Abstract
Objective
The purpose of this study was to review the literature on current challenges and propose solutions for the optimal utilization of the electronic health records (EHRs) in chiropractic practice.
Methods
A search was performed in the PubMed, Index of Chiropractic Literature, and Current Index to Nursing and Allied Health Literature databases from November 2005 to February 2015. A combination of the following key words was used: electronic health records, electronic medical records, implementation, documentation, benefits, and challenges. Articles were categorized into common problems and solutions. These were filtered by application to chiropractic or educational institutions.
Results
The search resulted in 45 papers, which included case reports of EHR implementation, governmental insurance reports, commentaries, controlled studies, narrative reviews of past experiences with conversion from paper systems, and the implementation of EHRs in small offices and chiropractic offices. Minimal literature was found that directly related to chiropractic EHRs. Improper utilization, incorrect use of the software, faulty implementation, workflow burdens, financial considerations, and insufficient training were found to negatively affect the quality of the record.
Conclusions
Documentation errors are often innate in the EHR software. Improper utilization, insufficient training, or difficulty in integration of the EHR into the clinical office setting results in poor implementation of the electronic version of the clinical record. Solutions that may decrease documentation errors include EHR training, continued financial incentives, and appropriate implementation process and utilization of available software features.
Key Indexing Terms: Electronic Health Records, Chiropractic, Health Education, Ethics
Introduction
The quality of health care records came into question in the 1960s when Weed1 published a report on the lack of interprofessional communication about patient care that was affecting the quality of the care rendered. He created the problem-oriented medical record (POMR) and opined that the health care record was “central to patient care and the teaching of healthcare.”1 The POMR provided organization of the health care record and continuity of care between physicians and interns.1 This improved patient care, and the system was eventually adopted by medicine and then by other health care providers. Fifteen years later, the chiropractic profession instituted this system. Thereafter, the third-party payors required an increased level of documentation of the medical necessity of care. By the late 1990s, managed care reinforced the necessity of a POMR and the daily SOAP (Subjective, Objective, Assessment, and Plan) notes. Licensing board complaints, regarding the insufficient quality of the records, resulted in the introduction of new board policy guidelines and regulations on documentation and record keeping.2, 3 Many managed care organizations also issued policy guidelines. In 2006, the Federation of Chiropractic Licensing Boards passed a resolution that further strengthened the implementation of appropriate documentation. This resolution recommended that “all state boards require a course in the topic of documentation for re-licensure,” and that the Council of Chiropractic Education (CCE) “accredited colleges provide training in documentation in the basic Doctor of Chiropractic curriculum.”3 Documentation of the clinical encounter with the patient and the decision-making process became a required part of the clinical record. In 2008, the chiropractic “best practices” document informed the clinician of the importance of the clinical process during the encounter.4 Meanwhile, payors increased the extent and the degree of the record reviews.5 Despite the professional recommendations and insurance requirements, the American Chiropractic Association stated that the lack of appropriate documentation in clinical records continued to show up in audits and was compromising the practices of a number of practitioners because of third-party payor denials.6, 7, 8
This necessity of an increased level of documentation created a burden on the practicing clinician, which led to evolution of the electronic format. Early efforts to enter the electronic health record (EHR) movement resulted in the implementation of barcoded note-capturing software, rather than a true EHR. The software was expected to increase doctor efficiency and decrease the time for documentation. The software companies imagined their barcoded systems would enable practitioners to see more patients in their workday. The weakness in this initial EHR system is that it only provided an organized directory of patients’ health without sufficient variability or customization to clearly document the specifics of the patient encounter.5, 9 This resulted in repetition of language, findings, courses of care, outcomes, duration, and dosages. This type of note-capturing generates similar daily notes because of the electronically generated repetitive information. It failed to substantiate the care rendered.5
There are currently numerous EHR software programs available for the practicing doctor of chiropractic. However, it is unknown how the practitioner may know which EHR system is most appropriate for clinical documentation or how he or she should implement it for maximum utility. Therefore, the purpose of this paper is to review the literature of the current challenges of chiropractic EHRs and to provide suggestions for future direction.
Methods
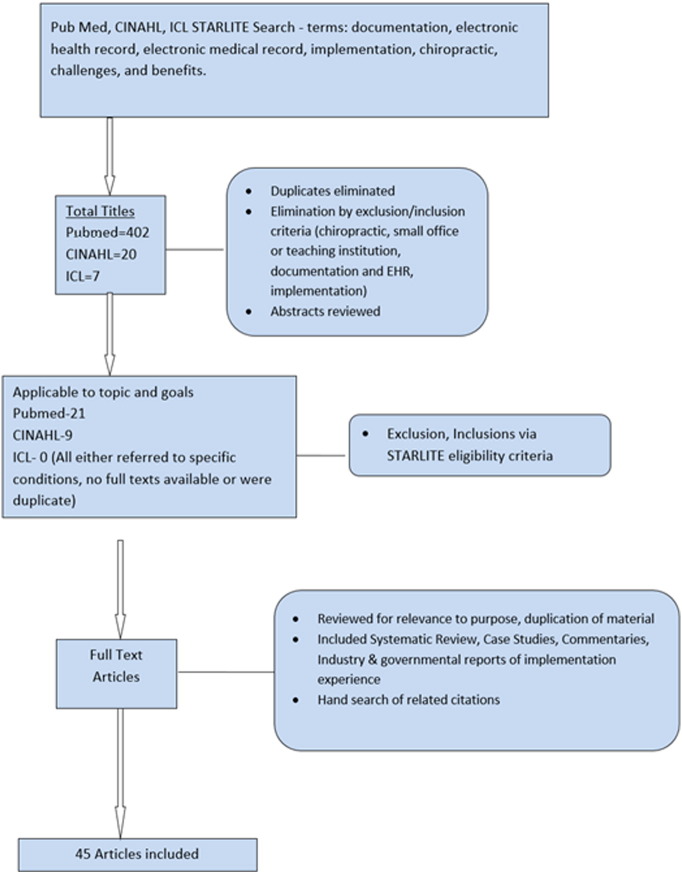
The literature search was conducted from November 2014 through February 2015. STARLITE (sampling strategy, type of study, approaches, range of years, limits, inclusion and exclusions, terms used, electronic sources) search strategy with the terms documentation, electronic health record, implementation, benefits, and challenges was used10 (Fig 1). The study included narrative reviews, commentaries, case studies, case series, surveys, clinical case studies, randomized controlled studies, governmental reports, and insurance company reports. The study also included reports on the progress of implementation of EHRs, quality of documentation, or experience in teaching facilities. The search was limited to the English language, and the databases searched were PubMed, Current Index to Nursing and Allied Health Literature, and Index of Chiropractic Literature. The search was further limited to articles directly applicable to small chiropractic offices and teaching clinics. Reference tracking was used to identify additional citations. Large national network or hospital studies, radiology- or laboratory-related studies, and studies that involved specific conditions were excluded because the implementation problems were not likely to be applicable to individual chiropractic practice or teaching facilities. The final results eliminated duplicates and those citations that were not relevant to the topics of interest.
Fig 1.
Search strategy diagram. STARLITE, sampling strategy, type of study, approaches, range of years, limits, inclusion and exclusions, terms used, electronic sources.
Results
A total of 45 full-text articles from all databases were used. There were reports of implementation in small medical offices,11 satisfaction with EHR systems,12, 13 and methods of importing the documentation content.14 All of these reports indicated consistent problems that affected the quality of the documentation. Commentaries revealed the use and misuse of the documentation information generated by EHR systems.14 One study looked at the sociological aspect of EHR systems and how it affected the quality of care.15 This study provided insight into the doctor-computer-patient relationship, with the computer demanding more attention than the patient. The computer intervention resulted in the doctor missing nonverbal patient communication, resulting in a negative effect on quality of care. There were 10 governmental and private insurance reports found and 8 used. These reports reviewed the overall EHR system utilization rate and provided an overview of the trend. Common themes noted throughout the articles reviewed were difficulties in utilization of all the features of the new software, intrusive change in workflow, financial constraints on small office budgets, and imposition in the doctor-patient relationship, which often led to dissatisfaction in practice. There was inconsistent reporting on the effects of EHRs on changes in quality of care but consensus on the other issues.
An analysis of the utilization reports demonstrated an increase in health care utilization of EHRs over the past 14 years. Hing16 reported that the national health statistics manifested 34.8% utilization by office-based physicians. This showed an increase of 91% over the 2001 statistics.16 Use increased from 34% to 78% of office-based physicians in 2013.17 Current usage in chiropractic has been estimated by Smith of the American Chiropractic Association to be only 33% of the profession, lagging behind other office-based physicians.18 Electronic health record conversion from paper files increased over the past 12 years. Group practices were more likely to use EHRs (74.3%) than solo practices were (20.6%). A higher use rate of EHRs was found in multispecialty practices (52.5%) than in single-specialty (30.3%) or in non-hospital associated practices (20%) or nonacademic practices (14%).16, 19, 20 To increase the utilization of EHRs for documentation, the 2009 American Recovery and Reinvestment Act included funding to promote their adoption by practitioners. As of March 2015, $20 billion in incentives were provided to all provider types.16 Of this amount, $195 million has gone to chiropractic physicians, indicating that there is a growing percentage of federally qualified, meaningful use EHRs in chiropractic offices.21
The American Recovery and Reinvestment Act also directed health information technology to promote improved quality and efficiency of care and to reduce medical errors. Hospitals adopted EHRs, with 97% reporting possession of a certified EHR and 76% having adopted it in 2014.22 Smaller practitioner offices were slower in adoption.22, 23 In 2008, the American Medical Association (AMA) reported an even lower figure than the national health statistics, with only 17% of office-based physicians utilizing EHRs in some form, and only 4% of these were fully functional in the office.24 In 2014, the AMA reported only 2% of office-based physicians qualifying for stage 2 meaningful use.25 It appears that, in spite of the incentives to foster EHR use, actual implementation was slower in the independent offices, and full-feature capabilities were not implemented.
The AMA, the Institute of Medicine, and many nonprofit and professional organizations promoted increased adoption to improve public health, patient safety, quality, medical liability defense, and research.26 “Pay for Performance Plans” promoted use of EHRs as part of their measurement for quality-of-care goals. This was reinforced in November 2016 by Medicare with a new rule that promotes a merit-based incentive payment system through the certified EHR technology.27 The Agency for Healthcare Research and Quality reported that use of EHRs supported a consistently higher standard of care across the country.28
Discussion
To the best of the author’s knowledge, this is the first paper to review the literature on the challenges and solutions to EHR implementation in chiropractic practice. The findings indicate that the primary challenges with EHRs were in proper documentation, financial constraints, logistical changes in workflow, intrusion into the doctor-patient relationship, and difficulty in implementing the new process. The literature revealed the potential pitfalls of introduction of new errors into patient records. The pitfalls differed depending on the size of the practice, health care system, or teaching facility.
Challenges: Documentation Errors
This literature review revealed the common occurrence of problems with the use of templates and macros.12 These generated an unnecessary volume of notes with redundant and irrelevant information. The high volume resulted in inefficiency of review time, similar to illegible handwritten notes. In many instances, template-based notes introduced false information to the record as a result of the user clicking a wrong box, calling up old data, or using old notes as a template with failure to update that portion of the data or note. Doctor transition would exacerbate this problem, when one doctor took over care from another. The new doctor may not have been familiar with the software and might have relied on the previous notes by invoking the “copy forward” notes option without updating the case. This is particularly apparent in teaching clinics. Weis points out that “templates, macros, automated data points, and copy-forward of an entire old note are just a few of the content-importing technology techniques”14 that create efficiencies of care and opportunities to improve the delivery of care and track the care but are often abused and misused, resulting in misrepresentation of the patient encounter as a result of cloned notes. The Veterans Administration reviewed 243 patient records from 1993 to 2002 and found that 2645 notes contained significant amounts of copied text, indicating a high prevalence in that care organization. This included diagnostic errors that were inadvertently copied and pasted from previous notes.14 This literature analysis revealed these practices to be a common occurrence in the records. This practice prohibited the integration of the appropriate clinical evidence into the EHR.
Although positive software features were available to improve the documentation, there was reported insufficient utilization of these features.29 Boonstra’s systematic review provided a good summary of the problems with EHRs. He concluded that this major change in a practice requires a “change manager” to oversee all of the implementation.30 He also pointed out that various barriers to full utilization of all available software features contributed to these errors as an underlying cause.23, 30
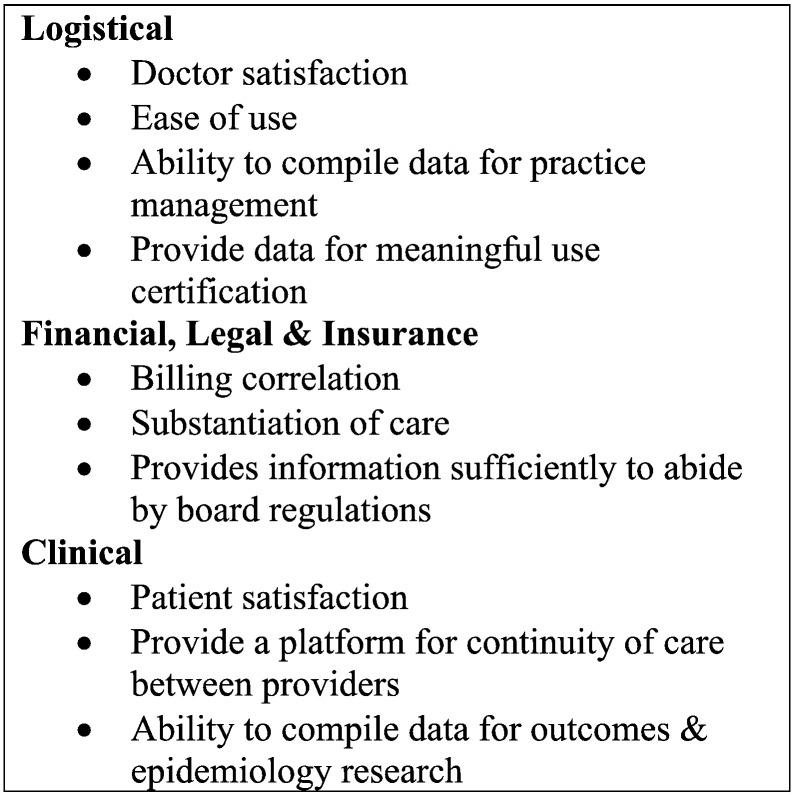
The Medicare Comprehensive Error Rate Testing review process found many common errors being carried through from the written record to the EHR entry. Although the notes are more legible than the written record, the carry-through errors include incomplete progress notes with insufficient detail, lack of a date or a signature, and lack of documentation of orders of different procedures or care plans. The Medicare chiropractic reviews revealed insufficient documentation to prove that care was not maintenance care.31 Thorough documentation is necessary for third-party payors to evaluate the medical necessity of care. It is also necessary for quality of care. Electronic health records are intended to overcome the problems of insufficient clinical detail by providing the basic clinical, financial, legal, and insurance needs of documentation32 (Fig 2). However, the reviewed literature revealed that there is a high rate of failure of the utilization of all of the features of EHRs. Poor information is available to inform the practitioner of what is required for utilization of all the features of the software program and successful implementation of the EHR.33
Fig 2.
Basic requirements of electronic health record system.
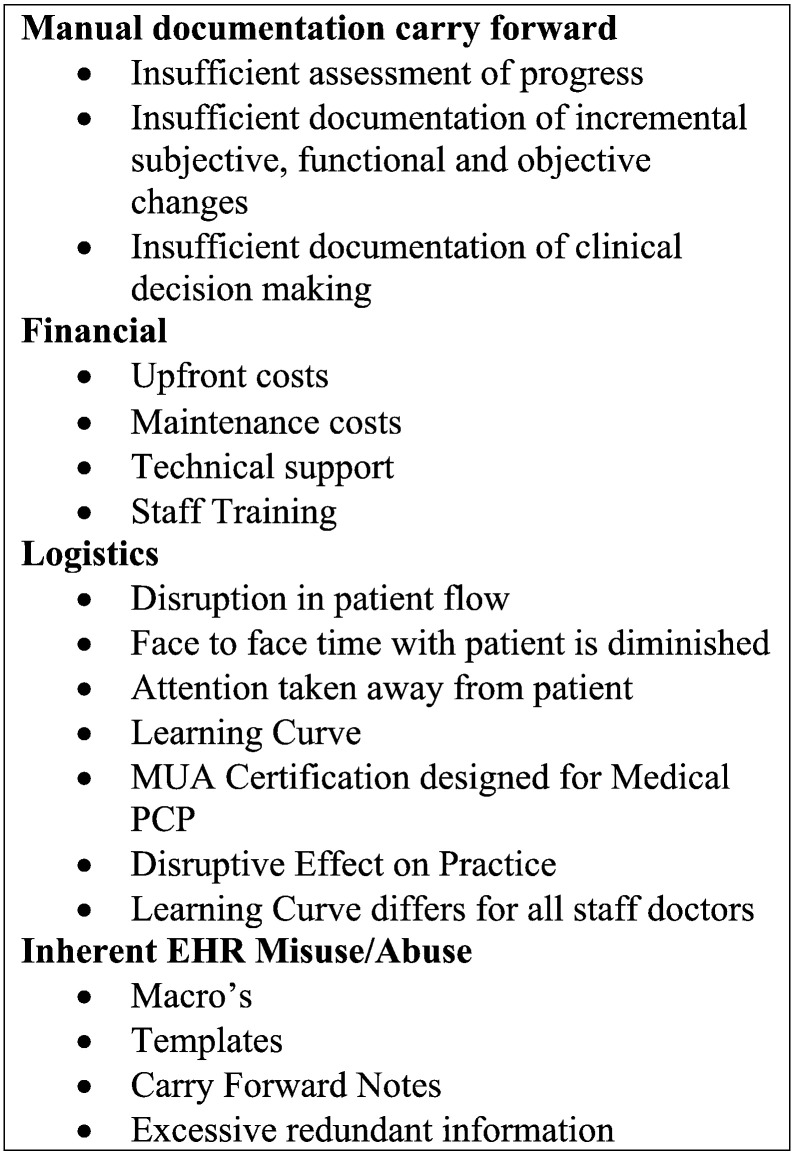
Challenges: Barriers to Implementation
Inappropriate EHR implementation can result in financial problems, logistical problems, and inherent misuse or abuse of the EHR (Fig 3). High costs, lack of certification of some products, and initial disruptive effects on practices all contribute to the difficulty in integration of the EHRs into practice. The disconnect among who pays for the EHR, who profits from it, and who is in charge of the implementation presents significant challenges that have prevented full EHR use in small independent offices.22, 34 Smaller independent offices have more difficulty absorbing the large upfront costs, decreased revenue during initial implementation, ongoing maintenance costs, and increased costs of hardware and software.22, 34 This is in spite of the potential long-term savings.
Fig 3.
Challenges in electronic health record (EHR) implementation.
A major implementation barrier was the lack of training of staff and doctors.35 This resulted in a decreased quality of clinical documentation and subsequent decrease in practice satisfaction.12, 13 Other barriers to full software feature implementation of EHRs have been reported to include a lack of incentive because of no vested interest in the EHR system by many users, psychosocial factors, financial factors, insufficient software training and utilization, lack of involvement of all staff in the implementation process, interoperability of different software systems, and a misunderstanding of the basic needs of documentation.23, 30, 34, 36, 37
Challenges: Doctor Satisfaction
Doctor satisfaction with use of the EHR is a factor in the degree of implementation and utilization. A RAND (Research and Development corporation) study performed by Friedberg for the AMA in 2013 revealed that the EHR and the resultant implementation burdens they put on practitioners are a major reason for doctor’s lack of satisfaction with practice.12 Sixty-five percent opined that the EHR failed to improve their job satisfaction. The EHR’s effect on job satisfaction exceeded the effect of health care delivery system changes on doctors’ job satisfaction. Despite this, 61% still felt that the EHR improved the quality of care, but many felt that it interfered with face-to-face time with the patient. This was often due to the doctor having to face the screen to enter data instead of facing the patient, causing him or her to miss body language, emotional responses, or opportunities to ask clarifying questions. Doctors were forced to divide their attention between the computer and the patient. If they chose to provide all their attention to the patient, they were burdened with lengthening their work hours to enter the data at lunchtime or after hours. The doctor is inhibited from creating a trusting, confident relationship with the patient. Surprisingly, in spite of the problems with EHRs, less than 20% of practitioners desired a return to manual records.12
Benefits of EHR Documentation
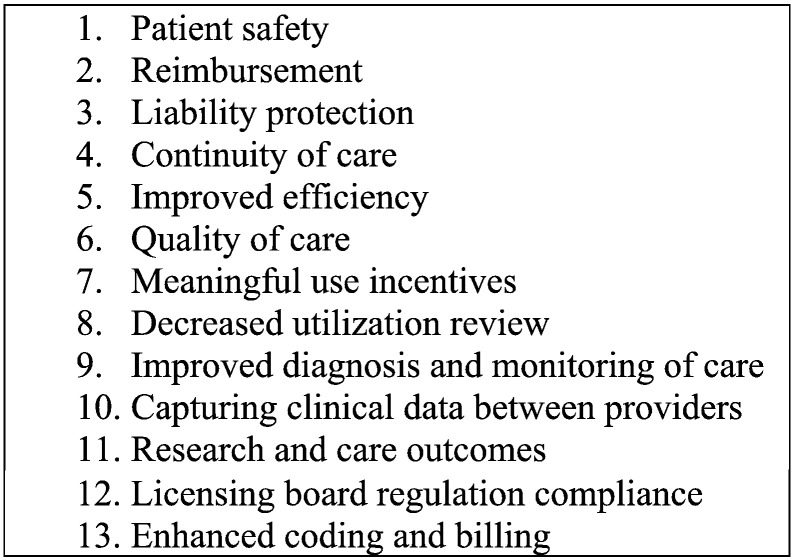
Electronic health records have inherent potential benefits that allow for improved quality of the clinical documentation in a more efficient manner. Some of the chiropractic EHR programs link up to a common database of prescription drugs. This allows doctors of chiropractic to obtain important information on the medications a patient takes, which would diminish the reliance on the accuracy of a patient’s ability to recite medication lists. Other programs have specific features to increase efficiency, quality, continuity of care, and patient safety. These benefits should provide an incentive for further EHR utilization by chiropractic physicians. Additional essential contemporary issues that any EHR documentation should satisfy (Fig 4)38 include protection of the legal liability of the practitioner, enhanced reimbursement, and public health issues.
Fig 4.
Essential issues that an electronic health record must satisfy.
Samaan38 reported that the implementation of EHRs resulted in a decreased frequency of incomplete charts 3 days postvisit and an increase in evaluation/management level coding, which resulted in increased income. There was also an eventual decrease in number of support staff, after the prolong implementation period.38 This would indicate the potential of EHRs to improve efficiency and improve the budget of the chiropractic office. Liang39 noted a perspective about the potential of EHRs to introduce new evidence from the patient population and to diffuse literature-based evidence into practice more quickly via integration of best practices into the clinical support software.39 This creates potential to enhance the ability of the chiropractic practitioner to improve the clinical documentation, decision making, and quality of care. Additional long-term savings through financial efficiencies and decreased staff are also reported,38 which support the financial benefit to the small chiropractic office.
As Dr. Weed stated 45 years ago, the clinical record is still central to care.1 This remains true, regardless of the format. However, the realization of the potential advantages of EHRs has lagged behind the implementation in spite the increased adoption rate. Regardless, the literature reports continue to expound the potential.40 Electronic health records literature specific to chiropractic practice is sparse. This review revealed only 4 peer-reviewed manuscripts and other trade journal, association, and governmental reports that address chiropractic documentation.
Recommendations for the Profession
Basic Needs of Documentation
Chiropractic EHR systems need to have features that allow customization of each encounter, to allow the appropriate documentation that attends to the basic documentation needs. Gutheil outlined 3 basic principles for documentation (Fig 2): the risk-benefit analysis, the use of clinical judgment, and patients’ capacity to participate in their own care.41 He refers to the necessity to document not only the risks, but also the benefits of care. This is especially important to comply with fully informed consent. It also protects the clinician’s liability and segues to the second principle of documenting the clinical judgment. An important factor related to clinical judgment is that it must be congruent with the clinical needs documented in the subjective presentation, objective findings, and overall patient assessment. The third principle states that the patient should be the primary master. Therefore, the records, whether written or electronic, need to relate the participation of the patient in his or her own care. This can be done through direct quotes in the subjective section, outcome measures, or recording the patient’s responses to the care. Documentation of these principles is difficult with preprogramed macros and templates and need customization.
To integrate the clinical data in an appropriate manner, it is recommended that the provider purchase and implement an EHR that fulfills the basic needs (Fig 2). Copied or cloned information must be reviewed and edited by the provider with each note generation. The note must be specific and pertinent to that clinical encounter. Copying entire sections of a document should be prohibited to avoid note redundancy. Students and doctors need to be trained to avoid overdocumentation by inserting false or irrelevant information. Training should also include proper use of macros, templates, or repetitive auto-population of fields in the software system. Histories, and both subjective and objective findings, need to be specifically constructed on each visit. Electronic health records will not innately correct carry-forward input problems. Repetitive pasting or carrying forward of the diagnosis in the Assessment section of the daily note fails to provide any ongoing clinical decision making. This is vital to support the level of the coding or the substantiation of the care. In consideration of federal compliance and legal protection, even with a sophisticated EHR system, there must be capability for the individual doctor to sign the notes. In doing so, the signer acknowledges responsibility for the content.
Funding of EHRs in Chiropractic
Small offices, which predominate in chiropractic, have financial difficulties in making the change to EHRs. The government incentive has expired, and other incentives are needed that encourage the change. Ryan42 reported that financial incentives for conversion to EHRs promote implementation with associated quality in care. One such experiment was successfully instituted by North Shore Hospital, NY. They found that most offices that lacked EHRs were small offices. Ryan reported an offer of up to $40 000 per office for the conversion to, and implementation of, EHRs. The study found that financial incentives and technical support resulted in improved quality of care.43 This study provides an indication of the need for ongoing financial incentives as governmental incentives expire. Because the majority of chiropractic practices are small offices, a similar incentive by payors would help in the sharing of the expense for the demands of the payors.
Purchasing EHRs
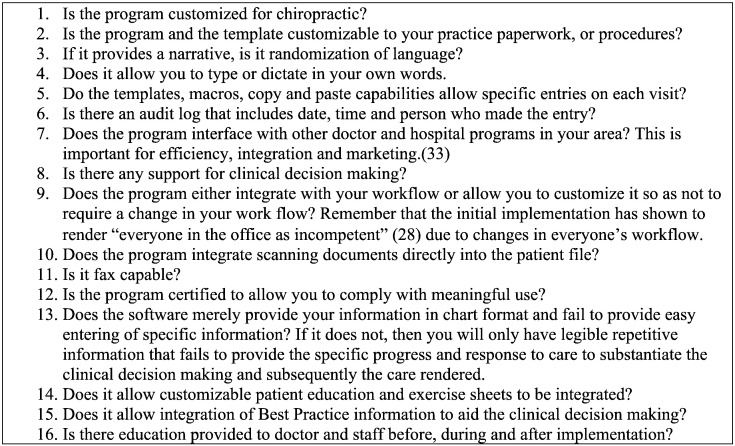
The ability to integrate the appropriate clinical data into the EHR is dependent on the quality of the software purchased. In consideration of the level of technical, compliance, and documentation knowledge and sophistication of the average doctor of chiropractic, providers need preliminary EHR training to guide them in their EHR evaluation and purchase. McGregor37 did a fine job of outlining the stages of evaluation. A number of pointed questions are outlined for advice (Fig 5). Diamond et al44 also provide a nice scorecard to compare vendors. They set up a method of comparing vendors and looking at support, hardware, software, workflows, and reporting with specific criteria outlined.44 Maust35 discusses the necessary training and outlines specific questions to ask vendors. Without proper purchase and training, documentation would remain insufficient, regardless of the investment.
Fig 5.
Questions to ask when purchasing an electronic health record (EHR) system. (Data from McGregor.38)
EHR Implementation
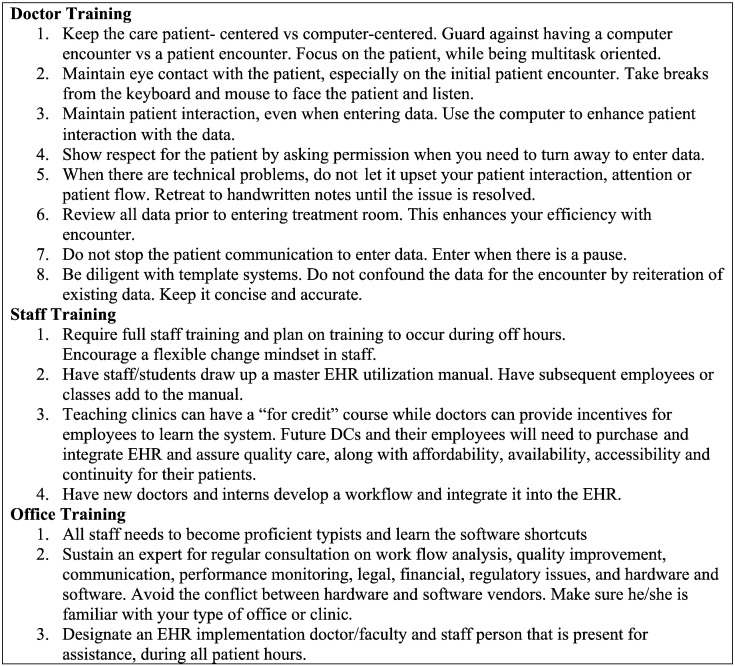
After an appropriate EHR purchase is made, the ability to integrate the clinical data is still contingent on an implementation plan for all doctors, interns, staff, and allied health assistants. The success of full implementation and utilization of all features depends on the training.45 This includes the training in the sociological aspect of utilizing the EHR during the patient contact. Some suggestions are intuitive but need to be emphasized (Fig 6).15, 36, 46, 47
Fig 6.
Recommendations for optimal electronic health record (EHR) implementation and documentation. (Data from Maust,35 Fleurant,45 Bostrom,36 Torda,46 Fredericks,15 and Lyons.47)
Wuerth48 makes the following additional suggestions: Be patient; competency in EHRs can take up to a year. Until that time, one can expect a decrease in productivity. He also emphasizes the importance of not allowing the EHR to direct patient contact, but that it is important to allow patients to participate in the EHR. Facing the patient instead of the computer for most of the encounter is integral to the contact.
In spite of the difficulties, the training of new doctors will need to include how to integrate quality data and any literature references into the documented electronic record. Training in the appropriate EHR begins with the new doctors entering the occupation. Interns in teaching institutions may only obtain an introduction to EHRs. They will often have insufficient time in their clinic rotations to become competent and proficient.48 It might be difficult to institute EHRs in a teaching clinic, unless the attending clinicians are the primary providers of care vs the interns. It is likely that workflows would never get established because of the ongoing EHR learning, adaptation periods, and transitional nature of interns. The constant transition period would cause longer patient wait times and further prolong the intern-patient contact time, decrease patient flow, and diminish income. Because of the growing need for the chiropractor to provide clinical evidence in the documentation, it is still suggested that interns be provided additional training and simulated entries for virtual patients before entering the clinical environment.
Most EHR documentation errors are innate in the EHR software. As an incidental note, the high prevalence of inherent errors from these sources, regardless of the specialty, appears to contradict a perception of documentation fraud by the individual practitioner. Chiropractic record improvement will require diligence to the educational process, purchase of the appropriate EHR software, attention to the implementation process, training of staff and chiropractors, appropriate utilization, and attentiveness to the data entry by the treating doctor. It will also require the practitioner to maximize the existing features of the software and customize it to the practice. Funding from sources outside the chiropractic profession might be necessary to reach all the goals of the quality chiropractic EHR. Until these issues are addressed, the clinical data may continue to be deficient in the EHR. This would result in an ongoing inability to demonstrate the necessity of care.
Finally, documentation serves many stakeholders. Readers other than the treating doctor will include the consulting doctor, other health care practitioners involved in the care, the payor, the insurer, the reviewer, and, if it goes to court for any reason, the attorney. The necessary contents of the record are outlined in Medicare meaningful use criteria and by the National Committee for Quality Assurance.49 Most of these government and quality assurance guidelines target the primary care practitioner. Although some of it does not immediately apply to chiropractic practitioners, they are now being held responsible to a similar level of documentation by the payors. Overall, if doctors of chiropractic can follow the recommendations in this paper, then they can provide sufficient clinical documentation in the electronic record for all potential readers of the record. Additional resources on EHR implementation are available through the American Academy of Family Physicians and the National Institutes of Health.50, 51, 52
Limitations
Because this was a narrative review aimed at generating possible directions for the chiropractic profession, it was limited in scope. The search strategy used may have missed relevant papers. In addition, other important search engines were not used, and therefore, relevant papers to this topic may have been omitted. The search and review was performed by only one person, so some bias may have been introduced with interpretation.
Conclusions
This review revealed that the current quality of the documentation in EHRs remains a challenge, with insufficient documentation to substantiate the quality and necessity of care. Common errors in using the EHRs were found in both chiropractic and other health care practitioners. These errors were more often a result of problems with software misuse or abuse, budgetary constraints, insufficient training, or carry-forward errors from manual methods. Electronic health records training, continued financial incentives, appropriate implementation processes, and utilization of available software features may decrease documentation errors.
Funding Sources and Conflicts of Interest
No funding sources or conflicts of interest were reported for this study.
Acknowledgments
The author thanks Claire Noll, MS, CGS, MLIS, of the Texas Chiropractic College Library system for her helpful assistance. The author acknowledges Dr. John Ward and Dr. Cheryl Hawk for their input with this manuscript.
References
- 1.Weed LL. Medical records, patient care, and medical education. Irish J Med Sci. 1964;39(6):271–282. doi: 10.1007/BF02945791. [DOI] [PubMed] [Google Scholar]
- 2.State of Massachusetts . 1999. Standards of Practice and Professional Conduct, 233 CMR 4.05. [Google Scholar]
- 3.Federation of Chiropractic Licensing Boards . FCLB; Greeley, CO: 2006. Documentation and Record Keeping, Resolution #2-06; p. 2006. [Google Scholar]
- 4.Triano JJ. What constitutes evidence for best practice? J Manipulative Physiol Ther. 2008;31(9):637–643. doi: 10.1016/j.jmpt.2008.10.009. [DOI] [PubMed] [Google Scholar]
- 5.Levinson D. Dept. of Health and Human Services, Office of the Inspector General; Washington, DC: 2009. Inappropriate Medicare Payments for Chiropractic Services. [Google Scholar]
- 6.Schetchikova NV. Documentation with EHR—easier, faster, better? ACA News. 2011 Jan. [Google Scholar]
- 7.Kline CM. Chiropractic summit: for the good of the profession. ACA News. 2014 May [Google Scholar]
- 8.Levinson H. Managed care and chiropractic part ii: challenges ahead. J Am Chiropr Assoc. 2008;45(3):7–12. [Google Scholar]
- 9.Quick Notes, Inc Laser Barcoding System. 1988-2015. http://www.qnotes.com/quix/ Available at:
- 10.Booth A. “Brimful of STARLITE": toward standards for reporting literature searches. J Med Libr Assoc. 2006;94(4):421–429. e205. [PMC free article] [PubMed] [Google Scholar]
- 11.Nemeth LS, Stuart GW, Ornstein SM. Implementing change in primary care practices using electronic medical records: a conceptual framework. Implement Sci. 2008;3:3. doi: 10.1186/1748-5908-3-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Friedberg M, Chen P, Van Busam KR. RAND Corporation; Santa Monica, CA: 2013. Factors Affecting Physician Professional Satisfaction and Their Implications for Patient Care, Health Systems, and Health Policy. [PMC free article] [PubMed] [Google Scholar]
- 13.Gallegos A. Are you satisfied? What drives physician professional satisfaction in a time of dwindling face-time with patients? Mich Med. 2014;113(2):10–14. [PubMed] [Google Scholar]
- 14.Weis JM, Levy PC. Copy, paste, and cloned notes in electronic health records: prevalence, benefits, risks, and best practice recommendations. Chest. 2014;145(3):632–638. doi: 10.1378/chest.13-0886. [DOI] [PubMed] [Google Scholar]
- 15.Fredericks M, Lyons L, Kondellas B, Ross MW, Hang L, Fredericks J. Chiropractic physicians: an analysis of select issues for the use of electronic medical records and the patient-practitioner relationship within the society-culture-personality model. J Chiropr Humanit. 2009;16(1):13–20. doi: 10.1016/j.echu.2010.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hing E, Hsiao C-J. Electronic medical record use by office-based physicians and their practices: United States, 2007. Natl Health Stat Report. 2010;31(23):1–11. [PubMed] [Google Scholar]
- 17.Hsiao CJ, Hing E. Use and characteristics of electronic health record systems among office-based physician practices: United States, 2001-2013. NCHS Data Brief. 2014;143:1–8. [PubMed] [Google Scholar]
- 18.Smith M., Young M. Information technology for clinical and business applications in chiropractic practice. J Am Chiropr Assoc. 2010;47(3):10–17. [Google Scholar]
- 19.Bates DW. Rockville, MD; Agency for Healthcare Research & Quality: 2008. Statewide Implementation of Electronic Health Records. [Google Scholar]
- 20.Li J, Talaei-Khoei A, Seale H, Ray P, MacIntyre CR. Health care provider adoption of eHealth: systematic literature review. Interact J Med Res. 2013;2(1) doi: 10.2196/ijmr.2468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Center for Medicare and Medicaid Services . Center for Medicare and Medicaid Services; Washington, DC: 2015. Medicare Incentive Payments. E.I. Program. [Google Scholar]
- 22.Goetz Goldberg D, Kuzel AJ, Feng LB, DeShazo JP, Lov LE. EHRs in primary care practices: benefits, challenges, and successful strategies. Am J Manag Care. 2012;18(2):e48–e54. [PubMed] [Google Scholar]
- 23.Valdes I, Kibbe DC, Tolleson G, Kunik ME, Petersen LA. Barriers to proliferation of electronic medical records. Inform Prim Care. 2004;12(1):3–9. doi: 10.14236/jhi.v12i1.102. [DOI] [PubMed] [Google Scholar]
- 24.Belletti D, Zacker C, Mullins CD. Perspectives on electronic medical records adoption: electronic medical records (EMR) in outcomes research. Patient Relat Outcome Meas. 2010;1:29–37. doi: 10.2147/prom.s8896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.American Medical Association Release of disappointing meaningful use data prompts industry leaders to urge HHS to take immediate action. AMA News Room. 2014 November 4 [Google Scholar]
- 26.Berko C. Better documentation, better reimbursement. Today’s Chiropractic. 2002;31(6):56–58. [Google Scholar]
- 27.Centers for Medicare & Medicaid Services Medicare Program; Merit-Based Incentive Payment System (MIPS) and Alternative Payment Model (APM) Incentive Under the Physician Fee Schedule, and Criteria for Physician-Focused Payment Models. https://www.federalregister.gov/documents/2016/11/04/2016-25240/medicare-program-merit-based-incentive-payment-system-mips-and-alternative-payment-model-apm Available at: Accessed December 22, 2016. [PubMed]
- 28.Agency for Healthcare Research and Quality . AHRQ Publication No. 01-P020. Agency for Healthcare Research and Quality; Rockville, MD: 2006. Practice-Based Research Networks (PBRNs) Fact Sheet. [Google Scholar]
- 29.Price M, Singer A, Kim J. Adopting electronic medical records: are they just electronic paper records? Can Fam Physician. 2013;59(7):e322–e329. [PMC free article] [PubMed] [Google Scholar]
- 30.Boonstra A, Broekhuis M. Barriers to the acceptance of electronic medical records by physicians from systematic review to taxonomy and interventions. BMC Health Serv Res. 2010;10:231. doi: 10.1186/1472-6963-10-231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Medicare Learning Network . Department of Health & Human Services, Centers for Medicare & Medicaid Services; Rockville, MD: 2014. Complying with Medical Record Documentation Requirements. [Google Scholar]
- 32.Scott RW. 4th ed. Jones & Bartlett Learning; Burlington, MA: 2011. Legal, Ethical, and Practical Aspects of Patient Care Documentation : a Guide for Rehabilitation Professionals; p. xix. [Google Scholar]
- 33.Logan J. Electronic health information system implementation models—a review. Stud Health Technol Inform. 2012;178:117–123. [PubMed] [Google Scholar]
- 34.Baron RJ, Fabens E, Schiffman M, Wolf E. Electronic health records: just around the corner? Or over the cliff? Ann Intern Med. 2005;143(3):222–226. doi: 10.7326/0003-4819-143-3-200508020-00008. [DOI] [PubMed] [Google Scholar]
- 35.Maust D. Implementation of an electronic medical record in a health system: lessons learned. J Nurses Staff Dev. 2012;28(1):E11–E15. doi: 10.1097/NND.0b013e318240a715. [DOI] [PubMed] [Google Scholar]
- 36.Bostrom AC, Schafer P, Dontje K, Pohl JM, Nagelkerk J, Cavanagh SJ. Electronic health record: implementation across the Michigan Academic Consortium. Comput Inform Nurs. 2006;24(1):44–52. doi: 10.1097/00024665-200601000-00011. [DOI] [PubMed] [Google Scholar]
- 37.McGregor DM. Evaluation of the steps for implementation of electronic health records for a small chiropractic practice in Northern Michigan. J Chiropr Humanit. 2009;16(1):54–56. doi: 10.1016/j.echu.2010.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Samaan Z, Klein MD, Mansour ME, DeWitt TG. The impact of the electronic health record on an academic pediatric primary care center. J Ambul Care Manage. 2009;32(3):180–187. doi: 10.1097/JAC.0b013e3181ac9667. [DOI] [PubMed] [Google Scholar]
- 39.Liang L. The gap between evidence and practice. Health Affairs. 2007;26(2):w119–w121. doi: 10.1377/hlthaff.26.2.w119. [DOI] [PubMed] [Google Scholar]
- 40.Eisenberg M, Hom J, Sharp C. The electronic health record as a healthcare management strategy and implications for obstetrics and gynecologic practice. Curr Opin Obstet Gynecol. 2013;25(6):476–481. doi: 10.1097/GCO.0000000000000029. [DOI] [PubMed] [Google Scholar]
- 41.Gutheil TG. Fundamentals of medical record documentation. Psychiatry (Edgmont) 2004;1(3):26–28. [PMC free article] [PubMed] [Google Scholar]
- 42.Ryan AM, McCullough CM, Shih SC, Wang JJ, Ryan MS, Casalino LP. The intended and unintended consequences of quality improvement interventions for small practices in a community-based electronic health record implementation project. Med Care. 52(9):826-832. [DOI] [PubMed]
- 43.Shea S, Hripcsak G. Accelerating the use of electronic health records in physician practices. N Engl J Med. 2010;362(3):192–195. doi: 10.1056/NEJMp0910140. [DOI] [PubMed] [Google Scholar]
- 44.Diamond E, French K, Gronkiewicz C, Borkgren M. Electronic medical records: a practitioner's perspective on evaluation and implementation. Chest. 2010;138(3):716–723. doi: 10.1378/chest.09-1328. [DOI] [PubMed] [Google Scholar]
- 45.Fleurant M, Kell R, Jenter C. Factors associated with difficult electronic health record implementation in office practice. J Am Med Inform Assoc. 2012;19(4):541–544. doi: 10.1136/amiajnl-2011-000689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Torda P, Han ES, Scholle SH. Easing the adoption and use of electronic health records in small practices. Health Aff (Millwood) 2010;29(4):668–675. doi: 10.1377/hlthaff.2010.0188. [DOI] [PubMed] [Google Scholar]
- 47.Lyons JP, Klasko S. Introduction of an electronic medical record system into physician practice offices: why is it so #%!&-ing hard for everybody? Part III. J Med Pract Manage. 2011;27(1):36–39. [PubMed] [Google Scholar]
- 48.Wuerth R, Campbell C, King WJ. Top 10 tips for effective use of electronic health records. Paediatr Child Health. 2014;19(3):138. doi: 10.1093/pch/19.3.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.National Committee for Quality Assurance (NCQA) Guidelines for medical record documentaion. 2009. http://www.ncqa.org/portals/0/policyupdates/supplemental/guidelines_medical_record_review.pdf Available at: Accessed January 22, 2015.
- 50.AAFP Things to think about before going live—selecting & implementing an EHR. http://www.aafp.org/practice-management/health-it/product.html Available at: Accessed March 3, 2015.
- 51.US Dept of Health and Human Services Practice Transformation Toolkit. https://www.healthit.gov/providers-professionals/implementation-resources/practice-transformation-toolkit Available at: Accessed November 14, 2017.
- 52.US Dept of Health and Human Services. How to implement EHRs https://www.healthit.gov/providers-professionals/ehr-implementation-steps Available at: Accessed November 14, 2017.