Abstract
Aims
Clavicle fracture nonunions are extremely rare in children. The aim of this systematic review was to assess what factors may predispose children to form clavicle fracture nonunions and evaluate the treatment methods and outcomes.
Methods
We performed a systematic review according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines, aiming to find papers reporting clavicle fracture nonunion in children under the age of 18 years. Data was collected on patient demographics, fracture type, mechanism of injury (MOI), surgical intervention and reported outcome. Two independent reviewers evaluated all the data.
Results
A total of 13 articles reporting 21 cases of clavicle fracture nonunion were identified. The mean age at time of injury was 11.4 years (4 to 17). Falls were the most common MOI. The majority of nonunions occurred after displaced fractures on the right side. Six were refractures. Mean time of presentation following injury was 13.5 months (4 to 60). In all, 16 were treated surgically. Radiographic union was eventually achieved in 12 cases, with functional outcome satisfactory in all cases.
Conclusion
Clavicle nonunion is an extremely rare but possible complication in children. The majority occur after displaced right-sided fractures or refractures and present around one year after injury. Surgical fixation provides good radiographic healing and functional outcomes.
Level of evidence
IV
Keywords: Clavicle, fracture, nonunion, paediatric
Introduction
Clavicle fractures are among the most common bony injuries in the paediatric population, accounting for 7% to 15% of all paediatric fractures.1,2 Approximately 95% of clavicle fractures in children occur within the middle third.2-4 The vast majority of these fractures are treated conservatively with a supportive sling and yield excellent results.2,4-11 Whilst clavicle fracture nonunion is a recognized complication in the adult population, with reported rates ranging from 6% to 12%,12-14 the incidence of nonunion in the paediatric population is extremely rare.
There are currently very few published retrospective reviews that include the incidence of clavicle nonunion in children.15,16 We present findings from a systematic review of the literature on this rare condition. We aim to discuss potential risk factors for occurrence of clavicle fracture nonunion and re-examine the current management of clavicle fractures in the paediatric population.
Materials and methods
Search strategy
A systematic review was conducted according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.17 An online literature search was carried out on all databases through the OVID interface, from their inception to the search date of 15 August 2017. These include Embase, MEDLINE, PsychINFO and Journals@Ovid. The search strategy terms used on MEDLINE (via OVID) are shown in Table 1. In addition, searches of grey literature were conducted using Google Scholar, Web of Science and British Medical Journal Case Reports. The search strategy was modified for the other databases. The reference list for each potentially eligible text was reviewed to identify any additional relevant articles.
Table 1.
Search terms used to interrogate MEDLINE (via OVID)
| 1. Clavicle [mp = title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] |
| 2. Nonunion [mp = title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] |
| 3. Non-union [mp = title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] |
| 4. 2 or 3 |
| 5. 1 and 4 |
| 6. Child [mp = title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] |
| 7. Paediatric [mp = title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] |
| 8. 6 or 7 |
| 9. 5 and 8 |
Eligibility criteria and identification
The systematic review included studies of any design reporting on: 1) nonunion following a clavicle fracture; 2) patients under the age of 18. We excluded: 1) papers with insufficient demographic details such as the age or gender of the patient; 2) cases of nonunion in skeletal dysplasias or congenital pseudoarthroses; and 3) papers written in languages other than English.
Two authors (KH and JK) conducted electronic searches independently. Screening of the titles and abstracts to identify potentially eligible citations were also conducted independently. Disagreements were resolved in consensus. The senior author (YG) was consulted when required to assess the suitability of the text for inclusion. Potentially eligible texts were read and reviewed in full. Both reviewers demonstrated substantial agreement.
Data extraction and critical appraisal
Two reviewers (KH, JK) independently extracted all data relevant for systematic review with the use of a data collection table. The data extracted included: age at injury, gender, mechanism of injury (MOI), laterality of injury, fracture displacement, site (medial, middle or lateral third), history of refracture, time from injury to diagnosis of nonunion, treatment (surgical or conservative) and evidence of radiological union. Data extraction was deemed complete once all reviewers were in complete agreement.
Results
The initial literature search resulted in a total of 315 articles. Once duplicates were removed, 212 articles remained. An initial screening of titles and abstracts yielded 92 potentially eligible articles. Inclusion and exclusion criteria were utilized on the full texts of these. From this, 19 potentially eligible papers were identified. A paper written in French18 and a case of cleidocranial synostosis19 were excluded. Four papers without any details on individual patients’ age and gender were excluded.3,20-22 This resulted in a total of 13 articles4, 15, 16, 23-32 reporting 21 cases of clavicle nonunion in patients under the age of 18.
An overview of the literature selection process is shown in Figure 1.
Fig. 1.
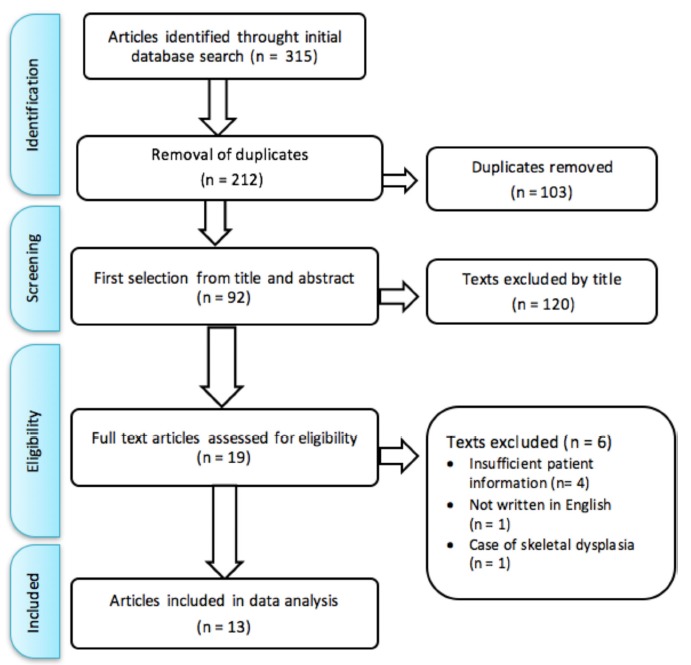
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram of data selection process.
Table 2 gives an overview of the data extracted from the literature search. A total of 13 articles reporting 21 cases of clavicle nonunion were identified. A total of 14 patients were male and the mean age at time of injury was 11.4 years (4 to 17). The MOI was stated in 17 of cases. Falls were the most common MOI and caused 14 of these 17 cases. Two children fractured their clavicle in a road traffic accident and one during karate. In the 12 cases where laterality was stated, 11 were right-sided fractures. The location of the fracture was mentioned in 14 cases, of which two were fractures of the lateral third of the clavicle and 12 were fractures of the middle third. In the 12 cases where fracture displacement was stated or could be interpreted from radiographs, ten were displaced fractures. Six were cases of nonunion that occurred after a refracture. There were two notable cases of nonunion, one resulting in development of an arteriovenous fistula of the external jugular vein23and one case of nonunion in a four-year-old boy with vitamin D deficiency.24
Table 2.
Literature review of paediatric post-traumatic mid-shaft clavicle fractures
| Author | Journal | No. | Age (yrs) | Gender | MOI | Laterality | Fracture site (lateral, middle or medial third) | Displaced | Refracture | Additional clinical information | Time from injury to diagnosis of nonunion (mths) | Treatment | Evidence of radiological union |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Nogi et al (1975)28 | Clin Orthop Relat Res | 1 | 12 | M | Fall | Right | Lateral | NS | No | - | 6 | S | NS |
| 2 | 7 | M | Fall | NS | NS | NS | No | - | * | S | Yes | ||
| 3 | 12 | M | Fall | NS | NS | NS | Yes | - | * | C | No | ||
| Wilkins and Johnston (1983)16 | J Bone Joint Surg Am | 4 | 13 | M | Fall | NS | NS | NS | No | - | 10 | C | No |
| 5 | 15 | F | Fall | NS | NS | NS | Yes | † | 12 | S | Yes | ||
| 6 | 17 | M | Fall | NS | NS | NS | Yes | ‡ | 60 | S | No | ||
| 7 | 17 | M | RTA | NS | NS | NS | No | - | 12 | C | No | ||
| Caterini et al (1998)29 | Arch Orthop Trauma Surg | 8 | 7 | F | Fall | Right | Middle | Yes | No | - | 14 | S | Yes |
| Jain et al. (2009)27 | Shoulder & Elbow | 9 | 7 | F | Fall | Right | Middle | NS | Yes | - | 14 | S | Yes |
| 10 | 9 | F | NS | Right | Middle | Yes | No | - | 23 | S | NS | ||
| Spapens et al (2010)30 | JPO B | 11 | 8 | F | Fall | Right | Middle | No | No | - | 12 | S | Yes |
| Gupta et al (2010)31 | N Am J Med Sci | 12 | 8 | M | Fall | Right | Middle | NS | No | - | 12 | C | No |
| Pourtaheri et al (2012)32 | Orthopedics | 13 | 10 | M | Fall | Right | Middle | Yes | No | - | 4 | S | NS |
| Strauss et al (2012)4 | Journal of Emergency Medicine | 14 | 17 | M | NS | NS | Lateral | Yes | NS | - | NS | NS | NS |
| Wu et al (2013)23 | N Am J Med Sci | 15 | 13 | M | NS | Right | Middle | Yes | No | ** | 6 | S | Yes |
| Randsborg et al (2014)25 | JPO | 16 | 15 | M | Fall | NS | Middle | Yes | No | - | 5.5 | S | Yes |
| Smith and Williams (2016)26 | JPO B | 17 | 9 | M | Fall | Right | Middle | Yes | Yes | * | 9 | S | Yes |
| Duplantier and Waldron (2016)24 | JPO B | 18 | 4 | M | Fall | Right | Middle | Yes | No | †† | 6 | S | Yes |
| Pennock et al (2017)15 | Journal of Shoulder and Elbow Surgery | 19 | 12 | F | Karate | Right | Middle | Yes | No | - | 7 | S | Yes |
| 20 | 13 | M | RTA | NS | NS | Yes | Yes | ‡‡ | 9 | S | Yes | ||
| 21 | 14 | F | NS | Left | Middle | No | No | - | 21 | S | Yes |
excluded due to presumed error in original text
nonunions occurred after three ipsilateral refractures
metalwork failure after surgical management
nonunion lead to development of an arteriovenous fistula of the external jugular vein
case of nonunion in a vitamin D deficient child
clavicle fracture and closed head injury. Required three operations to manage as follows: (1) plate and bone graft at nine months post injury after presenting with symptomatic nonunion (2) removal of metalwork and regrafting six months later (3) dual plating with bone and morphogenetic protein grafting three years later
MOI, mechanism of injury; NS, not stated; RTA, road traffic accident; S, surgical; C, conservative
Time from injury to diagnosis of nonunion was stated in 18 of the cases. These cases presented with a mean time of 13.5 months following initial injury (4 to 60). Management strategy was stated in 20 of the cases. In all, 16 were treated surgically by means of open reduction and internal fixation (ORIF). In six cases a bone graft was used. Of the 21 total cases, whether or not radiographic union was eventually achieved was stated in 17 cases. There were five persistent nonunions in total (four of which were treated conservatively and one persistent nonunion post-surgery following three ipsilateral refractures). Of the 16 surgically managed nonunions, whether or not radiographic union was eventually achieved was stated in 13 cases. In all, 12 of these eventually achieved radiographic union. Of the five persistent nonunions, four were asymptomatic. Where reported, the functional outcome was satisfactory in all cases.
Discussion
Clavicle fractures are common injuries in both adults and children.1,2,33,34 In children, management is normally non-operative with a supportive sling and avoidance of high-risk activity such as contact sports for several weeks. There is ample evidence to demonstrate the efficacy of this line of management.2,4-11
Primary surgical fixation of clavicle fractures in children is uncommon. In a retrospective review of 939 children with clavicle fractures over a 21-year period, only 15 (1.6%) required operative intervention. The most common indication was potential skin perforation.35 There has been recent debate in the literature regarding the management of clavicle fractures in children, especially in those approaching skeletal maturity. Whilst better functional outcomes following surgery have been previously reported,36 there is recent evidence to suggest there is no difference in outcomes between operative and nonoperative management.8,37,38 Primary operative fixation is mainly reserved for open or impending open fractures, polytrauma, floating shoulder injuries, completely displaced and significantly shortened fractures in adolescents or high-performing adolescent athletes.7-9,39-41
Paediatric clavicle fracture nonunion is extremely rare. Even in large retrospective reviews of clavicle fractures in children, no nonunions have been identified. For example, Kessler et al3 found no cases of nonunion in their retrospective study of 791 children and adolescent clavicle fractures; 28% of these fractures were displaced and 2.2% were refractures. A retrospective study in Ireland of 190 clavicle fractures (35% displaced) in children aged less than 16 years, found that none went on to develop nonunion.11 Randsborg et al25 retrospectively reviewed the outcome of 185 clavicle fractures in the adolescent population (37.8% being displaced mid-shaft fractures) and found only one case of nonunion and one case of delayed union at two-year follow-up, both of which were completely displaced. Strauss et al4 found only one case of clavicle fracture nonunion and three delayed unions across their four-year series of 537 children. They deemed predictors for delayed union and nonunion to be complete fracture displacement and increasing age.
A limited number of reviews have specifically looked at the incidence of clavicle nonunion in children. A recent retrospective ten-year review across nine hospitals sought to find all cases of clavicle nonunion in patients younger than 19 years. A total of 25 cases were identified, with a mean age of 14.5 years (10.0 to 18.9). In all, 13 of these were completely displaced fractures and eight were refractures. All of these were managed surgically.15 A 21-year review of clavicle fracture nonunion in both adults and children identified 31 cases of clavicle nonunion. Six of these were in children, with only two in children aged less than 15 years old.16 In all, 21 fractures were completely displaced and seven were refractures. As acknowledged by Pennock et al,15 such a limited set of cases makes drawing larger conclusions and analysis of risk stratification difficult. This systematic review re-affirms that completely displaced fractures and refractures of the ipsilateral clavicle may be more predisposed to nonunion.
It is important to distinguish fracture nonunion from congenital pseudoarthrosis of the clavicle.42 These generally occur in females on the right side,43,44 and present at birth as a painless lump on the clavicle that can grow with time without any history of trauma. The distinctive radiographic features were described by Owen.10,45
We note with interest that the vast majority of the cases occurred on the right side. Smith and Williams26 have made the connection between this and the predominance of congenital pseudoarthrosis on the right side. They hypothesized that these may be underlying subclinical pseudoarthroses not visible on a plain radiograph that predispose the clavicle to fracture and subsequent nonunion. There is no clear laterality predominance of clavicle fractures in adults33,34 and published epidemiological data on the laterality of clavicle fractures in children is too limited to explore a hand dominance hypothesis.
It is noteworthy that of the cases reviewed, only five nonunions (24%) occurred in children older than 14 years, compared with 16 (76%) in children younger than 14 years. We would expect to see a greater incidence of nonunion in adolescents as they approach skeletal maturity and the adult clavicle nonunion rate of 6% to 12%.12-14 Although this has been the case in other series,3,4,15 the relatively younger mean age of 11 years in this review could be attributed to reporting bias of this rare outcome.
Surgical fixation was performed in 16 of the 20 cases where management strategy was reported. All cases managed surgically with an ORIF from 2009 onwards (n = 11) utilized plate and screw fixation. Six of these cases used bone grafting. Other ORIF techniques used included screw fixation alone or intramedullary fixation. Radiographic union was achieved in 12 of the 17 cases where this was reported. Good functional outcomes were achieved in all cases. This would suggest that stabilization of these fractures is key in achieving fracture consolidation and supports the hypothesis of inadequate biomechanics for fracture healing and not inadequate physiology.
Despite its rarity, clavicle fracture nonunion in children remains possible and must be taken into consideration when managing this common injury. Jain et al27 suggested that all children should have radiographic evidence of fracture union prior to discharge from the orthopaedic outpatient clinic. However, the majority of evidence suggests that serial imaging of the clavicle in asymptomatic children is unnecessary.11,46 While symptomatic nonunions following displaced clavicle fractures in adults are quite common12-14, this review demonstrates this is not the case for children, and conservative management should remain the mainstay of primary treatment. However, clinicians should be aware that, unsurprisingly, completely displaced fractures and refractures may show a greater propensity to nonunion.
We do not advocate routine utilization of serial radiographs and follow-up appointments to confirm fracture union. We do advocate a pragmatic approach to the treatment of these seemingly benign injuries. Parents or guardians should be given appropriate information regarding management and red flags and be advised to report any on-going pain following a standard period of supportive sling treatment.
There is little contention on the management of clavicle fracture in children. Nonunion is a rare but possible complication which can be managed successfully with surgical fixation. This review re-affirms that completely displaced fractures and refractures may show a greater propensity to nonunion. It is important that clinicians are aware of this rare complication and are prepared to offer surgical fixation when nonunion is identified. Further work is needed on further risk factors that may predispose children to clavicle fracture nonunion.
Clinical Relevance
This is a systematic review of a rare outcome of a very common paediatric fracture. This review re-iterates previously proposed risk factors for clavicle nonunion to allow clinicians to be vigilant in their identification and treatment of this rare, but potentially debilitating outcome.
Compliance with Ethical Standards
Funding Statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Ethical Statement
Ethical approval: This research does not involve human participants or animals.
Informed consent: Informed consent was not required. The study was registered with the Joint Research and Enterprise Office.
References
- 1.Rennie L, Court-Brown CM, Mok JYQ, Beattie TF.. The epidemiology of fractures in children. Injury 2007;38:913-922. [DOI] [PubMed] [Google Scholar]
- 2.Calder JDF, Solan M, Gidwani S, Allen S, Ricketts DM.. Management of paediatric clavicle fractures--is follow-up necessary? An audit of 346 cases. Ann R Coll Surg Engl 2002;84:331-333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kessler J, Gardner I, Corral J.. Pediatric clavicular shaft fractures treated nonoperatively: assessment of treatment results, fracture patterns, modes of injury, and patient demographics. Annual Meeting of the Pediatric Orthopaedic Society of America 2009;30. [Google Scholar]
- 4.Strauss BJ, Carey TP, Seabrook JA, Lim R.. Pediatric clavicular fractures: assessment of fracture patterns and predictors of complicated outcome. J Emerg Med 2012;43:29-35. [DOI] [PubMed] [Google Scholar]
- 5.Wilkes JA, Hoffer MM.. Clavicle fractures in head-injured children. J Orthop Trauma 1987;1:5-58. [DOI] [PubMed] [Google Scholar]
- 6.Boutis K. Common pediatric fractures treated with minimal intervention. Pediatr Emerg Care 2010;26:152-157. [DOI] [PubMed] [Google Scholar]
- 7.Caird MS. Clavicle shaft fractures. J Pediatr Orthop 2012;32:S1-S4. [DOI] [PubMed] [Google Scholar]
- 8.Parry JA, Van Straaten M, Luo TD, et al. . Is there a deficit after nonoperative versus operative treatment of shortened midshaft clavicular fractures in adolescents? J Pediatr Orthop 2017;37:227-233. [DOI] [PubMed] [Google Scholar]
- 9.Rapp M, Prinz K, Kaiser MM.. Elastic stable intramedullary nailing for displaced pediatric clavicle midshaft fractures. J Pediatr Orthop 2013;33:608-613. [DOI] [PubMed] [Google Scholar]
- 10.Rang M. Children’s fractures. London: Lippincott Williams & Wilkins, 1983. [Google Scholar]
- 11.O’Neill BJ, Molloy AP, Curtin W.. Conservative management of paediatric clavicle fractures. Int J Pediatr 2011;2011:172571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Robinson CM, Court-Brown CM, McQueen MM, Wakefield AE.. Estimating the risk of nonunion following nonoperative treatment of a clavicular fracture. J Bone Joint Surg [Am] 2004;86-A:1359-1365. [DOI] [PubMed] [Google Scholar]
- 13.Liu W, Xiao J, Ji F, Xie Y, Hao Y.. Intrinsic and extrinsic risk factors for nonunion after nonoperative treatment of midshaft clavicle fractures. Orthop Traumatol Surg Res 2015;101:197-200. [DOI] [PubMed] [Google Scholar]
- 14.Ban I, Troelsen A.. Risk profile of patients developing nonunion of the clavicle and outcome of treatment—analysis of fifty five nonunions in seven hundred and twenty nine consecutive fractures. Int Orthop 2016;40:587-593. [DOI] [PubMed] [Google Scholar]
- 15.Pennock AT, Edmonds EW, Bae DS, et al.. Adolescent clavicle nonunions: potential risk factors and surgical management. J Shoulder Elbow Surg 2018;27:29-35. [DOI] [PubMed] [Google Scholar]
- 16.Wilkins RM, Johnston RM.. Ununited fractures of the clavicle. J Bone Joint Surg [Am] 1983;65-A:773-778. [PubMed] [Google Scholar]
- 17.Liberati A, Altman DG, Tetzlaff J, et al.. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009;339:b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ropars M, Bey M, Bouin M, et al.. Posttraumatic nonunion of the clavicle in a child: case report. Rev Chir Orthop Reparatrice Appar Mot 2004;90:666-669. [DOI] [PubMed] [Google Scholar]
- 19.Qureshi AA, Kuo KN.. Posttraumatic cleidoscapular synostosis following a fracture of the clavicle. A case report. J Bone Joint Surg [Am] 1999;81-A:256-258. [DOI] [PubMed] [Google Scholar]
- 20.Endrizzi DP, White RR, Babikian GM, Old AB.. Nonunion of the clavicle treated with plate fixation: A review of forty-seven consecutive cases. J Shoulder Elbow Surg 2008;17:951-953. [DOI] [PubMed] [Google Scholar]
- 21.Heyworth BE, May C, Carsen S, et al.. Outcomes of operative and non-operative treatment of adolescent mid-diaphyseal clavicle fractures. Orthop J Sports Med 2014;2:2325967114S00064. [Google Scholar]
- 22.Carsen S, Bae DS, Kocher MS, et al.. Outcomes of operatively treated nonunions and symptomatic mal-unions of adolescent diaphyseal clavicle fractures. Orthop J Sports Med 2015;3:2325967115S00078. [Google Scholar]
- 23.Wu F, Marriage N, Ismaeel A, et al.. Posttraumatic nonunion of the clavicle in a 13-year-old boy causing an arteriovenous fistula. N Am J Med Sci 2013;5:663-665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Duplantier NL, Waldron S.. Post-traumatic nonunion of the clavicle in a 4-year-old boy and the importance of vitamin D level testing. J Pediatr Orthop B 2016;25:78-80. [DOI] [PubMed] [Google Scholar]
- 25.Randsborg P-H, Fuglesang HFS, Røtterud JH, Hammer O-L, Sivertsen EA.. Long-term patient-reported outcome after fractures of the clavicle in patients aged 10 to 18 years. J Pediatr Orthop 2014;34:393-399. [DOI] [PubMed] [Google Scholar]
- 26.Smith NW, Williams N.. Post-traumatic nonunion of a clavicle fracture in a 9-year-old child. J Pediatr Orthop B 2016;25:74-77. [DOI] [PubMed] [Google Scholar]
- 27.Jain N, Peravali B, Muddu B.. Clavicle nonunion in children a report of two cases and a review of the literature. Shoulder Elbow 2009;1:40-42. [Google Scholar]
- 28.Nogi J, Heckman JD, Hakala M, Sweet DE.. Nonunion of the clavicle in a child. A case report. Clin Orthop Relat Res 1975;110:19-21. [DOI] [PubMed] [Google Scholar]
- 29.Caterini R, Farsetti P, Barletta V.. Posttraumatic nonunion of the clavicle in a 7-year-old girl. Arch Orthop Trauma Surg 1998;117:475-476. [DOI] [PubMed] [Google Scholar]
- 30.Spapens N, Degreef I, Debeer P.. Posttraumatic pseudarthrosis of the clavicle in an 8-year-old girl. J Pediatr Orthop B 2010;19:188-190. [DOI] [PubMed] [Google Scholar]
- 31.Gupta A, Singal RP, Singal R, et al.. Report of two cases of nonunion of clavicle treated with nonsurgical management. N Am J Med Sci 2010;2:544-546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pourtaheri N, Strongwater AM.. Clavicle nonunion in a 10-year-old boy. Orthopedics 2012;35:e442-443. [DOI] [PubMed] [Google Scholar]
- 33.Nowak J, Mallmin H, Larsson S.. The aetiology and epidemiology of clavicular fractures. Injury 2000;31:353-358. [DOI] [PubMed] [Google Scholar]
- 34.Postacchini F, Gumina S, De Santis P, Albo F.. Epidemiology of clavicle fractures. J Shoulder Elbow Surg 2002;11:452-456. [DOI] [PubMed] [Google Scholar]
- 35.Kubiak R, Slongo T.. Operative treatment of clavicle fractures in children: a review of 21 years. J Pediatr Orthop 2002;22:736-739. [PubMed] [Google Scholar]
- 36.Namdari S, Ganley TJ, Baldwin K, et al.. Fixation of displaced midshaft clavicle fractures in skeletally immature patients. J Pediatr Orthop 2011;31:507-511. [DOI] [PubMed] [Google Scholar]
- 37.Bae DS, Shah AS, Kalish LA, Kwon JY, Waters PM.. Shoulder motion, strength, and functional outcomes in children with established malunion of the clavicle. J Pediatr Orthop 2013;33:544-550. [DOI] [PubMed] [Google Scholar]
- 38.Schulz J, Moor M, Roocroft J, Bastrom TP, Pennock AT.. Functional and radiographic outcomes of nonoperative treatment of displaced adolescent clavicle fractures. J Bone Joint Surg [Am] 2013;95:1159-1165. [DOI] [PubMed] [Google Scholar]
- 39.Vander Have KL, Perdue AM, Caird MS, Farley FA.. Operative versus nonoperative treatment of midshaft clavicle fractures in adolescents. J Pediatr Orthop 2010;30:307-312. [DOI] [PubMed] [Google Scholar]
- 40.Fanter NJ, Kenny RM, Baker CL, Baker CL 3rd, Baker CL Jr.. Surgical treatment of clavicle fractures in the adolescent athlete. Sports Health 2015;7:137-141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mehlman CT, Yihua G, Bochang C, Zhigang W.. Operative treatment of completely displaced clavicle shaft fractures in children. J Pediatr Orthop 2009;29:851–855. [DOI] [PubMed] [Google Scholar]
- 42.Fitzwilliams D. Hereditary cranio-cleido-dysostosis. Lancet 1910;2:1466-1475. [Google Scholar]
- 43.Galvin JW, Dannenbaum JH, Grassbaugh JA, Eichinger JK.. Pseudarthrosis of the clavicle. Orthopedics 2014;37:295-350. [DOI] [PubMed] [Google Scholar]
- 44.Gibson DA, Carroll N. Congenital pseudarthrosis of the clavicle. J Bone Joint Surg [Br] 1970;52-B:629-643. [PubMed] [Google Scholar]
- 45.Owen R. Congenital pseudarthrosis of the clavicle. J Bone Joint Surg [Br] 1970;52-B:644-652. [PubMed] [Google Scholar]
- 46.Adamich JS, Howard A, Camp M.. Do all clavicle fractures in children need to be managed by orthopaedic surgeons? Pediatr Emerg Care 2017. September 18. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]


