Abstract
Introduction
Offering HPV vaccine in settings beyond the traditional medical home holds promise for increasing the currently low levels of coverage. As adolescents frequently visit dentists, dental practices may be one such alternative vaccination setting. This study assessed parent attitudes about the roles dental providers could play in HPV prevention, including vaccine provision.
Methods
In September 2016, we conducted an online survey using a national sample (n=1,209) of U.S. parents of adolescent children aged 11–17. Adolescents’ mean age was 14; 53% were male and 62% were non-Hispanic white. We identified correlates of parents’ comfort with dentists as HPV vaccinators using multivariable logistic regression.
Results
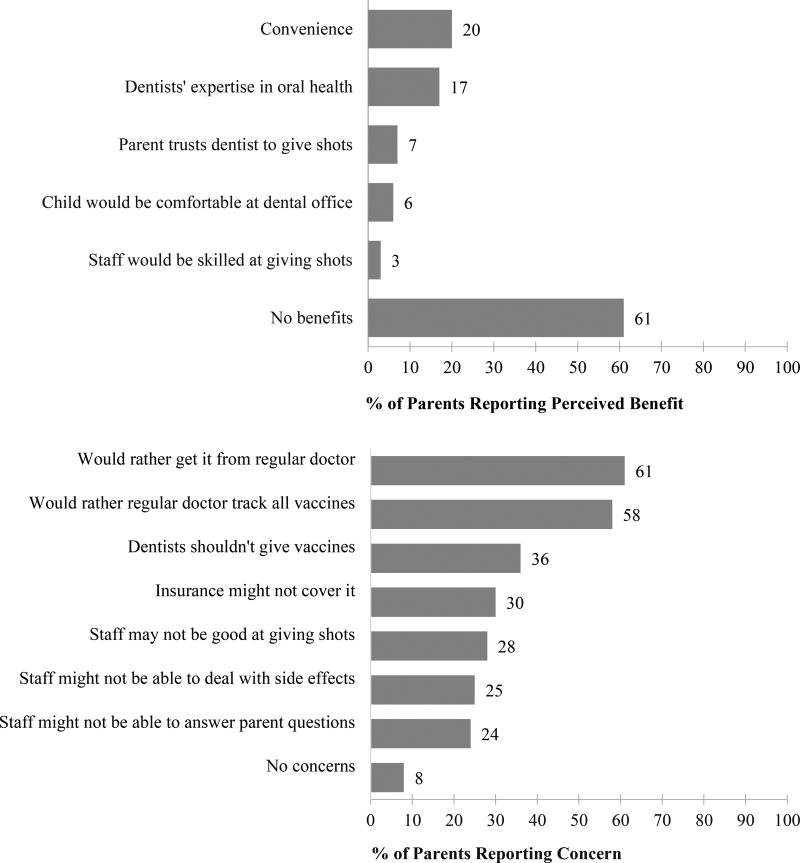
Overall, 23% of parents reported that they would feel comfortable with their child receiving HPV vaccine from a dentist. In multivariable analyses, parents had greater odds of being comfortable if they perceived 2 or more benefits of dentists providing HPV vaccinations (OR=6.82, 95% CI:4.44–10.47) or had higher trust in their child’s primary care provider (OR=1.46, 95% CI:1.06–1.83). Parents had lower odds of comfort if their child was female (OR=0.68, 95% CI:0.51–0.89) or if they had 2 of more concerns (OR=0.12, 95% CI: 0.07–0.19). Convenience (20%) and oral health expertise (20%) were the most commonly cited benefits of dentists administering the vaccine. Wanting their child’s regular provider to administer and track vaccinations (61% and 58%, respectively), and lack of insurance coverage (30%) were the most commonly cited concerns. Parents expressed somewhat greater comfort with roles dentists might play in promoting HPV vaccination other than vaccine delivery, such as providing education.
Conclusions
Parents in this sample had low comfort with dentists as HPV vaccinators. Findings from this study highlight concerns to be addressed before dental consider offering HPV vaccination in the future. Further research should assess dentists’ perspectives and explore alternative roles for dental providers in HPV prevention efforts.
1. Introduction
Though human papillomavirus (HPV) vaccine has been available since 2006, coverage for adolescents in the U.S. remains low, with only 30% of boys and 40% of girls having completed the series by age 17 [1]. Parental hesitancy towards HPV vaccination is one reason for low uptake in adolescent populations, with many parents choosing initially to refuse or delay HPV vaccination, reporting that they do not know enough about it, and having concerns about its safety or effectiveness [2–4]. As with other vaccinations, additional barriers include low levels of preventive medical care among adolescents and missed opportunities for provider recommendation during existing clinical encounters [5–10]. As a multi-dose series, these barriers may be heightened for HPV vaccination [8,11]. Given these challenges, improving vaccination coverage to prevent HPV-associated cancers of the head, neck, and genital tract may require significant systems-level change.
Most adolescents receive vaccines at their primary care provider’s office, but offering vaccination in alternative settings beyond the medical home has potential for increasing coverage, particularly for follow-up doses of the vaccine [12,13]. Currently, primary care providers deliver a wide range of preventive services to adolescents, including HPV vaccination and counseling, posing serious challenges given resource and time constraints on the provider and patient sides [14]. In response to these challenges, school-based clinics and pharmacies have emerged as promising alternative settings to promote and administer HPV vaccine [15,16]. In addition, the potential for dentists to use their offices as a setting for HPV vaccination and education has gained attention among dental professionals and public health researchers [14,17,18]. Dentists have grown increasingly interested in improving population health through preventive oral care, and many dentists already perform and receive reimbursement for oral cancer screenings [17,19].
Because HPV vaccination is recommended for pre-teens and young adolescents and parents are the primary decision-makers for their children’s health care, parental acceptability of both the vaccine and delivery approach, are critical [1,20]. No currently available evidence demonstrates whether parents would support administration of HPV vaccine in dentists’ offices, or dentists providing education on HPV or HPV vaccine. Thus, we sought to: (1) explore parents’ comfort with dentists in HPV prevention roles, (2) identify factors correlated with high acceptability of dentists administering HPV vaccinations, and (3) assess parents’ perceived benefits and concerns with this approach.
2. Methods
2.1 Participants and Procedures
We conducted an online survey administered to a national sample of parents of adolescents ages 11–17 in September 2016. Survey respondents were members of a standing panel of U.S. adults maintained by GfK, a survey research company [21]. Participants were recruited through list-assisted addressed based sampling with phone call follow-ups for non-responsive households [21]. Respondents received points exchangeable for small cash payments from the company as an incentive for completing surveys. Harvard Pilgrim Health Care Institute’s Institutional Review Board (IRB) approved the original study’s protocol. The University of Minnesota IRB determined this secondary analysis exempt from review. Of the 2580 panelists invited to complete the eligibility screening survey, a total of 1253 met the inclusion criteria and completed the survey (response rate = 59% based on the American Association of Public Opinion Research formula 4) [22]. The present analysis excluded 44 respondents with missing data, resulting in a final analytic sample size of 1209 parents.
2.2 Measures
Throughout the survey, parents were asked to answer questions about their 11–17 year old child; parents with multiple children in the age range were asked to answer about the child with the most recent birthday. The survey provided parents with information about oral HPV and dentists as vaccinators before items about dentists’ HPV prevention roles: “Some types of HPV can cause mouth and throat cancer. The HPV vaccine can protect against some of these types,” and “In some states, dentists who have completed special training are allowed to give vaccines.”
A single item assessed parent comfort with dentists as HPV vac cinators: “Imagine you and your [son/daughter] decided to get [him/her] the HPV vaccine, how comfortable would you be with [child’s name] getting the HPV vaccine from a dentist?” Four survey questions assessed parents’ comfort with dentists taking on other HPV prevention roles including: providing written information about HPV vaccine, talking to parents about HPV vaccine, talking to children about HPV vaccine, and finally, recommending that children get the HPV vaccine from their regular doctor. Response options for all comfort variables used a 5-point scale ranging from “very uncomfortable” (1) to “very comfortable” (5). Consistent with the approach taken in other research [13], we dichotomized responses into “comfortable” (responses of “very comfortable” and “somewhat comfortable”) or “not comfortable” (responses of “very uncomfortable,” “somewhat uncomfortable,” and “neither uncomfortable nor comfortable”) for analyses.
The survey assessed parents’ perceived benefits and concerns with dentists administering HPV vaccinations with two parallel questions: “What [benefits/concerns] would you have with [child’s name] getting the HPV vaccine at the dentist’s office?” Parents selected all that apply from predefined lists developed based on existing literature about HPV vaccination and alternative vaccination settings [13,23,24]. Potential benefits included: convenience, trust in dentist to administer the vaccine, belief that dental office staff would have appropriate skills to administer the vaccine, child’s comfort at the dental office, and dental expertise in oral health. Potential concerns (or perceived drawbacks) included: that insurance might not cover the vaccine, that staff may not be good at giving shots, that staff might not be able to answer questions, that staff might not be able to deal with side effects, the belief that dentists should not give vaccines, preference for vaccine delivery by child’s regular care provider, and preference for regular provider to keep track of all of their child’s vaccines. Additionally, parents could also select “I would see no [benefits/concerns].”
Parents reported demographic information about themselves, their child, their household and their child’s access to health care services. Information about the parents included sex, race/ethnicity, education level, and their perceptions of the quality of their relationship with their child’s healthcare provider [25]. Information about the household included income and urbanicity (based on living within a metropolitan statistical area, as defined by the U.S. Census Bureau) [26]. Information about the child included sex, age, race/ethnicity and health care access and use including whether they had health insurance, a regular health provider and regular oral health care clinic, and their HPV vaccination status. For vaccination status, which reflects parents’ HPV vaccination intent and behavior, we combined two separate items assessing the number of doses of HPV vaccine the child had received and, for those who reported none, parent’s intent to vaccinate their child to create a three-level variable (not vaccinated and does not intend to vaccinate in next 12 months; not vaccinated but intends to vaccinate in next 12 months; and vaccinated).
2.3 Analyses
We first descriptively assessed parents’ comfort with potential HPV prevention roles. We then used bivariate logistic regression to identify correlates of comfort with dentists as HPV vaccinators, and entered all significant variables (p < .05) into a multivariable logistic regression model. We conducted all analyses using Stata software version 14.2 (Statacorp, College Station, TX). Significance testing used two-tailed tests and a critical α of 0.05, unless otherwise noted.
3. RESULTS
3.1 Sample Characteristics
Characteristics of the study sample are shown in Table 1. About half of parents were female and most had at least some college education or more. Parents reported similar proportions of children by sex. Most parents reported living in an urban area, over half had at least some college education, and over half reported household incomes about $75,000. Almost all children had health insurance coverage and very few had not visited a dental clinic for routine care within the last year.
Table 1.
Demographic characteristics of parents, their children, and their households
| n | (%) | |
|---|---|---|
| Parent characteristics | ||
| Sex | ||
| Male | 590 | (48.8) |
| Female | 619 | (51.2) |
| Educational attainment | ||
| ≤ High school degree | 479 | (39.6) |
| Some college, no degree | 316 | (26.1) |
| College degree or more | 414 | (34.2) |
| Child characteristics | ||
| Sex | ||
| Male | 636 | (52.6) |
| Female | 573 | (47.4) |
| Age, in years | ||
| 11–12 | 326 | (27.0) |
| 13–15 | 496 | (41.0) |
| 16–17 | 387 | (32.0) |
| Race/Ethnicity | ||
| White, non-Hispanic | 751 | (62.1) |
| Black, non-Hispanic | 102 | (8.4) |
| Hispanic | 251 | (20.8) |
| Other, non-Hispanicb | 105 | (8.7) |
| Household characteristics | ||
| Annual income | ||
| <$35,000 | 252 | (20.8) |
| $35,000–$74,999 | 335 | (27.7) |
| ≥$75,000 | 622 | (51.5) |
| Urbanicitya | ||
| Rural | 167 | (13.8) |
| Urban | 1042 | (86.1) |
| Healthcare-related characteristics | ||
| Child has health insurance coverage | ||
| No | 65 | (5.4) |
| Yesc | 1144 | (94.6) |
| HPV vaccination status | ||
| Not vaccinated, does not intend to vaccinate in next 12 months | 414 | (34.2) |
| Not vaccinated, intends to vaccinate in next 12 months | 522 | (43.2) |
| Vaccinatedd | 273 | (22.6) |
As determined by MSA status
Other race includes adolescents whose parents identified them as Asian, American Indian or Alaska Native, Native Hawaiian or Pacific Islander, more than one race, or none of these.
Child has either private or public health insurance coverage
Child has received at least 1 dose of HPV vaccine
3.2 Parent Comfort with Dentists in HPV Prevention Roles
About a quarter (23%) of parents reported that they would feel “very” or “somewhat” comfortable with their child receiving HPV vaccine from a dentist (together categorized as “comfortable”); about a quarter were “neither comfortable nor uncomfortable” (22%) and the remainder were either “somewhat” or “very” uncomfortable (55%; together categorized as “not comfortable”). A higher proportion of parents expressed comfort with dentists performing other, non-vaccinator HPV prevention roles. Parents expressed the greatest comfort with dentists providing written information about HPV (51%), with fewer expressing comfort with dentists speaking with them directly about HPV vaccine (48%), recommending that they seek HPV vaccination from their child’s regular care provider (46%), or speaking with their child about HPV vaccine (41%).
3.3 Correlates of Comfort with Dentists as HPV Vaccinators
Table 2 presents results of logistic regression models. In multi- variable analyses, parents had greater odds of being comfortable with a dentist administering HPV vaccine if: they had high (vs. low) quality relationships with their child’s primary care provider (OR = 1.27, 95% CI 0.96–1.68; they intended to get their child HPV vaccine in the next 12 months (OR = 2.02, 95% CI 1.44–2.83); of if their child had already received at least 1 dose of HPV vaccine (OR = 2.23, 95% CI 1.52–3.27). Parents of female children had lower odds of being comfortable than did parents of males (OR = 0.65, 95% CI 0.50–0.86).
Table 2.
Correlates of parents’ comfort with dentists administering HPV vaccinations to their adolescent children
| Comfortable (N=273) |
Not Comfortable (N=936) |
Bivariate | Multivariable | |||||
|---|---|---|---|---|---|---|---|---|
| n | (%) | n | % | OR | 95% CI | OR | 95% CI | |
| Parent characteristics | ||||||||
| Sex | ||||||||
| Male | 140 | (23.7) | 450 | (76.3) | Ref | --- | ||
| Female | 133 | (21.5) | 486 | (78.5) | 0.88 | (0.67–1.15) | --- | |
| Educational attainment | ||||||||
| High school degree or less | 108 | (22.6) | 371 | (77.5) | Ref | |||
| Some college, no degree | 61 | (19.3) | 255 | (80.7) | 0.82 | (0.58–1.17) | --- | |
| College degree or more | 104 | (25.1) | 310 | (74.9) | 1.15 | (0.85–1.57) | --- | |
| Child characteristics | ||||||||
| Sex | ||||||||
| Male | 164 | (25.8) | 472 | (74.2) | Ref | Ref | ||
| Female | 109 | (19.0) | 464 | (81.0) | 0.68 | (0.51–0.89)** | 0.65 | (0.50–0.86)** |
| Age, in years | ||||||||
| 11–12 | 66 | (20.3) | 260 | (79.8) | Ref | --- | ||
| 13–15 | 118 | (23.8) | 378 | (76.2) | 1.23 | (0.88–1.73) | --- | |
| 16–17 | 89 | (23.0) | 298 | (77.0) | 0.89 | (0.82 –1.69) | --- | |
| Race/Ethnicity | ||||||||
| White, non-Hispanic | 164 | (21.8) | 587 | (78.2) | Ref | --- | ||
| Black, non-Hispanic | 21 | (20.6) | 81 | (79.4) | 0.93 | (0.56–1.55) | --- | |
| Hispanic | 61 | (24.3) | 190 | (75.7) | 1.15 | (0.82–1.61) | --- | |
| Other, non-Hispanica | 27 | (25.7) | 78 | (74.3) | 1.24 | (0.77–1.98) | --- | |
| Household characteristics | ||||||||
| Annual income | ||||||||
| <$35,000 | 57 | (22.6) | 195 | (77.4) | Ref | |||
| $35,000–$74,999 | 67 | (20.0) | 268 | (80.0) | 0.86 | (0.57–1.27) | --- | |
| ≥$75,000 | 149 | (24.0) | 473 | (76.1) | 1.08 | (0.76–1.53) | --- | |
| Urbanicityb | ||||||||
| Rural | 45 | (27.0) | 122 | (73.1) | Ref | --- | ||
| Urban | 228 | (21.9) | 814 | (78.1) | 0.76 | (0.52–1.10) | --- | |
| Healthcare-related characteristics | ||||||||
| Child has health insurance coverage | ||||||||
| No | 11 | (16.9) | 54 | (83.1) | Ref | |||
| Yes | 262 | (22.9) | 882 | (77.1) | 1.45 | (0.75–2.83) | ||
| Parent-provider relationship qualityc | ||||||||
| Low | 121 | (19.71) | 493 | (80.3) | Ref | Ref | ||
| High | 152 | (25.6) | 443 | (74.5) | 1.40 | (1.07–1.83)* | 1.27 | (0.96–1.68) |
| Adolescent has regular dental clinic | ||||||||
| No | 18 | (25.7) | 52 | (74.3) | Ref | --- | ||
| Yes | 255 | (22.4) | 884 | (77.6) | 0.83 | (0.48–1.45) | --- | |
| Number of times/year adolescent visits dental clinic for routine work | ||||||||
| none | 17 | (21.8) | 61 | (78.2) | Ref | --- | ||
| 1 | 72 | (21.9) | 257 | (78.1) | 1.01 | (0.55–1.83) | --- | |
| ≥2 | 184 | (22.9) | 618 | (77.1) | 1.07 | (0.61–1.87) | --- | |
| HPV vaccination status | ||||||||
| Not vaccinated, does not intend to vaccinate in next 12 months | 61 | (14.7) | 353 | (85.3) | Ref | Ref | ||
| Not vaccinated, intends to vaccinate in next 12 months | 136 | (26.1) | 386 | (74.0) | 2.04 | (1.46–2.85)*** | 2.02 | (1.44–2.83)*** |
| Vaccinatedd | 76 | (27.8) | 197 | (72.2) | 2.23 | (1.53–3.26)*** | 2.23 | (1.52–3.27)*** |
Note. Percentages may not total 100 due to rounding. OR: odds ratio. CI: confidence interval. Dashes (---) indicate the variable was not included in the multivariable model because it was not associated at p<.05 in bivariate analyses.
Other race includes adolescents whose parents identified them as Asian, American Indian or Alaska Native, Native Hawaiian or Pacific Islander, more than one race, or none of these.
As determined by MSA status
Based on mean of 4 items assessing: overall satisfaction, having information needs met, spending enough time, and following a provider’s advice (α=.81)
Child has received at least 1 dose of HPV vaccine
p<.05
p<.01
p<001
3.4 Perceived Benefits and Concerns
Fig. 1 presents parents’ perceived benefits and concerns with dentists administering HPV vaccine. Over half of parents (61%) indicated that they saw no benefits to this approach. The most frequently endorsed benefits were convenience (20%) and dentists’ expertise in oral health care (17%). Fewer than one in ten parents endorsed any of the remaining benefits. In contrast, only 8% of parents reported that they had no concerns. Almost two-thirds of parents indicated that they would want their child’s regular provider to administer their HPV vaccines (61%), or that they wanted their child’s primary care provider to keep track of all their child’s vaccinations (58%). Over one in four parents reported having each of the remaining concerns, which included the belief that dentists should not administer vaccines, insurance might not cover vaccine, and staff “may not be good at giving shots.”
Figure 1.
Parents’ perceived benefits and concerns with dentists as HPV vaccinators
4. Discussion
4.1 Findings
HPV vaccine administration in alternative settings has the potential to increase low vaccination coverage among adolescents in the U.S. Dental practices are regularly accessed by most adolescents, yet, to our knowledge, this is the first study to examine parents’ perceptions of dentists as HPV vaccinators. In this sample, we found that only one quarter of parents would feel comfortable with dentists administering HPV vaccine to their adolescent children. Comfort was somewhat greater among parents whose children had already received HPV vaccine and among those who intend to have their children vaccinated than among those who did not intend to vaccinate in the next 12 months. Previous research using similar methods has found greater levels of parental acceptability with other potential alternative vaccination settings such as schools and pharmacies [13,15]. Since few dental practices currently administer any type of vaccines, this difference may reflect parents’ greater familiarity with other alternative settings that currently offer vaccines. Despite their low levels of comfort with dentists as vaccinators, parents reported somewhat higher levels of comfort with dentists in other HPV prevention roles including providing written information about vaccination or talking to parents about HPV. Parents with male children were more likely to report higher comfort with their child receiving HPV, findings that parallel a 2013 study exploring parent comfort with HPV vaccine in other alternative settings [13]. This difference may be due in part to patterns of parental concerns about HPV vaccination which vary by adolescents’ sex. For example, recent research finds that fewer parents of boys (vs. girls) report concerns about side effects, which may translate into greater comfort with vaccination in an alternative setting [27]. These findings, along with those regarding parents’ perceived concerns and benefits highlight potential areas for future research and intervention.
Many parents reported concerns, including the belief that staff may not be good at giving shots, that insurance may not cover vaccination, and that staff may not be able to deal with side effects. In previous studies exploring oral health care providers’ capacity to participate in HPV vaccination or education delivery, focus group participants including dentists and dental hygienists identified many of these concerns as barriers they would need to address before their workplaces could take on additional HPV prevention roles [17]. Though over half of parents reported that they would see no benefits with getting their child vaccinated at a dentist’s office, parents who selected at least one benefit most often cited the potential convenience and dentists’ expertise in oral health. Both benefits support delivering valuable HPV education to parents and adolescents in dental office settings. Current best practice guidelines encourage primary care providers to present HPV vaccination as a routine intervention designed to prevent cancer, bundling it with other adolescent vaccines with historically higher uptake, and addressing parent questions and concerns as needed [28]. When parents are exposed to more recommendations from trusted health experts to get their child HPV vaccine, they may be more likely to follow through with vaccination [5]. Dentists could be valuable allies to adolescents’ regular care providers since they may interact with adolescent patients and parents more regularly and can reinforce HPV vaccination recommendations.
For dental practices to become viable alternative setting for HPV vaccination, significant changes to existing infrastructure and policy would be needed. For example, only some states, including Minnesota and Illinois, currently allow specially trained dentists to vaccines at all [29,30]. If allowed to administer vaccines, dental offices would need to be equipped for legal and safe refrigerated vaccine storage for vaccination to be feasible [15]. Additionally, private insurers would need to reimburse a new category of providers for time spent educating or vaccinating patients, and government payers such as the Vaccines for Children (VFC) program, would need to allow dentist reimbursement. Dental practices would also need to be able to access and use state immunization registry systems and the Vaccine Adverse Effects Reporting System (if their patients suffered any side-effects from HPV vaccine) [31]. Participation in these systems is necessary to facilitate effective care coordination and reporting but could require an additional investment in time and training.
4.2 Strengths and Limitations
This study offers novel information about parent attitudes towards dentists in HPV vaccination and other HPV-prevention roles and is strengthened by a large sample. Limitations include a cross- sectional design and parent report. Although our sample was drawn from a national panel that is similar to the U.S. population on many demographic characteristics, as with other survey research, our findings may not be generalizable to parents who opted not to participate [21]. While parents are the primary decision-makers regarding HPV vaccination as children age, young people become increasingly involved in these decisions [31]. Thus, future research should investigate the attitudes of preteens and adolescents themselves. Further, survey questions asked parents to consider a hypothetical situation where they had already decided for their child to get vaccinated, which means responses may not reflect their actual comfort or behavior if faced with a real opportunity to have their child vaccinated by a dentist. Despite the hypothetical scenario, it is also possible that our findings reflect parents’ attitudes towards HPV vaccine, at least in part, rather than solely their comfort with dental practices as an alternative setting. Additionally, the survey did not include some variables that may influence parental attitudes towards HPV vaccination and dentists as vaccinators. For example, families with limited access to their child’s physician or who have accessed health care in setting outside the traditional medical home (e.g., school-based clinics, pharmacies) may have more interest in receiving vaccines in an oral health care setting.
4.3 Conclusions
Our findings in this study exploring parent comfort with dentists as HPV vaccinators suggest that a focus on non-vaccination HPV prevention and education roles in the alternative setting of dental practices may be most fruitful. Future research should more thoroughly assess dentists’ readiness to deliver effective HPV counseling or education and establish whether this practice would make a meaningful difference in adolescent HPV vaccination rates. Establishing a solid evidence base before changing preventive health care delivery policies and practices could facilitate greater acceptance among parents, and more efficient implementation by providers. Improving adolescent HPV vaccination coverage remains an important public health goal. Whether through partnering with oral health providers for educational or communication-focused interventions, or through administering HPV vaccine through dental practices, the use of dental offices as alternative settings to promote adolescent HPV vaccination merits further investigation.
Highlights.
This study assessed parents’ comfort with dental providers in HPV prevention roles
Only one-quarter of parents were comfortable with dentists administering HPV vaccine
More parents were comfortable with dentists in non-vaccination roles
Acknowledgments
The authors thank Drs. Rachael Hardeman and Sarah Gollust for their feedback on this project.
Funding: This work was supported by the National Cancer Institute (K22 CA186979) and the Maternal and Child Health Bureau (T71MC00025). The funders played no role in the design and conduct of the study; collection, management, analysis, and interpretation of data; preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication.
Footnotes
Conflict of Interest: None.
References
- 1.Meites E, Kempe A, Markowitz LE. Use of a 2-dose schedule for human papillomavirus vaccination—updated recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Morb and Mortal Wkly Rep. 2016;65:1405–8. doi: 10.15585/mmwr.mm6549a5. https://doi.org/10.15585/mmwr.mm6549a5. [DOI] [PubMed] [Google Scholar]
- 2.Thompson EL, Rosen BL, Vamos CA, Kadono M, Daley EM. Human papillomavirus vaccination: what are the reasons for nonvaccination among U.S. adolescents? J Adolesc Health. 2017;61(3):288–93. doi: 10.1016/j.jadohealth.2017.05.015. https://doi.org/10.1016/j.jadohealth.2017.05.015. [DOI] [PubMed] [Google Scholar]
- 3.Darden PM, Thompson DM, Roberts JR, Hale JJ, Pope C, Naifeh M, Jacobson RM. Reasons for not vaccinating adolescents: National Immunization Survey of Teens, 2008–2010. Pediatrics. 2013;131(4):645–51. doi: 10.1542/peds.2012-2384. https://doi.org/10.1542/peds.2012-2384. [DOI] [PubMed] [Google Scholar]
- 4.Gilkey MB, Calo WA, Marciniak MW, Brewer NT. Parents who refuse or delay HPV vaccine: differences in vaccination behavior, beliefs, and clinical communication preferences. Hum Vaccin Immunother. 2017;13(3):680–6. doi: 10.1080/21645515.2016.1247134. https://doi.org/10.1080/21645515.2016.1247134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zimet GD, Rosberger Z, Fisher WA, Perez S, Stupiansky NW. Beliefs, behaviors and HPV vaccine: correcting the myths and the misinformation. Prev Med. 2013;57:414–8. doi: 10.1016/j.ypmed.2013.05.013. https://doi.org/10.1016/j.ypmed.2013.05.013. [DOI] [PubMed] [Google Scholar]
- 6.Jemal A, Simard EP, Dorell C, Noone AM, Markowitz LE, Kohler B, et al. Annual report to the nation on the status of cancer, 1975–2009, featuring the burden and trends in human papillomavirus(HPV)-associated cancers and HPV vaccination coverage levels. J Natl Cancer Inst. 2013;105:175–201. doi: 10.1093/jnci/djs491. https://doi.org/10.1093/jnci/djs491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gilkey MB, Malo TL, Shah PD, Hall ME, Brewer NT. Quality of physician communication about human papillomavirus vaccine: findings from a national survey. Cancer Epidemiol Biomark Prev. 2015;24:1–8. doi: 10.1158/1055-9965.EPI-15-0326. https://doi.org/10.1158/1055-9965.EPI-15-0326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gilkey MB, Calo WA, Moss JL, Shah PD, Marciniak MW, Brewer NT. Provider communication and HPV vaccination: the impact of recommendation quality. Vaccine. 2016;34:1187–92. doi: 10.1016/j.vaccine.2016.01.023. https://doi.org/10.1016/j.vaccine.2016.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ylitalo KR, Lee H, Mehta NK. Health care provider recommendation, human papillomavirus vaccination, and race/ethnicity in the US National Immunization Survey. Am J Public Health. 2013;103:164–9. doi: 10.2105/AJPH.2011.300600. https://doi.org/10.2105/AJPH.2011.300600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nordin JD, Solberg LI, Parker ED. Adolescent primary care visit patterns. Ann Fam Med. 2010;8:511–6. doi: 10.1370/afm.1188. https://doi.org/10.1370/afm.1188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Holman DM, Benard V, Roland KB, Watson M, Liddon N, Stokley S. Barriers to human papillomavirus vaccination among US adolescents: a systematic review of the literature. JAMA Pediatr. 2014;168:76. doi: 10.1001/jamapediatrics.2013.2752. https://doi.org/10.1001/jamapediatrics.2013.2752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Middleman AB, Tung JS. At what sites are parents willing to have their 11 through 14-year-old adolescents immunized? Vaccine. 2010;28:2674–8. doi: 10.1016/j.vaccine.2010.01.006. https://doi.org/10.1016/j.vaccine.2010.01.006. [DOI] [PubMed] [Google Scholar]
- 13.McRee AL, Reiter PL, Pepper JK, Brewer NT. Correlates of comfort with alternative settings for HPV vaccine delivery. Hum Vaccin Immunother. 2013;9:306–13. doi: 10.4161/hv.22614. https://doi.org/10.4161/hv.22614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shepperd JA, Howell JL, Catalanotto F, Dodd VJ, Logan HL. The decision to counsel adolescents about HPV. Am J Health Behav. 2013;37:755–62. doi: 10.5993/AJHB.37.6.4. https://doi.org/10.5993/AJHB.37.6.4. [DOI] [PubMed] [Google Scholar]
- 15.Shah PD, Gilkey MB, Pepper JK, Gottlieb SL, Brewer NT. Promising alternative settings for HPV vaccination of US adolescents. Expert Rev Vaccin. 2014;13:235–46. doi: 10.1586/14760584.2013.871204. https://doi.org/10.1586/14760584.2013.871204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Calo WA, Gilkey MB, Shah P, Marciniak Macary W, Brewer NT. Parents’ willingness to get human papillomavirus vaccination for their adolescent children at a pharmacy. Prev Med. 2017;99:251–6. doi: 10.1016/j.ypmed.2017.02.003. https://doi.org/10.1016/j.ypmed.2017.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Daley E, Dodd V, DeBate R, Vamos C, Wheldon C, Kline N, et al. Prevention of HPV-related oral cancer: assessing dentists’ readiness. Public Health. 2014;128:231–8. doi: 10.1016/j.puhe.2013.12.002. https://doi.org/10.1016/j.puhe.2013.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Daley E, Debate R, Dodd V, Dyer K, Fuhrmann H, Helmy H, et al. Exploring awareness, attitudes, and perceived role among oral health providers regarding HPV-related oral cancers. J Public Health Dent. 2011;71:136–42. doi: 10.1111/j.1752-7325.2011.00212.x. https://doi.org/10.1111/j.1752-7325.2011.00212.x. [DOI] [PubMed] [Google Scholar]
- 19.Rutkoski H, Fowler B, Mooney R, Pappas L, Dixon BL, Pinzon LM, et al. Pilot test of survey to assess dental and dental hygiene student human papillomavirus-related oropharyngeal cancer knowledge, perceptions, and clinical practices. J Cancer Educ. 2017:1–8. doi: 10.1007/s13187-017-1165-z. https://doi.org/10.1007/s13187-017-1165-z. [DOI] [PubMed]
- 20.McRee AL, Reiter PL, Brewer NT. Vaccinating adolescent girls against human papillomavirus—who decides? Prev Med. 2010;50:213–4. doi: 10.1016/j.ypmed.2010.02.001. https://doi.org/10.1016/j.ypmed.2010.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.GfK. KnowledgePanel design summary. [accessed 4.27.17];KnowledgePanel overview. 2016 Available from: http://www.knowledgenetworks.com/ganp/docs/KnowledgePanel(R)-Design-Summary.pdf.
- 22.The American Association for Public Opinion Research. Standard definitions: final dispositions of case codes and outcome rates for surveys. [accessed 7.20.17];2016 :9. Available from: http://www.aapor.org/Standards-Ethics/Standard-Definitions-(1).aspx.
- 23.Crosignani P, De Stefani A, Fara GM, Isidori AM, Lenzi A, Liverani CA, et al. Towards the eradication of HPV infection through universal specific vaccination. BMC Public Health. 2013;13:642. doi: 10.1186/1471-2458-13-642. https://doi.org/10.1186/1471-2458-13-642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Perkins RB, Clark JA. Providers’ perceptions of parental concerns about HPV vaccination. J Health Care Poor Underserved. 2012;24:828–39. doi: 10.1353/hpu.2013.0080. https://doi.org/10.1353/hpu.2013.0080. [DOI] [PubMed] [Google Scholar]
- 25.Saha S, Arbelaez JJ, Cooper LA. Patient-physician relationships and racial disparities in the quality of health care. Am J Public Health. 2003;93:1713–9. doi: 10.2105/ajph.93.10.1713. https://doi.org/10.2105/AJPH.93.10.1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.United States Census Bureau. Metropolitan and micropolitan – guidance for data users. [accessed 4.29.17];2016 Available from: https://www.census.gov/programs-surveys/metro-micro/guidance.html.
- 27.Lindley MC, Jeyarajah J, Yankey D, Curtis CR, Markowitz LE, Stokley S. Comparing human papillomavirus knowledge and intentions among parents of boys and girls. Hum Vaccin Immunother. 2016;12 doi: 10.1080/21645515.2016.1157673. https://doi.org/10.1080/21645515.2016.1157673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bernstein HH, Bocchini JA. The need to optimize adolescent immunization. Pediatrics. 2017;139:e1–e15. doi: 10.1542/peds.2016-4186. https://doi.org/10.1542/peds.2016-4186. [DOI] [PubMed] [Google Scholar]
- 29.Office of the Revisor of Statutes – State of Minnesota. 150A.055-2016 Minnesota Statutes. [accessed 7.11.17];2016 Available from: https://www.revisor.mn.gov/statutes/?id=150A.055.
- 30.Illinois General Assembly. [accessed 7.11.17];2014 Public Act 098-0665; Available from: http://www.ilga.gov/legislation/publicacts/fulltext.asp?Name=0980665.
- 31.Centers for Disease Control and Prevention. Vaccine adverse event reporting system. VAERS website. [accessed 5.8.17];2017 Available from: https://vaers.hhs.gov/index.