Abstract
This study was to explore its characteristics in a Chinese cultural setting. The sample comprised 791 suicide attempters and an equal number of controls matched on age, gender, and location from selected rural counties in China. Conditional logistic regression model was used to examine the association between NLEs and suicide risk. The impact of NLEs on attempted suicide was further examined using regression-based method to explore its mediation effect. The types of NLEs that were most likely to precede a suicide attempt in rural sample included the events in marriage/love, family/home, and friend/relationship. Rural women were more likely to experience more interpersonal conflicts than rural men. About 75.6% of suicide attempters had experienced at least one NLE, and NLEs were strongly associated with attempted suicide. Total effect (0.676), direct effect (0.501), and the total indirect effect (0.301) of NLEs on suicide attempts were significantly mediated by hopelessness and depression. Negative life events play a crucial role in predicting suicidal attempt in rural China, and they are mediated by depression and hopelessness.
Keywords: negative life event, suicide attempt, depression, hopelessness, gender
INTRODUCTION
Suicide attempt is the most important predictor of suicide constituing a major public health issue worldwide (WHO, 2014). The risk of completed suicide among individuals who attempted suicide was 38–40 times higher than that of the general population (Brown et al., 2005). A Global Health Observatory data showed that previous attempt was key risk factor for suicide which ranked as the second leading cause of dealth globally (WHO, 2016). Understanding risk factors for attempted suicide is of great value in suicide prevention (Zhang et al., 2015).
As one of risk factors for suicide, negative life events (NLEs) can cause negative or adverse life pattern changes for most individuals (Dohrenwend et al., 1978). A study from 23 Disease Surveillance Sites in China showed that all the people who died by attempting suicide experienced negative life events during the past year and the top four were conflicts with spouse or other family members, physical illnesses and financial problems (Li et al., 2008). For completed suicides, life events were reported in 92.3% and the top four life events were family poverty, terminal illnesses, and quarreling with partner or family members (Zhang & Ma, 2012). Previous studies have also found that common NLEs related to suicidal behavior and suicide attempts included interpersonal problems (especially those leading onto intense emotional issues), financial issues, unemployment and physical illnesses (Phillips, Yang, et al., 2002). Suicidal risk increased with frequency and time duration of NLEs (Liu & Tein, 2005). Studies in the West have also identified that the major life events preceding most suicide cases included interpersonal loss/conflict, financial trouble, and physical illnesses (Bagge et al., 2013; Dalgard et al., 2006; McFeeters et al., 2015). There were some negative life events which were in common between these two cultures but there were some life events that were unique to Western context such as childhood abuse (Dieserud et al., 2002), criminal activities (Yen et al., 2005).
Negative life events were closely related to suicidal behaviors, and the acute and chronic stress resulting from negative life events were independent risk factors for suicide behavior (Li et al., 2008) and they were still significant predictors even after controlling for mental disorders such as major depressive disorders in suicide attempters (Cui et al., 2003; Yen et al., 2005). Hardt and Johnson (2010) investigated 96 adolescent primary care patients and found that depressive symptoms mediated minor negative life events to suicidality. Furthermore, a study in Chinese college students demonstrated that depression played a mediating role between negative life events and suicidal ideation (Wu et al., 2012). In a cross-sectional multinational study, it’s found that depression only mediated between NLEs and suicidality in female patients (Park et al., 2015). NLEs during childhood period were found to be partially mediated by psychological problems such as depression and hopelessness (Dieserud et al., 2002). Some previous studies showed that the prevalance of mental disorders among Chinese suicides was lower than the West (about 40%–70%) (Phillips, Li, et al., 2002; Zhang et al., 2010). However, less literature was found that focuses on the mediating effect between hopelessness (Kay et al., 2009) and negative life events (Jaiswal et al., 2016; Osvath et al., 2004).
Psychological strain was hypothesized to precede psychopathology and suicidal behaviors in China (Zhang & Lv, 2014; Zhang et al., 2011) and it was a function of sociology and environment factors which may affect an individual’s lives, and also how one copes with negative life events. Although the relationship between NLEs and sucide attempts have been empirically established by many previous studies, not many studies have focused on how negative life events affect suicide attempts in China, moreso, in rural population of China. A unique feature of this study was the examination of how depression and hopelessness, when taken together, act as mediators between NLEs and suicidal behaviors.
The aims of the present study are: (1) to compare the frequency, intensity and type of NLEs between suicide attempters and living controls; (2) to estimate the risk of attempted suicide associated with NLEs between males and females; (3) to explore the mediating effect of negative life events between hopelessness and depression, and attempted suicide in rural China.
METHODS
Samples
A 1:1 matched case-control study was performed in 13 rural counties of Shandong (a more developed industrial and agricultural province in Northern China) and Hunan (an agricultural province in Central South China) between January 2012 and June 2013. The rural counties were randomly selected in data collection sites supported by the NIMH grants for which the lead author was the principle investigator. Two hospitals in each site were selected based on the size and large inpatients enrollment, and a coordinator was hired to conduct interviews for each suicidal patient. A total of 791 suicide attempters whose injury and wounds need hospitalization or emergency treatment were consecutively enrolled from the various hospital emergency departments. An equal number of matched controls was systematically and randomly selected from the same areas and matched with the study group in terms of age (±3 years), gender, and locations. Those controls that have close relationships with suicide attempters, such as friends and colleagues were excluded.
Interview Procedure
The participants were first approached by medical staff of the hospitals, or the leaders of village committee. The suicide attempters were interviewed either in the emergency room or at the attempters’ home using a structured questionnaire. All respondents were interviewed face-to-face right away or scheduled for two months later after suicidal incidents once they signed the written informed consents. Attempters who were too physically weak to respond to some of the questions during the interviews were assisted by family members. All investigators were trained in interviewing skills for the study. The interview of controls was conducted at the control’s home or village clinic with the same instruments by the same interview team. Each interview averaged about 1.5 hours.
Instruments
Demographic factors included age, gender (male =1, female =0), education level, marital status (ever married =1[including married, separated, windowed, divorced, remarried and single but dating] and never married =0 [single and not dating]), occupation (peasant=1, not peasant =0[such as self-employed, public service staff, factory worker, student, teacher, village doctor and others]), and pesticide stored at home (yes =1, no =0). Family suicide history was questioned by whether any family member had died of suicide before (yes =1, no =0). Physical illness was assessed by whether the subject had any physical illness at the time of suicide act or interview (yes =1, no =0). The Chinese version of the Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Disorders (SCID) (Gu & Chen, 1993; Spitzer et al., 1988) [Prevalence, treatment, and associated disability of mental disorders in four provinces in China during 2001–05: an epidemiological survey] was used to diagnose mental disorders for both attempters and controls by qualified psychiatrists. A total of 27 Axis I mental disorders were included and respondents who were diagnosed for any mental diseases or not were recorded yes (1) and no (0)). Family annual income was measured in yuan (RMB). The exchange rate of RMB to the US dollars was approximately 6.3 RMB to one US dollar during the study period.
The modified version of Paykel’s Interview for Recent Life Events (IRLE) (Paykel, 1997; Paykel et al., 1971) was used to assess life events that happened in the past year before suicide incident or the interview for controls. We added 19 culturally specific items in consideration of characteristics of rural China based on original 45 items. There are 64 items in terms of Marriage/Love (14 items), Family/Home (18 items), Work/Business (10 items), Health/Hospital (13 items), Law/Legal (4 items) and Friend/Relationship (5 items). The date the event happened, the number of times it happened, whether it is good or bad for the target, the influence to the target’s mental health and the duration were included in IRLE, and only the number of negative life events were included in the study. The intensity of negative life event is equal to the degree of impact multiplied by duration and by number of times (Yang & Zhang, 1999). Studies showed that IRLE had high reliability and validity in Chinese population (Zhang et al., 2003).
The Beck Hopelessness Scale (BHS) (Beck, 1978) was utilized to measure the extent of respondents’ negative attitudes or pessimism about the future. The scale has 20 items and each of them is assessed by 5 choices from 1 (strongly disagree) to 5 (strongly agree). The Chinese version of BHS has been proven to be validated with suicide attempters in China (Cronbach’s alpha coefficient=0.95) (Zhang et al., 2015). High scores indicate stronger negative attitudes about the future.
The Center for Epidemiologic Study Depression Scale (CES-D) was used to assess respondents’ depression level (Radloff, 1977). It consists of 20 items on how research objects felt in the past week with five options (ranging from 0=less than one day, 1=1–2 days, 2=3–4 days, to 3=5–7 days), and four positively formulated items 4, 8, 12, and 16 were reversely recoded. CES-D can be used to measure the prevalence of depressive symptoms in Chinese rural and non-clinical samples (Cronbach’s alpha coefficient=0.95) (Zhang et al., 2012). The total score is within 0–60, and higher score indicates higher depressive symptoms.
Ethical Statement
The study obtained approvals from The Institutional Review Board (IRB) of both the Chinese and American institutions where the principal researcher is affiliated to. Written informed consents were signed by both suicide attempters and community controls before the interview according to ethical guidelines. For those participants under 18 years old, informed consent from their parents were obtained.
Data analyses
Descriptive analyses and Chi-square test were used to compare the difference on socio-demographic variables between two groups. Conditional logistic regression model was used to analyze the relationships between NLEs and risk of suicide attempts and the relevant factors predicting suicide. Hayes’ PROCESS macro (Hayes, 2013), a regression-based analysis were performed in mediation analysis. Bootstrap methods were utilized to verify the indirect effect and to produce bias-corrected confidence. Attempted suicide or not is set as the dependent variable. All tests were two sided and the significance level was set at 0.05. All analyses were conducted using SPSS (version19.0).
FINDINGS
Characteristics of suicide attempters and controls
The study comprised 791 suicide attempters aged 15–54 and 791 controls aged 13–53. The number of males (293) in attempters and controls was the same, and so was the number of females (498). There were no significant differences between two groups in terms of age, gender and marital status respectively. More suicide attempters reported low educational level, high percentage of peasant occupation, pesticide stored at home, family suicide history and were more likely to suffer from physical diseases and mental disorders compared with controls. The suicide attempters scored significantly higher in the depression and hopelessness scales than the controls. Negative life events of the past year were reported in 75.6% (n=598) of suicide attempters and 34.8% (n=275) of living controls and it indicated that attempters were more likely than the controls to experience a negative life event. See Table 1.
Table 1.
Description and comparison of characteristics between suicide attempters and controls (N=1582)
| Variable | Suicide attempters (N=791) | Controls (N=791) | t/x2 | P |
|---|---|---|---|---|
|
| ||||
| Mean±SD/N (%) | Mean±SD/N (%) | |||
| Age | 31.66±8.10 | 31.77±8.05 | −0.280 | 0.779 |
| Gender | - | - | ||
| Male (1) | 293 (37.0) | 293 (37.0) | ||
| Female (0) | 498 (63.0) | 498 (63.0) | ||
| Education (years) | 6.90±3.26 | 8.85±3.72 | −11.109 | 0.000 |
| Marital status | 0.041 | 0.840 | ||
| Ever Married (1) | 658 (83.4) | 655 (83.0) | ||
| Never Married (0) | 131 (16.6) | 134 (17.0) | ||
| Occupation | 15.398 | 0.000 | ||
| Peasant (1) | 422 (53.4) | 344 (43.5) | ||
| Others (0) | 369 (46.6) | 447 (56.5) | ||
| Pesticide stored at home | 5.712 | 0.017 | ||
| Yes (1) | 478 (60.4) | 431 (54.5) | ||
| No (0) | 313 (39.6) | 360 (45.5) | ||
| Family suicide history | 28.144 | 0.000 | ||
| Yes (1) | 56 (7.1) | 13 (1.7) | ||
| No (0) | 728 (92.9) | 773 (98.3) | ||
| Physical illness | 21.069 | 0.000 | ||
| Yes (1) | 133 (17.0) | 72 (9.2) | ||
| No (0) | 648 (83.0) | 711 (90.8) | ||
| Mental disorder | 65.898 | 0.000 | ||
| Yes (1) | 81 (10.3) | 7 (0.9) | ||
| No (0) | 709 (89.7) | 783 (99.1) | ||
| Family annual income (yuan) | 27,320.4±38,182.1 | 32,736.2±36,235.4 | −2.894 | 0.004 |
| Hopelessness (BHS) | 53.57±15.36 | 38.31±10.42 | 23.109 | 0.000 |
| Depression (CES-D) | 19.04±16.94 | 3.98±6.39 | 23.390 | 0.000 |
| Negative life events | 598 (75.6) | 275 (34.8) | 250.049 | 0.000 |
Comparison of NLEs between suicide attempters and controls (N=1582)
64 items of NLEs were shown in Table 2. Preliminary results showed that Marriage/Love (44.1%) and Family/Home (31.2%) related life events were very common in suicide attempters. The attempters scored higher than controls in four categories of life events: Marriage/Love, Family/Home, Work/Business, Friend/Relationship (p<0.05).
Table 2.
The negative life events comparison between suicide attempters and living controls in rural China (N=1582)
| Life events | Suicide attempters (n=791) | Living controls (n=791) | c2 | P | ||
|---|---|---|---|---|---|---|
|
| ||||||
| n | % | n | % | |||
| Marriage/Love | 349 | 44.1 | 45 | 5.7 | 312.350 | 0.000 |
| 1. Wedding | 5 | 0.6 | 1 | 0.1 | 1.506 | 0.220 |
| 2. In love/engaged | 5 | 0.6 | 5 | 0.6 | 0.000 | 1.000 |
| 3. Disappointed in love affair | 23 | 2.9 | 3 | 0.4 | 15.616 | 0.000 |
| 4. Separated due to discord | 26 | 3.3 | 6 | 0.8 | 12.732 | 0.000 |
| 5. Living apart from spouse | 16 | 2.1 | 2 | 0.3 | 10.926 | 0.001 |
| 6. Legally divorced | 10 | 1.3 | 0 | 0 | 8.140 | 0.004 |
| 7. Spouse unfaithful | 31 | 3.9 | 0 | 0 | 31.580 | 0.000 |
| 8. Self being unfaithful | 11 | 1.4 | 0 | 0 | 11.077 | 0.001 |
| 9. Marriage life interfered by others | 15 | 1.9 | 0 | 0 | 15.144 | 0.000 |
| 10. Breakup of romantic relationship | 4 | 0.5 | 0 | 0 | 2.256 | 0.133 |
| 11. Quarreling with partner | 273 | 34.5 | 19 | 2.4 | 270.958 | 0.000 |
| 12. Fighting with partner | 70 | 8.8 | 14 | 1.8 | 39.427 | 0.000 |
| 13. Physically abused | 32 | 4.0 | 3 | 0.4 | 24.572 | 0.000 |
| 14. Dissatisfaction with sexual life | 5 | 0.6 | 2 | 0.3 | 0.574 | 0.449 |
| Family/Home | 247 | 31.2 | 97 | 12.3 | 83.581 | 0.000 |
| 15. Children having left home | 3 | 0.4 | 1 | 0.1 | 0.251 | 0.617 |
| 16. Children having got married/parents married | 1 | 0.1 | 0 | 0 | 0.000 | 1.000 |
| 17. Parents/child separate/divorce | 3 | 0.4 | 0 | 0 | 1.336 | 0.248 |
| 18. Quarreling with family | 138 | 17.4 | 7 | 0.9 | 130.294 | 0.000 |
| 19. Fighting with family members | 19 | 2.4 | 0 | 0 | 19.231 | 0.000 |
| 20. Major loss in home/property | 25 | 3.2 | 19 | 2.4 | 0.842 | 0.359 |
| 21. Family poverty | 36 | 4.6 | 31 | 3.9 | 0.383 | 0.536 |
| 22. Disputing over dowry/gifts | 2 | 0.3 | 0 | 0 | 0.501 | 0.479 |
| 23. In discord with spouse’s mother | 32 | 4.0 | 2 | 0.3 | 27.052 | 0.000 |
| 24. Having a baby | 7 | 0.9 | 1 | 0.1 | 3.147 | 0.076 |
| 25. Being pregnant/wife | 9 | 1.1 | 4 | 0.5 | 1.933 | 0.164 |
| 26. Abortion (wife) | 15 | 1.9 | 6 | 0.8 | 3.909 | 0.048 |
| 27. Children having had a baby/parents had a baby | 0 | 0 | 0 | 0 | - | - |
| 28. Being barren (husband or wife) | 0 | 0 | 0 | 0 | - | - |
| 29. Breaching the one child policy | 1 | 0.1 | 2 | 0.3 | 0.000 | 1.000 |
| 30. Sterilization (husband or wife) | 2 | 0.3 | 7 | 0.9 | 1.788 | 0.181 |
| 31. Menopause | 0 | 0 | 0 | 0 | - | - |
| 32. Problems in disciplining children | 23 | 2.9 | 37 | 4.7 | 4.414 | 0.065 |
| Work/Business | 94 | 11.9 | 70 | 8.8 | 3.918 | 0.048 |
| 33. Business failed | 9 | 1.1 | 6 | 0.8 | 0.606 | 0.436 |
| 34. Fired from job | 5 | 0.6 | 1 | 0.1 | 1.506 | 0.220 |
| 35. Laid off/unemployed | 17 | 2.1 | 2 | 0.3 | 11.986 | 0.001 |
| 36. Being promoted | 0 | 0 | 0 | 0 | - | - |
| 37. Quarreling with boss | 12 | 1.5 | 1 | 0.1 | 9.385 | 0.002 |
| 38. Leaving the job | 18 | 2.3 | 5 | 0.6 | 7.456 | 0.006 |
| 39. Spouse leaving the job | 8 | 1.0 | 1 | 0.1 | 4.023 | 0.045 |
| 40. Decrease in income | 52 | 6.6 | 56 | 7.1 | 0.159 | 0.690 |
| 41. Quitting school | 7 | 0.9 | 1 | 0.1 | 3.141 | 0.076 |
| 42. Being frustrated in school/work | 5 | 0.6 | 4 | 0.5 | 0.000 | 1.000 |
| Health/Hospital | 141 | 17.8 | 133 | 16.8 | 0.283 | 0.595 |
| 43. Being diagnosed of terminal illness | 16 | 2.0 | 5 | 0.6 | 5.839 | 0.016 |
| 44. Hospitalization | 60 | 7.6 | 19 | 2.4 | 22.397 | 0.000 |
| 45. Spouse hospitalized | 10 | 1.3 | 13 | 1.6 | 0.397 | 0.529 |
| 46. In-home assistance | 1 | 0.1 | 3 | 0.4 | 0.252 | 0.616 |
| 47. Life threatening illness parents/spouse/children | 24 | 3.0 | 29 | 3.7 | 0.488 | 0.485 |
| 48. Being injured from accident | 7 | 0.9 | 12 | 1.5 | 1.332 | 0.248 |
| 49. Close friend terminally illness | 0 | 0 | 8 | 1.0 | 6.156 | 0.013 |
| 50. Death of child | 2 | 0.3 | 1 | 0.1 | 0.000 | 1.000 |
| 51. Death of a parent | 14 | 1.8 | 14 | 1.8 | 0.000 | 1.000 |
| 52. Death of spouse | 0 | 0 | 0 | 0 | - | - |
| 53. Death of a sibling | 1 | 0.1 | 1 | 0.1 | 0.000 | 1.000 |
| 54. Death of a close relative | 32 | 4.0 | 52 | 6.6 | 5.029 | 0.025 |
| 55. Death of a close friend | 4 | 0.5 | 5 | 0.6 | 0.000 | 1.000 |
| Law/Legal | 9 | 1.1 | 5 | 0.6 | 1.153 | 0.283 |
| 56. Being victimized of a crime | 0 | 0 | 1 | 0.1 | 0.000 | 1.000 |
| 57. Serving jail time | 3 | 0.4 | 0 | 0 | 1.336 | 0.248 |
| 58. Legal trouble | 8 | 1.0 | 2 | 0.3 | 3.623 | 0.057 |
| 59. Being sued/suing someone | 5 | 0.6 | 2 | 0.3 | 0.574 | 0.449 |
| Friend/Relationship | 85 | 10.7 | 22 | 2.8 | 39.784 | 0.000 |
| 60. Tensions with friends or neighbors | 17 | 2.1 | 3 | 0.4 | 9.925 | 0.002 |
| 61. Face loss | 49 | 6.2 | 6 | 0.8 | 34.829 | 0.000 |
| 62. Being threatened | 8 | 1.0 | 1 | 0.1 | 4.023 | 0.045 |
| 63. Being sexually abused | 0 | 0 | 0 | 0 | - | - |
| 64. Daily life out of routine | 24 | 3.0 | 14 | 1.8 | 2.696 | 0.101 |
A series of NLEs and attempted suicide
The association between a series of NLEs and attempted suicide was shown in Table 3. Suicide attempters experienced more NLEs than controls (p<0.01), with a mean number of 1.83 and 0.61 respectively. The conditional logistic regression model showed that the more NLEs an individual experienced, the higher the risk of suicide. Compared to individuals who reported no NLEs, those who experienced 1 or 2 NLEs have over 5 times greater likelihood of attempting suicide and the risk increased to 12 times for those who experienced 3 or more NLEs after adjusting for demographic and psychological factors. The intensity of NLEs that suicide attempters (5.07±10.44) reported was more than that the controls (1.07±3.11). Attempters who experienced greater intensity of NLEs had over 5–17 times greater risk compared to those who experienced low intensity of NLEs. For suicide attempters, the top three categories were Marriage/Love events (44.1%), Family/Home events (31.2%) and Health/Hospital events (17.8%). Three types of NLEs including Marriage/Love, Family/Home and Friend/Relationship related life events were still significantly associated with attempted suicide even after controlling for demographic variables and mental disorders, with the adjusted OR value from 2.36 to 5.43 (p<0.05).
Table 3.
NLEs related to risk of attempted suicide by conditional logistic regression model (N=1582)
| Variable | Suicide attempters (N=791) Mean±SD/n (%) |
Controls (N=791) Mean±SD/n (%) |
OR (95%CI) | Adjusted OR (95% CI) * |
|---|---|---|---|---|
| Number | 1.83±1.77 | 0.61±1.02 | 2.22(1.95–2.52) | 1.65(1.38–1.99) |
| 0 | 189(24.7) | 494(64.9) | 1 | 1 |
| 1–2 | 428(55.9) | 229(30.1) | 6.07(4.49–8.20) | 5.40(3.84–7.59) |
| 3 | 149(19.5) | 38(5.0) | 16.97(10.80–26.67) | 12.69(7.51–21.44) |
| Intensity | 5.07±10.44 | 1.07±3.11 | 1.286(1.22–1.34) | 1.17(1.10–1.24) |
| 0 | 238(30.1) | 573(72.4) | 1 | 1 |
| 1–16 | 518(65.5) | 213(26.9) | 5.83 (4.49–7.58) | 4.20(2.83–6.23) |
| >16 | 35(4.4) | 5(0.6) | 17.94 (6.65–48.44) | 4.48(0.53–38.13) |
| Category | ||||
| Marriage/Love | 349(44.1) | 45(5.7) | 6.03(4.37–8.31) | 5.43(3.81–7.76) |
| Family/Home | 247(31.2) | 97(12.3) | 2.48(1.93–3.20) | 2.46(1.83–3.30) |
| Work/Business | 94(11.9) | 70(8.8) | - | - |
| Health/Hospital | 141(17.8) | 133(16.8) | - | - |
| Law/Legal | 9(1.1) | 5(0.6) | - | - |
| Friend/Relationship | 85(10.7) | 22(2.8) | 3.29 (1. 91–5.68) | 2.36(1.31–4.25) |
Adjusted for education level, occupation, family annual income, family history of suicide, physical illness, and mental disorders. P<0.05
Specific NLEs and attempted suicide
We also studied the impact of NLEs on suicide attempters between the genders. Specific NLEs associated with attempted suicide were analyzed by a series of conditional logistic regressions adjusted with demographic characteristics. 17 NLEs were significantly related to elevated risk of attempting suicide in all 1582 respondents. Quarrelling with family had the highest risk (OR=26.56) with 17.4% in all partcipants. The highest frequency of negative life events (34.5%) in suicide attempters was quarreling with partner (OR=23.67). There were 5 events (Disappointed in love affair, Quarreling with partner, Quarreling with family, Tensions with friends or neighbor and Face-loss) out of the 17 NLEs in male respondents that were associated with increased risk of attempted suicide. For female counterparts, there were 10 out of the 17 NLEs still significantly related to increased suicidal risk. Of the 10 NLEs, 7 are about interpersonal relationships. Rural women were more likely to be vulnerable to interpersonal conflicts than rural men. Hospitalization was the unique life event significantly associated with increased risk of attempted suicide in female respondents. See Table 4.
Table 4.
The frequency and suicide risk of negative life events in suicide attempters by gender (N=1582)
| Negative life event | Total (N=1582) | Female (N=586) | Male (N=996) | |||
|---|---|---|---|---|---|---|
|
| ||||||
| Frequency (%)# | Adjusted OR* (95%CI) | Frequency (%)# | Adjusted OR* (95%CI) | Frequency (%)# | Adjusted OR* (95%CI) | |
| 3 Disappointed in love affair | 2.9/0.4 | 10.49(2.21–49.65) | - | - | 5.8/0.7 | 22.66(1.00–509.73) |
| 4 Separated due to discord | 3.3/0.8 | 4.85(1.73–13.63) | 3.0/0.6 | 5.11(1.47–17.78) | - | - |
| 5 Living apart from spouse | 2.1/0.3 | 5.07(1.60–16.09) | - | - | - | - |
| 7 Spouse unfaithful | 3.9/0 | 12.21(2.74–54.31) | - | - | - | - |
| 11 Quarreling with partner | 34.5/2.4 | 23.67(12.67–44.22) | 38.2/2.4 | 24.98(13.70–45.55) | 28.3/2.4 | 12.46(4.80–32.36) |
| 12 Fighting with partner | 8.8/1.8 | 4.53(2.34–8.74) | 10.8/2.0 | 5.94(2.99–11.80) | - | - |
| 13 Physically abused | 4.0/0.4 | 14.13(3.15–63.26) | 5.6/0.4 | 12.52(2.62–59.73) | - | - |
| 18 Quarreling with family | 17.4/0.9 | 26.56(10.23–68.97) | 15.1/1.0 | 16.00(5.70–44.85) | 21.5/0.7 | 130.00(12.15–1390.41) |
| 23 Discord with spouse’s mother | 4.0/0.3 | 11.02(3.02–40.25) | 5.0/0.4 | 10.03(2.57–39.15) | - | - |
| 24 Having a baby | 0.9/0.1 | 9.34(1.04–83.66) | - | - | - | - |
| 26 Abortion (wife) | 1.9/0.8 | 4.92(1.57–15.46) | 2.4/0.8 | 7.05(1.57–31.61) | - | - |
| 35 Laid off/unemployed | 2.1/0.3 | 14.70(1.82–118.64) | - | - | - | - |
| 37 Quarreling with boss | 1.5/0.1 | 26.10(2.34–290.34) | - | - | - | - |
| 38 Leaving the job | 2.3/0.6 | 4.35(1.14–16.61) | - | - | - | - |
| 44 Hospitalization | 7.6/2.4 | - | 8.0/2.0 | 2.34(1.04–5.28) | - | - |
| 60 Tensions with friends/neighbors | 2.1/0.4 | 12.01(2.53–56.97) | 2.8/0.4 | 8.50(1.04–69.32) | 1.0/0.3 | 11.94(1.21–117.29) |
| 61 Face-loss | 6.2/0.8 | 5.91(2.34–14.93) | 4.4/0.4 | 11.29(2.31–54.98) | 9.2/1.4 | 4.24(1.10–16.33) |
Adjusted for education level, occupation, family annual income, and family history of suicide.
refers to proportion of NLEs in suicide attempters and controls, respectively.
The Impact of Negative Life Events on Attempted Suicide
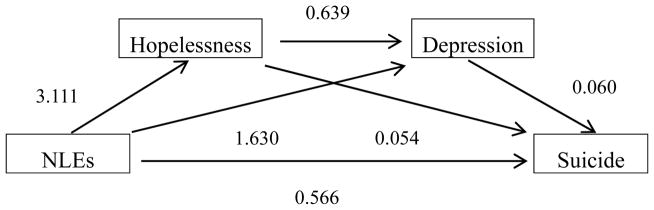
Table 5 shows results of the mediation analyses with number of NLEs as the independent variable, scores of depression and hopelessness as the mediator, and suicide attempts as the dependent variable. The mediation model (see Figure 1) was perfomed using logistic regression. The total and direct effect of negative life events on suicide was approximately 0.676 (SE = 0.056, p< 0.001), and 0.502 (SE = 0.062, p< 0.001) with a standardized coefficient of 0.566 (SE = 0.230, p<0.001), respectively. The total indirect effect of negative life events on suicide mediated by hopelessness and depression was about 0.302 (SE = 0.035, 95%CI=0.2351–0.3702). As zero is not included in the 95% confidence interval by bootstrapping analyses with 5000 resamples, it can be concluded that the indirect effect (mediation effect) is significant. Path analyses were conducted to evaluate the direct and indirect effect of negative life events on suicidality. All the path coefficients were standardized regression weighted and reported in Figure 1 (p<0.05). Only the significant paths were displayed.
Table 5.
The effect of negative life events (NLEs) on suicide attempt (N=1582)
| Path | Effect | SE | z | P | LLCI | ULCI |
|---|---|---|---|---|---|---|
| Total Effects of NLEs on Suicide | 0.6761 | 0.0557 | 12.1380 | 0.000 | 0.5669 | 0.7853 |
| Direct Effects of NLEs on Suicide | 0.5019 | 0.0628 | 7.9897 | 0.000 | 0.3788 | 0.6250 |
| Bootstrap LLCI |
Bootstrap ULCI |
|||||
| Total Indirect Effects of NLEs on Suicide | 0.3016 | 0.0348 | 0.2351 | 0.3702 | ||
| NLEs on Suicide by Hopelessness | 0.1216 | 0.0214 | 0.0819 | 0.1654 | ||
| NLEs on Suicide by Hopelessness and Depression | 0.0924 | 0.0159 | 0.0642 | 0.1258 | ||
| NLEs on Suicide by Depression | 0.0877 | 0.0176 | 0.0581 | 0.1261 |
Figure 1.
The mediation effect model of NLEs on the relationship between hopelessness, depression and attempted suicide
DISCUSSION
In this sample of Chinese rural suicide attempters, we have provided more empirical evidence in surport of the notion that negative life events played a significant role in predicting suicidal behavior. Our study revealed that suicide attempters suffered more negative life events than those non-suicidal people. In our study, about 79.3% suicide attempters experienced at least one negative life event before the suicidal behavior. Another more recent study showed that 83.1% of the attempters’ negative life events had occurred over the past year (Zhang et al., 2015) and about 92.3% of suicide victims had experienced at least one type of negative life events in rural China (Zhang & Ma, 2012).
NLEs were significanltly correlated with increased risk of attempted suicide in China (Jiang et al., 2013; Y. Li et al., 2012; Liu et al., 2016). Psychological strain can explain the phenomenon and it postluates that strain resulted from at least two conflicting stressors (Zhang, 2005; Zhang & Song, 2006). When someone confronts a life crisis and is not able to resolve it, he or she experiences coping strain. Psychological strain are presumed to be the underlying reason for suicide since the conflicting pressures are so unbearable that the victims kill themselves to escape from the sufferings (Stack & Wasserman, 2007).
Marriage/love, family/home and friend/relationship events were independently associated with attempted suicide after adjusting for demographic factors, which was consistent with studies on suicidal victims in rural China (Zhang & Ma, 2012). Notably, there were many negative life events about interpersonal relationships such as quarreling with partner, family or friends, etc. It has also been found that most negative life events that rural suicide victims with depression experienced include interpersonal relationships (Jia & Zhang, 2015b). By contrast, we did not find financial troubles and health problems in the 17 NLEs, which were more commonly reported among suicidal population in Western societies (Foster, 2011) and Chinese completed suicides (Zhang et al., 2004). It seems that negative life events affecting suicidal behavior mainly are due to psychological reasons rather than material and physical health reasons. In a collectivism culture, people might get mutual social support in dealing with life stresses (Triandis, 2000). Contrary to western cultures focusing on individualism, Chinese traditional society emphasise family and work group goals above individual needs (Jia & Zhang, 2015a). The Chinese family are collectivistic within family relationship and family bonds while individualistic at the community and society levels (Zhang, 2000). Once a Chinese rural individual came across negative life events about interpersonal relationship, he may be isolated with low social cohesion. It affects the individual’s sense of purpose, security and connectedness and leads to suicide as a way to cope with the difficulty (WHO, 2014). The results affirm the importance of supportive relationships to mitigate the harmful effects of negative life events on mental health.
The differences in nagetive life events can explain the gender difference in psychopathology in Asian (Park et al., 2015) and European patients (Dalgard et al., 2006). It is clear that female individuals suffer from more negative life events than her counterparts. Confucianism imposes heavy burdens on women, for example, accepting an arranged marriage, bearing a son to continue her husband’s family heritage, and serving her husband and the senior family members (Zhang & Liu, 2012a). The inferior status of Chinese women (below that of men and senior family members) and the Confucian ethic of female subordination makes them more vulnerable to family adversity (Zhang & Liu, 2012b). Thus, such life events as fighting with partner will be experienced differently by women from that of men. Additionally, rural women are often particularly susceptible to problems with relationships due to their difficulty in expressing their anger because of the cultural transitions based on the legacy of Confucian traditions (Jia & Zhang, 2015b). In all, rural individuals affected by negative life events tend to seek death as a solution to solve the problems due to the lack of coping mechanism and social support system (Zhang et al., 2004). For suicide prevention practice in Chinese rural areas, cultural aspects should be considered together with measures to enhance coping strategies and social support system especially for women.
In this study, the association between negative life events and suicidal behaviors can be explained by a model with depression and hopelessness as mediators. We identified that negative life events directly cause attempted suicide as a result to cope with or avoid the difficulties and stress caused (Beautrais, 2000). The indirect effects of negative life events on attempted suicide included the mediated effect of hopelessness and depression through the mechanism of generating and aggravating psychiatric symptoms (Horesh et al., 2011). This supports previous studies indicating that depression can mediate the association of negative life events with suicidality (Hardt & Johnson, 2010; Park et al., 2015) and risk of suicide attempts increases with the increase in hopelessness (Jaiswal et al., 2016). Suicidal attempts were largely attributable to depression and hopelessness (Cheung et al., 2006). Hopelessness was highly correlated with depression and sensitivity to depression. NLEs may be considered as a predictive factor rather than a sufficient factor. It highlights that it may be effective to assess and intervene depressed and hopeless patients who experienced NLEs even if they do not show severe psychopathology.
Finally, consistent with previous studies in China, the results also suggested that lower education level (Liu et al., 2016), being farmers (Jiang et al., 2013), having pesticide stored at home (Zhang et al., 2006), family suicide history (Conner et al., 2007), physical illness (Zhao et al., 2010), mental disorders (X. Li et al., 2012) were significantly associated with elevated risk of suicide attempts. The lower prevalence of mental disorders in our study may be due to the difference in prevalence of mental disorders in the general population in China. This fact, from a new angle, shows that there may be more important factors than mental illness contributing to suicide. All those potential risk factors require further studying on the associations with suicide attempts.
Several limitations of the study should be noted. Firstly, the data was obtained from suicide attempters whose injury and wounds need hospitalization, and the samples cannot represent suicide attempters who did not need medical care. Secondly, given that negative life events may also cause biological stress systems imbalance and lead to suicidal behavior (Sunnqvist et al., 2008), the biological mechanism of NLEs on suicidal behavior also needs to be further studied. Thirdly, results may not be generalizable to all suicide attempters in the cross-sectional study. Future studies may include new population in China or other countries.
Despite these limitations, our study still contributes to our understanding of the mechanism of how negative life events affect suicidal behavior. The major findings were that negative life events played a crucial role in predicting suicidal behavior and can be mediated by depression and hopelessness. Evaluation and intervention of hopelessness and depression would be helpful to prevent suicide induced by negative life events.
Acknowledgments
The research was supported by the United States National Institute of Mental Health (NIMH): R01 MH068560. We also thank all interviewers for their unique contribution to the study.
The authors declared that they had no conflicts of interest with respect to their authorship or the publication of this article.
References
- Bagge CL, Glenn CR, Lee HJ. Quantifying the impact of recent negative life events on suicide attempts. Journal of abnormal psychology. 2013;122(2):359–368. doi: 10.1037/a0030371. [DOI] [PubMed] [Google Scholar]
- Beautrais AL. Risk factors for suicide and attempted suicide among young people. Australian and New Zealand Journal of Psychiatry. 2000;34(3):420–436. doi: 10.1046/j.1440-1614.2000.00691.x. [DOI] [PubMed] [Google Scholar]
- Beck AT. Beck Hopeless Scale. San Antonio, TX: Psychological Corporation; 1978. [Google Scholar]
- Brown GK, Ten Have T, Henriques GR, Xie SX, Hollander JE, Beck AT. Cognitive therapy for the prevention of suicide attempts: a randomized controlled trial. Jama. 2005;294(5):563–570. doi: 10.1001/jama.294.5.563. [DOI] [PubMed] [Google Scholar]
- Cheung YB, Law CK, Chan B, Liu KY, Yip PSF. Suicidal ideation and suicidal attempts in a population-based study of Chinese people: risk attributable to hopelessness, depression, and social factors. Journal of affective disorders. 2006;90(2–3):193–199. doi: 10.1016/j.jad.2005.11.018. [DOI] [PubMed] [Google Scholar]
- Conner KR, Phillips MR, Meldrum SC. Predictors of low-intent and high-intent suicide attempts in rural China. American Journal of Public Health. 2007;97(10):1842–1846. doi: 10.2105/ajph.2005.077420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui S, Yang R, He F, Zheng Y. Case-control analysis and follow-up study on risk factors of suicide attempt in a rural population in Shandong Province. Journal of Hygiene Research. 2003;32(6):562–564. [PubMed] [Google Scholar]
- Dalgard OS, Dowrick C, Lehtinen V, Vazquez-Barquero JL, Casey P, Wilkinson G, Ayuso-Mateos JL, Page H, Dunn G, Group O. Negative life events, social support and gender difference in depression: a multinational community survey with data from the ODIN study. Social psychiatry and psychiatric epidemiology. 2006;41(6):444–451. doi: 10.1007/s00127-006-0051-5. [DOI] [PubMed] [Google Scholar]
- Dieserud G, Forsen L, Braverman MT, Roysamb E. Negative Life Events in Childhood, Psychological Problems and Suicide Attempts in Adulthood: A Matched Case-Control Study. Archives of suicide research. 2002;6(4):291–308. doi: 10.1080/13811110214525. [DOI] [Google Scholar]
- Dohrenwend BS, Krasnoff L, Askenasy AR, Dohrenwend BP. Exemplification of a method for scaling life events: the Peri Life Events Scale. Journal of Health and Social Behavior. 1978;19(2):205–229. [PubMed] [Google Scholar]
- Foster T. Adverse life events proximal to adult suicide: a synthesis of findings from psychological autopsy studies. Archives of suicide research. 2011;15(1):1–15. doi: 10.1080/13811118.2011.540213. [DOI] [PubMed] [Google Scholar]
- Gu J, Chen Y. Instruction Manual for the Structured Clinical Interview for DSM-III-R (Chinese Edition) Kaohsiung: Kaohsiung Medical College, Taiwan; 1993. [Google Scholar]
- Hardt J, Johnson JG. Suicidality, depression, major and minor negative life events: a mediator model. Psycho-social medicine. 2010;7:1–8. doi: 10.3205/psm000067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. Guilford Press; 2013. [Google Scholar]
- Horesh N, Apter A, Zalsman G. Timing, quantity and quality of stressful life events in childhood and preceding the first episode of bipolar disorder. Journal of Affective Disorders. 2011;134(1–3):434–437. doi: 10.1016/j.jad.2011.05.034. [DOI] [PubMed] [Google Scholar]
- Jaiswal SV, Faye AD, Gore SP, Shah HR, Kamath RM. Stressful life events, hopelessness, and suicidal intent in patients admitted with attempted suicide in a tertiary care general hospital. Journal of postgraduate medicine. 2016;62(2):102–104. doi: 10.4103/0022-3859.180556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jia C-X, Zhang J. Confucian Values, Negative Life Events, and Rural Young Suicide with Major Depression in China. OMEGA-Journal of Death and Dying. 2015a doi: 10.1177/0030222815575014. 0030222815575014. [DOI] [PubMed] [Google Scholar]
- Jia C-X, Zhang J. Confucian values, negative life events, and rural young suicide with major depression in China. OMEGA - Journal of Death and Dying, ePub. 2015b:1–12. doi: 10.1177/0030222815575014. ePub. [DOI] [PubMed] [Google Scholar]
- Jiang C, Li X, Phillips MR, Xu Y. Matched case-control study of medically serious attempted suicides in rural China. Shanghai archives of psychiatry. 2013;25(1):22–31. doi: 10.3969/j.issn.1002-0829.2013.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kay N, Li K, Xiao X, Nokkaew N, Park BH. Hopelessness and Suicidal Behavior among Chinese, Thai and Korean College Students and Predictive Effects of the World Health Organization’s WHOQOL-BREF. International Electronic Journal of Health Education. 2009;12:16–32. [Google Scholar]
- Li X, Phillips M, Zhang Y. The study of the validity of a suicide-specific life event scale and suicide behavior. Chinese Journal of Nervous and Meatal Disease. 2008;34(3):156–160. doi: 10.3969/j.issn.1002-0152.2008.03.008. [DOI] [Google Scholar]
- Li X, Phillips MR, Cohen A. Indepth interviews with 244 female suicide attempters and their associates in northern China: understanding the process and causes of the attempt. Crisis. 2012;33(2):66–72. doi: 10.1027/0227-5910/a000108. [DOI] [PubMed] [Google Scholar]
- Li Y, Li Y, Cao J. Factors associated with suicidal behaviors in mainland China: a meta-analysis. BMC public health. 2012;12(1):524. doi: 10.1186/1471-2458-12-524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu BP, Liu X, Jia CX. Characteristics of suicide completers and attempters in rural Chinese population. Comprehensive Psychiatry. 2016;70:134–140. doi: 10.1016/j.comppsych.2016.07.005. [DOI] [PubMed] [Google Scholar]
- Liu X, Tein JY. Life events, psychopathology, and suicidal behavior in Chinese adolescents. Journal of Affective Disorders. 2005;86(2–3):195–203. doi: 10.1016/j.jad.2005.01.016. [DOI] [PubMed] [Google Scholar]
- McFeeters D, Boyda D, O’Neill S. Patterns of stressful life events: distinguishing suicide ideators from suicide attempters. Journal of affective disorders. 2015;175:192–198. doi: 10.1016/j.jad.2014.12.034. [DOI] [PubMed] [Google Scholar]
- Osvath P, Vörös V, Fekete S. Life events and psychopathology in a group of suicide attempters. Psychopathology. 2004;37(1):36–40. doi: 10.1159/000077018. [DOI] [PubMed] [Google Scholar]
- Park S, Hatim Sulaiman A, Srisurapanont M, Chang S-m, Liu CY, Bautista D, Ge L, Choon Chua H, Pyo Hong J. The association of suicide risk with negative life events and social support according to gender in Asian patients with major depressive disorder. Psychiatry Research. 2015;228(3):277–282. doi: 10.1016/j.psychres.2015.06.032. [DOI] [PubMed] [Google Scholar]
- Paykel ES. The Interview for Recent Life Events. Psychological Medicine. 1997;27(2):301–310. doi: 10.1017/S0033291796004424. [DOI] [PubMed] [Google Scholar]
- Paykel ES, Prusoff BA, Uhlenhuth EH. Scaling of life events. Archives of General Psychiatry. 1971;25(4):340–347. doi: 10.1001/archpsyc.1971.01750160052010. [DOI] [PubMed] [Google Scholar]
- Phillips MR, Li X, Zhang Y. Suicide rates in China, 1995–99. The Lancet. 2002;359(9309):835–840. doi: 10.1016/S0140-6736(02)07954-0. [DOI] [PubMed] [Google Scholar]
- Phillips MR, Yang G, Zhang Y, Wang L, Ji H, Zhou M. Risk factors for suicide in China: a national case-control psychological autopsy study. Lancet (London, England) 2002;360(9347):1728–1736. doi: 10.1016/s0140-6736(02)11681-3. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale a self-report depression scale for research in the general population. Applied psychological measurement. 1977;1(3):385–401. [Google Scholar]
- Spitzer RL, Williams JBW, Gibbon M, First AB. Instruction Manual for the Structured Clinical Interview for DSM-III-R (SCID, 6/1/88 Revision) New York: Biometrics Research Department, New York State Psychiatric Institute; 1988. [Google Scholar]
- Stack S, Wasserman I. Economic strain and suicide risk: a qualitative analysis. Suicide & Life-threatening Behavior. 2007;37(1):103–112. doi: 10.1521/suli.2007.37.1.103. [DOI] [PubMed] [Google Scholar]
- Sunnqvist C, Westrin A, Traskman-Bendz L. Suicide attempters: biological stressmarkers and adverse life events. European Archives of Psychiatry and Clinical Neuroscience. 2008;258(8):456–462. doi: 10.1007/s00406-008-0819-6. [DOI] [PubMed] [Google Scholar]
- Triandis HC. Cultural syndromes and subjective well-being. Culture and Subjective Well-being. 2000:13–36. [Google Scholar]
- WHO. Preventing suicide: A global imperative. Geneva: World Health Organization; 2014. [Google Scholar]
- WHO. World health statistics 2016: monitoring health for the SDGs, sustainable development goals. Geneva: World Health Organization; 2016. [Google Scholar]
- Wu J, Wu YT, Feng SX, Meng H, Chen H. Mediating effects on depression regarding the relationship between negative life events and suicide ideation among college students. Zhonghua Liu Xing Bing Xue Za Zhi. 2012;33(11):1111–1114. [PubMed] [Google Scholar]
- Yang D, Zhang Y. Life Event Scale. In: Xiangdong W, Xinlin W, Hong M, editors. The Mental Health Scale (Revised Edition) Beijing: Chinese Mental Health Journal Publisher; 1999. pp. 101–108. [Google Scholar]
- Yen S, Pagano ME, Shea MT, Grilo CM, Gunderson JG, Skodol AE, McGlashan TH, Sanislow CA, Bender DS, Zanarini MC. Recent life events preceding suicide attempts in a personality disorder sample: findings from the collaborative longitudinal personality disorders study. Journal of consulting and clinical psychology. 2005;73(1):99–105. doi: 10.1037/0022-006x.73.1.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J. Collectivism or individualism: An analysis of Chinese interactive culture. American Review of China Studies. 2000;1(2):57–65. [Google Scholar]
- Zhang J. Conceptualizing a Strain Theory of Suicide (Review) Chinese Mental Health Journal. 2005;19(11):778–782. [Google Scholar]
- Zhang J, Conwell Y, Wieczorek WF, Jiang C, Jia S, Zhou L. Studying Chinese suicide with proxy-based data: reliability and validity of the methodology and instruments in China. The Journal of Nervous and Mental Disease. 2003;191(7):450–457. doi: 10.1097/01.nmd.0000081613.03157.d9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J, Conwell Y, Zhou L, Jiang C. Culture, risk factors and suicide in rural China: a psychological autopsy case control study. Acta Psychiatrica Scandinavica. 2004;110(6):430–437. doi: 10.1111/j.1600-0447.2004.00388.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J, Jia S, Jiang C, Sun J. Characteristics of Chinese suicide attempters: an emergency room study. Death Studies. 2006;30(3):259–268. doi: 10.1080/07481180500493443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J, Liu EY. The confucian ethic of female subordination and depression among young people in rural China. Interdisciplinary Journal of Research on Religion. 2012a;8:3. [Google Scholar]
- Zhang J, Liu EY. Confucianism and youth suicide in rural China. Review of Religious Research. 2012b;54(1):93–111. [Google Scholar]
- Zhang J, Lv J. Psychological strains and depression in Chinese rural populations. Psychology, health & medicine. 2014;19(3):365–373. doi: 10.1080/13548506.2013.808752. [DOI] [PubMed] [Google Scholar]
- Zhang J, Ma Z. Patterns of life events preceding the suicide in rural young Chinese: a case control study. Journal of Affective Disorders. 2012;140(2):161–167. doi: 10.1016/j.jad.2012.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J, Song ZS. A Preliminary Test of the Strain Theory of Suicide. Chinese Journal of Behavioral Medical Science. 2006;15(6):487–489. (in Chinese) [Google Scholar]
- Zhang J, Sun W, Kong Y, Wang C. Reliability and validity of the Center for Epidemiological Studies Depression Scale in 2 special adult samples from rural China. Comprehensive Psychiatry. 2012;53(8):1243–1251. doi: 10.1016/j.comppsych.2012.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J, Wieczorek WF, Conwell Y, Tu XM. Psychological strains and youth suicide in rural China. Social science & medicine (1982) 2011;72(12):2003–2010. doi: 10.1016/j.socscimed.2011.03.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J, Xiao S, Zhou L. Mental disorders and suicide among young rural Chinese: a case-control psychological autopsy study. American Journal of Psychiatry. 2010;167(7):773–781. doi: 10.1176/appi.ajp.2010.09101476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang WC, Jia CX, Zhang JY, Wang LL, Liu XC. Negative life events and attempted suicide in rural China. PLoS One. 2015;10(1):e0116634. doi: 10.1371/journal.pone.0116634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao P, Yang R, Phillips MR. Age-specific characteristics of serious suicide attempters in China. Suicide & life-threatening behavior. 2010;40(4):383–393. doi: 10.1521/suli.2010.40.4.383. [DOI] [PubMed] [Google Scholar]