Abstract
Aims
Basal insulin (BI) treatment initiation and dose titration in type 2 diabetes (T2DM) are often delayed. Such “clinical inertia” results in poor glycaemic control and high risk of long‐term complications. This survey aimed to determine healthcare professional (HCP) and patient attitudes to BI initiation and titration.
Methods
An online survey (July–August 2015) including HCPs and patients with T2DM in the USA, France and Germany. Patients were ≥18 years old and had been on BI for 6 to 36 months, or discontinued BI within the previous 12 months.
Results
Participants comprised 386 HCPs and 318 people with T2DM. While >75% of HCPs reported discussing titration at the initiation visit, only 16% to 28% of patients remembered such discussions, many (32%–42%) were unaware of the need to titrate BI, and only 28% to 39% recalled mention of the time needed to reach glycaemic goals. Most HCPs and patients agreed that more effective support tools to assist BI initiation/titration are needed; patients indicated that provision of such tools would increase confidence in self‐titration. HCPs identified fear of hypoglycaemia, failure to titrate in the absence of symptoms, and low patient motivation as important titration barriers. In contrast, patients identified weight gain, the perception that titration meant worsening disease, frustration over the time to reach HbA1c goals and fear of hypoglycaemia as major factors.
Conclusion
A disconnect exists between HCP‐ and patient‐perceived barriers to effective BI titration. To optimize titration, strategies should be targeted to improve HCP–patient communication, and provide support and educational tools.
Keywords: basal insulin, insulin analogues, insulin therapy, type 2 diabetes
1. INTRODUCTION
Basal insulin (BI) therapy is integral to the management of people with type 2 diabetes (T2DM) uncontrolled on oral therapies.1 BI dose titration is required to optimize treatment.2 Although insulin titration algorithms have been published,3, 4 the literature continues to report a significant delay in treatment initiation and intensification in people with T2DM with suboptimal glycaemic control.5, 6, 7 More than 50% of people with T2DM initiated on insulin therapy do not achieve the recommended HbA1c target (<7.0 %).8 Failure to achieve glycaemic targets has been shown in several studies,9, 10, 11, 12 with many patients also being unable to maintain long‐term glycaemic control. For example, in a study in the USA, 57% of those who initially achieved glycaemic goals were unable to sustain control over 2.5 years of follow‐up.12 Together these findings indicate that there is a clear unmet need to optimize BI titration in clinical practice.
The delay in BI treatment initiation or dose optimization in individuals not achieving glycaemic targets with their current treatment is often termed clinical inertia and can arise for several reasons. Both patients and healthcare professionals (HCPs) may focus on more immediate issues, such as fear of hypoglycaemia and/or weight gain, which may distract from the need to achieve glycaemic target.13 HCPs also often have limited time with each patient, and clinical inertia is more frequent when medical appointments are short.14 Managing the complex care needs of individuals with T2DM may also contribute to clinical inertia; for each additional clinical concern mentioned by a patient with HbA1c >7.0 % during a consultation, it has been reported that the likelihood of their diabetes treatment being intensified at that visit was reduced by 49%.14
Poor glycaemic control is associated with long‐term diabetes‐related macrovascular and microvascular complications, including cardiovascular disease, retinopathy, neuropathy, renal failure, and peripheral vascular disease.15, 16 The need to reduce delays in BI initiation and improve titration is relevant for people with T2DM newly initiated on BI therapy, as well as people currently on insulin therapy who are not achieving their targets. For patients who may need to intensify their diabetes treatment, insulin titration optimization could delay the need for additional antihyperglycaemic medication, thereby decreasing the burden of treatment. This market research survey was conducted to help understand HCP and patient attitudes to BI therapy titration, in order to identify how barriers to successful titration can be addressed.
2. METHODS
2.1. Survey design
An online market research survey of HCPs and patients with T2DM in the USA, France and Germany was conducted (July–August 2015). The survey evaluated the current attitudinal and behavioral variables of respondents and took approximately 45 minutes to complete. The survey questions (Tables S1 and S2) were developed by Sanofi with medical expert input, tested online before launch, and validated in English, French, and German. The survey was developed and conducted in line with European Society for Opinion and Marketing Research (ESOMAR) and European Pharmaceutical Market Research Association (EphMRA) guidelines.17, 18 Online informed consent was obtained from each participant before survey completion.
2.2. Survey participants
Participants were recruited by email from existing worldwide panels, and the survey managed by an independent supplier (Halls & Partners LLC, New York, New York). Patients and HCPs received remuneration for their involvement in the survey in consideration of their time and expertise (depending on the country and recruiter). As the HCPs and people with T2DM who participated were independent of each other, the HCPs did not necessarily provide health care for the participants with T2DM.
2.3. Inclusion criteria
2.3.1. HCPs
The HCPs surveyed were primary care practitioners (PCPs; USA and Germany), nurses (France), nurse practitioners (NPs; USA), certified diabetes educators (CDEs; USA), and endocrinologists/diabetologists (France and Germany). All HCPs were responsible for BI initiation and titration recommendations (PCPs, endocrinologists/diabetologists, NPs) or education on BI titration (nurses and CDEs). In the EU, HCPs had to treat ≥20 (PCPs) or ≥40 (endocrinologists/diabetologists) patients with T2DM per month. In the USA, PCPs and NPs had to treat ≥50 patients with T2DM per month. Nurses and CDEs had to manage ≥20 (EU) or ≥50 (USA) patients with T2DM per month.
2.3.2. Patients
Patients surveyed were to be ≥18 years old with T2DM and on any BI (including BI analogs and NPH insulin) for 6 to 36 months. Patients who had discontinued BI within the past 12 months were also eligible. While reports on the percentages of patients who discontinue BI vary,19, 20 based on an estimated total sample size of 120 patients per country and results of a French study indicating that approximately 25% of patients discontinued BI within 1 year of treatment initiation,21 it was estimated that ~30 patients per country who had discontinued BI would be included in the patient sample.
2.4. Data analysis and statistics
Quality control checks were performed during the data analysis. Descriptive statistics were used to assess survey responses, with percentages calculated based on the number of responders to the respective questionnaire item. The margin of error was ±5% at the 95% confidence interval, based on the number of HCPs and patients recruited.
3. RESULTS
3.1. Survey population
Overall, 1529 HCPs and 11 588 patients with T2DM were screened. Large numbers of people were ineligible to participate because of the specific eligibility criteria (patients with T2DM on BI, HCP initiating basal insulin and/or in charge of titration education and recommendation). The final survey was undertaken by 386 HCPs and 318 patients (Figure S1).
Approximately half of the total number of HCPs were PCPs (Table 1). A large proportion of HCPs in the USA (PCPs, NPs, CDEs) spent most of their professional time in an office‐based practice or clinic (Table 1). Similarly, respondents from Germany (PCPs and endocrinologists/diabetologists) spent most of their time in an office‐based practice, whereas those from France (nurses/CDEs, endocrinologists/diabetologists) spent most of their time in a hospital setting. There were differences in the level of support available to HCPs in Germany, France and the USA, in which 13%, 30% and 34%, respectively, were able to refer patients to another HCP (eg, general practitioner, nurse or pharmacist) for ongoing support.
Table 1.
HCP and patient characteristics
| USA | France | Germany | Total | |
|---|---|---|---|---|
| HCP characteristics | N = 175 | N = 105 | N = 106 | N = 386 |
| HCP specialties, n (%) | ||||
| Primary care physician | 115 (66) | – | 75 (71) | 190 (49) |
| Endocrinologist/diabetologist | – | 75 (71) | 31 (29) | 106 (27) |
| Nurse practitioner | 30 (17) | – | – | 30 (8) |
| Nurse/certified diabetes educator | – | 30 (29) | – | 30 (8) |
| Certified diabetes educator | 30 (17) | – | – | 30 (8) |
| Primary practice setting, n (%) | ||||
| Office‐based practice setting | 87 (50) | – | – | – |
| Private group practice | 66 (38) | – | – | – |
| Private solo practice | 21 (12) | – | – | – |
| Other | 1 (1) | – | – | – |
| Percentage of time spent in hospital setting, mean (SD) | – | 67 (37) | 30 (43) | – |
| Patient characteristics | N = 152 | N = 76 | N = 90 | N = 318 |
|---|---|---|---|---|
| Current BI user, n (%)a | 106 (70)b | 66 (87)b | 71 (79) | 243 (76) |
| Self‐titrating, n (%)c | 43 (41) | 30 (45) | 22 (31) | 95 (39) |
| HCP‐managed titration, n (%)c | 63 (59) | 36 (55) | 49 (69) | 148 (61) |
| Patient has reached pre‐breakfast SMPG target, n (%)c | 74 (70) | 43 (65) | 42 (59) | 159 (65) |
| Patient has reached HbA1c target, n (%)c | 47 (44) | 36 (55) | 42 (59) | 125 (51) |
| Discontinued BI user, n (%) | 46 (30)b | 10 (13)b | 19 (21) | 75 (24) |
| Age, years, mean (SD) | 55.3 (14.2) | 46.4 (13.9) | 53.1 (13.2) | 52.5 (14.2) |
| Male, n (%) | 102 (67) | 40 (53)d | 67 (74)d | 209 (66) |
| Employment status, n (%) | ||||
| Employed | 76 (50) | 54 (71) | 54 (60) | 184 (58) |
| Retired | 59 (39) | 15 (20) | 30 (33) | 104 (33) |
| Homemaker | 11 (7) | 4 (5) | 4 (4) | 19 (6) |
| Unemployed | 6 (4) | 3 (4) | 2 (2) | 11 (3) |
| Highest level of education completed, n (%) | ||||
| High school or less | 7 (5) | 12 (16) | 18 (20) | 37 (12) |
| Graduated from high school or equivalent | 23 (15) | 21 (28) | 38 (42) | 82 (26) |
| College or associate degree | 64 (42) | 22 (29) | 13 (14) | 99 (31) |
| University degree | 34 (22) | 18 (24) | 5 (6) | 57 (18) |
| Postgraduate degree | 24 (16) | 3 (4) | 16 (18) | 43 (14) |
| Duration of T2DM, years, mean (SD) | 11.4 (10.4)e | 7.0 (6.2) | 8.4 (5.8)e | 9.5 (8.6) |
| Current diabetes medications, n (%) | ||||
| Biguanides | 60 (39) | 11 (14) | 9 (10) | 80 (25) |
| Sulfonylureas | 11 (7) | 9 (12) | 1 (1) | 21 (7) |
| Thiazolidinediones | 6 (4) | 0 (0) | 2 (2) | 8 (3) |
| DPPIV inhibitors | 23 (15) | 4 (5) | 6 (7) | 33 (10) |
| GLP‐1 receptor agonists | 13 (9) | 7 (9) | 3 (3) | 23 (7) |
| BI | 106 (70) | 60 (79) | 67 (74) | 233 (73) |
| Rapid‐acting insulin | 9 (6) | 5 (7) | 12 (13) | 26 (8) |
| Regular human insulin | 12 (8) | 0 (0) | 8 (9) | 20 (6) |
| NPH insulin | 0 (0) | 7 (9) | 4 (4) | 11 (3) |
| Premix insulin | 22 (14) | 9 (12) | 4 (4) | 35 (11) |
Abbreviations: BI, basal insulin; DPPIV, dipeptidyl peptidase IV; GLP‐1, glucagon‐like peptide 1; HCP, healthcare professional; NPH, neutral protamine Hagedorn; SD, standard deviation; T2DM, type 2 diabetes.
BI user includes both BI analogs and NPH insulin.
France vs USA, P ≤ .01.
Percentage expressed as percent of current BI users.
France vs Germany, P ≤ .01.
USA vs Germany, P < .05.
Overall, nearly half of the total number of patients had not reached their HbA1c target (48.6%) and approximately one‐third (34.6%) had not reached their pre‐breakfast self‐monitored plasma glucose (SMPG) target (based on patient recall). Approximately three‐quarters of the surveyed patients were current BI users, and 75 were discontinued users (Table 1). Patients who discontinued BI were younger, had lower mean bodyweight, and were more likely to be administering twice‐daily insulin injections (Table S3). Discontinued BI users felt more restricted by having to manage their diabetes, were more concerned about hypoglycaemia, and found it more difficult to integrate insulin into their daily routine (Table S3). Given the small sample size (n = 75), and that the results for current and discontinued BI users did not generally differ, separate results for discontinued BI users have not been reported.
3.2. Physician perspectives
3.2.1. Key communication factors
Overall, the majority of HCPs (77%) agreed that communicating the need to increase BI dose over time was extremely/very important (75%–79%, per country). However, 45% of HCPs (USA: 53%; France: 22%; Germany: 54%) indicated that training and educating patients on titration was extremely/very challenging, given the limited time available to spend with patients. Regardless, 80% of HCPs (76%–84%) reported discussing titration at the BI initiation visit, and most HCPs (90%; 88%–92%) also felt that they could clearly explain the steps to be taken during the titration process. One‐third of HCPs (33%; 30%–36%) reported discussing the anticipated time to reach glycaemic goal with patients at the initiation visit. Once the decision had been taken to initiate BI, overall one‐third (33%) of HCPs reported discussing the fasting SMPG target as the goal to achieve during titration with all patients (Figure 1), although the main glycaemic target discussed by HCPs varied by country (Figure S2). Generally, relatively few HCPs (13%) reported discussing the anticipated final insulin dose required with all patients (Figure 1), but this was discussed by more HCPs in Germany (Figure S2C).
Figure 1.
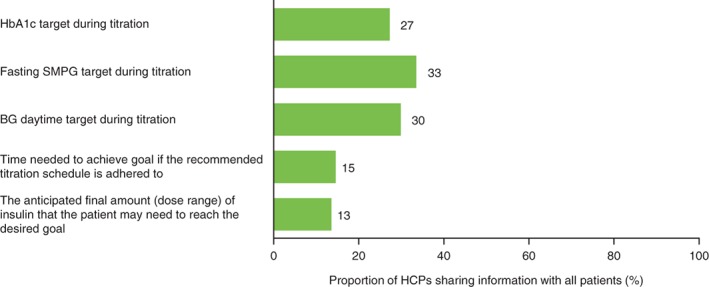
Information on basal insulin titration shared by HCPs with all patients. Abbreviations: BG, blood glucose; HCP, healthcare professional; SMPG, self‐monitored plasma glucose
3.2.2. Self‐titration and potential barriers to attainment of HbA1c targets
HCPs indicated that on average, 44% of their patients (Germany: 36%; USA: 42%; France: 55%) managed their own BI titration, and 38% of HCPs (USA: 33%; France: 57%; Germany: 28%) expressed a preference for patients to self‐titrate. Overall, HCPs perceived the main barriers to target attainment in self‐titrating patients to be fear of hypoglycaemia (74%), patient's hesitancy to increase the BI dose in the absence of symptoms (66%), and low patient involvement/motivation (63%; Figure 2); the same 3 factors were perceived as being the main barriers to target attainment in Germany and the USA, while in France, concern over weight gain was also thought to be a main concern of patients (Figure S3).
Figure 2.
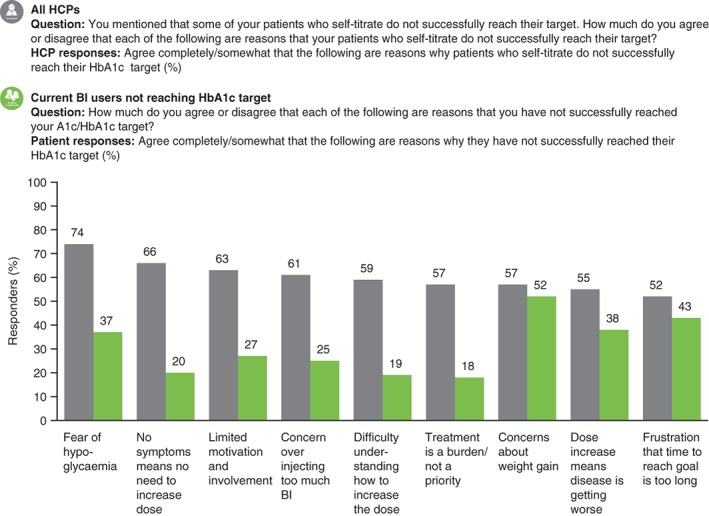
Barriers to self‐titration identified by HCPs and patients. The top 9 of 14 potential response options are shown for HCPs, with the corresponding response options shown for patients. BI, basal insulin; HCP, healthcare professional
3.2.3. Support tools
HCPs used or recommended several educational and support tools to help patients with BI initiation and titration, including support from medical staff (telephone or office visit) (66%; 64%–66%, per country), educational pamphlets (64% overall; USA: 54%; France: 69%; Germany: 75%) and paper diaries (for SMPG results and BI dose) (61% overall; USA: 59%; France: 51%; Germany: 75%). In the USA, France and Germany, 85%, 69% and 77% of HCPs, respectively, agreed completely or somewhat that there was a need for more effective support tools/materials to assist with BI initiation and dose titration.
3.3. Patient perspectives
3.3.1. Key communication factors
Overall, 76% of patients (USA: 83%; France: 63%; Germany: 74%) expressed some degree of confidence in being able to dose BI correctly, although many reported being unaware of the need to titrate BI dose (37% overall; USA: 42%; France: 33%; Germany: 32%). Patient‐identified factors that would increase confidence when self‐titrating included further information about the HbA1c target during the titration period, the amount of time needed to achieve their goal, and the anticipated final BI dosage (Figures 3 and S4).
Figure 3.
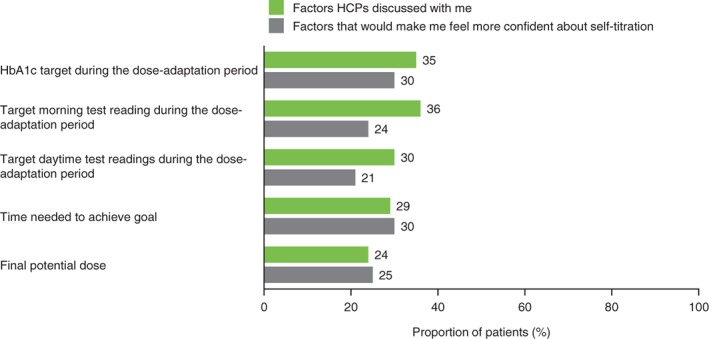
Provision of information on titration factors: factors recalled by patients as being discussed with HCPs, and those factors patients consider would increase confidence in self‐titration. HCP, healthcare professional
3.3.2. Self‐titration and potential barriers to attainment of HbA1c targets
Just over half of the total number (58% overall; USA: 53%; France: 60%; Germany: 64%) of self‐titrating current BI users expressed a preference towards self‐titration, while a minority (6% overall; USA: 11%; France: 3%; Germany: 2%) of current BI users with HCP‐managed titration expressed a preference towards self‐titration. In contrast, only 38% of HCPs overall indicated that they would prefer patients to self‐titrate, although this percentage was higher in France (USA: 33%; France: 57%; Germany: 28%). Reasons why HCPs preferred to manage titration themselves included that it avoided errors, provided effective control and ensured patient compliance.
Current BI users who had not reached their HbA1c target highlighted several reasons that, in their opinion, would/did contribute to not being able to increase their dose (Figures 2 and S3), including concerns over weight gain, perception that BI dose increase meant worsening of disease, fear of hypoglycaemia and frustration that the time to reach their HbA1c goal was too long.
3.3.3. Support tools
Patients indicated that they had used, or received, a recommendation to use a number of support tools including support from their physician (35% overall; USA: 33%; France: 33%; Germany: 40%), educational pamphlets (31% overall; USA: 36%; France: 22%; Germany: 31%) and a paper diary (for SMPG results and BI dose) (31% overall; USA: 37%; France: 20%; Germany: 31%).
3.4. HCP and patient perspectives: comparing and contrasting viewpoints
3.4.1. Communication
Although HCPs recognized the importance of discussing titration and 80% overall (76%–84%) reported doing so at the initiation visit, only 22% of patients overall (16%–28%) recalled this discussion taking place. Patients identified several factors that would make them feel more confident about self‐titration, including receiving further details on the target morning test reading, having the HbA1c target as the goal to achieve during the period of dose adaptation, and knowing the amount of time needed to reach glycaemic targets. However, many patients did not recall HCPs discussing these factors with them (Figures 3 and S4).
3.4.2. Potential barriers to attainment of HbA1c targets
Differences were observed between the perceived barriers to optimal titration by patients and those perceived to be patient barriers by HCPs (Figures 2 and S3). Frustration over time to reach goal was a factor identified by patients contributing to not reaching HbA1c target (43% overall; USA: 37%; France: 57%; Germany: 41%). However, the majority of HCPs (88%–89%) preferred that patients reached their goal safely, even if it may take longer. SMPG targets for patients who were not elderly or frail were 135 and 124 mg/dL (7.5 and 6.9 mmol/L), respectively, for PCPs and NPs in the USA, 111 and 125 mg/dL (6.2 and 6.9 mmol/L), respectively, for endocrinologists/diabetologists and nurses/CDEs in France, and 145 and 142 mg/dL (8.0 and 7.9 mmol/L), respectively, for PCPs and endocrinologists/diabetologists in Germany. Patients were most commonly concerned about weight gain, whereas physicians identified patient fear of hypoglycaemia as the main barrier to HbA1c target achievement (Figures 2 and S3). In addition, lower proportions of patients than HCPs reported concerns about barriers to titration, particularly relating to fear of hypoglycaemia and low motivation and involvement. Therefore, many HCPs may overestimate patient concerns about insulin titration.
3.4.3. Support tools to assist with BI initiation and titration
Although some support tools were recommended by HCPs and used by patients, the majority of HCPs (78%; USA: 85%; France: 69%; Germany: 77%) and patients (57%; USA: 49%; France: 66%; Germany: 62%) agreed that a need remains for more effective tools to assist with BI initiation and titration. HCPs and patients identified several solutions with potential to positively impact upon the titration process, including educational tools, peer support programmes and mobile applications. Patients reported that willingness to self‐titrate and confidence in self‐management success would be increased by the availability and utilization of a number of these tools, including simple titration algorithms and patient support programmes (Table 2).
Table 2.
Support tools to assist with BI initiation and titration
| Patient responses: potential support tools that may increase | ||
|---|---|---|
| Willingness to self‐titrate (net difference in responsesa [%]) | Confidence in self‐management success (net difference in responsesa [%]) | |
| HCP support + educational tools | +10 | +20 |
| Simple titration algorithm | +29 | +20 |
| Patient support programme | +19 | +20 |
| App/meter to recommend dose | +16 | +7 |
Abbreviation: HCP, healthcare professional.
Net difference: the number of patients reporting an increase minus number of patients reporting a decrease.
4. DISCUSSION
This survey was aimed at achieving a better understanding of the barriers to optimal BI titration, in order to aid the discovery of ways to overcome these barriers in the future. Although HCPs recognized the importance of communicating the need to increase BI dose to patients, and the majority reported doing so, many patients did not recall this. The survey results are consistent with reports that patients forget a significant amount of newly learned diabetes‐related information within 2 weeks of receiving it, irrespective of literacy levels,22 and suggest that key information regarding BI titration should be reinforced at regular intervals, and by different means, to maintain patient confidence in managing their diabetes. Overall, the results of this market research survey highlight the importance of supportive tools, not only to educate and inform patients at home, but also for use during visits, to allow HCPs to have more quality time to listen to patients’ questions, address any anxieties, provide reassurance, and to repeat titration instructions, if needed.
Although most HCPs recognized the importance of communicating the need to increase BI dose, 1 in 5 HCPs did not discuss this need at the initiation visit, suggesting that more effective communication methods and additional support tools/materials may be needed by HCPs to assist patients with BI initiation and titration. Time constraints during the BI initiation visit appear to be a particular problem in the USA and France, in which 53% and 32% of HCPs, respectively, agreed completely/somewhat that they had limited time to provide all relevant information to the patient, versus 20% of HCPs in Germany. Reach13 recently highlighted that the patient–doctor relationship during a consultation should be considered as a conversation between 2 people. Such a conversation can be considered as the essence of patient education, and by raising sometimes unspoken attitudes regarding insulin initiation or titration, can help to address the issue of clinical inertia.13 The need for an open clinical conversation regarding BI initiation and dose titration is highlighted by the results of the current survey, which indicate that HCPs are more likely to overestimate barriers to reaching target HbA1c levels than patients. Therefore, if these perceived barriers are not discussed and addressed, HCPs may delay treatment initiation or titration.
The present survey identified a disconnect between HCP‐perceived and patient‐perceived barriers to optimal titration. HCPs generally preferred a slow and safe approach to titration, even if it takes longer for patients to achieve their glycaemic target. Mean SMPG targets recommended by HCPs for patients who were not elderly or frail tended to be either above, or at the higher end of, targets recommended by the American Diabetes Association (80–130 mg/dL [4.4–7.2 mmol/L]), the American Association of Clinical Endocrinologists (<110 mg/dL [<6.1 mmol/L]) and the European Society of Cardiology and the European Association for the Study of Diabetes (<120 mg/dL [<6.7 mmol/L]), indicating the conservative approach taken by most HCPs.23, 24, 25 However, this approach may be overcautious, as patients who were not at target were frustrated about the length of time taken to reach the target and were less concerned about hypoglycaemia than HCPs perceived them to be. Again, this finding suggests the need for open communication regarding the likely length of BI titration, with HCPs balancing the need for safety, while considering and discussing the wishes of their patients to see timely results.
A disconnect between HCP‐perceived and patient‐perceived barriers to titration was also reported in a systematic meta‐analysis performed by Polinski et al.;26 while injection‐related aversions (not assessed in the present survey) and the perceived burden of diseases were identified as barriers to insulin progression (defined by the authors as switching from basal to a premixed insulin regimen, adding bolus doses and/or increasing dosing frequency) for patients, HCPs were concerned about the patients’ ability to handle more complex treatment regimens. Polinski et al.26 also suggested that barriers to insulin titration may be reduced by providing educational interventions to both physicians and patients. Likewise, in the present survey, both HCPs and patients reported that more effective support tools, as well as better HCP understanding of patient needs, were required to assist with BI initiation and titration.
The results presented here further suggest that different types of support tools may be useful, when adapted to each patient's choice and needs. Several mobile applications, internet portals, and websites are currently available to help patients improve their diabetes care including patient support programmes that allow individualized support at home using integrated supportive tools. However, there are currently limited data available to show the effectiveness and cost‐benefits of these tools in diabetes self‐management, and large studies may be needed to support their use.27
The use of more effective communication techniques and support tools may improve patient understanding and ensure that the key information required is received, at the right time and in the right place, to optimize BI titration, improve glycaemic control, and reduce the risk of long‐term diabetes‐related complications. For example, in the Microalbuminuria Education and Medication Optimization (MEMO) study, patients who received intensive intervention with structured patient education achieved greater reductions in HbA1c and improvements in cardiovascular risk factors than those receiving usual care from their HCP.28 Intensive intervention versus standard care resulted in significant improvements in HbA1c (7.1 % vs 7.8 %, P < .0001), systolic BP (129 vs 139 mm Hg, P < .0001), diastolic BP (70 vs 76 mm Hg, P < .001), total cholesterol (3.7 vs 4.1 mmol/L, P = .001), moderate hypoglycaemia (11.2% vs 29.0%; P = .001) and severe hypoglycemia (0% vs 6.3%, P = .07), respectively.28
The limitations of this survey include its geographic profile (only 3 countries), and the limited sample size of the HCP and patient populations (owing to the specific inclusion criteria). The patients and HCPs were not matched (ie, patients were not necessarily treated by the HCPs), which may limit the interpretation of the differences between patient and HCP preferences. Participants who completed the survey may not be representative of the general patient population, as the survey was conducted online and patients participated on a voluntary basis. This approach may have introduced a selection bias, such that only the most motivated or educated patients were included. The educational needs of a representative patient population may have therefore been underestimated. The large number of questions included may have limited the ability of respondents to accurately answer all of the questions, particularly those towards the end of the survey. The survey was also limited by the use of patient recall of HbA1c levels and BI doses, as opposed to utilizing actual measurements, which should be taken into consideration when drawing conclusions based on these data. However, a strength of this survey is that it reflected the real‐life experiences of both patients with T2DM and the wide range of multidisciplinary HCPs who provide diabetes care in different clinical and geographic settings.
In conclusion, this survey, conducted in the USA, France and Germany, provides important insights into differences between HCP and patient understanding of the need to titrate BI over time to achieve optimum glycaemic control. Improving HCP–patient communication, and providing additional educational tools and support on the titration process to increase patient confidence, both at the initiation visit and at home, may help to optimize dose titration. This in turn could reduce healthcare costs and improve treatment adherence. The results highlight the need for future research to identify appropriate support materials or tools to overcome barriers to effective titration, for both HCPs and patients, to improve glycaemic control and enhance patient outcomes.
Supporting information
Figure S1. HCP and patient flow by country.
Figure S2. Information on basal insulin titration shared by HCPs with all patients.
Figure S3. Barriers to self‐titration identified by HCPs and patients.
Figure S4. Provision of information on titration factors: factors recalled by patients as being discussed with HCPs, and those factors patients consider would increase confidence in self‐titration.
Table S1. Questions asked of patients.
Table S2. Questions asked of HCPs.
Table S3. Clinical and attitudinal differences between current versus discontinued BI users.
ACKNOWLEDGEMENTS
This online market research survey was sponsored by Sanofi and was performed by Halls & Partners LLC, New York, New York. The authors thank the survey participants for taking part in this survey. Editorial and writing assistance was provided by Sharon Eastwood, DPhil, of Fishawack Communications and was funded by Sanofi.
Conflicts of interest
L. B. has served on an advisory panel for Abbott, AstraZeneca, BD, Eli Lilly, Janssen, Lifescan, Novo Nordisk, Sanofi; has been a consultant to Abbott, AstraZeneca, Bayer, BD, Boehringer Ingelheim, Eli Lilly, Janssen, Lifescan, Merck, Novo Nordisk, Sanofi; and has served on a speakers bureau for Abbott, AstraZeneca, Bayer, BD, Boehringer Ingelheim, Eli Lilly, Janssen, Lifescan, Merck, Novo Nordisk, Sanofi. M. B. and M. M. are employees of Sanofi. S. E. has no conflicts of interest to declare.
Author contributions
L. B. was involved in data analysis and interpretation, writing and critical revision of the manuscript. M. B. was involved in the design of the survey, acquisition of data, data analysis and interpretation, writing and critical revision of the manuscript. M. M. was involved in the design of the survey, acquisition of data, data analysis and interpretation, writing and critical revision of the manuscript. S. E. was involved in data analysis and interpretation, writing and critical revision of the manuscript.
Berard L., Bonnemaire M., Mical M., Edelman S. Insights into optimal basal insulin titration in type 2 diabetes: Results of a quantitative survey. Diabetes Obes Metab. 2018;20:301–308. https://doi.org/10.1111/dom.13064
Funding information This online market research survey was sponsored by Sanofi and was performed by Halls & Partners LLC, New York, New York.
REFERENCES
- 1. American Diabetes Association . Standards of medical care in diabetes – 2017. Diabetes Care. 2017;40:S1–S135.27979885 [Google Scholar]
- 2. Ross SA, Tildesley HD, Ashkenas J. Barriers to effective insulin treatment: the persistence of poor glycemic control in type 2 diabetes. Curr Med Res Opin. 2011;27(suppl 3):13–20. [DOI] [PubMed] [Google Scholar]
- 3. Nathan DM, Buse JB, Davidson MB, et al. Medical management of hyperglycemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy: a consensus statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2009;32:193–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Strange P. Treat‐to‐target insulin titration algorithms when initiating long or intermediate acting insulin in type 2 diabetes. J Diabetes Sci Technol. 2007;1:540–548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Khunti K, Nikolajsen A, Thorsted BL, Andersen M, Davies MJ, Paul SK. Clinical inertia with regard to intensifying therapy in people with type 2 diabetes treated with basal insulin. Diabetes Obes Metab. 2016;18:401–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Calvert MJ, McManus RJ, Freemantle N. Management of type 2 diabetes with multiple oral hypoglycaemic agents or insulin in primary care: retrospective cohort study. Br J Gen Pract. 2007;57:455–460. [PMC free article] [PubMed] [Google Scholar]
- 7. Nichols GA, Koo YH, Shah SN. Delay of insulin addition to oral combination therapy despite inadequate glycemic control: delay of insulin therapy. J Gen Intern Med. 2007;22:453–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Stark Casagrande S, Fradkin JE, Saydah SH, Rust KF, Cowie CC. The prevalence of meeting A1C, blood pressure, and LDL goals among people with diabetes, 1988–2010. Diabetes Care. 2013;36:2271–2279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bennett H, McEwan P, Bergenheim K, Gordon J. Assessment of unmet clinical need in type 2 diabetic patients on conventional therapy in the UK. Diabetes Ther. 2014;5:567–578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Khunti K, Caputo S, Damci T, et al. The safety and efficacy of adding once‐daily insulin detemir to oral hypoglycaemic agents in patients with type 2 diabetes in a clinical practice setting in 10 countries. Diabetes Obes Metab. 2012;14:1129–1136. [DOI] [PubMed] [Google Scholar]
- 11. Kostev K, Dippel FW, Rathmann W. Glycemic control after initiating basal insulin therapy in patients with type 2 diabetes: a primary care database analysis. Diabetes Metab Syndr Obes. 2015;8:45–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wu N, Aagren M, Boulanger L, Friedman M, Wilkey K. Assessing achievement and maintenance of glycemic control by patients initiating basal insulin. Curr Med Res Opin. 2012;28:1647–1656. [DOI] [PubMed] [Google Scholar]
- 13. Reach G. Patients' nonadherence and doctors' clinical inertia: two faces of medical irrationality. Diabetes Manage. 2015;5:167–181. [Google Scholar]
- 14. Parchman ML, Pugh JA, Romero RL, Bowers KW. Competing demands or clinical inertia: the case of elevated glycosylated hemoglobin. Ann Fam Med. 2007;5:196–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Stratton IM, Adler AI, Neil HA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321:405–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Adler AI, Stratton IM, Neil HA, et al. Association of systolic blood pressure with macrovascular and microvascular complications of type 2 diabetes (UKPDS 36): prospective observational study. BMJ. 2000;321:412–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. European Pharmaceutical Market Research Association . Code of conduct. http://www.ephmra.org/code-of-conduct. 2016. Accessed July 2016.
- 18. European Society for Opinion and Marketing Research . Global guideline: online research. https://www.esomar.org/uploads/public/knowledge‐and‐standards/codes‐and‐guidelines/ESOMAR‐GRBN‐Online‐Research‐Guideline‐October‐2015.pdf. 2015. Accessed July 2016.
- 19. Ascher‐Svanum H, Lage MJ, Perez‐Nieves M, et al. Early discontinuation and restart of insulin in the treatment of type 2 diabetes mellitus. Diabetes Ther. 2014;5:225–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Wei W, Pan C, Xie L, Baser O. Real‐world insulin treatment persistence among patients with type 2 diabetes: measures, predictors and outcomes. Endocr Pract. 2014;20:52–61. [DOI] [PubMed] [Google Scholar]
- 21. Roussel R, Charbonnel B, Behar M, Gourmelen J, Emery C, Detournay B. Persistence with insulin therapy in patients with type 2 diabetes in France: an insurance claims study. Diabetes Ther. 2016;7:537–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kandula NR, Malli T, Zei CP, Larsen E, Baker DW. Literacy and retention of information after a multimedia diabetes education program and teach‐back. J Health Commun. 2011;16(suppl 3):89–102. [DOI] [PubMed] [Google Scholar]
- 23. American Diabetes Association . 5. glycemic targets. Diabetes Care. 2016;39(suppl 1):S39–S46. [DOI] [PubMed] [Google Scholar]
- 24. Garber AJ, Abrahamson MJ, Barzilay JI, et al. Consensus statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the comprehensive type 2 diabetes management algorithm—2016 executive summary. Endocr Pract. 2016;22:84–113. [DOI] [PubMed] [Google Scholar]
- 25. Montalescot G, Sechtem U, Achenbach S, et al. 2013 ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J. 2013;34:2949–3003. [DOI] [PubMed] [Google Scholar]
- 26. Polinski JM, Smith BF, Curtis BH, et al. Barriers to insulin progression among patients with type 2 diabetes: a systematic review. Diabetes Educ. 2013;39:53–65. [DOI] [PubMed] [Google Scholar]
- 27. Shah VN, Garg SK. Managing diabetes in the digital age. Clin Diabetes Endocrinol. 2015;1:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Crasto W, Jarvis J, Khunti K, et al. Multifactorial intervention in individuals with type 2 diabetes and microalbuminuria: the Microalbuminuria Education and Medication Optimization (MEMO) study. Diabetes Res Clin Pract. 2011;93:328–336. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. HCP and patient flow by country.
Figure S2. Information on basal insulin titration shared by HCPs with all patients.
Figure S3. Barriers to self‐titration identified by HCPs and patients.
Figure S4. Provision of information on titration factors: factors recalled by patients as being discussed with HCPs, and those factors patients consider would increase confidence in self‐titration.
Table S1. Questions asked of patients.
Table S2. Questions asked of HCPs.
Table S3. Clinical and attitudinal differences between current versus discontinued BI users.


