Abstract
Self-ear cleaning is the insertion of objects into the ear canal to clean it, a widespread practice that has the potential to compromise its integrity as a natural, selfcleansing mechanism, and a risk factor for possible injuries. The practice is common among young adults and highest in university than any other graduates. This study aimed to determine the self-ear cleaning practices and associated risk of injury and related symptoms in undergraduate students at KwaZulu-Natal University. The descriptive survey utilized a self-administered questionnaire. Of the 206 participants that responded, 98% engaged in self-ear cleaning, with 75% indicating that it was beneficial. The commonest method (79.6%) being the use of cotton buds, with an associated injury rate of 2.4%. There was no statistically significant associations between those who used or did not use cotton buds and the symptoms experienced. The complications indicate that self-ear cleaning does pose a risk for injury, necessitating more community information and education.
Key words: Self-ear cleaning, ear injury, ear related symptoms, cotton buds, benefit, risk
Introduction
Self-ear cleaning is a widespread practice that has the potential to compromise the integrity of the ear as a natural, self-cleansing mechanism.1-3 The general consensus in the medical community is that the practice is pervasive.4 In developing regions, the morbidity and mortality associated with ear disease and injuries remain a significant but neglected public health problem.5 Self-ear cleaning is described as the insertion of objects into the ear canal to clean it due to the belief that for ear hygiene it is necessary to remove the excess cerumen,1,6 or that cerumen is perceived as a cosmetic nuisance, 7 its presence being an indication for removal.8
The external auditory meatus has the ability to clean itself, which is made possible by the cleansing function of cerumen, a naturally occurring substance that cleans, protects and lubricates the external auditory canal.1 It is usually unnecessary to clean the ear canal, as excessive cleaning increases humidity and softens the ear canal lining, which can result in infection and irritation of the ear that can cause changes to the skin lining and thereby impair normal functioning. 9,10
Cerumen, with its content of lysosomes, glycoproteins, immunoglobulins, lipids and trace elements, has a bactericidal action that plays a significant role in maintaining the local host defence mechanism in the ear.11 It has a high acidic pH (about 4 to 5), which is unfavourable for organisms and helps reduce the risk of infection in the auditory canal.7 It constantly migrates towards the outer part of the external auditory canal, this being assisted by jaw movement.12 Foreign materials adhere to the cerumen, thus preventing it from plugging the ear or reaching the tympanic membrane,11 a process that makes cleaning the ear canal unnecessary.13 An unprofessional attempt to clean the ear canal or habitual wax removal is a potential risk for ear related symptoms and injuries, including pain, earache, bleeding, tympanic membrane perforations and weakening of the external auditory canals local defence against bacterial and fungal infections.2 The risk is even greater when this is done as a blind procedure without direct inspection of the ear canal using objects not designed to remove wax and foreign bodies in the ear, such as cotton buds and loose tip cotton swabs, feathers, sticks and a variety of other objects.2,5
Many individuals do produce an excessive amount of cerumen that builds up over time and may become impacted, thus obstructing the flow of sound to the eardrum.14 This can result in various symptoms, including but not limited to itchiness, pain, irritation and hearing difficulty, thereby perpetuating the desire to clean the ear.4 The prevalence of cerumen impaction is about 6% in the general population1,15 and in young adults aged 21-30 years is estimated to be at approximately 17.6%.5 However, both the lack of public awareness regarding the availability of treatment options and the lack of active practice by health professionals has resulted in an increase in self-ear cleaning practice.15
There is poor awareness about the risks associated with self-ear cleaning as well as the function of wax within the ear. Studies conducted in Nigeria indicated that 93.4% of young educated adults performed self-ear cleaning, and related the perceived benefit to removing that wax, which they regarded as dirt in the ear canal.1,7,2 The other reasons cited include itchiness, to reduce pain, improve hearing, soothing and for cosmetic appeal5. Injuries and associated symptoms relating to ear-cleaning practices are largely preventable if the public is educated appropriately in the area of self-ear cleaning and its associated risk factors.1 Oladeji et al.16 emphasize the need for medical education of health workers and health education for the general public to improve their understanding of caring for the ear and the dangers of self-ear cleaning. However, other practitioners argue that cotton bud injuries are over stated.17 Evidence derived from research into how adults, particularly young adults, clean their ears, the factors influencing self-ear cleaning and if they experience ear related symptoms or injury could facilitate education programmes. The association between ear cleaning and ear injury has not been conclusively demonstrated, and few studies have rigorously addressed the issue, necessitating more research in this area.1,4 The aim of the study was therefore to determine self-ear cleaning practices (Objective 1) and the associated risk of ear injuries and ear-related symptoms (Objective 2) in a group of undergraduate health science students at the University of KwaZulu-Natal.
Materials and Methods
A descriptive survey design with quantitative methods of analysis was employed, and all first to final year undergraduate students in the School of Health Sciences at the University of KwaZulu-Natal, irrespective of gender or ethnicity, were invited to participate. Convenience sampling was used, with participants being selected based on accessibility, availability, flexibility and feasibility.18 The students were registered in the disciplines of Pharmacy, Speech Language Pathology, Optometry, Physiotherapy, Occupational Therapy, Dental Therapy and Sports Science, while those in Audiology were excluded from the main study, given their prior knowledge about ear care and hygiene practices.
A power calculation was conducted using a 5% margin of error and a confidence of 95%, with a sample size of 284 students (approximately 20% of the total students registered in the School of Health Sciences) being required, of which, 206 replied, yielding a response rate of 73%. Ethics approval (SHSREC 015/15) was obtained from the University of KwaZulu-Natal’s School of Health Sciences Research Ethics committee and all ethical principles were adhered to.
A self-administered questionnaire was used that was adapted from Olaosun1 and Amutta et al.2 and included other questions based on a perusal of recent literature. The questionnaire consisted of 25 questions, including open-ended, closed-ended and multiple choice response questions. Participants were given an information document and a consent form with the questionnaire after obtaining gatekeeper access from the relevant personnel at the university. Collection boxes were placed in the respective disciplines into which the completed questionnaires were placed. Participants were given five days to complete the questionnaire, after which a reminder was sent and an additional five days given in an attempt to improve the response rates. In order to ensure reliability and validity of the questionnaire, a pilot study was conducted on 10 audiology students to improve its face/content validity. Questions used in other published studies were incorporated to improve the validity of the questionnaire.
The Statistical Package for the Social Sciences (SPSS) version 21 programme was used to analyze the data with the assistance of two statisticians. Descriptive statistics were applied to analyse the questions relating to the frequency of cleaning the ear, the approximate duration of self-ear cleaning, the reasons of self-ear cleaning, the methods used and the parts of the ear being cleaned. Inferential statistics was applied to determine the level of significance between the means of the various groups (disciplines) as a whole by applying the one-way ANOVA test. The relationship/association between the methods used for self-ear cleaning and symptoms experienced, gender differences related to the frequency of ear cleaning and the relationship between ethnicity and the perception of benefit was analysed using the Chi Squared test (Pearson and Fisher Exact), with a significance of 5%.
Results
The results are presented for the 206 respondents with respect to the two objectives of the study. The average age ranged from 20-21 years old, with the majority being female (158, 76.6%) and 48 (23.4 %) being male, yielding a ratio of 3:1. The study included participants of different ethnicities, with the majority (95, 46.1%) being Black African, followed by Indian students (81, 39.3%). There was an equal representation of participants from first to final year of study. The majority of participants were from the disciplines of Physiotherapy (19.9%), Speech Therapy (18%), Occupational Therapy and Pharmacy (17.5%).
Objective 1: To determine self-ear cleaning practices of health sciences university students
This objective focussed on the perception of benefit, ownership of cotton buds, parts of the ear cleaned and frequency of ear cleaning, the influence of family members with regards to self-ear cleaning, and the reasons and methods used to clean the ear. The majority (n=201, 98%) of the 206 participants practice self-ear cleaning, of whom, 75%, (n=115) perceived this to be beneficial. Some participants believed that self-ear cleaning is non-beneficial and may even be harmful (Figure 1).
Figure 1.
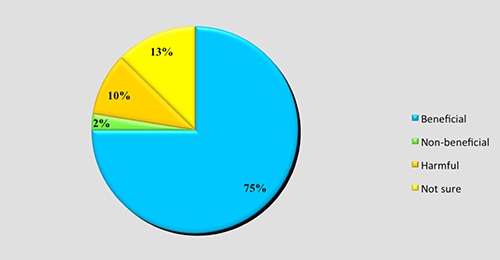
Participants’ perceptions towards self-ear cleaning.
Regarding their ownership of cotton buds, the responses revealed that 80% (n= 165) did own some, with 14.1% (n=29) indicating that they carry some with them. With respect to the part of their ear they clean, 17.5% (n=36) indicated that they clean outside of the ear only, 7.3% (n=15) cleaned inside only, while 75.2% (n=155) cleaned both inside and outside their ear canal. There was a statistically significant result between the groups means of the different disciplines (P=0.014). When participants were required to state the frequency with which they practice self-ear cleaning, 32% (n=66) reported doing so once a day and 27% (n=55) cleaned them once a week (Figure 2).
Figure 2.
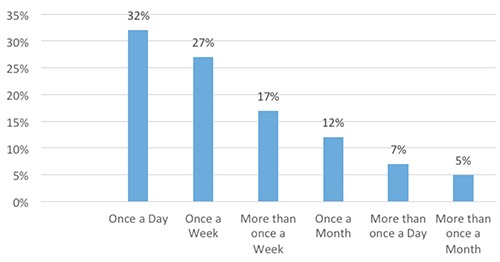
Frequency of self-ear cleaning.
Of the 206, 90.2% (n=184) stated that their siblings engaged in self-ear cleaning, among whom 84.3% (n=172) used cotton buds. It was also found that 93.2% (n=192) of their parents practice self-ear cleaning, of whom 87.9% (n=184) used ear-buds. For the parents’ self-ear cleaning practices, a statistically significant difference between the groups means as a whole was found (P=0.016). Within this context, 74.8% (n=154) participants stated that they had learned self-ear cleaning from a family member, and started in their childhood. Additional sources included friends, the internet, general practitioner and ENT specialists.
When considering the reasons for selfear cleaning, many participants indicated more than one reason, thus 275 responses were obtained (Figure 3), the main one being due to wax 36% (n=99) and dirt 31% (n=85), followed by itchiness and the fact that it was soothing.
Figure 3.
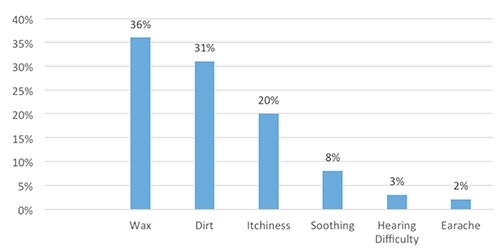
Reasons for practicing self-ear cleaning.
The most common method amongst the university students across disciplines were cotton buds (65%) (Figure 4). This was followed by the use of a towel/hanky, (20%) while other methods included cleaning with the finger, matchstick and a hairpin. Some participants used more than one method to clean their ears.
Figure 4.
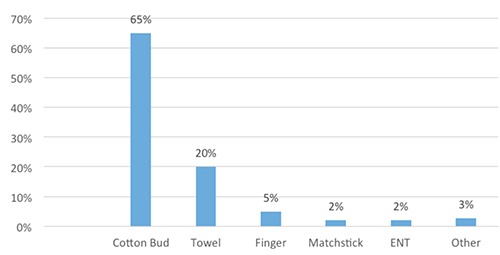
Methods of self-ear cleaning.
Objective 2: To determine the associated risk of ear injuries and earrelated symptoms
This objective focussed on the ear injuries and ear related symptoms experienced, the relationship between users and non-users of cotton buds, the symptoms experienced and where the participants seek help with the above. A large number of participants (n=154, 74.7%) stated that they understood that self-ear cleaning can damage the eardrum/ ear, whilst 24.5% (n=50) said that no damage will occur. Of the 206 participants, five (2.4%) stated they experienced ear related injuries, with two having experienced perforated tympanic membranes, of whom one required tympanoplasty. Three participants experienced lacerations and ear infections, with all stating that their injuries were due to cotton buds being inserted into the ear. About 154 (74.7%) indicated that they had experienced some ear related symptoms due to self-cleaning, while 25.2% (n=52) had not. The leading symptoms found in participants were itchiness (n=85/137, 62%), earache (n=73/128, 57%), feeling of fullness in the ear (n=39/102, 38.2%), followed by tinnitus, hearing difficulty and ear discharge (Figure 5).
Figure 5.
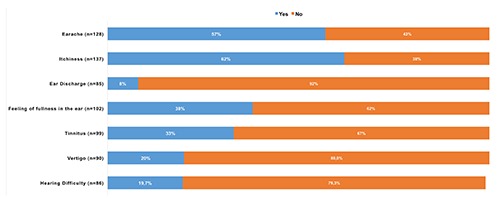
Ear related symptoms experienced by participants.
The relationship between those who used cotton buds and symptoms experienced, and those that did not use cotton buds and the symptoms experienced were determined using the Chi squared test. The Pearson Chi Squared test revealed no statistically significant association between the use of cotton buds and symptoms experienced between users and non-users. (Table 1). However the symptoms appear to be more prevalent in those that used cotton buds versus those that did not use cotton buds to clean their ears. Some the participants had sought some form of intervention, with the professional most consulted being audiologist, followed by an ENT specialist and general practitioner
Table 1.
Symptoms experienced by cotton bud users and non-users.
| Symptoms* | Use cotton buds | Not use cotton buds | Total | X2 | P value | Significant |
|---|---|---|---|---|---|---|
| Earache | 60 (82%) | 13 (18%) | 73/128 | 1.221 | 0.269 | No |
| Itchiness | 69 (81%) | 16 (19%) | 85/137 | 0.001 | 0.970 | No |
| Ear discharge | 7 (71%) | 2 (29%) | 9/85 | - | 1.000 | No |
| Feeling of fullness | 29 (74%) | 10 (16%) | 39/102 | 0.042 | 0.837 | No |
| Tinnitus | 25 (76%) | 8 (24%) | 33/99 | 1.635 | 0.210 | No |
| Vertigo | 12 (67%) | 6 (33%) | 18/90 | - | 0.087 | No |
| Hearing difficulty | 15 (88%) | 2 (12%) | 17/86 | - | 0.741 | No |
*Symptoms 3, 6 and 7 (Fishers Exact test) one cell had an expected count of less than 5; Symptoms 1, 2, 4, and 5 (Pearson Chi Squared test).*Symptoms 3, 6 and 7 (Fishers Exact test) one cell had an expected count of less than 5; Symptoms 1, 2, 4, and 5 (Pearson Chi Squared test).
Discussion
The findings of the current study are consistent with others cited in the literature, which report a prevalence of over 90% for self-ear cleaning.1,3,7 Amutta et al.2 also found that self-ear cleaning was widely practiced in a community based study in all groups in Nigeria, being highest amongst young adults 21-30 years, and higher in university graduates than any other graduates1. Oladeji et al.16 also found it to be very high (94%) in health workers, which is of concern, considering that they should be practicing safe and healthy ear care methods. A study conducted with physicians in Nigeria6 showed that 76.3% of physicians practiced self-ear cleaning, mainly for reasons of hygiene. The present study also found that this practice was highly prevalent among young adults in the School of Health Sciences. As a pamphlet was distributed to the participants about safe ear care and good ear hygiene practices after they had completed the questionnaire, it is envisaged that they would now be more aware about the associated risks related to self-ear cleaning. This study revealed the need for urgent action to be taken to educate health workers and the general population about self-ear cleaning in order to prevent complications.
Self-ear cleaning was higher in those who perceived the practice to being beneficial, and was being done to remove wax, dirt and debris, itchiness and to soothe the ear.1,16,19 The reasons provided for engaging in self-ear cleaning are uniform across the various studies, although the extent to which symptoms and injuries occur differed. Most participants in this study stated that they engaged in self-ear practices due to wax, dirt and itchiness, this being similar to the study by Lee et al. (2004)3 and Gadanya et al. (2016).6 This differed from the study by Olajide et al. (2015)19 which attributed itchiness as the main reason for self-ear cleaning, while Amutta2 cited dirt, itchy ears then wax, these three reasons being consistent across the studies as main reasons.
Self-ear cleaning has been found to compromise the integrity of the ear as a self-cleansing mechanism.2 According to Afolabi et al. (2009),7 this habit needs to be discouraged, as it is a slow otologic poison, (p 43) that can lead to various risks. This suggests the need for education and information about self-ear cleaning, especially at the primary health care level, as part of health promotion and disease prevention initiatives. Doctors and nurses also need to be trained at primary health care level on wax removal and referral for more complicated cases, such as those with perforations or ear discharge.20 It is also important to iterate that ear wax is not synonymous with dirt, but is a naturally occurring substance that prevents infection and foreign bodies from entering the ear.1,5
Other studies have alluded to gender differences in the frequency of ear cleaning, with more females cleaning more frequently than males.1,16 The association between the frequency of ear cleaning and gender did not yield a statistically significant relationship in this study versus the Oladeji et al. (2015)16 study, where it was found to be highly significant (P=0.004). However, the results of the current study must be interpreted with caution, given that the female to male ratio was 3:1. The majority of participants in this study cleaned their ears quite frequently, which was also found in other studies.2,7 Furthermore, the risk for ear injury was exacerbated by the fact that the cotton buds were the main object of choice for ear cleaning, as used by majority of participants, which closely approximates the findings of the studies conducted in Nigeria1,2,16,15 and Pakistan.21
A study on 50 participants aged 15 to 74 years of age found that the majority (92%) used cotton buds to clean their ears,3 with 36% having practised self-ear cleaning daily, many doing so more than once a day, while 54% self-ear cleaned once or more in a week. In a similar study, Amutta et al. 2 found that 91.2% clean their ears with a cotton bud, 1.9% used a feather, 1.3% used a broomstick, 1.3% used their finger and 0.6% used a matchstick. In a study conducted by Adegbiji et al.5 of 385 people aged 17 years and above, 80% used objects to practice self-ear cleaning, 74.4% used soapy water during a bath, whilst only 8% had the knowledge of the ear being a self-cleaning mechanism. A possible explanation for the findings in the studies conducted in Nigeria, and other developing contexts, is that people from poor socio-economic contexts are most involved in this practice.7 These findings differ to a hospital-based study conducted by Hobson and Lavy22 in London, which showed the use of cotton buds in only 53% of participants.
Most participants had cleaned their ears since childhood, influenced by parents and siblings in developing the habit. Initiatives to modify this practice should therefore also include caregivers and parents.1,4,23 Ownership of cotton buds perpetuate the practice of self-ear cleaning, which has been shown to be is modifiable through education efforts.1 It is also reported that many people may use cotton buds without coming to harm, with the potential harm needing to be elucidated.22
In this study, five participants reported injuries, including perforations, due to the use of cotton buds, and were common reasons for patients attending ear, nose and throat referral clinics.15 Other studies also showed an injury rate of between 2-5%, including bruising and bleeding in the external auditory canal.7,20 Lee et al.3 reported a 2% injury rate in the study conducted in Malaysia, this being similar to the current study findings, while in the Ammuta et al2 study, up to 25% of participants reported complications. This current study did not include which ear was traumatized, but in the study by Adedeji,24 the right ear was at greater risk due to the right hand dominance in the majority of the population.
According to Olajide, Usman and Eletta19 74.1% of participants did not have information about the dangers of cotton bud usage in the ear and had poor knowledge about the ear as a self-cleansing mechanism. Hobson and Lavy22 stated that as many as 93% of their participants were ignorant of the harmful effects of overzealous cotton bud use. Whatever the reason for the use of the cotton bud, it can scratch, weaken and traumatize the ear canal, causing infection to set in easily.19,23
The negative effects of self-ear cleaning practices were noted in a study done by Ahmed et al.,21 were it was found that approximately 34.3% of the population experienced neurodermatitis, 28.3% otitis externa, 26.8% contact dermatitis, 8.9% impacted cerumen, and 1.5% tympanic membrane perforations. The most frequently seen ear injuries in the ENT practices are the ends of cotton buds and matchstick ends stuck in the ear canal, often inserted to relieve itchiness.25 According to Kumar and Ahmed (2008),26 cotton bud use is unnecessary and can cause some dangerous complications.
Education and information about the risks must be disseminated as widely as possible across all age groups. Amutta et al.2 indicated that while the loose tip cotton bud would be better to use to dry out the excess water after getting wet as it is more absorbent, many preferred the commonly available ones due to their aesthetic appeal. Cerumen management may be conducted by doctors, ENT specialists, audiologists and other trained health care personnel, who will advise on treatment options. A number of treatment options are also available to remove cerumen and include the use of a cerumenolytic, topical therapy, irrigation, suctioning, syringing and other manual removal techniques.27 In South Africa, approximately 36% of professionals, including audiologists, practice cerumen management14,28 compared to 87% of audiologists and 69% of medical practitioners in United States of America (USA).29
Itchiness and earache seemed to be the most common symptoms experienced because of self-ear cleaning, this being consistent with other studies.7,19,21 For the ear related symptoms experienced in this study, there was no statistically significant relationship between users of cotton buds and non-users. This suggests that while people mainly use cotton buds, they may not necessarily have any symptoms as a result of its use, but could have an increased risk of injury. However, this is not conclusive, and more research may be warranted to demonstrate the relationship between these factors. Sperling and Portney (2016)4 argue that, given the large numbers of the population that use cotton buds, the risk of injury is very low, and that rather that dissuading self-ear cleaning, practitioners should be advocating for safer use that addresses the frequency of cotton bud usage and the depth of insertion into the canal. Finally, the results obtained from this study may not be generalized to all students at the university or elsewhere.
Conclusions
Young educated adults do engage in self-ear cleaning, which can potentially increase the risk of ear injury and ear related symptoms. There needs to be more public health education to discourage people from the acts of self-ear cleaning, and to inform them about how the ear naturally cleans itself, and how to address issues of itchiness, wax impaction and so forth. It is important that cerumen management be done by qualified personnel, as removal by inexperienced persons can cause damage to the ear. The medical advice against self-ear cleaning is not widely known, this information being needed to gain insight into the above-mentioned areas so that appropriate health education, awareness and training programs may be devised.
Acknowledgements
The following students are acknowledged for their contribution to the undergraduate research project Sivashnee Thaver, Hazel Phakathi, Gcinile Shoyisa and Yusuf Suder.
References
- 1.Olaosun OA. Self-ear-cleaning among educated young adults in Nigeria. J Fam Med Primary Care 2014;3:17-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Amutta SB, Mufutau AY, Kufre RI, et al. Sociodemographic factors and prevalence of self-ear cleaning in Sokoto Metropolis. Int J Otolaryngol Head Neck Surg 2013;2:1-4. [Google Scholar]
- 3.Lee LM, Govindaraju R, Hon SK. Cotton bud and ear cleaning- a loose tip cotton bud. Med J Malaysia 2004;60: 85-8. [PubMed] [Google Scholar]
- 4.Sperling NM, Portnoy WM. To swab or not to swab: appropriate medical advice regarding self ear cleaning. Int J Head Neck Surg 2016;7:1-4. [Google Scholar]
- 5.Adegbiji WA, Alabi BS, Olajuyin OA, Nwawolo CC. Earwax impaction: symptoms, predisposing factors and perception among Nigerians. Indian J Med Res 2014;1:1-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gadanya M, Abubakar S, Ahmed A, Maje AZ. Prevalence and attitude of self-ear cleaning with cotton buds among doctors at Aminu Kano Teaching Hospital, Northwestern Nigeria. Nig J Surg Res 2016;16:2-17. [Google Scholar]
- 7.Afolabi AO, Kodiya AM, Bakari A, Ahmad BM. Attitude of self-ear cleaning in black Africans: any benefit?. East Afr J Public Health 2009;6:43-6. [DOI] [PubMed] [Google Scholar]
- 8.Sharp JF, Wilson JA, Ross L, Barr-Hamilton R.M. Ear wax removal: a survey of current practice. BMJ 1990:301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nutall T, Cole LK. Ear cleaning: The UK and US perspective. Vet Dermatol 2004;15:127-36. [DOI] [PubMed] [Google Scholar]
- 10.Poulton S, Yau S, Anderson D, Bennet D. Ear wax management. Roy Austr Coll Gen Pract 2015;44:10. [PubMed] [Google Scholar]
- 11.Oron Y, Lazar-Zwecker I, Levy D, et al. Cerumen removal: comparison of cerumenolytic agents and effect on cognition among the elderly. Archiv Gerontol Geriatr 2009;5:1-4. [DOI] [PubMed] [Google Scholar]
- 12.Roland PS, Marple BF, Mayerhoff WL. Hearing loss (2nd ed). New York: Thieme Medical Publishers, Inc.; 1997. [Google Scholar]
- 13.Beatrice F, Bucolo S, Cavallo R. Earwax, clinical practice. Am Acad Otolaryngol Head Neck Surg 2009;29:1-20. [Google Scholar]
- 14.Gelfand S. Essentials of audiology (3rd Ed). New York: Thieme Medical Publishers; 2009. [Google Scholar]
- 15.Olajide TG. Cerumen impaction: challenges and management profile in a rural health facility. Niger Med J 2015;56:390-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Oladeji SM, Babatunde OT, Adenekan AK, et al. Self-ear cleaning among health workers in Nigeria. J Dental Med Sci 2015;14:122-6. [Google Scholar]
- 17.Shakeel M, Nair S, Ahmad Z, Gordon A. Forgotten cause of ear infection: forgotten cotton buds. J Otolaryngol ENT Res 2015;3:00078. [Google Scholar]
- 18.Maxwell DL, Satake E. Research and statistical methods in communication sciences and disorders. New York: Thomson/Delmar Learning; 2006. [Google Scholar]
- 19.Olajide TG, Usman AM, Eletta AP. Knowledge, attitude and awareness of hazards associated with use of cotton bud in a Nigerian Community. Int J Otolaryngol Head Neck Surg 2015;4:248-53. [Google Scholar]
- 20.Ullauri A, Smith A, Espinel C, et al. WHO ear and hearing disorders: Ecuador National Study 2008-2009. Hindawi Publishing Corporation, Conference papers in Science, 2014. [Google Scholar]
- 21.Ahmed S, Zaheer SAI, Shabeer SMA, et al. Association of dermatological conditions of external ear with the use of cotton buds. Indian J Med Res 2014;10:1-7. [Google Scholar]
- 22.Hobson J, Lavy J. The use and abuse of cotton buds. J Roy Soc Med 2005;98: 360-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Smith M, Darrat I, Seidman M. Otologic complications of cotton swab use: one institution’s experience. Laryngoscope 2012;122:409-11. [DOI] [PubMed] [Google Scholar]
- 24.Adedeji TO, Olaosun AO, Tobih JE. An audit of otologic injuries in a Nigerian Tertiary Health Faciity. East Central Afr J Surg 2014;2014:19. [Google Scholar]
- 25.Reynolds T. Ear, nose and throat problems in accident and emergency. Natl Inst Health 2004;18:47-53. [DOI] [PubMed] [Google Scholar]
- 26.Kumar S, Ahmed S. Use of cotton buds and its complications. J Surg Pak (International) 2008;13:3. [Google Scholar]
- 27.Roland PS, Smith TL, Schwartz SR, et al. Clinical practice guideline: cerumen impaction. Am Acad Otolaryngol Head Neck Surg Found 2008;10:1-17. [DOI] [PubMed] [Google Scholar]
- 28.Biagio L, Swanepoel DW, Laurent C, Lundberg T. Paediatric otitis media at a primary healthcare clinic in South Africa. South Afr Med J 2014;8:1-4. [DOI] [PubMed] [Google Scholar]
- 29.Cilento CL. Position statement on licensed audiologists in the Commonwealth of Virginia managing cerumen (ear wax). Am Acad Otolaryngol Head Neck Surg 2012;1:2-4. [Google Scholar]


