Abstract
OBJECTIVES
Research estimates that a significant percentage of individuals with Mild Cognitive Impairment (MCI) experience functional difficulties. In addition to reduced accuracy on measures of everyday function, cross-sectional research has demonstrated that speed of performing instrumental activities of daily living (IADLs) is slowed in individuals with MCI. The present study investigated whether baseline and longitudinal changes in speed and accuracy of IADL performance differed between persons with MCI and cognitively normal peers.
DESIGN
Linear mixed models were used to estimate group differences in longitudinal performance on measures of IADLs.
SETTING
Assessments were conducted at university and medical research centers.
PARTICIPANTS
The sample consisted of 80 participants with MCI and 80 control participants who were enrolled in the Alzheimer’s Disease Research Center’s Measuring Independent Living in the Elderly Study (MILES).
MEASUREMENTS
IADL speed and accuracy were directly assessed using selected domains of the Financial Capacity Instrument, the Timed IADL assessment, and driving-related assessments (Useful Field of View, Road Sign Test).
RESULTS
Individuals with MCI performed worse on speed and accuracy measures of IADLs in comparison to cognitively normal peers and demonstrated significantly steeper rates of decline over 3 years in either speed or accuracy in all domains assessed.
CONCLUSION
Both speed and accuracy of performance on measures of IADL are valuable indices for early detection of functional change in MCI. The performance pattern may reflect a trade-off between speed and accuracy that can guide clinical recommendations for maintaining patient independence.
Keywords: Aging, MCI, Instrumental Activities of Daily Living
OBJECTIVE
Mild Cognitive Impairment (MCI), often conceptualized as a symptomatic predementia phase of cognitive decline, is approximately 2–5 times more common than dementia, with a prevalence of 10 to 20 percent in adults aged 65 and older.1 Diagnostic criteria for MCI include evidence of cognitive impairment but preservation of independence in functional abilities and a lack of significant impairment in social or occupational functioning.1
Emerging evidence estimates that approximately one third of individuals with MCI experience subtle difficulties in functional abilities as measured by performance-based assessments as well as informant and self-report rating instruments.2–6 Specifically, performance on instrumental activities of daily living (IADL) that require more complex cognitive processes, such as financial management, medical management, and driving, may show disease-related decline in MCI, providing a window of opportunity for early detection.7
In comparison to cognitively normal controls, individuals with MCI perform worse and take longer to complete tasks on a number of performance-based assessments of IADL.6,8–10 Studies of financial capacity have demonstrated that patients with MCI performed worse overall on the Financial Capacity Instrument (FCI) than healthy controls.11–13 In addition, individuals with MCI performed worse and took longer to complete the Day-Out Task (DOT), which requires participants to prepare for a day out (i.e. prepare a picnic basket, plan a bus route).8 Wadley and colleagues (2007) found that although the accuracy of task completion on the Timed IADL test (TIADL) was comparable for persons with MCI and controls, individuals with MCI took significantly longer to complete the tasks.1 In summary, an evaluation of both speed and accuracy of task completion on measures of higher order functional abilities is useful in detecting subtle functional deficits in MCI, and speed of task completion may be a more sensitive marker of early functional deficits than accuracy.
Trajectories of functional decline may help differentiate individuals with MCI from older individuals who experience normal age-related cognitive decline.15–17 Longitudinal studies of change in everyday performance indicate that individuals with MCI have faster rates of decline on self-reported measures of IADL and ADL in comparison to controls.14 Differential rates of decline on measures of financial skills are evident between individuals with MCI and controls, and accelerated rates of decline in financial skills may serve as a marker for incipient dementia.15 Nonetheless, few studies have examined longitudinal changes in completion time on performance-based measures of IADL.
Understanding longitudinal changes in speed and accuracy on performance-based measures of functional abilities may shed light on the nature of IADL restriction in older adults, which, ultimately, may improve early clinical detection of restrictions suggestive of MCI and encroaching dementia.18–19 In this study, we investigated whether baseline and longitudinal changes in speed and accuracy of IADL performance differed between persons with amnestic MCI and cognitively normal peers. We hypothesized that baseline differences in speed and accuracy of everyday tasks would increase over time, such that individuals with MCI would have steeper performance declines relative to cognitively normal peers, illustrating a faster rate of functional decline in these two dimensions than what is experienced in normal aging.
METHODS
Participants
Participants were recruited from the Alzheimer’s Disease Research Center (ADRC) at the University of Alabama at Birmingham (UAB). All potential participants underwent neurological and neuropsychological examination through the Clinical Core of the ADRC. Medical records and family reports also were obtained. Following initial evaluation, a team of neurologists, neuropsychologists, and nursing staff determined the diagnoses of participants during annual ADRC consensus conferences using Petersen/Mayo criteria for MCI.20 Specifically, participants (or proxies) had a memory complaint, abnormal memory for age on objective testing (≥ −1.5 SD), normal basic activities of daily living, normal general cognitive function, and no dementia. Participants with differential medical or psychiatric diagnoses that might account for cognitive difficulties were excluded. Participants with a diagnosis of MCI or determined to be cognitively normal during the ADRC consensus process were invited to participate in the Measuring Independent Living in the Elderly Study (MILES), a five-year longitudinal study of cognitive abilities and real world tasks in individuals with MCI and normal controls.
The current analyses included 80 participants with MCI and 80 healthy control participants enrolled in MILES who were matched at the group level on age and education. Written informed consent was obtained from all participants, and all study procedures were approved by the UAB Institutional Review Board. Participants underwent clinical and research evaluations at baseline and at 1 to 4 annual follow-up visits, depending upon the timing of their enrollment. Eight of the healthy controls and 17 of the MCI patients withdrew from the study for the following reasons: deceased (n=8), health problems (n=7), moved away (n=3), and other/unknown reasons (n=7). All other missing data at follow-up were due to the fact that the study continued to enroll participants during the entire study period, which did not allow all participants to complete all annual follow-ups. The number of participants who contributed complete data to the longitudinal models at baseline and the four annual follow-up visits were 154, 127, 96, 52, and 25, respectively.
Measures
Demographic and Medical Variables
We obtained participant demographics including age, gender, race, level of education, living situation, and use of anti-dementia medications through self-report questionnaires. Global cognitive status was assessed using the total score from the Dementia Rating Scale (DRS-2),21 and depressive symptoms were assessed using the Geriatric Depression Scale – Short Form (GDS)22 which consists of 15 “yes/no” items that assess symptoms of depression over the past week. Visual acuity, with corrective lenses when applicable, was assessed using the Early Treatment Diabetic Retinopathy Study (ERDRS) chart.23 Possible scores on visual acuity ranged from 1–100, corresponding to Snellen scores ranging from 20/123 (1) to 20/16 (100).
Everyday Performance Variables
Financial abilities were assessed using a subset of tasks from the Financial Capacity Instrument24; which tested domains of financial conceptual knowledge, cash transactions, bank statement management, and bill payment. This subset of domains has been found to differentiate well between individuals with MCI and cognitively healthy adults.11,25 Accuracy scores of financial abilities were calculated as the sum of scores on all tasks across the four domains (possible range 0 – 141), with higher scores indicative of better performance. Speed of financial abilities task completion was defined as the ratio of time to complete a task to the time allotted for a task, using two timed tasks (2b: calculating a medical deductible, and 7c: preparing a bill for mailing). For example, a person taking 30 secs to complete a task with a time limit of 120 secs would score .25 on that task. This method was chosen to convert the two tasks, which had different time allowances, to the same metric. The proportion of completion time for each task was averaged; lower scores represent faster speed of completion.
The Timed Instrumental Activities of Daily Living test (TIADL)26 is a performance-based measure of everyday function during which participants are asked to complete tasks measuring five domains of Instrumental Activities of Daily Living (IADL): communication, finances, food, shopping, and medicine. Participants are instructed to complete all tasks “as quickly as you can.” For each item, the examiner recorded the time (in tenths of seconds) and accuracy of task completion. Composite speed and accuracy scores on the TIADL are used in the current analyses. TIADL accuracy is the sum of accuracy scores across TIADL tasks (ranging for each task from 1—completed within the time limit with no errors—to 3—not completed within the time limit or with major errors), which were reverse-coded, so that higher scores indicated better performance. TIADL speed is the sum of completion time for each domain task.
The Useful Field of View (UFOV)27 and Road Signs Test (RST)28 are computer-based tasks which we used as proxies for identifying “at-risk” drivers, due to their established predictive utility for driving skills and safety, including risk of future state-recorded motor vehicle crash.29 The UFOV measures the briefest display duration at which one can process multiple stimuli in the visual field, using three increasingly complex visual search tasks (identification, divided attention, selective attention). The stimulus duration (ranging from 16–500 ms) at which a participant can correctly perform 75% of trials within a given task is calculated. The resulting scores are summed and coded into pre-established crash risk categories (1 = very low risk, 2 = low risk, 3 = low–moderate risk, 4 = moderate–high risk, and 5 = high risk). 30, 31
The RST measures reaction time to varying traffic signs using a “go, no-go” paradigm. It measures how quickly an individual notices that one traffic sign changes relative to other signs. The task presents four international road signs (pedestrians, bicycles, left-turn arrows, and right-turn arrows) at various latencies and locations on a computer screen. Participants move the computer mouse in the direction of the arrow signs or click the mouse in response to the pedestrian or bicycle signs only in the absence of a red slash across the sign. The signs are presented in blocks of three and six (13 trials of each condition). The computer-generated response time is the time in milliseconds between the onset of the target stimulus and the participant’s correct response. Any errors committed prior to the correct response on a given trial are not penalized but may add to response time on a given trial. We used the sum of the RST scores on 3 and 6 stimuli tasks in the current analyses as a measure of complex reaction time and information processing speed related to driving.32
Statistical Analyses
Baseline differences between those with MCI and controls for demographic and clinical variables were analyzed using independent samples t-tests for continuous variables and Pearson’s chi-square tests for dichotomous variables.
Linear mixed models 33 were used to estimate differences in longitudinal performance on the measures of financial abilities, UFOV, RST, and TIADL between those with and without a baseline diagnosis of MCI. Mixed models are beneficial for analyzing repeated-measures data because they account for missing data over time and intra-individual correlations of data. Separate models were created for speed and accuracy in each of the domains. Unconditional models assessed the significance of within-subjects variability over time. Because the interaction between diagnosis and time was of primary interest a priori, all unconditional models were followed with conditional models additionally adjusted for diagnosis, the interaction between diagnosis and linear and quadratic effects of time, and between-subjects covariates (centered at the mean) other than the DRS-2 that contributed significantly to the mixed models. The significance level for all analyses was p<.05. All statistical analyses were performed using SPSS 22.0.
Due to the instability of the MCI construct, planned sensitivity analyses were conducted using only individuals identified as stable healthy controls (n=58) or stable/declining MCI (n=63), based on first and last available ADRC diagnosis, to reduce the possible influence of preclinical impairment among controls and “reversion to normal” among MCI participants.
RESULTS
Demographic and Sample Characteristics
Table 1 displays baseline demographic and functional variables by group. The MCI group obtained significantly lower DRS-2 scores by definition, endorsed more depressive symptoms on the GDS, and had poorer corrected far visual acuity. The MCI group was more likely to live with others and included a greater proportion of men than cognitively normal peers. Neither GDS, visual acuity, nor gender significantly contributed to the mixed model analyses, so they were excluded from subsequent analyses. Age alone was a significant contributor to the models and was included as a covariate in all models.
Table 1.
Baseline Demographic and Clinical Characteristics of Study Participants
| Characteristic | Controls (n=80) | MCI (n=80) | Effect | P |
|---|---|---|---|---|
| Age (y) | 68.58±7.5 | 70.57±7.6 | t = 1.67 | .097 |
| Gender, n (%) | X2 = 4.95 | .026 | ||
| Women | 51 (63.8) | 37 (46.3) | ||
| Men | 29 (36.3) | 43 (53.8) | ||
| Race, n (%) | X2 = 0.00 | 1.000 | ||
| White | 66 (82.5) | 66 (82.5) | ||
| Black | 14 (17.5) | 14 (17.5) | ||
| Education (y) | 15.23±2.5 | 15.08±3.0 | t = −.34 | .731 |
| DRS-2 Total | 138.62±5.5 | 132.29±6.9 | t = −5.91 | <.001 |
| GDS | 4.09±4.2 | 7.87±5.2 | t = 4.92 | <.001 |
| Live Alone, n (%) | 24 (30.0) | 11 (13.8) | t = 6.18 | .013 |
| Far Visual Acuitya | 81.08±7.2 | 76.15±13.1 | t = −2.94 | .004 |
| Financial Task Accuracyb | 131.09±8.7 | 118.00±19.5 | – | |
| Financial Task Speedc | 0.31±0.1 | 0.41±0.2 | – | |
| TIADL Accuracyd | 28.49±.8 | 27.73±1.74 | – | |
| TIADL Speede | 82.80±22.5 | 146.91±83.5 | – | |
| UFOV Risk Categoryf | 1.46±.9 | 2.40±1.4 | – | |
| RST Speedg | 3.20±.7 | 4.59±2.7 | – |
NOTE. Values are mean ± SD unless otherwise indicated.
Continuous variables differences were analyzed with independent samples t-tests and dichotomous variables were analyzed with chi-square.
P-values for functional performance measures are not included because baseline differences were assessed in mixed model analyses (see Table 2).
Abbreviations: GDS, Geriatric Depression Scale; DRS-2, Dementia Rating Scale 2nd Edition; TIADL, Timed Instrumental Activities of Daily Living; UFOV, Useful Field of View; RST, Road Signs Test.
Far visual acuity mean values correspond to Snellen scores of 20/20 (controls) and 20/22 (MCI group).
Possible score range on financial ability accuracy (0, 141).
Possible score range on financial ability speed (0,1).
Possible score range on TIADL Accuracy (8, 29).
Possible score range on TIADL Speed (0,180).
Possible score range on UFOV Risk Category (1, 5).
Abbreviations: FCI, Financial Capacity Instrument; UFOV, Useful Field of View; TIADL, Timed Instrumental Activities of Daily Living; RST, Road Signs Test; Diagnosis, Baseline Diagnosis; Age was centered at the mean, 69.57 years; Time2 refers to the rate of change over time,
p<.05, two tailed;
p<.01, two tailed;
p<.001, two tailed.
Unconditional Growth Models
The results of the unconditional, repeated measures mixed models for each speed and accuracy measure of everyday function revealed a significant linear effect of visit for models of UFOV risk category suggesting a reduction in level of risk over time, and a significant quadratic effect of time (Time2) for financial task accuracy and TIADL speed. No other unconditional models revealed significant effects of time in the full sample.
Conditional Growth Models
Conditional mixed models for each outcome measure included age (mean-centered), baseline diagnosis, Diagnosis × Time interaction, and Diagnosis × Time2 interaction. Table 2 presents the parameter estimates for conditional models of speed and accuracy of everyday task completion. The addition of age (mean-centered), baseline diagnosis, and Diagnosis × Time improved the model fit for FCI speed, UFOV risk category, RST speed, and TIADL accuracy in comparison to the unconditional models that included only the linear trend of time. Similarly, the addition of the covariates and Diagnosis × Time2 interaction improved the model fit for FCI accuracy and TIADL speed in comparison to the unconditional models that included only the linear and quadratic trends for time.
Table 2.
Summary of Conditional Mixed Effects Models for Speed and Accuracy of Task Completion on Measures of Everyday Function.
| Financial Task Accuracy | Financial Task Speed | TIADL Accuracy | TIADL Speed | UFOV Risk Category | RST Speed | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Effect | Estimate | SE | Estimate | SE | Estimate | SE | Estimate | SE | Estimate | SE | Estimate | SE |
| Fixed effects | ||||||||||||
| Intercept | 130.29*** | 1.61 | 0.31*** | 0.02 | 28.53*** | 0.12 | 85.27*** | 7.56 | 1.47*** | 0.12 | 3.29*** | 0.26 |
| Time | −0.52 | 1.09 | −0.01 | 0.01 | 0.05 | 0.05 | 7.49 | 6.68 | −0.07 | 0.04 | −0.01 | 0.09 |
| Time2 | 0.10 | 0.31 | — | — | — | — | −1.21 | 1.82 | — | — | — | — |
| Age | −0.53*** | 0.14 | 0.01*** | 0.00 | −0.02* | 0.01 | 2.35*** | 0.60 | 0.04*** | 0.01 | 0.10*** | 0.02 |
| Diagnosisa | −12.10*** | 2.28 | 0.09** | 0.03 | −0.59** | 0.17 | 59.88*** | 10.76 | 0.90*** | 0.15 | 1.18** | 0.36 |
| Diagnosisa × Time | 3.23* | 1.62 | 0.02 | 0.01 | −0.10 | 0.08 | −30.42** | 10.24 | 0.02 | 0.06 | 0.34* | 0.14 |
| Diagnosisa × Time2 | −1.63** | 0.47 | — | — | — | — | 12.01*** | 2.83 | — | — | — | — |
Notes.
Cognitively normal peers were the reference group.
Abbreviations: FCI, Financial Capacity Instrument; UFOV, Useful Field of View; TIADL, Timed Instrumental Activities of Daily Living; RST, Road Signs Test; Diagnosis, Baseline Diagnosis. Age was centered at the mean, 69.57 years. The values represented in the Diagnosis row are the baseline differences in intercept for participants with MCI relative to controls on each task. Time2 refers to the rate of change over time.
p<.05, two tailed;
p<.01, two tailed;
p<.001, two tailed.
Main effects of Age and Diagnosis
Older age and a diagnosis of MCI at baseline were associated with reduced performance on all measures of speed and accuracy of everyday task performance. Figure 1 displays the predicted trajectories of change on all measures of everyday function for the MCI group and cognitively normal peers. Figure 1 depicts that individuals with MCI performed worse on measures of TIADL accuracy, obtained significantly worse UFOV risk category scores, and were slower on timed financial tasks at baseline. This difference was maintained across the four annual follow-up visits with no appreciable changes in financial task speed (Figure 1A), TIADL accuracy scores (Figure 1D), or UFOV risk categories (Figure 1F) over time.
Figure 1.
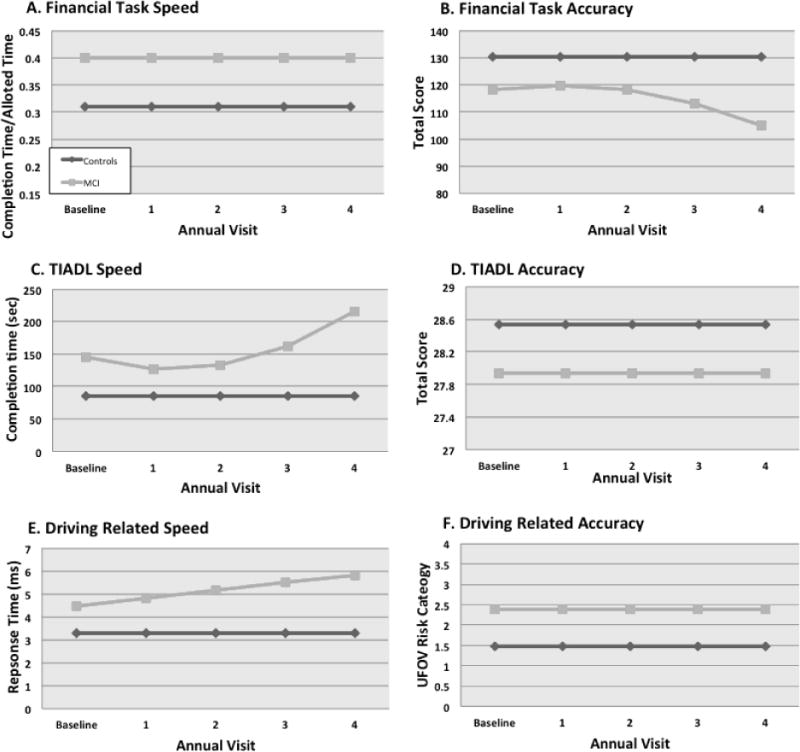
A–F. Estimated longitudinal trajectories of change in speed and accuracy of performance on measures of everyday function.
Notes. Financial task speed and accuracy measured with four domains of the Financial Capacity Instrument; TIADL, Timed Instrumental Activities of Daily Living; Driving related speed measured with Road Signs Test; Driving related accuracy measured with the Useful Field of View Risk Categories; Values are derived from linear mixed-effects models of the complete sample (n=160) adjusted for significant factors including age, time, baseline diagnosis, baseline diagnosis × time interaction, and baseline diagnosis × time2 interaction. Age was centered at the mean, 69.57 years. For speed measures (A, C, E), higher scores indicate slower performance. For accuracy measures (B, D), higher scores indicate better performance, while for UFOV Risk (F) higher scores indicate greater driving risk.
Interactions of Diagnosis and Time
There was a significant interaction between time and baseline diagnosis for models of RST speed suggesting that individuals with MCI performed increasingly slowly on the RST over time while cognitively normal controls remained relatively stable (Figure 1E).
The Baseline Diagnosis × Time and Baseline Diagnosis × Time2 interactions were significant for models of financial task accuracy (Figure 1B) and TIADL time (Figure 1C), showing that individuals with MCI perform worse over time on financial task accuracy and speed of TIADL task completion, respectively. Additionally, participants with MCI experienced an accelerated rate of decline on these tasks over the four annual follow-up visits. In contrast, financial task accuracy and TIADL speed remained relatively stable for cognitively normal controls over time.
Sensitivity Analyses
Sensitivity analyses were conducted using only individuals whose first and last available ADRC diagnosis indicated that they were a stable healthy control (n=58) or had stable/declining MCI (n=63), to ensure robust group classification. These results confirmed the findings from models using the full sample, with no appreciable differences in the magnitude, valence, and significance of results (data not shown).
CONCLUSIONS
The primary finding of this study is that older adults with MCI perform worse than cognitively normal peers on measures of speed and accuracy of everyday function, with significantly steeper rates of decline on select measures. The results confirm our hypothesis that individuals with MCI would have steeper rates of decline on all three domains of everyday functioning; however, the results were not uniform across domains. Individuals with MCI had steeper rates of decline than control participants on measures of financial task accuracy, TIADL speed, and RST speed. The results of this longitudinal study extend previous findings from cross- sectional studies of speed and accuracy of TIADL in which individuals with MCI performed comparably to cognitively normal peers on measures of accuracy but worse on measures of speed.9 It is likely that the relatively larger sample size of the current analyses provided sufficient power to detect baseline differences in accuracy of financial task performance between those with MCI and cognitively healthy peers. These results confirm that everyday tasks that require sustained attention and information processing speed take longer for persons with MCI to accomplish successfully, and this disparity in task completion time increases over time for common everyday tasks and driving-related skills represented by TIADL speed and RST speed, respectively. Our results provide partial support for the idea that differences and changes in speed, rather than accuracy, on instrumental activities of daily living and driving-related behaviors are more sensitive markers of decline in persons with MCI.
Contrary to our hypothesis, our results did not show significant group differences in longitudinal changes in speed and accuracy on all tasks of functional abilities.. While measures of speed of driving skills (RST) and TIADL showed significant declines over time, the comparable markers of accuracy of driving skills (UFOV Risk Category) and TIADL did not. Similarly, the rate of decline for accuracy on financial tasks accelerated with time, but speed on these tasks remained stable over time for individuals with MCI.
This pattern of results illustrates a striking trade-off between speed and accuracy of performance on measures of functional abilities that preferentially affected those with MCI in this study.25 The speed-accuracy trade-off (SAT) theorizes that speed and accuracy for cognitive processes, such as visual scanning, are interdependent. Due to limited rate of information flow, the faster one responds, the more errors one is prone to make. Conversely, the more one tries to be accurate, the more likely one is to reduce speed of performance.34, 35 Our results illustrate that persons with MCI are more vulnerable to SAT effects than cognitively healthy peers. Although the speed of financial task performance did not change significantly over time either for those with MCI or cognitively healthy peers, accuracy of performance significantly declined over time for those with MCI but not for cognitively healthy peers. In other words, individuals with MCI maintained their speed on financial tasks over time, but this likely compromised their accuracy on financial tasks, with steeper rates of decline. This SAT phenomenon was also evidenced by the performance patterns on measures of driving abilities and TIADL. Consequently, an evaluation of both speed and accuracy on measures of functional abilities is critical to understand the subtle functional deficits and changes in functional efficiency that are characteristic of individuals with MCI.
Measures of both speed and accuracy of everyday task performance are valuable indicators of functional change in MCI, and they may improve the sensitivity of routine cognitive screenings to detect MCI and associated functional changes that restrict patient independence. Early and accurate detection of MCI is currently limited by the lack of consensus/standards for assessing IADL restriction in older adults and those with MCI, by subclinical presentation of functional deficits, and by underreporting of IADL difficulties by patients and caregivers.18, 19 The inclusion of longitudinal assessments of speed and accuracy of everyday task performance holds promise for improving our ability to detect and monitor functional changes in MCI and may serve as meaningful outcomes for intervention trials.
Early detection of MCI provides a strategic intervention point in the clinical management of functional sequelae and might help delay progression to impairment.36 Promising research demonstrates the feasibility of cognitive training for improved speed of information processing in older adults that may benefit everyday function. 37, 38 Furthermore, clinicians should routinely monitor patients with MCI for declines in financial skills, IADL and driving abilities and provide patients and their families with clinical guidance on these issues, as well as strategies to accommodate significant declines in speed and/or accuracy. Patient recommendations may be optimized by addressing the speed/accuracy trade-offs to which patients with MCI are more susceptible than persons experiencing normal cognitive aging. In particular, our results highlight the value of providing recommendations to accommodate situations in which increased task completion time or reduced accuracy might jeopardize functional independence. For example, individuals with MCI may benefit from extended time to perform certain tasks that represent critical activities such as handling finances. They also may benefit from an explanation of the speed/accuracy trade-off and how this could necessitate a reduction in the number of tasks completed during a day. Simple early interventions such as these that target functional losses may promote patient independence, reduce caregiver burden, and improve overall quality of life.
It is important to note that our study utilized a relatively modest sample size that may have resulted in conservative estimates of trajectories of change on tasks of everyday performance across groups. In addition, the use of rolling recruitment resulted in fewer observations at later follow-up visits, potentially biasing our results toward the null. Although our sample included a range of education levels, generalizability may be limited to older adults with higher education. Further research is needed to expand the generalizability of our findings to more diverse populations, including different subtypes of MCI. The majority of participants enrolled in this study were classified as having amnestic MCI. A valuable extension of our current research would be to examine differential rates of functional decline across MCI subtypes, particularly among those with primary nonamnestic deficits who likely represent etiologies other than or in addition to AD.
The current study utilized validated performance-based tasks to assess financial abilities, TIADL, and driving skills. However, future studies may benefit from including naturalistic assessment of everyday activities in MCI.39 In particular, measures of processing speed have been found to be unique predictors of everyday function directly observed in a naturalistic environment, but not necessarily of performance-based measures or informant report of IADL.40 Therefore, naturalistic assessment may enhance our understanding of speed and accuracy on everyday activities in individuals with MCI. The results of this study suggest that clinicians and patients may benefit from routine monitoring of speed and accuracy of functional change in older adults and persons with MCI. Patient recommendations may be optimized by addressing individual discrepancies between speed and accuracy. Earlier and more accurate detection of functional change in MCI may provide an opportunity to implement strategic interventions to improve both speed and accuracy in accomplishing tasks of everyday functioning, and thereby, promote independence.
Acknowledgments
Funding Source: This research was supported by grants from the National Institute on Aging to the UAB Alzheimer Disease Research Center, P50 AG16582, and the UAB Edward R. Roybal Center, P30 AG022838.
Grant Support: This research was supported by grants from the National Institute on Aging (Alzheimer Disease Research Center), P50 AG16582, and the Edward R. Roybal Center, P30 AG022838.
Sponsor’s Role: Research reported in this publication was supported by the National Institute on Aging of the National Institutes of Health. The NIA played no role in the design, methods, subject recruitment, data collections, analysis and preparation of paper. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflicts of Interest and Source of Funding: H. Randall Griffith provides expert testimony. Karlene Ball holds stock in the Visual Awareness Research Group (formerly Visual Awareness, Inc.), and Posit Science, Inc., the companies that market the Useful Field of View Test and speed of processing training software. Posit Science acquired Visual Awareness, and Dr. Ball continues to collaborate on the design and testing of these assessment and training programs as a member of the Posit Science Scientific Advisory Board. Daniel C. Marson provides expert testimony. Daniel C. Marson is the inventor of the Financial Capacity Instrument (FCI), a form of which was used in this paper. He does not receive royalties.
Author Contributions
All authors made 1) substantial contributions to conception and design, or acquisition of data, or analysis and interpretation of data; 2) drafting the article or revising it critically for important intellectual content; and 3) final approval of the manuscript to be submitted and published.
Caroline L. Lassen-Greene: Draft of manuscript, critical revisions for important intellectual content, analysis and interpretation of data
Kayla Steward: Analysis and interpretation of data, critical revisions of article for important intellectual content
Ozioma Okonkwo: Acquisition of data, analysis and interpretation, critical revisions for important intellectual content
Ellen Porter: Acquisition of subjects and data, critical revisions for important intellectual content
Michael Crowe: Conception and design, analysis and interpretation of data, critical revisions for important intellectual content
David E. Vance: Analysis and interpretation of data, critical revisions for important intellectual content
H. Randall Griffith: Acquisition of subjects and data, critical revisions for important intellectual content
Karlene Ball: Conception and design, acquisition of data, critical revisions for important intellectual content
Daniel C. Marson: Conception and design; acquisition of subjects and data; critical revisions for important intellectual content
Virginia G. Wadley: Conception and design; acquisition of subjects and data; analysis and interpretation of data; critical revisions for important intellectual content
References
- 1.Langa KM, Levine DA. The diagnosis and management of mild cognitive impairment: a clinical review. JAMA. 2014;312(23):2551–2561. doi: 10.1001/jama.2014.13806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tuokko H, Morris C, Ebert P. Mild cognitive impairment and everyday functioning in older adults. Neurocase. 2005;11(1):40–47. doi: 10.1080/13554790490896802. [DOI] [PubMed] [Google Scholar]
- 3.Farias ST, Mungas D, Reed BR, et al. MCI is associated with deficits in everyday functioning. Alzheimer Dis Assoc Disord. 2006;20(4):217–223. doi: 10.1097/01.wad.0000213849.51495.d9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peres K, Chrysostome V, Fabrigoule C, et al. Restriction in complex activities of daily living in MCI: impact on outcome. Neurology. 2006;67(3):461–466. doi: 10.1212/01.wnl.0000228228.70065.f1. [DOI] [PubMed] [Google Scholar]
- 5.Okonkwo O, Griffith HR, Belue K, et al. Medical decision-making capacity in patients with mild cognitive impairment. Neurology. 2007;69(15):1528–1535. doi: 10.1212/01.wnl.0000277639.90611.d9. [DOI] [PubMed] [Google Scholar]
- 6.Goldberg TE, Koppel J, Keehlisen L, et al. Performance-based measures of everyday function in mild cognitive impairment. Am J Psychiatry. 2010;167(7):845–853. doi: 10.1176/appi.ajp.2010.09050692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gauthier S, Gelinas I, Gauthier L. Functional disability in Alzheimer’s disease. Int Psychogeriatr. 1997;9:163–5. doi: 10.1017/s1041610297004857. [DOI] [PubMed] [Google Scholar]
- 8.Schmitter-Edgecombe M, Woo E, et al. Characterizing multiple memory deficits and their relation to everyday functioning in individuals with mild cognitive impairment. Neuropsychology. 2009;23(2):168– 177. doi: 10.1037/a0014186. [DOI] [PubMed] [Google Scholar]
- 9.Wadley VG, Okonkwo O, Crowe M, et al. Mild cognitive impairment and everyday function: evidence of reduced speed in performing instrumental activities of daily living. Am J Geriatr Psychiatry. 2008;16(5):416–424. doi: 10.1097/JGP.0b013e31816b7303. [DOI] [PubMed] [Google Scholar]
- 10.Pereira FS, Yassuda MS, Oliveira AM, et al. Profiles of functional deficits in mild cognitive impairment and dementia: benefits from objective measurement. J Int Neuropsychol Soc. 2010;16:297–305. doi: 10.1017/S1355617709991330. [DOI] [PubMed] [Google Scholar]
- 11.Griffith HR, Belue K, Sicola A, et al. Impaired financial abilities in mild cognitive impairment. Neurology. 2003;60:449–457. doi: 10.1212/wnl.60.3.449. [DOI] [PubMed] [Google Scholar]
- 12.Sherod MG, Griffith HR, Copeland J, et al. Neurocognitive predictors of financial capacity across the dementia spectrum: normal aging, mild cognitive impairment, and Alzheimer’s disease. J Int Neuropsychol Soc. 2009;15:258–67. doi: 10.1017/S1355617709090365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yeh YC, Lin KN, Chen WT, et al. Functional disability profiles in amnestic mild cognitive impairment. Dement Geriatr Cogn Disord. 2011;31:225–32. doi: 10.1159/000326910. [DOI] [PubMed] [Google Scholar]
- 14.Wadley VG, Crowe M, Marsiske M, et al. Changes in everyday function among individuals with psychometrically defined Mild Cognitive Impairment in the Advanced Cognitive Training for Independent and Vital Elderly Study. J Am Geriatr Soc. 2007;55:1192–1198. doi: 10.1111/j.1532-5415.2007.01245.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Triebel KL, Martin R, Griffith HR, et al. Declining financial capacity in mild cognitive impairment: A 1-year longitudinal study. Neurology. 2009;73(12):928–934. doi: 10.1212/WNL.0b013e3181b87971.j. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tabert MH, Albert SM, Borukhova-Milov L, et al. Functional deficits in patients with mild cognitive impairment: prediction of AD. Neurology. 2002;58:758–764. doi: 10.1212/wnl.58.5.758. [DOI] [PubMed] [Google Scholar]
- 17.Jekel K, Damian M, Wattmo C, et al. Mild cognitive impairment and deficits in instrumental activities of daily living: a systematic review. Alzheimers Res Ther. 2015;7(1):17. doi: 10.1186/s13195-015-0099-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Okonkwo OC, Wadley VG, Griffith HR, et al. Awareness of deficits in financial abilities in patients with mild cognitive impairment: going beyond self-informant discrepancy. Am J Geriatr Psychiatry. 2008;16:650–9. doi: 10.1097/JGP.0b013e31817e8a9d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Albert SM, Michaels K, Padilla M, et al. Functional significance of Mild Cognitive Impairment in elderly patients without a dementia diagnosis. Am J Geriatr Psychiatry. 1999;7:213–220. doi: 10.1097/00019442-199908000-00005. [DOI] [PubMed] [Google Scholar]
- 20.Petersen RC, Smith GE, Waring SC, et al. Mild cognitive impairment: clinical characterization and outcome. Arch Neurol. 1999;56:303–308. doi: 10.1001/archneur.56.3.303. [DOI] [PubMed] [Google Scholar]
- 21.Jurica PJ, Leitten CL, Mattis S. Dementia Rating Scale. 2nd. Lutz, Florida: Psychological Assessment Resources; 2001. [Google Scholar]
- 22.Yesavage J. Geriatric depression scale. Psychopharmacol Bull. 1988;24:709–713. [PubMed] [Google Scholar]
- 23.Ferris FL, Kassoff A, Bresnick GH, et al. New visual acuity charts for clinical research. Am J Ophthalmol. 1982;94:91–96. [PubMed] [Google Scholar]
- 24.Marson DC, Sawrie SM, Snyder S, et al. Assessing financial capacity in patients with Alzheimer Disease: a conceptual model and prototype instrument. Arch Neurology. 2000;57(6):877–84. doi: 10.1001/archneur.57.6.877. [DOI] [PubMed] [Google Scholar]
- 25.Okonkwo O, Wadley VG, Griffith HR, et al. Cognitive correlates of financial abilities in mild cognitive impairment. J Am Geriatr Soc. 2006;54:1745–1750. doi: 10.1111/j.1532-5415.2006.00916.x. [DOI] [PubMed] [Google Scholar]
- 26.Owsley C, Sloane M, McGwin G, et al. Timed instrumental activities of daily living tasks: relationship to cognitive function and everyday performance assessments in older adults. Gerontology. 2002;48:254–265. doi: 10.1159/000058360. [DOI] [PubMed] [Google Scholar]
- 27.Ball K, Owsley C. The useful field of view test: a new technique for evaluating age-related declines in visual function. Journal of the American Optometric Association. 1993;64(1):71–79. [PubMed] [Google Scholar]
- 28.Ball K, Owsley C. Increasing mobility and reducing accidents of older drivers. In: Schaie KW, Pietrucha M, editors. Mobility and Transportation in the Elderly. New York, NY: Springer Publishing Co Inc; 2000. pp. 213–251. [Google Scholar]
- 29.Owsley C, Ball K, McGwin G, Jr, et al. Visual processing impairment and risk of motor vehicle crash among older adults. JAMA. 1998;279:1083–1088. doi: 10.1001/jama.279.14.1083. [DOI] [PubMed] [Google Scholar]
- 30.Edwards JD, Vance DE, Wadley VG, et al. Reliability and validity of useful field of view test scores as administered by personal computer. J Clin Exp Neuropsychol. 2005;27:529–43. doi: 10.1080/13803390490515432. [DOI] [PubMed] [Google Scholar]
- 31.Wood JM, Chaparro A, Lacherez P, et al. Useful field of view predicts driving in the presence of distracters. Optom Vis Sci. 2012;89(4):373–381. doi: 10.1097/OPX.0b013e31824c17ee. [DOI] [PubMed] [Google Scholar]
- 32.Willis SL, Tennstedt SL, Marsiske M, et al. Long-term effects of cognitive training on everyday functional outcomes in older adults. JAMA. 2006;296(23):2805–2814. doi: 10.1001/jama.296.23.2805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Laird NM, Ware JH. Random-effects models for longitudinal data. Biometrics. 1982;38(4):963–974. [PubMed] [Google Scholar]
- 34.Dutilh G, Wagenmakers EJ, Visser I, et al. A phase transition model for the speed-accuracy trade-off in response time experiments. Cogn Sci. 2011;35(2):211–250. doi: 10.1111/j.1551-6709.2010.01147.x. [DOI] [PubMed] [Google Scholar]
- 35.Chen B, Perona P. Speed versus accuracy in visual search: Optimal performance and neural architecture. J Vis. 2015;15(16):9. doi: 10.1167/15.16.9. [DOI] [PubMed] [Google Scholar]
- 36.Burns A, Zaudig M. Mild cognitive impairment in older people. Lancet. 2016;360(9349):1963–1965. doi: 10.1016/S0140-6736(02)11920-9. [DOI] [PubMed] [Google Scholar]
- 37.Ross LA, Edwards JD, O’Connor ML, et al. The transfer of cognitive speed of processing training to older adults’ driving mobility across 5 Years. J Gerontol B Psychol Sci Soc Sci. 2015:1–11. doi: 10.1093/geronb/gbv022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Willis SL, Tennstedt SL, Marsiske M, et al. Long-term effects of cognitive training on everyday functional outcomes in older adults. JAMA. 2006;296:2805–2814. doi: 10.1001/jama.296.23.2805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schmitter-Edgecombe M, Parsey CM. Assessment of functional change and cognitive correlates in the progression from healthy cognitive aging to dementia. Neuropsychology. 2015;28(6):881–893. doi: 10.1037/neu0000109.Assessment. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Seelye AM, Schmitter-Edgecombe M, Cook DJ, et al. Naturalistic assessment of everyday activities and prompting technologies in mild cognitive impairment. J Int Neuropsychol Soc. 2013;19(04):442–452. doi: 10.1017/S135561771200149X. [DOI] [PMC free article] [PubMed] [Google Scholar]


