Abstract
Introduction
The objective of this study was to assess the differences in HPV-related knowledge, attitudes, and beliefs among African American and non-Hispanic white women and to determine their communication preferences for cancer-related information.
Methods
Data was obtained from the National Cancer Institute's (NCI) 2014 Health Interview National Trends Survey (HINTS), a cross-sectional survey of U.S. adults 18 years of age or older. Descriptive statistics, bivariate and multivariate logistic regression were used to identify differences in awareness and knowledge. Data was collected in 2014 and analyzed in 2016.
Results
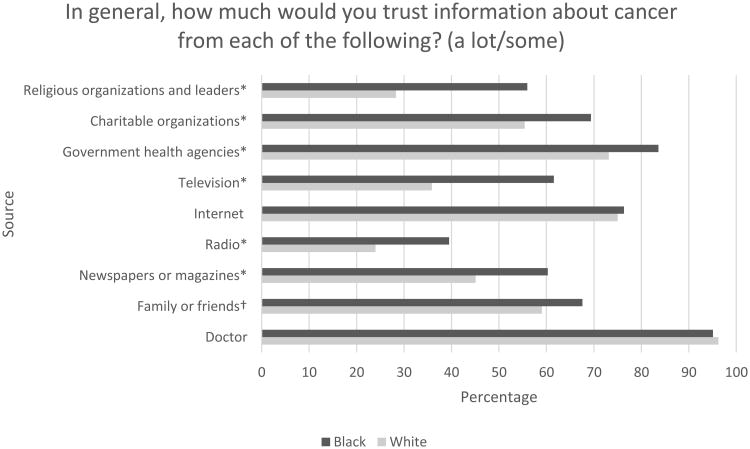
HPV awareness (71% vs. 77%) and knowledge that HPV causes cervical cancer (64% vs. 81%) was significantly lower among blacks. Additionally, there were significant disparities in awareness of the HPV vaccine (66% vs. 79%), with only 25% of Black women indicating that they or a family member was recommended the HPV vaccine by a health care professional. There were also differences in cancer communication preferences. Blacks were more likely than Whites to trust cancer information from family (OR 2.7, confidence interval [CI] 0.725-10.048), television (OR 3.0, 95% [CI] 0.733-12.296), government health agencies (OR 5.8, [CI] 0.639-52.818), and religious organizations (OR 6.4, 95% [CI] 1.718-23.932).
Conclusion
Study results indicate that racial/ethnic differences exist in HPV knowledge/awareness and cancer communication preferences. These results highlight the need to increase HPV prevention and education efforts using methods that are tailored to Black women. To address HPV/cervical cancer disparities, future interventions should utilize preferred communication outlets to effectively increase HPV knowledge and vaccine awareness.
Introduction
Cervical cancer is the fourth most common cancer among all women worldwide. In the United States (U.S.), there are disproportionately higher incidence rates among African American women as compared to non-Hispanic Whites.1 African American women experience a 41% higher incidence of cervical cancer and are twice as likely to die from this disease in comparison to non-Hispanic White women.3 It is estimated that 2290 new cases of invasive cervical cancer and 750 cervical cancer deaths will occur among African American women in the U.S. in 2016.3 These disparities in cervical cancer incidence and mortality are completely preventable and largely attributed to a) socioeconomic disparities and b) lack of treatment and utilization of care. With the annual Papanicolaou (Pap) test, most cervical neoplasias, the precancerous form of cervical cancer, can be detected and treated before they become malignant. Likewise, cervical cancer can be prevented by the human papillomavirus (HPV) vaccine that protects against the most common cancer-causing HPV infections.2
Human papillomavirus is the most common sexually transmitted virus in the U.S. and is responsible for causing almost all cervical cancers.4,5 It is also known to cause most vaginal, vulvar, anal, rectal, penile, and oropharyngeal cancers (American Cancer Society, 2015). The Centers for Disease Control and Prevention (CDC) estimates about 79 million Americans are currently infected with HPV and an additional 14 million become infected each year.6
There are three HPV vaccines (Gardasil®, Gardasil 9®, and Ceravix®) approved by the US Food and Drug Administration (FDA) for females.7,8, 9 All three vaccines are effective against high-risk HPV genotypes 16 and 18, which account for approximately 70% of cervical cancers worldwide.8 Quadrivalent Gardasil also protects against HPV types 6 and 11, which are responsible for approximately 90% of genital warts. Gardasil 9 additionally protects against five high-risk types 31, 33, 45, 52, and 58.9 The vaccines consist of three doses given over a six-month period. The blanket recommendation from the Advisory Committee on Immunization Practices (ACIP) is that the vaccine be given to adolescents age 11 to 12, at the same time as the tetanus–diphtheria–acellular pertussis (Tdap) vaccine and the meningococcal vaccine.10 The vaccine can also be administered to females between the ages of 9 and 26.
The HPV vaccine is covered under most private insurance plans in accordance with the Affordable Care Act (ACA) which requires coverage for recommended preventive services. Uninsured adolescents 18 years and under are also able to receive the vaccine at no cost via the Vaccines for Children (VFC) Program, Children's Health Insurance Program (CHIP), or Medicaid. Despite the widespread availability of vaccines targeting HPV, vaccination uptake remains lower than desired. The goal of Healthy People 2020 is to have 80% of adolescent girls vaccinated by 2020. As of 2014, only 34.4% of adolescent females ages 13 to 15 received three doses of the HPV vaccine, despite this being a slight increase from the 2013 rate of 32.7%.11 Thus, additional efforts to increase uptake of the HPV vaccine are needed, including addressing the barriers to care.
There are several barriers to HPV vaccination including the individual factors such as lack of HPV vaccine knowledge and awareness, misinformation about HPV transmission, as well as the system-level factors of lack of effective patient-provider education and provider recommendation of the HPV vaccine.12,13 Lack of access to accurate, actionable healthcare information has been suggested as a contributing factor to disparities in HPV transmission and cervical cancer prevention.14 Previous studies indicate that provider recommendation is associated with increased uptake of vaccines15,16 and lack of physician recommendation is one of the most cited reasons for not vaccinating women.17 In order to increase HPV vaccination rates, public health interventions to increase HPV knowledge and awareness and reduce vaccination barriers are necessary. Furthermore, to specifically address the disparities in HPV-related information, communication strategies need to be tailored to African American women. In doing so, we may reduce the gaps in HPV knowledge, attitudes, and beliefs among African American women and potentially narrow and eliminate the cervical cancer disparity.
Regarding HPV awareness, previous studies have demonstrated differences among ethnic minority women in the UK18, among caregivers of adolescent girls age 10 to 18 in North Carolina14, among adult women in the U.S.19, among young females aged 18-2420, and among U.S. adults prior to HPV vaccine licensure.21 These studies were limited by geographic location, small convenience samples, or a narrow array of measures, thus limiting generalizability of their findings.
The purpose of this study is to assess the differences in HPV-related knowledge, attitudes, and beliefs between African American and non-Hispanic White women in the U.S. We also examined the differences in cancer communication methods between these two groups. To our knowledge, no other studies have examined racial differences in preference between various sources of cancer information. This study examines a wide variety of HPV-related measures using a recently surveyed large sample of the U.S. population. Thus, it provides a more current depiction of HPV knowledge, attitudes, and beliefs among women in the U.S.
Methods
Data source
Data was obtained from the National Cancer Institute's (NCI) 2014 Health Information National Trends Survey (HINTS) Cycle 4, a cross-sectional survey of U.S. adults 18 years of age or older. Data was collected from August through November 2014 via mailed questionnaires (N=3,742, response rate= 34.44%). A two-stage design was utilized. A full HINTS 4 methodology report has been provided by the NCI.22
Outcome variables
Survey participants were asked four HPV knowledge and awareness questions. These included: (1) Have you ever heard of HPV? HPV stands for Human Papillomavirus. It is not HIV, HSV, or herpes (yes/no). Those who responded yes were asked the following follow-up questions: (2) Do you think HPV can cause cervical cancer? (yes/no/not sure); (3) Do you think that HPV is a sexually transmitted disease (STD)? (yes/no/not sure); and (4) Do you think HPV requires medical treatment or will it usually go away on its own without treatment? (requires medical treatment/will usually go away on its own).
All participants were then asked the following questions on HPV vaccine knowledge, awareness, and beliefs: (5) A vaccine to prevent HPV infection is available and is called the HPV shot, cervical cancer vaccine, GARDASIL®, or Cervarix®. Before today, have you ever heard of the cervical cancer vaccine or HPV shot? (yes/no); (6) In your opinion, how successful is the HPV vaccine at preventing cervical cancer? (not at all successful/ a little successful/ pretty successful/ very successful/ don't know); and (7) Including yourself, is anyone in your immediate family between the ages of 9 and 27 years old? (yes/no). Participants who responded yes to the last question were asked the following follow-up questions on HPV vaccine recommendations: (8) In the last 12 months, has a doctor or health care professional ever talked with you or an immediate family member about the HPV shot or vaccine? (yes/no/don't know) and (9) In the last 12 months, has a doctor or health care professional recommended that you or someone in your immediate family get an HPV shot or vaccine?
In regards to the degree of trust in various sources of cancer information, participants were also asked the following question: In general, how much would you trust information about cancer from each of the following? (A doctor/ family or friends/ newspapers or magazines/ radio/internet/ television/ government health agencies/ charitable organizations/ religious organizations and leaders).
Statistical analyses
Statistical analyses were conducted using Statistical Analysis System (SAS), version 9.3. Weighted, unadjusted prevalence estimates were calculated for HPV-related items in HINTS 4, Cycle 4 and bivariate logistic regression was used to evaluate all outcome measures. Multivariate logistic regression analyses were then conducted for the statistically significant variables from the bivariate analyses. Weighted data reflect the national female population. Missing data was excluded from analyses. For logistic regression, responses to questions 2, 3, 8, and 9 were dichotomized to yes vs. no/not sure. Question 6 was dichotomized to not at all successful/a little successful/ don't know vs. pretty successful/very successful.
Results
Table 1 shows the sociodemographic characteristics for the 1,468 Black and White female survey respondents. About 76% of women were non-Hispanic White and 24% were non-Hispanic Black. The majority of women were between the ages of 50 and 64, had completed at least some college, and were married or living as married.
Table 1. Sociodemographic Characteristics of Female Participants by Race (N=1468).
| Characteristic | White % (N) | Black % (N) |
|---|---|---|
| Number of women | 1109 | 359 |
| Age | ||
| 18-34 | 16 (177) | 13 (46) |
| 35-49 | 18 (197) | 29 (99) |
| 50-64 | 36 (397) | 40 (137) |
| 65-74 | 16 (178) | 13 (46) |
| 75+ | 13 (143) | 5 (19) |
| Education | ||
| Less than high school | 5 (50) | 8 (28) |
| High school graduate | 18 (202) | 21 (76) |
| At least some college | 77 (853) | 71 (254) |
| Household income | ||
| $0 to $19,999 | 17 (171) | 36 (122) |
| $20,000 to $74,999 | 48 (491) | 45 (151) |
| $75,000 or more | 34 (355) | 19 (66) |
| Marital status | ||
| Married/ living as married | 52 (567) | 28 (97) |
| Divorced/ widowed/separated | 35 (382) | 39 (137) |
| Single, never been married | 13 (143) | 33 (113) |
The results from bivariate analyses for HPV knowledge, attitudes, and beliefs are shown in Table 2. HPV awareness was significantly different between Blacks and Whites (71% vs. 77%, p=0.0153), and knowledge that HPV causes cervical cancer was significantly lower among Blacks (64% vs. 81%, p<0.001). Furthermore, only 50% of Blacks believed that HPV is an STD, compared to 68% of White women (p<0.001). At least 90% of both Black and White women believed HPV requires medical attention.
Table 2. Distribution of HPV Knowledge, Awareness, and Beliefs by Race.
| White | Black | P-value | |
|---|---|---|---|
|
|
|||
| N (%) | N (%) | ||
| Have you ever heard of HPV? | 0.0153 | ||
| Yes | 851 (77) | 252 (71) | |
| No | 255 (23) | 105 (29) | |
| Do you think HPV can cause cervical cancer? | <0.001 | ||
| Yes | 682 (81) | 157 (64) | |
| No | 161 (19) | 87 (36) | |
| Do you think that HPV is a sexually transmitted disease (STD)? | <0.001 | ||
| Yes | 575 (68) | 124 (50) | |
| No or not sure | 269 (32) | 122 (50) | |
| Do you think HPV requires medical treatment or will it usually go away on its own without treatment? | 0.0861 | ||
| Requires medical treatment | 747 (90) | 227 (94) | |
| Will usually go away on its own | 81 (10) | 15 (6) | |
| Before today, have you ever heard of the cervical cancer vaccine or HPV shot? | <0.001 | ||
| Yes | 870 (79) | 236 (66) | |
| No | 231 (21) | 119 (34) | |
| In your opinion, how successful is the HPV vaccine at preventing cervical cancer? | 0.1903 | ||
| Not at all, a little successful or don't know | 55 (15) | 17 (21) | |
| Very or pretty successful | 310 (85) | 64 (79) | |
| In the last 12 months, has a doctor or health care professional ever talked with you or an immediate family member about the HPV shot or vaccine?* | 0.2182 | ||
| Yes | 150 (36) | 48 (31) | |
| No or don't know | 266 (64) | 109 (69) | |
| In the last 12 months, has a doctor or health care professional recommended that you or someone in your immediate family get an HPV shot or vaccine?* | 0.1604 | ||
| Yes | 126 (31) | 38 (25) | |
| No or don't know | 287 (69) | 117 (75) | |
Note: Respondents to this question indicated that, including themselves, someone in their immediate family was between the ages of 9 and 27 years old
Table 2 shows results of bivariate analyses for HPV vaccine knowledge, awareness, and communication. There were significant differences in awareness of the HPV vaccine (66 % vs. 79%, p<0.001), yet the majority of Black and White women believed the HPV vaccine is very/pretty successful at preventing cervical cancer (79% vs. 85%, p=0.1903). Among women who were between the ages of 18 and 27 or who had an immediate family member between the ages of 9 and 27, only 31% of Black women and 36% of White women had discussed the vaccine with a doctor or health care professional (p=0.2182). Furthermore, among this group of women, only 25% of Black women and 31% of White women indicated that a health care professional recommended the HPV vaccine to them or a family member (p=0.1604). The degree of trust in various sources of cancer information by both Black and White women is shown in Figure 1. While over 95% of all women who responded trusted their doctors for cancer information, Black women were significantly more likely to trust all sources than White women except for the doctor and the internet.
Figure 1. Trusted Sources of Cancer Information.
*p<0.001, †p<0.005
Multivariate analyses for all significant measures are shown in Table 3. Blacks were more likely to trust cancer information a lot/some from family (OR 2.7, confidence interval [CI]=0.725-10.048), television (OR 3.0, 95% CI=0.733-12.296), government health agencies (OR 5.8, 95% CI=0.639-52.818), and religious organizations a lot/some (OR 6.4, 95% CI=1.718-23.932).
Table 3. Odds Ratios of Trusted Sources of Cancer Communication by Race.
| Variable | Unweighted OR (95% CI) | Weighted OR (95% CI) |
|---|---|---|
| Trust information about cancer from family | 2.699 (0.725 - 10.048) | 2.276 (2.066 - 2.507)* |
| Trust information about cancer from newspapers or magazines | 0.817 (0.179 - 3.736) | 0.639 (0.566 - 0.721)* |
| Trust information about cancer from radio: | 0.198 (0.039 - 1.002) | 0.261 (0.231 - 0.295)* |
| Trust information about cancer from television: | 3.001 (0.733 - 12.296) | 3.317 (2.987 - 3.684)* |
| Trust information about cancer from government health agencies | 5.808 (0.639 - 52.818) | 7.219 (5.951 - 8.757)* |
| Trust information about cancer from charitable organizations | 0.844 (0.171 - 4.174) | 0.884 (0.778 - 1.005) |
| Trust information about cancer from religious organizations or leaders | 6.412 (1.718 - 23.932)† | 8.854 (8.000 - 9.801)* |
p<0.001
When weighted to represent the female U.S. population, Black women were significantly less likely than White women to know that HPV is an STD (OR 0.41, 95% CI=0.372-0.448); to have heard of the HPV vaccine (OR 0.31, 95% CI=0.262-0.369); or to trust information about cancer from newspapers or magazines (OR 0.64, 95% CI=0.566-0.721), the radio (OR 0.26, 95% CI=0.231-0.295), or charitable organizations (OR 0.884 95% CI=0.778-1.005). However, Black women were 1.2 times more likely than White women to know that HPV causes cervical cancer (95% CI=1.061-1.32), 2.3 times more likely to trust cancer information from family (95% CI=2.066-2.507), 3.3 times more likely to trust cancer information from television (95% CI=2.987-3.684), 7.2 times more likely to trust cancer information from government health agencies (95% CI=5.951-8,757) and 8.9 times more likely to trust cancer information from religious organizations or leaders (95% CI 8.0-9.801).
Discussion
Despite high awareness of HPV among Black women (71%), awareness was lower than among White women (77%) and many Black women also lacked knowledge about its characteristics. Over a third of Black women did not know the role HPV plays in cervical cancer and half did not know that it is an STD. Only 66% of Black women had previously heard of the HPV vaccine as compared to 79% of White women.
Our findings suggest that despite the introduction of the first HPV vaccine, over ten years ago, there are significant differences in HPV-related knowledge, attitudes, and beliefs between Black and White women in the U.S. This lack of HPV and HPV vaccine knowledge potentially serves as a barrier to HPV and cervical cancer prevention. Increasing knowledge of HPV is a critical step in reducing both HPV infection and cervical cancer incidence and mortality among African American women. In addition, this finding highlights the need to increase vaccine promotion efforts, in the hopes of reaching the Healthy People 2020 goal of 80% HPV vaccination completion rate among adolescents age 13-15 years old.11
While the highest proportions of all women cited doctors as a trusted source of cancer information, HPV prevention communication between these participants and their doctors was low among both Black and White women in this study. Among women who were either vaccine-eligible or had an immediate family member who was vaccine-eligible, 69% of Blacks and 64% of Whites had not discussed the HPV vaccine with a health care professional within the past twelve months. Among the same respondents, 75% of Black women and 69% of White women were not given an HPV vaccine recommendation by a health care professional. These findings are shocking considering that previous studies highlight the importance of health care professionals providing information on HPV and the vaccine.23,24 Women who received a strong physician recommendation were four times more likely to be vaccinated.24 However, because the majority of participants in this study were not vaccine-eligible and data on the number of participants who were parents/guardians of individuals who were vaccine-eligible was not obtained, it is difficult to assess the full implications of these findings. Nonetheless, to increase HPV vaccination rates, physician based-public health interventions should be implemented to increase knowledge, awareness and acceptability of the HPV vaccines among both health care providers and patients.
Historically, African Americans have been distrustful of health care professionals.25 Prior studies indicate that distrust of government agencies have caused some African Americans to not trust cancer information from these agencies.21 However, in this study, Blacks had a high degree of trust in doctors. They were also more likely than White women to trust government health agencies, television, and family and friends. Future research should utilize various methods to disseminate information about HPV and vaccine promotion. There is a need for community based interventions targeting African American women. Based on the trusted cancer communication sources, our recommendation is that religious organizations be targeted first, followed by government agencies.
Study Limitations
There are several limitations for this study. First, since the data is cross-sectional, inferences about the representativeness of the sample cannot be established. Secondly, the HINTS survey relied on self-reported data and could be subject to bias. Additionally, the surveyed female population was older in age and well-educated, which could have affected both the relevance of HPV vaccine communication with their health care providers and their HPV knowledge.
Conclusion
The study results indicate that racial/ethnic disparities exist in HPV knowledge, attitudes, and beliefs. These results highlight the need to increase HPV prevention and education efforts using methods that are tailored to African American women. To address HPV-related cervical cancer disparities, future interventions should utilize preferred communication outlets to most effectively and accurately convey the association between HPV infection and cervical cancer and increase awareness of the HPV vaccine.
Acknowledgments
This study was supported by Award Number U54 CA118638 from the National Institutes of Health.
Footnotes
Conflict of Interest: The National Institutes of Health did not have any role in study design; collection, analysis, and interpretation of data; writing the report; and the decision to submit the report for publication.
Financial disclosure: No financial disclosures were reported by the authors of this paper.
References
- 1.American Cancer Society. Cancer Facts & Figures 2016. 2016 [Google Scholar]
- 2.American Cancer Society. Cancer Facts & Figures for African Americans 2016-2018. Atlanta: American Cancer Society; 2016. [Google Scholar]
- 3.Desantis CE, Siegel RL, Sauer AG, et al. Cancer statistics for African Americans, 2016: Progress and opportunities in reducing racial disparities. CA: A Cancer Journal for Clinicians. 2016;66(4):290–308. doi: 10.3322/caac.21340. [DOI] [PubMed] [Google Scholar]
- 4.Walboomers JMM, Jacobs MV, Manos MM, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. The Journal of Pathology. 1999;189(1):12–19. doi: 10.1002/(sici)1096-9896(199909)189:1<12∷aid-path431>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 5.Viens LJ, Henley SJ, Watson M, et al. Human Papillomavirus–Associated Cancers — United States, 2008–2012. MMWR Morbidity and Mortality Weekly Report MMWR Morb Mortal Wkly Rep. 2016;65(26):661–666. doi: 10.15585/mmwr.mm6526a1. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Centers for Disease Control and Prevention; [Accessed July 14, 2016]. Genital HPV Infection - Fact Sheet. http://www.cdc.gov/STD/HPV/STDFact-HPV.htm. Published May 19, 2016. [Google Scholar]
- 7.Siddiqui MAA, Perry CM. Human Papillomavirus Quadrivalent (types 6, 11, 16, 18) Recombinant Vaccine (Gardasil): Profile Report 1. BioDrugs. 2006;20(5):313–316. doi: 10.2165/00063030-200620050-00006. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. FDA licensure of bivalent human papillomavirus vaccine (HPV2, Cervarix) for use in females and updated HPV vaccination recommendations from the Advisory Committee on Immunization Practices (ACIP) Morbidity and Mortality Weekly Report. 2010;59(20):626–629. [PubMed] [Google Scholar]
- 9.Petrosky E, Bocchini JA, Hariri S, et al. Use of 9-Valent Human Papillomavirus (HPV) Vaccine: Updated HPV Vaccination Recommendations of the Advisory Committee on Immunization Practices. Morbidity and Mortality Weekly Report. 2015;64(11):300–304. [PMC free article] [PubMed] [Google Scholar]
- 10.Robinson CL, Child A. Advisory Committee on Immunization Practices Recommended Immunization Schedules for Persons Aged 0 Through 18 Years — United States, 2016. MMWR Morbidity and Mortality Weekly Report MMWR Morb Mortal Wkly Rep. 2016;65(4):1–2. doi: 10.15585/mmwr.mm6504a4. [DOI] [PubMed] [Google Scholar]
- 11.Office of Disease Prevention and Health Promotion. Immunization and Infectious Diseases. [Accessed July 14, 2016];Healthy People 2020. https://www.healthypeople.gov/2020/topics-objectives/topic/immunization-and-infectious-diseases. Published 2015.
- 12.Gerend MA, Shepherd MA, Lustria MLA. Increasing Human Papillomavirus Vaccine Acceptability by Tailoring Messages to Young Adult Women's Perceived Barriers. Sexually Transmitted Diseases. 2013;40(5):401–405. doi: 10.1097/olq.0b013e318283c8a8. [DOI] [PubMed] [Google Scholar]
- 13.Beavis AL, Levinson KL. Preventing Cervical Cancer in the United States: Barriers and Resolutions for HPV Vaccination. Frontiers in Oncology. 2016;6(19) doi: 10.3389/fonc.2016.00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hughes J, Cates JR, Liddon N, Smith JS, Gottlieb SL, Brewer NT. Disparities in How Parents Are Learning about the Human Papillomavirus Vaccine. Cancer Epidemiology Biomarkers & Prevention. 2009;18(2):363–372. doi: 10.1158/1055-9965.epi-08-0418. [DOI] [PubMed] [Google Scholar]
- 15.Dorell C, Yankey D, Kennedy A, Stokley S. Factors That Influence Parental Vaccination Decisions for Adolescents, 13 to 17 Years Old: National Immunization Survey-Teen, 2010. Clinical Pediatrics. 2012;52(2):162–170. doi: 10.1177/0009922812468208. [DOI] [PubMed] [Google Scholar]
- 16.Moss JL, Reiter PL, Rimer BK, Brewer NT. Collaborative patient-provider communication and uptake of adolescent vaccines. Social Science & Medicine. 2016;159:100–107. doi: 10.1016/j.socscimed.2016.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Roberts JR, Thompson D, Rogacki B, et al. Vaccine hesitancy among parents of adolescents and its association with vaccine uptake. Vaccine. 2015;33(14):1748–1755. doi: 10.1016/j.vaccine.2015.01.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Marlow LAV, Wardle J, Forster AS, Waller J. Ethnic differences in human papillomavirus awareness and vaccine acceptability. Journal of Epidemiology & Community Health. 2009;63(12):1010–1015. doi: 10.1136/jech.2008.085886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gelman A, Nikolajski C, Schwarz EB, Borrero S. Racial Disparities in Awareness of the Human Papillomavirus. Journal of Women's Health. 2011;20(8):1165–1173. doi: 10.1111/j.1525-1446.2011.00958.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ford JL. Racial and Ethnic Disparities in Human Papillomavirus Awareness and Vaccination among Young Adult Women. Public Health Nursing. 2011;28(6):485–493. doi: 10.1111/j.1525-1446.2011.00958.x. [DOI] [PubMed] [Google Scholar]
- 21.Friedman AL, Shepeard H. Exploring the Knowledge, Attitudes, Beliefs, and Communication Preferences of the General Public Regarding HPV: Findings From CDC Focus Group Research and Implications for Practice. Health Education & Behavior. 2007;34(3):471–485. doi: 10.1097/lgt.0b013e318168e607. [DOI] [PubMed] [Google Scholar]
- 22.National Cancer Institute. Health Information National Trends Survey 4 (HINTS 4) Cycle 4 Methodology Report. [Accessed July 18, 2016]; http://hints.cancer.gov/docs/Instruments/HINTS-FDA_Methodology_Report.pdf. Published February 2015.
- 23.Zimet GD. Improving adolescent health: Focus on HPV vaccine acceptance. Journal of Adolescent Health. 2005;37(6):S17–S23. doi: 10.1016/j.jadohealth.2005.09.010. [DOI] [PubMed] [Google Scholar]
- 24.Rosenthal S, Weiss T, Zimet G, Ma L, Good M, Vichnin M. Predictors of HPV vaccine uptake among women aged 19–26: Importance of a physician's recommendation. Vaccine. 2011;29(5):890–895. doi: 10.1016/j.vaccine.2009.12.063. [DOI] [PubMed] [Google Scholar]
- 25.Jacobs EA, Rolle I, Ferrans CE, Whitaker EE, Warnecke RB. Understanding African Americans' views of the trustworthiness of physicians. J Gen Intern Med Journal of General Internal Medicine. 2006;21(6):642–647. doi: 10.1111/j.1525-1497.2006.00485.x. [DOI] [PMC free article] [PubMed] [Google Scholar]