Abstract
Background/Objective
The aim of this study was to determine whether unilateral manual needling at nonacupoints could result in bilateral strength gain similar to that found in electroacupuncture at specific acupoints.
Methods
Fifty healthy male volunteers with an age range of 19–27 years were recruited and randomly allocated into five groups: (1) manual acupuncture and (2) electroacupuncture at two acupoints (ST-36 and ST-39); (3) manual acupuncture and (4) electroacupuncture at two nonacupoints on the tibialis anterior muscle; and (5) control group. The intervention groups received needling in each session on the right leg for 15 minutes in Week 1, 20 minutes in Week 2, and 30 minutes in Weeks 3–8, three sessions per week. The maximal isometric ankle dorsiflexion strength and muscle activation (as determined by twitch interpolation) of both legs were assessed pre, post, 2 weeks post, and 3 weeks post the experimental period.
Results
Mixed models (linear) with repeated-measures analysis identified significant strength gains (p < 0.01) after the intervention period in both limbs, while no significant differences were detected between the intervention groups and between the two legs, and no change was found in the control group. A significant improvement in muscle activation (p < 0.01) was also observed in both legs in the intervention groups.
Conclusion
It was concluded that both unilateral manual and electric needling caused significant bilateral strength gain, and this effect was not specific to the selected acupoints or electric stimulation. The strength gain was sustained for at least 3 weeks after the 8-week intervention.
Keywords: Acupuncture, Detraining, Muscle activation, Muscle strength
Introduction
It has been repeatedly reported in the literature that single-limb resistance exercise can affect muscle strength in both the muscle under training and the homologous muscle in the contralateral limb, a phenomenon known as cross education or cross transfer.1, 2 Furthermore, unilateral electromyostimulation has also been shown to increase strength in both limbs, possibly related to the influence of sensory inputs.3, 4 Interestingly, there have been recent reports that unilateral electroacupuncture and manual acupuncture at selected acupoints can also induce a crossover effect on the expression of strength in the contralateral limb, with the magnitude being similar to that found in resistance training or transcutaneous electromyostimulation.5, 6 These findings may have potential implications in the practice of physical conditioning and rehabilitation, as well as in advancement of our understanding of cross education, because most of the previous reports on cross education were based on voluntary resistance training.7, 8, 9 In this paper, we refer to “acupuncture” as applying needles at known acupoints following the practice in traditional Chinese medicine, and “needling” as applying needles at sham points (points not identified in traditional Chinese medicine); in addition, we use “cross education” for the effects of voluntary training and “cross transfer” for the effects of electromyostimulation training or needling.
Regarding the bilateral effect of unilateral electroacupuncture on muscle strength,5 it can be argued that the effect can be caused by either acupuncture at certain acupoints,10 or electric stimulation applied through needles. It has been speculated that the strength gain could be related to the sensory inputs associated with electric stimulation.3, 4 The effect may not necessarily be caused by stimulation at specific acupoints, as reported in some investigations where intramuscular needling was not used or electric needling was applied to sham points.6 Furthermore, it has been reported that manual acupuncture at selected acupoints can also induce cross-transfer effect similar to that induced by electroacupuncture.6 It would be interesting to find whether manual needling at sham points can induce a similar effect. Such evidence would be essential in understanding whether it is necessary to stimulate certain acupoints and use electric stimulation to cause cross transfer. If manual needling at sham points could induce similar bilateral strength gain, it would support the speculation that sensory input is a common and critical factor in manifesting cross transfer. In addition to the implications in therapy or rehabilitation, there have been increased interests in the field of sport science on the effect of acupuncture (or needling) as an ergogenic aid to neuromuscular function and sport performance; however, the published work in this area is still very limited.11, 12, 13
Therefore, the main aim of this study was to determine whether unilateral manual needling at sham points could induce similar bilateral changes in muscle strength to that induced by electroacupuncture or manual acupuncture. A null hypothesis was proposed that there would be no difference between the cross-transfer effects induced by manual needling on sham points and that induced by acupuncture at specific acupoints. This study also investigated whether the changes in muscle strength could be maintained after the intervention period, which had not been determined previously. Such evidence would assist practitioners in selecting an appropriate method of intervention, aiming to improve muscle strength.
It has been suggested that the phenomenon of cross education or cross transfer is mainly due to an adaptation in the nervous system, because no evidence of muscle hypertrophy has been reported.1, 2, 4, 14 To determine adaptations to training in the nervous system, twitch interpolation technique is frequently used for assessment of individual's capacity in activating muscles.15, 16 The second aim of this study was to determine whether the capacity of muscle activation could be improved by acupuncture or needling. A null hypothesis was proposed that there would be no difference between muscle activation induced by manual needling on sham points and that induced by acupuncture at specific acupoints.
Methods
Participants
Fifty healthy men with a mean age of 22.3 years (range 19–27 years) volunteered for the study. The participants were first given an individual registration number and then randomly allocated into five groups (n = 10 in each group) according to a random number table. The five groups were as follows: manual acupuncture at acupoints (MAcu); electroacupuncture at acupoints (EAcu); manual needling on sham points (MSham); electric needling on sham points (ESham); and control (CON).
The participants were university students who were physically active but not athletes. The inclusion criteria for participation were that the participants had no musculoskeletal or neurological disorders, had not been involved in regular strength training or structured sport training during the 6 months prior to the study, and had no previous experience with acupuncture or electric stimulation. All participants were right-foot dominant, as identified using an established questionnaire.17 The experimental procedures were approved by the Human Research Ethics Committee of Southern Cross University and conducted in compliance with the Declaration of Helsinki. Consent was obtained from all participants prior to the commencement of the study.
The sample size was determined by a priori estimation, using the G*Power 3 program (version 3.0.3).18 The predicted minimum number of participants for analysis of variance with repeated measures was 25 (5 in each of the 5 groups), with the assumptions of an effect size of 0.4, a power of 0.80, and an alpha level of 0.05. Therefore, 10 participants in each group were thought to have sufficient statistical power to determine the effect and could accommodate potential dropout in the present study. Physical characteristics of the participants who completed the study (there were 5 dropouts) are summarized in Table 1. Post hoc calculation based on the results of this study indicated that the effect size was higher than 0.57 in all experimental groups and the statistical power was 1.0.
Table 1.
Physical characteristics of participants.
| MAcu |
MSham |
EAcu |
ESham |
CON |
Total |
||
|---|---|---|---|---|---|---|---|
| N | 9 | 8 | 10 | 8 | 10 | 45 | |
| Age (y) | Mean | 21.6 | 20.9 | 22.5 | 22.1 | 24.2 | 22.3 |
| SD | 1.7 | 1.8 | 2.5 | 2.2 | 1.5 | 2.2 | |
| Mass (kg) | Mean | 62.3 | 74.8 | 67.4 | 69.5 | 66.3 | 67.8 |
| SD | 8.5 | 12.3 | 8.9 | 7.1 | 7.1 | 9.4 | |
| Height (cm) | Mean | 171.3 | 175.4 | 172.7 | 176.1 | 173.7 | 173.7 |
| SD | 6.1 | 5.7 | 6.2 | 4.7 | 7.2 | 6.1 |
CON = control; EAcu = electroacupuncture on acupoints; ESham = needling with electric stimulation on sham points; MAcu = manual acupuncture on acupoints; MSham = manual needling on sham points; SD = standard deviation.
Procedures
The dorsiflexion muscle group was chosen as the subject in this study because its function is essential to normal gait, and the dorsiflexors are often more significantly impaired than the plantar flexors in patients with hemiparesis.7, 19 The acupoints of ST-36 and ST-39 were used in the electroacupuncture and manual acupuncture groups for comparison, because these acupoints are suggested to have the effects of retarding muscle atrophy, motor impairment, pain, hemiplegia, and paralysis of the lower extremities, and have been used in previous investigations on cross transfer.5, 6, 20
Participants in the experimental groups received corresponding acupuncture or needling on the right leg, three sessions per week, for 8 weeks. All participants were familiarized with the testing device and procedure on the testing day, and given 1 minute ankle rotation exercise at a comfortable pace and intensity prior to each session to warm up, and a similar exercise after each session to cool down.
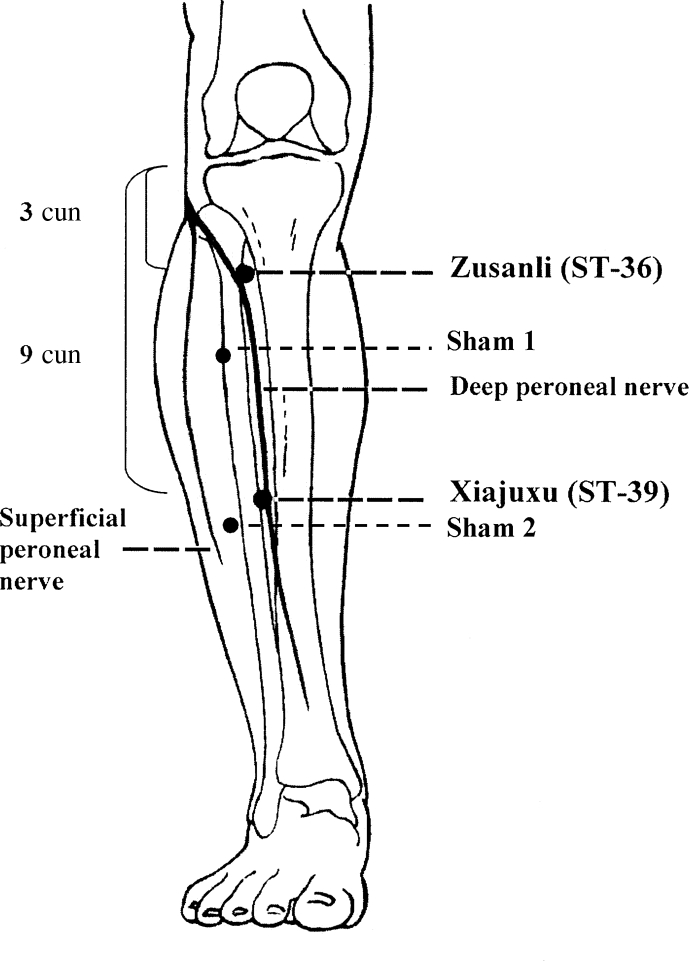
The MAcu and EAcu groups received manual acupuncture or electroacupuncture at the acupoints of Zusanli (ST-36) and Xiajuxu (ST-39) (Figure 1). The locations of these acupoints had been described in a previous report.5 For the MSham and ESham groups, acupuncture needles were applied to the muscle belly of the tibialis anterior, ∼3 cm laterally to the anterior crest of the tibia, at one point on the top one-third and another point on the lower one-third of the muscle, respectively, avoiding any known traditional Chinese medicine meridian channels and acupoints (Figure 1).
Figure 1.
Locations of the acupoints ST-36 and ST-39, and sham points on the tibialis anterior muscle. Cun is a unit for relative length used in traditional Chinese medicine. The breadth of participant's index, middle, ring, and little fingers, at the level of proximal interphalangeal joint at the dorsum of the middle finger, is 3 cun. Sham points are located at the top one-third and lower one-third on the muscle belly of the tibialis anterior muscle, and 3 cm lateral to the anterior crest of the tibia. Note. The figure is reproduced with permission.
Acupuncture or needling was performed by a qualified acupuncturist. For all participants in the experimental groups, a stainless-steel acupuncture needle with a diameter of 0.3 mm and a length of 50 mm (GB2024-94; Suzhou Medical Appliance Company, Ltd, Suzhou, China) was inserted perpendicularly (90°) to the skin into the muscle at the designated locations to a depth of 20–30 mm (with consideration of the leg size and the feeling of Deqi). At the acupoints, a feeling of “Deqi” was experienced by the participants. Deqi is a mixture of aching, pressure, soreness, heaviness, fullness, warmth, cooling, numbness, tingling, and dull pain, but not sharp pain.21 The participants were asked to describe their feeling and the acupuncturist determined whether Deqi was achieved. At the sham points, the needle was inserted to the same depth as that for the acupoints; however, it was not necessarily to experience Deqi.
The time of treatment in each session was progressively increased from 15 minutes for the 1st week to 20 minutes in Week 2 and 30 minutes in Weeks 3–8. For the MAcu and MSham groups, twirling and lift-thrusting techniques were applied for 15 seconds every 5 minutes. For the EAcu and ESham groups, an electroacupuncture apparatus (SDZ-II; Suzhou Medical Appliance Company, Ltd) was used to deliver constant-current square-wave pulses at a frequency of 40 Hz, pulse width of 1 millisecond, with a gradually increased intensity up to the maximal level that participants could tolerate (the electric current range was 2.2–2.9 mA). The cathode of the stimulator was connected to the needle on the proximal side and the anode to the distal needle. The stimulation was applied continuously for the same time period in each session as that for the MAcu group. Participants took a supine position and were instructed not to voluntarily contract the muscle during the needling. For safety considerations, dorsiflexion force was not monitored when needles were in the muscle. Electroacupuncture induced visible contractions, while manual acupuncture did not induce any visible muscle contraction.
The CON and experimental groups maintained their normal daily activities without being engaged in any specific physical training. For a more appropriate control of the potential effects from the experimental environment, all participants in the CON group also visited the laboratory three times per week. They participated in the same warm-up and cool-down activities, but otherwise rested during the session.
Prior to and after the 8-week intervention, all participants were tested for their maximal voluntary contraction strength (MVC). The static dorsiflexion contractions were performed on a custom-built device, during which the participants took a supine position, with the nontested leg fully extended and relaxed. The leg under testing was strapped to the testing device by Velcro belts around the foot, leg, and thigh, with the ankle joint at 15° plantar flexion and knee joint angle at full extension. A force transducer (MCL-S; Beijing Zhengkai Instruments Co., Ltd, Beijing, China) was mounted on a metal bar with foam padding, which was placed on the back of the foot at the level of the metatarsophalangeal joint. With the heel supported, and rotation axis of the device and ankle joint aligned, the location of the metal bar was adjusted according to the foot size. This location was recorded for each individual for the postintervention test. Signals from the force transducer were fed into a Medlab data acquisition system (Medlab-U8C; Nanjing Mei-Yi Science and Technology Co., Ltd, Nanjing, China) at an analog-to-digital conversion rate of 500 Hz. The participants were asked to perform three or more maximal dorsiflexions against the force transducer as quickly and forcefully as possible. Each contraction was maintained for 3–5 seconds, followed by 1 minute recovery. To ensure maximal exertion during the MVC test, the guidelines proposed in the literature were considered.22 These included the following: (1) all maximal efforts were accompanied by standardized instruction, verbal encouragement, and practice; (2) visual feedback of performance was given on a computer monitor; and (3) additional one or two trials were allowed if the participants felt that they could do better. The highest force value of successful contractions of each participant was used in statistical analysis.
After completion of the MVC tests, muscle activation was assessed using a twitch interpolation technique.15 The motor point was located by applying percutaneous electrical stimulation, via an electrical stimulator (Digitimer DS-7AH; Digitimer, Letchworth Garden City, UK), with the cathode (a metal bar) placed on the upper part of the anterior tibialis muscle and the anode on the lower part of the muscle. By repeatedly adjusting the location of the cathode and gradually increasing the current, the point where visible twitches were observed with a minimum current was defined as the motor point. After carefully cleaning the skin using alcohol wipes, and shaving the hair if needed, a 4 cm × 4 cm self-adhesive electrode was attached to the motor point (cathode), and the anode was attached at ∼5 cm below the cathode. Locations of the electrodes were recorded, and the same locations were used in the postintervention test.
The stimulator (Digitimer) was controlled by the Medlab system with customized software for this research. The stimulator was triggered once the peak force in a contraction was detected. When there was no further increase of the force for 200 milliseconds during a contraction, this force was defined as the peak force, and it was not less than 90% of the MVC level. Once triggered, a train of 10 square-wave pulses, each with a pulse width of 200 microseconds, at 50 Hz frequency, was delivered. Prior to the formal test, the current was gradually increased in repeated trials to the level that the participants could maximally tolerate (feeling uncomfortable and pain). In the formal trials, participants were requested to exert maximal dorsiflexion as quickly and forcefully as they could and maintain the effort for approximately 3–5 seconds. In each trial, two stimuli were applied. The first stimulus was given at 200 milliseconds after the peak force was identified (automatically by Medlab software), and the participants relaxed the muscle once they received the stimulus. The second stimulus was delivered automatically 5 seconds after the first stimulation on the relaxed muscle. The additional force induced by the first stimulus above the peak force during maximal voluntary contraction was recorded as the superimposed twitch force A, and the maximal force induced by the second stimulus on the relaxed muscle was recorded as the control twitch force B. The muscle activation level was determined as follows15:
| Voluntary muscle activation (%) = (1 – A/B) × 100% | (1) |
The result of a successful trial was used in statistical analysis.
To investigate the “detraining” effect, participants of the four intervention groups were tested for ankle dorsiflexion MVC again at the time points of 2 weeks and 3 weeks post the intervention period. Since the CON group did not show a significant change in muscle strength and activation during the 8-week experimental period, this group was not tested at these time points.
Statistical analysis
To determine the effects of the interventions, mixed models (linear) with repeated measures analysis was performed for the fixed effects of Group (5 groups), Leg (right and left), and Treatment (pre and post, with diagonal covariance structure). A full factorial model with all two- and three-way interactions was initially considered, and the final model had the three-way and the Leg by Group interactions excluded. To determine the “detraining” effects, a similar analysis was performed for the four experimental groups (CON group did not participate in this component), and the Treatment factor included four time points (pre, post, 2-week post, and 3-week post). If a significant interaction was detected, Bonferroni adjustment was applied in post hoc analysis to compare the mean values, with an alpha level of 0.05 being set for statistical significance. These statistical analyses were performed using SPSS statistical package (version 20; IBM SPSS Statistics, Armonk, New York, United States).
Results
Forty-five participants completed the 8-week intervention successfully. Five participants withdrew from the study due to personal reasons. The number of participants in each group who completed the study are shown in Table 1. The control group did not participate in the “detraining” component of the study, while all other participants (n = 35) completed the 2-week posttest, and 32 participants completed the 3-week posttest (3 participants withdrew from the last test due to personal reasons) with eight in MAcu, seven in MSham, nine in EAcu, and eight in ESham groups.
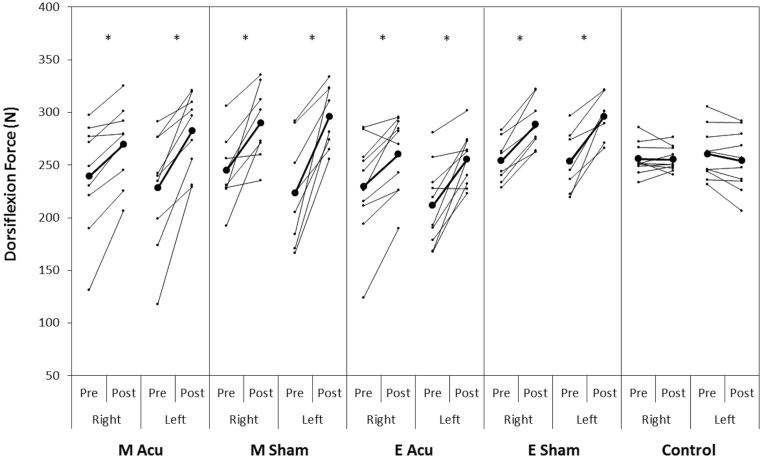
With respect to MVC, results of the mixed models with repeated-measures analyses indicated that there was a significant effect of Treatment (pre vs. post, F = 135.431, p < 0.001), and interactions of Treatment by Group (F = 12.525, p < 0.001) and Treatment by Leg (F = 5.018, p = 0.027). Post hoc pair-wise comparisons for the Treatment by Group interaction indicated that all the four experimental groups showed significant improvements in dorsiflexion MVC after 8 weeks of intervention (F = 34.928–74.610, p < 0.001), while the CON group showed no change (F = 0.038, p = 0.846; Figure 2, Table 2). However, no significant differences were found in MVC between the groups, in neither pre- nor posttests (p > 0.05). For the Treatment by Leg interaction, the post hoc comparison found that there were significant strength gains after the 8 weeks in both the right (F = 63.900, p < 0.001) and the left (F = 82.462, p < 0.001) leg in the intervention groups. Furthermore, MVC in the right leg was slightly higher than that in the left leg in the pretest (F = 4.085, p = 0.049), but no difference was found between the two legs in the posttest (F = 1.103, p = 0.299).
Figure 2.
Effects of 8 weeks of unilateral acupuncture at acupoints or needling at sham points on the right leg on ankle dorsiflexion force of both legs. The larger dots and thick lines represent the group means, and the smaller dots and thin lines represent individual data in each group. *p < 0.05, post > pre. EAcu = electroacupuncture on acupoints; ESham = electroacupuncture on sham points; MAcu = manual acupuncture on acupoints; MSham = manual acupuncture on sham points.
Table 2.
Comparisons of group means between ankle dorsiflexion strength measured pre and post 8 weeks of intervention.
| Group | Leg | Pre | Post | Variation (%) |
|---|---|---|---|---|
| MAcu | R | 239.2 ± 53.2 | 269.5 ± 37.7* | 12.7 |
| L | 228.0 ± 55.9 | 282.2 ± 36.3* | 23.8 | |
| Combined | 233.6 ± 53.2 | 275.8 ± 36.4* | 18.0 | |
| MSham | R | 244.9 ± 34.2 | 290.0 ± 35.6** | 18.4 |
| L | 223.2 ± 50.4 | 295.9 ± 30.2* | 32.6 | |
| Combined | 234.0 ± 43.1 | 293.0 ± 32.0* | 25.2 | |
| EAcu | R | 229.7 ± 47.8 | 260.2 ± 36.7* | 13.3 |
| L | 211.7 ± 38.5 | 255.6 ± 24.8* | 20.7 | |
| Combined | 220.7 ± 43.3 | 257.9 ± 30.6* | 16.9 | |
| ESham | R | 254.1 ± 20.7 | 288.5 ± 23.8* | 13.5 |
| L | 253.3 ± 27.7 | 296.0 ± 20.3* | 16.9 | |
| Combined | 253.7 ± 23.6 | 292.2 ± 21.7* | 15.2 | |
| Control | R | 255.8 ± 15.2 | 255.3 ± 11.7 | −0.2 |
| L | 260.3 ± 24.4 | 253.9 ± 28.6 | −2.5 | |
| Combined | 258.0 ± 19.9 | 254.6 ± 21.3 | −1.3 |
Data are presented as mean ± SD in Newton.
*p < 0.01, post compared with pre.
EAcu = electroacupuncture on acupoints; ESham = electroacupuncture on sham points; L = left; MAcu = manual acupuncture on acupoints; MSham = manual acupuncture on sham points; R = right; SD = standard deviation.
Most of the participants in the intervention groups volunteered for the follow-up strength tests at 2 and 3 weeks post intervention. The results of mixed models with repeated-measures analyses detected a significant fixed effect of Treatment (pre, post, post 2 weeks, and post 3 weeks; F = 16.772, p < 0.001) and Group (F = 8.791, p < 0.001). No significant interaction was found for Treatment by Group (F = 0.808, p = 0.601), indicating that all four groups demonstrated a similar trend of change (Table 3). In addition, no significant difference between the changes in the two legs (F = 2.337, p = 0.128) and no significant interactions of Treatment by Leg (F = 1.121, p = 0.343) were observed, indicating that the two legs had a similar trend of change. Post hoc analyses with Bonferroni adjustment showed that the dorsiflexion strength was significantly increased after the 8-week intervention, and the strength was maintained for at least 3 weeks post intervention (results of the 2 legs were combined because no effect of Leg was detected), while after 3 weeks, the strength became lower than that at the post (p = 0.004) but still higher than the pre (p < 0.001; Table 3).
Table 3.
Comparisons of ankle dorsiflexion strength measured pre, post, 2 weeks post, and 3 weeks post 8-week interventions.a
| Leg | Pre | Post | Post 2 wk | Post 3 wk |
|---|---|---|---|---|
| R | 241.9 ± 6.97 | 277.0 ± 5.69** | 271.8 ± 5.27** | 268.2 ± 4.55* |
| L | 229.1 ± 7.40 | 282.4 ± 4.78** | 266.3 ± 4.99** | 257.8 ± 3.70**,*** |
| Combined | 235.5 ± 5.09 | 279.7 ± 3.72** | 269.0 ± 3.63** | 263.0 ± 2.94**,*** |
Data are presented as mean ± SD in Newton.
*p < 0.05, compared with pre.
**p < 0.01, compared with pre.
***p < 0.01, compared with post.
L = left; R = right; SD = standard deviation.
There were no significant interactions for Treatment by Group and Treatment by Leg. Therefore, the strength values of the four groups were combined for each time point to demonstrate the effect of Treatment.
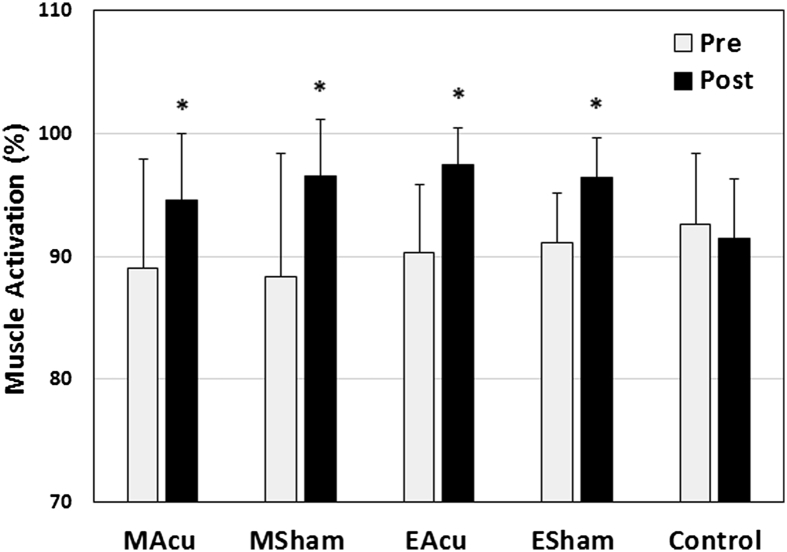
With respect to voluntary muscle activation, mixed models with repeated-measures analysis detected a significant effect of Treatment (pre to post, F = 33.407, p = 0.001) and a significant interaction of Treatment by Group (F = 4.296, p = 0.003). No other significant main effects (Leg and Group) and interactions were detected. Post hoc analysis with Bonferroni adjustment for the Treatment by Group interaction showed that there were no significant differences between the groups in the pretest (F = 0.702, p = 0.593), and a near-significant difference in the posttest (F = 2.509, p = 0.055). All intervention groups showed a significant increase in muscle activation (5.3–8.3%) after the 8-week intervention (all p < 0.01), while the CON group had no change (−1.2%) during the same period (p = 0.456) (Figure 3).
Figure 3.
Effects of 8 weeks of unilateral acupuncture at acupoints or needling at sham points on muscle activation (mean ± SD), as determined by twitch interpolation technique. *p < 0.05, post > pre. EAcu = electroacupuncture on acupoints; ESham = electroacupuncture on sham points; MAcu = manual acupuncture on acupoints; MSham = manual acupuncture on sham points; SD = standard deviation.
Discussion
Both null hypotheses were accepted because no significant differences were found in the bilateral strength gains and improved muscle activation between the MSham and other experimental groups. Sham points have been used as a “control” for the effect of acupuncture.23, 24, 25 In a review of the literature on the specificity of acupoints, it was reported that nearly 60% of the trials did not find significant difference in the outcomes between acupuncture at acupoints and sham points.25 It has been noted that it is difficult to perform “placebo” controlled trials for acupuncture, because it is difficult to find an adjacent point that is placed at a large enough distance from the acupoint without overlapping with another acupoint or a meridian channel,26 and both electroacupuncture and manual acupuncture at acupoints or sham points cause a level of pain that may produce a “placebo effect.”23, 25 The present study also found no significant difference in the strength gains between the MAcu, MSham, EAcu, and ESham groups, which is in line with the above mentioned observations. Furthermore, the participants of the present study were healthy men rather than patients. Therefore, we would not consider interpreting the findings according to the theoretical framework of traditional Chinese medicine, but simply to demonstrate the effectiveness of needling at acupoints and sham points in improving muscle strength, in the paradigm of cross transfer.
There have been increased interests in the effect of acupuncture on muscle function and sport performance.11, 12, 13, 27 It has been reported that one session of bilateral acupuncture or electrical stimulation at certain acupoints can significantly affect muscle strength.13, 28 The current study provided further evidence for the positive effect of long-term acupuncture or needling on muscle strength. Furthermore, this study demonstrated that the strength gain caused by needling did not appear to be specific to the selected acupoints (ST-36 and ST-39) and electric stimulation, because manual needling at sham points resulted in similar bilateral strength gain.
It is beyond the objective of this study to examine the possible mechanisms for the cross-transfer effect induced by intramuscular needling. However, we would adopt the viewpoint that the bilateral effects of unilateral acupuncture or needling and electrical stimulation would be related to plasticity of the nervous system,26, 29 although the possibility of peripheral adaptations should not be excluded.1, 4, 30 Results of the twitch interpolation test underscored the viewpoint by demonstrating a significant improvement in muscle activation after the intervention. The average improvement was 5.3–8.3% in the intervention groups, while no significant change was found in the control group. It confirms that the neural adaptation played an important role in the bilateral strength gain found in this study, although the increased muscle activation, as determined by the twitch interpolation method, could not fully account for the 13.3–32.6% increase in strength.
For the potential neural mechanisms underlying adaptations to voluntary resistance training, it has been hypothesized that at the supraspinal levels the contralateral strength gain could be due to either “crossed activation,” e.g., activation of neural circuits on one side that chronically modifies the efficacy of motor pathways that project to the opposite untrained limb, or “bilateral-access,” e.g., the untrained limb may access these modified neural circuits during training, which may subsequently lead to an increased capacity to drive the untrained muscles and thus result in increased strength.30, 31 However, the electrical stimulation or acupuncture applied to the muscles does not involve voluntary activation of the muscle. Therefore, the above-proposed mechanisms for resistance training-induced cross education may not fully explain the current findings. It is speculated that the sensory inputs caused by the acupuncture or electric stimulation might play a significant role in manifesting the cross-transfer effect.
The essential role of sensory afferents in mediating cross transfer is further supported by the effect of manual needling as found in this study. The manual needling did not appear to have activated the motor nerve effectively, because no visible muscle contraction was observed. Therefore, the cross-transfer effect caused by manual acupuncture or needling does not seem to be related to activation of motor nerve fibers and the contraction intensity, but must be related to the neural plasticity associated with the sensory inputs. Needle penetration and manipulation are noxious stimuli that may have an inhibitory effect on pain or certain motor reflexes.32, 33 Whether and how acupuncture or needling at various intensities and durations affects sensory and motor functions at different levels in the nervous system are still unclear. There have been reports utilizing functional magnetic resonance imaging to investigate the cortical responses to acupuncture, with equivocal findings. It has been reported that unilateral electroacupuncture at ST-36 and ST-39 induced wider bilateral activation in the brain (primary and secondary somatosensory cortices, supplementary motor area, prefrontal association cortex, cingulate gyrus, etc.) than that induced by transcutaneous electric stimulation, while manual acupuncture at these acupoints did not induce comparable activations according to the functional magnetic resonance imaging signals.34 However, another functional magnetic resonance imaging study demonstrated that manual acupuncture at ST-36 modulated neural activity at multiple levels of the cerebro-cerebellar and limbic systems.35 Further research is needed to determine how the sensory inputs are translated to cortical plasticity in motor performance. A study that employed the transcranial magnetic stimulation technique to investigate the changes in motor-evoked potentials in hand-muscle response to acupuncture has found that needling at both an acupoint (ST38) and a nonacupoint on the leg induced large motor-evoked potential facilitation in abductor digitiminimi and first dorsal interosseous muscles of both sides. The effect was maintained even after needle extraction, indicating that acupuncture or needling is able to induce plastic changes in the central nervous system.36
To our knowledge, this was the first study that investigated the sustainability of the improved muscle strength after several weeks of intramuscular needling. The results showed that 3 weeks after the “treatment,” the dorsiflexion strength was still higher than the baseline in both limbs, although there was a declining trend (Table 3). The participants maintained their normal physical activity levels, and did not engage in other specific exercise and training that might affect their muscle strength. This information would be useful in designing training and rehabilitation programs with respect to training/treatment frequency and interval.
Conclusion
This study demonstrated that both unilateral manual acupuncture and electroacupuncture on tibialis anterior muscle for 8 weeks caused significant bilateral strength gain in dorsiflexion, and this cross-transfer effect did not appear to be specific to the selected acupoints and electric stimulation because manual needling at sham points induced a similar outcome. Improved muscle activation partially accounted for the strength gain; however, the mechanisms underlying the adaptations to the needling require further study. The strength gain was sustained for at least 3 weeks after the 8-week needling intervention.
Conflicts of interest
The authors declare that they have no conflicts of interest in relation to this work.
Funding/support
This work was supported by Southern Cross University, Tianjin Key Laboratory of Exercise Physiology and Sports Medicine, Tianjin Higher Education Innovative Team Fund, and China National Key Technology R&D Program (2012BAK21B00).
Acknowledgments
The authors appreciate the guidance on acupuncture given by Dr Qing-Wen Li and Bo Zhou; contributions from Gang Xu, Zhaojun Wang and Jun Liang, Tianjin University of Sport, in data collection; and the advice given by Dr Margaret Rolfe, Southern Cross University, for statistical analysis.
References
- 1.Zhou S. Chronic neural adaptations to unilateral exercise: mechanisms of cross education. Exerc Sport Sci Rev. 2000;28:177–184. [PubMed] [Google Scholar]
- 2.Hendy A.M., Spittle M., Kidgell D.J. Cross education and immobilisation: mechanisms and implications for injury rehabilitation. J Sci Med Sport. 2012;15:94–101. doi: 10.1016/j.jsams.2011.07.007. [DOI] [PubMed] [Google Scholar]
- 3.Hortobagyi T., Scott K., Lambert J. Cross-education of muscle strength is greater with stimulated than voluntary contractions. Motor Control. 1999;3:205–219. doi: 10.1123/mcj.3.2.205. [DOI] [PubMed] [Google Scholar]
- 4.Bezerra P., Zhou S., Crowley Z. Effects of unilateral EMS superimposed on voluntary training on strength and cross-sectional area. Muscle Nerve. 2009;40:430–437. doi: 10.1002/mus.21329. [DOI] [PubMed] [Google Scholar]
- 5.Huang L.P., Zhou S., Lu Z. Bilateral effect of unilateral electroacupuncture on muscle strength. J Altern Complement Med. 2007;13:539–546. doi: 10.1089/acm.2007.6250. [DOI] [PubMed] [Google Scholar]
- 6.Zhou S., Huang L.P., Liu J. Bilateral effects of 6 weeks' unilateral acupuncture and electroacupuncture on ankle dorsiflexors muscle strength: a pilot study. Arch Phys Med Rehabil. 2012;93:50–55. doi: 10.1016/j.apmr.2011.08.010. [DOI] [PubMed] [Google Scholar]
- 7.Dragert K., Zehr E.P. High-intensity unilateral dorsiflexor resistance training results in bilateral neuromuscular plasticity after stroke. Exp Brain Res. 2013;225:93–104. doi: 10.1007/s00221-012-3351-x. [DOI] [PubMed] [Google Scholar]
- 8.Farthing J.P., Zehr E.P. Restoring symmetry: clinical applications of cross-education. Exerc Sport Sci Rev. 2014;42:70–75. doi: 10.1249/JES.0000000000000009. [DOI] [PubMed] [Google Scholar]
- 9.Pearce A.J., Hendy A., Bowen W.A. Corticospinal adaptations and strength maintenance in the immobilized arm following 3 weeks unilateral strength training. Scand J Med Sci Sports. 2013;23:740–748. doi: 10.1111/j.1600-0838.2012.01453.x. [DOI] [PubMed] [Google Scholar]
- 10.Lin Y.P., Pan L. Current research on Juci. J Yun Nan Chin Med. 2004;25:41–43. [Google Scholar]
- 11.Hübscher M., Vogt L., Ziebart T. Immediate effects of acupuncture on strength performance: a randomized, controlled crossover trial. Eur J Appl Physiol. 2010;110:353–358. doi: 10.1007/s00421-010-1510-y. [DOI] [PubMed] [Google Scholar]
- 12.Ahmedov S. Ergogenic effect of acupuncture in sport and exercise: a brief review. J Strength Cond Res. 2010;24:1421–1427. doi: 10.1519/JSC.0b013e3181d156b1. [DOI] [PubMed] [Google Scholar]
- 13.Yang H.Y., Liu T.Y., Kuai L. Electrical acupoint stimulation increases athlete’s rapid strength. Chin Acupunct Moxibustion. 2006;26:313–315. [PubMed] [Google Scholar]
- 14.Lee M., Carroll T.J. Cross education: possible mechanisms for the contralateral effects of unilateral resistance training. Sports Med. 2007;37:1–14. doi: 10.2165/00007256-200737010-00001. [DOI] [PubMed] [Google Scholar]
- 15.Shield A., Zhou S. Assessing voluntary muscle activation with the twitch interpolation technique. Sports Med. 2004;34:253–267. doi: 10.2165/00007256-200434040-00005. [DOI] [PubMed] [Google Scholar]
- 16.Xu G., Huang L.P., Zhou S. Chronic knee injuries impair voluntary activation of quadriceps femoris. Chin J Sports Med. 2012;31:109–112. [Google Scholar]
- 17.Li X.T. Handedness in Chinese. Acta Psychol Sin. 1983;15:27–35. [Google Scholar]
- 18.Faul F., Erdfelder E., Lang A.G. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175–191. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- 19.MacIntosh B.J., Mraz R., Baker N. Optimizing the experimental design for ankle dorsiflexion fMRI. Neuroimage. 2004;22:1619–1627. doi: 10.1016/j.neuroimage.2004.03.035. [DOI] [PubMed] [Google Scholar]
- 20.Beijing College of Traditional Chinese Medicine, Shanghai College of Traditional Chinese Medicine, Nanjin College of Traditional Chinese Medicine, The Acupuncture Institute of the Academy of Traditional Chinese Medicine . 1st ed. Foreign Languages Press; Beijing, China: 1980. Essentials of Chinese Acupuncture. [Google Scholar]
- 21.Hui K.K.S., Nixon E.E., Vangel M.G. Characterization of the “deqi” response in acupuncture. BMC Complement Altern Med. 2007;7:33. doi: 10.1186/1472-6882-7-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gandevia S.C. Spinal and supraspinal factors in human muscle fatigue. Physiol Rev. 2001;81:1725–1789. doi: 10.1152/physrev.2001.81.4.1725. [DOI] [PubMed] [Google Scholar]
- 23.Lundeberg T., Lund I., Sing A. Is placebo acupuncture what it is intended to be? Evid Based Complement Altern Med. 2011;2011:1–5. doi: 10.1093/ecam/nep049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang H., Bian Z., Lin Z. Are acupoints specific for diseases? A systematic review of the randomized controlled trials with sham acupuncture controls. Chin Med. 2010;5:1. doi: 10.1186/1749-8546-5-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Moffet H.H. Sham acupuncture may be as efficacious as true acupuncture: a systematic review of clinical trials. J Altern Complement Med. 2009;15:213–216. doi: 10.1089/acm.2008.0356. [DOI] [PubMed] [Google Scholar]
- 26.Han J.S. Acupuncture analgesia: areas of consensus and controversy. Pain. 2011;152:S41–S48. doi: 10.1016/j.pain.2010.10.012. [DOI] [PubMed] [Google Scholar]
- 27.Yan T., Hui-Chan C.W.Y. Transcutaneous electrical stimulation on acupuncture points improves muscle function in subjects after acute stroke: a randomized controlled trial. J Rehabil Med. 2009;41:312–316. doi: 10.2340/16501977-0325. [DOI] [PubMed] [Google Scholar]
- 28.Ozerkan K.N., Bayraktar B., Sahinkaya T. Comparison of the effectiveness of the traditional acupuncture point, ST.36 and Omura's ST.36 point (True ST. 36) needling on the isokinetic knee extension & flexion strength of young soccer players. Acupunct Electrother Res. 2007;32:71–79. doi: 10.3727/036012907815844129. [DOI] [PubMed] [Google Scholar]
- 29.Balogun J.A., Biasci S., Han L. The effects of acupuncture, electroneedling and transcutaneous electrical stimulation therapies on peripheral haemodynamic functioning. Disabil Rehabil. 1998;20:41–48. doi: 10.3109/09638289809166052. [DOI] [PubMed] [Google Scholar]
- 30.Carroll T.J., Herbert R.D., Munn J. Contralateral effects of unilateral strength training: evidence and possible mechanisms. J Appl Physiol. 2006;101:1514–1522. doi: 10.1152/japplphysiol.00531.2006. [DOI] [PubMed] [Google Scholar]
- 31.Lee M., Hinder M.R., Gandevia S.C. The ipsilateral motor cortex contributes to cross-limb transfer of performance gains after ballistic motor practice. J Physiol. 2010;588(Pt 1):201–212. doi: 10.1113/jphysiol.2009.183855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Takakura N., Yajima H., Takayama M. Inhibitory effect of needle penetration on vibration-induced finger flexion reflex in humans. Acupunct Med. 2010;28:78–82. doi: 10.1136/aim.2009.001149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Xu W.D., Zhu B., Rong P.J. The pain-relieving effects induced by electroacupuncture with different intensities at homotopic and heterotopic acupoints in humans. Am J Chin Med. 2003;31:791–802. doi: 10.1142/S0192415X03001478. [DOI] [PubMed] [Google Scholar]
- 34.Huang L., Zhou S., Hu X. An fMRI investigation on brain activity in response to unilateral acupuncture, electroacupuncture and electromyostimulation on ST36 and ST39. In: Saad M., editor. Acupuncture—Concepts and Physiology. InTech-Open Access Publisher; Rijeka, Croatia: 2011. pp. 49–68. [Google Scholar]
- 35.Hui K.K.S., Liu J., Marina O. The integrated response of the human cerebro-cerebellar and limbic systems to acupuncture stimulation at ST 36 as evidenced by fMRI. Neuroimage. 2005;27:479–496. doi: 10.1016/j.neuroimage.2005.04.037. [DOI] [PubMed] [Google Scholar]
- 36.Maioli C., Falciati L., Marangon M. Short- and long-term modulation of upper limb motor-evoked potentials induced by acupuncture. Eur J Neurosci. 2006;23:1931–1938. doi: 10.1111/j.1460-9568.2006.04698.x. [DOI] [PubMed] [Google Scholar]