Abstract
Over 16.7 million workers in Thailand (42 percent of the working population) are engaged in agriculture, disproportionately from the lower socioeconomic strata of Thai society. Most agricultural workers (over 93 percent) work in the informal sector without the protections of regulations or enforcement of labor or health and safety laws or enrollment in a social security system. Although Thailand’s use of herbicides, fungicides, and insecticides is growing, there is little regulation of the sale, use, or application of these potentially toxic chemicals. This paper summarizes the research to date on occupational health and safety for Thai agricultural workers, identifies gaps in pesticide regulations and the current systems for occupational health and safety and social support for Thai agricultural workers, and makes recommendations for future policy and research initiatives to fill the identified gaps.
Keywords: agricultural health and safety, pesticides, Thailand, informal work, occupational health
In 2012, the International Labor Organization reported that there were approximately 1.3 billion agricultural workers worldwide. This represents half of the total world labor force. Almost 60 percent of these agricultural workers were in developing countries, with a great majority found in the Asia-Pacific region.1 In Thailand, agricultural work is the economic foundation of the nation, and rural areas are home to more than 70 percent of the population.2 Among the working population, 42 percent work in agriculture (16.7 million); however, 93 percent of these agricultural workers are in the informal sector. About 44 percent are women.3 The Thai Ministry of Labor defines informal sector workers as individuals who do not have employee status under the Labor Protection Act. Instead, they are self-employed workers who typically have no stable wages, little economic security, and no formal occupational health and safety programs at work.4
Agricultural wage earners and their families often live in poverty, with an average monthly income of only 3,112 baht (the Thai currency equal to ~US $100) compared to the overall average for Thai workers of 22,873 baht (~US $750).2 As a result, more than 20 percent of agricultural families have debt.2 These data do not reflect the even lower income of the many migrant agricultural workers from Myanmar, Cambodia, and Laos. Their numbers and income are undocumented, as few are officially registered as migrant workers with the Thai government.
Agricultural work is physically demanding, with tasks that vary according to the seasonal needs of planting, nurturing, and harvesting. Since agricultural work is carried out in the open air, workers are exposed to the intense conditions of the equatorial climate of Thailand, which also brings with it exposure to insect-borne diseases (transmitted by mosquitos and other insects), parasites, animal bites, and allergic reactions to plants other than those being cultivated. In addition, exposure to grain and animal allergens, smoke from burning of rice fields and other agricultural fields, and the widespread use of chemicals that are potential skin and respiratory irritants and toxicants make the work highly hazardous.1,5 However, the only general information on the prevalence of these hazards among Thai agricultural workers was a 2009 survey of informal sector workers that found 31 percent (24,344) of the agricultural workers reported work-related hazards such as exposure to dust, chemicals, noise, and animal bites. The survey also identified the need to provide more training about safe work practices.6
Accidents and Injuries
Although data on illnesses and injuries are not systematically collected by the Thai government for informal sector agricultural workers, such data are collected for formal sector workers. A survey of the general health status of Thai labor in 2011 found that the major health problems reported by agricultural workers were cuts by sharp objects or a machine during work (67 percent), falls (12 percent), burns (5 percent), accidents with a tractor or vehicle (3 percent), crushing (9 percent), pesticide poisoning (3 percent), and other unspecified injuries (1 percent).2 In a survey of rice farmers from nine Thai villages, over 35 percent reported injuries from hand-operated, motorized plowing machines, over 80 percent reported injuries from stepping on sharp objects during plowing, and 49 percent reported punctures from bamboo sticks during planting. In addition, these workers reported loud noise and vibration from working with plowing machines, motorized pesticide sprayers, and harvesting trucks.5
Data on confined space deaths are not consistently collected in Thailand. However, there are reports of multiple incidents of confined space casualties in rice mills and silos, suggesting that this common hazard in a frequent agricultural task may be putting workers at risk of crushing or asphyxiation in oxygen-deficient atmospheres.7–9
Musculoskeletal Disorders
As with agricultural work worldwide, farmers are at risk for musculoskeletal disorders due to repeated bending, awkward postures, repetitive motions, and heavy lifting. Despite the heavy manual labor involved in agriculture, few studies have evaluated the musculoskeletal problems of agricultural workers. The above-cited survey of rice farmers from nine Thai villages found that over 65 percent reported musculoskeletal problems from lifting heavy rice sacks and seed containers, carrying backpack pesticide sprayers, and lifting heavy pumping hoses.5
Pesticides in Thai Agriculture
Thailand continues to increase its total annual import of pesticides. The most common type of pesticides imported is herbicides, followed by insecticides and fungicides (Figure 1).10 Within Thailand, data on in-country manufacture of pesticides and volume of pesticides used in agriculture are not available. However, in interviews, Thai agricultural workers report they typically use a variety of pesticides, applying them an average of three to four times a month.11,12 In a 2012 study of 202 rice, sugarcane, and vegetable agricultural workers in five districts of Suphanburi province, agricultural workers reported using eighty-seven different commercial brands of insecticides, ninety-three brands of plant hormones, and fifty-six brands of chemicals for the “control of plant diseases.” The type (active ingredient) of herbicide most commonly used in these commercial products was glyphosate (43 percent), followed by 2,4-D, butachlor, and paraquat/gramoxone.13 The insecticide most commonly used in these commercial products was abamectin (60 percent), followed by chloropyrifos, carbofuran, and cypermethrin. In northern Thailand, in addition to the use of mancozeb fungicide (47%–58% of farmers) and methomyl insecticides, a large percentage of farmers also reported the use of abamectin, paraquat, glyphosate, 2,4-D, and cypermethrin.11
Figure 1.
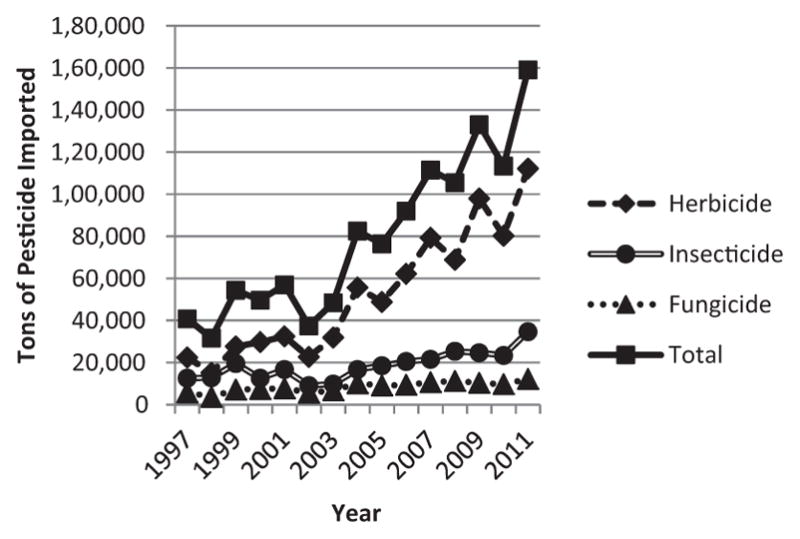
Pesticide imports into Thailand.
Source: Ministry of Agricultural and Cooperatives Office of Agricultural Economics.10
Exposure to Pesticides in Thailand
A number of studies have also reported the measured levels of the urinary metabolites of a variety of pesticides used by agricultural workers in Thailand.11,14–16 Several of these studies have also found measurable levels of urinary metabolites of pesticides that have been banned in Thailand.11,17 For example, Panuwet et al.17 found urinary metabolites of methyl parathion in agricultural workers from northern Thailand two years after the import ban was put in place, despite the short half-life of this pesticide in humans.
In Thailand, application of pesticides typically occurs through spraying with motorized backpack units (see Figures 2 and 3). Several studies have measured exposures to agricultural workers during spraying operations.15,18 Despite the fact that they had sprayed for only one to two hours, about 18 percent of agricultural workers spraying ethion (organophosphate pesticide) by backpack or open boat pump (see Figure 4) had levels exceeding the eight-hour Threshold Limit Value–Time Weighted Average of 0.05 mg/m3 recommended by the American Conference of Governmental Industrial Hygienists.15 Almost all exposure measurements of vegetable farmers spraying dicrotophos exceeded the U.S. National Institute of Occupational Safety and Health recommended eight-hour Permissible Exposure Limit of 0.25 mg/m3 even though spraying occurred for only thirty minutes to one hour. However, among these same farmers, measurements of chlorpyrifos and profenofos were lower than recommended levels among these sprayers.18
Figure 2.

Backpack pesticide sprayer in Thailand.
Figure 3.
Rice field sprayers in Thailand.
Figure 4.
Boat pesticide sprayer (liquid insecticide sits in bottom of open boat).
In Thailand, extended and multigenerational family members frequently live together. Due to the predominance of agricultural land use and work, many of these extended families live near agricultural lands on which at least some of their family members work. Therefore, in addition to the pesticide exposures experienced by agricultural workers on the job, these other family members may also be at risk. During application, pesticides may be blown toward the home or nearby schools, resulting in inhalation exposures or contamination of the soil and building surfaces. Agricultural workers may “bring home” pesticides on their clothes or skin, or pesticides may be stored near living quarters, resulting in home contamination. Children may also be exposed in utero or by the breast milk of mothers who are agricultural workers.
Thai women in their twenty-eighth week of pregnancy who lived close to agricultural farmlands, or were agricultural workers, were found to have significantly higher levels of dialkyl phosphate urinary metabolites (from organophosphates and carbamate insecticides) than did other pregnant women.19 Other studies have found exposure to similar levels of organophosphate pesticides put the fetus at risk for neurodevelopmental effects.19
Secondary school students in Chiangmai Province whose parents were agricultural workers were found to have significantly higher urinary pyrethroid insecticide metabolites than did other children.20 In addition, children living inside or near farm areas during the spraying season had significantly higher levels of dialklyphosphate metabolites (from organophosphate and carbamate insecticides), compared to the children living outside farm areas.21 The chlorpyrifos pesticide levels in the air and surfaces of farm families’ homes were higher than, though not statistically significantly different from, those of non-farm families in the chili-growing area of Ubonratchathani province.22 These studies suggest that the children of agricultural workers may be at risk for a range of health effects if chronically exposed throughout their development.
Acute and Chronic Health Effects from Pesticide Exposures in Thailand
Thailand does not have a systematic poisoning surveillance system to monitor all the types poisoning cases seen at health facilities. However, a poison control center set up in a hospital in Bangkok reported that out of the 15,016 patients referred to the phone center from 2001 through 2004, 42 percent of the poisonings were attributable to pesticides. This is quite different from data for Western countries, where poisoning from household products and pharmaceuticals is more common.23 The most common pesticide poisoning agents reported were insecticides (carbamates, organophosphates, and pyrethroids) followed by herbicides (glyphosates and paraquats).23
In 2011, the Bureau of Occupational and Environmental Diseases of the Thai Ministry of Public Health evaluated the health risk of 533,524 agricultural workers in seventy-four provinces in Thailand using the services of the primary care units (PCUs) and community hospitals. The agricultural workers were interviewed and fingertip blood samples taken to test for plasma pseudocholinesterase, which is inhibited when workers are exposed to excessive levels of certain insecticides (organophosphates, carbamates). The results showed that 173,243 (32 percent) of the agricultural workers had levels of plasma pseudocholinesterase enzyme considered “risky” or “unsafe” (>75 units/ml).24 In 2012, the blood tests for another 117,131 agricultural workers in sixteen provinces found that 30 percent of them again had “risky” or “unsafe” levels of plasma pseudocholinesterase. 24 Another study of chili farmers also found high rates of “risky” or “unsafe” plasma pseudocholinesterase inhibition using the colorimetric reactive paper test.12 However, these studies may represent an underestimate of the true risk faced by agricultural workers, since depression of the plasma enzyme after exposure persists for only a few days to weeks. Thus, the timing of sample collection relative to when the pesticide was sprayed is crucial for understanding the extent of the true risk from organophosphate and carbamate pesticide exposures experienced by agricultural workers.25
Due to the risk of acute poisoning possible from the commonly used organophosphate and carbamate pesticides, most of the health research regarding Thai agricultural workers has collected data on self-reported poisoning-related symptoms.12,26,27 Phataraphon and Chapman looked at 420 rice farmers in Sukhothai Province and found that either during or within twenty-four hours of spraying, 53 percent of the farmers had experienced neuromuscular symptoms, 34 percent respiratory symptoms, and 10 percent digestive system symptoms. Over a period of one year, 68 percent of the farmers reported experiencing either these symptoms or effects on the eyes, skin, or nails.26 Of 380 chili farmers surveyed, 38 percent reported dizziness, 31 percent headache, 27 percent nausea and vomiting, and 27 percent fever in relation to pesticide use.12
To date, few studies of chronic disease among Thai agricultural workers have been reported. In one study, an ecological linkage was made between the amount of pesticides used in a province and the prevalence of Parkinson’s disease. Two provinces (Chainat and Singburi) in the central region of Thailand that used the largest amount of pesticides also had the highest prevalence of Parkinson’s disease. The authors discuss the need for a population-based case–control study, with individual level exposure data, to follow-up this finding.28 A hospital-based case–control study of aplastic anemia that collected interview data, and used Thai industrial hygienists as exposure assessors, found increased odds ratios for high exposures to organophosphates (OR = 3.20, CI = 1.87–5.46), carbamates (OR = 4.75, CI = 1.92–11.75), organochlorines (OR = 6.04, CI = 1.31–27.84), and paraquat (OR = 2.17, CI = 1.11–4.25).29
Reducing Exposures to Pesticides
A number of studies have evaluated the training, hygiene, use patterns, and frequency of personal protective equipment (PPE) usage among agricultural workers. Seventy-seven percent of rice farmers in Sukhothai province reported receiving no training in safe pesticide use.30 Among chili farmers, 77 percent were reported to have a low level of knowledge about the use of PPE during pesticide use.31 Sixty percent reported not using gloves during mixing or spraying pesticides.32 In Phitsanulok, agricultural workers who grow rice, vegetables, and fruit reported that only 21 percent wear long-sleeved shirts or boots when spraying, and only 9 percent showered after handling pesticides. Although 64 percent reported using mouth or nose covers, these were most likely knit balaklavas or cotton cloth wrapped around the face.33
Higher cholinesterase inhibition (a marker of higher exposure) has been statistically associated with reports by agricultural workers that they used pesticides at higher than recommended concentrations, mixed their own pesticides, or did not use PPE.27 In another study, chili farmers who had low knowledge of pesticide risks or poor pesticide protection behaviors were found to have a significantly elevated risk of abnormal serum cholinesterase levels.12
To date, most of the intervention research around exposure reduction has focused on education. Work Improvement in Neighborhood Development (WIND) was a participatory occupational safety and health (OSH) program for agricultural workers, initiated in Vietnam and expanded to other countries, including Thailand, by the International Labor Organization.34 The WIND training program for agricultural workers is composed of five topics: (1) material storage and handling; (2) work posture, work station design, and ergonomic equipment for work; (3) machine safety; (4) work environment and chemical hazard control; and (5) hygiene and work organization. In addition, many trainers cover other topics such as social security and OSH regulations, and the reduction/recycling of materials to reduce global warming. The WIND participatory training program uses a community workshop approach that starts with learning from local examples of good safety and health practice, working in a group to develop locally feasible actions, agreeing on the changes to be implemented, and developing steps for follow-up.35 Implementation of the WIND program in Chainat province resulted in several improvements including construction of resting areas, plans for toilets in the fields, increased understanding of the health hazards of agricultural chemicals, and increased use of PPE. The participants also began making organic fertilizer and developed an organic anti-snail pesticide.36 To date, the WIND program has been implemented only on a voluntary basis by local PCUs (village clinics) where special funding has been received from the district administration, and no published reports have been generated from these efforts.
Other researchers have used a participatory health promotion model to impact occupational health among Thai agricultural workers, with good success. In Pathumthani, a study compared the use of bio-fertilizers and bio-pest-control with the use of chemical fertilizers and pesticides in rice farming and found that the “biological” field produced the same amount of rice as the “chemical” field, but cost less money to produce the rice. At the end of the study, the authors conclude that through demonstrations and dissemination of the results to neighboring farmers and schools, a local network of users of biological methods was created and a sustainable model for alternative farming developed.5 Among rice farmers in the Khlong Seven area, a combination of home and community participatory activities (surveys and training) regarding agrochemical safety resulted in significant improvements in self-reported knowledge, beliefs, behaviors, and home pesticide safety.37 Improvements were evaluated by pre- and postintervention questionnaires. Scores were combined on a series of questions about basic knowledge of agrochemical safety behaviors, as well as questions on beliefs, including perceived susceptibility, hazard severity, benefits, and barriers to using agrochemicals. The survey also included questions on behavior that asked about self-care practices before, during, and after handling agrochemicals and home pesticide safety questions that asked about storage and disposal of agrochemicals, and emergency phone numbers in the event of poisoning. Using pre- and post-training questionnaires to evaluate knowledge, attitudes, and practices, other Thai researchers have also reported significant improvements following a training program.38
Regulations
The International Labor Organization has provided guidance on health and safety in agriculture in its book Safety and Health in Agriculture: Code of Practice, which was endorsed and approved for publication by the Governing Body of the International Labor Organization at its 310th Session (March 2011).39
Most agricultural workers are not covered by Thai labor laws since they are not hired by an employer, or if hired they are not employed for the required 180 continuous days. Instead, they are covered under a Thai Department of Labor Protection Notification called “Guidance on Occupational Safety, Health and Environment for Informal Workers, 2013.”40 This notification requires that all informal workers, including self-employed persons, take care of their own workplaces in order to promote safety and health at work and to meet applicable standards. However, the Department of Labor is still developing a mechanism for the effective enforcement of this notification as well as for the provision of OSH support services to the informal sector.41
Regulation of pesticides in Thailand is covered under the Hazardous Substance Act of 1992, which was amended in 2001 and 2008.42–44 The act sets up a governing body called the Hazardous Substance Committee with members from four agencies: the Food and Drug Administration, the Department of Agriculture, the Department of Livestock Development, and the Department of Fisheries. The registration, production, distribution, and sale of pesticides are controlled by the Department of Agriculture, which first requires registrants to provide data on chemical and toxicological properties and ecosystem impacts, and then conducts efficacy and residue testing in the field before registration of a pesticide. Once registered, there is little or no oversight on the quality control, end use, or sale of registered pesticides or on the disposal of pesticides. There are reported to be over 26,000 retailers licensed to sell the over 20,000 pesticide formulations available in Thailand, and there are no restrictions on the advertising or sale of these products.45
Gaps in the Protections Afforded Informal Sector Agricultural Workers
Workers in the informal sector, including most Thai agricultural workers, can fall outside the standard social support systems developed by governments because they are not part of the regular tax and regulatory structures that are set up with formal sector employers.
Social Security
Thai government investment plans and policies have strongly focused on programs to improve the economic status and security of agricultural workers, as opposed to ensuring occupational health and safety. Agricultural workers are not part of the Thai social security system set up for formal workers. In 2011, the government of Prime Minister Abhisit Vejjajiva, of the Democrat party, began a program through which informal workers could contribute to the social security system and the government would do a 30 percent match to the contribution.46 Although not at the same level of coverage as workers in the formal economy, this scheme would enable informal sector workers to access sickness, disability, and death benefits, as well as a higher retirement benefit at age 60 (after fifteen years of contributions). However, the cost of 100 to 150 baht per month (~US $3–5) is considered too expensive for most agricultural workers, and few have enrolled.41,47
Universal Health Care System and Occupational Health Services
In 2002, Prime Minister Thaksin Shinawatra of the Thai Rak Thai party introduced a new universal health care coverage scheme to help uninsured individuals. 48 Since then, agricultural workers have been covered under what was called the “30 Baht Scheme,” referring to the co-pay cost for health care (~US $1). The universal health care coverage scheme provides access to some preventive care and illness/injury treatment at government health centers and community hospitals and uses community health volunteers to focus on health promotion and disease prevention.47 Despite universal health care coverage scheme, only 39 percent of agricultural workers have had a routine physical check-up, in part because 57 percent did not consider themselves to have any current health problems.2
Under the Ministry of Public Health, the foundation of the health-care system is the PCU, which is a village clinic staffed by public health nurses, with assistance from village health volunteers and a local public health officer. PCU staff provide preventive care, health education, and treatment of common health problems and can refer patients to district- and/or provincial-level hospitals for further diagnosis and treatment. From 2004 through 2007, the Ministry of Public Health participated in a pilot program to provide basic occupational health services at the PCU level. Activities included development of a five-day training curriculum for health officers by OSH experts, to enable them to identify work-related conditions and provide health services. However, for most PCU staff, OSH training remains very basic, and in general, PCU staff gain their knowledge about OSH for agriculture and the treatment of pesticide poisoning from on-the-job training.49 Although there is a system to refer occupational illnesses to district and provincial hospitals, this assumes that the PCU staff are able to identify a set of symptoms as work-related. In general, the focus of work-related diseases has been on the ten-disease groups for which surveillance data are collected: lung and respiratory diseases, physical factor diseases (heat, noise, cold), skin diseases, musculoskeletal diseases, zoonotic and plant-caused diseases, poisoning by metals, solvents, gases, pesticides, and other chemicals. Since Thailand has few occupational health physicians who can diagnose occupational illnesses and can develop medical programs for implementation at the community level, most of the focus on agricultural health has remained on pesticide poisoning (usually from organophosphate and carbamate insecticides).
Currently, in Thailand, there is only one reactive paper test produced for testing pseudocholinesterase activity in serum when agricultural workers are exposed to organophosphate or carbamate insecticides. This test was reported to have a sensitivity of 77 percent and specificity of 90 percent when used at 25°C.50 However, in Thailand, the temperature in the field is typically closer to 35°C, which is likely to affect the test method. In addition, no evaluation of potential interferences from cross-reactions of other chemicals was reported.50 Of even greater significance is that currently no field tests are available for other insecticides or for any herbicides, which are the most widely used pesticides in Thailand. Currently, the reactive paper test is used only for large-scale public health screening, not as a medical diagnostic tool. For those whose test shows unsafe levels of cholinesterase, the local public health officer will conduct health education on the effects of pesticide exposure and the use of PPE.
Occupational Safety and Health Training
There is no required training or education for Thai agricultural workers in the choice of, or appropriate and safe use of, pesticides for their crops. Among the more than 860 agricultural workers in Nakornsawan province surveyed by members of the Thailand Pesticide Action Network (ThaiPAN), 80 percent got their information about how to choose and use pesticides from pesticide companies or their representatives.51 During interviews, these agricultural workers reported that the pesticide companies directly advertised their products to them, took agricultural workers who used their products abroad for sight-seeing, and provided food and parties for pesticide customers.51 When interviewed as part of a study by ThaiPAN members, rice farmers in Yasothon province reported that they selected the type of pesticide to use based on recommendations from neighbors (32 percent), pesticide shops (27 percent), pesticide applicators hired to spray pesticides for them (23 percent), and advertisements (7 percent).52 In a peer-reviewed study, 38 percent of agricultural workers reported that they got their information on pesticide use from commercial media/public broadcast (including television, radio, newspaper, leaflets, pamphlets, and billboards).33 In Supanburi, 48 percent of the rice and sugar cane farmers interviewed by ThaiPAN members reported believing that mixing a variety of pesticides would increase the efficiency of plant protection, as would using a higher concentration of pesticide than that specified on the label. They also believed that they should use pesticides once a week, even if no plant disease was present.13
Recommendations
As described, little is known about many areas of agricultural workers’ health and safety, including musculoskeletal disease and unsafe conditions. More research is needed to clearly identify the activities with the highest ergonomic and safety risks for agricultural workers. At this time all OSH efforts for agricultural workers come through the Provincial and District Public Health Offices. These public health officers have no formal training in occupational health and safety. Either OSH specialists should be trained within the Provincial and District Public Health Offices, or the Ministry of Labor should extend its work to comprehensively cover informal sector workers. If adequate budget and staff were provided to the provincial and regional offices of the Labor Protection and Welfare Department in the Ministry of Labor, these safety officers and industrial hygienists could provide OSH consultations to small farms, as they now do for small and medium-sized formal sector enterprises. In addition, if the Thai governmental offices could make available appropriate discounted PPE, rather than relying on the farmer to select the appropriate equipment and pay retail costs, pesticide exposures could be reduced.
Increasing the OSH training of PCU medical staff, and linking these clinics with trained safety and industrial hygiene staff from the Labor Protection and Welfare Department, would greatly improve the provision of services, since identification of health issues could be linked more directly with preventive services. Universal training in basic OSH concepts for the existing community health volunteers who work with the PCUs would also aid in developing safer agricultural practices.
Government supports for organic farming and integrated pest management approaches could be proactive. An environmental tax on pesticide sales could be used to support agricultural workers during the transition to organic methods. The Hazardous Substances Act should be amended to regulate the advertising and incentive marketing of pesticides, and to require government-mandated training in appropriate pesticide use and OSH for licensure of sellers and purchasers of pesticides. OSH training staff and resources could be supported by a tax or fee on pesticide sales or manufacturers. Such regulations would greatly increase the likelihood of safer and more efficacious use of pesticides.
New tools for field surveillance of pesticide exposures are also needed. The lack of a simple test that can be used for field-based evaluations of exposure to a variety of common pesticides is an important gap for public health workers trying to implement exposure control interventions, as well as for researchers trying to understand the health risks of the wide range of pesticides in use in Thailand.
Finally, further research is needed to evaluate the long-term health impacts of the widespread use of pesticides by Thailand’s 16.7 million agricultural workers. Herbicides are the most widely used pesticides in Thailand, and little research has been done on their human health impacts. Recent reports from the Ministry of Health suggest that herbicide poisoning reports are increasing, largely due to exposures to paraquat/gramoxone. Studies using existing cancer or other disease registries would be an important step, including following up the limited findings of an association of pesticide use with aplastic anemia and Parkinson’s disease. 28,29 The developmental and endocrine impacts of pesticide exposures among the children of agricultural workers are also important areas for research that could influence future pesticide policies in Thailand.
Conclusion
Thailand remains a major agricultural exporter in Southeast Asia. Most of the farms are still relatively small, family-oriented operations that operate in the informal sector economy. In the focus on industrial development, those engaged in agriculture have not received the attention needed to ensure their future prosperity and health. The King of Thailand has long promoted a philosophy called the “Sufficient Economy.” This philosophy urges that the country’s development expectations be moderated, that individuals and communities appreciate the resources they have, and that economic development follow a course of careful risk management. Such an approach, if focused on developing policies to protect and support informal sector agricultural workers, would ensure Thai agriculture remained a sustainable industry, while at the same time protecting both the environment and human health. This paper outlines several areas where immediate action would improve the health of agricultural workers as well as several areas where more information is needed to define future policies. However, in May of 2014, a military coup ousted the government of Prime Minister Yingluck Shinawatra replacing it with a military-run “National Council for Peace and Order.” In August 2014, General Prayuth Chan-ocha, the head of the National Council for Peace and Order, was elected as Prime Minister by the Parliament, and democratic elections are not planned until October 2015 at the earliest. This political uncertainty and the resulting economic uncertainty within Thailand make substantial policy changes unlikely in the near future.
Acknowledgments
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: this work was supported by the Fogarty International Center and the National Institute of Environmental Health Sciences of the National Institutes of Health, and the National Institute for Occupational Safety and Health of the U.S. Centers for Disease Control and Prevention, under the Global Environmental and Occupational Health program awards (1R24TW009560 and 4R24TW009558).
Biographies
Orawan Kaewboonchoo is an associate professor of Public Health Nursing at the Faculty of Public Health, Mahidol University, Bangkok, Thailand. She has worked as an instructor at Mahidol University since 1988. She is the program chair of the Master of Nursing Science in Occupational Health. Dr. Kaewboonchoo’s research areas include occupational health surveillance, workplace health promotion, job stress, and psychosocial factors at work. She is part of the National Institutes of Health-funded Mahidol—University of Massachusetts Lowell Center for Work Environment, Nutrition and Development (CWEND) Project.
Pornpimol Kongtip is an associate professor in the Department of Occupational Health and Safety, Faculty of Public Health, Mahidol University. Dr. Kongtip’s research interests include a broad range of occupational and environmental exposure assessments, health risk assessments, and biological monitoring. Along with Dr. Susan Woskie, Dr. Kongtip is a Principal Investigator on the planning grant from NIH to develop a GeoHealth Hub for Occupational and Environmental Health in Thailand and Southeast Asia. Together they also received NIH pilot funding to investigate the impact of in-utero pesticide exposures on child development
Susan Woskie is a professor at the Department of Work Environment, College of Health Sciences, University of Massachusetts Lowell, where she directs Occupational & Environmental Hygiene Graduate Program. Dr. Woskie’s research has focused on exposure assessment for epidemiologic studies and exposure control interventions in a variety of industries and environments. Dr. Woskie first went to Thailand in 2006 as a Fogarty International Senior Scholar. In 2011, Dr. Woskie and Dr. Kongtip launched the Center for Work, Environment, Nutrition and Development (CWEND), a collaboration between Mahidol University Faculty of Public Health and University of Massachusetts Lowell College of Health Sciences, which focused on fostering occupational and environmental health research and training in Southeast Asia.
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.International Labour Office (ILO) [accessed 12 March 2014];Safety and halth in agriculture programme on safety, health, and the environment. 2012 www.ilo.org/wcmsp5/groups/public/-ed_protect/-protrav/-safework/documents/publication/wcms_110193pdf.
- 2.Thailand National Statistical Office. [accessed 12 March 2014];Health status of Thai labor. 2012 http://service.nso.go.th/nso/nsopublish/pubs/pubsfiles/LaborHealty.pdf.
- 3.Thailand National Statistical Office. [accessed 14 March 2014];Informal employed persons survey. 2012 http://web.nso.go.th/en/survey/lfs/imp/imp09.htm.
- 4.Department of Labour Protection and Welfare Occupational Safety and Health Bureau, Ministry of Labour. [accessed 7 April 2014];National profile on occupational safety and health of Thailand. 2012 www.ilo.org/wcmsp5/groups/public/-asia/-ro-bangkok/-sro-bangkok/documents/policy/wcms_192111.pdf.
- 5.Buranatrevedh S, Sweatsriskul P. Model development for health promotion and control of agricultural occupational health hazards and accidents in Pathumthani, Thailand. Ind Health. 2005;43:669–676. doi: 10.2486/indhealth.43.669. [DOI] [PubMed] [Google Scholar]
- 6.Thai Health Promotion Foundation. [accessed 11 January 2014];Development plan for improving quality of life of informal workers. 2012 http://v-reform.org/wpcontent/uploads/2012/07/.pdf.
- 7.Yenjai P, et al. Hazardous atmosphere in the underground pits of rice mills in Thailand. Asian Biomed. 2012;6:867–864. [Google Scholar]
- 8.Yenjai P, et al. Hazardous gases and oxygen depletion in a wet paddy pile: an experimental study in a simulating underground rice mill pit, Thailand. Ind Health. 2012;50:540–547. doi: 10.2486/indhealth.ms1307. [DOI] [PubMed] [Google Scholar]
- 9.Swaddiwudhipong W, et al. Lack of safety systems in agricultural settings in rural Thailand: a report of three worker death[s] J Med Assoc Thailand. 2010;93:865–869. [PubMed] [Google Scholar]
- 10.Ministry of Agricultural and Cooperatives Office of Agricultural Economics. [accessed 14 September 2014];Summary of imported pesticides [in Thai] 2014 www.oae.go.th/ewt_news.php?nid=146&filename=index.
- 11.Panuwet P, et al. Concentrations of urinary pesticide metabolites in small-scale farmers in Chiang Mai Province, Thailand. Sci Total Environ. 2008;407:655–668. doi: 10.1016/j.scitotenv.2008.08.044. [DOI] [PubMed] [Google Scholar]
- 12.Kachaiyaphum P, et al. Serum cholinesterase levels of Thai chili-farm workers exposed to chemical pesticides: prevalence estimates and associated factors. J Occup Health. 2010;52:89–98. doi: 10.1539/joh.q9003. [DOI] [PubMed] [Google Scholar]
- 13.Prasertsung N. Situation of pesticides used in rice fields in Suphanburi Province. [accessed 29 June 2014];Proceedings of the conference on chemical pesticides. 2012 www.thaipan.org/sites/default/files/conference2555/conference2555_1_10.pdf.
- 14.Hanchenlaksh C, et al. Urinary DAP metabolite levels in Thai farmers and their families and exposure to pesticides from agricultural pesticide spraying. Occup Environ Med. 2011;68:625–627. doi: 10.1136/oem.2010.060897. [DOI] [PubMed] [Google Scholar]
- 15.Kongtip P, et al. Ethion exposure and biological monitoring in vegetable farmers. J Med Assoc Thailand. 2011;94:286–294. [PubMed] [Google Scholar]
- 16.Kongtip P, et al. Assessment of occupational exposure to malathion and bifenthrin in mosquito control sprayers through dermal contact. J Med Assoc Thailand. 2013;96(Suppl 5):S82–S91. [PubMed] [Google Scholar]
- 17.Panuwet P, et al. Urinary paranitrophenol, a metabolite of methyl parathion, in Thai farmer and child populations. Arch Environ Contam Toxicol. 2009;57:623–629. doi: 10.1007/s00244-009-9315-x. [DOI] [PubMed] [Google Scholar]
- 18.Jaipieam S, et al. Inhalation exposure of organophosphate pesticides by vegetable growers in the Bang-Rieng Subdistrict in Thailand. J Environ Public Health. 2009;2009:452373. doi: 10.1155/2009/452373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kongtip P, et al. Organophosphate urinary metabolite levels during pregnancy, delivery and postpartum in women living in agricultural areas in Thailand. J Occup Health. 2014;55:367–375. doi: 10.1539/joh.13-0040-oa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Panuwet P, et al. Urinary pesticide metabolites in school students from Northern Thailand. Int J Hygiene Environ Health. 2009;212:288–297. doi: 10.1016/j.ijheh.2008.07.002. [DOI] [PubMed] [Google Scholar]
- 21.Petchuay C, et al. Biological monitoring of organophosphate pesticides in preschool children in an agricultural community in Thailand. Int J Occup Environ Health. 2006;12:134–141. doi: 10.1179/oeh.2006.12.2.134. [DOI] [PubMed] [Google Scholar]
- 22.Norkaew S, et al. Indirect exposure of farm and non-farm families in an agricultural community in Ubonratchathani Province, Thailand. J Health Res. 2013;27:79–84. [Google Scholar]
- 23.Wananukul W, et al. Human poisoning in Thailand: the Ramathibodi poison center’s experience (2001–2004) Clin Toxicol. 2007;45:582–588. doi: 10.1080/15563650701382789. [DOI] [PubMed] [Google Scholar]
- 24.Itsaraphan P. Health risks of agriculturists and the general population from pesticide toxicity. [accessed 23 June 2014];Proceedings of the conference on chemical pesticides. 2012 Nov;:15–16. www.thaipan.org/sites/default/files/conference2555/conference2555_1_02.pdf.
- 25.Roberts JR, Reigart JR. Recognition and management of pesticide poisoning. 6. Office of Pesticide Programs, U.S. Environmental Protection Agency; Washington, DC: 2013. [accessed 29 June 2014]. www2.epa.gov/pesticide-worker-safety/recognition-and-management-pesticide-poisonings. [Google Scholar]
- 26.Phataraphon M, Chapman RS. Factors influencing pesticide use-related symptoms among rice farmers in Sukhothai Province. J Health Res. 2010;24(suppl 1):13–20. [Google Scholar]
- 27.Jintana S, et al. Cholinesterase activity, pesticide exposure and health impact in a population exposed to organophosphates. Int Arch Occup Environ Health. 2009;82:833–842. doi: 10.1007/s00420-009-0422-9. [DOI] [PubMed] [Google Scholar]
- 28.Bhidayasiri R, et al. A national registry to determine the distribution and prevalence of parkinson’s disease in Thailand: implications of urbanization and pesticides as risk factors for parkinson’s disease. Neuroepidemiology. 2011;37:222–230. doi: 10.1159/000334440. [DOI] [PubMed] [Google Scholar]
- 29.Prihartono N, et al. Risk of aplastic anemia and pesticide and other chemical exposures. Asia Pacific J Public Health. 2011;23:369–377. doi: 10.1177/1010539511403605. [DOI] [PubMed] [Google Scholar]
- 30.Markmee P, Chapman RS. Factors influencing pesticide use-related symptoms among rice farmers in Sukhothai Province. J Health Res. 2010;24:13–20. [Google Scholar]
- 31.Norkaew S, et al. Knowledge, attitude and practice (KAP) of using personal protective equipment (PPE) for chili-growing farmers in Huarua Sub-District Mueang District, Ubonrachathani Province Thailand. J Health Res. 2010;24:93–100. [Google Scholar]
- 32.Taneepanichskul N, et al. Pesticide application and safety behaviour among male and female chili-growing farmers in Hua Rua Sub-District, Ubon Ratchathani Province, Thailand. J Health Res. 2012;26:193–197. [Google Scholar]
- 33.Plianbangchang P, Jetiyanon K, Wittaya-Areekul S. Pesticide use patterns among small-scale farmers: a case study from Phitsanulok, Thailand. Southeast Asian J Trop Med Public Health. 2009;40:401–410. [PubMed] [Google Scholar]
- 34.Kawakami T, Khai T, Kogi K. Developing the wind training programme in Asia: participatory approaches to improving safety, health and working conditions of farmers. International Labor Organization, ILO Subregional Office; East Asia-Bangkok: 2009. [accessed 23 June 2014]. www.ilo.org/asia/whatwedo/publications/WCMS_120488/lang-en/index.htm. [Google Scholar]
- 35.Kazutaka K. Roles of participatory action-oriented programs in promoting safety and health at work. Saf Health Work. 2012;3:155–165. doi: 10.5491/SHAW.2012.3.3.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Arphorn S, Brooks R, Permsirivanich P. Chainat: a case study in occupational health and safety promotion for farmers. Ind Health. 2006;44:98–100. doi: 10.2486/indhealth.44.98. [DOI] [PubMed] [Google Scholar]
- 37.Raksanam B, et al. Multi-approach model for improving agrochemical safety among rice farmers in Pathumthani, Thailand. Risk Manag Health Pol. 2012;5:75–82. doi: 10.2147/RMHP.S30749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Janhong K, et al. Health promotion program for the safe use of pesticides in Thai farmers. Southeast Asian J Trop Med Public Health. 2005;36(Suppl 4):258–261. [PubMed] [Google Scholar]
- 39.International Labor Organization (ILO) [accessed 23 April 2014];Safety and health in agriculture: code of practice. 2011 www.ilo.org/global/publications/books/WCMS_159457/lang-en/index.htm.
- 40.Ministry of Labor. [accessed 24 July 2014];Notification entitled guidance on occupational safety, health and environment for informal workers. 2013 www.oshthai.org/upload/file_linkitem/20130808081348_2.pdf.
- 41.Kongtip P, et al. Informal workers in Thailand: occupational health and social security disparities. New Solut: J Environ Occup Health Policy. doi: 10.1177/1048291115586036. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Government of Thailand. Hazardous Substance Control Act (HCSA) B.E. 2535. The Royal Gazette. 1992;103(39) [Google Scholar]
- 43.Government of Thailand. Hazardous Substance Control Act (HCSA) B.E. 2544. The Royal Gazette. 2001;18(206) [Google Scholar]
- 44.Government of Thailand. Hazardous Substance Control Act (HCSA) B.E. 2551. The Royal Gazette. 2008;125(38) [Google Scholar]
- 45.Panuwet P, et al. Agricultural pesticide management in Thailand: situation and population health risk. Environ Sci Pol. 2012;17:72–81. doi: 10.1016/j.envsci.2011.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Thailand Social Security Office. [accessed 26 September 2014];Benefits of insured under Social Security Act Section 40, B.E. 2556. 2013 www.sso.go.th/wpr/category.jsp?lang=en&cat=876.
- 47.Institute of Population and Social Research. [accessed 13 March 2014];Assessment system, universal coverage in the first decade, 2012, B.E. 2555. 2001–2010 www.hisro.or.th/main/download/10UCS_Thai.pdf.
- 48.Government of Thailand. [accessed 18 July 2014];National Health Security Act B.E. 2545. www.nhso.go.th/eng/Files/Userfiles/file/Thailand_NHS_Act.pdf.
- 49.Kaewboonchoo O, et al. Participatory capacity building in occupational disease surveillance among primary care unit (PCU) health personnel. Southeast Asian J Trop Med Public Health. 2011;42:1262–1268. [PubMed] [Google Scholar]
- 50.Tovivich S. Measurement of pesticide exposure using reactive paper. J Governmental Pharm Organ. 1994;20:36–44. [Google Scholar]
- 51.Munsak N. Pesticides used in Nongtangoo, Nongkrod and Bunpotpisai District, Nakornsawan Province. [accessed 30 June 2014];Proceedings of the conference on chemical pesticides. 2012 www.thaipan.org/sites/default/files/conference2555/conference2555_0_09.pdf.
- 52.Yongant S. Usage and impact of pesticides in Nasamile District, Yasothon Province. [accessed 30 June 2014];Proceedings of the conference on chemical pesticides. 2012 www.thaipan.org/sites/default/files/conference2555/conference2555_1_09.pdf.




