Abstract
Background
Early detection followed by prompt intervention is essential for the treatment of periprosthetic joint infection (PJI). D-dimer, a fibrin degradation product, characteristically changes rapidly during early postoperative period and has a short half-life. The aim of this prospective study was to measure postoperative change of D-dimer level after joint arthroplasty in conjunction with ESR and CRP.
Methods
ESR, CRP, and D-dimer levels were measured on the day before surgery, postoperative days 1, 2, 3, and 5 and weeks 2 and 6 in 65 patients who underwent elective primary total hip arthroplasty (38 hips in 38 patients) or total knee arthroplasty (27 knees in 27 patients). We compared perioperative changes of the three biomarkers.
Results
ESR level was elevated from postoperative day 1 and reached a peak level of 45 mm/h at postoperative day 5. The elevation persisted until postoperative week 6. CRP level was elevated from postoperative day 1 and reached a peak level of 10 mg/dl between postoperative day 2 and day 3. The CRP level was decreased to the normal level around postoperative week 2. D-dimer level was sharply elevated and peaked to 4.5 μg/dl at postoperative day 1. At postoperative day 2, it decreased to baseline level. After then, it slowly elevated again and reached a second peak at postoperative week 2.
Conclusion
D-dimer showed a more rapid rise and fall than ESR and CRP in very early postoperative period. The D-dimer test might be effective in early detection of PJI, if combined with levels of ESR and CRP. The postoperative change of D-dimer in our study can serve as a baseline for early diagnosis of PJI.
Keywords: D-Dimer, Periprosthetic joint infection, Total hip arthroplasty, Total knee arthroplasty
Background
Periprosthetic joint infection (PJI) after total hip arthroplasty (THA) or total knee arthroplasty (TKA) is one of the most dreadful complications and it has extremely negative effects on the physical, emotional, social, and economic aspects of a patient’s life [1–4]. To eradicate the infection, a diagnosis of PJI in its early stage is very important [4–7]. Serum erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) have been generally used as a screening test for infection because of their simplicity and cost-effectiveness [8]. However, they have low sensitivity and specificity and these may increase under several conditions in addition to infection [8–11]. Therefore, there have been some trials to establish a new single reference standard [6, 9].
D-dimers are fibrin degradation products formed as a result of fibrin clot dissolution by plasmin. This test is typically done in patients with suspected venous thromboembolism (VTE), manifested as deep vein thrombosis (DVT) or pulmonary embolism (PE). However, the increased fibrin production, which is manifested by the elevated D-dimer concentration, can also be observed in other clinical conditions, such as cancer, infection, inflammation, surgery, injuries, hemorrhages, and many others [12]. It could imply that elevated D-dimer level does not have a confirmatory value due to low specificity of the assay. However, it characteristically shows sharp increase up to double levels and decrease to the baseline level within a short time during early postoperative period. After then, it also shows second peak after maintaining at the steady level for a while [12]. With these characteristics, D-dimer was tried for the diagnosis of PJI. Serum D-dimer outperformed both ESR and serum CRP, with a sensitivity of 89% and a specificity of 93%. ESR and CRP had a sensitivity of 73 and 79% and a specificity of 78 and 80%, respectively [13].
Some patients could be suspected to have an infection at the immediate postoperative period. In this situation, rapid decision whether irrigation and debridement should be done to preserve the implanted prosthesis is an important issue because it is a time-honored procedure and it should be performed before the establishment of drug-resistant biofilm on the implant or before osteomyelitis becoming entrenched in periprosthetic bone [14]. However, CRP hits a peak on day 2 or 3 after surgery and diminishes to a normal value by postoperative week 2 and ESR shows slower natural progress than CRP. Therefore, we can miss the chance to save the implant using an early intervention if we only rely on these tests.
Thus, we were interested in whether D-dimer level shows a sharp change at an early postoperative period and it can be used as a promising biomarker for an early diagnosis of the infection by combining the natural progress with commonly used tests such as ESR and CRP. We hypothesized that the D-dimer will show a rapid change of the natural progress at a very early postoperative period. The aim of this study was to measure postoperative change of D-dimer level after joint arthroplasty in conjunction with ESR and CRP.
Methods
Ethical approval for this prospective study was obtained from IRB of our hospital. Sixty-five volunteers scheduled for either elective primary THR (38 hips in 38 patients) or TKR (27 knees in 27 patients) surgery were recruited with their informed consent. Inclusion criteria are as follows: patients scheduled for THA or TKA due to primary or secondary osteoarthritis, not having significant preoperative comorbidity with a Charlson comorbidity index (CCI) < 2, and no sign of inflammation and adverse event during test period. Exclusion criteria are as follows: (1) inflammatory arthritis such as rheumatoid arthritis, (2) patients who have taken preoperative pharmacologic DVT prophylaxis or suspicious DVT, (3) revision THA or TKA, and (4) patients who have missing data at all scheduled time points.
All TKAs were performed with an intraoperative tourniquet. The tourniquet was inflated just before the skin incision and deflated after the cementation was completed. After a midline skin incision, a medial parapatellar approach was performed. Intramedullary guide was used for the femur and extramedullary guide for the tibia. The posterior cruciate was sacrificed and fixed-bearing TKA were implanted in all patients. All prostheses were fixed with cement. An intra-articular closed-suction drainage after TKA was used for 24 h. All THAs were performed with the Kocher-Langenbeck approach. The short external rotators were detached with electrocautery as close as possible from their insertion, and posterior capsule was exposed. After posterior capsulotomy, the femoral head was dislocated posteriorly. The femoral neck was cut at the base and the femoral head was removed. The femoral stem and acetabular cup were inserted through the posterior approach without cement. After implantation of the prosthesis, we repaired the capsule and short external rotators. Closed-suction drainage after THA was also used for 24 h. We used tranexamic acid at subcutaneous tissue both THA and TKA.
ESR, CRP, and D-dimer values were collected on the day before surgery, postoperative days 1, 2, 3, and 5 and weeks 2 and 6. The D-dimer level in venous plasma was assessed by an immunoturbidimetric assay, STA Liatest D-Di (Diagnostica Stago, Asnieres sur Seine, France) on a STA-R analyzer (Diagnostica Stago). According to the data provided by the manufacturer (Diagnostica Stago), the measuring range of STA Liatest is from 0.27 μg/ml (fibrinogen equivalent unit, FEU) to 4.0 μg/ml without dilution and with dilution up to 20.0 μg/ml (FEU). The cutoff value of 0.50 μg/ml showed a negative predictive value of 95 to 100% from two studies that tested the use of STA Liatest D-Di as an aid in the diagnosis of DVT [15, 16].
For the evaluation, preoperative demographic data and values of each test at the scheduled time points were compared between THA and TKA. In addition, change of the percentage of each test value compared to the maximal level at the early postoperative period was also performed to verify the effectiveness of each test.
Statistical analysis
Statistical analysis was performed using R version 3.3.1 (The R Foundation for Statistical Computing). Comparison of ESR, CRP, and D-dimer between preoperative and postoperative values was performed using a paired t test because most of variables followed normal distribution. Comparison on the early postoperative value of the D-dimer was performed using Tukey HSD test.
Funding source
This study was supported by Corentec (Cheonan, South Korea).
Results
Detailed demographic data of patients were presented in Table 1. There was a male dominance in THA patients (M:F = 24:14) and female dominance in TKA patients (M:F = 3:24). Age was older in TKA group than in THA group. Values of each test at the scheduled time points were presented as a box plot in Fig. 1. Mean and standard deviation (SD) values were presented and these were compared between THA and TKA in Table 2. In ESR, values showed a statistically significant difference between groups at the postoperative day 2 and week 2 and they were not consistently high or low in each group. In CRP, postoperative 2-week value showed a statistically significant difference between groups and higher value was observed in the TKA group. In D-dimer, values showed a statistically significant difference between groups at the preoperative value and postoperative day 5 and they were consistently high in the THA group.
Table 1.
Demographic data
| THA | TKA | |||||
|---|---|---|---|---|---|---|
| Dx | AVN | OA | p | OA | AVN | p |
| (N = 19) | (N = 19) | (N = 25) | (N = 2) | |||
| Sex | ||||||
| F | 1 (5.3%) | 13 (68.4%) | 23 (92.0%) | 1 (50.0%) | ||
| M | 18 (94.7%) | 6 (31.6%) | 2 (8.0%) | 1 (50.0%) | ||
| Age | 54.6 ± 14.2 | 60.1 ± 10.9 | 0.192 | 69.9 ± 7.1 | 76.5 ± 0.7 | 0.207 |
| Weight | 65.6 ± 10.6 | 64.3 ± 7.1 | 0.654 | 61.2 ± 9.9 | 67.0 ± 8.5 | 0.431 |
| Height | 169.8 ± 6.7 | 158.7 ± 9.7 | 0 | 151.7 ± 7.7 | 157.5 ± 0.7 | 0.306 |
| BMI | 22.7 ± 3.4 | 25.7 ± 3.2 | 0.01 | 26.7 ± 4.8 | 27.0 ± 3.7 | 0.924 |
Fig. 1.
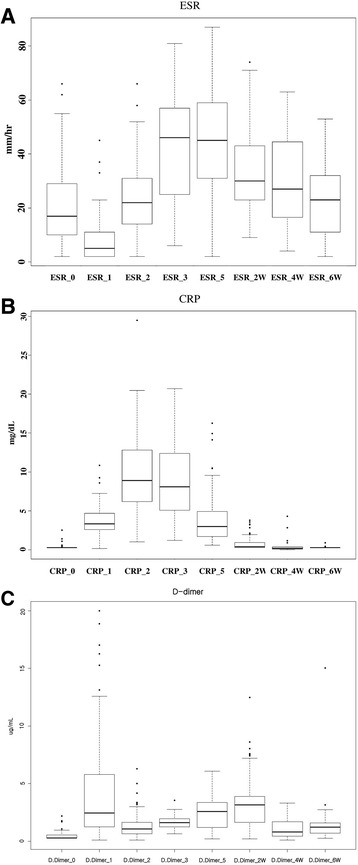
Values of each test (a ESR, b CRP, and c D-dimer) that are presented as a box plot at each time points; median line in box plot means median, and box means quartile range (QR)
Table 2.
Values of each test at the scheduled time points
| POD | THA | TKA | p value | POD | THA | TKA | p value | POD | THA | TKA | p value |
|---|---|---|---|---|---|---|---|---|---|---|---|
| (N = 38) | (N = 27) | (N = 38) | (N = 27) | (N = 38) | (N = 27) | ||||||
| ESR_0 | 21.4 ± 17.4 | 19.6 ± 12.0 | 0.636 | CRP_0 | 0.4 ± 0.4 | 0.3 ± 0.1 | 0.073 | D-dimer_0 | 0.6 ± 0.4 | 0.4 ± 0.3 | 0.019 |
| ESR_1 | 9.6 ± 10.3 | 7.3 ± 7.9 | 0.328 | CRP_1 | 4.0 ± 2.1 | 3.7 ± 1.8 | 0.558 | D-dimer_1 | 5.2 ± 4.9 | 3.9 ± 5.8 | 0.351 |
| ESR_2 | 27.9 ± 15.5 | 18.0 ± 12.8 | 0.008 | CRP_2 | 9.5 ± 4.4 | 10.2 ± 5.9 | 0.573 | D-dimer_2 | 1.5 ± 1.0 | 1.3 ± 1.4 | 0.607 |
| ESR_3 | 44.3 ± 18.9 | 35.1 ± 22.1 | 0.212 | CRP_3 | 8.6 ± 4.4 | 10.5 ± 6.0 | 0.306 | D-dimer_3 | 1.6 ± 0.5 | 1.9 ± 0.8 | 0.157 |
| ESR_5 | 45.8 ± 19.6 | 44.3 ± 18.5 | 0.749 | CRP_5 | 4.2 ± 3.0 | 4.2 ± 4.2 | 0.943 | D-dimer_5 | 3.1 ± 1.2 | 1.7 ± 1.4 | 0 |
| ESR_2W | 30.6 ± 13.8 | 40.0 ± 18.3 | 0.022 | CRP_2W | 0.5 ± 0.6 | 1.2 ± 1.1 | 0.005 | D-dimer_2W | 3.7 ± 1.7 | 2.7 ± 3.0 | 0.13 |
| ESR_6W | 22.0 ± 14.7 | 28.4 ± 12.1 | 0.228 | CRP_6W | 0.3 ± 0.1 | 0.3 ± 0.0 | 0.125 | D-dimer_6W | 1.5 ± 2.4 | 1.8 ± 0.5 | 0.502 |
Serial change of each test was diagramed in Fig. 2. In Fig. 2a, all tests were presented using a serial graph. Comparative graphs between D-dimer and ESR and between D-dimer and CRP were presented in Fig. 2b, c. ESR elevated from postoperative day 1, peaked at postoperative day 5 (peak level 45 mm/h), and was still high at the postoperative week 6. CRP elevated from postoperative day 1, peaked between postoperative days 2 and 3 (peak level 10 mg/dl), and decreased to the normal level at around postoperative week 2. D-dimer sharply elevated and peaked at postoperative day 1 (peak level 4.5 μg/dl). At postoperative day 2, it decreased to nearly baseline level. After then, it slowly elevated again and reached second peak at postoperative week 2.
Fig. 2.
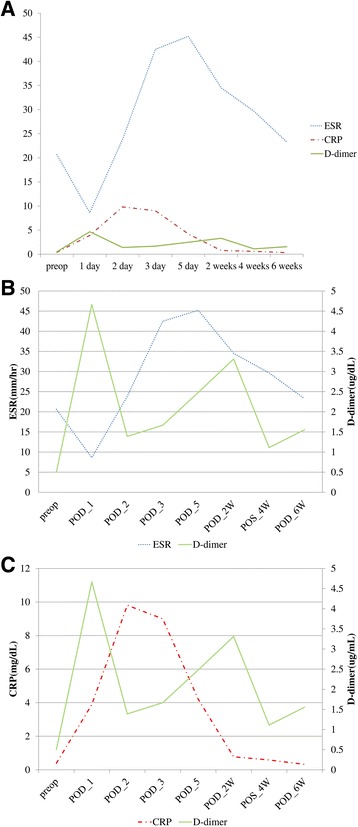
Serial change of each test that is presented as a graph (a); comparative graphs were also presented between ESR and D-dimer (b) and between CRP and D-dimer (c)
Change of the percentage of each value compared to the maximal level at the early postoperative period was presented in Table 3. Elevation of the D-dimer during postoperative day 1 showed a statistically significant difference (83.4% elevation compared to the maximal level, p = 0.000) and decrease during postoperative day 2 also showed a statistically significant difference (65.5% decrease compared to the maximal level, p < 0.001). However, the change between postoperative days 2 and 3 was not statistically significant (2.2% elevation compared to the maximal level, p = 0.303). ESR and CRP also showed statistically significant differences during postoperative days 1, 2, and 3, but changes were smaller compared to those of D-dimer. In the comparison of the D-dimer level, they showed statistically significant differences between baseline and postoperative day 1 and between postoperative days 1 and 2. However, there was no statistical difference between baseline and postoperative day 2 and the level of the D-dimer decreased to the baseline level at the postoperative day 2 (Fig. 3).
Table 3.
Change of the percentage of each test value compared to the maximal level at the early postoperative period
| PreOP vs POD_1 | POD_1 vs POD_2 | POD_2 vs POD_3 | |
|---|---|---|---|
| D-dimer | |||
| Mean difference (%) | 83.4 | − 65.5 | 2.2 |
| p value | 0.000 | 0.000 | 0.303 |
| CRP | |||
| Mean difference (%) | 34.9 | 59.2 | − 5.0 |
| p value | 0.000 | 0.000 | 0.034 |
| ESR | |||
| Mean difference (%) | − 24.1 | 30.4 | 29.9 |
| p value | 0.000 | 0.000 | 0.000 |
Fig. 3.
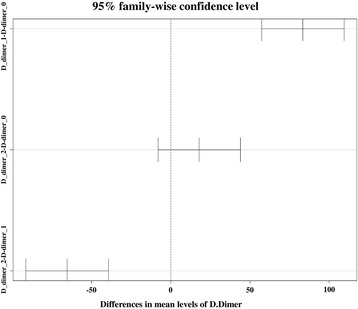
Comparison of the D-dimer level at the early postoperative period; differences in mean levels were presented as 95% confidence interval
Discussion
The principal findings of this study were (1) ESR started to increase at postoperative day 1, hits a peak on day 5, and maintained a slightly elevated level at postoperative week 6; (2) CRP started to increase after operation, hits a peak on day 2 or 3 and diminished to a normal level at postoperative week 2; and (3) D-dimer sharply increased after operation, hits a peak on day 1, sharply decreased on day 2, after then slowly increased up to postoperative week 2, and decreased to the nearly normal level at postoperative week 6. From our analysis, we could assume that absence of the sharp decrease on day 2 or 3 in D-dimer may be abnormal. Additionally, it was also assumed that it would be abnormal if there is no decrease on day 5 results of the ESR and CRP compared to results of day 3 and an additional sharp increase of the D-dimer.
Lower limb orthopedic surgery such as THA and TKA results in increased coagulation and inflammatory reactions postoperatively [17]. Oelsner et al. [18] reported that acute phase response was both predictable and consistent in healthy person after THA and TKA; however, there was a different response to TKA and THA and the peak CRP and fibrinogen were significantly higher for TKA than THA. In a study by Hughes et al. [17], THA and TKA resulted in similar changes of coagulation and non-specific inflammatory biomarkers such as ESR, CRP, and D-dimer. Bytniewski et al. [12] also reported that the distribution of D-dimer values throughout the entire postoperative period was not specific in any group.
Most important problem of biomarkers is that they are not specific to the infection and they can be elevated in with various causes. Kim et al. [8] evaluated the causes of elevated CRP level in the early postoperative period after primary TKA. They reported that 24% caused by postoperative infection, 20% by idiopathic cause, 16% by urologic problem, 14% by gastrointestinal problem, 13% by vascular problem, and 13% by respiratory problem. Therefore, diagnosis of PJI commonly relies on a combination of clinical judgment, serologic testing, information obtained from joint aspiration, radiologic assessment, and microbiologic as well as histopathologic testing obtained at the surgery [19, 20]. However, of these methods, serologic tests are most widely used as a primary screening test to predict infection.
D-dimer was originally used in screening DVT or PE after total joint arthroplasty. It has been also controversial in diagnosing DVT or PE because of low specificity [12, 21–23]. However, one important characteristic of D-dimer is that it shows sharp increase up to double levels and decrease to the baseline level within a short time during early postoperative period [12]. According to recent literature, serum D-dimer is a marker for the diagnosis of PJI, and the median D-dimer level was significantly higher for the patients with PJI than for the patients with aseptic failure [13]. Our results also showed the sharp increase and decrease within postoperative day 1, and it hit the peak more than double levels within a short time period. Additionally, it showed dull slope after the abrupt change even though there was second peak at postoperative week 2. It means that it only takes within 1 day for the first peak and more than 2 weeks for the second peak. Therefore, this information could be helpful in diagnosing postoperative infection in the earlier time period with combination of basic screening tests such as ESR and CRP.
Our study has some limitations that should be considered. First, there was no control group and serial assessment was only performed with patients who were not infected. Therefore, we do not know how values can change after infection. Second, time interval between postoperative day 5 and week 2 and between weeks 2 and 6 is long; there could be different results in terms of peak level and period of the ESR and second peak of the D-dimer. Third, we usually perform diagnostic procedure for detecting DVT in patients who show symptoms. However, there was no patient who showed suspicious symptoms of DVT. Therefore, we cannot know how many patients had silent DVT or pulmonary thromboembolism. Finally, values showed a little large range. Therefore, it would be a little difficult to apply all patients that have different characteristics. Nevertheless, we could find a dramatic change of the D-dimer level during early postoperative period and it could enable us to determine whether the arthroplasty is abnormal or not. Furthermore, the judgment would be more accurate if we consider all three tests together.
Conclusion
D-dimer showed a rapid and different pattern of the change at a very early postoperative period. It was assumed that this test would be used effectively in diagnosing early postoperative infection with the combination of the ESR and CRP. This natural progress can serve as a baseline for early diagnosis of infection.
Acknowledgements
We appreciate the statistical support from Ms. Sang Mee Hwang.
Funding
This study was supported by Corentec (Cheonan, South Korea).
Availability of data and materials
None
Abbreviations
- CCI
Charlson comorbidity index
- CRP
C-reactive protein
- DVT
Deep vein thrombosis
- ESR
Erythrocyte sedimentation rate
- PE
Pulmonary embolism
- PJI
Periprosthetic joint infection
- SD
Standard deviation
- THA
Total hip arthroplasty
- TKA
Total knee arthroplasty
- VTE
Venous thromboembolism
Authors’ contributions
YSL and KHK contributed to the study concept and design. YKL, SBH, and CHN coordinated the sampling and data collection. YSL and YKL contributed to the data analysis. YKL, KHK, and YSL contributed in writing the manuscript. KHK and YSL contributed to the critical review of the manuscript. All authors approved the final manuscript.
Authors’ information
Not applicable
Ethics approval and consent to participate
Ethical approval was obtained from IRB of Seoul National University Bundang Hospital. Informed consent was obtained from all participants.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Yong Seuk Lee, Email: smcos1@daum.net.
Young-Kyun Lee, Phone: 82-31-787-7204, Email: ykleemd@gmail.com.
Seung Bum Han, Email: sbhan1107@gmail.com.
Chang Hyun Nam, Email: changcap@hanmail.net.
Javad Parvizi, Email: javadparvizi@gmail.com.
Kyung-Hoi Koo, Email: khkoo@snu.ac.kr.
References
- 1.Parvizi J, Cavanaugh PK, Diaz-Ledezma C. Periprosthetic knee infection: ten strategies that work. Knee Surg Relat Res. 2013;25(4):155. doi: 10.5792/ksrr.2013.25.4.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Parvizi J, Ghanem E, Azzam K, et al. Periprosthetic infection: are current treatment strategies adequate? Acta Orthop Belg. 2008;74(6):793. [PubMed] [Google Scholar]
- 3.Wyatt MC, Beswick AD, Kunutsor SK, et al. The alpha-defensin immunoassay and leukocyte esterase colorimetric strip test for the diagnosis of periprosthetic infection: a systematic review and meta-analysis. J Bone Joint Surg Am. 2016;98(12):992. doi: 10.2106/JBJS.15.01142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Parvizi J, Shohat N, Gehrke T. Prevention of periprosthetic joint infection: new guidelines. Bone Joint J. 2017;99-B(4 Supple B):3. doi: 10.1302/0301-620X.99B4.BJJ-2016-1212.R1. [DOI] [PubMed] [Google Scholar]
- 5.Whitehouse MR, Parry MC, Konan S, et al. Deep infection after hip arthroplasty: staying current with change. Bone Joint J. 2016;98-B(1 Suppl A):27. doi: 10.1302/0301-620X.98B1.36294. [DOI] [PubMed] [Google Scholar]
- 6.George DA, Gant V, Haddad FS. The management of periprosthetic infections in the future: a review of new forms of treatment. Bone Joint J. 2015;97-B(9):1162. doi: 10.1302/0301-620X.97B9.35295. [DOI] [PubMed] [Google Scholar]
- 7.Choi HR, Agrawal K, Bedair H. The diagnostic thresholds for synovial fluid analysis in late periprosthetic infection of the hip depend on the duration of symptoms. Bone Joint J. 2016;98-B(10):1355. doi: 10.1302/0301-620X.98B10.37615. [DOI] [PubMed] [Google Scholar]
- 8.Kim TW, Kim DH, Oh WS, et al. Analysis of the causes of elevated C-reactive protein level in the early postoperative period after primary total knee arthroplasty. J Arthroplast. 2016;31(9):1990. doi: 10.1016/j.arth.2016.02.037. [DOI] [PubMed] [Google Scholar]
- 9.Berbari E, Mabry T, Tsaras G, et al. Inflammatory blood laboratory levels as markers of prosthetic joint infection: a systematic review and meta-analysis. J Bone Joint Surg Am 2010; 92(11):2102. [DOI] [PubMed]
- 10.McArthur BA, Abdel MP, Taunton MJ, et al. Seronegative infections in hip and knee arthroplasty: periprosthetic infections with normal erythrocyte sedimentation rate and C-reactive protein level. Bone Joint J. 2015;97-B(7):939. doi: 10.1302/0301-620X.97B7.35500. [DOI] [PubMed] [Google Scholar]
- 11.Parvizi J, Haddad FS. Periprosthetic joint infection: the last frontier. Bone Joint J. 2015;97-B(9):1157. doi: 10.1302/0301-620X.97B9.37018. [DOI] [PubMed] [Google Scholar]
- 12.Bytniewski P, Machala W, Romanowski L, et al. The dynamics of D-dimer level fluctuation in patients after the cemented and cementless total hip and total knee replacement. J Orthop Surg Res. 2014;9:89. doi: 10.1186/s13018-014-0089-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shahi A, Kheir MM, Tarabichi M, et al. Serum D-Dimer test is promising for the diagnosis of periprosthetic joint infection and timing of reimplantation. J Bone Joint Surg Am. 2017;99(17):1419. doi: 10.2106/JBJS.16.01395. [DOI] [PubMed] [Google Scholar]
- 14.Fehring TK, Odum SM, Berend KR, et al. Failure of irrigation and debridement for early postoperative periprosthetic infection. Clin Orthop Relat Res. 2013;471(1):250. doi: 10.1007/s11999-012-2373-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bucek RA, Koca N, Reiter M, et al. Algorithms for the diagnosis of deep-vein thrombosis in patients with low clinical pretest probability. Thromb Res. 2002;105(1):43. doi: 10.1016/S0049-3848(01)00411-X. [DOI] [PubMed] [Google Scholar]
- 16.Schutgens RE, Haas FJ, Gerritsen WB, et al. The usefulness of five D-dimer assays in the exclusion of deep venous thrombosis. J Thromb Haemost. 2003;1(5):976. doi: 10.1046/j.1538-7836.2003.00148.x. [DOI] [PubMed] [Google Scholar]
- 17.Hughes SF, Hendricks BD, Edwards DR, et al. Lower limb orthopaedic surgery results in changes to coagulation and non-specific inflammatory biomarkers, including selective clinical outcome measures. Eur J Med Res. 2013;18:40. doi: 10.1186/2047-783X-18-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Oelsner WK, Engstrom SM, Benvenuti MA, et al. Characterizing the acute phase response in healthy patients following total joint arthroplasty: predictable and consistent. J Arthroplast. 2016; [DOI] [PMC free article] [PubMed]
- 19.Parvizi J. New definition for periprosthetic joint infection. Am J Orthop (Belle Mead NJ) 2011;40(12):614. [PubMed] [Google Scholar]
- 20.Parvizi J, Gehrke T. Definition of periprosthetic joint infection. J Arthroplast. 2014;29(7):1331. doi: 10.1016/j.arth.2014.03.009. [DOI] [PubMed] [Google Scholar]
- 21.Song K, Yao Y, Rong Z, et al. The preoperative incidence of deep vein thrombosis (DVT) and its correlation with postoperative DVT in patients undergoing elective surgery for femoral neck fractures. Arch Orthop Trauma Surg. 2016;136(10):1459. doi: 10.1007/s00402-016-2535-4. [DOI] [PubMed] [Google Scholar]
- 22.Chen CJ, Wang CJ, Huang CC. The value of D-dimer in the detection of early deep-vein thrombosis after total knee arthroplasty in Asian patients: a cohort study. Thromb J. 2008;6:5. doi: 10.1186/1477-9560-6-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gambhir RP. Another nail in the coffin for role of D-dimer in diagnosis of postoperative deep vein thrombosis. Ann R Coll Surg Engl. 2009;91(4):355. doi: 10.1308/003588409X428324. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
None


