.10 | 33.02±3.35 | −1.446 | 0.155 |
| Inferior nerve fiber layer | 32.43±2.15 | 34.48±4.04 | −2.176 | 0.037 | |
| Superior ganglion cell layer | 70.50±2.12 | 70.48±7.05 | 0.014 | 0.989 | |
| Inferior ganglion cell layer | 70.18±2.40 | 69.63±7.05 | 0.353 | 0.727 | |
| Optic disc | Superior area | 125.14±11.24 | 119.61±14.28 | 1.504 | 0.140 |
| Inferior area | 128.48±13.00 | 124.73±13.60 | 0.971 | 0.337 | |
| Nasal area | 68.18±10.60 | 72.91±15.68 | −1.678 | 0.101 | |
| Temporal area | 68.64±8.88 | 73.21±13.59 | −1.751 | 0.087 | |
| Mean thickness | 97.61±6.89 | 97.62±28.48 | −0.006 | 0.995 |
P<0.05 indicates significant difference.
Discussion
In a high-altitude environment, factors such as low atmospheric oxygen, low humidity, and strong ultraviolet radiation can induce a series of pathophysiologic phenomena that can result in disorders of the cardiovascular, respiratory, and ocular systems. The first report of this ocular phenomenon was published in 1968, where Singh et al3 observed one case of a papilledema, retinal vein dilation, and retinal hemorrhage and three cases of vitreous hemorrhage in individuals who had ascended to a high altitude for a short period of time. In 1970, Frayser et al4 reported nine cases of retinal hemorrhage and tortuositas vasorum retinae, including one case with acute headache and choked disc, in individuals who had ascended to high altitude. As a consequence of these reports, Chinese researchers became concerned with the health of communities living in the high-altitude regions of areas like Tibet and Qinghai and subsequently undertook their own studies over the following decades.
In a study by Yi,5 patients treated in an ophthalmology clinic over 8 years in Tibet were observed for symptoms of high-altitude oculopathy, with many of them diagnosed with bulbar conjunctival vascular dilatation, pterygium, cataract, visual dysfunction, and high intraocular pressure. Zhang6 analyzed 48 adults with a visual acuity <0.5 logMAR who had migrated to Tibet and found that in 10 of them, their decreased vision was caused by cataracts probably induced by chronic hypoxia and long-term ultraviolet radiation, and other reasons included retinal hemorrhage and maculopathy. Furthermore, Wang et al has reported a clinical case of sharply decreased vision caused by plateau hypoxia,7 indicating that people without acclimatization have a higher incidence and severity of high-altitude oculopathy. Therefore, it is important to understand the prevalence of high-altitude oculopathy and to ultimately use this information to aid in the prevention and treatment of this condition. Currently, the majority of studies start observing changes inside the eye using modern advanced instrumentation instead of only investigating the surface of the eye. Fischer et al8 adopted OCT and microdetermination to quantify changes in central retinal structure and function of 14 healthy subjects during rapid ascent to a high-altitude area (4559 m), and results found an increase of total retinal thickness. Ascaso et al9 employed OCT to conduct complete ophthalmologic examinations for 12 healthy male mountaineers after four high-altitude expeditions in the Himalayas, and results indicated that average peripapillary RNFL thickness as well as the RNFL thickness of superior and temporal quadrants got a notable increase and that VIRA was much higher than that at baseline altitude. In this study, OCT was also used to determine the fine structure of retina such as thickness of the RNFL and GCL in the macula and the RNFL in the optic disc.
According to the findings from this study, Chinese military personnel who entered Tibet had a thicker RNFL in the superior and inferior quadrants of the optic disc and a thinner RNFL in the nasal and temporal quadrants. These findings were consistent with the histological distribution of the RNFL from other studies.10, 11 A month after the personnel entered Tibet, there were significant changes in their retinae and upon returning to baseline altitude for 3 months, most readings were back to normal. However, ocular lesions including ischemic optic neuropathy, permanent myopia and cortical amaurosis were observed in nine people.
Abnormal thickness of the macula and the RNFL in the optic disc is associated with numerous ocular disease states. Thinning of the RNFL is a characteristic trait of glaucoma12, 13 and changes in RNFL thickness are evident in patients with myopia.14, 15 Furthermore, RNFL thickness is increased in individuals with amblyopia,16 and the thickness of the GCL in the macula is increased in patients with diabetes.17 Environmental conditions including low atmospheric oxygen, low humidity, and high ultraviolet radiation, which are experienced in high-altitude environments such as the Tibetan plateau, can also cause changes in RNFL and GCL thickness. According to a study conducted on the retinae of rescuers who rapidly entered a high-altitude environment, the ascent caused retinal vascular filling and expanding, with severity positively correlated with altitude.18 In 2014, Willmann et al19 reviewed previous studies linked to HACE as well as retina and optic nerve at high-altitude environment and discussed the relevance of acute mountain sickness to the swelling of optic disc, the increasing of retinal vessel diameter and vascular leakage. In the same year, Willmann et al20 used semi-automated vascular chart software to analyze infrared picture of eye fundus obtained from HRA+OCT and first quantified the changes of retinal vessel diameter at an altitude of 4559 m, and the results indicated the correlation between retinal venous distention and HAH level. As suggested above, high altitude can result in retinopathy, and the reason may be that hypoxic conditions at high-altitude cause retinal microcirculation disorder, arteriovenous filling and expanding and even papilledema. Consequently, this could explain why the military personnel involved in our study had a thicker RNFL in the optic disc after ascending to the Tibetan plateau. Furthermore, increasing macular thickness is associated with vascular dilatation and changes in vascular permeability.21 Three months after the military personnel returned to baseline altitude, their retinal condition had recovered to its normal state, demonstrating that increases in atmospheric oxygen were able to restore nerve and blood vessel function. In addition, some participants in our study did develop permanent ocular lesions, indicating that individuals who reside in high-altitude environments need to be aware of the risk of developing ocular disease.
In summary, this study employed OCT to investigate structural and functional changes in the retinae of Chinese military personnel who rapidly ascended to the high-altitude environment of the Tibetan plateau, indicating that the novel imaging technique can monitor the disease progress accurately and intuitively. We found that temporary alterations in the thickness of the RNFL and GCL were evident. In addition, some personnel also developed permanent ocular lesions upon returning to baseline altitude. The application of OCT provides basis for the application and breakthrough of some key technologies in the field of fundus image processing. These findings assist in understanding the effect of rapid ascent to high-altitude environment on retina, and provide theoretical foundation and monitoring method for prevention of high-altitude oculopathy.
Acknowledgments
This work was supported by Scientific Research General Program of Joint logistics Department in Southwest Military Area Command Jinan Military Area Command; Grant: CJN15J084.
Footnotes
The authors declare no conflict of interest.
References
- Fu R, Zhang X, Liu BC, Chen CJ, Yi GR. A survey of stereoscopic vision function of 226 soldiers in high altitude areas. J Third Mil Med Univ 2005; 27: 66–75. [Google Scholar]
- Yang J. A survey on crystalline lens of 370 officers of Han nationality 4000 meters above the sea level. Chin J Ocul Trauma Occup Eye Dis 2000; 22: 559. [Google Scholar]
- Singh I, Khanna PK, Srivastava MC. Acute mountain sickness. New Engl J Med 1969; 280: 143–145. [DOI] [PubMed] [Google Scholar]
- Frayser R, Houston CS, Bryan AC, Rennie ID, Gray G. Retinal hemorrhage at high altitude. New Engl J Med 1970; 282: 1183–1184. [DOI] [PubMed] [Google Scholar]
- Yi GR. The eye manifestation of altitude sickness. Chin J Pract Ophthalmol 1996; 14: 200–202. [Google Scholar]
- Zhang J. Analysis on reason of 48 adult patients with impaired vision. Med J Natl Defending Forces Southwest China 1999; 9: 299–301. [Google Scholar]
- Wang CX, Wang HY. Report of a case of impaired vision caused by Plateau hypoxia. Clin J Med Off 2006; 34: 346. [Google Scholar]
- Fischer MD, Willmann G, Schatz A, Schommer K, Zhour A, Zrenner E et al. Structural and functional changes of the human macula during acute exposure to high altitude. PLoS One 2012; 7: e36155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ascaso FJ, Nerín MA, Villén L, Morandeira JR, Cristóbal JA. Acute mountain sickness and retinal evaluation by optical coherence tomography. Eur J Ophthalmol 2012; 22: 580–589. [DOI] [PubMed] [Google Scholar]
- Medeiros FA, Zangwill LM, Bowd C, Vessani RM, Susanna Jr R, Weinreb RN. Evaluation of retinal nerve fiber layer, optic nerve head, and macular thickness measurements for glaucoma detection using optical coherence tomograpgy. Am J Ophthalmol 2005; 139: 44–55. [DOI] [PubMed] [Google Scholar]
- Varma R, Bazzaz S, Lai M. Optical tomography-measured retinal nerve fiber layer thickness in normal latinos. Invest Ophthalmol Vis Sci 2003; 44: 3369–3373. [DOI] [PubMed] [Google Scholar]
- Fortune B, Cull G, Reynaud J, Wang L, Burgoyne CF. Relating retinal ganglion cell function and retinal nerve fiber layer (RNFL) retardance to progressive loss of RNFL thickness and optic nerve axons in experimental glaucoma. Invest Ophthalmol Vis Sci 2015; 56: 3936–3944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suh MH, Yoo BW, Park KH, Kim H, Kim HC. Reproducibility of spectral-domain optical coherence tomography RNFL map for glaucomatous and fellow normal eyes in unilateral glaucoma. J Glaucoma 2015; 24: 238–244. [DOI] [PubMed] [Google Scholar]
- Zhao JJ, Zhuang WJ, Yang XQ, Li SS, Xiang W. Peripapillary retinal nerve fiber layer thickness distribution in Chinese with myopia measured by 3D-optical coherence tomography. Int J Ophthalmol 2013; 6: 626–631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi JA, Kim JS, Park HY, Park H, Park CK. The foveal position relative to the optic disc and the retinal nerve fiber layer thickness profile in myopia. Invest Ophthalmol Vis Sci 2014; 55: 1419–1426. [DOI] [PubMed] [Google Scholar]
- Chen W, Chen J, Huang J, Xu J, Zhang F, Lu F. Comparison of macular and retinal nerve fiber layer thickness in untreated and treated binocular amblyopia. Curr Eye Res 2013; 28. [DOI] [PubMed] [Google Scholar]
- Kim JJ, Im JC, Shin JP, Kim IT, Park DH. One-year follow-up of macular ganglion cell layer and peripapillary retinal nerve fibre layer thickness changs after panretinal photocoagulation. Br J Ophthalmol 2014; 98: 213–217. [DOI] [PubMed] [Google Scholar]
- He L, Li J, Lv HD, Su F, Wang JB. Impacts of different altitudes on retinal blood vessels of relief personnel after the emergent entry into Plateau. Chin J Dis Med 2014; 2: 439–444. [Google Scholar]
- Willmann G, Gekeler F, Schommer K, Bärtsch P. Update on high altitude cerebral edema including recent work on the eye. High Alt Med Biol 2014; 15: 112–122. [DOI] [PubMed] [Google Scholar]
- Willmann G, Fischer MD, Schommer K, Bärtsch P, Gekeler F, Schatz A. Missing correlation of retinal vessel diameter with high-altitude headache. Ann Clin Transl Neurol 2014; 1: 59–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li L, Guan RJ, Zhang R. The curative effect observation about the treatment of Lucentis in choroid neovascularization of high altitude. Chin J Pract Ophthalmol 2015; 33: 528–531. [Google Scholar]


