Abstract
Background
Guided growth by tension band plating is commonly used to correct coronal plane deformity. The purpose of this study was to measure the effect and further define parameters that influence results in coronal plane deformity around the knee.
Methods
The retrospective multicentre study included data on 967 physes in 537 patients, with an average follow-up of 16 months after plate insertion. Alignment analysis was compared preoperatively and in at least two measurements postoperatively, as well as with parameters that influence the rate and amount of correction.
Results
Average age at plate implantation was 11.35 years (SD 3.29).
Of those with femoral deformities, 85% of the patients finished the treatment and of those, 70% were corrected to standard alignment, while 14% have not yet achieved correction, and are still growing.
Of those with tibial deformities, 75% of the patients finished the treatment and of those 80% were corrected to standard alignment, while 25% have not yet achieved correction and are still growing.
The calculated rate of correction was 0.77°/month for the femur and 0.79°/month for the tibia.
In terms of complications, the overall rate of infection was 1.48%. In three patients (0.55%) screw breakage was recorded.
Factors found to significantly influence the amount of correction were age at plate implantation and direction of deformity.
Conclusion
Temporary hemiepiphysiodesis takes the advantage of physiological physeal growth to effectively treat angular deformities. Success of treatment is influenced by the age of the patient at plate implantation and direction of deformity.
Level of Evidence
IV
Keywords: hemiepiphysiodesis, guided growth, limb deformity, complications
Introduction
Angular deformities can be treated with corrective osteotomies and application of internal or external fixation. In children, this major intervention can be avoided using temporary hemiepiphysiodesis – guided growth.
Blount and Clarke1 first described the use of a staple for hemiepiphyseal arrest in 1949, and since then, many other procedures attempting to guide epiphyseal growth have been discussed and published.2-4
Hemiepiphysiodesis using a tension-band plate (TBP) for correction of valgus/varus deformities around the knee and for a variety of pathological conditions was first introduced in 2007 by Stevens.5 Since then, the indications have been expanded, including more rare diagnoses.6
The aim of this study was to measure the effect of temporary hemiepiphysiodesis for coronal plane deformities around the knee and to further define parameters that influence success.
Materials and methods
The retrospective multicentre study was conducted at five centres: in each centre approval was obtained from the local institutional review board.
Inclusion criteria were knee angular deformity in the coronal plane treated by different types of tension band plating and at least one preoperative and two postoperative digital-based full-length anteroposterior weight-bearing radiographs. The interval elected depended on the treating surgeon.
Only two-hole plates had been used; the 8-plate by Orthofix (Lewisville, Texas), a dynamic compression plate and the peanut plate by Biomet (Warsaw, Indiana). The majority of those used were 8 plate.
The deformity analysis of all radiographs was done in each centre by a designated investigator using TraumaCad software (product of Voyant Health - a Brainlab company, Munich, Germany). The investigators included paediatric orthopaedic surgeons as well as residents in orthopaedic surgery. This method has already been proven as a reliable tool in terms of intra- and inter-observer variability as shown in Segev et al.7 In their study, five paediatric orthopaedic surgeons measured 50 digital radiographs on three separate days using the TraumaCad system and found that there were no clinically important biases; the variability between specialists and residents was non-significant.
The mechanical lateral distal femoral angle (mLDFA) and the mechanical medial proximal tibial angle (mMPTA) were recorded and analyzed. Normal values for both were considered 87° SD 2°.8
All medical records for each patient were reviewed, including surgical reports and radiographs. The underlying aetiology was recorded as well as the age on the day of plate implantation. Remaining growth was estimated by subtracting the age of the patient on the day of plate implantation from 17 years for male patients and from 15 years for female patients. The use of this cutoff value amount method has been validated and has previously been used for various implementations, including the multiplier method for predicting limb-length discrepancy.9
Alignment analysis was compared preoperatively and in at least two measurements postoperatively; rate of correction was calculated and univariate and multivariate analyses were performed to determine parameters that influenced the rate and amount of correction.
Complications including screw breakage, postoperative infection and limited range of motion (ROM) were recorded. Early limited ROM was defined as failure to achieve 90° of flexion of the knee and lag extension by the end of the first month post-surgery. Late was defined as limited if not achieved the full ROM.
Postoperative infection was divided into ‘early’ (within the first postoperative month) and ‘late’ (after the first postoperative month).
Data was recorded and uploaded to a web-based central database by each centre.
Statistical analysis
Univariate and multivariate analyses were performed to determine parameters that influenced the rate and amount of correction.
Results
Patients
Data on 967 physes around the knee (distal femur and proximal tibia) in 537 patients was included, with a mean follow-up of 16 months (13 to 21) after plate insertion. The first follow-up radiograph was taken at a mean 3.4 months (1 to 9.1) while the second radiograph was taken at a mean 8.3 months (4.2 to 18). Patients included in our study group include diverse aetiologies for the deformity. The primary diagnoses are shown in Table 1.
Table 1.
The primary diagnoses
| Aetiology | Number of patients | Percentage | Average age (yrs) | Male:Female ratio |
|---|---|---|---|---|
| Idiopathic | 206 | 38.4 | 12.57 | 110:96 |
| Congenital | 105 | 19.6 | 9.37 | 59:46 |
| Blount’s disease | 46 | 8.6 | 9.47 | 28:18 |
| Metabolic (rickets) | 30 | 5.6 | 12.13 | 16:14 |
| Multiple exostoses | 26 | 4.8 | 12.71 | 19:7 |
| Post-traumatic | 25 | 4.7 | 11.64 | 18:7 |
| Syndrome | 21 | 3.9 | 12.52 | 7:14 |
| Skeletal dysplasia | 20 | 3.7 | 11.14 | 12:8 |
| Others* | 58 | 10.6 |
Others include: Post-tumour resection, mucopolysaccharidosis, Marfan, trisomy 21, post-surgery, cerebral palsy, post-infectious, idiopathic hemihypertrophy.
The most common aetiology was idiopathic (38.4%) with 372 physes in 206 patients; the second (19.6%) with 190 physes in 105 patients was congenital abnormalities – including congenital short femur, fibular hemimelia; then Blount’s disease (8.6%) with 90 physes in 46 patients; and metabolic (5.6%) – mainly including rickets in 58 physes in 30 patients.
Femoral correction
In all, 444 patients (85%) completed the treatment, and of those 311 (70%) were corrected to standard alignment (mLDFA between 85° and 89°); 75 (14.4%) have not yet achieved correction and are still growing. The mLDFA was changed at a mean of 0.77°/month (0.14°/month to 1.42°/month).
Figure 1 demonstrates the difference between the initial femoral deformity compared with the last follow-up based on the aetiology; the initial deformity is spread on the grids in a wide range and the last follow-up measurements are concentrated in the normal range of 85° to 90°.
Fig. 1.
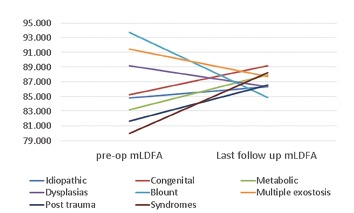
Initial femoral deformity (represented by mechanical lateral distal femoral angle (mLDFA)) compared with the last follow-up in different deformity aetiologies.
Tibial correction
In all, 341 patients (75%) had completed the treatment and of those, 250 (80%) were corrected to standard alignment (mMPTA 85° to 89°); 107 (24%) have not yet achieved correction and are still growing.
Medial proximal tibial angle changed at a mean of 0.79°/month (0.12°/month to 1.65°/month).
The difference between the femoral and the tibial change was not statistically significant.
Figure 2 demonstrates the difference between the initial tibial deformity compared with the last follow-up based on the aetiology: the initial deformity is spread on the grids in a wide range and in most cases the mMPTA is improving in time except for the syndromes’ group. Please pay attention also to the dysplasia, multiple exostosis Blount’s disease and syndromes groups - which do not achieve full correction.
Fig. 2.
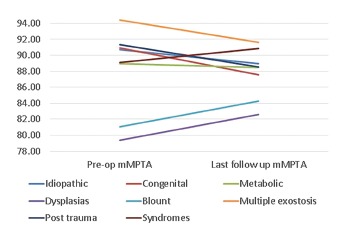
Initial tibial deformity (represented by mechanical medial proximal tibial angle (mMPTA)) compared with the last follow-up in different deformity aetiologies.
Patients‘ age
Age at plate implantation affects the success of treatment. Using Pearson correlation revealed that femur and tibia patients who had more than three years of growth at plate implantation had a better chance of achieving the surgical goal – for the femur, R = 0.67 (p = 0.030), for the tibia, R = 0.72 (p = 0.019).
Deformity direction
Using Pearson correlation shows that varus in the femur had a negative influence on the amount of correction, R = -0.74 (p = 0.021) while varus in the tibia had a positive influence on the amount of correction, R = 0.68 (p = 0.044).
Complications
The overall rate of infection was 1.48% (8 patients) (Table 2). In three patients (0.53%) screw breakage was recorded. Seven of them (87.5%) occurred in procedures done at the medial aspect of the knee.
Table 2.
Complications
| Aetiology | Bone location | Plate site | |
|---|---|---|---|
| Early postoperative infection | Idiopathic | Both tibias. | Lateral |
| Idiopathic | Both femurs and tibias | Medial | |
| Post-tumour | Right tibia | Medial | |
| Multiple exostoses | Left femur and tibia | Medial | |
| Late postoperative infection | Post-tumour | Both tibias | Medial |
| Congenital | Right femur and tibia | Medial | |
| Dysplasia | Both femurs and tibias | Medial | |
| Metabolic | Both femurs | Medial | |
| Early limited range of movement | Idiopathic | Both tibias | Lateral |
| Idiopathic | Right femur and both tibias | Medial | |
| Blount’s disease | Right femur and tibia | Lateral | |
| Blount’s disease | Left femur and tibia | Medial | |
| Not specified | Right tibia | Lateral | |
| Syndrome | Right femur | Lateral | |
| Late limited range of movement | Congenital | Left femur | Medial |
| Congenital | Both tibias | Medial | |
| Congenital | Both femurs | Medial | |
| Congenital | Left femur | Medial | |
| Congenital | Right tibia | Medial | |
| Metabolic | Both femurs and tibias | Lateral | |
| Dysplasia | Right femur | Lateral | |
| Screw breakage | Blount’s disease | Both tibias | Lateral |
| Blount’s disease | Right tibia | Lateral | |
| Post-trauma | Both tibias | Medial |
There were three cases of documented broken screws and all were metaphyseal tibial screws. Early limited ROM was recorded in six patients (1.12%), while late limited ROM was recorded in seven patients (1.3%). Four of them were diagnosed with early limited ROM that has not been resolved and three were not detected earlier.
Discussion
Our study includes data on 967 physes in 537 patients. In all, 70% of the femoral deformities and 80% of the tibial deformities were corrected to standard alignment (mLDFA and mMPTA between 85° and 89°) in a mean follow-up of 16 months after plate insertion.
Different definitions of success might explain different success rates: Burghardt and Herzenberg10 demonstrated a rate of around 90% of treatment success: in their series, success was defined as reaching either full deformity correction or avoiding the need for realignment osteotomy in the treated limb segment.
Another explanation for the relatively lower success rates presented in this series is the diversity of the primary diagnosis of the patients. Patients in our study group include diverse aetiologies for the deformity with idiopathic making up less than 40%, while the rest are pathologic physes which usually have a lower success rate of correction.6 The largest study of pathologic physes in the literature was conducted by Yilmaz et al.11 A total of 29 children (50 limbs) with skeletal dysplasia were treated with TBPs to correct varus or valgus deformity. In all, 89% of valgus deformities were corrected and 58% of varus deformities were corrected – results that correlate with our study results. Many authors have explained failures as a result of the age of the patient and the fact that there was not enough growth potential left for guided growth.10, 12 Chronological age is a controversial parameter, as is bone age which is based on the Greulich and Pyle Radiographic Atlas of Skeletal Development.13 This atlas is based on the development of children who were maturing in 1930s America and differences in ethnicity and access to medical and nutritional resources make application in a modern context problematic. We have used remaining growth; subtracting the age at day of plate implantation from 17 years for male patients and from 15 years for female patients. We found that patients who had more than three years of growth at plate implantation had a better chance of achieving the surgical goal.
In terms of rate of correction in our diverse group of patients, mLDFA was changed at a mean of 0.77°/month and mMPTA was changed at a mean of 0.79°/month.
There was no statistically significant difference between the two rates of correction of the femur and tibia in our study, despite well-known evidence that the growth rate of the distal femoral growth plate is 9 mm per year while the growth rate of the proximal tibial growth plate is 6 mm per year.14 The numbers quoted above had been validated on a study population composed mainly of patients with poliomyelitis. Our findings can be explained by the diversity of the primary diagnosis of the patients – including idiopathic as well as pathologic physes.
Previous studies have tried to calculate the rate of correction; Burghardt and Herzenberg10 found that the mLDFA changed at an average of 0.65°/month while the mMPTA changed at an average of 0.58°/month (their study population included diverse aetiologies). Ballal et al15 found a mean rate of correction of 0.7° per month in the femur (0.3° to 1.5°) and 0.5° per month in the tibia.
Guzman et al16 measured a 0.32°/month change in the anatomic lateral distal femoral angle (in an idiopathic genu valgum group of patients). The differences in the rate of correction between the studies are probably due to the diversity of diagnoses. Previous studies such as that of Mielke and Stevens17 showed that idiopathic cases demonstrate faster correction rate when compared with pathological physes.
Wiemann et al18 studied physeal stapling versus 8-plate hemiepiphysiodesis for guided correction of angular deformity about the knee. In their study, 39 patients with different aetiologies were treated with staples and 24 with 8-plates. They found the rate of correction was 0.825°/month with the staple and 0.925°/month with a TBP. They did not specify whether the rate above was for the femur or tibia.
In terms of complications, there were four cases of early postoperative infection within the first postoperative month and four cases of late postoperative infection after the first postoperative month documented. The overall rate of infection was 1.48%, mostly non-idiopathic. Out of those eight cases of infection, seven were in procedures done at the medial aspect of the knee. This may have been a result of knocked knees leading to a continuous rub on the wound from the other leg as well as from the pants worn.
There were three documented cases of broken screws: two of them were patients with Blount’s disease, one was a patient with post-traumatic malalignment; all the broken screws were metaphyseal tibial screws.
In the Wiemann et al18 study quoted above, one patient with Blount’s disease from the 8-plate group had screw breakage.
Schroerlucke et al19 published a study on a series of 23 patients with 31 angular deformities and found implant failure in eight (26%) of 31 proximal tibia constructs. All eight failures occurred in patients with Blount’s disease and involved breakage of the tibial metaphyseal screw.
Histological examination of the physis of patients with Blount’s disease reveals disorganization and misalignment of cells within cartilaginous zones and areas of cystic degeneration and necrosis, as well as regions where enchondral ossification has ceased.20, 21 The cyclic loading of the varus knee along with an abnormal pathological condition could create significant movement at the physis and cause the screw failure secondary to fatigue.
Limited ROM was recorded in six patients at the early postoperative period and in seven patients later. We have not found any common denominator between those cases.
There are several limitations in our study that should be acknowledged. The diversity of the primary diagnosis of the patients represents a potential advantage – making it the largest study ever published dealing with this subject, but at the same time, it may have been the cause of the inconclusive results in apparently obvious parameters such as the finding that there was no statistically significant difference between the rate of correction of the femur and tibia.
We were unable to assess rebound growth due to insufficient follow-up data until skeletal maturity in some of the patients. The rebound phenomenon requires further studying, but since it is a simple and well-tolerated procedure, it does not preclude re-starting treatment if it occurs.5
We were unable to estimate the impact of weight on failure due to limited data on this parameter – data was available only for 183 out of 537 patients (34%). Data collected did not include measurement of mechanical axis deviation which primarily affects the knee but also has an effect on the hip, ankle and subtalar joints.22 This study is focused on coronal plain deformities around the knee – distal femur and proximal tibia – and those are better represented by the mLDFA and the mMPTA.
In conclusion, temporary hemiepiphysiodesis takes advantage of physiological physeal growth to effectively treat angular deformities with low complication rates. It was proven to be a recommended first line of treatment in diverse cases before osteotomy. Success of treatment is influenced by the age of the patient at plate implantation, and direction of deformity.
Compliance with Ethical Standards
Funding Statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Ethical Statement
Ethical approval: This retrospective multicentre study was conducted at five centres. In each centre, approval was obtained from the local institutional review board. The article does not contain any studies with animals performed by any of the authors.
Informed consent: For this type of study formal consent is not required.
ICMJE Conflict of interest statement
R. Rödl has received royalties from Merete Medical.
J. E. Herzenberg is a consultant for the following companies: Orthofix, Orthopediatrics, Smith Nephew, Nuvasive.
U. Narayanan is a member of the AO Foundation-Pediatric Expert Group.
All other authors declare that they have no conflict of interest.
References
- 1.Blount WP, Clarke GR. Control of bone growth by epiphyseal stapling; a preliminary report. J Bone Joint Surg [Am] 1949;31-A:464-478. [PubMed] [Google Scholar]
- 2.Eidelman M, D’Agostino P. Hemiepiphysiodesis around the knee by percutaneously guided and grooved staple. J Pediatr Orthop B 2005;14:434-435. [DOI] [PubMed] [Google Scholar]
- 3.Horton GA, Olney BW. Epiphysiodesis of the lower extremity: results of the percutaneous technique. J Pediatr Orthop 1996;16:180-182. [DOI] [PubMed] [Google Scholar]
- 4.Métaizeau JP, Wong-Chung J, Bertrand H, Pasquier P. Percutaneous epiphysiodesis using transphyseal screws (PETS). J Pediatr Orthop 1998;18:363-369. [PubMed] [Google Scholar]
- 5.Stevens PM. Guided growth for angular correction: a preliminary series using a tension band plate. J Pediatr Orthop 2007;27:253-259. [DOI] [PubMed] [Google Scholar]
- 6.Shabtai L, Herzenberg JE. Limits of Growth Modulation Using Tension Band Plates in the Lower Extremities. J Am Acad Orthop Surg 2016;24:691-701. [DOI] [PubMed] [Google Scholar]
- 7.Segev E, Hemo Y, Wientroub S, et al. . Intra- and interobserver reliability analysis of digital radiographic measurements for pediatric orthopedic parameters using a novel PACS integrated computer software program. J Child Orthop 2010;4:331-341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Paley D. Principles of Deformity Correction. Ed Herzenberg JE. Berlin, Heidelberg: Springer-Verlag, 2002. [Google Scholar]
- 9.Paley D, Bhave A, Herzenberg JE, Bowen JR. Multiplier method for predicting limb-length discrepancy. J Bone Joint Surg [Am] 2000;82-A:1432-1446. [DOI] [PubMed] [Google Scholar]
- 10.Burghardt RD, Herzenberg JE. Temporary hemiepiphysiodesis with the eight-Plate for angular deformities: mid-term results. J Orthop Sci 2010;15:699-704. [DOI] [PubMed] [Google Scholar]
- 11.Yilmaz G, Oto M, Thabet AM, et al. . Correction of lower extremity angular deformities in skeletal dysplasia with hemiepiphysiodesis: a preliminary report. J Pediatr Orthop 2014;34:336-345. [DOI] [PubMed] [Google Scholar]
- 12.Boero S, Michelis MB, Riganti S. Use of the eight-Plate for angular correction of knee deformities due to idiopathic and pathologic physis: initiating treatment according to etiology. J Child Orthop 2011;5:209-216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Greulich WW, Pyle SI. Radiographic Atlas of Skeletal Development of the Hand and Wrist. 2nd ed. Stanford, CA: Stanford University Press, 1959. [Google Scholar]
- 14.Menelaus MB. Correction of leg length discrepancy by epiphysial arrest. J Bone Joint Surg [Br] 1966;48-B:336-339. [PubMed] [Google Scholar]
- 15.Ballal MS, Bruce CE, Nayagam S. Correcting genu varum and genu valgum in children by guided growth: temporary hemiepiphysiodesis using tension band plates. J Bone Joint Surg [Br] 2010;92-B:273-276. [DOI] [PubMed] [Google Scholar]
- 16.Guzman H, Yaszay B, Scott VP, Bastrom TP, Mubarak SJ. Early experience with medial femoral tension band plating in idiopathic genu valgum. J Child Orthop 2011;5:11-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mielke CH, Stevens PM. Hemiepiphyseal stapling for knee deformities in children younger than 10 years: a preliminary report. J Pediatr Orthop 1996;16:423-429. [DOI] [PubMed] [Google Scholar]
- 18.Wiemann JM IV, Tryon C, Szalay EA. Physeal stapling versus 8-plate hemiepiphysiodesis for guided correction of angular deformity about the knee. J Pediatr Orthop 2009;29:481-485. [DOI] [PubMed] [Google Scholar]
- 19.Schroerlucke S, Bertrand S, Clapp J, Bundy J, Gregg FO. Failure of Orthofix eight-Plate for the treatment of Blount disease. J Pediatr Orthop 2009;29:57-60. [DOI] [PubMed] [Google Scholar]
- 20.Thompson GH, Carter JR. Late-onset tibia vara (Blount’s disease). Current concepts. Clin Orthop Relat Res 1990;:24-35. [PubMed] [Google Scholar]
- 21.Carter JR, Thompson GH, Leeson MC, et al. . Physeal histopathology in late-onset tibia vara In: Uhthoff HK, Wiley JJ, eds Behavior of the Growth Plate. New York, NY: Raven Press; 1988:285. [Google Scholar]
- 22.Paley D, Tetsworth K. Mechanical axis deviation of the lower limbs. Preoperative planning of uniapical angular deformities of the tibia or femur. Clin Orthop Relat Res 1992;280:48-64. [PubMed] [Google Scholar]


