Abstract
We examined whether a history of self-reported childhood sexual abuse (CSA) moderates the relationship between obesity and mental health symptoms (depression, anxiety, and posttraumatic stress disorder) in an ethnically diverse sample of low-income women. A community sample of 186 women completed self-report measures and had their weight and height measured. Body mass index and CSA had an interactive effect on all mental health measures, such that obese women with a CSA history reported substantially higher levels of all symptoms. These results give greater specificity to the obesity–mental health link reported in previous studies and provide possible directions for targeted intervention.
Keywords: obesity, depression, anxiety, PTSD, childhood sexual abuse
Introduction
Obesity and mood disorders are two of the most common chronic health problems in the United States, particularly among women. More than 65% of women meet criteria for overweight (body mass index [BMI] ≥ 25), and more than one third meet criteria for obesity (BMI ≥ 30; Ogden, Carroll, Kit, & Flegal, 2014). Mood and anxiety disorders are also prevalent, particularly among women. Among women, the lifetime prevalence rate for major depression disorder is 22.1%, for generalized anxiety disorder is 7.7%, and for posttraumatic stress disorder (PTSD) is 11.7% (Kessler, Petukhova, Sampson, Zaslavsky, & Wittchen, 2012). These prevalence rates are concerning because obesity and mental health symptoms are highly prevalent and related to a number of serious chronic medical disorders such as type 2 diabetes and heart disease (Dong et al., 2004; Evans et al., 2005; Mokdad et al., 2003).
Further complicating these health problems is their common comorbidity. Several syntheses of prospective studies indicate a bidirectional relationship between obesity and depression, with both conditions increasing the subsequent risk of the other (Blaine, 2008; Luppino et al., 2010). Although depression has been the focus of obesity and mental health comorbidity research, a similar pattern emerges with related mental health conditions. For example, results from other meta-analyses indicate there is a positive association between anxiety and obesity (Gariepy, Nitka, & Schmitz, 2010) and PTSD and obesity (Scott, McGee, Wells, & Oakley Browne, 2008). These findings are consistent with Katon’s (2003) conceptual model of the interaction between depression and anxiety disorders and chronic medical conditions such as obesity.
Although there is theoretical and empirical support for the relationship between obesity and mental health symptoms, the magnitude of this association is often modest, and several studies have reported no relationship (see Atlantis & Baker, 2008). Small to moderate effect sizes may reflect heterogeneity within the population, with certain subgroups more prone to experiencing comorbid obesity and psychiatric symptoms. In their literature review, Stunkard, Faith, and Allison (2003) highlighted the need to study moderators of the obesity–mental health link and proposed adverse childhood experiences as one possible moderating factor. To date, however, most research aimed at identifying subgroups at greater risk and has focused on sociodemographic characteristics, such as gender, race, and education (Simon et al., 2006). While this research is informative, identifying characteristics that moderate the obesity–mental health link can provide insight into potential underlying mechanisms and targets for intervention. Childhood sexual abuse (CSA) may be a particularly important adverse childhood experience to study due to its prevalence among women and the documented association between CSA and long-lasting psychiatric and physical health outcomes (Gustafson & Sarwer, 2004).
The goal of this study is to test whether CSA moderates the relationship between obesity and mental health. Approximately 15–30% of women experience an unwanted sexual experience during childhood (Gilbert et al., 2009). Katon (2003) suggests that childhood adversity, including CSA, is a risk factor in the interaction between mood/anxiety disorders and chronic medical illness. CSA is a known risk factor for obesity and depression, anxiety, and PTSD symptoms (Danese & Tan, 2013; Fergusson, McLeod, & Horwood, 2013; Rohde et al., 2008). Although relatively unstudied, there are several reasons to believe CSA may increase the likelihood for co-occurring obesity and psychiatric symptoms by compounding the risk that each condition poses to the other. For example, women who have experienced CSA report a more negative self-concept (McAlpine & Shanks, 2010) and more body image disturbance (Wenninger & Heiman, 1998). Consequently, survivors of CSA who are obese may be especially likely to engage in negative self-appraisals, which in turn contribute to depression and related mood disorders. Additionally, women who report CSA endorse more maladaptive consumptive coping strategies to manage emotional distress, including binge eating, compared to women without a CSA history (Sarin & Nolen-Hoeksema, 2010). As a result, women with CSA history who experience ongoing negative affect may be more likely to become obese (Rohde et al., 2008). Finally, CSA may result in hypothalamic-pituitary-adrenal axis (HPA) axis dysregulation, which in turn has implications for subsequent mental health symptoms (Hulme, 2011) and eating behaviors (Sominsky & Spencer, 2014).
In sum, existing research suggests CSA survivors may be at heightened risk for the co-occurrence of obesity and poor mental health; however, few studies have examined this possibility. Low-income women are a particularly vulnerable group due to the high rates of CSA reported by women who were raised in a low-income household (Butler, 2013). Family income is also associated with women’s mental health symptoms (Gupta & Huston, 2009). In this study, we test whether a history of CSA magnifies the association between obesity and mental health symptoms (depression, anxiety, and PTSD) in an ethnically diverse sample of low-income women. Identifying subgroups of women at elevated risk can provide insight into the mechanisms underlying comorbidity in obesity and mental health and help inform more targeted intervention services.
Methods
Participants and Procedures
Participants included 186 women in a low-income city (age in years, M = 41.58, SD = 8.04, Range = 20.83–66.42; BMI, M = 31.94, SD = 7.03, Range = 17.29–49.44). These women were participating in a larger National Institutes of Health-funded study of the cultural context of adolescent health that focused on adolescent–female caretaker dyads. Of the participants, 58% were Latina, 22% were African American, and 20% were non-Hispanic White. Educationally, 22% of women had not completed high school, 67% had a high school degree, and 11% had a bachelor’s degree. Participants were recruited from city schools, community centers, Young Women’s Christian Association (YWCA), local media outlets, and word of mouth. Interviews were conducted in English and Spanish (20%) based on participant preference. Participants completed survey instruments privately using Audio Computer Assisted Survey Instruments (ACASI) in their preferred language, and then had their height and weight measured. Interviews took approximately 2 hr, and participants were compensated US$40 each for their time. All procedures were approved by the University of Connecticut Institutional Review Board.
Measures
BMI
Participants had their weight measured without shoes to the nearest 0.1 pound using a digital scale (BT-350e; Tanita, Arlington Heights, IL). Height was measured to the nearest 0.25 inch using a height rod on a standard spring scale. Weight and height were converted to BMI as kg/m2 and were categorized (healthy weight, overweight, and obese) using Centers for Disease Control and Prevention (CDC, 2011) standard weight status categories.
Mental health symptoms
The 9-item Patient Health Questionnaire (PHQ; Spitzer, Williams, Kroenke, Hornyak, & McMurray, 2000) was used to assess depressive symptoms (α = .84, clinical cutoff = total score ≥10). The 7-item Generalized Anxiety Domain of the Brief Symptom Inventory (BSI; Derogatis, 1993) was used to assess anxiety symptoms (α = .87, clinical cutoff = total score > 65). The 17-item Posttraumatic Checklist-Civilian (PCL-C; Ruggiero, Del Ben, Scotti, & Rabalais, 2003) was used to assess PTSD symptoms (α = .95, clinical cutoff for civilians = total score > 35). All of these widely validated instruments measure symptoms based on Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition, Text Revision) criteria.
Sexual abuse history
Participants were asked via ACASI about the occurrence of several adverse events during childhood prior to age 18, including whether anyone ever did something sexual to them that was forced, unwanted, or against their will. Participants were asked to respond “yes” or “no.” Although retrospective reports of CSA have limitations (e.g., recall bias and mood-based memory effects), this type of measure has demonstrated validity (Widom, 1997) and reliability (Fergusson, Horwood, & Boden, 2011) as well as predictive utility in accounting for variability in mental health outcomes (Kendler & Aggen, 2014).
Control variables
Race/ethnicity, marital status, and an Socioeconomic status (SES) risk composite (no high school (HS) degree, living in subsidized housing, child receives free/reduced lunch) were used as control variables. Endorsement of childhood physical abuse was used as a covariate to isolate the potential effects of sexual abuse from other forms of maltreatment.
Data Analytic Plan
Tests of main and interactive effects of CSA and BMI weight category (healthy weight, overweight, and obese) on mental health symptoms (depression, anxiety, and PTSD) were conducted using multivariate analysis of covariance (MANCOVA), controlling for covariates.
Results
Based on CDC (2011) percentiles calculated from BMI measures, 17% of the participants were healthy weight, 27% of participants were overweight, and 56% were obese (BMI M = 31.94, SD = 7.02). Approximately 36% of the sample reported CSA. Based on established cutoffs for the PHQ-9, BSI Anxiety, and PCL-C, 22% of women reported clinically elevated depressive symptoms, 25% reported elevated anxiety, and 26% had scores above cutoffs for screening for PTSD.
The first set of analyses examined the bivariate relationship between BMI and CSA history. Women who reported CSA did not have a higher BMI than women who did not report CSA (M = 32.57, SD = 7.19 vs. M = 31.43, SD = 6.99, respectively), t(182)= −1.05, p = .30. Similarly, CSA history was not significantly associated with BMI weight category (healthy weight, overweight, or obese), χ2 = 2.36, df = 2, p = .31.
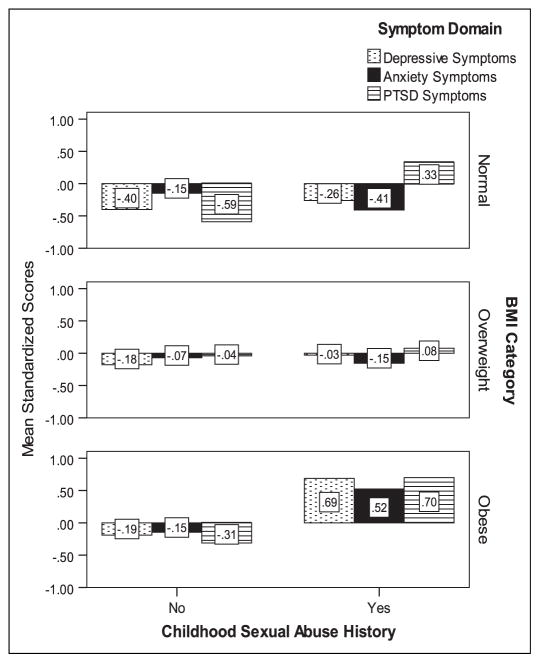
Next, MANCOVA was used to test for main effects and interactive effects of CSA history and BMI category on mental health symptoms, controlling for covariates. In multivariate analysis with all three symptoms domains included as dependent variables, there was a significant omnibus main effect of BMI, F(6,330) = 2.25, p < .05, η2 = .04, CSA history, F(6,165) = 2.83, p < .05, η2 = .05, and the interaction term, F(6,330) = 3.07, p < .01, η2 = .05). Of note, the CSA × BMI interaction was significant for each of the three outcomes: depressive symptoms, F(2,167)=4.29, p < .05, η2 = .05, anxiety symptoms, F(2,167) = 3.70, p < .05, η2 = .04, and PTSD symptoms, F(2,167)=5.20, p < .01, η2 = .06. Figure 1 shows group differences in mental health symptoms in standardized scores (to compare across symptom domain) based on BMI category and CSA history groups. As shown, women who were obese and reported a CSA history also reported substantially more severe symptoms compared to all other women. In contrast, obese women without a CSA history did not show a significant elevation in symptoms. For women without CSA, rates of clinically elevated depression scores (≤10 on PHQ-9) for women who were a healthy weight, overweight, and obese were 4%, 10%, and 15%, respectively, and these rates were 12%, 24%, and 47% for women with a self-report CSA history. Of note, nearly half of obese women with a CSA history reported elevated depressive symptoms, compared to only 15% of obese women without a CSA history. A similar pattern was evident in the rate of clinically elevated anxiety and PTSD symptoms.
Figure 1.
Standardized mean score differences in mental health symptoms in women by child sexual abuse (CSA)history and body mass index (BMI) category. The figure depicts the CSA history (x-axis) × BMI category interaction for all three symptom domains (depressive, anxiety, and posttraumatic stress disorder [PTSD] symptoms). The y-axis reflects mean standardized scores for each symptom domain (standardized within symptom measure across the sample). Standardized z scores were used to allow for comparison of results for the three symptom domains.
In the initial analysis, we included self-reported physical abuse as a control variable because different forms of abuse often co-occur (Finkelhor, Turner, Ormrod, & Hamby, 2009), and we were interested in whether CSA has a specific effect on the obesity–mental health link. If only CSA was included, significant results may emerge because CSA is acting as a proxy of some other form of abuse; however, given the co-occurrence of CSA and CPA, controlling for this variable in analysis could also lead to biased results. Consequently, we ran two post hoc analyses. First, we conducted the above-mentioned analyses without physical abuse as a covariate, and all significant results remained. Second, we ran the moderation model with CPA as the potential moderator in place of CSA. No significant interactions were found. These results suggest CSA may have a distinct effect on the obesity–mental health link relative to other forms of childhood maltreatment.
Conclusion
A wide body of research indicates that obesity and poor mental health are correlated in the general population, although the magnitude of this association is modest (Atlantis & Baker, 2008). Results from this study suggest that the modest relationship found in many studies may obscure important subgroup differences, particularly among low-income women. Specifically, women with a CSA history and obesity may be very likely to experience clinically elevated depression, anxiety, and PTSD symptoms; however, obese women without this history may have the same mental health risk as women who are not obese, at least among low-income populations. This distinction is important because it suggests generalizing findings about the obesity–mental health link may lead to erroneous conclusions about the risk for poor mental health in most obese women. Notably, in this sample there was not a significant relationship between obesity and CSA history. In other words, women with a CSA history are not more likely to be obese, but if they are obese and have a CSA history, they are more likely to experience mental health symptoms.
There are several reasons why CSA might magnify the association between obesity and poor mental health. For example, both CSA and obesity are stigmatized characteristics in our society, and having multiple stigmatized identities can have a synergistically negative effect on well-being (Quinn, 2006). Prospective studies that incorporate measures of potential mechanisms (e.g., emotional eating, externally derived self-worth, and shame proneness) would provide further insight as would ethnographic studies to capture potential differences in the meaning ascribed to CSA in healthy weight and women who are obese.
The primary limitations of this study include the brief assessment of CSA history and limited measurement of height and weight. A more detailed assessment of CSA (i.e., age, duration, and severity of CSA) would have been beneficial in light of findings that suggest there is a particularly strong association between obesity and depression among women who experienced severe forms of abuse (Gustafson & Sarwer, 2004). The current study only measured height and weight once, however multiple weight measurements increases the accuracy of BMI calculations. This study is also cross sectional; longitudinal research would allow for identification of mechanisms that contribute to the group differences.
Although replication and prospective research on mechanisms is needed, our findings do have some clinical implications. For example, assessing trauma history in obese women seeking mental health services may help identify key targets for treatment. More broadly, this area of research highlights the potential importance of programs for low-income women that integrate physical and mental health services in one setting. Given the prevalence and cost of obesity and depression within this population, interventions that try to target both debilitating conditions are needed.
Acknowledgments
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was conducted with support to the second author from National Institutes of Health (R21HDO65185).
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Atlantis E, Baker M. Obesity effects on depression: Systematic review of epidemiological studies. International Journal of Obesity. 2008;32:881–891. doi: 10.1038/ijo.2008.54. [DOI] [PubMed] [Google Scholar]
- Blaine B. Does depression cause obesity?: A meta-analysis of longitudinal studies of depression and weight control. Journal of Health Psychology. 2008;13:1190–1997. doi: 10.1177/1359105308095977. [DOI] [PubMed] [Google Scholar]
- Butler AC. Child sexual assault: Risk factors for girls. Child Abuse & Neglect. 2013;37:643–652. doi: 10.1016/j.chiabu.2013.06.009. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Body mass index. 2011 Retrieved October 2014, from http://www.cdc.gov/healthyweight/assessing/bmi/index.html.
- Danese A, Tan M. Childhood maltreatment and obesity: Systematic review and meta-analysis. Molecular Psychiatry. 2013;19:544–555. doi: 10.1038/mp.2013.54. [DOI] [PubMed] [Google Scholar]
- Derogatis L. BSI brief symptom inventory: Administration, scoring, and procedures manual. 4. Minneapolis, MN: National Computer Systems; 1993. [Google Scholar]
- Dong M, Giles WH, Felitti V, Dube S, Williams J, Chapman D, Anda R. Insights into causal pathways for ischemic heart disease: Adverse Childhood Experiences Study. Circulation. 2004;10:1761–1766. doi: 10.1161/01.CIR.0000143074.54995.7F. [DOI] [PubMed] [Google Scholar]
- Evans DL, Charney DS, Lewis L, Golden RN, Gorman JM, Krishman KR, Valvo WJ. Mood disorders in the medically ill: Scientific review and recommendations. Biological Psychiatry. 2005;58:175–189. doi: 10.1016/j.biopsych.2005.05.001. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, Boden JM. Structural equation modeling of repeated retrospective reports of childhood maltreatment. International Journal of Methods in Psychiatric Research. 2011;20:93–104. doi: 10.1002/mpr.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fergusson DM, McLeod GH, Horwood L. Childhood sexual abuse and adult developmental outcomes: Findings from a 30-year longitudinal student in New Zealand. Child Abuse & Neglect. 2013;37:664–674. doi: 10.1016/j.chiabu.2013.03.013. [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Turner H, Ormrod R, Hamby SL. Violence, abuse, and crime exposure in a national sample of children and youth. Pediatrics. 2009;124:1411–1423. doi: 10.1542/peds.2009-0467. [DOI] [PubMed] [Google Scholar]
- Gariepy G, Nitka D, Schmitz N. The association between obesity and anxiety disorders in the population: A systematic review and meta-analysis. International Journal of Obesity. 2010;34:407–419. doi: 10.1038/ijo.2009.252. [DOI] [PubMed] [Google Scholar]
- Gilbert R, Widom C, Browne K, Fergusson D, Webb E, Janson S. Burden and consequences of child maltreatment in high-income countries. Lancet. 2009;373:68–81. doi: 10.1016/S0140-6736(08)61706-7. [DOI] [PubMed] [Google Scholar]
- Gupta AE, Huston AC. Depressive symptoms and economic outcomes of low-income women: A review of the social causation, social selection, and interactionist hypotheses. Social Issues and Policy Review. 2009;3:103–140. [Google Scholar]
- Gustafson TB, Sarwer DB. Childhood sexual abuse and obesity. Obesity Reviews. 2004;5:129–135. doi: 10.1111/j.1467-789X.2004.00145.x. [DOI] [PubMed] [Google Scholar]
- Hulme PA. Childhood sexual abuse, HPA axis regulation, and mental health: An integrative review. Western Journal of Nursing Research. 2011;33:1069–1097. doi: 10.1177/0193945910388949. [DOI] [PubMed] [Google Scholar]
- Katon W. Clinical and health services relationship between major depression, depressive symptoms, and general medical illness. Society of Biological Psychiatry. 2003;54:216–226. doi: 10.1016/s0006-3223(03)00273-7. [DOI] [PubMed] [Google Scholar]
- Kendler K, Aggen S. Clarifying the causal relationship in women between childhood sexual abuse and lifetime major depression. Psychological Medicine. 2014;44:1213–1221. doi: 10.1017/S0033291713001797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Petukhova M, Sampson NA, Zaslavsky AM, Wittchen H. Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. International Journal of Methods in Psychiatric Research. 2012;21:169–184. doi: 10.1002/mpr.1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luppino S, de Wit L, Bouvy P, Stijnen T, Cuijpers P, Penninx B, Zitman F. Overweight, obesity, and depression: A systematic review and meta-analysis of longitudinal studies. Archives of General Psychiatry. 2010;67:220–229. doi: 10.1001/archgenpsychiatry.2010.2. [DOI] [PubMed] [Google Scholar]
- McAlpine SJ, Shanks A. Self-concept and attributions about other women in women with a history of childhood sexual abuse. Clinical Psychology & Psychotherapy. 2010;17:196–210. doi: 10.1002/cpp.671. [DOI] [PubMed] [Google Scholar]
- Mokdad AH, Ford ES, Bowman BA, Dietz WH, Vinicor F, Bales VS, Marks JS. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. Journal of the American Medical Association. 2003;289:76–79. doi: 10.1001/jama.289.1.76. [DOI] [PubMed] [Google Scholar]
- Ogden C, Carroll M, Kit B, Flegal K. Prevalence of childhood and adult obesity in the United States, 2011–2012. Journal of the American Medical Association. 2014;311:806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinn DM. Concealable versus conspicuous stigmatized identities. In: Levin S, van Laar C, editors. Stigma and group inequality: Social psychological perspectives. Mahwah, NJ: Lawrence Erlbaum Associates Publishers; 2006. pp. 83–103. [Google Scholar]
- Rohde P, Ichikawa L, Simon G, Ludman E, Linde J, Jeffery R, Operskalski B. Associations of child sexual and physical abuse with obesity and depression in middle aged women. Child Abuse & Neglect. 2008;32:878–887. doi: 10.1016/j.chiabu.2007.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruggiero K, Del Ben K, Scotti J, Rabalais A. Psychometric properties of the PTSD checklist—Civilian version. Journal of Traumatic Stress. 2003;16:495–502. doi: 10.1023/A:1025714729117. [DOI] [PubMed] [Google Scholar]
- Sarin S, Nolen-Hoeksema S. The dangers of dwelling: An examination of the relationship between rumination and consumptive coping in survivors of childhood sexual abuse. Cognition and Emotion. 2010;24:71–85. [Google Scholar]
- Scott KM, McGee MA, Wells JE, Browne MO. Obesity and mental disorders in the adult general population. Journal of Psychosomatic Research. 2008;64:97–105. doi: 10.1016/j.jpsychores.2007.09.006. [DOI] [PubMed] [Google Scholar]
- Simon GE, Von Korff M, Saunders K, Miglioretti DL, Crane PK, van Belle G, Kessler RC. Association between obesity and psychiatric disorders in adult population. Archives of General Psychiatry. 2006;63:824–830. doi: 10.1001/archpsyc.63.7.824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sominsky L, Spencer SJ. Eating behavior and stress: A pathway to obesity. Frontiers in Psychology. 2014;5 doi: 10.3389/fpsyg.2014.00434. Retrieved July 2, 2015 from Psychinfo. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R, Williams J, Kroenke K, Hornyak R, McMurray J. Validity and utility of the PRIME-MD patient health questionnaire in assessment of 3000 obstetric-gynecologic patients. American Journal of Obstetrics and Gynecology. 2000;183:759–769. doi: 10.1067/mob.2000.106580. [DOI] [PubMed] [Google Scholar]
- Stunkard AJ, Faith MS, Allison KC. Depression and obesity. Biological Psychiatry. 2003;54:330–337. doi: 10.1016/s0006-3223(03)00608-5. [DOI] [PubMed] [Google Scholar]
- Wenninger K, Heiman JR. Relating body image to psychological and sexual functioning in child sexual abuse survivors. Journal of Traumatic Stress. 1998;11:543–562. doi: 10.1023/A:1024408830159. [DOI] [PubMed] [Google Scholar]
- Widom CS. Accuracy of adult recollections of early childhood abuse. In: Read JD, Lindsay DS, editors. Recollections of trauma: Scientific evidence and clinical practice. New York, NY: Plenum Press; 1997. pp. 49–78. [Google Scholar]