Abstract
Condyloma acuminatum (CA) is a human papillomavirus-induced sexually transmitted disease which is characterised by epithelial proliferation in the genital region, perianal region, oral cavity and larynx. It was first reported by Knapp and Uohara in 1967. The disease is more common in children and teenagers and appears as solitary or multiple, pinkish, sessile papules or plaques with pebbled surface or as pedunculated papillary lesions. Oral lesions commonly affect the lips, floor of the mouth, lateral and ventral surfaces of tongue, buccal mucosa, soft palate and rarely gingiva. The present report deals with a case of CA affecting a 75-year-old male patient with emphasis on clinical presentation, histological features and importance of PCR for establishment of definitive diagnosis. This case is unique because CA is extremely rare in geriatric age group.
Keywords: sexual transmitted infections (viral), human papilloma virus
Background
Condyloma acuminatum (CA) is a human papillomavirus (HPV)-induced sexually transmitted disease which is characterised by epithelial proliferation in the genital region, perianal region, oral cavity and larynx.1
More than 100 subtypes of HPV have been identified out of which subtypes 6 and 11 are commonly associated with the disease though HPV 2, 53 and 54 have also been detected in some cases. Rarely, the high-risk subtypes of HPV 16 and 18 may be isolated especially from anogenital lesions.1
The incubation period of HPV is 3 weeks to 8 months.2
The first case of oral CA was reported by Knapp and Uohara in 1967.2
Oral CA can also be caused by orogenital sexual transmission or hand-to-mouth autoinoculation in adults.3
Cases of CA have been less reported than other sexually transmitted diseases like genital herpes, gonorrhoea and chlamydial infection but deserves much attention as it can affect both sexual partners, foetuses and also due to carcinogenic potential of HPV infection.4
Here, we discuss a rare case of CA affecting oral mucosa of a 75-year-old male patient. The case is unique because CA is extremely rare in the geriatric age group, and there was no history of any high-risk sexual behaviour given by the patient.
Case presentation
A 75-year-old, edentulous, male patient from urban area reported to the Department of Oral and Maxillofacial Pathology, Guru Nanak Institute of Dental Sciences & Research, Kolkata, India, with the chief complaint of difficulty in wearing denture due to presence of multiple growths of varying sizes present in the oral cavity since 15 years.
The patient was under regular medication for hypertension and hyperglycaemia and was under prophylactic antiplatelet drug.
The patient was using complete denture since 3 years. The lesions on the alveolar ridges increased in size after use of dentures. He had consulted his local dentist who referred him to our institute.
Personal history of the patient was not corroborative to any sexually transmitted disease.
Extraorally, no abnormality was detected and no regional lymphadenopathy was present.
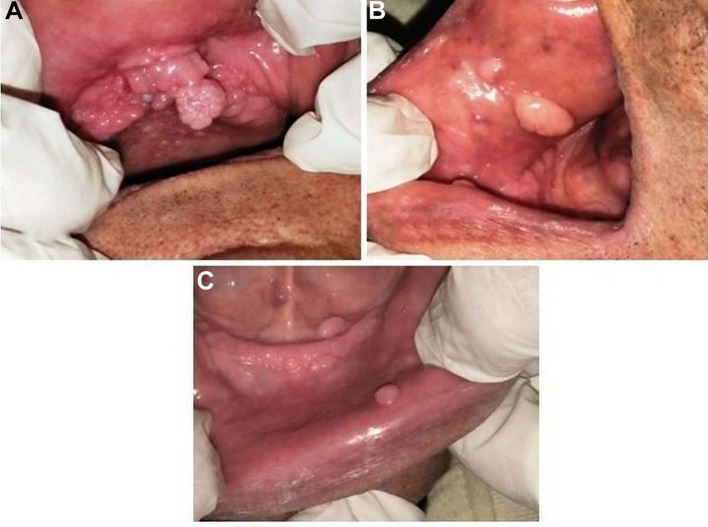
Intraoral examination revealed the presence of completely edentulous upper and lower alveolar ridges. There were multiple, soft, non-tender, non-compressible, non-reducible, non-pulsatile growths of varying sizes present all over the alveolar ridge, palate, buccal mucosa and floor of the mouth. Most of these growths showed warty appearance of the overlying mucosa (figure 1A,B,C). No dermatological or genital growth was detected on general examination of the patient.
Figure 1.
Intraoral photograph showing presence of multiple, small wart-like lesions over the (A) alveolar ridge, palate, (B) buccal mucosa and (C) floor of the mouth.
Investigations
Orthopantomogram findings were non-corroborative to the lesion.
All haematological parameters were within normal limits. Preoperative serology revealed that the patient was ELISA negative for HIV and hepatitis.
Excisional biopsy was performed from two growths—one from the papilliferous growth in the upper anterior alveolar ridge and another from a growth in the right buccal mucosa and sent for histopathological evaluation.
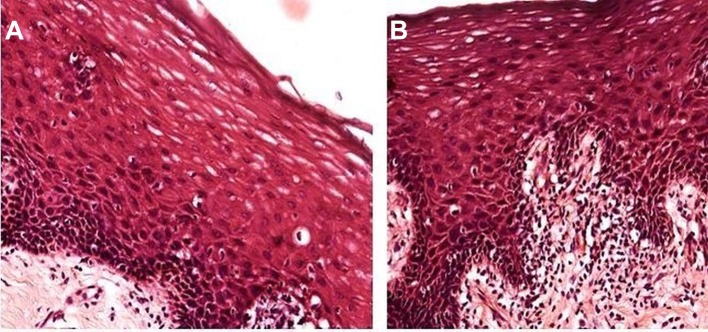
The sections stained with H&E showed the presence of parakeratinised stratified squamous epithelium supported by connective tissue cores with marked acanthosis and pseudoepitheliomatous hyperplasia (figure 2). The most striking feature was the presence of cells in the superficial cell layers which exhibited hyperchromatic nuclei with perinuclear clear zones—the koilocytes. These koilocytes were indicative of the presence of HPV infection. Presence of intense chronic inflammatory cell infiltrate was noted in the connective tissue stroma (figure 3A,B).
Figure 2.
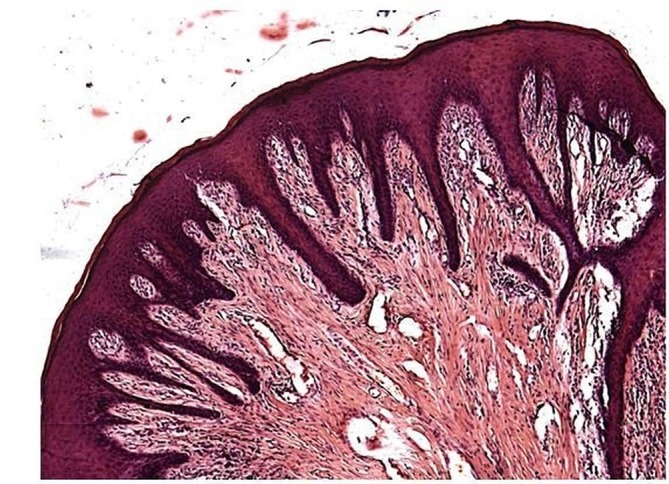
H&E stained section (x5) showing hyperplastic stratified squamous epithelium with papillary projections supported by connective tissue cores.
Figure 3.
(A,B) H&E stained sections (x20) showing ‘koilocytes’ (cells with hyperchromatic nuclei surrounded by clear halo) in the superficial layers of the epithelium.
To establish a definite diagnosis, PCR sequencing of the tissue sample was performed for detection of HPV and identification of its specific genotype. The investigation confirmed the presence of HPV genotype 6.
Differential diagnosis
The presence of wart-like lesions exhibiting pseudoepitheliomatous hyperplasia accompanied with koilocytic changes narrowed our differential diagnosis to Heck’s disease, CA or verruca vulgaris (VV).
Clinically, the lesions of Heck’s disease and CA are very similar. But a careful examination shows that the papules of Heck’s disease are flatter than those of CA. Moreover, the lesions of Heck’s disease are usually seen on the lips, tongue and buccal mucosa while those of CA are more common on the ventral tongue and floor of the mouth.5 Histologically, hyperparakeratosis and marked acanthosis of surface epithelium are noted in Heck’s disease. Since the thickened mucosa extends upwards and not down into the connective tissue, the lesional rete ridges are at the same level with adjacent normal rete ridges. The lesional rete ridges are wider, confluent and club shaped. Koilocytes and ‘mitosoid cells’ are occasionally present.1
In case of oral VV, concomitant cutaneous involvement is almost always present. Skin of the hands is commonly affected in VV.6 Presence of dermatological lesion is essential for clinically diagnosing VV, whereas skin lesions may or may not be present in case of CA. When the oral mucosa is involved in VV, the lesions are usually found on the vermilion border of lips, labial mucosa or anterior tongue in contrast to the ventral surface of the tongue and floor of the mouth in CA. Histologically, there is papillary epithelial proliferation with hyperkeratosis and prominent granular cell layer in VV. Multiple finger-like projections consist of radially oriented rete pegs which are characteristic of the lesion which are not seen in CA.7
Thus, a confirmatory diagnosis can be established by amalgamation of clinical features, histopathological evaluation and identification of the specific HPV genotype.
The presence of oral lesions in the form of elevated nodular warts having multifocal distribution without any dermatological manifestations, characteristic histopathological features and association with HPV genotype 6 confirmed the diagnosis of the case as ‘condyloma acuminatum’.
Treatment
Treatment modalities are aimed at elimination of as many visible lesions as possible. Excision of the lesions can be performed by simple scalpel or by cryosurgery, electrodessication or laser ablation. Recurrences are common due to persistence of the virus especially in persons with low immune status.2 The patient under discussion was referred to the Department of Oral & Maxillofacial Surgery for surgical management, but the patient refused any surgical treatment due to his old age and high chances of recurrence after surgery.
Outcome and follow-up
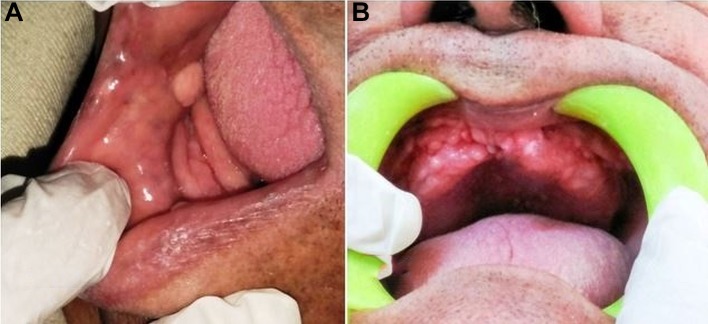
The patient was kept on regular periodic follow-up. No recurrence was noted in the two growths that were excised. The other lesions did not show any further increase in size or change in the surface mucosa. No new lesion was noted over a period of 6 months (figure 4A,B).
Figure 4.
(A,B) Intraoral photograph showing no recurrence of lesions 6 months postexcision.
Discussion
CA is a sexually transmitted disease affecting the oral and anogenital region caused by HPV, mostly HPV 6 and 11 and occasionally by 16 and 18.2
HPV resides in the basal epithelial cells of the mucosa and skin. It may cause malignant transformation in association with other cofactors.8 9 Out of more than 100 types of HPV that have been detected, only 24 are related to oral lesions with varying oncogenic potential.10 Oral squamous cell carcinoma (OSCC) is associated with HPV in 50% of cases.11 The high-risk HPV that have the highest chances of causing malignant transformation are HPV 16, 18, 26, 31, 33, 35, 39, 45, 51, 52, 53, 56, 58, 59, 66, 68, 73 and 82. Among these, HPV 16 and 18 are most commonly and HPV 31, 32 and 35 are less frequently associated with OSCC.12
The disease is commonly seen in teenagers and young adults1 and most patients diagnosed with CA give some history of sexual exposure in the recent past.2 10 13 14
The patient under discussion had multiple growths of varying sizes in the oral cavity since 15 years and had visited his local dentist 3 years back for fabrication of complete dentures. He recently experienced difficulty in wearing dentures and increase in size of the lesions for which he consulted his local dentist again who referred him to our institute.
This case is unique and deserves special mention because the patient is of geriatric age group and no history of any high-risk sexual behaviour was given by him.
The lesions had been present in his oral cavity for 15 years but could not be diagnosed by his oral healthcare provider. Hence, proper diagnosis and clinical differentiation of CA from other wart-like lesions is essential to provide rehabilitation to the patient.
Oral lesions are most common on the lips, floor of the mouth, tongue, buccal mucosa and soft palate. The lesions appear as solitary or multiple, sessile or pedunculated, pinkish papules or papillary lesions with pebbled surface.2 7 The clinical presentation and oral site involvement in our case were in accordance with those reported in the literature.
Diagnosis of oral lesions of CA is based on history, clinical examination and biopsy of the lesions.
H&E stained sections of biopsy tissue show presence of non-keratinised or parakeratinised stratified squamous epithelium with papillary surface projections supported by thin connective tissue cores. The epithelium shows pseudoepitheliomatous hyperplasia with moderate-to-marked degrees of basilar hyperplasia and acanthosis.1 7 There is presence of a peculiar form of cytological atypia characterised by large, pleomorphic, hyperchromatic and angular nuclei in the superficial layers of the epithelium, and the basal layers are least affected. These features help to distinguish CA from conventional dysplasia where the basal layers are inevitably involved.15 The papillary projections of epithelium are broader and blunter in CA, whereas they are thinner in squamous papilloma and VV. This is an important histological feature in differentiating CA from these two lesions.1 The pathognomonic feature of HPV infection is the presence of koilocytes in the superficial layers of the epithelium. Koss and Durfee in 1956, named the squamous cells with enlarged nuclei and sharply demarcated perinuclear clear zone, surrounded by a rim of cytoplasm, as ‘koilocytes’ (from Greek, a hollow cell).16 Ayre postulated that long-standing inflammation or viral infection was responsible for the occurrence of these odd-looking squamous cells and that the perinuclear vacuoles represented degenerative changes.17 Doorbar suggested that cytoplasmic vacuolisation may play an important role in the fragility of the keratinocytes in the superficial layers of the epithelium facilitating the release of viral-laden nuclei from HPV lesions.18
PCR sequencing helps establish definitive diagnosis. In this case, PCR assay confirmed the presence of HPV 6 thus confirming the diagnosis as CA.
Treatment of CA is not always necessary. The lesions are self-limiting and in 20%–30% of cases, the lesions regress spontaneously within 6 months, while in 60% of cases, the lesions resolve in a year. Conventional treatment of CA includes surgical or pharmacological management. Surgical modalities range from scalpel surgery to use of electrocautery and laser techniques. Other treatment options include use of cytotoxic agents like podophyllin, trichloroacetic acid and 5-fluorouracil.19 20 Alternatively, intralesional injection of human fibroblast interferon (IFN-β) has also shown remission in some cases.21 But the use of these drugs have been reported only in cases of genital lesions. Topical application of imiquimod for oral lesions has been effective in some cases.7 The choice of treatment is based on multiple factors, such as lesion size, number and site. Other factors of equal significance in considering treatment modality include patient preference, cost, availability of the drugs and adverse effects.14
Recurrences are quite common and reported in 20%–30% of patients undergoing treatment which may occur in same or different locations.14 According to some authors, recurrence may be due to the long incubation period of HPV (2–3 months) which can result in new lesions and/or by subsequent infection with the same or different subtypes of the virus through autoinoculation or transmission from other persons.13
The patient under discussion refused treatment due to his old age and high-recurrence potential of HPV lesions. However, he was kept under regular follow-up, and the two excised lesions did not recur, and no new lesions were noted over a period of 6 months.
Learning points.
Oral condyloma acuminatum (CA) is a less-reported human papillomavirus (HPV)-induced lesion affecting the oral region.
A thorough clinical history, examination and proper investigation are necessary to establish proper diagnosis of the disease.
Awareness about orofacial HPV infections is important because of its association with oral squamous cell carcinoma.
Hence, physicians and dentists must be able to differentiate CA from other wart-like lesions in and around the oral cavity.
Acknowledgments
The authors gratefully acknowledge thecontributions made by Professor (Dr.) R. R. Paul, Deputy Directorcum-in-charge, Research and Development, GNIDSR, Kolkata and Professor (Dr.) M.Pal, HOD, Department of Oral and Maxillofacial Pathology, GNIDSR, Kolkata, for theirvaluable guidance and support in every step.
Footnotes
Contributors: RS: acquisition of data, preparing the manuscript. NS: conception and design, correction of manuscript. MAS: analysis and interpretation of data, correction of manuscript. RPC: acquisition of data, planning and designing.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Neville BW, Damm DD, Allen CM, et al. . Epithelial Pathology : Neville BW, Damm DD, Allen CM, Oral and maxillofacial pathology. 3rd St. Louis: Saunders, 2009:362–452. [Google Scholar]
- 2.Rimkevičius A, Pūrienė A, Gaigalas M. Condyloma acuminatum: some aspects. Acta Med Litu 2011;18:43–6. 10.6001/actamedica.v18i2.1813 [DOI] [Google Scholar]
- 3.Kui LL, Ziu HZ, Ning LY. Condyloma Acuminatum and Human Papilloma Virus Infection in the Oral Mucosa of Children. Pediatric Dentistry J 2003;25:2. [PubMed] [Google Scholar]
- 4.Rein ME Skin and mucous membrane lesions : Mandell GL, Douglas RG, Bennett JE, Principles and practice of infectious diseases. 2nd edn New York: John Wiley, 1985:712–6. [Google Scholar]
- 5.Mansouri Z, Bakhtiari S, Noormohamadi R. Extensive Focal Epithelial Hyperplasia: A Case Report. Iran J Pathol 2015;10:300–5. [PMC free article] [PubMed] [Google Scholar]
- 6.Philipone E, Yoon AJ. Papillary lesions : Oral Pathology in the Pediatric Patient A Clinical Guide to the Diagnosis and Treatment of Mucosal Lesions. Switzerland: Springer International Publishing, 2017:23–31. [Google Scholar]
- 7.Sapp JP, Eversole SR, Wysocki GP. et al. . Oral Infections : Sapp JP, Lewis R, Eversole SR, George P, Wysocki GP, Contemporary Oral & Maxillofacial Pathology. 2nd ed: Mosby:207–51. [Google Scholar]
- 8.Mannarini L, Kratochvil V, Calabrese L, et al. . Human Papilloma Virus (HPV) in head and neck region: review of literature. Acta Otorhinolaryngol Ital 2009;29:119–26. [PMC free article] [PubMed] [Google Scholar]
- 9.Ritchie JM, Smith EM, Summersgill KF, et al. . Human papillomavirus infection as a prognostic factor in carcinomas of the oral cavity and oropharynx. Int J Cancer 2003;104:336–44. 10.1002/ijc.10960 [DOI] [PubMed] [Google Scholar]
- 10.Dos Reis HL, Rabelo PC, de Santana MR, et al. . Oral squamous papilloma and condyloma acuminatum as manifestations of buccal-genital infection by human papillomavirus. Indian J Sex Transm Dis 2009;30:40–2. 10.4103/0253-7184.55484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Flaitz CM, Hicks MJ. Molecular piracy: the viral link to carcinogenesis. Oral Oncol 1998;34:448–53. 10.1016/S1368-8375(98)00057-8 [DOI] [PubMed] [Google Scholar]
- 12.Fakhry C, Sugar E, D’Souza G, et al. . Two-week versus six-month sampling interval in a short-term natural history study of oral HPV infection in an HIV-positive cohort. PLoS One 2010;5:e11918 10.1371/journal.pone.0011918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Percinoto AC, Danelon M, Crivelini MM, et al. . Condyloma acuminata in the tongue and palate of a sexually abused child: a case report. BMC Res Notes 2014;7:467 10.1186/1756-0500-7-467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.dos Reis HLB, Oliveira SPde, Camisasca DR, et al. . In: Shailendra K, Saxena , Oral HPV Related Diseases: A Review and an Update, Trends in Infectious Diseases and Antonio Chambo Filho, 2014. InTech. [Google Scholar]
- 15.Speight PM, Pm S. Update on oral epithelial dysplasia and progression to cancer. Head Neck Pathol 2007;1:61–6. 10.1007/s12105-007-0014-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Koss LG, Durfee GR. Unusual patterns of squamous epithelium of the uterine cervix: cytologic and pathologic study of koilocytotic atypia. Ann N Y Acad Sci 1956;63:1245–61. 10.1111/j.1749-6632.1956.tb32134.x [DOI] [PubMed] [Google Scholar]
- 17.Ayre JE. Cancer Cytology of the Uterus. New York: Grune Stratton, 1951. [Google Scholar]
- 18.Doorbar J. The papillomavirus life cycle. J Clin Virol 2005;32:7–15. 10.1016/j.jcv.2004.12.006 [DOI] [PubMed] [Google Scholar]
- 19.Margolis S. Therapy for Condyloma Acuminatum: A Review. Clinical Infectious Diseases 1982;4:S829–S836. 10.1093/clinids/4.Supplement_4.S829 [DOI] [Google Scholar]
- 20.Simmons PD. Genital warts. Int J Dermatol 1983;22:410–4. 10.1111/j.1365-4362.1983.tb02159.x [DOI] [PubMed] [Google Scholar]
- 21.Schonfeld A, Nitke S, Schattner A, et al. . Intramuscular human interferon-beta injections in treatment of condylomata acuminata. Lancet 1984;1:1038–41. [DOI] [PubMed] [Google Scholar]