Abstract
Background
Hypoxemia is the most common complication during endotracheal intubation of critically ill adults. Intubation in the ramped position has been hypothesized to prevent hypoxemia by increasing functional residual capacity and decreasing the duration of intubation, but has never been studied outside of the operating room.
Methods
Multicenter, randomized trial comparing the ramped position (head of the bed elevated to 25°) with the sniffing position (torso supine, neck flexed, and head extended) among 260 adults undergoing endotracheal intubation by pulmonary and critical care medicine fellows in four ICUs between July 22, 2015, and July 19, 2016. The primary outcome was lowest arterial oxygen saturation between induction and 2 minutes after intubation. Secondary outcomes included Cormack-Lehane grade of glottic view, difficulty of intubation, and number of laryngoscopy attempts.
Results
The median lowest arterial oxygen saturation was 93% (interquartile range [IQR], 84%-99%) with the ramped position vs 92% (IQR, 79%-98%) with the sniffing position (P = .27). The ramped position appeared to increase the incidence of grade III or IV view (25.4% vs 11.5%, P = .01), increase the incidence of difficult intubation (12.3% vs 4.6%, P = .04), and decrease the rate of intubation on the first attempt (76.2% vs 85.4%, P = .02), respectively.
Conclusions
In this multicenter trial, the ramped position did not improve oxygenation during endotracheal intubation of critically ill adults compared with the sniffing position. The ramped position may worsen glottic view and increase the number of laryngoscopy attempts required for successful intubation.
Trial Registry
ClinicalTrials.gov; No.: NCT02497729; URL: www.clinicaltrials.gov
Key Words: endotracheal intubation, hypoxemia, randomized trial
Abbreviations: IQR, interquartile range; Spo2, arterial oxygen saturation measured by pulse oximetry
FOR EDITORIAL COMMENT SEE PAGE 693
Hypoxemia complicates nearly one-half of all endotracheal intubations in the ICU.1, 2 Physiologic abnormalities that decrease the volume of available oxygen (eg, diminished functional residual capacity) and anatomic characteristics that prolong the time required for intubation (eg, poor glottic view) may increase a critically ill patient’s risk of periprocedural desaturation, cardiac arrest, and death.3, 4
Patient position during endotracheal intubation may affect the risk of hypoxemia by modifying both the volume of available oxygen5, 6, 7, 8, 9, 10 and the time required for intubation.11, 12, 13 Currently, the two most common patient positions during emergent intubation are the sniffing position (torso supine, neck flexed forward, and head extended)14, 15 and the ramped position (torso and head elevated).13, 16, 17, 18 During elective intubations in the operating room, the ramped position increases functional residual capacity, thereby postponing desaturation compared with the sniffing position.19, 20, 21, 22 The ramped position may also achieve better anatomic alignment of the upper airway, improving glottic view and shortening the time to successful intubation among both adults who are obese11, 23 and not obese.12, 16, 24
Despite these promising data from studies of preoperative intubation, ramped positioning during intubation outside the operating room has been examined in only two prior studies, both observational cohorts that reported fewer complications with use of the ramped position.13, 25 Because optimal patient position during urgent and emergent intubation remains unclear,15, 17, 26, 27 we conducted a multicenter, randomized trial comparing the ramped position with the sniffing position during endotracheal intubation of critically ill adults. We hypothesized that the lowest arterial oxygen saturation would be higher with the ramped position.
Materials and Methods
Study Design
The Checklists and Upright Positioning in endotracheal intubation of critically ill patients (Check-UP) study was a randomized, multicenter, pragmatic trial comparing the ramped position with the sniffing position during endotracheal intubation of critically ill adults. The trial was factorialized to also compare use of a written preintubation checklist with usual care, details of which will be reported separately. The study protocol was approved with waiver of informed consent by the institutional review boards at each study site (e-Appendixes 1 and 2).
Study Participants
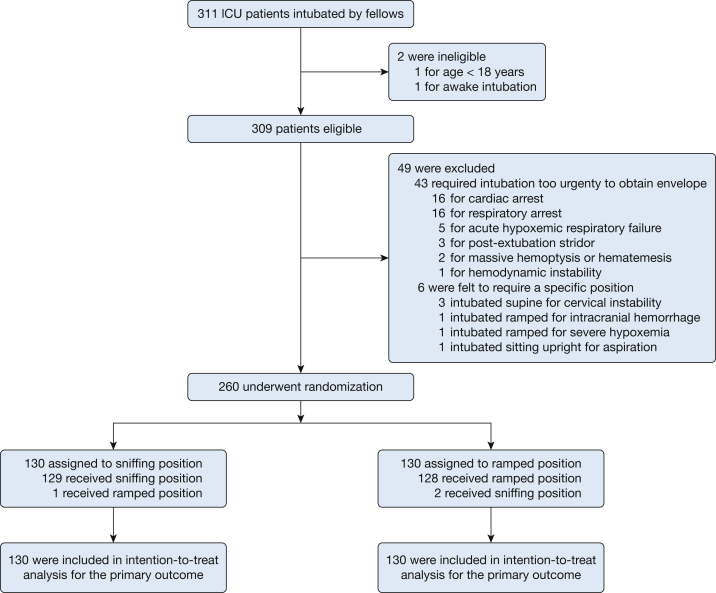
From July 22, 2015, to July 19, 2016, we enrolled patients undergoing endotracheal intubation in ICUs of four tertiary care centers in the United States (study site characteristics in e-Appendix 1). Patients ≥ 18 years of age undergoing endotracheal intubation by a pulmonary and critical care medicine fellow with the planned use of sedation and neuromuscular blockade were eligible. Patients were excluded if (1) intubation was required too emergently to perform randomization or (2) treating clinicians felt a specific patient position was required for the safe performance of the procedure (Fig 1).
Figure 1.
Enrollment, randomization, intervention, and analysis.
Randomization
Patients were randomized to the ramped position or the sniffing position in a 1:1 ratio using computer-generated blocks of 4, 8, and 12, stratified by study site. Group assignments were placed in sequentially numbered opaque envelopes, which remained sealed until the decision was made that a patient qualified for the study.
Study Treatments
For patients assigned to the ramped position, electronic bed controls were used to elevate the head of the bed to 25°, keeping the lower half of the bed parallel to the floor (e-Appendix 1). The patient’s occiput was positioned on the superior edge of the mattress such that the patient’s face was roughly parallel to the ceiling.
For patients assigned to the sniffing position, the entire bed remained horizontal while folded blankets or towels were placed beneath the patient’s head and neck to flex the neck relative to the torso and to slightly extend the head relative to the neck. In the sniffing position group, elevation of the shoulders or torso was not permitted.
A detailed description of the ideal positioning in each study group was available to operators throughout the trial (e-Appendix 1), and a pictorial demonstration of both positions was present during every intubation. Clinicians and study personnel were not blinded to group assignment.
Data Collection
Data collection during intubation was performed by independent observers not involved with the performance of the procedure. The accuracy of data collection by the independent observers was confirmed by concurrent assessment of the same outcomes by the primary investigators for a convenience sample of 10% of study intubations.
Cormack-Lehane grade of glottic view,28 subjective difficulty of intubation, and airway complications during the procedure were reported by the operator. Data on baseline characteristics, pre- and postlaryngoscopy management, and clinical outcomes were collected from the medical record by study personnel.
Study Outcomes
The primary outcome was the lowest arterial oxygen saturation measured by pulse oximetry (Spo2) between induction and 2 minutes after successful endotracheal tube placement (lowest arterial oxygen saturation). Prespecified secondary outcomes (e-Appendix 3) included the incidence of hypoxemia (Spo2 < 90%), severe hypoxemia (Spo2 < 80%), desaturation (an absolute decrease in Spo2 > 3%), Cormack-Lehane grade of glottic view,13 operator-reported difficulty of intubation, number of laryngoscopy attempts, and time from induction to successful intubation.29
Statistical Analysis
Complete details of the prespecified statistical analysis plan29 are available in e-Appendix 3. Assuming an SD in lowest arterial oxygen saturation of 14%, enrollment of 260 patients provided 80% statistical power at an α level of 0.05 to detect an absolute difference between groups in lowest arterial oxygen saturation of 5%—the minimum difference considered clinically meaningful in prior studies.1, 2, 30, 31, 32, 33 Categorical variables were reported as frequencies and compared using Fisher exact test or χ2 test. Continuous variables were reported as median and interquartile range (IQR) and compared with the Mann-Whitney rank-sum test. Agreement between the two methods of measurement was examined using Spearman rank correlation coefficient and Bland-Altman analysis.
The primary analysis was an unadjusted, intention-to-treat comparison of patients randomized to the ramped position vs the sniffing position regarding the primary outcome of lowest arterial oxygen saturation.
Four prespecified secondary analyses were performed. The first was the effect of the intervention on secondary and tertiary outcomes. The second was the effect of the intervention on the primary outcome relative to prespecified patient and procedural characteristics (Spo2, Fio2, SaO2/Fio2 ratio, and receipt of noninvasive ventilation in the 6 hours prior to intubation; Spo2 at induction; BMI; MACOCHA score; use of video laryngoscopy; and operator’s prior intubating experience) as assessed by statistical tests of interaction (subgroup analyses). The third was the comparison of the primary outcome between patients who received the sniffing position and those who received the ramped position (per-protocol analysis). The fourth was the linear regression modeling of the relationship between group assignment and the primary outcome after accounting for prespecified covariates (e-Appendix 3).
In sensitivity analyses, missing data for the primary outcome were imputed using the oxygen saturation at induction, a value of 100% in the ramped position group and 0% in the sniffing position group, and vice versa. A two-sided P value < .05 determined significance. Analyses were performed using SPSS Statistics v.24 (IBM) or R version 3.2.0 (R Foundation for Statistical Computing).
Results
Baseline Characteristics
Of 311 ICU patients intubated by fellows during the study period, 260 met no exclusion criteria and were enrolled (Fig 1). Patients randomized to the sniffing position (n = 130) and the ramped position (n = 130) were similar at baseline (Table 1, e-Tables 1 and 2). Sepsis, altered mental status, and pneumonia were the most common active medical conditions, and hypoxemic respiratory failure was the indication for almost 60% of intubations (e-Table 3). The sniffing and ramped position groups were similar regarding preintubation difficult airway characteristics, method of preoxygenation, oxygen saturation at induction, induction agent and neuromuscular blocker, and choice of laryngoscopy device (Table 1, e-Tables 4 and 5).
Table 1.
Patient and Operator Characteristics at Baseline
| Characteristics | Sniffing Position (n = 130) | Ramped Position (n = 130) |
|---|---|---|
| Patient characteristics | ||
| Age, y | 56 (45-64) | 56 (47-65) |
| Men | 79 (60.8) | 79 (60.8) |
| White | 93 (71.5) | 83 (64.3) |
| BMI, kg/m2 | 27.3 (24.0-32.6) | 26.7 (23.9-33.3) |
| APACHE II score | 22 (18-26) | 21 (18-27) |
| Vasopressors | 28 (21.5) | 26 (20.0) |
| Active medical conditions at intubationa | ||
| Sepsis | 58 (44.6) | 58 (44.6) |
| Gastrointestinal bleeding | 24 (18.5) | 23 (17.7) |
| Altered mental status | 52 (40.0) | 56 (43.1) |
| Hepatic encephalopathy | 22 (16.0) | 19 (14.6) |
| Pneumonia | 38 (29.2) | 48 (36.9) |
| Acute respiratory distress syndrome | 15 (11.5) | 16 (12.3) |
| Cardiogenic pulmonary edema | 7 (5.4) | 11 (8.5) |
| Aspiration | 9 (6.9) | 9 (6.9) |
| Indications for intubationa | ||
| Hypoxemic respiratory failure | 75 (57.7) | 77 (59.2) |
| Hypercarbic respiratory failure | 20 (15.4) | 20 (15.4) |
| Altered mental status | 48 (36.9) | 46 (35.4) |
| Hemodynamic instability | 8 (6.2) | 18 (13.8) |
| Preprocedural | 17 (13.1) | 17 (13.1) |
| MACOCHA scoreb | 2 (1-7) | 3 (1-6) |
| One or more difficult airway characteristicsc | 55 (42.3) | 58 (44.6) |
| Reintubation within 24 h of extubation | 16 (12.4) | 18 (14.0) |
| Lowest oxygen saturation in prior 6 h, % | 91 (88-94) | 91 (87-94) |
| Highest Fio2 in prior 6 h | 0.51 (0.30-1.00) | 0.40 (0.28-0.80) |
| BiPAP use in prior 6 h | 45 (34.6) | 37 (28.5) |
| Preoxygenationa | ||
| Non-rebreather mask | 58 (44.6) | 62 (47.7) |
| BiPAP | 37 (28.5) | 35 (26.9) |
| Bag-valve-mask ventilationd | 23 (17.7) | 26 (20.0) |
| Standard nasal cannulae | 9 (6.9) | 6 (4.6) |
| High-flow nasal cannulaf | 3 (2.3) | 5 (3.8) |
| Oxygen saturation at induction, % | 99 (93-100) | 99 (95-100) |
| Systolic BP at induction, mm Hg | 118 (101-137) | 121 (103-142) |
| Operator characteristicsg | ||
| Total No. of prior intubationsh | 58 (35-90) | 59 (31-81) |
| Prior intubations with the laryngoscope used | 30 (20-50) | 32 (20-50) |
| Months of fellowship training | 23.6 (13.3–30.2) | 21.9 (12.6–29.9) |
Data are presented as No. (%) or median (interquartile range). The study groups were similar regarding oxygen saturation at the time of induction (P = .19) and systolic BP at the time of induction (P = .48). APACHE II = Acute Physiology and Chronic Health Evaluation II (range, 0-71, with higher scores indicating higher severity of illness); BiPAP = bilevel positive airway pressure; MACOCHA score = ”Mallampati score III or IV, apnea syndrome (obstructive), cervical spine limitation, opening mouth < 3 cm, coma, hypoxia, anesthesiologist nontrained” score which predicts difficulty of endotracheal intubation in the ICU on a scale from 0 (easy) to 12 (very difficult).4
Patients could have more than one.
Preinduction MACOCHA scores were available for the 116 of 260 (45%) patients who were randomized to a written, preprocedure checklist as part of the factorialized study group assignment. Additional details are available in e-Table 4.
Difficult airway characteristics included BMI > 30 kg/m2, obstructive sleep apnea, upper gastrointestinal bleeding, limited mouth opening, limited neck mobility, witnessed aspiration, airway mass or infection, epistaxis or oral bleeding, and head or neck radiation. Additional details are available in e-Table 4.
Bag-valve-mask ventilation was routinely accompanied by use of a positive end-expiratory pressure valve set to 5 to 10 cm H2O.
Standard nasal cannula delivered < 6 L/min of nonhumidified oxygen.
High-flow nasal cannula delivered up to 70 L/min of humidified oxygen via the Optiflow Nasal High Flow device (Fisher & Paykel Healthcare).
Operators included 30 pulmonary and critical care medicine fellows who each performed a median of 6 (interquartile range, 2-13) study intubations.
Among the 260 intubations in the trial, there were 192 (73.8%) intubations for which the operator’s self-reported number of prior intubations in sniffing and ramped positions was available. The median number of prior intubations in the sniffing position was 37 (interquartile range, 18-37) compared with 10 (interquartile range, 6-15) in the ramped position.
Patient Position
One patient assigned to the sniffing position was intubated in the ramped position, and two patients assigned to the ramped position were intubated in the sniffing position (Fig 1). Among the convenience sample of 35 intubations observed by the primary investigators, the median angle of the head of the bed in the sniffing position group was 0° (IQR, 0°-0°) compared with 25°(IQR, 23°-25°) in the ramped position group (P < .001).
Airway Management
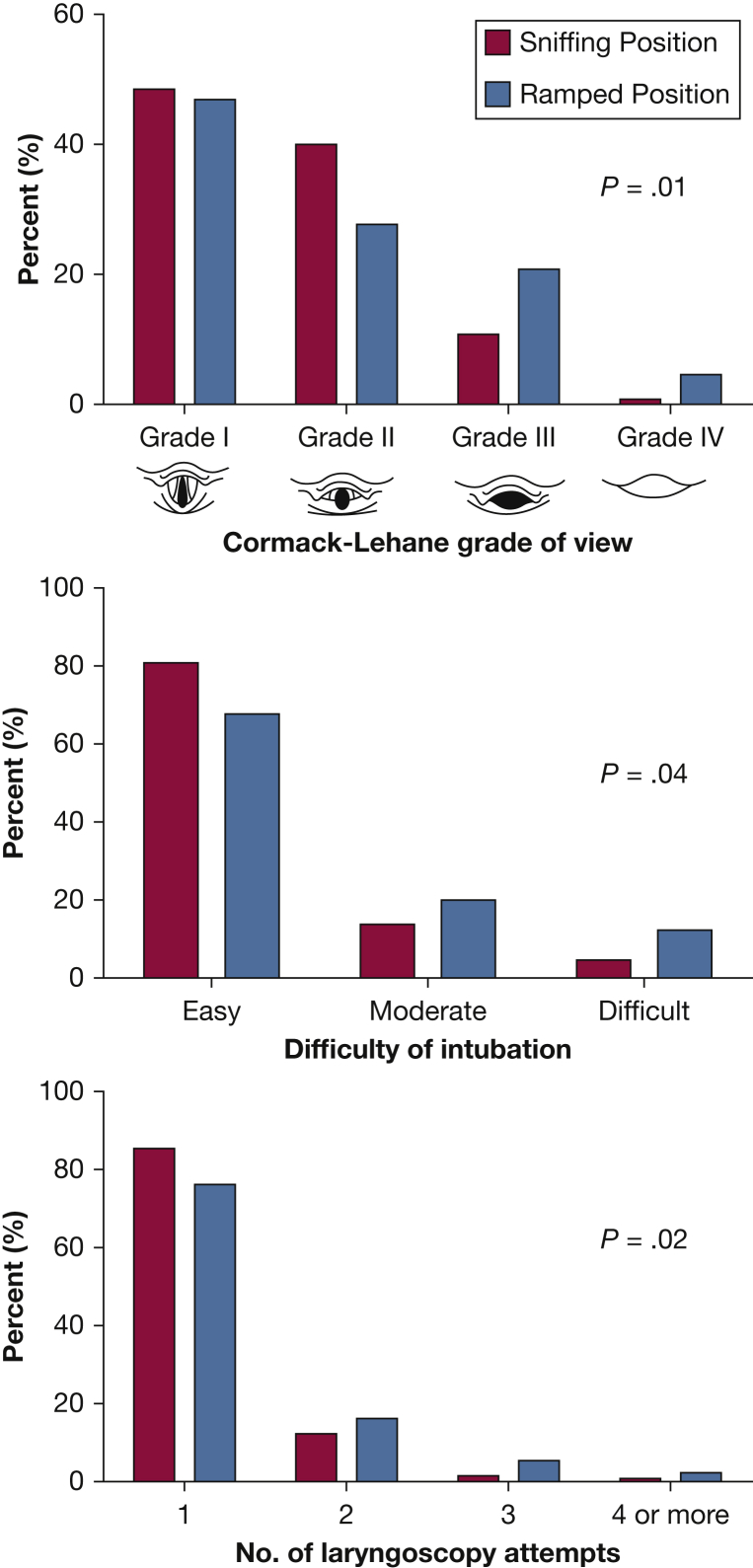
Operator-reported Cormack-Lehane grade of view and ease of intubation were better with the sniffing position than the ramped position (Fig 2, Table 2). Successful intubation on the first attempt was more common in the sniffing position group (85.4% vs 76.2%; P = .02). Fewer patients in the sniffing position group required use of an endotracheal tube introducer (bougie) (6.2% vs 19.2%; P = .002) or a second laryngoscopy device (6.2% vs 16.2%; P = .01). Rates of repositioning after induction, aspiration, and esophageal intubation did not differ between groups (e-Table 6).
Figure 2.
A-C, Procedural outcomes by study group. Cormack-Lehane grade of glottic view (A), operator-reported difficulty of intubation (B), and the number of laryngoscopy attempts required for successful intubation (C) are displayed for patients assigned to the sniffing position (red) and the ramped position (blue).
Table 2.
Outcomes of Endotracheal Intubation
| Outcomes | Sniffing Position (n = 130) |
Ramped Position (n = 130) |
P Value |
|---|---|---|---|
| Oxygenation outcomes | |||
| Lowest oxygen saturation, % | 92 (79-98) | 93 (84-99) | .27 |
| Lowest oxygen saturation < 90% | 53/127 (41.7) | 50/127 (39.4) | .70 |
| Lowest oxygen saturation < 80% | 36/127 (28.3) | 26/127 (20.5) | .14 |
| Decrease in oxygen saturation, % | 4.0 (0-15) | 3.0 (0-13) | .37 |
| Decrease in oxygen saturation > 3% | 65 (51.6) | 62 (48.8) | .66 |
| Hemodynamic outcomes | |||
| Lowest systolic BP, mm Hg | 110 (93-131) | 114 (91-133) | .69 |
| Decrease in systolic BP, mm Hg | 3 (0-17) | 3.5 (0-24) | .61 |
| New or increased vasopressor | 24 (18.5) | 24 (18.5) | > .99 |
| Procedural outcomesa | |||
| Time from induction to secured airway, s | 110 (75-157) | 119 (81-214) | .09 |
| Endotracheal tube introducer usedb | 8 (6.2) | 25 (19.2) | .002 |
| Second laryngoscope type required | 8 (6.2) | 21 (16.2) | .01 |
| Repositioning after induction required | 4 (3.1) | 9 (6.9) | .25 |
| Clinical outcomes | |||
| Duration of mechanical ventilation, d | 3 (2-7) | 3 (2-8) | .86 |
| Ventilator-free daysc | 0 (0-24) | 15.5 (0-25) | .13 |
| Mean ± SD | 10.6 ± 11.9 | 12.7 ± 11.9 | … |
| ICU length of stay,c d | 5 (3-11) | 6 (3-13) | .19 |
| ICU-free days | 0 (0-21) | 11 (0-23) | .74 |
| Mean ± SD | 9.1 ± 10.6 | 11.3 ± 10.9 | … |
| Died within 1 h of intubation | 2 (2.6) | 0 (0.0) | .50 |
| Died before hospital discharge | 64 (49.2) | 53 (40.8) | .17 |
Data are presented as No. (%), median (interquartile range), or as otherwise indicated.
Endotracheal tube introducer includes tracheal tube introducer, gum elastic bougie, or bougie.
The distribution of ventilator-free days and ICU-free days was similar overall between study groups. A total of 53% of patients in the sniffing position group, however, experienced zero ventilator-free days and ICU-free days, resulting in a median value of 0. A total of 43% of patients in the ramped position group experienced zero ventilator-free and ICU-free days.
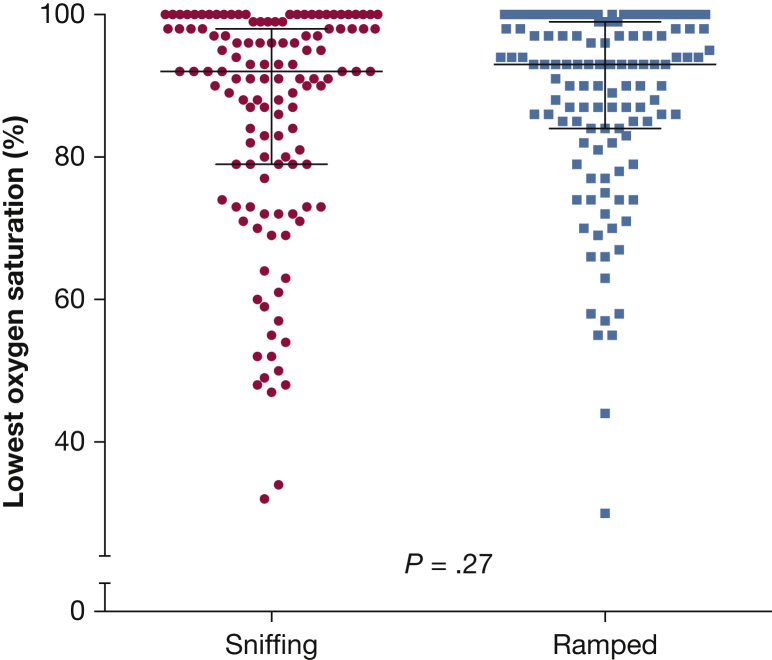
Primary Outcome
The median lowest arterial oxygen saturation during the procedure did not differ between the sniffing and ramped position groups (92%; IQR, 79%-98% vs 93%; IQR, 84%-99%, respectively; P = .27) (Fig 3, Table 2). In multivariable regression adjusting for prespecified covariates, patient position did not impact the lowest arterial oxygen saturation (e-Table 7). Agreement was strong between values for lowest arterial oxygen saturation recorded concurrently by the independent observers and the primary investigators (Spearman R2 = 0.998 in the convenience sample of 35 patients; P < .001) (e-Fig 1).
Figure 3.
Lowest arterial oxygen saturation by study group. The primary outcome of lowest arterial oxygen saturation between induction and 2 minutes after completion of endotracheal intubation (lowest oxygen saturation) is displayed for patients randomized to the sniffing position (circles) and the ramped position (squares). Horizontal bars represent median and interquartile range.
Secondary Analyses
The sniffing and ramped position groups did not differ regarding secondary oxygenation outcomes, hemodynamic outcomes, or clinical outcomes (Table 2, e-Table 6).
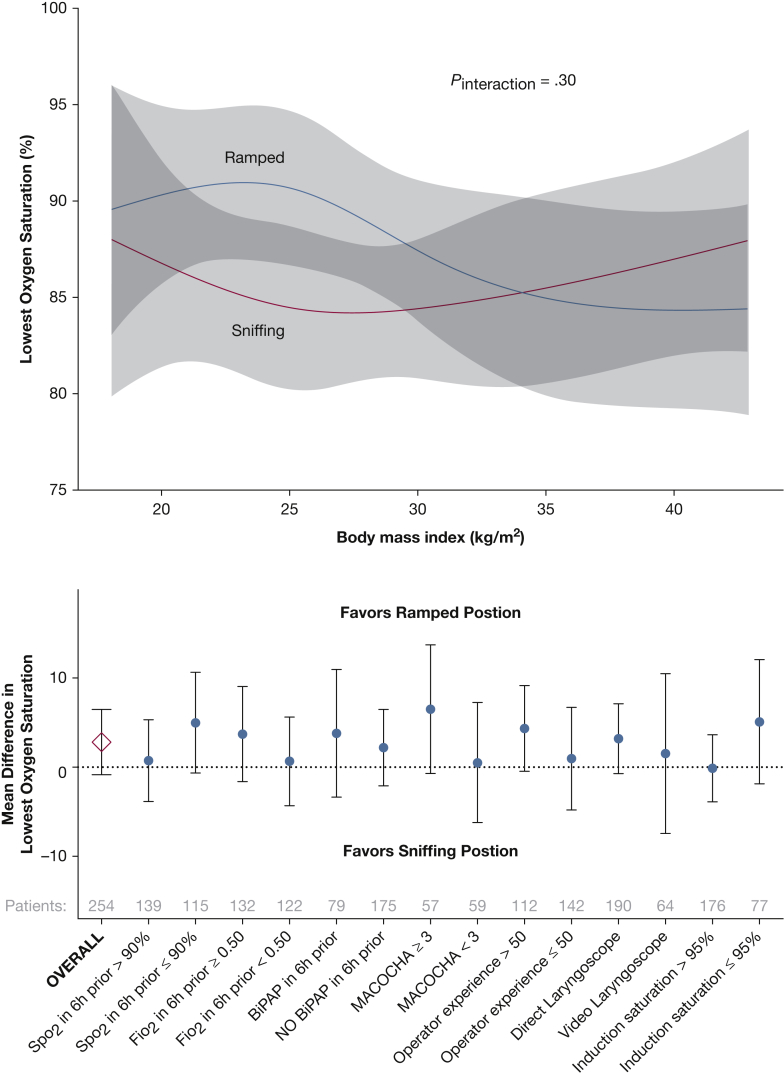
Although the point estimate for lowest oxygen saturation appeared to favor the ramped position among patients with lower Spo2 and higher Fio2 prior to induction, there was no statistically significant difference between the sniffing and ramped positions in any of the prespecified subgroups (e-Fig 2, Fig 4). Grade of glottic view, difficulty of intubation, and number of attempts were worse with the ramped position than the sniffing position across the full range of BMIs (e-Fig 3). In a post hoc analysis, the operator’s prior number of intubations in the assigned position during the trial did not modify the effect of the assigned position on procedural outcomes (e-Fig 4). Similarly, in a post hoc analysis of the 192 (73.8%) intubations for which the operator’s self-reported number of prior intubations in the ramped position was available, the operator’s prior experience with the ramped position did not modify the effect of patient position on lowest oxygen saturation (P value for interaction = .90), grade of view (P value for interaction = .20), or number of laryngoscopy attempts (P value for interaction = .23). There was no interaction between use of a written preintubation checklist and assigned patient position regarding lowest arterial oxygen saturation (P value for interaction = .94).
Figure 4.
A, B, Heterogeneity of treatment effect. (A) The mean and 95% CI for the primary outcome of lowest arterial oxygen saturation is displayed relative to BMI for patients in each study group. (B) The mean difference in lowest arterial oxygen saturation (%) between the ramped position and the sniffing position is given for patients in prespecified subgroups present at the time of induction. Vertical bars represent the 95% CI around the mean difference. P values for the interaction between study group assignment and each variable were all > .10, except for oxygen saturation at the time of induction (P value for the interaction = .08). BiPAP = bilevel positive airway pressure; Fio2 in 6 hours prior = highest fraction of inspired oxygen in the 6 hours before intubation; MACOCHA = “Mallampati score III or IV, apnea syndrome (obstructive), cervical spine limitation, opening mouth < 3 cm, coma, hypoxia, anesthesiologist nontrained” score which predicts difficulty of endotracheal intubation in the ICU on a scale from 0 (easy) to 12 (very difficult).4 Values for the MACOCHA score were calculated immediately prior to induction for those patients randomized to a written preintubation checklist as part of the factorialized design; Spo2 in 6 hours prior = lowest noninvasively measured arterial oxygen saturation in the 6 hours before intubation.
Three patients in each arm of the study were missing values for lowest arterial oxygen saturation. In sensitivity analyses imputing the missing values as described in the Methods section, there remained no differences between the ramped and sniffing positions.
A per-protocol analysis comparing patients intubated in the sniffing position (n = 131) with patients intubated in the ramped position (n = 129) demonstrated no difference between groups in lowest oxygen saturation but did demonstrate better grade of view, easier intubation, and fewer laryngoscopy attempts with the sniffing position (e-Fig 5, e-Tables 8 and 9).
Discussion
This multicenter, randomized trial comparing the ramped position with the sniffing position during endotracheal intubation of critically ill adults found that the ramped position did not significantly increase the lowest arterial oxygen saturation. The ramped position appeared to worsen glottic view and increase the number of attempts required for successful intubation.
Patient Position and Procedural Outcomes
All prior controlled trials of patient positioning during endotracheal intubation occurred in the operating room. Three crossover studies of patients undergoing elective surgery,12, 23, 24 one trial during bariatric surgery,11 and one trial of patients undergoing elective surgery with an anticipated difficult airway16 all suggested that the ramped position provided a better glottic view than the sniffing position. None compared difficulty of intubation, time to intubation, or complications between positions.
Our trial found that the ramped position worsened glottic view and increased the number of attempts required for successful intubation. There are several potential explanations for these discordant results. Operator experience34, 35, 36 may affect the ease of laryngoscopy in a given position. In several prior studies, all intubations were performed by one or two senior anesthesiologists at a single center.11, 20 Our trial involved 30 operators across multiple centers, with the average operator having performed 60 previous intubations. Therefore, our findings may generalize to settings in which airway management is performed by trainees, but whether results would be similar among expert operators remains unknown. Similarly, whether the same results would be seen in a population of operators whose prior intubating experience was predominantly in the ramped position remains unknown.
Although the technique used to achieve the ramped positioning in our trial mirrored that of prior studies,12, 20, 37 almost one-half of the patients in our trial had altered mentation, and maintaining ideal head and neck positioning may have been more challenging than with patients undergoing elective surgery.11, 12, 16, 23, 24 Similarly, the design of an ICU bed differs from that of an operating room table. Access to the patient’s head and airway may be more easily obtained with an operating room table in the ramped position than an ICU bed in the same position.
Patient Position and Oxygenation
Four randomized trials have compared the ramped position with the sniffing position regarding desaturation.19, 20, 21, 22 In each study, 25 to 50 patients undergoing elective surgery were placed in either the ramped or supine position and intubated. After intubation, the endotracheal tube was disconnected, and the time required for the patient’s oxygen saturation to fall below 92% to 95% was recorded. This “duration of apnea without desaturation” ranged from 1 minute to > 10 minutes and was at least 30 seconds longer with the ramped position in each study.
Our trial differs from these prior studies in both design and patient population. Our primary outcome of lowest arterial oxygen saturation is an established end point in ICU intubation trials1, 2, 32, 33 and is linked to periprocedural cardiac arrest and death.3 In contrast, “duration of apnea without desaturation” has never been examined outside of the operating room, and its applicability to emergent intubation is unknown. Patients in prior trials were all undergoing elective surgery, and those with cardiopulmonary disease were deliberately excluded.19, 20, 21, 22 Preoxygenation may have been better in the operating room than during our trial in the ICU, in which less than one-half of patients underwent noninvasive ventilation for preoxygenation1 and 25% had an oxygen saturation < 95% at induction. Moreover, the effect of the ramped positioning on ventilation-perfusion matching and functional residual capacity may be greater among patients undergoing elective surgery with normal lung function than among critically ill adults. Alternatively, the ramped position may actually have improved patients’ pulmonary function in our trial—as suggested by trends in favor of the ramped positioning among patients with more severe preintubation hypoxemia—but any benefit in pulmonary function was counterbalanced by duration of intubation in the ramped position, resulting in no overall difference in oxygenation between groups.
Strengths and Limitations
To our knowledge, our study is the largest trial comparing the ramped position with the sniffing position during intubation and the first to examine patient positioning during intubation outside of the operating room. The study design included randomization to balance baseline confounders, concealed allocation to prevent selection bias, conduct at multiple centers to increase generalizability, and collection of study end points by an independent observer to minimize observer bias. Rates of protocol noncompliance and missing data were low.
Our study also has limitations. The nature of the study intervention did not allow blinding. We excluded patients experiencing cardiac or respiratory arrest. Despite moderate size, our trial was not powered to detect differences in specific patient subgroups, such as those with severe hypoxemia. Because the only aspect of the intubation procedure our study controlled was patient position, our ability to examine the interaction between patient position and other procedural factors (eg, video laryngoscopy, shape of the laryngoscope blade) is limited. Finally, our study controlled patient position only during intubation and does not inform the optimal position for preoxygenation.
Conclusions
Ramped positioning of critically ill adults during endotracheal intubation does not appear to significantly improve oxygenation compared with intubation in the sniffing position. Ramped positioning may worsen glottic view and increase the number of attempts required for intubation.
Acknowledgments
Authors contributions: M. W. S. and D. R. J. had full access to the study data, conducted the analysis, and take responsibility for the integrity of the data and the accuracy of the analysis. Study concept and design: M. W. S., D. R. J., and T. W. R. Acquisition of data: M. W. S., D. R. J., D. W. R., J. D. C., R. J. L., A. N. Z., B. P. d.B., J. I. S., Y. A. K., A. M. J., W. S. S., and T. W. R. Analysis and interpretation of data: M. W. S., D. R. J., D. W. R., J. D. C., A. M. J., and T. W. R. Drafting of the manuscript: M. W. S., D. R. J., and T. W. R. Revision of the manuscript for intellectual content: M. W. S., D. R. J., D. W. R., J. D. C., R. J. L., A. N. Z., B. P. D., J. I. S., Y. A. K., A. M. J., W. S. S., and T. W. R. Statistical analysis: M. W. S., D. R. J., and T. W. R. Study supervision: M. W. S., D. R. J., D. W. R., B. P. D., J. I. S., A. M. J., W. S. S., and T. W. R.
Financial/nonfinancial disclosures: The authors have reported to CHEST the following: T. W. R. served on an advisory board for Avisa Pharma, LLC, and as the Director of Medical Affairs for Cumberland Pharmaceuticals, Inc. None declared (M. W. S., D. R. J., D. W. R., J. D. C., R. J. L., A. N. Z., B. P. d.B., J. I. S., Y. A. K., A. M. J., W. S. S.).
Role of sponsors: Funding institutions had no role in conception, design, or conduct of the study; collection, management, analysis, interpretation, or presentation of the data; or preparation, review, or approval of the manuscript.
*Writing Committee Members for the Check-UP Investigators: David R. Janz, Bennett P. deBoisblanc, Yasin A. Khan (Louisiana State University, New Orleans, LA); Jairo I. Santanilla (Ochsner Health System, New Orleans, LA); Matthew W. Semler, Todd W. Rice, Jonathan D. Casey, Robert J. Lentz (Vanderbilt University Medical Center, Nashville, TN); Derek W. Russell, Aline N. Zouk, William S. Stigler (University of Alabama at Birmingham, Birmingham, AL); Aaron M. Joffe (University of Washington, Harborview, Seattle, WA).
Collaborators: Grady P. Creek, Jody L. Haddock, Derek J. Vonderhaar, Nicole C. Lapinel, Sneha D. Samant, Rose Paccione, Kevin Dischert, Abdulla Majid-Moosa, Joaquin Crespo, Michael B. Fashho (Louisiana State University, New Orleans, LA); Daniel T. Matthews, Jeannette Zinggeler Berg, Tufik R. Assad, Andrew C. McKown, Luis E. Huerta, Emily G. Kocurek, Stephen J. Halliday, Vern E. Kerchberger, Christopher M. Merrick, Melissa A. Warren, Ryan M. Brown, Wesley H. Self (Vanderbilt University Medical Center, Nashville, TN); Roozbeh Sharif, Bryan Garcia, Swati Gulati, Chao He, David C. LaFon (University of Alabama at Birmingham, Birmingham, AL).
Other contributions: We thank the patients, nurses, respiratory therapists, residents, and attending physicians of the intensive care units at Vanderbilt University, University Medical Center New Orleans, Ochsner Medical Center Jefferson Campus, and University of Alabama at Birmingham for making this study possible.
Additional information: The e-Appendixes, e-Figures, and e-Tables can be found in the Supplemental Materials section of the online article.
Footnotes
FUNDING/SUPPORT: M. W. S. was supported by a National Heart, Lung, and Blood Institute T32 award [Grant HL087738 09]. Data collection used the Research Electronic Data Capture (REDCap) tool developed and maintained with Vanderbilt Institute for Clinical and Translational Research grant support [Grant UL1 TR000445 from the National Center for Advancing Translational Sciences/National Institutes of Health].
Contributor Information
Matthew W. Semler, Email: matthew.w.semler@vanderbilt.edu.
Pragmatic Critical Care Research Group:
Grady P. Creek, Jody L. Haddock, Derek J. Vonderhaar, Nicole C. Lapinel, Sneha D. Samant, Rose Paccione, Kevin Dischert, Abdulla Majid-Moosa, Joaquin Crespo, Michael B. Fashho, Daniel T. Matthews, Jeannette Zinggeler Berg, Tufik R. Assad, Andrew C. McKown, Luis E. Huerta, Emily G. Kocurek, Stephen J. Halliday, Vern E. Kerchberger, Christopher M. Merrick, Melissa A. Warren, Ryan M. Brown, Wesley H. Self, Roozbeh Sharif, Bryan Garcia, Swati Gulati, Chao He, and David C. LaFon
Supplementary Data
References
- 1.Baillard C., Fosse J.-P., Sebbane M. Noninvasive ventilation improves preoxygenation before intubation of hypoxic patients. Am J Respir Crit Care Med. 2006;174(2):171–177. doi: 10.1164/rccm.200509-1507OC. [DOI] [PubMed] [Google Scholar]
- 2.Semler M.W., Janz D.R., Lentz R.J. Randomized trial of apneic oxygenation during endotracheal intubation of the critically ill. Am J Respir Crit Care Med. 2016;193(3):273–280. doi: 10.1164/rccm.201507-1294OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mort T.C. The incidence and risk factors for cardiac arrest during emergency tracheal intubation: a justification for incorporating the ASA guidelines in the remote location. J Clin Anesth. 2004;16(7):508–516. doi: 10.1016/j.jclinane.2004.01.007. [DOI] [PubMed] [Google Scholar]
- 4.De Jong A., Molinari N., Terzi N. Early identification of patients at risk for difficult intubation in the intensive care unit: development and validation of the MACOCHA score in a multicenter cohort study. Am J Respir Crit Care Med. 2013;187(8):832–839. doi: 10.1164/rccm.201210-1851OC. [DOI] [PubMed] [Google Scholar]
- 5.Ibañez J., Raurich J.M. Normal values of functional residual capacity in the sitting and supine positions. Intensive Care Med. 1982;8(4):173–177. doi: 10.1007/BF01725734. [DOI] [PubMed] [Google Scholar]
- 6.Richard J.C., Maggiore S.M., Mancebo J., Lemaire F., Jonson B., Brochard L. Effects of vertical positioning on gas exchange and lung volumes in acute respiratory distress syndrome. Intensive Care Med. 2006;32(10):1623–1626. doi: 10.1007/s00134-006-0299-y. [DOI] [PubMed] [Google Scholar]
- 7.Van Beers F., Vos P. Semi-upright position improves ventilation and oxygenation in mechanically ventilated intensive care patients. Crit Care. 2014;18(Suppl 1):P258. [Google Scholar]
- 8.Ceylan B., Khorshid L., Güneş Ü.Y., Zaybak A. Evaluation of oxygen saturation values in different body positions in healthy individuals. J Clin Nurs. 2016;25(7-8):1095–1100. doi: 10.1111/jocn.13189. [DOI] [PubMed] [Google Scholar]
- 9.Hoste E.A., Roosens C.D., Bracke S. Acute effects of upright position on gas exchange in patients with acute respiratory distress syndrome. J Intensive Care Med. 2005;20(1):43–49. doi: 10.1177/0885066604271616. [DOI] [PubMed] [Google Scholar]
- 10.Solis A., Baillard C. [Effectiveness of preoxygenation using the head-up position and noninvasive ventilation to reduce hypoxaemia during intubation] Ann Fr Anesthèsie Rèanimation. 2008;27(6):490–494. doi: 10.1016/j.annfar.2008.04.006. [in French] [DOI] [PubMed] [Google Scholar]
- 11.Collins J.S., Lemmens H.J., Brodsky J.B., Brock-Utne J.G., Levitan R.M. Laryngoscopy and morbid obesity: a comparison of the “sniff” and “ramped” positions. Obes Surg. 2004;14(9):1171–1175. doi: 10.1381/0960892042386869. [DOI] [PubMed] [Google Scholar]
- 12.Lee B.J., Kang J.M., Kim D.O. Laryngeal exposure during laryngoscopy is better in the 25 degrees back-up position than in the supine position. Br J Anaesth. 2007;99(4):581–586. doi: 10.1093/bja/aem095. [DOI] [PubMed] [Google Scholar]
- 13.Khandelwal N., Khorsand S., Mitchell S.H., Joffe A.M. Head-elevated patient positioning decreases complications of emergent tracheal intubation in the ward and intensive care unit. Anesth Analg. 2016;122(4):1101–1107. doi: 10.1213/ANE.0000000000001184. [DOI] [PubMed] [Google Scholar]
- 14.Horton W.A., Fahy L., Charters P. Defining a standard intubating position using “angle finder.”. Br J Anaesth. 1989;62(1):6–12. doi: 10.1093/bja/62.1.6. [DOI] [PubMed] [Google Scholar]
- 15.Berkow L. Airway management for induction of general anesthesia. In: Hagberg C., Crowley M., editors. UpToDate. UpToDate; Waltham, MA: 2016. [Google Scholar]
- 16.Lee J.H., Jung H.C., Shim J.H., Lee C. Comparison of the rate of successful endotracheal intubation between the “sniffing” and “ramped” positions in patients with an expected difficult intubation: a prospective randomized study. Korean J Anesthesiol. 2015;68(2):116–121. doi: 10.4097/kjae.2015.68.2.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bair A. Rapid sequence intubation for adults outside the operating room. In: Post T., editor. UpToDate. UpToDate; Waltham, MA: 2015. [Google Scholar]
- 18.Orebaugh S. Direct laryngoscopy and endotracheal intubation in adults. In: Wolfson A., Hagberg C.A., editors. UpToDate. UpToDate; Waltham, MA: 2016. [Google Scholar]
- 19.Boyce J.R., Ness T., Castroman P., Gleysteen J.J. A preliminary study of the optimal anesthesia positioning for the morbidly obese patient. Obes Surg. 2003;13(1):4–9. doi: 10.1381/096089203321136511. [DOI] [PubMed] [Google Scholar]
- 20.Dixon B.J., Dixon J.B., Carden J.R. Preoxygenation is more effective in the 25 degrees head-up position than in the supine position in severely obese patients: a randomized controlled study. Anesthesiology. 2005;102(6):1110–1115. doi: 10.1097/00000542-200506000-00009. [DOI] [PubMed] [Google Scholar]
- 21.Lane S., Saunders D., Schofield A., Padmanabhan R., Hildreth A., Laws D. A prospective, randomised controlled trial comparing the efficacy of pre-oxygenation in the 20 degrees head-up vs supine position. Anaesthesia. 2005;60(11):1064–1067. doi: 10.1111/j.1365-2044.2005.04374.x. [DOI] [PubMed] [Google Scholar]
- 22.Ramkumar V., Umesh G., Philip F.A. Preoxygenation with 20° head-up tilt provides longer duration of non-hypoxic apnea than conventional preoxygenation in non-obese healthy adults. J Anesth. 2011;25(2):189–194. doi: 10.1007/s00540-011-1098-3. [DOI] [PubMed] [Google Scholar]
- 23.Cattano D., Melnikov V., Khalil Y., Sridhar S., Hagberg C.A. An evaluation of the rapid airway management positioner in obese patients undergoing gastric bypass or laparoscopic gastric banding surgery. Obes Surg. 2010;20(10):1436–1441. doi: 10.1007/s11695-009-9885-8. [DOI] [PubMed] [Google Scholar]
- 24.Lebowitz P.W., Shay H., Straker T., Rubin D., Bodner S. Shoulder and head elevation improves laryngoscopic view for tracheal intubation in nonobese as well as obese individuals. J Clin Anesth. 2012;24(2):104–108. doi: 10.1016/j.jclinane.2011.06.015. [DOI] [PubMed] [Google Scholar]
- 25.Turner J.S., Ellender T.J., Okonkwo E.R. Feasibility of upright patient positioning and intubation success rates at two academic emergency departments. Am J Emerg Med. 2017 doi: 10.1016/j.ajem.2017.02.011. [DOI] [PubMed] [Google Scholar]
- 26.Weingart S.D., Levitan R.M. Preoxygenation and prevention of desaturation during emergency airway management. Ann Emerg Med. 2012;59(3):165–175.e1. doi: 10.1016/j.annemergmed.2011.10.002. [DOI] [PubMed] [Google Scholar]
- 27.Akihisa Y., Hoshijima H., Maruyama K., Koyama Y., Andoh T. Effects of sniffing position for tracheal intubation: a meta-analysis of randomized controlled trials. Am J Emerg Med. 2015;33(11):1606–1611. doi: 10.1016/j.ajem.2015.06.049. [DOI] [PubMed] [Google Scholar]
- 28.Cormack R.S., Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia. 1984;39(11):1105–1111. [PubMed] [Google Scholar]
- 29.Matthew W. Semler. Checklists and Upright Positioning in endotracheal intubation of critically ill patients (Check-UP) Trial. Data analysis plan: ramped position vs sniffing position. https://starbrite.vanderbilt.edu/rocket/page/CHECKUP. Accessed August 4, 2016.
- 30.Taha S.K., Siddik-Sayyid S.M., El-Khatib M.F., Dagher C.M., Hakki M.A., Baraka A.S. Nasopharyngeal oxygen insufflation following pre-oxygenation using the four deep breath technique. Anaesthesia. 2006;61(5):427–430. doi: 10.1111/j.1365-2044.2006.04610.x. [DOI] [PubMed] [Google Scholar]
- 31.Baraka A.S., Taha S.K., Siddik-Sayyid S.M. Supplementation of pre-oxygenation in morbidly obese patients using nasopharyngeal oxygen insufflation. Anaesthesia. 2007;62(8):769–773. doi: 10.1111/j.1365-2044.2007.05104.x. [DOI] [PubMed] [Google Scholar]
- 32.Miguel-Montanes R., Hajage D., Messika J. Use of high-flow nasal cannula oxygen therapy to prevent desaturation during tracheal intubation of intensive care patients with mild-to-moderate hypoxemia. Crit Care Med. 2015;43(3):574–583. doi: 10.1097/CCM.0000000000000743. [DOI] [PubMed] [Google Scholar]
- 33.Vourc’h M., Asfar P., Volteau C. High-flow nasal cannula oxygen during endotracheal intubation in hypoxemic patients: a randomized controlled clinical trial. Intensive Care Med. 2015;41(9):1538–1548. doi: 10.1007/s00134-015-3796-z. [DOI] [PubMed] [Google Scholar]
- 34.Konrad C., Schüpfer G., Wietlisbach M., Gerber H. Learning manual skills in anesthesiology: Is there a recommended number of cases for anesthetic procedures? Anesth Analg. 1998;86(3):635–639. doi: 10.1097/00000539-199803000-00037. [DOI] [PubMed] [Google Scholar]
- 35.Je S., Cho Y., Choi H.J., Kang B., Lim T., Kang H. An application of the learning curve-cumulative summation test to evaluate training for endotracheal intubation in emergency medicine. Emerg Med J. 2015;32(4):291–294. doi: 10.1136/emermed-2013-202470. [DOI] [PubMed] [Google Scholar]
- 36.de Oliveira Filho G.R. The construction of learning curves for basic skills in anesthetic procedures: an application for the cumulative sum method. Anesth Analg. 2002;95(2):411–416. doi: 10.1097/00000539-200208000-00033. table of contents. [DOI] [PubMed] [Google Scholar]
- 37.Rao S.L., Kunselman A.R., Schuler H.G., DesHarnais S. Laryngoscopy and tracheal intubation in the head-elevated position in obese patients: a randomized, controlled, equivalence trial. Anesth Analg. 2008;107(6):1912–1918. doi: 10.1213/ane.0b013e31818556ed. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.