Abstract
Purpose
Lateral condyle fractures of the humerus are common in the paediatric population, accounting for up to 20% of elbow fractures. Traditional management involves internal fixation with Kirschner (K)-wires, however, this has been associated with complications and insufficiently rigid fixation. Recently, cannulated screws have been proposed as a more stable method of fixation. While cannulated screws have been thought to allow earlier range of movement and shorten time to union, data regarding the biomechanical performance and optimal screw placement is scarce. We hypothesize that cannulated screw fixation is superior to K-wire fixation and screw placement can enhance the stability of the construct.
Methods
Paediatric humerus sawbones with Milch II fractures were fixed with one of three methods. Fractures were reduced with either a single cannulated screw either through the centre of the capitellum (oblique), or placed up the lateral column across the growth plate (lateral), or fixed with two K-wires. Fixed sawbone fractures were then mechanically tested in two directions simulating in vivo forces.
Results
The lateral screw construct had a higher maximum force to failure, higher stiffness and absorbed higher energy as compared with the K-wire fixation and oblique screw under an anterior force. When loaded from the posterior direction, only the lateral column screw was better than K-wire fixation.
Conclusions
Screw fixation is a biomechanically effective alternative to K-wire fixation, especially when placed up the lateral column of the distal humerus. Further clinical studies are required before transcapitellar screw fixation can be adopted.
Keywords: Paediatric, fracture, Milch II, Kirschner-wire, screw
Introduction
Lateral condyle fractures of the distal humerus are common in the paediatric population, accounting for up to 20% of elbow fractures, and are the most common physeal injury in this location.1-3 They are commonly classified using the Milch criteria in which injuries are characterized by a fracture line that passes from the posterolateral metaphysis of the distal humerus and extends into the apex of the trochlear.3
Milch type II fractures have historically been associated with a high incidence of early and late complications, including overgrowth of the lateral condyle, premature physeal closure, malunion, nonunion, tardive ulnar nerve palsy, physeal arrest leading to a so-called ‘fishtail deformity’, and avascular necrosis particularly of the capitellum.4-9
Traditional management of these fractures with displacement >2 mm has been internal fixation with Kirschner (K)-wires through either open or closed methods.10-17 However, K-wire fixation has been associated with a relatively high incidence of complications, including pin-site infection, skin necrosis, pain and discomfort. Further, fixation with K-wires prevents early mobilization and does not provide sufficiently rigid fixation.
Recently, the use of cannulated screw fixation has been proposed as an alternative method of fixation that may provide a more stable construct, allow earlier range of movement and shorten time to union.10,12-16,18,19 Screw fixation can utilize the metaphyseal spike and not cross the growth plate, or alternatively be placed across the growth plate as are K-wires. Data regarding the biomechanical performance of screw fixation is scarce. One recent study concluded that screw fixation provided superior stability to divergent K-wires in a synthetic bone model of Milch II fractures.20 However, we feel that the biomechanical and fracture geometry modelling had subtle but important differences to those observed in the clinical setting. Furthermore, optimal screw placement has yet to be examined. In this biomechanical sawbone study, we hypothesize that screw fixation will be biomechanically superior to wire fixation and that the ideal screw position should be placed into the lateral column of the distal humerus across the growth plate.
Materials and methods
For this study, 48 paediatric sawbone humerus models (Model #1052; Sawbones, Vashon Island, Washington) were used. A custom-made jig was used to create a reproducible fracture, with fracture osteotomies made with a 0.5 mm kerf saw for minimal material loss. Three groups of fixation were created for comparison (n = 16 for each group). Fractures were fixed with either a single 4.0 mm partially threaded cannulated screw (stainless steel, length 42 mm, 21 mm thread, #207.642; Synthes, North Ryde, Australia), a single 4.0 mm cannulated screw (stainless steel, length 50 mm, 25 mm thread, #207.750; Synthes), or a third group fixed with two 1.6 mm K-wires (Synthes). A custom-made jig was used to ensure that K-wire and screw insertion was reproduced consistently in each of the three groups.
Mechanical testing was performed using an Instron 5944 (Instron, Norwood, Massachusetts) with data collected using the accompanying BlueHill 3 software (Instron). A custom aluminium and epoxy cradle was made for clamping the model for each testing condition1. Anterior and posterior forces which replicate forces in vivo were applied to the fragment with models clamped to the respective cradles. Models were tested through five cycles, with a 1 kN load cell used to apply a force at a rate of 0.5 mm/sec to a displacement of 2 mm. Force and displacement were measured for analysis. Maximum load was calculated as the highest load recorded for each sample, stiffness was calculated as the gradient of the linear portion of the curve and energy was calculated as the area under the curve.
Clinically, following fixation of lateral condyle fractures, the elbow is immobilized in approximately 90° of flexion. The two main forces acting on the fracture in this position are either an external rotation/posterior translational load exerted by the radial head or an internal rotation/anterior translation force from the common extensor muscles. A recent biomechanical study by Bloom et al21 also demonstrated that Milch II fractures are most unstable when loaded in torsion, supporting the hypothesis that this is a pathway leading to failure of fixation. Thus, fixed fracture models were each tested using anterior and posterior forces (i.e. perpendicular to the long axis of the humerus). To represent these hypothesized modes of failure, the humeri were tested in both a posterior direction, with the force centered over the capitellum, and an anterior direction, with the force directed over the lateral supracondylar ridge.
Statistical analysis was conducted using GraphPad Prism (Version 6; GraphPad Software, La Jolla, California). Maximum force, stiffness and energy were recorded and averaged for each sample. Data distribution for each group was tested for normality using the D’Agostino and Pearson omnibus normality test. Following this, data was determined to be parametric and was analyzed by analysis of variance with post hoc analysis using Tukey’s multiple comparisons test.
Results
The Milch II lateral condyle fractures clinically observed at the Children’s Hospital at Westmead, NSW, Australia were found to conventionally feature a fracture line through the physis with sagittal and oblique components. A cutting jig was built that would allow this fracture pattern to be recreated in all the sawbone humeri. Cut sawbones were anatomically reduced and held with either a single 42 mm long partially threaded screw through the centre of the capitellum (oblique group), a single 50 mm long screw length placed up the lateral column (lateral group) or fixed with two 1.6 mm K-wires with 25° divergence placed bicortically (Fig. 2). Screw placement in the lateral column group was placed to avoid the capitellar ossific nucleus and olecranon fossa with a starting point just posterior to the mid-sagittal plane of the humerus to allow an uninterrupted passage, while the screw in the oblique group passed at approximately 45° in the coronal plane on a trajectory through the capitellar ossific nucleus and olecranon fossa but not protruding into it. A custom jig was created that was able to insert the screw and K-wire fixation constructs reproducibly within groups. A total of 48 synthetic humeri models were included for the final biomechanical analysis. These were evenly distributed into three groups containing 16 specimens.
Fig. 2.
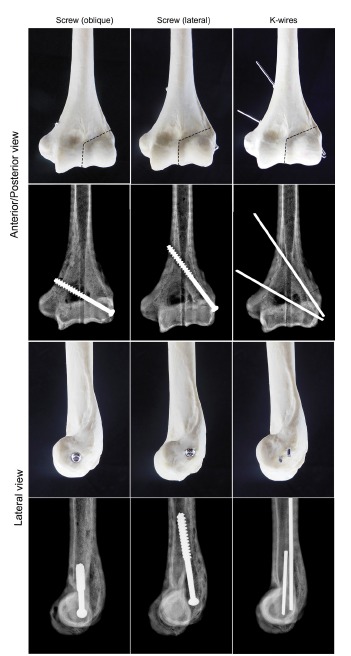
Photographs and radiographs of the various fixation methods of the lateral condyle fracture model in the humerus. In the photographs, the black dotted line represents the fracture line.
Fig. 1.
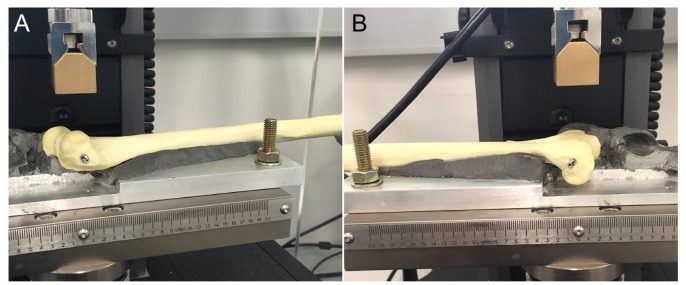
The mechanical testing jig cradle to support the compression testing of the fracture fragment in (a) the anterior direction and (b) the posterior position.
To examine the effects of external rotation on the fracture fragment, the reduced sawbone fragments were mechanically tested perpendicularly from the posterior direction (Fig. 3). In this loading direction, the oblique and lateral column screw positions had a higher maximum load than the K-wire group (130.9 N and 119.8 N versus 95.3 N; p < 0.01). The two constructs with differing screw placements were stiffer than fixation with K-wires (1028.2 N/mm and 956.5 N/mm versus 558.9 N/mm; p < 0.01). The energy absorbed in the oblique screw group was higher than lateral screw and K-wire groups (0.108 J versus 0.090 J and 0.075 J; p < 0.05 and p < 0.01, respectively).
Fig. 3.
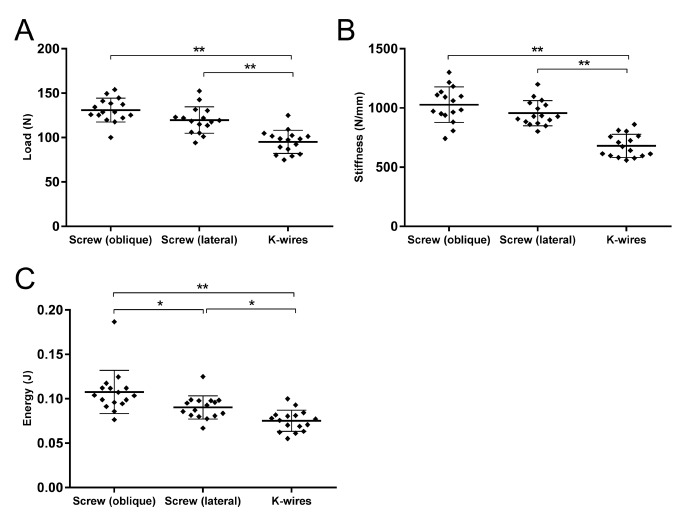
The maximum load (a), stiffness (b) and energy absorbed (c) of humeral lateral condyle fractures loaded posteriorly to represent external rotation (*, p < 0.05; **, p < 0.01) (K-wire, Kirschner-wire).
The fracture fragments were also loaded in an anterior direction, which was conducted to simulate internal rotation (Fig. 4). The maximum load achieved in this direction was significantly higher in the lateral screw position than in the oblique screw or K-wire fixation methods (104.3 N versus 59.7 N and 66.2 N; p < 0.01). This pattern was also seen in the stiffness (1193.9 N/mm versus 870.5 N/mm and 643.9 N/mm) and absorbed energy parameters (0.0554 J versus 0.0340 J and 0.0385 J), where the lateral screw fixation was superior to the other methods (p < 0.01).
Fig. 4.
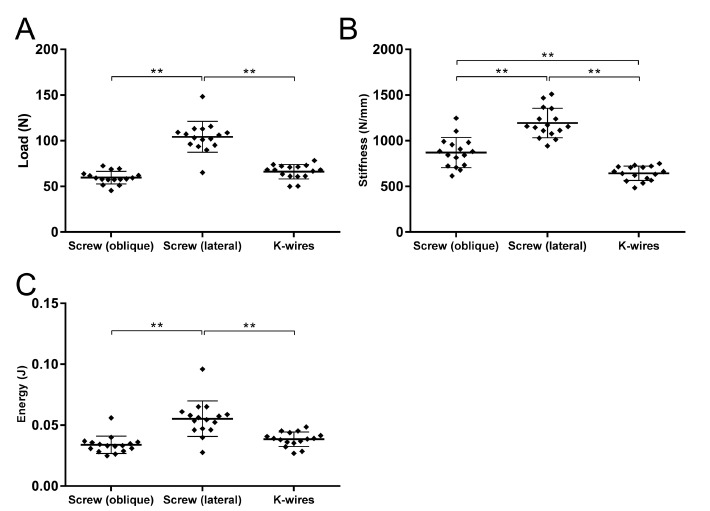
The maximum load (a), stiffness (b) and energy absorbed (c) of humeral lateral condyle fractures loaded anteriorly to represent internal rotation (**, p < 0.01) (K-wire, Kirschner-wire).
In both loading directions, the K-wire fixation was outperformed by one or both of the screw fixation methods. In the posterior direction however, the most stable fixation was achieved by the oblique screw position. However, during testing it was also noted that there was minor fragment displacement in the screw fixation groups that was a combination of rotation and translation of the fragment.
Discussion
Management of displaced paediatric lateral condyle fractures continues to challenge the orthopaedic surgeon. While K-wire fixation has previously been the standard treatment for displaced lateral condyle fractures, the use of screw fixation has grown in popularity. Recent studies have reported faster union time in lateral condyle fractures that had undergone screw fixation when compared with K-wires.18 This is further clinical evidence for the use of screw fixation, as the significant growth disturbance cubitus varus is thought to be directly proportional to fracture consolidation time.22
Multiple studies have examined the use of screw fixation in the lateral condyle clinically.10,13,15,18,19,23,24 However, little evidence is available regarding the optimal position of screw placement for lateral condyle fractures. Screws have been described as being placed through the centre or periphery of the capitellar physis, or through the metaphyseal portion of the fracture. We have found no data on results regarding screw position and currently the final decision rests with the preference of the treating surgeon.
Concerns regarding the risk of possible physeal arrest and angular deformity following screw fixation of Milch II lateral condyle fractures have not been conclusively answered in the literature. Three studies18-20,22 comparing K-wire with lag screw fixation of lateral condyle fractures did not report significant differences in physeal arrest or rates of avascular necrosis (AVN) between groups even up to ten-year follow-up.22 However, in the study by Li and Xu19 three out of four capitellar screws developed cubitus valgus without AVN, suggesting this position may create an impairment of growth on the capitellar physis. Several other studies have reported variable rates of AVN varying from 0% to 11%,10,13,15,18,19,21 however interpretation of this data remains hampered by the lack of long-term follow-up.
There is little evidence available regarding the biomechanical strength of screw fixation of lateral condyle fractures. One recent biomechanical study of paediatric lateral condyle fractures (Milch type II) concluded that single screw fixation provided increased stability of the construct when compared with 60° divergent K-wires when tested axially.20 The authors are not aware of any studies investigating an optimal screw placement for Milch II fractures.
This study demonstrates that fixation stability in lateral condyle fractures is dependent on interplay of fracture geometry, mode of fixation and position of components. Observation during testing indicated that displacement was a combination of rotation and translation of the fragment, both of which cause displacement of the joint surface. We postulate that whilst the screws resisted translation better than wires, the fragment rotated around the single screw more readily when subjected to the offset force. Placing the screw up the lateral column allowed a longer thread to be used, improving stiffness in translation and also decreasing the moment arm between the force through the lateral supracondylar ridge and the screw. Concordantly, this position also increased the moment arm to the centre of the capitellum, decreasing resistance to rotation in posteriorly directed capitellar force. Accordingly, the more oblique, shorter screw was less stiff in translation, resisted rotation from the capitellar force better and was more vulnerable to fragment rotation under a posterior force through the supracondylar ridge.
In comparison with other studies reported in the literature, our model had two important differences. Firstly, the fracture model we produced consisted of two distinct planes comprising of an oblique metaphyseal line and a vertical intra-articular component and varies from the commonly used classification systems in the literature. The current variety of classification systems of lateral condyle fractures do not focus on the detail of the fracture geometry, with the attention being focused on displacement patterns or the intra-articular location of the fracture line. For example, the original Milch classification is dependent on the location of fracture line in the articular surface, and the integrity of what was described as the lateral trochlear wall.1 This is often simplified to Milch I fractures being those that have a fracture lateral to the trochlear groove and no elbow dislocation, and Milch II as those that have a fracture running medial to the trochlear groove. However, in our experience, intra-operative arthrograms typically demonstrate a fracture that consists of an oblique metaphyseal component and a vertical intra-articular line and has previously been described by Weiss and colleagues.25 We feel this is particularly important as fracture geometry alters fragment stability especially when under compression with screws and therefore is an important feature to replicate in biomechanical modelling. To our knowledge lateral condyle fractures have not been modelled in this way in biomechanical testing.
Secondly, we believe that the loading points on the fracture fragments used in this study are reflective of those seen when the child is immobilized or in a post-operative sling. Milch described three main mechanisms of lateral condyle fractures, either an abduction/compression (cubitus valgus) or adduction/tension avulsion type (cubitus varus) force on the extended elbow perpendicular to the long axis of the humerus, or a force directed along the longitudinal axis of the humerus on a partially flexed elbow.3 In our model, sawbone humeri were tested with either a posterior force directed through the centre of the capitellum, or an anterior force centred over the lateral supracondylar ridge to mimic the pull of the common extensor muscle. Both forces replicated a torsional stress on the distal humerus and this has previously been shown to be the most vulnerable plane for lateral condyle fractures fixed with K-wires.21 A previous biomechanical study comparing K-wire fixation with screws in a synthetic model was done by applying a force directly through the pin or screw that was holding the fragment.20 In our model the forces were applied to the actual fragment itself and not the implant as we felt this more accurately reflected in vivo conditions.
Our study has limitations that are inherent of those associated with biomechanical testing. The model and testing conditions do not account for individual variations in bone age, size, quality and variation amongst fracture patterns. Fracture fixation and testing was also performed without the influence of surrounding soft tissues which are likely to play a role both in the stability of the reduction as well as the mode of failure of fixation. Significantly, heterogeneity of the paediatric distal humerus with age-related composition of cartilage and ossification centres was not modelled. This limits applicability of the model with regards to fixation strength, pull-out strength and fracture site mechanics. As there was a rotational component to displacement, the end point of testing of a 2-mm displacement at the site of force application does not necessarily correlate directly with the same displacement at the articular surface. Thirdly, force was applied to the capitellum using a flat testing plate surface rather than a more congruent surface replicating the radial head. While the centre of force is unlikely to have changed, it is conceivable that the concavity of the radial head may have resisted rotation of the fragment better and better replicated in vivo conditions. Finally, our modelling did not allow for variation in fracture geometry and we acknowledge that in some circumstances the fracture geometry may not permit placement of a lateral column screw due to a short metaphyseal spike. We believe that lateral condyle fractures have a spectrum of morphologies potentially changing the behaviour of the fracture, however we have based our modelling on what colleagues have previously described25 and what is representative of the injuries presenting to our institution.
In summary, this study demonstrates in a synthetic paediatric bone model the biomechanical advantage of using a laterally positioned screw for the fixation of Milch II lateral condyle fractures in comparison with either an obliquely positioned screw or two divergent K-wires. Further research is required to examine if these findings are applicable to clinical practice and to assess if the use of screw fixation across the physis is associated with subsequent growth disturbance.
Compliance with Ethical Standards
Funding Statement
This project was awarded a grant from the Australian Orthopaedic Association Research Foundation. The grant covered the costs of the materials used in this study only.
Ethical Statement
Ethical approval: This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent: Not required.
ICMJE Conflict of interest statement D. G. Little reports non-financial support from Novartis, grants from Amgen, grants from Celgene, grants from N8 Medical, personal fees from Orthopediatrics, outside the submitted work. All other authors declare no conflicts of interest.
References
- 1.Flynn JC, Richards JF Jr, Saltzman RI. Prevention and treatment of non-union of slightly displaced fractures of the lateral humeral condyle in children. An end-result study. J Bone Joint Surg [Am] 1975;57-A:1087-1092. [PubMed] [Google Scholar]
- 2.Landin LA. Fracture patterns in children. Analysis of 8,682 fractures with special reference to incidence, etiology and secular changes in a Swedish urban population 1950-1979. Acta Orthop Scand Suppl 1983;202:1-109. [PubMed] [Google Scholar]
- 3.Milch H. Fractures and Fracture Dislocations of the Humeral Condyles. J Trauma 1964;4:592-607. [DOI] [PubMed] [Google Scholar]
- 4.Beaty JH. Fractures of the lateral humeral condyle are the second most frequent elbow fracture in children. J Orthop Trauma 2010;24:438. [DOI] [PubMed] [Google Scholar]
- 5.Cates RA, Mehlman CT. Growth arrest of the capitellar physis after displaced lateral condyle fractures in children. J Pediatr Orthop 2012;32:e57-e62. [DOI] [PubMed] [Google Scholar]
- 6.Launay F, Leet AI, Jacopin S, et al. Lateral humeral condyle fractures in children: a comparison of two approaches to treatment. J Pediatr Orthop 2004;24:385-391. [PubMed] [Google Scholar]
- 7.Morrissy RT, Wilkins KE. Deformity following distal humeral fracture in childhood. J Bone Joint Surg [Am] 1984;66-A:557-562. [PubMed] [Google Scholar]
- 8.Tejwani N, Phillips D, Goldstein RY. Management of lateral humeral condylar fracture in children. J Am Acad Orthop Surg 2011;19:350-358. [DOI] [PubMed] [Google Scholar]
- 9.Wadsworth TG. Injuries of the capitular (lateral humeral condylar) epiphysis. Clin Orthop Relat Res 1972;85:127-142. [DOI] [PubMed] [Google Scholar]
- 10.Baharuddin M, Sharaf I. Screw osteosynthesis in the treatment of fracture lateral humeral condyle in children. Med J Malaysia 2001;56 Suppl D:45-47. [PubMed] [Google Scholar]
- 11.Cardona JI, Riddle E, Kumar SJ. Displaced fractures of the lateral humeral condyle: criteria for implant removal. J Pediatr Orthop 2002;22:194-197. [PubMed] [Google Scholar]
- 12.Chou PH, Feng CK, Chiu FY, Chen TH. Isometric measurement of wrist-extensor power following surgical treatment of displaced lateral condylar fracture of the humerus in children. Int Orthop 2008;32:679-684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Conner AN, Smith MG. Displaced fractures of the lateral humeral condyle in children. J Bone Joint Surg [Br] 1970;52-B:460-464. [PubMed] [Google Scholar]
- 14.Saraf SK, Khare GN. Late presentation of fractures of the lateral condyle of the humerus in children. Indian J Orthop 2011;45:39-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sharma JC, Arora A, Mathur NC, et al. Lateral condylar fractures of the humerus in children: fixation with partially threaded 4.0-mm AO cancellous screws. J Trauma 1995;39:1129-1133. [DOI] [PubMed] [Google Scholar]
- 16.Sulaiman AR, Munajat I, Mohd EF. A modified surgical technique for neglected fracture of lateral humeral condyle in children. J Pediatr Orthop B 2011;20:366-371. [DOI] [PubMed] [Google Scholar]
- 17.Thomas DP, Howard AW, Cole WG, Hedden DM. Three weeks of Kirschner wire fixation for displaced lateral condylar fractures of the humerus in children. J Pediatr Orthop 2001;21:565-569. [PubMed] [Google Scholar]
- 18.Gilbert SR, MacLennan PA, Schlitz RS, Estes AR. Screw versus pin fixation with open reduction of pediatric lateral condyle fractures. J Pediatr Orthop B 2016;25:148-152. [DOI] [PubMed] [Google Scholar]
- 19.Li WC, Xu RJ. Comparison of Kirschner wires and AO cannulated screw internal fixation for displaced lateral humeral condyle fracture in children. Int Orthop 2012;36:1261-1266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schlitz RS, Schwertz JM, Eberhardt AW, Gilbert SR. Biomechanical analysis of screws versus K-wires for lateral humeral condyle fractures. J Pediatr Orthop 2015;35:e93-e97. [DOI] [PubMed] [Google Scholar]
- 21.Bloom T, Chen LY, Sabharwal S. Biomechanical analysis of lateral humeral condyle fracture pinning. J Pediatr Orthop 2011;31:130-137. [DOI] [PubMed] [Google Scholar]
- 22.Hasler CC, von Laer L. Prevention of growth disturbances after fractures of the lateral humeral condyle in children. J Pediatr Orthop B 2001;10:123-130. [PubMed] [Google Scholar]
- 23.Loke WP, Shukur MH, Yeap JK. Screw osteosynthesis of displaced lateral humeral condyle fractures in children: a mid-term review. Med J Malaysia 2006;61 Suppl A:40-44. [PubMed] [Google Scholar]
- 24.Shirley E, Anderson M, Neal K, Mazur J. Screw fixation of lateral condyle fractures: results of treatment. J Pediatr Orthop 2015;35:821-824. [DOI] [PubMed] [Google Scholar]
- 25.Weiss JM, Graves S, Yang S, et al. A new classification system predictive of complications in surgically treated pediatric humeral lateral condyle fractures. J Pediatr Orthop 2009;29:602-605. [DOI] [PubMed] [Google Scholar]


