Abstract
Purpose
The purpose of this article was to assess segregation’s role on race differences in hypertension among non-Hispanic Blacks and Whites aged 50 and over.
Method
Hypertension was defined as systolic blood pressure (BP) ≥ 140 mmHg, diastolic BP ≥ 90 mmHg, or self-reported antihypertensive medication use. Segregation measures combined race, neighborhood racial composition, and individual and neighborhood poverty level. Logistic models produced odds ratios and 95% confidence intervals (CIs) for each segregation category, adjusting for health-related factors.
Results
Blacks in Black (OR = 2.54, CI = [1.61, 4.00]), White (OR = 2.56, CI = [1.24, 5.31]), and integrated neighborhoods (OR = 3.23, CI = [1.72, 6.03]) had greater odds of hypertension compared with Whites in White neighborhoods. Poor Whites in poor neighborhoods (OR = 1.74, CI = [1.09, 2.76]), nonpoor Blacks in nonpoor (OR = 3.03, CI = [1.79, 5.12]) and poor neighborhoods (OR = 4.08, CI = [2.16, 7.70]), and poor Blacks in nonpoor (OR = 4.35, CI = [2.17, 8.73]) and poor neighborhoods (OR = 2.75, CI = [1.74, 4.36]) had greater odds compared with nonpoor Whites in nonpoor neighborhoods.
Conclusion
Interventions targeting hypertension among older adults should consider neighborhood compositions.
Keywords: African American older adults, racial health disparities, neighborhoods, segregation, hypertension
Hypertension affects more than 67 million adults in the United States (Nwankwo, Yoon, Burt, & Gu, 2013). More specifically, one in three adults has been diagnosed with hypertension and its prevalence increases with age. More than half of Americans older than 55 and more than 65% of Americans older than 65 have hypertension (Go et al., 2013). Previous research has shown that there are disparities between Blacks’ and Whites’ prevalence of hypertension (Delgado, Jacobs, Lackland, Evans, & de Leon, 2012; Thorpe et al., 2014). Among adults in the United States, 33.9% and 31.3% of White men and women have hypertension whereas 43.0% and 45.7% of Black men and women have the condition, respectively (Go et al., 2013).
The U.S. government has taken a strong interest in decreasing and eliminating health disparities (National Prevention Council, 2011; National Center for Health Statistics, 2012). However, little progress has been achieved as Black adults still have higher rates of various diseases, including hypertension (Gillespie & Hurvitz, 2013). Several individual-level variables, such as socioeconomic status (SES), and health-related behaviors, have been tested to account for the disparities in hypertension prevalence. However, differences persist after accounting for them. With the U.S. population “aging” to include a larger number of older adults and its racial demographics shifting as the number of minorities increase, it has become imperative to understand variables that can explain racial differences in hypertension in older adults.
Efforts to understand racial disparities in hypertension prevalence in older adults are hindered by the strong correlation between racial status and SES. In the United States, African Americans tend to have lower SES, resulting in fewer socioeconomic resources at their disposal than Whites (Thorpe, Brandon, & LaVeist, 2008; Williams & Collins, 2001). Because of the correlation, detangling the direct effect of SES on health disparities in hypertension prevalence in older adults separate from racial effects is problematic (LaVeist et al., 2007). Often, multivariate regression is used to model disparities in health statuses in older adults and SES is included as a covariate in the model to address the race/SES confounding. While it is commonly used, it may not be enough to adjust for the total confounding of race and SES (LaVeist et al., 2007). In addition, previous work has shown that disparities in health statuses persist across SES levels for Blacks, not just at lower SES levels (Landrine & Corral, 2009). As a result, focus has shifted to accounting for social context and factors, such as neighborhood-level variables, when assessing racial health disparities between Black and White older adults. One particular neighborhood-level variable that may offer more insight into racial health disparities between Black and White older adults is residential segregation.
Residential segregation is a potential explanation for the differences in hypertension prevalence in older adults. Race in the United States, particularly for older Blacks, is an important determinant of the life course. In many cases, the neighborhoods that older Blacks live in have adverse aspects, such as lower numbers of grocery stores, higher crime rates, and exposure to toxins (Kramer & Hogue, 2009; Landrine & Corral, 2009; Williams & Collins, 2001). Therefore, racial segregation can lead to different exposures that can be associated with adverse outcomes including hypertension (Diez Roux & Mair, 2010; Thorpe et al., 2008). Failing to account for the differential health risk exposures between Black and White older adults may lead investigators to draw erroneous conclusions regarding the etiology of race differences in hypertension prevalence among older adults.
Prior work has examined the effects of residential segregation on hypertension prevalence among adults. For example, Thorpe et al. (2008) found that social and environmental exposures resulting from residential segregation explained a significant proportion of racial differences in hypertension prevalence. This was done by comparing findings from the Exploring Health Disparities in Integrated Communities (EHDIC) study, which accounted for social and environmental exposures, with findings from the National Health and Nutrition Examination Survey (NHANES) 1999–2004, which did not account for such exposures. Morenoff et al. (2007) found that adjusting for social context, such as gentrification and age composition of the neighborhood, eliminated race disparities in hypertension between Blacks and Whites. Kershaw et al. (2011) found that racial disparities in hypertension are modified by racial segregation and neighborhood poverty. While these studies have provided key information to our understanding of how residential segregation might impact disparities in hypertension, none of these studies focused on this relationship among community-dwelling older adults. However, Svetkey, George, Burchett, Morgan, and Blazer (1993) found that Black older adults aged 65 and older have significantly higher odds of hypertension compared with White older adults. In addition, Delgado et al. (2012) found racial differences in hypertension prevalence, awareness, and control in non-Hispanic African Americans and Whites 65 years and older. Investigating the role of residential segregation in the relationship between race and hypertension prevalence may explain some of the racial disparities in hypertension previously reported.
To our knowledge, while other studies have assessed the relationship between race and hypertension in older adults (Delgado et al., 2012; Svetkey et al., 1993) as well as the role of residential segregation in explaining existing disparities in hypertension prevalence of all adults (Kershaw et al., 2011; Morenoff et al., 2007; Thorpe et al., 2008), no other study has sought to assess the role of residential segregation in the existence of disparities of hypertension prevalence between Black and White communitydwelling older adults, separate from younger adults. It is useful to observe the relationships in community-dwelling older adults separately from younger adults, as the current cohort of older adults in the United States have lived during a period of lawful residential segregation in this country. As a result, it is possible that the impact of residential segregation on health disparities might differ between older adults and younger adults who did not live during the period of legally enforced residential segregation (Williams & Collins, 2001).
The purpose of this study is to examine the relationship between race, residential segregation, and hypertension prevalence in Black and White older adults 50 years of age and older in the United States. In particular, this study examined (a) whether hypertension prevalence in older adults is higher in predominantly Black neighborhoods compared with predominantly White neighborhoods, (b) whether hypertension prevalence in older adults is higher in poor neighborhoods compared with nonpoor neighborhoods, and (c) whether the influence of neighborhood racial composition and poverty concentration varies between Black and White older adults. It was hypothesized as follows:
Hypothesis 1: Black and White older adults living in predominantly Black neighborhoods have higher odds of hypertension compared with White older adults living in predominantly White neighborhoods.
Hypothesis 2: Poor older adults living in poor neighborhoods have higher odds of hypertension compared with nonpoor older adults living in nonpoor neighborhoods.
Hypothesis 3: Black and White poor older adults living in poor neighborhoods have higher odds of hypertension compared with nonpoor White older adults living in nonpoor neighborhoods.
Method
Sample
The NHANES was designed to determine the health, functional, and nutritional status of the U.S. population. Since 1999, NHANES has been conducted as a continuous, annual survey with public use data files released in 2-year periods. Each iteration of this cross-sectional survey is a nationally representative sample of the civilian, noninstitutionalized population of the United States. The survey oversamples participants 12 to 19 years of age and 60 years of age and older, Blacks, Mexican Americans, and low-income individuals. Each of the surveys uses a stratified, multistage probability sample design. Data were collected from respondents first in a home interview to gather information regarding the participant’s health history, health behaviors, health utilization, and risk factors. At the conclusion of the interview, participants were invited to receive a physical examination at a mobile examination center. Among those who participated in the examination, a nationally representative subset underwent laboratory tests. Additional details regarding the NHANES data collection or design can be found elsewhere (National Center for Health Statistics [NCHS], 2004).
For the purposes of this study, we linked NHANES data to 2000 U.S. Census data to measure residential segregation and concentrated poverty within participants’ residential census tract (United States Census Bureau, 2001). Because of the need to access participants’ census tract information, the analysis was performed at the NCHS Research Data Center under the supervision of NCHS staff to preserve the privacy, anonymity, and confidentiality of NHANES respondents. In this study, we use the combined 1999–2004 data sets of adults aged 50 and older who completed the household interview, physical examination, and laboratory components.
We restricted the analysis to non-Hispanic Black (n = 442) and non-Hispanic White (n = 1,603) adults aged 50 years and older, for a total of 2,045 subjects. The analysis included only non-Hispanic White and non-Hispanic Black adults due to the small sample sizes of other minority groups present in the NHANES data. In many studies of older adults, the minimum age is 65 years. However, decreasing the minimum age to 50 years provided a much larger sample size for the Black participants in this study.
Dependent Variable
Three to four measurements of blood pressure were taken in one visit after resting quietly in a sitting position for 5 min and the mean value was recorded (NCHS, 2003–2004). Hypertension was defined as having an average systolic blood pressure (SBP) of 140 or above, an average diastolic blood pressure (DBP) of 90 or above, or having a reported history of taking antihypertensive medication. A binary variable was created to identify individuals who were considered hypertensive compared with those who were not.
Key Independent Variables
Census tracts were used as proxies for neighborhoods because they are permanently defined subdivisions with similar neighborhood characteristics (Krieger, Chen, Waterman, Rehkopf, & Subramanian, 2005). Instead of using a formal measure of residential segregation, a race–poverty–place variable was used, which took into account an individual’s race, an individual’s poverty level, the racial composition of the participant’s neighborhood, and the poverty level of the participant’s neighborhood. Three categorical measures of residential segregation with binary values were created: race–place, poverty–place, and race–poverty–place. These variables, and the cutoffs used to define them, have been used elsewhere (Gaskin et al., 2014).
The race–place variable represented residential segregation as combinations of individual race and neighborhood racial composition. A neighborhood was deemed predominantly Black, White, or Other if 65% or more of the inhabitants of the neighborhood identified as being of that race. If not, the neighborhood was labeled integrated. Each study participant was categorized into one of eight categories: White in a predominantly White neighborhood, White in a predominantly Black neighborhood, White in a predominantly Other race neighborhood, White in an integrated neighborhood, Black in a predominantly White neighborhood, Black in a predominantly Black neighborhood, Black in a predominantly Other race neighborhood, and Black in an integrated neighborhood.
The poverty–place variable represented residential segregation as combinations of individual poverty with neighborhood poverty. The poverty line of an individual was defined as the ratio of income to poverty level, as defined by the federal government. An individual was considered “poor” if their income was 200% of the federal poverty line or less. A neighborhood was deemed a “poor” neighborhood if at least 20% of its inhabitants were considered poor, using the requirement stated in the previous sentence. The four categories are nonpoor in a nonpoor neighborhood, nonpoor in a poor neighborhood, poor in a nonpoor neighborhood, and poor in a poor neighborhood.
The race–poverty–place variable combined the two previous variables to create a measure that represents the combinations of individual race, individual poverty, and neighborhood poverty. The eight categories are nonpoor White in a nonpoor neighborhood, nonpoor White in a poor neighborhood, poor White in a nonpoor neighborhood, poor White in a poor neighborhood, nonpoor Black in a nonpoor neighborhood, nonpoor Black in a poor neighborhood, poor Black in a nonpoor neighborhood, and poor Black in a poor neighborhood.
Covariates
Age was measured as a continuous variable in years. Gender was included as a binary variable, with female being the reference group. Race was measured as a dichotomous variable, with White being the reference group. Urban residence was measured as a binary variable, with living in a rural area serving as the reference group. Education was defined as the highest level completed and measured categorically as less than ninth grade, ninth to 11th grade, high school diploma or completion of general education development (GED) (reference), some college, and college graduate or higher. Insurance type was defined categorically as private insurance (reference), Medicare, Medicaid, State Children’s Health Insurance Program (SCHIP), or other government source, and uninsured. Body mass index (BMI) was measured and categorized as normal (BMI < 25), overweight (BMI between 25 and 29.9), and obese (BMI > 30), with normal being the reference group. The number of comorbidities was defined as the number of the following conditions an individual had: kidney disease, angina, coronary heart disease, and diabetes. Each condition was defined as a binary variable, where 1 indicated that the individual was diagnosed with the condition. We then summed across the binary variables to determine the number of chronic conditions each participant reported. Those participants who reported 0 or 1 comorbid conditions served as the reference group. Finally, individual poverty ratio and an indicator representing neighborhood poverty were included in the race–place models. Individual poverty was categorized into five levels: below 100% of federal poverty level (FPL), 100% to 199% of FPL, 200% to 299% of FPL, 300% to 399% of FPL, and 400% or more of FPL, with 400% or more of FPL serving as the reference group. Neighborhood poverty was dichotomized, with neighborhoods with less than 20% of its inhabitants considered poor serving as the respective reference groups.
Analysis Plan
Means and standard deviations were calculated for age. Proportions were calculated for the categorical variables. Age for each race was compared using a z-test while categorical variables for each race were compared using a chi-square test.
Logistic regression was used to estimate the disparities in hypertension prevalence between Blacks and White older adults while accounting for the covariates. A series of models were fit for a base model that did not include residential segregation measures as well as for each of the three measures of residential segregation. Model 1 adjusted for race (when not accounted for using segregation measures), age, gender, and urban residence. Model 2 also adjusted for education, insurance type, individual poverty/income ratio, and neighborhood poverty (when not accounted for using segregation measures). Last, Model 3 adjusted for BMI and number of comorbidities. Parameter estimates and standard errors were adjusted using the multistage sampling design with Taylor linearization methods. Following the algorithm designed by NCHS, we created a 6-year sample weight variable by assigning two thirds of the 4-year weight for 1999–2002 if the person was sampled in that time period or assigning one third of the 2-year weight for 2003–2004 if the person was sampled in that time frame. p values less than .05 were considered statistically significant. Stata version 13 (StataCorp, 2013) were used to conduct all analyses.
Results
The distribution of hypertension prevalence among independent variables is displayed in Table 1. The prevalence of hypertension in Black and White older adults differs with regard to some of the covariates. Black older adults have higher rates of hypertension than White older adults (0.79 vs. 0.59; p < .001). The rate for female older adults is higher than the rate for male older adults (0.68 vs. 0.58; p < .001). Older adults with less than a ninth-grade education (0.63), some college (0.64), or a college degree (0.51) have lower rates of hypertension than those who have a high school diploma (0.67), while those with ninth- through 12th-grade educations with no diploma have higher rates (0.73; p < .001). The rates of hypertension tended to increase as income decreased. Older adults with an income of 400% of the federal poverty line or more have the lowest rate of hypertension at 0.53, followed by older adults between 300% and 399% FPL (0.59), older adults between 100% and 199% FPL (0.68), older adults between 200% and 299% FPL (0.70), and older adults at or below FPL (0.74; p < .001). Those with Medicare (0.73) or Medicaid or other government-provided health insurance (0.63) have higher rates of hypertension than those with private health insurance (0.60), while those with no health insurance have lower rates (0.52; p < .001). Overweight and obese older adults (0.63 and 0.74) have higher rates than older adults with normal BMI (0.53; p < .001). Those with two or more comorbid conditions have higher rates of hypertension than those with none or one comorbid condition (0.76 vs. 0.62; p < .001). Older adults who live in neighborhoods in which 20% or more of the inhabitants are considered poor have higher rates of hypertension than those who do not live in such neighborhoods (0.74 vs. 0.60; p < .001). Older adults who live in predominantly Black neighborhoods (0.78), predominantly Other race neighborhoods (0.73), and integrated neighborhoods (0.61) have higher rates of hypertension than older adults living in predominantly White neighborhoods (0.60; p < .001).
Table 1.
Distribution of Hypertension Prevalence by Select Characteristics.
| Independent variables |
Categories | Hypertension prevalence (n = 1,288) | ||
|---|---|---|---|---|
|
| ||||
| N | Proportion | p value | ||
| Individual race | Black | 347 | 0.785 | <.001 |
| White (Ref) | 941 | 0.587 | ||
| Gender | Male | 695 | 0.580 | <.001 |
| Female (Ref) | 593 | 0.680 | ||
| Neighborhood area type | Urban | 1,048 | 0.632 | .716 |
| Rural (Ref) | 240 | 0.622 | ||
| Education | Less than 9th grade | 192 | 0.634 | <.001 |
| 9th–12th grade, no diploma | 175 | 0.729 | ||
| High school graduate (Ref) | 359 | 0.671 | ||
| Some college | 333 | 0.642 | ||
| College graduate or higher | 229 | 0.511 | ||
| Individual poverty status | Household poverty below FPL | 155 | 0.742 | <.001 |
| Household poverty 1–1.99 FPL | 345 | 0.685 | ||
| Household poverty 2–2.99 FPL | 263 | 0.703 | ||
| Household poverty 3–3.99 FPL | 144 | 0.593 | ||
| Household poverty 4 or above FPL (Ref) | 381 | 0.533 | ||
| Insurance status | Private insurance (Ref) | 773 | 0.599 | <.001 |
| Medicare | 391 | 0.727 | ||
| Medicaid, SCHIP, other insurance | 63 | 0.630 | ||
| Uninsured | 61 | 0.521 | ||
| Body mass index category | Normal/underweight (Ref) | 318 | 0.531 | <.001 |
| Overweight | 554 | 0.630 | ||
| Obese | 416 | 0.735 | ||
| Comorbid conditions | 0–1 comorbid conditions (Ref) | 1,159 | 0.618 | <.001 |
| 2 or more comorbid conditions | 129 | 0.763 | ||
| Neighborhood poverty level | Less than 20% poor inhabitants (Ref) | 999 | 0.603 | <.001 |
| 20% or more poor inhabitants | 289 | 0.745 | ||
| Neighborhood racial composition | Predominantly White neighborhood (Ref) | 881 | 0.603 | <.001 |
| Predominantly Black neighborhood | 197 | 0.782 | ||
| Predominantly Other race neighborhood | 38 | 0.731 | ||
| Integrated neighborhood | 172 | 0.612 | ||
Note. FPL = federal poverty level, SCHIP=State Children’s Health Insurance Program.
Table 2 displays hypertension prevalence for each segregation category. Combining individual race and neighborhood racial composition showed that Black older adults have higher rates of hypertension, regardless of neighborhood racial composition, than White older adults in predominantly White neighborhoods. The hypertension rates for Black older adults are 0.79, 0.72, 0.91, and 0.79 for predominantly White, Black, Other race, and integrated neighborhoods, respectively, while the rate for White older adults in predominantly White neighborhoods is 0.60 (p < .001). Combining individual poverty and neighborhood poverty concentration showed that poor older adults in poor neighborhoods had the highest rate of hypertension (0.76), followed by nonpoor in poor neighborhoods (0.73), poor in nonpoor neighborhood (0.68), and nonpoor older adults in nonpoor neighborhoods (0.58; p < .001). Combining individual race, individual poverty, and neighborhood poverty concentration showed that poor White older adults and Black older adults have higher rates of hypertension than nonpoor White older adults. Poor White older adults in nonpoor neighborhoods (0.65), poor Whites in poor neighborhoods (0.72), nonpoor Black older adults in nonpoor neighborhoods (0.72), nonpoor Blacks in poor neighborhoods (0.84), poor Blacks in nonpoor neighborhoods (0.83), and poor Blacks in poor neighborhoods (0.77) have higher rates of hypertension than nonpoor White older adults in nonpoor neighborhoods (0.56; p < .001).
Table 2.
Distribution of Hypertension Prevalence by Segregation Categories.
| Independent variables |
Categories | Hypertension Prevalence (n = 1,288) |
||
|---|---|---|---|---|
|
| ||||
| n | Proportion | p value | ||
| Race–place Individual race and neighborhood racial composition | White in White neighborhood (Ref) | 1,389 | 0.598 | <.001 |
| White in Black neighborhood | 5 | 0.400 | ||
| White in Other race neighborhood | 30 | 0.600 | ||
| White in integrated neighborhood | 179 | 0.508 | ||
| Black in Black neighborhood | 247 | 0.789 | ||
| Black in White neighborhood | 71 | 0.718 | ||
| Black in Other race neighborhood | 22 | 0.909 | ||
| Black in integrated neighborhood | 102 | 0.794 | ||
| Poverty–place Individual poverty and neighborhood poverty concentration | Nonpoor in nonpoor neighborhood (Ref) | 1,166 | 0.572 | <.001 |
| Poor in nonpoor neighborhood | 491 | 0.676 | ||
| Nonpoor in poor neighborhood | 166 | 0.729 | ||
| Poor in poor neighborhood | 222 | 0.757 | ||
| Race–place–poverty Individual race and poverty and neighborhood poverty concentration | Nonpoor White in nonpoor neighborhood (Ref) | 1,064 | 0.558 | <.001 |
| Nonpoor White in poor neighborhood | 51 | 0.490 | ||
| Poor White in nonpoor neighborhood | 416 | 0.649 | ||
| Poor White in poor neighborhood | 72 | 0.722 | ||
| Nonpoor Black in nonpoor neighborhood | 102 | 0.716 | ||
| Nonpoor Black in poor neighborhood | 115 | 0.835 | ||
| Poor Black in nonpoor neighborhood | 75 | 0.827 | ||
| Poor Black in poor neighborhood | 150 | 0.773 | ||
Table 3 displays estimated odds of hypertension, controlling for race, concentrated poverty, and neighborhood racial composition as well as estimated odds of hypertension under the race–place model. The base model assessed whether individual-level variables, neighborhood racial composition, and neighborhood poverty level separately explained the odds of hypertension. Blacks have an estimated 3.45 (95% confidence interval [CI] = [2.20, 5.39]) times higher odds of hypertension compared with Whites. The odds of having hypertension for males was 0.71 (95% CI = [0.56, 0.90]) times the odds for females. As expected, the odds of hypertension increased as age increased, 1.06 (95% CI = [1.05, 1.08]) for each yearly increase in age. Overweight and obese subjects had 1.61 (95% CI = [1.30, 1.98]) and 3.13 (95% CI = [2.39, 4.08]) times higher odds of hypertension compared with subjects with BMI falling within the normal range. In addition, those with two or more comorbid conditions had 1.94 (95% CI = [1.25, 3.03]) times greater odds of hypertension compared with those with none or one comorbid condition. However, individual poverty, neighborhood poverty, and neighborhood racial composition did not significantly explain odds of hypertension.
Table 3.
Estimated Odds of Hypertension Controlling for the Race, Concentrated Poverty, and Racial Composition of Neighborhood and Race–Racial Composition of Neighborhood (Race–Place).
| Base model | Race–place model | |||
|---|---|---|---|---|
|
|
|
|||
| OR | 95% CI | OR | 95% CI | |
| Race | ||||
| White | Ref | Ref | — | — |
| Black | 3.45 | [2.20, 5.39] | — | — |
| Neighborhood concentrated poverty | 1.21 | [0.87, 1.68] | 1.20 | [0.86, 1.68] |
| Neighborhood racial composition | ||||
| Predominantly White neighborhood | Ref | Ref | — | — |
| Predominantly Black neighborhood | 0.73 | [0.43, 1.23] | — | — |
| Predominantly Other race neighborhood | 1.02 | [0.48, 2.17] | — | — |
| Integrated neighborhood | 0.83 | [0.59, 1.15] | — | — |
| Race–place categories | ||||
| White in White neighborhood | — | — | Ref | Ref |
| White in Black neighborhood | — | — | 0.63 | [0.16, 2.57] |
| White in Other race neighborhood | — | — | 0.94 | [0.38, 2.36] |
| White in integrated neighborhood | — | — | 0.81 | [0.57, 1.14] |
| Black in Black neighborhood | — | — | 2.54 | [1.61, 4.00] |
| Black in White neighborhood | — | — | 2.56 | [1.24, 5.31] |
| Black in Other race neighborhood | — | — | 6.09 | [0.82, 45.31] |
| Black in integrated neighborhood | — | — | 3.23 | [1.73, 6.04] |
| Gender | ||||
| Female | Ref | Ref | Ref | Ref |
| Male | 0.71 | [0.56, 0.90] | 0.71 | [0.56, 0.90] |
| Age (years) | 1.06 | [1.05, 1.08] | 1.06 | [1.05, 1.08] |
| Neighborhood type | ||||
| Nonurban neighborhood | Ref | Ref | Ref | Ref |
| Urban neighborhood | 0.81 | [0.61, 1.09] | 0.81 | [0.61, 1.08] |
| Education | ||||
| Less than 9th grade | 0.75 | [0.52, 1.07] | 0.75 | [0.52, 1.07] |
| 9th–12th grade, no diploma | 0.82 | [0.47, 1.43] | 0.82 | 0.47, 1.43] |
| High school graduate | Ref | Ref | Ref | Ref |
| Some college | 1.08 | [0.79, 1.48] | 1.09 | [0.80, 1.48] |
| College graduate or higher | 0.72 | [0.50, 1.04] | 0.72 | [0.50, 1.04] |
| Household poverty ratio | ||||
| Household poverty 4 or higher | Ref | Ref | Ref | Ref |
| Household poverty 3–3.99 FPL | 0.99 | [0.64, 1.55] | 0.99 | [0.64, 1.54] |
| Household poverty 2–2.99 FPL | 1.47 | [0.94, 2.30] | 1.48 | [0.95, 2.31] |
| Household poverty 1–1.99 FPL | 1.18 | [0.85, 1.64] | 1.18 | [0.84, 1.65] |
| Household poverty below FPL | 1.44 | [0.91, 2.27] | 1.44 | [0.91, 2.26] |
| Insurance type | ||||
| Private insurance | Ref | Ref | Ref | Ref |
| Medicare | 1.03 | [0.74, 1.43] | 1.03 | [0.74, 1.43] |
| Medicaid, SCHIP, other government insurance | 0.93 | [0.57, 1.54] | 0.93 | [0.57, 1.54] |
| No insurance | 0.69 | [0.40, 1.20] | 0.69 | [0.40, 1.20] |
| BMI categories | ||||
| Normal/underweight | Ref | Ref | Ref | Ref |
| Overweight | 1.61 | [1.30, 1.98] | 1.60 | [1.30, 1.98] |
| Obese | 3.13 | [2.39, 4.08] | 3.12 | [2.39, 4.08] |
| Number of comorbidities | ||||
| 0 or 1 comorbid conditions | Ref | Ref | Ref | Ref |
| 2 or more comorbid conditions | 1.94 | [1.25, 3.03] | 1.94 | [1.24, 3.02] |
Note. OR = odds ratio; CI = confidence interval; FPL = federal poverty level; SCHIP=State Children’s Health Insurance Program; BMI = body mass index.
Hypothesis 1
The race–place model (Table 3) assessed whether an older adult’s racial status compared with the racial composition of their neighborhood explained their odds of having hypertension. The model also found that Black older adults living in predominantly Black, predominantly White, and integrated neighborhoods have odds of 2.54 (95% CI = [1.61, 4.00]), 2.56 (95% CI = [1.24, 5.31]), and 3.23 (95% CI = [1.73, 6.04]), respectively, compared with White older adults living in predominantly White neighborhoods. However, it did not find significantly altered odds for Black older adults living in neighborhoods with a predominant racial group other than Blacks and Whites. The model also found that age, gender, BMI, and number of comorbidities remained significantly associated with the odds of hypertension. The estimates and confidence intervals for the significant predictors remained strongly unchanged after accounting for the combination of individual racial status and neighborhood racial composition, compared with accounting for individual racial status alone.
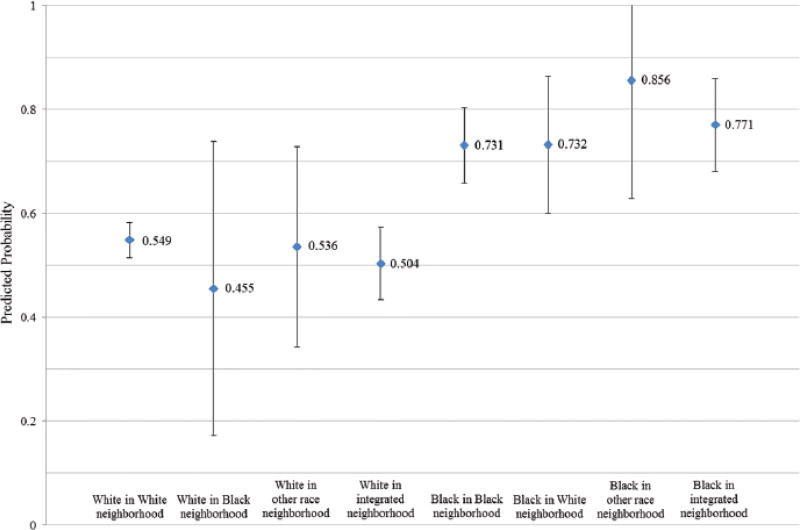
Figure 1 illustrates the predicted probability and 95% confidence interval of being hypertensive for each race-place category. The race-place categories corresponding to Black older adults have higher probabilies of hypertension compared to the categories corresponding to White older adults. However, the predicted probability for Black older adults living in predominantly other race neighborhoods has a wider 95% confidence interval than the other race-place categories for Black older adults.
Figure 1.
Predicted probabilities of hypertension based on race–place model.
Hypothesis 2
Table 4 displays estimated odds of hypertension, controlling for race, under the poverty–place and the race–poverty–place models. The poverty–place model assessed whether the combination of an older adult’s poverty status and their neighborhood’s poverty concentration explained their odds of having hypertension. Including the combination of individual poverty status and neighborhood poverty concentration did help explain some of the racial disparity in hypertension between Blacks and Whites. However, Black older adults still have 3.00 (95% CI = [2.09, 4.30]) times higher odds of hypertension compared with White older adults. Age, gender, BMI, and number of comorbidities remained significant predictors with associations relatively unchanged from the base model. In addition, older adults who graduated college have odds of hypertension 0.68 (95% CI = [0.49, 0.95]) times that of older adults who only graduated high school. Most importantly, the model did not find significant associations between the combination of individual and neighborhood poverty and the odds of having hypertension for anyone.
Table 4.
Estimated Odds of Hypertension Controlling for the Combinations of Individual and Neighborhood Poverty (Poverty–Place) and Individual Race, Poverty, and Neighborhood Poverty (Race–Poverty–Place).
| Poverty–place model |
Race–poverty– place model |
|||
|---|---|---|---|---|
|
|
|
|||
| OR | 95% CI | OR | 95% CI | |
| Race | ||||
| White | Ref | Ref | — | — |
| Black | 3.00 | [2.09, 4.30] | — | — |
| Poverty-place categories | ||||
| Nonpoor in nonpoor neighborhood | Ref | Ref | — | — |
| Poor in nonpoor neighborhood | 1.06 | [0.78, 1.43] | — | — |
| Nonpoor in poor neighborhood | 1.05 | [0.61, 1.82] | — | — |
| Poor in poor neighborhood | 1.34 | [0.99, 1.83] | — | — |
| Race-poverty-place categories | ||||
| Nonpoor White in nonpoor neighborhood | — | — | Ref | Ref |
| Nonpoor White in poor neighborhood | — | — | 0.94 | [0.47, 1.88] |
| Poor White in nonpoor neighborhood | — | — | 1.04 | [0.77, 1.40] |
| Poor White in poor neighborhood | — | — | 1.74 | [1.09, 2.76] |
| Nonpoor Black in nonpoor neighborhood | — | — | 3.03 | [1.79, 5.12] |
| Nonpoor Black in poor neighborhood | — | — | 4.08 | [2.16, 7.70] |
| Poor Black in nonpoor neighborhood | — | — | 4.35 | [2.17, 8.73] |
| Poor Black in poor neighborhood | — | — | 2.75 | [1.74, 4.37] |
| Gender | ||||
| Female | Ref | Ref | Ref | Ref |
| Male | 0.70 | [0.55, 0.89] | 0.70 | [0.55, 0.89] |
| Age (years) | 1.07 | [1.05, 1.08] | 1.07 | [1.05, 1.08] |
| Neighborhood type | ||||
| Nonurban neighborhood | Ref | Ref | Ref | Ref |
| Urban neighborhood | 0.81 | [0.60, 1.10] | 0.82 | [0.60, 1.11] |
| Education | ||||
| Less than 9th grade | 0.77 | [0.53, 1.10] | 0.76 | [0.53, 1.09] |
| 9th–12th grade, no diploma | 0.85 | [0.49, 1.45] | 0.84 | [0.49, 1.45] |
| High school graduate | Ref | Ref | Ref | Ref |
| Some college | 1.06 | [0.79, 1.43] | 1.06 | [0.79, 1.43] |
| College graduate or higher | 0.68 | [0.49, 0.95] | 0.68 | [0.49, 0.95] |
| Insurance type | ||||
| Private insurance | Ref | Ref | Ref | Ref |
| Medicare | 1.06 | [0.77, 1.47] | 1.06 | [0.77, 1.47] |
| Medicaid, SCHIP, other government insurance | 0.99 | [0.60, 1.62] | 0.98 | [0.59, 1.62] |
| No insurance | 0.75 | [0.44, 1.27] | 0.75 | [0.44, 1.27] |
| BMI categories | ||||
| Normal/underweight | Ref | Ref | Ref | Ref |
| Overweight | 1.61 | [1.31, 1.97] | 1.60 | [1.31, 1.96] |
| Obese | 3.16 | [2.41, 4.14] | 3.16 | [2.41, 4.14] |
| Number of comorbid conditions | ||||
| 0 or 1 comorbid conditions | Ref | Ref | Ref | Ref |
| 2 or more comorbid conditions | 1.98 | [1.27, 3.08] | 1.97 | [1.27, 3.06] |
Note. OR = odds ratio; CI = confidence interval; SCHIP=State Children’s Health Insurance Program.
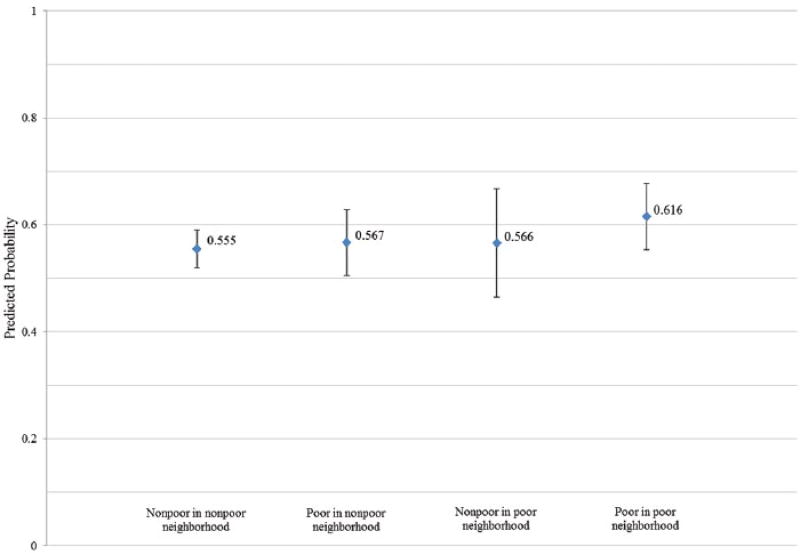
Figure 2 illustrates the predicted probability and 95% confidence interval of being hypertensive for each poverty-place category. The predicted probability for poor older adults living in poor neighborhoods is slightly higher than the other poverty-place categories, although no significant difference in odds of hypertension was detected for poor older adults living in poor neighborhoods.
Figure 2.
Predicted probabilities of hypertension based on poverty–place model.
Hypothesis 3
The race–poverty–place model (Table 4) assessed whether the combination of individual racial status, individual poverty status, and neighborhood poverty concentration explained the odds of having hypertension. The model found that not only Black older adults, regardless of individual and neighborhood poverty status, have significantly higher odds of hypertension but so do poor White older adults living in poor neighborhoods. Poor Whites in poor neighborhoods have increased odds of 1.74 (95% CI = [1.09, 2.76]), compared with nonpoor Whites in nonpoor neighborhoods. The odds of hypertension is 3.03 (95% CI = [1.79, 5.12]) times higher for nonpoor Blacks in nonpoor neighborhoods, 4.08 (95% CI = [2.16, 7.70]) times higher for nonpoor Blacks in poor neighborhoods, 4.35 (95% CI = [2.17, 8.73]) times higher for poor Blacks in nonpoor neighborhoods, and 2.75 (95% CI = [1.74, 4.37]) times higher for poor Blacks in poor neighborhoods, compared with nonpoor White older adults in nonpoor neighborhoods. The model did not find significant associations for nonpoor Whites or poor Whites living in nonpoor neighborhoods. As before, age, gender, BMI, number of comorbidities, and having a college degree were significant predictors of hypertension with associations very similar to those found in the base model and in the poverty–place model for having a college degree.
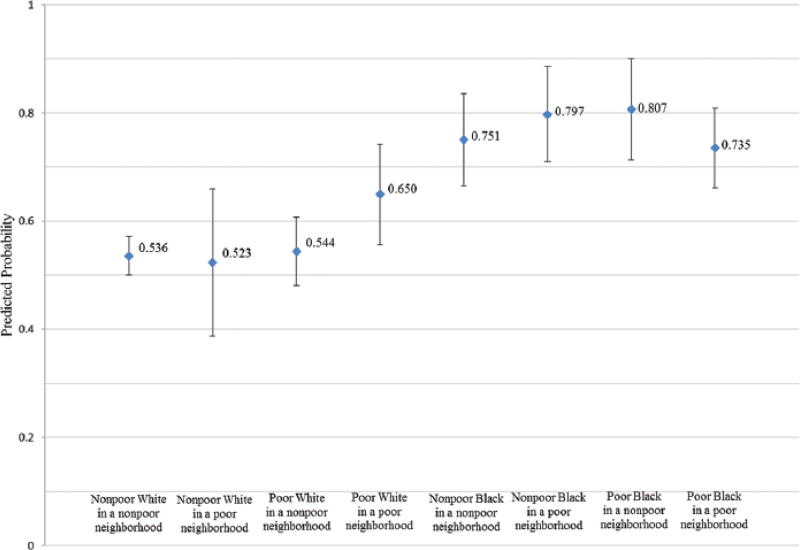
Figure 3 illustrates the predicted probability and 95% confidence interval of being hypertensive for each race-poverty-place category. The predicted probabilities for race-poverty-place categories corresponding to Black older adults are larger than the predicted probabilies for categories corresponding to White older adults. In addition, the predicted probability for poor White older adults living in poor neighborhoods is larger than the predicted probabilities for the other race-poverty-place categories corresponding to White older adults.
Figure 3.
Predicted probabilities of hypertension based on race–poverty–place model.
Discussion
The objectives of this study were to assess (a) whether hypertension prevalence in older adults is higher in predominantly Black neighborhoods compared with predominantly White neighborhoods, (b) whether hypertension prevalence in older adults is higher in poor neighborhoods compared with nonpoor neighborhoods, and (c) whether the influence of neighborhood racial composition and poverty concentration varies between Black and White older adults. The study found that Black older adults living in predominantly White, Black, or integrated neighborhoods have increased odds of hypertension compared with White older adults living in predominantly White neighborhoods. Perhaps more importantly, the study also found that while Black older adults have higher odds of hypertension regardless of individual and neighborhood poverty statuses, poor White older adults living in poor neighborhoods also have higher odds of hypertension compared with nonpoor Whites living in nonpoor neighborhoods. These findings underscore the importance of disentangling race-based residential segregation from race and hypertension prevalence among Black and White older adults.
The finding of significantly higher odds of hypertension for Black older adults living in predominantly White, Black, and integrated neighborhoods is consistent with other studies, such as Svetkey et al. (1993), which have shown increased odds of hypertension among Black older adults. In addition, finding that living in integrated neighborhoods does not decrease the odds of hypertension in Black older adults is consistent with prior work, specifically Kershaw et al. (2011), which found that although Blacks had significantly higher odds of hypertension, the race differences were smallest for those in low segregation areas. Previous work by Morenoff et al. (2007) showed that living in a neighborhood with a high number of Hispanic and/or foreign-born people did not significantly change the odds of hypertension in U.S. adults. This could be viewed as a similar finding to our finding that Black older adults living in predominantly Other race neighborhoods do not have significantly higher odds of hypertension compared with White older adults in predominantly White neighborhoods. However, such a statement is dependent on the makeup of the predominantly Other race neighborhoods. We encourage further research into this area.
While we found that Black older adults in predominantly White, Black, or integrated neighborhoods have significantly higher odds of hypertension compared with White older adults in predominantly White neighborhoods, we cannot make the same distinction for Black older adults living in neighborhoods where the predominant race of residents is neither Black nor White. There is a relatively small number of Black older adults who live in neighborhoods other than predominantly Black due to high rates of residential segregation for African Americans in the United States (Kramer & Hogue, 2009; Williams & Collins, 2001). It is plausible that most Blacks live in predominantly Black neighborhoods. Therefore, it creates small samples of Blacks who live in neighborhoods with a different predominant race, impairing our ability to detect a significant association for this category. In addition, Black older adults are a group that has been segregated and confined to certain neighborhoods (Williams & Collins, 2001). Even those who currently live in predominantly White and integrated neighborhoods may have previously lived in predominantly Black neighborhoods, which may have a lasting effect on their health status. Due to the differing experiences of segregation between younger and older adults, the issue of smaller samples of Blacks in predominantly other neighborhoods may be stronger or perhaps exclusive to older adults.
Our finding that Blacks have significantly higher odds of hypertension regardless of individual and neighborhood poverty status have been confirmed in some of the previously mentioned literature, such as Kershaw et al. (2011). However, the evidence that living in poor neighborhoods is associated with an increased odds of hypertension for poor White older adults compared with nonpoor White older adults in nonpoor neighborhoods has not been shown in prior work to our knowledge. This could be due to the race– poverty–place segregation measure. It is constructed as combinations of individual race and poverty status, as well as neighborhood poverty status. Such a fine partitioning allows our study to detect increased odds that other studies might not have found.
The increased odds of hypertension for Black older adults regardless of individual or neighborhood poverty may be related to selective survival, a common issue in the study of minority aging (Thorpe et al., 2012). As Blacks suffer higher rates of morbidity and shorter life expectancies, those who do live to older ages tend to be the healthiest of Black older adults (Thorpe et al., 2012). One of the advantages of using the minimum age of 50 in this study was that it helps minimize the presence of selective sampling by studying Blacks earlier in the life course, which would explain why we have similar findings to previous work that analyzed adults of all ages (Kershaw et al., 2011; Thorpe et al., 2008). However, if selective sampling is an issue despite the lower minimum age, it is possible that the robust health of this sample of Black older adults is protective against the effects of individual and neighborhood poverty. Another explanation is that prolonged effects of exposure to lawful segregation earlier in the life course may put people on a poor health trajectory, thus producing the differential health outcomes in later life.
The increased odds of hypertension for poor White older adults in poor neighborhoods compared with nonpoor Whites in nonpoor neighborhoods may be directly attributable to the effects of individual and neighborhood poverty. It is possible that the presence of both individual and neighborhood poverty interact to create a detrimental additive impact on health compared with the presence of individual or neighborhood poverty individually. In addition, because this finding is exclusive to older adults, there might be a cumulative effect of individual and neighborhood poverty across the life course that also may be creating an additive impact on health. Once again, we recommend further research that assess exposure to poverty across the life course. Finally, it is worth noting that the mechanisms that create higher prevalence of hypertension in older adults compared with younger adults may explain why we obtained a result that has not been previously found in all adults. Further research into these mechanisms is recommended.
Strengths and Limitations
This study has a number of strengths. First, this study uses NHANES, a nationally representative sample, linked to 2000 U.S. Census data to allow for an opportunity to understand the influence of residential segregation on race disparities in hypertension among community-dwelling older adults. Second, to our knowledge, there has never been a study conducted that looks at the relationship of race, residential segregation, and hypertension prevalence in community-dwelling older adults. Third, the study uses a combination of measured hypertension and self-reported use of antihypertensive medication, rather than using self-report alone.
Despite these strengths, the study does have limitations. This is a cross-sectional study, which makes causal inferences impossible. In addition, the study only utilized non-Hispanic Black and non-Hispanic White older adults. Future work in this area should consider Other racial/ethnic groups, such as Hispanics and Asians. Also, although the analysis adjusted for BMI levels and number of comorbidities, it did not adjust for other health variables such as self-rated health and included only a select number of conditions in determining the number of comorbidities. The study also pooled NHANES data from 1999–2004, therefore we must assume that associations between the independent variables and hypertension prevalence remained constant over time. We also used data from the 2000 U.S. Census to measure neighborhood metrics, such as racial composition and poverty and this assumes that the measures remain constant throughout the study period. In addition, because this analysis contains individual and neighborhood-level data, it seems logical to use multilevel modeling. However, after controlling for NHANES’s survey design, there were a small number of observations per census tract, making multilevel modeling unfeasible (Curtin et al, 2012). Last, as previously stated, the study used non-Hispanic Black and non-Hispanic White older adults aged 50 and older rather than aged 65 and older, to increase the sample size of community-dwelling non-Hispanic Black adults. Scholars conducting health disparities research in late life should ensure that they have sufficient numbers of non-Hispanic Blacks in their samples in the initial stages of analysis. If this is not the case, these scholars are encouraged to broaden the age range of the sample if possible (Thorpe et al., 2012). Even with the decrease in minimum age, associations for some residential segregation categories have larger standard errors than other residential segregation categories.
Conclusion
In a nationally representative sample, individual poverty as well as neighborhood poverty where White older adults live had an influence on their hypertension prevalence while Black older adults had greater odds of hypertension regardless of individual and neighborhood poverty levels. These findings highlight the importance of understanding how residential segregation, particularly the importance of concentrated poverty in neighborhoods, influence Black–White disparities in hypertension prevalence in older adults.
Partitioning racial status by individual and neighborhood poverty did not fully explain the disparity in hypertension prevalence between Black and White older adults. It is possible that unmeasured social factors that are associated with neighborhood poverty, such as lack of access to grocery store and health care facilities, contribute to the unaccounted racial differences in hypertension prevalence in Black and White older adults. Our race–poverty–place measure addresses the presence of neighborhood poverty but does not capture the experience associated with living in an area of poverty, such as stress and discrimination. Nevertheless, by extending the assessment of racial differences in hypertension prevalence to the neighborhood level, we believe that we were able to obtain a clearer picture of how race and poverty influence hypertension prevalence in Black and White older adults. Further research is necessary to identify the social factors that can account for the racial disparity of hypertension prevalence.
Policies that seek to reduce hypertension prevalence in older adults should consider not only individual-level interventions but also neighborhood-level interventions, particularly measures that seek to reduce levels of neighborhood poverty. However, based on the results, effective neighborhood interventions may have different implications for Black and White older adults. White older adults seem to benefit more from interventions on individual and neighborhood poverty compared with Black older adults, particularly because Black older adults have significantly higher odds of hypertension regardless of individual and neighborhood poverty. We would expect interventions on neighborhood poverty, such as increasing access to fresh foods and health care facilities, to affect poor Whites more than Blacks. Nevertheless, such policies may be beneficial for Black older adults as well. Interventions on neighborhood poverty such as increasing the minimum wage or promoting the development of businesses in poorer areas could also impact individual poverty levels, which may further help reduce the disparity. Not only do the results encourage officials to intervene on the economic conditions of neighborhoods, but it also emphasizes particular neighborhoods that have a more pressing need for health promoting strategies to remain vigilant in efforts to decrease hypertension prevalence, such as poor neighborhoods for poor White older adults and predominantly Black, White, and integrated neighborhoods for Black older adults. Placing existing interventions used to combat hypertension in these key areas may produce more beneficial results in decreasing hypertension prevalence, and thereby reducing the existing disparity. Policymakers should collaborate with key stakeholders in the community to determine and implement the appropriate interventions to reduce disparities in hypertension prevalence among community-dwelling older adults.
The appropriate interventions should not only consider neighborhood-level and individual-level effects on poverty but should also be geared toward older adults to attenuate existing disparities in hypertension prevalence between Black and White older adults. Examples of potentially effective neighborhood-level interventions include the building of senior citizen centers in communities, emphasizing deterrents of criminal activity against older adults, and the creation or modification of transportation systems to facilitate older adults’ access to grocery stores, health care facilities, and places of employment. Likewise, examples of potentially effective individual-level interventions include the implementation of training programs to assist older adults in re-entering or continuing in the workforce as well as increased emphasis on supporting older adults in the workplace, such as the creation of work programs for older adults. It is imperative that the specific needs of older adults, such as accessibility, be considered in creating policies to combat the disparity of hypertension prevalence.
Acknowledgments
Funding The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Epidemiology and Biostatistics of Aging training grant from the National Institute on Aging of the National Institutes of Health (Grant T32AG000247), the National Center on Minority Health and Health Disparities (NCMHD) of National Institutes of Health (Grant P60MD000214), and the National Heart, Lung, and Blood Institute (Grant 5R01HL092846-02).
Biographies
Therri Usher is a fifth-year doctoral student in the Department of Biostatistics in the Johns Hopkins Bloomberg School of Public Health (JHSPH) and a teaching fellow for the undergraduate Public Health Studies program. Her research interests include racial and socioeconomic health disparities in older adults as well as creating methods for mediation analysis applicable to the study of health disparities.
Darrell J. Gaskin is an associate professor in the Department of Health Policy and Management in JHSPH and deputy director of the Hopkins Center for Health Disparities Solutions (HCHDS). His research areas include health care disparities, safety net hospitals, and the study and improvement of health care access for vulnerable populations. He has experience investigating the relationship between “place” and health disparities.
Kelly Bower is an assistant professor in the Department of Community-Public Health in the Johns Hopkins School of Nursing and a faculty member in HCHDS. Her areas of scholarly expertise and interest include health disparities, health literacy, residential segregation, food store availability, obesity, fetal and infant mortality, and substance abuse.
Charles Rohde is a professor and former chair of the Department of Biostatistics at JHSPH and an affiliated faculty member in HCHDS. His research areas include statistical methods based on marginal, conditional, and profile likelihoods for determining evidence and investigating the role of interactions in generalized linear models within various contexts.
Roland J. Thorpe Jr. is an assistant professor in the Department of Health, Behavior, and Society at JHSPH, director of the Research on Men’s Health program in HCHDS, chair of the Gerontological Society of America’s Task Force on Minority Issues in Gerontology, and sits on the Advisory Committee on Minority Health at the U.S. Department of Health and Human Services.
Footnotes
Declaration of Conflicting Interests The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Curtin LR, Mohadjer L, Dohrmann S, Montaquila JM, Kruszon-Moran D, Mirel LB, Johnson CL. The National Health and Nutrition Examination Survey: Sample design, 1999–2006. National Center for Health Statistics. Vital and Health Statistics. 2012;2(155) [PubMed] [Google Scholar]
- Delgado J, Jacobs EA, Lackland DT, Evans DA, de Leon CFM. Differences in blood pressure control in a large population-based sample of older African Americans and non-Hispanic Whites. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences. 2012;67:1253–1258. doi: 10.1093/gerona/gls106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez Roux AV, Mair C. Neighborhoods and health. Annals of the New York Academy of Sciences. 2010;1186:125–145. doi: 10.1111/j.1749-6632.2009.05333.x. [DOI] [PubMed] [Google Scholar]
- Gaskin DJ, Thorpe RJ, Jr, McGinty EE, Bower K, Rohde C, Young JH, Dubay L. Disparities in diabetes: The nexus of race, poverty, and place. American Journal of Public Health. 2014;104:2147–2155. doi: 10.2105/AJPH.2013.301420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillespie CD, Hurvitz KA. Prevalence of hypertension and controlled hypertension—United States, 2007–2010. Atlanta, GA: Centers for Disease Control and Prevention; 2013. (Morbidity and Mortality Weekly Report) [PubMed] [Google Scholar]
- Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, Stroke SS. Heart disease and stroke statistics—2013 update: A report from the American Heart Association. Circulation. 2013;127:e6–e245. doi: 10.1161/CIR.0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kershaw KN, Diez Roux AV, Burgard SA, Lisabeth LD, Mujahid MS, Schulz AJ. Metropolitan-level racial residential segregation and black-white disparities in hypertension. American Journal of Epidemiology. 2011;174:537–545. doi: 10.1093/aje/kwr116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer MR, Hogue CR. Is segregation bad for your health? Epidemiologic Reviews. 2009;31:178–194. doi: 10.1093/epirev/mxp001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N, Chen JT, Waterman PD, Rehkopf DH, Subramanian SV. Painting a truer picture of US socioeconomic and racial/ethnic health inequalities: The Public Health Disparities Geocoding Project. American Journal of Public Health. 2005;95:312–323. doi: 10.2105/AJPH.2003.032482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landrine H, Corral I. Separate and unequal: Residential segregation and black health disparities. Ethnicity & Disease. 2009;19:179–184. [PubMed] [Google Scholar]
- LaVeist TA, Thorpe RJ, Mance GA, Jackson J, William C, Richardson NF. Overcoming confounding of race with socio-economic status and segregation to explore race disparities in smoking. Addiction. 2007;102:65–70. doi: 10.1111/j.1360-0443.2007.01956.x. [DOI] [PubMed] [Google Scholar]
- Morenoff JD, House JS, Hansen BB, Williams DR, Kaplan GA, Hunte HE. Understanding social disparities in hypertension prevalence, awareness, treatment, and control: The role of neighborhood context. Social Science & Medicine. 2007;65:1853–1866. doi: 10.1016/j.socscimed.2007.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Health Statistics. Examination components. Hyattsville, MD: 2003–2004. Retrieved from http://www.cdc.gov/nchs/data/nhanes/meccomp.pdf. [Google Scholar]
- National Center for Health Statistics. National Health and Nutrition Examination Survey data. Hyattsville, MD: 2004. Retrieved from http://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm. [Google Scholar]
- National Center for Health Statistics. Healthy people 2010: Final review. Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2012. [Google Scholar]
- National Prevention Council. National prevention strategy. Washington, DC: U.S. Department of Health and Human Services, Office of the Surgeon General; 2011. [Google Scholar]
- Nwankwo T, Yoon SS, Burt V, Gu Q. Hypertension among adults in the US: National Health and Nutrition Examination Survey, 2011–2012. Hyattsville, MD: National Center for Health Statistics, Centers for Disease Control and Prevention, United States Department of Health and Human Services; 2013. (NCHS Data Brief, No. 133) [Google Scholar]
- StataCorp. Stata statistical software: Release 13 [Computer software] College Station, TX: StataCorp LP; 2013. [Google Scholar]
- Svetkey LP, George LK, Burchett BM, Morgan PA, Blazer DG. Black/white differences in hypertension in the elderly: An epidemiologic analysis in central North Carolina. American Journal of Epidemiology. 1993;137:64–73. doi: 10.1093/oxfordjournals.aje.a116603. [DOI] [PubMed] [Google Scholar]
- Thorpe RJ, Bowie JV, Smolen JR, Bell CN, Jenkins ML, Jackson J, LaVeist TA. Racial disparities in hypertension awareness and management: Are there differences among African Americans and Whites living under similar social conditions? Ethnicity & Disease. 2014;24:269–275. [PMC free article] [PubMed] [Google Scholar]
- Thorpe RJ, Brandon DT, LaVeist TA. Social context as an explanation for race disparities in hypertension: Findings from the Exploring Health Disparities in Integrated Communities (EHDIC) Study. Social Science & Medicine. 2008;67:1604–1611. doi: 10.1016/j.socscimed.2008.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorpe RJ, Koster A, Bosma H, Harris TB, Simonsick EM, van Eijk JTM, Kritchevsky SB. Racial differences in mortality in older adults: Factors beyond socioeconomic status. Annals of Behavioral Medicine. 2012;43:29–38. doi: 10.1007/s12160-011-9335-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Census Bureau. Census 2000 summary file 1. Suitland, MD: 2001. Retrieved from http://www.census.gov/prod/cen2000/doc/sf1.pdf. [Google Scholar]
- Williams DR, Collins C. Racial residential segregation: A fundamental cause of racial disparities in health. Public Health Reports. 2001;116:404–416. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]