Abstract
Background
Medically underserved areas are composed of vulnerable populations with reduced access to ambulatory care services. Our goal was to determine the association between residence in a medically underserved area and severe sepsis incidence and mortality.
Methods
Using administrative data, we identified adults admitted with severe sepsis to nonfederal hospitals in South Carolina. We determined whether each resident lived in a medically underserved area or nonmedically underserved area from US Census and Department of Health and Human Services data. Age-adjusted severe sepsis incidence and mortality rates were calculated and compared between both residential classifications. Multivariate logistic regression measured the association between residence in a medically underserved area and mortality while adjusting for confounders.
Results
In 2010, 24,395 adults were admitted with severe sepsis and 1,446,987 (43%) adults lived in a medically underserved area. Residents of medically underserved areas were admitted more frequently with severe sepsis (8.6 vs 6.8 cases/1,000 people, P < .01) and were more likely to die (15.5 vs 11.9 deaths/10,000 people, P < .01), with increased odds of severe sepsis-related death (OR, 1.12) after adjustment for age, race, and severity of illness. ZIP code-based surrogates of socioeconomic status, including median income, proportion below poverty level, and educational attainment, however, had minimal association with sepsis mortality.
Conclusions
Residence in a medically underserved area is associated with higher incidence and mortality rates of severe sepsis and represents a novel method of access-to-care adjustment. Traditional access-to-care surrogates, however, are poorly associated with sepsis mortality.
Key Words: epidemiology, health-care disparities, racial disparities, sepsis
Abbreviations: ACSC, ambulatory care sensitive condition; DHHS, Department of Health and Human Services; ICD-9-CM, International Classification of Disease, 9th Edition, Clinical Modification; MUA, medically underserved area; PCP, primary care physician; SC, South Carolina
Severe sepsis is an enormous public health threat, with > 1.6 million cases annually in the United States,1 where it remains the 11th leading cause of death.2 Because severe sepsis is almost exclusively cared for in an inpatient setting, it is most commonly viewed in the context of hospital care and outcomes. However, increasing evidence suggests that ambulatory care sensitive conditions (ACSCs), such as diabetes mellitus and hypertension,3 and sociodemographics associated with poor access-to-care, such as race, education, and income,3, 4, 5 are important risk factors for the development and severity of sepsis. These associations raise the question of whether severe sepsis should be viewed from a broader health services perspective and arguably as an ACSC.
Historical attempts to examine the impact of access-to-care on severe sepsis in administrative data sets have been limited to ZIP code-based surrogates, including median income, proportion of the population below the poverty level, and educational attainment obtained from the US Census database.4 However, these variables can lack specificity regarding access to basic medical services. The Department of Health and Human Services (DHHS)6 can designate regions of the US medically underserved areas (MUAs) if they have critical deficiencies in health care and have vulnerable populations. Specifically, MUA status is granted based on a region’s score on four key variables: (1) the ratio of primary care physicians (PCPs) per 1,000 people, (2) the infant mortality rate, (3) the proportion of the population with income below the poverty level, and (4) the percentage of the population ≥ 65 years of age. Although MUA status is used to determine eligibility for federal aid, its utility as a research tool to examine the impact of access-to-care on health has not been explored.
We sought to examine if there is an association between MUA residence and sepsis incidence and mortality rates. We hypothesized that people living in an MUA will be admitted with severe sepsis more frequently and have higher sepsis-related mortality rates independent of previously described racial disparities in sepsis.4, 5 Additionally, we compared the strength of associations between MUA residence and traditionally used ZIP code-based covariates to determine the optimal methodology to control for access-to-care. Because of its geographic granularity and its assessment of physician availability, we hypothesized that MUA residence would be more closely associated with sepsis mortality than traditionally used ZIP code-based surrogates.
Methods
Study Design and Data Source
This was a retrospective cohort study of adults hospitalized with severe sepsis to nonfederal hospitals in South Carolina (SC) in the calendar year 2010 using the state’s hospital discharge database. This state was chosen based on its large proportion of the population who reside in MUAs and the accessibility of its MUA geographic data. MUA designation status was obtained from the SC Department of Health and Environmental Control.7 Population estimates were based on the US Census data from 20108 in order to accurately reflect the SC population during the year from which the hospital administrative data were analyzed.
Severe Sepsis Cohort Identification
We identified all patients, ≥ 20 years of age, who were admitted to an acute care hospital in 2010 and experienced severe sepsis during this admission. We identified a preliminary cohort using the International Classification of Disease, 9th Edition, Clinical Modification (ICD-9-CM) codes for severe sepsis (995.92) or septic shock (785.52). This method favors specificity over sensitivity when compared with alternative approaches.9, 10 Additionally, we identified a second cohort using a validated approach which combines the ICD-9-CM codes for septicemia (038.xx) and different organ failures11 and provides increased sensitivity when compared with the explicit coding approach.9 Because only a small proportion of these two preliminary cohorts overlapped, we elected to include patients in the final analysis cohort if they were identified by either coding approach in order to enhance generalizability.
Identification of MUA ZIP Codes
The SC Department of Health and Environmental Control7 provides a map of the state which displays all MUAs and non-MUAs with their ZIP code boundaries. This map was overlaid with a second map12 which contained labels for each individual ZIP code, and each ZIP code was manually assigned either: (1) MUA status if any part of that ZIP code was comprised of an MUA or (2) non-MUA status if no part of the ZIP code was designated as an MUA.
Data Collection
Adult population data for all MUA and non-MUA ZIP codes were extracted from the US Census database. Patient-level sociodemographic data, including age, sex, race, and insurance status, ICD-9-CM diagnosis and procedure codes, and mortality were extracted from the SC hospital discharge database. Deidentified hospital-level data, including urban/rural and teaching/nonteaching status for each severe sepsis admission, were similarly collected. A previously validated severe sepsis mortality prediction tool was used to risk adjust each member of the cohort.13 Briefly, this tool combines patient demographics with ICD-9-CM codes for both comorbidities and acute complications of sepsis. The tool generates a probability of mortality for risk adjustment with administrative data and has demonstrated excellent discrimination and external validity. Finally, ZIP code-level covariates that have historically been used as surrogates for access-to-care, including median income, proportion of the population below the poverty level, and educational attainment, were collected for each patient using US Census data.
Data Analysis
Using individual patient ZIP codes, we stratified the severe sepsis cohort into those who reside in MUAs and those who reside in non-MUAs and compared baseline characteristics between the groups using Student t test or χ2 test as appropriate. We calculated severe sepsis age-adjusted incidence and in-hospital mortality rates for each group using the population data for all MUA and non-MUA ZIP codes as denominators. Rates were compared between patients who reside in MUAs vs non-MUAs using the χ2 test, and ratio ratios were calculated. Additionally, we performed multivariable logistic regression modeling, with in-hospital mortality as the outcome variable. The model included a priori-selected patient covariates, including age, sex, race, insurance status, sepsis mortality probability (partitioned into quartiles: 0%-20%, 21%-40%, 41%-60%, and 61%-80%), and hospital covariates, including location and teaching status. In addition, we adjusted for median income by ZIP code, proportion of the population below the poverty level by ZIP code, and proportion of the population with high school education or lower by ZIP code in order to examine their associations with mortality compared with residence in an MUA. The regression models were manually constructed with the sequential addition of individual covariates. At each step, the model was reanalyzed, and covariates were removed if they did not contribute to the model’s predictive capability unless otherwise stated. Finally, to examine whether MUA residence may impact sepsis outcomes by modulating severity of illness, we compared the distribution of patients in each residence category across the mortality probability quartiles using the χ2 test.
All analyses were performed in SAS version 9.4 (SAS Institute). A two-sided α of 0.05 was considered the threshold for significance. The study was reviewed and approved by the institutional review board at the Medical University of South Carolina.
Results
Population Data and the Severe Sepsis Cohort
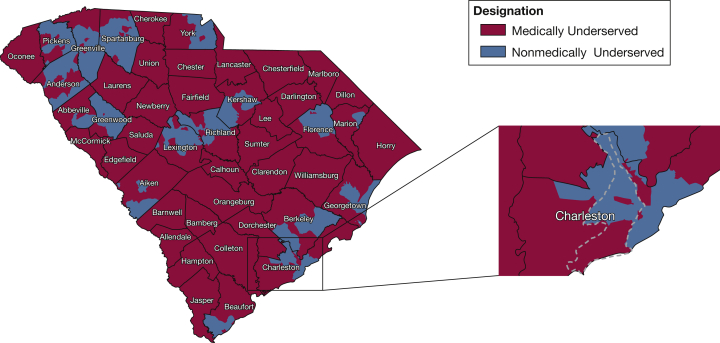
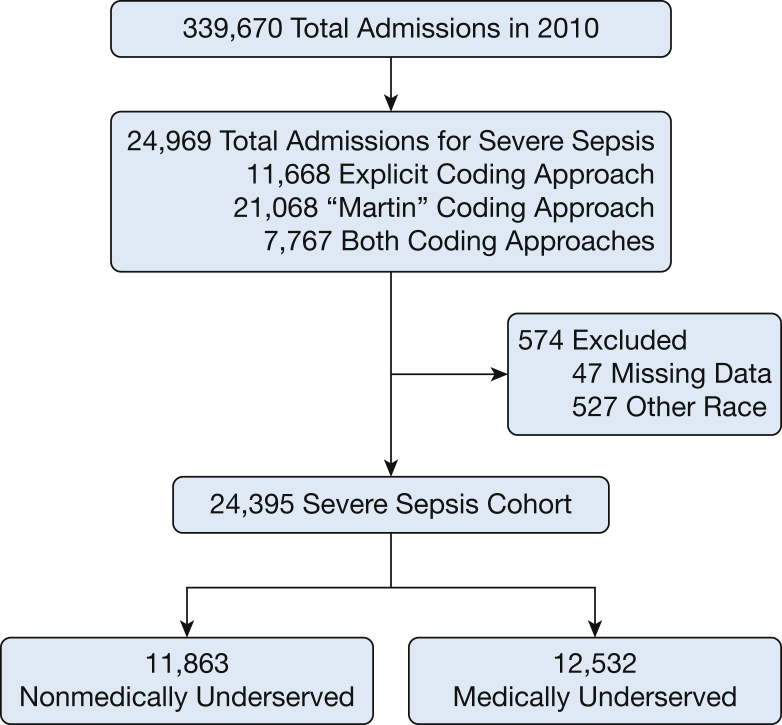
The total SC population ≥ 20 years of age in 2010 was 3,400,939. Of the 424 ZIP codes in the state, 246 were categorized as MUAs, representing 1,446,987 people ≥ 20 years of age (43%) (Fig 1). Approximately 34% (n = 490,473) of the population in MUA ZIP codes was of black race, whereas only 23% (n = 404,507) of the non-MUA population was black. In 2010, there were 339,670 admissions to nonfederal hospitals in SC. Of these, 11,668 contained an ICD-9-CM code for severe sepsis or septic shock, whereas 21,068 admissions met criteria for severe sepsis using the Martin coding strategy, and 7,767 met both coding criteria. Therefore, use of both coding strategies generated a total of 24,395 admissions in the severe sepsis cohort after exclusions, 51% of which (n =12,532) resided in MUAs (Fig 2). Table 1 compares baseline characteristics of patients from non-MUAs and MUAs in the severe sepsis cohort. Patients with sepsis from MUAs were younger, more likely to be of black race, and more likely to have Medicaid, whereas other characteristics were similar between the groups.
Figure 1.
South Carolina medically underserved areas. Most of the state’s geographic area is composed of medically underserved areas where 43% of the state’s adult population lives. Inset, An individual ZIP code (29455) is represented by the dashed line and demonstrates the socioeconomic and access-to-care heterogeneity that exists at the ZIP code level.
(Adapted with permission from the South Carolina Department of Health and Environmental Control.7)
Figure 2.
Overview of the analysis cohort.
Table 1.
Characteristics of Patients Hospitalized With Severe Sepsis Who Reside in Nonmedically Underserved and Medically Underserved Areas
| Characteristics | Nonmedically Underserved (n = 11,863) |
Medically Underserved (n = 12,532) |
P Value |
|---|---|---|---|
| Demographics | |||
| Age, mean ± SD (median), y | 67.4 ± 16.8 (69) | 65.8 ± 17.2 (68) | < .0001 |
| Male sex | 5,613 (47.3) | 5,895 (51.2) | .6665 |
| Black race | 3,384 (28.5) | 5,222 (41.7) | < .0001 |
| Insurance status | < .0001 | ||
| Medicare | 7,933 (66.9) | 8,247 (65.8) | |
| Medicaid | 1,069 (9.0) | 1,529 (12.2) | |
| Commercial insurance | 2,047 (17.3) | 1,935 (15.4) | |
| Other insurance | 814 (6.8) | 821 (6.5) | |
| Comorbidity burden | |||
| Charlson comorbidity index, score ± SD | 2.2 ± 2.1 | 2.2 ± 2.2 | .3452 |
| Severity of illness | |||
| Sepsis risk score, mean ± SD | 17.8 ± 12.7 | 17.6 ± 12.4 | .1802 |
| Outcomes | |||
| Deaths | 2,082 (17.6) | 2,257 (18.0) | .3482 |
Values are No. (%) or as otherwise indicated.
Age-Adjusted Incidence and Mortality Rates
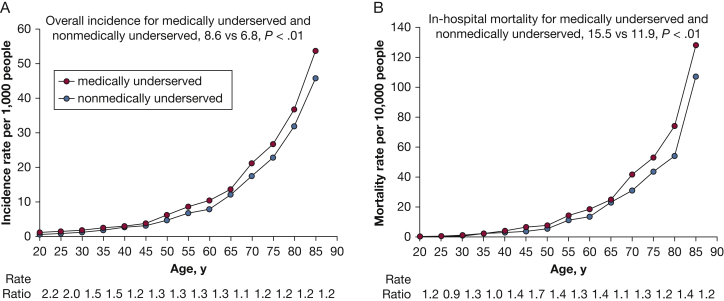
Residents of MUAs exhibited a higher incidence rate of admission with severe sepsis compared with residents of non-MUAs (8.6 vs 6.8 admissions per 1,000 people, P < .01) across all age groups (Fig 3A). Although the absolute difference in incidence rate was highest with increasing age, the rate ratios suggest that younger adults (< 40 years of age) experience the largest relative increase in severe sepsis incidence. Similarly, in-hospital mortality rates during admission with severe sepsis were higher in residents of MUAs (15.5 vs 11.9 deaths per 10,000; P < .01), with the largest absolute differences seen among older adults, whereas peak rate ratios were observed between 40 and 65 years of age (Fig 3B).
Figure 3.
Severe sepsis incidence and mortality rates by place of residence. A, Incidence rates of admissions with severe sepsis are significantly higher among patients who reside in medically underserved areas (P < .01), with the highest rate ratios in the 20- to 40-year old age group. B, Severe sepsis in-hospital mortality rates are similarly higher in patients who reside in medically underserved areas (P < .01), with peak rate ratios in the 40- to 65-year old age group.
MUA Residence Is Associated With Severe Sepsis Mortality
Multivariate logistic regression demonstrated that after adjustment, MUA residence was associated with a greater odds of dying with sepsis (OR, 1.12; 95% CI, 1.04-1.20) (Table 2). Sex and hospital teaching status were not associated with mortality in the multivariate analysis, and insurance status did not change the associations between covariates and mortality; therefore, all were excluded from the final model. This model was also used to measure the association between mortality and traditional ZIP code-based surrogates of access-to-care in order to characterize the relative strengths of these variables to predict mortality compared with MUA residence. The adjusted odds of dying with sepsis were slightly higher (OR, 1.05; 95% CI, 1.01-1.10) with every 10% increase in the proportion of the population with a high school education or less. No other associations were identified between ZIP code-based covariates and severe sepsis mortality.
Table 2.
Adjusted Odds of In-Hospital Mortality
| Variables | Model Including MUA | Model Including ZIP Code-Based Covariates |
|---|---|---|
| Patient covariates | ||
| Probability of mortality (increasing quartile) | 2.76 (2.63-2.89) | 2.72 (2.59-2.85) |
| Black race (Referent = white) | 1.13 (1.05-1.22) | 1.13 (1.05-1.23) |
| Age (5-y increase) | 1.12 (1.11-1.14) | 1.13 (1.11-1.14) |
| Hospital covariates | ||
| Rural location (referent = urban) | 0.80 (0.74-0.87) | 0.83 (0.76-0.91) |
| Access-to-care covariates | ||
| Residence in MUA | 1.12 (1.04-1.20) | N/A |
| Proportion of population with HS or less education (10% increase) | N/A | 1.05 (1.01-1.10) |
| Median income ($1,000 increase) | N/A | 1.00 (1.00 -1.01) |
| Proportion of the population below the poverty level (10% increase) | N/A | 0.99 (0.92-1.07) |
Values are OR (95% CI). HS = high school; MUA = medically underserved area; N/A = not applicable.
Severity of Illness Is Not Influenced by MUA Residence
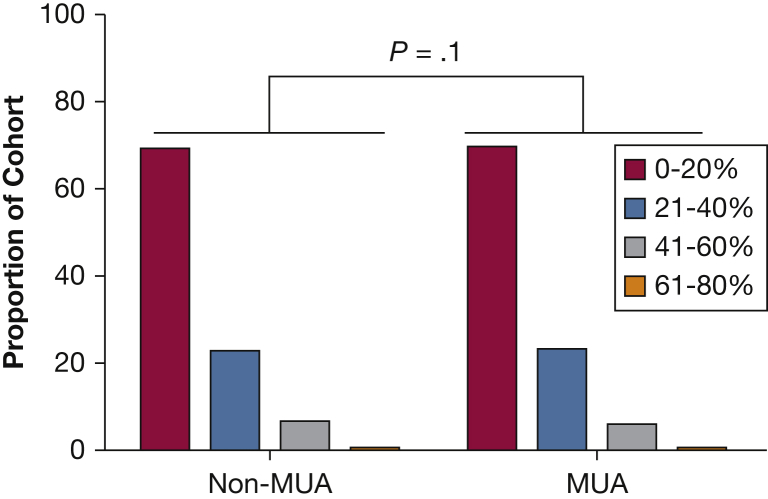
The proportion of patients in each quartile of the sepsis mortality probability score was compared between the non-MUA and MUA cohorts. The highest individual mortality probability in the data set was 80%; therefore, the quartiles were defined as quartile 1 (0%-20%), quartile 2 (21%-40%), quartile 3 (41%-60%), and quartile 4 (61%-80%) probability of mortality. There were no statistical differences in the proportion of patients in each quartile between the non-MUA and MUA cohorts (P = .11) (Fig 4).
Figure 4.
Severity of illness did not differ by place of residence. There was no significant difference between the proportion of patients within each risk quartile by place of residence (P = .10). Quartiles represented by the mortality probabilities (0%-20% = lowest risk quartile) as determined by the sepsis mortality prediction tool. MUA = medically underserved area.
Discussion
Residence in an MUA is associated with higher incidence rates of severe sepsis and higher odds of sepsis-related mortality. Although admissions with severe sepsis predominantly occur in older adults, younger adults (< 40 years of age) residing in MUAs incur the greatest proportionate increase in these admissions compared with age-matched non-MUA residents, whereas middle-aged adults (40-65 years of age) experience the greatest proportionate increase in mortality. The observed association between MUA residence and in-hospital mortality persists after adjustment for race and hospital location, suggesting that the link between place of residence and mortality is not exclusively a function of previously described racial disparity4, 5 or of care received at smaller, low-volume rural hospitals.14, 15 Interestingly, this association exists despite similar Charlson comorbidity index scores and severity of illness levels between patients who do and do not reside in MUAs. Finally, historical ZIP code-based methods of adjustment for access-to-care demonstrated minimal to no association with sepsis outcomes in this cohort.
Considerable efforts have been made to optimize inpatient care for sepsis because best practices improve mortality.16, 17, 18 However, these data suggest that sepsis outcomes are, in part, determined before a patient presents to a hospital. The MUA designation is determined by a composite score of a population’s age, economic status, and access to basic medical services. Multivariate logistic regression demonstrated that MUA residence increases the odds of severe sepsis mortality despite adjustment for age, median income, and proportion of the population below the poverty level. This suggests that access to basic medical services may be the key modifiable determinant of an MUA that is associated with severe sepsis outcomes. Because existing shortages of PCPs are projected to worsen,19 the MUA-related disparities in sepsis rates and outcomes observed here are unlikely to improve in the near future unless alternative care strategies, such as telemedicine, can be successfully leveraged.
Although these data do not establish a causal relationship, there are a number of possible mechanisms by which living in an MUA could plausibly impact severe sepsis incidence and outcomes. First, limited access to PCPs could critically delay the initial evaluation and treatment of infections that occur in the ambulatory setting. As such, some infections which could otherwise have been treated effectively in this setting could instead progress to cases of severe sepsis requiring hospital admission. Further, a shortage of PCPs may lead to inadequate management of chronic comorbidities, which could also impact both susceptibility to and outcomes of severe sepsis. Although the Charlson comorbidity index scores did not differ between the MUA and non-MUA cohorts in this study, this tool only measures the number of comorbidities a patient may have while not accounting for whether these comorbidities are adequately managed. Because the links between chronic comorbidities and sepsis incidence and complications are well established,3 poor comorbidity management may contribute to the MUA disparities identified here. Finally, the possibility of unidentified confounding factors cannot be ruled out. Medically underserved populations exhibit higher rates of risky behavior, such as smoking and alcohol abuse, than the general population,20, 21 and these behaviors have been linked to the risk of developing sepsis and complications from it.22, 23, 24, 25 Smoking and alcohol use, however, are commonly under-recognized in critically ill patients and underestimated in administrative databases26, 27; therefore, they could not be adequately adjusted for in this study. Future, prospective analyses of these potential mechanisms are warranted to better understand the risks of the medically underserved population.
Socioeconomic status and access-to-care are known to influence the outcomes of a wide variety of diseases.28 Historically, administrative database research has offered limited ability to adjust for these confounders because patient-level educational, financial, and access-to-care data are not included in most data sets. Investigators have accordingly used ZIP code-based surrogate measures of education and income. However, the ability of these variables to accurately adjust for socioeconomic status and access to care is unknown. The data presented here demonstrate that these traditional ZIP code-based measurements have little to no association with severe sepsis mortality. On the contrary, residence in an MUA was significantly associated with increased adjusted odds of death. Therefore, MUA residence may be a more sensitive adjustment tool, and its validity for research in other diseases should be explored.
This study has limitations. Residual confounding may exist in the regression model even after risk adjustment with the sepsis mortality prediction tool. Although this tool offers excellent discrimination and validity,13 it is limited by the absence of clinical data. This limitation likely explains the observation that care in rural hospitals was associated with reduced odds of mortality despite evidence that small-volume hospitals are associated with higher severe sepsis mortality rates.14, 15 An additional limitation of this study is the cumbersome approach required to assign MUA status to a particular ZIP code. The DHHS Health Resources and Services Administration29 currently allows users to search for MUA status by street address, but it does not allow for users to easily identify if an individual ZIP code contains MUAs. Modifications in the DHHS query system could greatly enhance the applicability of MUA status as a tool for future research.
Conclusions
Independent of race, residence in an MUA is a risk factor for the development of severe sepsis and dying from the disease. Poor access to care is a major contributor to these risks; therefore, severe sepsis can be viewed as an ACSC. Adjustment for MUA residence may be more accurate than traditional ZIP code-based methods of adjustment when working with administrative data sets.
Acknowledgments
Author contributions: A. J. G. takes responsibility for the integrity of the work as a whole. A. J. G., N. R. N., J. T. M., K. N. S., and D. W. F. all provided substantial contributions to the conception and design of the study and the analysis and interpretation of data. A. J. G. authored the manuscript. K. N. S., D. W. F., N. R. N., and J. T. M. provided critical review of the manuscript.
Financial/nonfinancial disclosures: None declared.
Role of sponsors: The sponsor had no role in the design of the study, the collection and analysis of the data, or the preparation of the manuscript.
Footnotes
FUNDING/SUPPORT: This study was funded by the Telemedicine & Advanced Technology Research Center, Department of Defense [Grant W81XWH-10-2-0057] to D. W. F. and K. N. S.; and the South Carolina Clinical & Translational Research Institute at the Medical University of South Carolina [NIH/NCATS Grants KL2 TR000060 and UL1 TR000062] to A. J. G.
References
- 1.Elixhauser A, Friedman B, Stranges E. Septicemia in U.S. hospitals, 2009. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville, MD; 2006. Statistical Brief #122.
- 2.Murphy S.L., Xu J., Kochanek K.D. Deaths: final data for 2010. Natl Vital Stat Rep. 2013;61(4):1–117. [PubMed] [Google Scholar]
- 3.Wang H.E., Shapiro N.I., Griffin R., Safford M.M., Judd S., Howard G. Chronic medical conditions and risk of sepsis. PloS One. 2012;7(10):e48307. doi: 10.1371/journal.pone.0048307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barnato A.E., Alexander S.L., Linde-Zwirble W.T., Angus D.C. Racial variation in the incidence, care, and outcomes of severe sepsis: analysis of population, patient, and hospital characteristics. Am J Respir Crit Care Med. 2008;177(3):279–284. doi: 10.1164/rccm.200703-480OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mayr F.B., Yende S., Linde-Zwirble W.T. Infection rate and acute organ dysfunction risk as explanations for racial differences in severe sepsis. JAMA. 2010;303(24):2495–2503. doi: 10.1001/jama.2010.851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Department of Health and Human Services - Health Resources and Services Administration. Guidelines for medically underserved areas/populations.
- 7.South Carolina Department of Health and Environmental Control. SC medically underserved areas. https://www.scdhec.gov/Health/docs/SC%20Medically%20Underserved%20Areas%20-%20Map.pdf. Accessed March 28, 2016.
- 8.United States Census Bureau. http://www.census.gov/. Accessed December 1, 2016.
- 9.Iwashyna T.J., Odden A., Rohde J. Identifying patients with severe sepsis using administrative claims: patient-level validation of the angus implementation of the international consensus conference definition of severe sepsis. Med Care. 2014;52(6):e39–e43. doi: 10.1097/MLR.0b013e318268ac86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Angus D.C., Linde-Zwirble W.T., Lidicker J., Clermont G., Carcillo J., Pinsky M.R. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29(7):1303–1310. doi: 10.1097/00003246-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 11.Martin G.S., Mannino D.M., Eaton S., Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348(16):1546–1554. doi: 10.1056/NEJMoa022139. [DOI] [PubMed] [Google Scholar]
- 12.Map of South Carolina zip codes. http://www.unitedstateszipcodes.org/maps/south-carolina-zip-code-map.png. Accessed December 3, 2016.
- 13.Ford D.W., Goodwin A.J., Simpson A.N., Johnson E., Nadig N., Simpson K.N. A severe sepsis mortality prediction model and score for use with administrative data. Crit Care Med. 2016;44(2):319–327. doi: 10.1097/CCM.0000000000001392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goodwin A.J., Simpson K.N., Ford D.W. Volume-mortality relationships during hospitalization with severe sepsis exist only at low case volumes. Ann Am Thor Soc. 2015;12(8):1177–1184. doi: 10.1513/AnnalsATS.201406-287OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Walkey A.J., Wiener R.S. Hospital case volume and outcomes among patients hospitalized with severe sepsis. Am J Respir Crit Care Med. Mar 1 2014;189(5):548–555. doi: 10.1164/rccm.201311-1967OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kumar A., Roberts D., Wood K.E. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med. 2006;34(6):1589–1596. doi: 10.1097/01.CCM.0000217961.75225.E9. [DOI] [PubMed] [Google Scholar]
- 17.Rivers E., Nguyen B., Havstad S. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345(19):1368–1377. doi: 10.1056/NEJMoa010307. [DOI] [PubMed] [Google Scholar]
- 18.Kaukonen K.M., Bailey M., Suzuki S., Pilcher D., Bellomo R. Mortality related to severe sepsis and septic shock among critically ill patients in Australia and New Zealand, 2000-2012. JAMA. 2014;311(13):1308–1316. doi: 10.1001/jama.2014.2637. [DOI] [PubMed] [Google Scholar]
- 19.Health Resources and Services Administration. Projecting the supply and demand for primary care practitioners through 2020. 2013. http://bhpr.hrsa.gov/healthworkforce/supplydemand/usworkforce/primarycare/projectingprimarycare.pdf. Accessed June 13, 2016.
- 20.Alverson E.M., Kessler T.A. Relationships between lifestyle, health behaviors, and health status outcomes for underserved adults. J Am Acad Nurse Pract. 2012;24(6):364–374. doi: 10.1111/j.1745-7599.2012.00697.x. [DOI] [PubMed] [Google Scholar]
- 21.Handley M.C., Avery D.M., Jr. Smoking in rural and underserved pregnant women. Nurs Clin North Am. 2015;50(3):577–584. doi: 10.1016/j.cnur.2015.05.010. [DOI] [PubMed] [Google Scholar]
- 22.O'Brien J.M., Jr., Lu B., Ali N.A. Alcohol dependence is independently associated with sepsis, septic shock, and hospital mortality among adult intensive care unit patients. Crit Care Med. 2007;35(2):345–350. doi: 10.1097/01.CCM.0000254340.91644.B2. [DOI] [PubMed] [Google Scholar]
- 23.Moss M., Bucher B., Moore F.A., Moore E.E., Parsons P.E. The role of chronic alcohol abuse in the development of acute respiratory distress syndrome in adults. JAMA. 1996;275(1):50–54. [PubMed] [Google Scholar]
- 24.Iribarren C., Jacobs D.R., Jr., Sidney S., Gross M.D., Eisner M.D. Cigarette smoking, alcohol consumption, and risk of ARDS: a 15-year cohort study in a managed care setting. Chest. 2000;117(1):163–168. doi: 10.1378/chest.117.1.163. [DOI] [PubMed] [Google Scholar]
- 25.Calfee C.S., Matthay M.A., Kangelaris K.N. Cigarette smoke exposure and the acute respiratory distress syndrome. Crit Care Med. 2015;43(9):1790–1797. doi: 10.1097/CCM.0000000000001089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hsieh S.J., Ware L.B., Eisner M.D. Biomarkers increase detection of active smoking and secondhand smoke exposure in critically ill patients. Crit Care Med. 2011;39(1):40–45. doi: 10.1097/CCM.0b013e3181fa4196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Al Kazzi E.S., Lau B., Li T., Schneider E.B., Makary M.A., Hutfless S. Differences in the prevalence of obesity, smoking and alcohol in the United States nationwide inpatient sample and the behavioral risk factor surveillance system. PloS One. 2015;10(11):e0140165. doi: 10.1371/journal.pone.0140165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cultler DM, Lleras-Muney A, Vogl T. Socioeconomic Status and Health: Dimensions and Mechanisms. Cambridge, MA; 2008. Working Paper 14333.
- 29.U.S. Department of Health and Human Services. Health Resources and Services Administration Data Warehouse. http://datawarehouse.hrsa.gov/tools/analyzers/geo/ShortageArea.aspx. Accessed March 24, 2016.