Abstract
Purpose
There are multiple skeletal maturity grading systems, but none of them utilizes the phalanges of the foot. To minimize radiation, it would be ideal if one could assess the skeletal maturity of a foot based on bones seen on routine foot radiographs, if guided growth is being considered as a treatment option. We developed a system that correlates changes of the appearance of the foot phalanges to peak height velocity (PHV) and the recently described calcaneal apophyseal ossification grading system.
Methods
We selected 94 children from the Bolton-Brush study, each with consecutive radiographs from age ten to 15 years old. Using the anteroposterior view, we analyzed the ossification patterns of the phalanges and developed a six-stage system. We then determined the PHV for each subject and defined its relationship with our system. Our system was then compared with the previously established calcaneal system.
Results
We calculated an Intraclass correlation coefficient (ICC) range of 0.957 to 0.985 with a mean of 0.975 and interclass reliability coefficient of 0.993 indicating that this method is reliable and consistent. Our system showed no significant difference between gender with respect to PHV, which makes it a reliable surrogate for determining bone age in paediatric and adolescent patients.
Conclusions
Our system has a strong association with the calcaneal system. It is a simple six-stage system that is reliable and correlated more strongly with PHV than chronological age. The system requires knowledge of the ossification markers used for each stage but is easily used in a clinical setting.
Keywords: Peak height velocity, foot, growth development, calcaneal, hallux valgus
Introduction
Skeletal maturity staging is used to determine a child’s current growth velocity and growth potential. Many paediatric diseases including growth, endocrine and chromosomal disorders depend on skeletal maturity systems to assess whether bone age and chronological age are concordant.1 If a discrepancy is seen, an underlying disorder may be suggested. While assessment of bone age is widely utilized by many paediatric physicians, current systems remain complex and traditionally involve comparing the patient’s radiographs to an atlas composed of standard images.2-4
A maturation system using radiographic imaging of the foot and ankle was created by Hoerr et al.2 Like its predecessor atlases of the hand and knee, the atlas made use of osseous landmarks as bone age indicators.2-4 A recent evaluation of the Hoerr atlas found a strong correlation between estimated ‘bone age’ and chronological age.5 However, this atlas was created before the concept of peak height velocity (PHV) was understood and does not relate skeletal maturity to PHV.
A maturity system of the foot that accounts for skeletal maturity relative to PHV would be a valuable tool for ascertaining skeletal maturity. For example, in determining treatment options for hallux valgus, hemiepiphysiodesis requires the patient to be skeletally immature, and osteotomies are typically performed after the patient is skeletally mature. If a maturity system could determine the amount of time before and after PHV is reached, it would be helpful in evaluating the timing of epiphysiodesis.6-8 Greene et al6 established normative values on growth of the first metatarsal but did not correlate their findings to PHV. A six-stage system of calcaneal apophyseal ossification, as previously described, allows for the identification of the period of growth before and after PHV and is highly reliable, but requires lateral views of the foot.9
In our study, given that a standard anteroposterior view is routinely used for evaluating the severity of foot pathologies, we explored the utility of the phalanges of the foot for assessing skeletal age. To avoid additional radiation exposure, our purpose was to generate a skeletal maturity system using existing radiographic images of foot pathologies and measure the maturity of the phalanges relative to PHV, which is a useful marker in timing growth and development.6-8
Materials and methods
The children in this study are the same as those used for the Greulich and Pyle atlas of the hand and the calcaneal apophyseal ossification system, in which serial anteroposterior and lateral foot radiographs of 94 children (49 female, 45 male) were followed for over a decade with consecutive radiographs, made at least yearly from age ten to 15 years, which is the age range most associated with PHV. These radiographs were part of the Bolton-Brush collection in Cleveland, Ohio, collected by Dr. T. Wingate Todd from 1929 to 1942. The Brush Inquiry consists of 4435 children from above average economic and educational status. Most children were white (92.2%) and the remainder were mostly black (7.7%).3,10-11
We had 732 anteroposterior and 738 lateral radiographs available for review. We evaluated all anteroposterior radiographs that clearly demonstrated all of the epiphyses of the proximal phalanges of the second through the fifth toes and the distal phalanx of the first toe which also had a matching lateral radiograph taken the same day that demonstrated the entire calcaneal apophysis. There were 728 matching sets of radiographs in total.
Using the anteroposterior view, we examined the degree of ossification and fusion of the digital proximal epiphyses of the proximal phalanges and the distal phalanx of the first ray. The lateral radiograph of the foot taken at the same session as the anteroposterior view was graded using the previously described calcaneal system.9 All radiographs were reviewed by the lead author (MRG). In all, 100 randomly selected sets of radiographs were evaluated by a board certified paediatric orthopedic surgeon (DRC), a resident with considerable experience in developing and using bone maturity assessment tools (ADN) and another resident without such experience (AMN). These three authors first graded 100 randomly selected sets of radiographs, then had a consensus building session led by MRG, then graded another 100 radiographs. Intraclass correlation coefficient (ICC) (two-way mixed model and absolute agreement) and interclass reliability coefficient were calculated using IBM SPSS (IBM, Chicago, Illinois) and all other statistics and graphs were generated using Excel 2016 (Microsoft, Redmond, Washington).
The subjects in this study had their heights taken each time radiographs were obtained. The PHV was calculated using these serial height measurements after the approach of Tanner and Davies14 using a cubic spline to determine the maximum velocity which was defined as PHV. The subject’s age for this value was used for the point in time of PHV.
Results
The ossification of the proximal phalanges and the distal phalanx of the great toe occurs in an orderly sequence. The ossification centre of the distal epiphysis of the great toe is first seen at 14 and 18 months of age for female and male patients, respectively. By 18 and 24 months, the ossification centres of all phalanges in female and male patients can be seen.2
The orderly ossification and fusion of the foot phalanges was divided into six stages, shown in Fig. 1. In metaphysis, epiphysis hook skeletal assessment (MEKKA) 0, at least one proximal phalanx has an epiphysis that is not as wide as its corresponding metaphysis. This finding is often most noticeable for the fifth proximal phalanx. MEKKA 1 is characterized by all digital proximal epiphyses of the proximal phalanges being as wide or wider than the metaphysis, or ‘covered’, as is the proximal epiphysis of the distal phalanx of the first digit. The epiphyseal plates of proximal phalanges 2 to 5 are concave in shape. MEKKA 2 is marked by the formation of a small, medial epiphyseal ‘hook’ over the metaphysis of the distal phalanx of the first ray. Presence of the ‘hook’ is diagnostic of stage 2, even if other criteria of stages 0 and 1 are not met. MEKKA 3 is marked by the initiation of fusion of the proximal epiphysis of the second, third and/or fourth proximal phalanges. Fusion typically starts in the centre of the physis. It is still possible to see the epiphyseal ‘hook’ on the first ray. In MEKKA 4, fusion of the proximal epiphysis of the first and/or fifth proximal phalanx is seen. Again, it is still possible to see the epiphyseal ‘hook’ on the first digit. In MEKKA 5, fusion of the digital proximal epiphysis and the proximal epiphysis of the distal phalanx of the first digit are complete. The complete ossification of the growth plate is represented by cortical continuity with or without the presence of a residual white physeal scar.
Fig. 1.
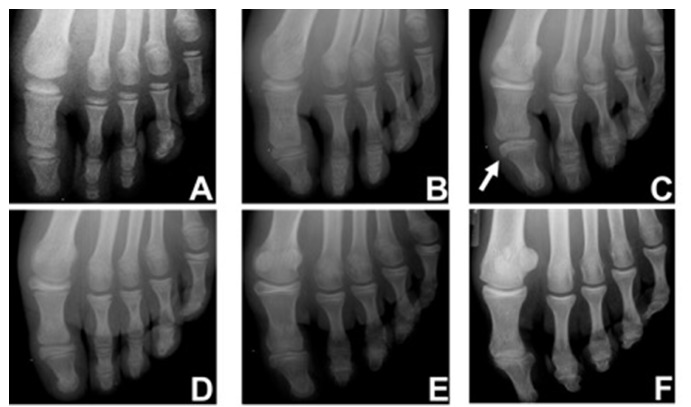
The metaphysis, epiphysis hook skeletal assessment (MEKKA) of the phalanges; (a) MEKKA 0: not all digital epiphyses of the proximal phalanges are covered; (b) MEKKA 1: all digital epiphyses of the proximal phalanges and the proximal epiphysis of the distal phalanx of the first digit are covered. It is ‘covered’ when the epiphysis is as wide or wider than the metaphysis. It can also be noted that the epiphyseal plate of the proximal phalanges 2 to 5 are concave; (c) MEKKA 2: capping of the metaphysis of the first digit by the epiphysis as represented by a small, medial epiphyseal ‘hook’ over the metaphysis; (d) MEKKA 3: initiation of fusion of the proximal epiphyses of the second, third and/or fourth proximal phalanges; (e) MEKKA 4: initiation of fusion of the proximal epiphyses of the first and/or fifth proximal phalanges; (f) MEKKA 5: complete ossification of all digital epiphyses of the proximal phalanges and the proximal epiphysis of the distal phalanx of the first digit.
Table 1 shows the years before the PHV and the range of ages relative to PHV for each MEKKA stage. The presence of the ‘hook’ of MEKKA 2 appears at a mean age of 1.79 years (4.55 to 0.31) before PHV. Fusion of the proximal epiphysis of digits 2, 3 and/or 4 is initiated in MEKKA 3 at a mean age of 0.59 years (3.50 to 1.05) before PHV, while complete fusion of all digital proximal epiphysis and the proximal epiphysis of the big toe occurs at a mean age of 3.90 years (1.55 to 6.89) after PHV.
Table 1.
Ossification of the proximal phalanges with respect to peak height velocity (PHV)
| Timing relative to PHV (yrs) | ||||
|---|---|---|---|---|
| Stage | Samples (n) | Mean | 95% confidence interval | Range |
| 0 | 102 | -5.00 | -5.28 to -4.72 | -8.55 to -1.69 |
| 1 | 67 | -2.61 | -2.88 to -2.33 | -5.15 to -0.57 |
| 2 | 87 | -1.79 | -2.00 to -1.58 | -4.55 to 0.31 |
| 3 | 79 | -0.59 | -0.79 to 0.40 | -3.50 to 1.05 |
| 4 | 179 | 0.72 | 0.57 to 0.86 | -2.18 to 2.93 |
| 5* | 35 | 3.90 | 3.43 to 4.36 | 1.55 to 6.89 |
first appearance of stage 5; there were 179 metaphysis, epiphysis hook skeletal assessment stage 5 radiographs that were made after the first appearance of stage 5 and were not used for calculations of the first appearance of stage 5
Figure 2 shows a comparison of the MEKKA and calcaneal system with respect to PHV. PHV is achieved in MEKKA 3 and between calcaneal stages 3 and 4. There was an overlap in the initiation of fusion between the two stages (a total of 33 children that are both MEKKA 3 and calcaneal stage 4). The timing of the MEKKA stages with respect to the PHV between gender is not statistically different as seen in Table 2. The chronological age for each MEKKA stage is shown in Table 3.
Fig. 2.
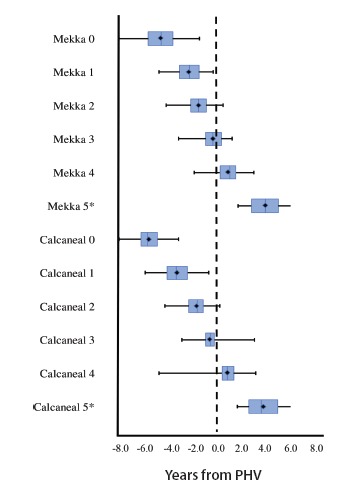
Comparison of the metaphysis, epiphysis hook skeletal assessment (MEKKA) and calcaneal system with respect to peak height velocity (PHV). A box-and-whisker plot shows the age with respect to PHV for the MEKKA and calcaneal stages. The black lines represent the range for each stage, while the blue box represents the middle 50% of the data. The blue line inside each box represents the median, while the black diamond in the middle represents the mean. Negative numbers represent years before PHV and positive numbers represent years after. Both MEKKA and calcaneal 5* represent the first appearance of complete fusion.
Table 2.
Ossification of the proximal phalanges with respect to peak height velocity (PHV) by gender
| Timing relative to PHV (yrs) | ||||
|---|---|---|---|---|
| Stage | Samples (n) | Mean | 95% confidence interval | Range |
| Female patients | ||||
| 0 | 56 | -5.18 | -5.52 to -4.84 | -7.57 to -2.23 |
| 1 | 40 | -2.82 | -3.18 to -2.46 | -5.15 to -0.61 |
| 2 | 48 | -1.79 | -2.06 to -1.51 | -3.78 to 0.04 |
| 3 | 39 | -0.51 | -0.78 to -0.23 | -1.99 to 1.05 |
| 4 | 88 | 0.71 | 0.50 to 0.93 | -2.18 to 2.93 |
| 5* | 26 | 4.10 | 3.53 to 4.67 | 1.55 to 6.89 |
| Male patients | ||||
| 0 | 46 | -4.78 | -5.25 to -4.31 | -8.55 to -1.69 |
| 1 | 27 | -2.29 | -2.71 to -1.87 | -4.66 to -0.57 |
| 2 | 39 | -1.80 | -2.12 to -1.48 | -4.55 to 0.31 |
| 3 | 40 | -0.67 | -0.96 to -0.39 | -3.50 to 0.96 |
| 4 | 91 | 0.72 | 0.52 to 0.92 | -1.76 to 2.43 |
| 5* | 9 | 3.32 | 2.66 to 3.98 | 2.12 to 5.08 |
first appearance of stage 5; there were 179 metaphysis, epiphysis hook skeletal assessment stage 5 radiographs that were made after the first appearance of stage 5 and were not used for calculations of the first appearance of stage 5
Table 3.
Ossification of the proximal phalanges with respect to chronological age by gender
| Age (yrs) | ||||
|---|---|---|---|---|
| Stage | Samples (n) | Mean | 95% confidence interval | Range |
| Female patients | ||||
| 0 | 56 | 5.87 | 5.46 to 6.28 | 3.10 to 10.0 |
| 1 | 40 | 8.28 | 7.8 to 8.76 | 5.96 to 12.0 |
| 2 | 48 | 9.55 | 9.24 to 9.86 | 7.78 to 12.3 |
| 3 | 39 | 10.8 | 10.5 to 11.1 | 9.0 to 13.0 |
| 4 | 88 | 12.1 | 11.8 to 12.3 | 9.0 to 15.2 |
| 5* | 26 | 15.2 | 14.6 to 15.8 | 11.9 to 18.0 |
| Male patients | ||||
| 0 | 46 | 8.24 | 7.74 to 8.74 | 3.78 to 12.01 |
| 1 | 27 | 10.9 | 10.5 to 11.3 | 8.01 to 13.01 |
| 2 | 39 | 11.7 | 11.3 to 12.0 | 9.62 to 14.0 |
| 3 | 40 | 12.6 | 12.2 to 12.9 | 9.15 to 14.1 |
| 4 | 91 | 13.9 | 13.7 to 14.1 | 10.9 to 17.0 |
| 5* | 9 | 16.5 | 15.8 to 17.2 | 15.0 to 18.1 |
first appearance of stage 5; there were 179 metaphysis, epiphysis hook skeletal assessment stage 5 radiographs that were made after the first appearance of stage 5 and were not used for calculations of the first appearance of stage 5
The trend, in general, between the mean and median and first and third quartile seems to overlap which suggests a normal distribution of the data. There is a distribution of MEKKA stages corresponding to specific calcaneal scores and vice versa as shown in Fig. 3.
Fig. 3.
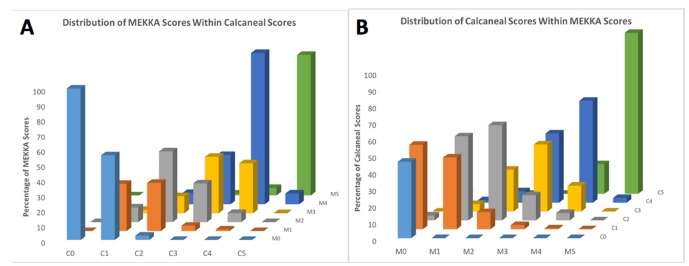
Distribution of calcaneal scores within metaphysis, epiphysis hook skeletal assessment scores (a) and vice versa (b).
The MEKKA and calcaneal stages were combined and for each combined stage with a sample size more than five, the mean number of years before or after PHV were plotted (Table 4 and Fig. 4).
Table 4.
Combined metaphysis, epiphysis hook skeletal assessment (MEKKA)/calcaneal stage: years from peak height velocity (PHV)
| Timing to relative PHV (yrs) | |||||
|---|---|---|---|---|---|
| Stage | n | Mean | sd | 95% confidence interval | Range |
| M0/C0 | 47 | -6.0 | 1.1 | -6.3 to -5.7 | -8.5 to -3.5 |
| M0/C1 | 52 | -4.2 | 1.1 | -4.5 to -3.9 | -6.3 to -1.9 |
| M0/C2* | 3 | -3.2 | 1.5 | -4.8 to -1.5 | -4.6 to -1.7 |
| M1/C1 | 29 | -3.1 | 1.1 | -3.5 to -2.7 | -5.1 to -0.9 |
| M1/C2 | 34 | -2.2 | 0.9 | -2.5 to -1.9 | -3.8 to -0.6 |
| M1/C3* | 3 | -1.1 | 0.6 | -1.82 to -0.5 | -1.8 to -0.6 |
| M1/C4* | 1 | -2.2 | - | - | - |
| M2/C1* | 9 | -2.8 | 0.5 | -3.1 to -2.4 | -3.6 to -1.8 |
| M2/C2 | 50 | -2.0 | 0.9 | -2.2 to -1.7 | -4.6 to 0.0 |
| M2/C3 | 22 | -1.4 | 0.8 | -1.7 to -1.0 | -3.2 to 0.0 |
| M2/C4* | 6 | -0.4 | 0.7 | -1.0 to 0.1 | -1.8 to 0.3 |
| M3/C2* | 12 | -1.5 | 0.4 | -1.7 to -1.3 | -1.9 to -0.6 |
| M3/C3 | 32 | -0.8 | 0.6 | -1.0 to -0.6 | -2.2 to 0.1 |
| M3/C4 | 33 | 0.1 | 0.6 | -0.1 to 0.3 | -1.5 to 1.1 |
| M4/C1* | 1 | -1.8 | - | - | - |
| M4/C2* | 8 | -0.9 | 0.3 | -1.1 to -0.6 | -1.2 to -0.4 |
| M4/C3 | 28 | -0.5 | 0.6 | -0.8 to -0.3 | -2.2 to 0.9 |
| M4/C4 | 110 | 0.9 | 0.7 | 0.7 to 1.0 | -1.0 to 2.2 |
| M4/C5 | 32 | 1.8 | 0.4 | 1.6 to 1.9 | 1.1 to 2.9 |
| M5/C3* | 1 | 3.0 | - | - | - |
| M5/C4* | 5 | 2.2 | 0.7 | 1.6 to 2.8 | 1.5 to 3.0 |
| M5/C5 | 206 | 3.5 | 1.1 | 3.3 to 3.7 | 1.6 to 7.0 |
combined stages had a sample size under 20 and were excluded from Figure 4; ‘M’ and ‘C’ followed by the stage number represent the MEKKA and calcaneal stages, respectively; four samples did not have a calcaneal stage and were excluded from this table
Fig. 4.
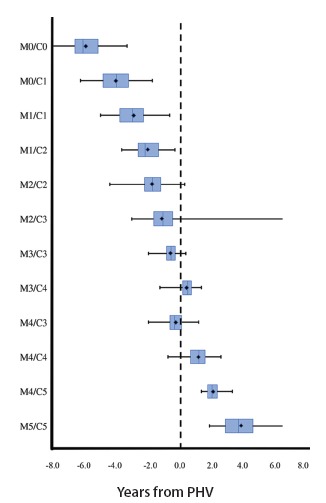
A box-and-whisker plot of the combined metaphysis, epiphysis hook skeletal assessment (MEKKA) (‘M’) and calcaneal (‘C’) stages show the years before (negative) and after (positive) the peak height velocity (PHV). The black lines represent the range for each stage, while the blue box represents the middle 50% of the data. The line inside each box represents the median, while the black diamond in the middle represents the mean. M0/C0 represents immaturity up to 8+ years before PHV while M5/C5 represents full maturity of up to 8+ years after PHV. Combined stages with sample size of < 20 were excluded from the graph but are shown in Table 4.
An ICC range of 0.957 to 0.985 with a mean of 0.975 and interclass reliability coefficient of 0.993 were calculated.
Discussion
Many methods for assessment of skeletal maturity have been developed. The most common system in use today remains the hand-wrist skeletal ages of Greulich and Pyle.3 However, it has been shown to yield a large inter-observer error12 and has been problematic when applied to different ethnic groups.13 Several attempts have been made to simplify the radiographic assessment of skeletal age in paediatric and adolescent patients such as the systems derived by Sanders et al and Heyworth et al.22-24 The Sanders method, derived from the Tanner-Whitehouse-III and Greulich and Pyle systems, uses ossification of the phalanges of the hand and wrist radiographs to define the skeletal maturity stage, which is then correlated with a predictive model of scoliosis curve progression.22
An atlas of skeletal development of the foot was developed by Hoerr et al using the same Bolton-Brush study cohort as Greulich and Pyle.2 Both atlases were created before the concept of PHV was described by Tanner.14,15 The Hoerr atlas established standard plates outlining the timing of appearance and patterns of ossification centers of the foot. Hoerr et al2 described the proximal phalanges of the second, third and fourth digits as the first to fuse, similar to the findings in our study. They also found the epiphyseal-diaphyseal fusion to be complete by age 17.5 years in male and 15.0 years in female patients. Similarly, our data showed a mean age of 16.5 years (15.0 to 18.1) in male and 15.2 years (11.9 to 18.0) in female patients for complete fusion. We also showed that regardless of gender, ossification of the proximal phalanges and distal phalanx of the great toe, with respect to PHV, does not differ significantly. The consistency of the MEKKA ossification method makes it a suitable system for assessing PHV and skeletal maturity of the foot. This is crucial in orthopaedic interventions that depend on skeletal maturity of the patients, such as epiphysiodesis for leg-length discrepancy, posterior spinal fusion for adolescent idiopathic scoliosis and even prophylactic pinning of the contralateral hip for a child with slipped capital femoral epiphysis.16-21 The MEKKA system also provides a valuable tool in the treatment and management of juvenile hallux valgus. Hemiepiphysiodesis of the great toe metatarsal is a treatment for juvenile hallux valgus6-7, however, this procedure requires an open epiphysis with growth potential that can be translated into angular correction of the deformity. The MEKKA system acts as a complimentary system to the calcaneal system, increasing the accuracy of predicted growth and PHV identification, facilitating the timing of surgery. Additionally, information about growth potential could be gathered retrospectively from previous hemiepiphysiodesis surgeries to judge the appropriateness of the timing of these surgical interventions. For surgeons concerned with lower extremity pathology, imaging necessary for the determination of MEKKA staging would likely already be obtained, minimizing the need for additional imaging.
The Risser system is one of the most commonly used skeletal maturity systems, due to the visibility of the iliac apophysis excursion on posteroanterior views of the spine and correlation with end of spinal growth.25 Similarly, the calcaneal system uses extension of the calcaneal apophysis to determine maturity. In contrast to the Risser system which primarily occurs after PHV, both the calcaneal and MEKKA systems have ossification stages occurring both before and after PHV, allowing localization of PHV.9 Moreover, the MEKKA system can assess maturity of the foot from an anteroposterior foot radiograph, whereas the calcaneal system requires a lateral foot radiograph. Neither the MEKKA nor the calcaneal system requires gonadal exposure to radiation. If anteroposterior and lateral foot radiographs are both obtained for a patient, they can have their calcaneal and MEKKA stages both determined for more precise determination of maturity relative to PHV.
Imaging becomes a limiting factor for the MEKKA staging system, as appreciation of the physis requires a radiograph to be taken nearly perpendicular to the physeal plate. This burden can be reduced if the indication for imaging is communicated. A specific limitation of the study is the age of the Bolton-Brush collection, as the radiographs are from 80 years ago. There is evidence that children are reaching puberty at an earlier age today.26 However, our study uses PHV rather than chronological age which compensates for the earlier puberty onset of children today. Other concerns include the lack of data from children with varying ethnic backgrounds, since the vast majority of patients in the Bolton-Brush study came from upper middle class, white families from the Cleveland area.11
In conclusion, our study described the ossification pattern of the phalanges of the foot, creating a system where an anteroposterior foot radiograph can be used to determine skeletal maturity relative to skeletal age and PHV. Our system was compared with the calcaneal apophysis system, and if an anteroposterior and lateral foot radiographs are both taken, the MEKKA and calcaneal systems can be combined to judge the maturity closely.
Compliance with Ethical Standards
Funding Statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Ethical Statement
Ethical approval: Our research study did not involve human participants and/or animals.
Informed consent: Not required.
ICMJE Conflict of interest statement
JOS reports grants from Paediatric Orthopaedic Society of North America, during the conduct of the study; grants from Scoliosis Research Society, personal fees from Nuvasive and others from DePuy, outside the submitted work. RWL reports royalties paid to his institution, a portion of which are placed into a research fund that he controls, outside the submitted work. All other authors declare no conflict of interest.
References
- 1.Kumar S. Tall stature in children: differential diagnosis and management. Int J Pediatr Endocrinol 2013;2013(suppl 1):53. [Google Scholar]
- 2.Hoerr NL, Pyle S, Francis C. Radiographic atlas of skeletal development of the foot and ankle: a standard reference. Springfield, Illinois: Charles C. Thomas Publisher, 1962. [Google Scholar]
- 3.Greulich WW, Pyle SI. Radiographic atlas of the skeletal development of the hand and wrist. 2nd ed. Stanford, California: Stanford University Press, 1959. [Google Scholar]
- 4.Pyle SI, Hoerr NL. Radiographic atlas of the skeletal development of the knee: a standard reference. Springfield, Illinois: Charles C Thomas Publisher, 1955. [Google Scholar]
- 5.Hackman L, Davies CM, Black S. Age estimation using foot radiographs from a modern Scottish population. J Forensic Sci 2013;58:S146-S150. [DOI] [PubMed] [Google Scholar]
- 6.Greene JD, Nicholson AD, Sanders JO, et al. . Analysis of serial radiographs of the foot to determine normative values for the growth of the first metatarsal to guide hemiepiphysiodesis for immature hallux valgus. J Pediatr Orthop 2017;37:338-343. [DOI] [PubMed] [Google Scholar]
- 7.Davids JR, McBrayer D, Blackhurst DW. Juvenile hallux valgus deformity: surgical management by lateral hemiepiphyseodesis of the great toe metatarsal. J Pediatr Orthop 2007;27:826-830. [DOI] [PubMed] [Google Scholar]
- 8.Morrissy RT, Weinstein SL. Lovell and Winter’s Pediatric Orthopaedics. 6th ed. Philadelphia, Pennsylvania: Lippincott Williams & Wilkins, 2006. [Google Scholar]
- 9.Nicholson AD, Liu RW, Sanders JO, Cooperman DR. Relationship of calcaneal and iliac apophyseal ossification to peak height velocity timing in children. J Bone Joint Surg 2015;97:147-154. [DOI] [PubMed] [Google Scholar]
- 10.Todd TW. Atlas of skeletal maturation (hand). St. Louis, Missouri: C.V. Mosby, 1937. [Google Scholar]
- 11.Nelson S, Hans MG, Broadbent BH Jr, Dean D. The brush inquiry: an opportunity to investigate health outcomes in a well-characterized cohort. Am J Hum Biol 2000;12:1-9. [DOI] [PubMed] [Google Scholar]
- 12.Cundy P, Paterson D, Morris L, Foster B. Skeletal age estimation in leg length discrepancy. J Pediatr Orthop 1988;8:513-515. [DOI] [PubMed] [Google Scholar]
- 13.Mansourvar M, Ismail MA, Raj RG, et al. . The applicability of Greulich and Pyle atlas to assess skeletal age for four ethnic groups. J Forensic Leg Med 2014;22:26-29. [DOI] [PubMed] [Google Scholar]
- 14.Tanner JM, Davies PS. Clinical longitudinal standards for height and height velocity for North American children. J Pediatr 1985;107:317-329. [DOI] [PubMed] [Google Scholar]
- 15.Tanner J, Healy M, Goldstein H, et al. Assessment of skeletal maturity and prediction of adult height (TW3). London: WB Saunders, 2001. [Google Scholar]
- 16.Sanders JO, Browne RH, McConnell SJ, et al. . Maturity assessment and curve progression in girls with idiopathic scoliosis. J Bone Joint Surg [Am] 2007;89-A:64-73. [DOI] [PubMed] [Google Scholar]
- 17.Song KM, Little DG. Peak height velocity as a maturity indicator for males with idiopathic scoliosis. J Pediatr Orthop 2000;20:286-288. [PubMed] [Google Scholar]
- 18.Sanders JO. Maturity indicators in spinal deformity. J Bone Joint Surg [Am] 2007;89-A(suppl 1):14-20. [DOI] [PubMed] [Google Scholar]
- 19.Sanders JO, Browne RH, Cooney TE, et al. . Correlates of the peak height velocity in girls with idiopathic scoliosis. Spine 2006;31:2289-2295. [DOI] [PubMed] [Google Scholar]
- 20.Hauspie R, Bielicki T, Koniarek J. Skeletal maturity at onset of the adolescent growth spurt and at peak velocity for growth in height: a threshold effect? Ann Hum Biol 1991;18:23-29. [DOI] [PubMed] [Google Scholar]
- 21.Hägg U, Taranger J. Skeletal stages of the hand and wrist as indicators of the pubertal growth spurt. Acta Odontol Scand 1980;38:187-200. [DOI] [PubMed] [Google Scholar]
- 22.Sanders JO, Khoury JG, Kishan S, et al. . Predicting scoliosis progression from skeletal maturity: a simplified classification during adolescence. J Bone Joint Surg [Am] 2008;90-A:540-553. [DOI] [PubMed] [Google Scholar]
- 23.Heyworth BE, Osei DA, Fabricant PD, et al. . The shorthand bone age assessment: a simpler alternative to current methods. J Pediatr Orthop 2013;33:569-574. [DOI] [PubMed] [Google Scholar]
- 24.Hans SD, Sanders JO, Cooperman DR. Using the Sauvegrain method to predict peak height velocity in boys and girls. J Pediatr Orthop 2008;28:836-839. [DOI] [PubMed] [Google Scholar]
- 25.Risser JC. The Iliac apophysis; an invaluable sign in the management of scoliosis. Clin Orthop 1958;11:111-119. [PubMed] [Google Scholar]
- 26.Duval-Beaupere G, Dubousset J, Queneau P, Grossiord A. A unique theory on the course of scoliosis. Presse Med 1970;78:1141-1146. [PubMed] [Google Scholar]


