Abstract
Background:
The present study was designed to evaluate the effectiveness of magnesium sulfate (MgSO4) in procedural sedation and analgesia (PSA) when combined with ketamine in patients with fractures in emergency departments and required short and painful emergency procedures.
Materials and Methods:
In this study, 100 patients with fractures and dislocations who were presented to the emergency departments and required PSA for short and painful emergency procedures were randomly allocated to groups of ketamine plus MgSO4 or ketamine alone. Train of four (TOF) stimulation pattern was assessed using nerve stimulator machine and compared between groups.
Results:
The mean age of studied patients was 46.9 ± 9.3 years old. 48% were male and 52% were female. No significant differences were noted between groups in demographic variables. The status of TOF, 2 min after the injection of ketamine (1.5 mg/kg), in both groups was similar. After the injection of the second dose of ketamine (1 mg/kg) the status of TOF in four patients in ketamine plus MgSO4 (0.45 mg/kg) group changed, it was three quarters but in ketamine group, the status of TOF in all patients was four quarters. The difference between groups was not statistically significant (P = 0.12).
Conclusion:
The findings revealed that for muscle relaxation during medical procedures in the emergency department, ketamine in combination with MgSO4 with this dose was not effective for muscle relaxation during procedures.
Keywords: Emergency room, ketamine, magnesium sulfate, procedural sedation and analgesia
Introduction
In the emergency room, effective and safe sedation have significant contributions in painful and unpleasant procedures. To achieve adequate pain control and muscle relaxation for reduction, procedural sedation and analgesia (PSA) commonly is used with agents which are safe, has a rapid onset of action, rapid recovery, and minimal adverse effects.[1] Today, a wide different spectrum of medications is used to induce PSA and publication evaluated the efficacy of various agents in the emergency room.
Ketamine is an antagonist receptor of N-methyl-D-aspartate (NMDA) and phencyclidine derivate sedative agent that induces a unique dissociative state resulting in amnesia, analgesia, and sedation.[2,3,4] Ketamine can be mixed with other agents and is a popular choice for many emergency department procedures and because protective reflexes are maintained when the agent is titrated correctly it is used extensively in developing countries for operative procedures also it is water-soluble and lipid-soluble and metabolize by liver.[5] The elimination half-life of ketamine is 2 h, with a 30 min duration of action. Many studies showed that ketamine could be used as a desirable and safe medication with low risk of emergence phenomena.[6,7,8,9,10]
Magnesium sulfate (MgSO4) is an endogenous voltage-dependent NMDA receptor channel blocker.[11,12] In different types of pain in humans and animals,[13,14,15] it has been demonstrated that MgSO4 alone has an analgesic effect.[16,17,18]
It is previously reported that MgSO4 may potentiate the effect of ketamine in anesthesia[19] and analgesia.[20,21] Synergistic interaction between MgSO4 and ketamine has been demonstrated in an in vitro[22] and animal study.[23] Up to today, in PSA, synergistic interaction between MgSO4 and ketamine has not been documented. Because of the possible higher effect of ketamine in combination with MgSO4, we hypothesized that a combination of ketamine and MgSO4 might be more effective than ketamine alone in PSA in the emergency department for some specific procedures. Therefore, the objective of the present study was to assess the effect of MgSO4 in PSA when combined with ketamine in patients with fractures and dislocations who were presented to the emergency departments and required short and painful emergency procedures.
Materials and Methods
Between January 2015 and March 2016, this prospective randomized controlled trial study was performed, on 100 patients with long bone fractures and/or dislocations who were presented to the Emergency Departments of Al-Zahra and Kashani, Isfahan, Iran and required PSA for short and painful emergency procedures. Patients with age between 20 and 50-year-old in both genders were eligible if they did not have known or suggestive renal and liver diseases with ASA lower than III. Patients with the following criteria did not include to the study: hemodynamic instability, alcohol influence, neuromuscular disease, pregnancy or lactation, a previous history of opioids abuse, benzodiazepines or ketamine and hypertensive (systolic blood pressure >145 mmHg and diastolic blood pressure >100 mmHg). The study protocol was approved by the Institutional Review Board and Ethics Committee of Isfahan University of Medical Sciences. Participate in the study was voluntarily and informed consent was obtained from agreed subjects before the intervention.
Using random-maker software “Random Allocation,” 100 eligible patients were randomly allocated to two 50-member groups of ketamine plus MgSO4 or ketamine alone. In both group by sedation induced was started the intravenous (IV) injection of 1.5 mg/kg of ketamine, after 2 min, this was followed by 10 min continuous infusion of MgSO4 (0.45 mg/kg MgSO4 solution in 100 cc normal saline) in ketamine plus MgSO4 group and ketamine group was followed by 10 min continuous infusion of normal saline. After that, patients in both groups received IV injection of 1 mg/kg of ketamine. Patients and nurses, who collected data, were blinded to the study groups.
Collected data included age, gender, body mass index, and train of four (TOF) stimulation pattern. TOF was assessed using nerve stimulator machine (Organon TOF-Watch, SX Sward Company, Dublin, Ireland), this was measured between 0 and 4 score based on nerve response to stimulation. If after sedation induced TOF was quarter or two quarters, they were allowed to follow with procedure, but in patients with TOF greater than two quarters following procedure was abandoned and patients were excluded from the study and procedure was down with in routine and standard method.
Statistical analyses were done using SPSS software (SPSS, Inc., Chicago, IL, USA, version 23). Descriptive data are reported as mean ± standard deviation or number (percent) as appropriate. Independent sample t-test and Chi-square test were used to comparing studied variables between groups as appropriate. The level of significance is considered to be <0.05.
Results
Figure 1 shows the flowchart of the study. In this study, 115 patients were reviewed to select 100 eligible patients, 15 patients did not enter the study (9 patients were not eligible, and 6 patients refused informed consent). One hundred eligible patients were randomly divided into two intervention group, and all patients completed the study and analyzed.
Figure 1.
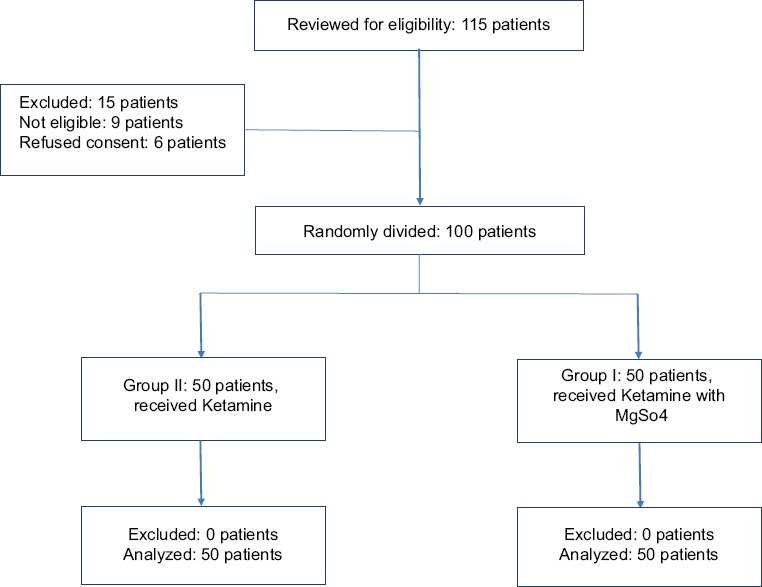
Flowchart of the study
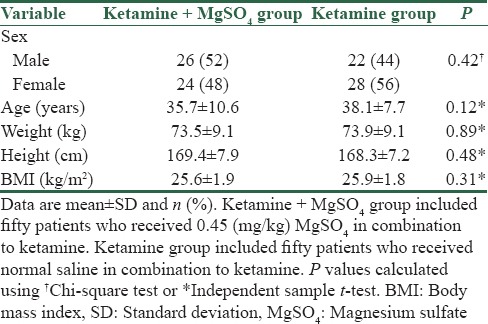
The mean age of the studied patients was 46.9 ± 9.3 years old. Of 100 studied patients 48% were male and 52% were female. Table 1 shows the demographic characteristics of patients in studied groups. Patients in ketamine group were older than patients in ketamine plus MgSO4 group but was not statistically significant (P = 12). Furthermore, no significant differences were noted between studied groups in the term of gender, weight, height, and BMI.
Table 1.
Characteristics of patients in studied groups
TOF status as the main outcome in this study was assessed between groups by Chi-square test and findings are shown in Figure 2. In both group, 2 min after the injection of ketamine, the status of TOF in all patients was four quarters. After the injection of the second dose of ketamine (12 min after the first injection of ketamine), the status of TOF in four patients in ketamine plus MgSO4 group changed to three quarters and in other 46 patients was four quarters, whereas in ketamine group, the status of TOF in all patients was four quarters; however, this difference between groups was not statistically significant (P = 0.12). All patients in both studied groups were excluded, and the procedure was down with in routine and standard method.
Figure 2.
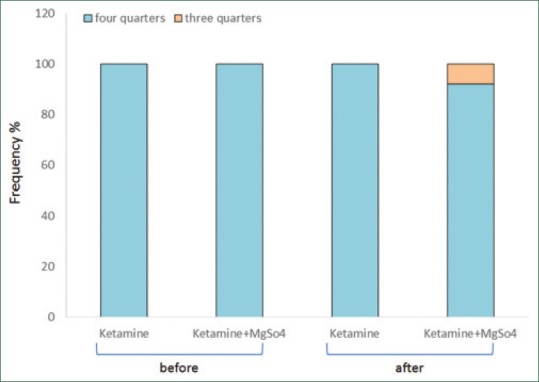
Comparison of frequency of the train of four statuses between study groups by Chi-square test. Ketamine + magnesium sulfate group included fifty patients who received 0.45 mg/kg magnesium sulfate in combination to ketamine. Ketamine group included fifty patients who received normal saline in combination to ketamine. Before injection of magnesium sulfate and after that the difference in percent of train of four between study groups for train of four status was not statistically significant (after, P = 0.12)
Discussion
PSA is a common emergency room clinical practice that during medical procedures improve pain, anxiety, and suffering for patients. Effective sedation enhances the performance of these procedures, with improvements in the patient and medical provider experience. The frequent use of PSA in emergency departments by emergency physicians shows the importance of the continued development of research and clinical evidence for this practice. In this study, MgSO4 was added to ketamine for PSA to assess muscle relaxation. Our findings showed that ketamine alone or in combination with MgSO4 was not effective for muscle relaxation during medical procedures, and there was no significant difference between ketamine alone or in combination with MgSO4.
PSA is intended to result in a continuum of depressed levels of consciousness that allows the patient to maintain airway control independently and continuously.[24] Short-term effects, rapid onset, and excellent sedative and analgesic effects of ketamine, make it as an appropriate choice for short and painful procedures. Several studies have continued to support the use ketamine in children and at present. It is widely used for children undergoing PSA in the emergency department.[25,26,27,28] However, in adults its use has not been well studied and limited studies addressing the use of ketamine as a sole agent in the adult PSA in emergency department.[29,30] Furthermore, emergence reactions including recovery agitation and increases in blood pressure and heart rate raise concerns about its use in adults.[31] Most complications are dose-dependent and observed in higher doses of anesthetic drugs, so, technique that allows to decrease in drug dosing less than that used can be and useful in PSA in emergency department. The IV combination of ketamine and propofol allows drug dosing that is less than that used with either propofol or ketamine as a sole agent and has gained a degree of interest for emergency department PSA patients.[32]
In in vitro and animal studies[22,23] synergistic interaction between MgSO4 and ketamine has been shown. Furthermore, it should be pointed out that this combination for postoperative analgesia was also investigated in humans, but with discrepancy in their results. In a clinical trial, pain or analgesic consumption in children undergoing tonsillectomy did not decrease when children received a small dose of ketamine and/or MgSO4 IV before the start of surgery.[33]
To the best of our knowledge, this study is the first to evaluate the combination of MgSO4 and ketamine for emergency department PSA. However, our findings did not show the difference between ketamine alone or in combination with MgSO4 in PSA. The reason that MgSO4 had no effectiveness in combination with ketamine in the present study may explain by low dose of MgSO4. Several mechanisms of action are reported for both MgSO4 and ketamine that may be responsible for the interaction. Both of MgSO4 and ketamine block the NMDA receptor activation by distinct mechanisms of action.[34,35] The other reported mechanisms for MgSO4 were, reduce the activity of presynaptic and postsynaptic calcium channels and to modulate the release of neurotransmitters, also influencing membrane potentials by exhibits modulator effects on sodium and potassium currents.[11,13] In the other hand, ketamine interacts with calcium and sodium channels, cholinergic transmission, dopamine receptors, and anti-inflammatory effects.[36] Hence, further studies with large samples are suggested to assess the effectiveness of different doses of MgSO4 in combination with ketamine for PSA in the emergency department setting.
Conclusion
The findings of this study revealed that for muscle relaxation during medical procedures in the emergency department, adding MgSO4 (0.45 mg/kg) to ketamine was not effective for muscle relaxation during procedures. However, further randomized, prospective studies are necessary to clarify the safety, efficacy, and effectiveness of the ketamine and MgSO4 combination for PSA in the emergency department setting.
Financial support and sponsorship
This research has been supported financially by Isfahan University of Medical Scinces.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We have to express our appreciation to the Dr. Azim Honormand for sharing their pearls of wisdom with us during this research.
References
- 1.Yatim FM. Intravenous ketamine is as effective as midazolam/fentanyl for procedural sedation and analgesia in the emergency department. Med J Malaysia. 2011;66:231. [PubMed] [Google Scholar]
- 2.Majidinejad S, Esmailian M, Emadi M. Comparison of intravenous ketamine with morphine in pain relief of long bones fractures: A Double Blind Randomized Clinical Trial. Emerg (Tehran) 2014;2:77–80. [PMC free article] [PubMed] [Google Scholar]
- 3.Hosseini M, Karami Z, Janzadenh A, Jameie SB, Haji Mashhadi Z, Yousefifard M, et al. The effect of intrathecal administration of muscimol on modulation of neuropathic pain symptoms resulting from spinal cord injury; an experimental study. Emerg (Tehran) 2014;2:151–7. [PMC free article] [PubMed] [Google Scholar]
- 4.Azizkhani R, Kanani S, Sharifi A, Golshani K, Masoumi B, Ahmadi O. Oral chloral hydrate compare with rectal thiopental in pediatric procedural sedation and analgesia; a randomized clinical trial. Emerg (Tehran) 2014;2:85–9. [PMC free article] [PubMed] [Google Scholar]
- 5.Messenger DW, Sivilotti ML. Evidence-Based Emergency Medicine. Oxford, UK: Wiley-Blackwell; 2009. Procedural sedation and analgesia; pp. 551–60. [Google Scholar]
- 6.Krauss B, Green SM. Procedural sedation and analgesia in children. Lancet. 2006;367:766–80. doi: 10.1016/S0140-6736(06)68230-5. [DOI] [PubMed] [Google Scholar]
- 7.Sahyoun C, Krauss B. Clinical implications of pharmacokinetics and pharmacodynamics of procedural sedation agents in children. Curr Opin Pediatr. 2012;24:225–32. doi: 10.1097/MOP.0b013e3283504f88. [DOI] [PubMed] [Google Scholar]
- 8.McGlone RG, Howes MC, Joshi M. The Lancaster experience of 2.0 to 2.5 mg/kg intramuscular ketamine for paediatric sedation: 501 cases and analysis. Emerg Med J. 2004;21:290–5. doi: 10.1136/emj.2002.003772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brown L, Green SM, Sherwin TS, Besh B, Denmark TK, Moynihan JA, Khan A. Ketamine with and without atropine: What's the risk of excessive salivation? Acad Emerg Med. 2003;10:482–3. [Google Scholar]
- 10.Kashani P, Yousefian S, Amini A, Heidari K, Younesian S, Hatamabadi HR. The effect of intravenous ketamine in suicidal ideation of emergency department patients. Emerg (Tehran) 2014;2:36–9. [PMC free article] [PubMed] [Google Scholar]
- 11.Herroeder S, Schönherr ME, De Hert SG, Hollmann MW. Magnesium – Essentials for anesthesiologists. Anesthesiology. 2011;114:971–93. doi: 10.1097/ALN.0b013e318210483d. [DOI] [PubMed] [Google Scholar]
- 12.Rondón LJ, Privat AM, Daulhac L, Davin N, Mazur A, Fialip J, et al. Magnesium attenuates chronic hypersensitivity and spinal cord NMDA receptor phosphorylation in a rat model of diabetic neuropathic pain. J Physiol. 2010;588:4205–15. doi: 10.1113/jphysiol.2010.197004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Srebro DP, Vuckovic S, Vujovic KS, Prostran M. Anti-hyperalgesic effect of systemic magnesium sulfate in carrageenan-induced inflammatory pain in rats: Influence of the nitric oxide pathway. Magnes Res. 2014;27:77–85. doi: 10.1684/mrh.2014.0364. [DOI] [PubMed] [Google Scholar]
- 14.Borazan H, Kececioglu A, Okesli S, Otelcioglu S. Oral magnesium lozenge reduces postoperative sore throat: A randomized, prospective, placebo-controlled study. Anesthesiology. 2012;117:512–8. doi: 10.1097/ALN.0b013e3182639d5f. [DOI] [PubMed] [Google Scholar]
- 15.Yousef AA, Al-deeb AE. A double-blinded randomised controlled study of the value of sequential intravenous and oral magnesium therapy in patients with chronic low back pain with a neuropathic component. Anaesthesia. 2013;68:260–6. doi: 10.1111/anae.12107. [DOI] [PubMed] [Google Scholar]
- 16.Soave PM, Conti G, Costa R, Arcangeli A. Magnesium and anaesthesia. Curr Drug Targets. 2009;10:734–43. doi: 10.2174/138945009788982487. [DOI] [PubMed] [Google Scholar]
- 17.Nechifor M. Magnesium involvement in pain. Magnes Res. 2011;24:220–2. doi: 10.1684/mrh.2011.0296. [DOI] [PubMed] [Google Scholar]
- 18.Morrison AP, Hunter JM, Halpern SH, Banerjee A. Effect of intrathecal magnesium in the presence or absence of local anaesthetic with and without lipophilic opioids: A systematic review and meta-analysis. Br J Anaesth. 2013;110:702–12. doi: 10.1093/bja/aet064. [DOI] [PubMed] [Google Scholar]
- 19.Irifune M, Shimizu T, Nomoto M, Fukuda T. Ketamine-induced anesthesia involves the N-methyl-D-aspartate receptor-channel complex in mice. Brain Res. 1992;596:1–9. doi: 10.1016/0006-8993(92)91525-j. [DOI] [PubMed] [Google Scholar]
- 20.DeRossi R, Pompermeyer CT, Silva-Neto AB, Barros AL, Jardim PH, Frazílio FO. Lumbosacral epidural magnesium prolongs ketamine analgesia in conscious sheep. Acta Cir Bras. 2012;27:137–43. doi: 10.1590/s0102-86502012000200007. [DOI] [PubMed] [Google Scholar]
- 21.Jahangiri L, Kesmati M, Najafzadeh H. Evaluation of analgesic and anti-inflammatory effect of nanoparticles of magnesium oxide in mice with and without ketamine. Eur Rev Med Pharmacol Sci. 2013;17:2706–10. [PubMed] [Google Scholar]
- 22.Liu HT, Hollmann MW, Liu WH, Hoenemann CW, Durieux ME. Modulation of NMDA receptor function by ketamine and magnesium: Part I. Anesth Analg. 2001;92:1173–81. doi: 10.1097/00000539-200105000-00019. [DOI] [PubMed] [Google Scholar]
- 23.Savic Vujovic KR, Vuckovic S, Srebro D, Medic B, Stojanovic R, Vucetic C, et al. A synergistic interaction between magnesium sulphate and ketamine on the inhibition of acute nociception in rats. Eur Rev Med Pharmacol Sci. 2015;19:2503–9. [PubMed] [Google Scholar]
- 24.Clinical policy for procedural sedation and analgesia in the emergency department. American College of Emergency Physicians. Ann Emerg Med. 1998;31:663–77. [PubMed] [Google Scholar]
- 25.McQueen A, Wright RO, Kido MM, Kaye E, Krauss B. Procedural sedation and analgesia outcomes in children after discharge from the emergency department: Ketamine versus fentanyl/midazolam. Ann Emerg Med. 2009;54:191–97.e1-4. doi: 10.1016/j.annemergmed.2009.04.015. [DOI] [PubMed] [Google Scholar]
- 26.Melendez E, Bachur R. Serious adverse events during procedural sedation with ketamine. Pediatr Emerg Care. 2009;25:325–8. doi: 10.1097/PEC.0b013e3181a341e0. [DOI] [PubMed] [Google Scholar]
- 27.Green SM, Roback MG, Krauss B, Brown L, McGlone RG, Agrawal D, et al. Predictors of airway and respiratory adverse events with ketamine sedation in the emergency department: An individual-patient data meta-analysis of 8,282 children. Ann Emerg Med. 2009;54:158–68.e1-4. doi: 10.1016/j.annemergmed.2008.12.011. [DOI] [PubMed] [Google Scholar]
- 28.Green SM, Roback MG, Krauss B, Brown L, McGlone RG, Agrawal D, et al. Predictors of emesis and recovery agitation with emergency department ketamine sedation: An individual-patient data meta-analysis of 8,282 children. Ann Emerg Med. 2009;54:171–80. doi: 10.1016/j.annemergmed.2009.04.004. [DOI] [PubMed] [Google Scholar]
- 29.Miner JR, Gray R, Delavari P, Patel S, Patel R, Plummer D. Alfentanil for procedural sedation in the emergency department. Ann Emerg Med. 2011;57:117–21. doi: 10.1016/j.annemergmed.2010.08.010. [DOI] [PubMed] [Google Scholar]
- 30.Dunn MJ, Mitchell R, Souza CD, Drummond G. Evaluation of propofol and remifentanil for intravenous sedation for reducing shoulder dislocations in the emergency department. Emerg Med J. 2006;23:57–8. doi: 10.1136/emj.2004.021410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Newton A, Fitton L. Intravenous ketamine for adult procedural sedation in the emergency department: A prospective cohort study. Emerg Med J. 2008;25:498–501. doi: 10.1136/emj.2007.053421. [DOI] [PubMed] [Google Scholar]
- 32.Jagoda AS, Campbell M, Karas S, Mariani PJ, Shepherd SM, Cantrill SV, et al. Clinical policy for procedural sedation and analgesia in the emergency department. Ann Emerg Med. 1998;31:663–77. doi: 10.1016/S0196-0644(98)70216-1. [DOI] [PubMed] [Google Scholar]
- 33.O’Flaherty JE, Lin CX. Does ketamine or magnesium affect posttonsillectomy pain in children? Paediatr Anaesth. 2003;13:413–21. doi: 10.1046/j.1460-9592.2003.01049.x. [DOI] [PubMed] [Google Scholar]
- 34.Oye I, Paulsen O, Maurset A. Effects of ketamine on sensory perception: Evidence for a role of N-methyl-D-aspartate receptors. J Pharmacol Exp Ther. 1992;260:1209–13. [PubMed] [Google Scholar]
- 35.Orser BA, Pennefather PS, MacDonald JF. Multiple mechanisms of ketamine blockade of N-methyl-D-aspartate receptors. Anesthesiology. 1997;86:903–17. doi: 10.1097/00000542-199704000-00021. [DOI] [PubMed] [Google Scholar]
- 36.Hirota K, Lambert DG. Ketamine: New uses for an old drug? Br J Anaesth. 2011;107:123–6. doi: 10.1093/bja/aer221. [DOI] [PubMed] [Google Scholar]


