Abstract
Objective
The picosecond 755 nm alexandrite laser using a diffractive lens array has demonstrated consistent clinical efficacy for improving the appearance of acne scarring and wrinkles amongst other benefits. This small pilot study is to assess the difference, if any, in clinical benefit if a higher than the standard protocol for number of pulses delivered to a tissue area is used compared to the standard protocol guidelines.
Method
Seven subjects received treatment to one side of the face with a standard protocol number of laser pulses with the other side of the face receiving higher than standard number of pulses from the same 755 nm picosecond laser using an additional diffractive lens array. Photographs at final follow up were compared to baseline by two blinded Board Certified Dermatologists and assessed for improvements to acne scarring using a 6‐point grading score, for wrinkles using the Fitzpatrick Wrinkle & Elastosis 3‐point grading scale and a Global Aesthetic Improvement Scale assessment. Subjects also completed a satisfaction questionnaire.
Results
For the acne scarring subjects, the average improvement from baseline to final follow up was 4.0 +/− 1.0 for the standard treated side and 4.5 +/− 0.5 for the high pulse side. There was no statistically significant difference between the two treated sides (P > 0.05, n = 3 paired t‐test). For the wrinkle subjects, the average grading of the standard pulse side improved from 2.0 +/− 0.82 to 1.75 +/− 1.0 from baseline to final follow‐up. The high pulse side improved from 1.5 +/− 1.0 to 1.125 +/− 0.25 from baseline to final follow‐up. There was no statistically significant difference between the improvement of the standard and high pulse treatment sides (P > 0.05, n = 4 paired t‐test). The comparison of baseline to final follow‐up images of each subject found both sides to be Much or Very Much improved with no statistically significant difference between the standard and high pulse sides (P > 0.05, n = 7 paired t‐test). Six of the seven subjects did not note any difference between the effect on different sides of the face and four of the seven rated their overall improvement after treatment as Good, three subjects as Reasonable and one subject with Slight Improvement. All subjects found the treatment comfortable and easy to tolerate and there was no increased incidence of side effects other than the mild occurrences typically observed for this type of treatment.
Conclusion
This is a small pilot study with limited subject numbers and further data is needed to be able to make firm conclusions of observed trends, which suggest that the use of higher than standard suggested protocol number of pulses with the diffractive lens array and the 755 nm picosecond laser does not appear to offer any additional benefit over that that can already be achieved with the standard number of pulses, but also does not increase risk of detrimental post treatment effects either. Lasers Surg. Med. 50:51–55, 2018. © 2017 The Authors. Lasers in Surgery and Medicine Published by Wiley Periodicals, Inc.
Keywords: Picosecond, non‐ablative, facial rejuvenation, wrinkle, acne scarring, laser
INTRODUCTION
The picosecond pulse duration laser at 755 nm has demonstrated consistent clinical efficacy for tattoo removal, pigment conditions, wrinkle removal and acne scarring 1, 2, 3, 4.
Initially exploited for enhancing removal of tattoo pigment over the nanosecond laser technologies, the picosecond duration is 10 times shorter than the traditional q‐switched nanosecond devices. This shorter pulse delivery creates more photomechanical shock than the nanosecond duration, with greater capacity for shattering ink or pigment and thus requires less treatments to remove tattoos than the longer nanosecond devices 5.
In the wake of this use for tattoo removal, a diffractive lens array was developed as an additional optic to attach to the 755 nm Alexandrite laser hand‐piece. Designed with a dense arrangement of micro‐lenses that alter distribution of the picosecond pulse into points of high fluence, which cover no more than 10% of the treatment spot in total, surrounded by a background coverage of low intensity irradiation. These high intensity areas receive around 20 times more energy compared to the background treatment area that receives low level exposure. The unique action of these micro‐beams stimulates neo‐collagenesis and neo‐elastinogenesis without ablation, even after multiple passes, via novel pressure injuries and cell signaling 6.
Studies have been reported that demonstrate the effectiveness of the 755 nm picosecond laser with diffractive lens array for the reduction of facial wrinkles 4 and photo‐damage on other areas such as the décolletage 7 and hands 8. The picosecond laser has a high specificity for its target but with less heat generation in the epidermal and dermal layers than is seen with longer pulse durations. This gives the opportunity for safer and more effective treatment options for darker Fitzpatrick skin types without the significant risks of thermal diffusion to the surrounding tissues and possible post‐inflammatory hyperpigmentation (PIH) that nanosecond pulse durations can produce. There are numerous studies published to support this 3, 9, 10.
Typical treatments are performed at 4–6 week intervals, although study work has demonstrated that a compressed treatment schedule of every 2–3 weeks has also proven safe and effective since there is no excessive tissue damage with the treatment that might prolong recovery and downtime 11. The standard treatment protocol from the Manufacturing Company of the device guide the number of pulses for a full‐face treatment to be around 5000–6000 pulses (3–4 passes) using the diffractive lens array. Investigative work presented during the 24th European Academy of Dermatology and Venereology Congress in Copenhagen by Dr. Luigi L. Polla suggested that the use of lower numbers of pulses than this standard protocol could reduce the clinical outcome on wrinkles and fine lines 12 which led this author to consider the possible role in the number of pulses performed on an area on clinical efficacy. The primary purpose of this study was to investigate the effect if any of using higher than standard numbers of pulses using a split face prospective study design on seven subjects seeking improvement in acne scars and skin rejuvenation.
MATERIALS AND METHODS
This pilot study investigated the outcomes from using the recommended standard pulse coverage with a diffractive lens array coupled with a picosecond domain 755 nm Alexandrite laser (PicoSure™, Cynosure Inc., Westford, MA) on one side of the face compared to the second side where a high pulse coverage was used. This investigator initiated study was conducted at Skinperium Laser Clinic, Boom, Belgium.
Seven subjects were enrolled on this study, three subjects with acne scars (average age 33 +/− 1 years) and four who were typical candidates that would benefit from rejuvenation (average age 62 +/− 10 years). Those subjects were recruited from the clinics typical demographic of patients presenting for elective treatments for tissue improvement. Skin types for these seven patients ranges from type II to IV.
Eligible subjects had to be healthy non‐smokers between 18 and 80 years. Subjects had to be willing to consent to participate in the study, to comply with the requirements of the study including the split face method of treatment, being photographed and able to attend all the treatment and follow up visits.
Subjects were randomly assigned one half of the face for treatment with the recommended pulse coverage for their treatment while the second half of the face had higher pulse coverage of approximately 1.7 times the normal number of pulses in the same session. Five treatments were performed, at four week intervals, and follow‐up visits were scheduled at 1, 3 and at least 6 months. Average final term follow‐up was 8 months +/− 2.5 months. A 6 mm spot size hand‐piece with diffractive lens array delivered a treatment fluence of 0.57 J/cm2, using 10 Hz repetition rate at a pulse duration of 750 picoseconds and with a 50% overlap of adjacent pulses. Standard treatment used an average of 3301 +/− 155 pulses for the half face, which involved approximately four complete passes of the tissue area. The half of the face receiving the high pulse treatment had an average of 5867 +/− 500 pulses delivered to the treatment area. This equates to approximately 1.7 times the standard treatment pulses on the high pulse treatment side.
Standardized 2‐D and 3‐D digital photographic images were taken at baseline, 1, 3 and at final follow‐up visit utilizing the Visia and Vectra photographic system respectively (Canfield Scientific, Inc.). Photographs were taken from three angles: full frontal (0°) and at profile from the left (45°) and from the right side (−45°) and were taken under controlled lighting conditions.
Two Board Certified Dermatologists, who were not involved in the treatments, ranked the photographs for overall acne scar improvement using a 6‐point grading score from 0 to 5 (see Table 1).
Table 1.
Acne Scar Improvement Score
| Score | Improvement | |
|---|---|---|
| 0 | <10% | No improvement |
| 1 | 10–24% | Minimal improvement |
| 2 | 25–49% | Moderate improvement |
| 3 | 50–74% | Good improvement |
| 4 | 75–89% | Very good improvement |
| 5 | >90% | Excellent improvement |
Wrinkles were assessed by the laser experts using the Fitzpatrick Wrinkle & Elastosis Scale (FWS) for rejuvenation (three‐point grading: 1 for fine wrinkles; 2 for fine to moderate wrinkles, moderate number of lines; 3 for fine to deep wrinkles, numerous lines with or without redundant skin folds). Finally, using a Global Aesthetic Improvement Scale Assessment (GAIS) (see Table 2.) overall improvement of the two sides of the face each from baseline to final follow‐up was recorded by each physician.
Table 2.
Global Aesthetic Improvement Scale
| Score | Improvement |
|---|---|
| 1 | Very much improved |
| 2 | Much improved |
| 3 | Improved |
| 4 | No change |
| 5 | Worse |
Data for the standard and high pulse treatment sides were statistically compared using students paired t‐Test. Subjects also completed a satisfaction questionnaire where they recorded overall improvement, if they noticed a difference from one side over the other and whether the treatment was comfortable and easy to tolerate.
RESULTS
Blinded assessment of the baseline and final follow‐up photographs of the three acne scar subjects were scored with an average improvement from baseline of 4.0 +/− 1.0 for the standard pulse side and 4.5 +/− 0.5 for the high pulse side. There was no statistically significant difference between the two treated sides (P = 0.225) (See Fig. 1).
Figure 1.
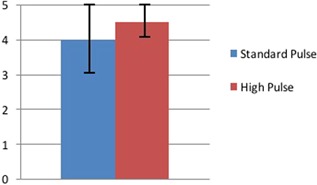
Average improvement scores for Acne Scarring of standard pulse and high pulse treatment areas at final follow‐up from a 6‐point grading score (0—no improvement, 1—minimal improvement, 2—moderate improvement, 3—good improvement, 4—very good improvement, and 5—excellent improvement).
For the blinded assessment of the four rejuvenation subjects, at baseline the side of the face to receive the standard number of pulses was graded at an average of 2.0 +/− 0.82 and the side of the face to receive the high pulse number of pulses at an average of 1.75 +/− 0.65. At follow‐up, the standard side of the faces had an average grading of 1.5 +/− 1.0. The high pulse side of the face was graded at an average of 1.125 +/− 0.25. There was no statistically significant difference between the improvement of the standard and high pulse treatment sides (P > 0.05) (See Fig. 2).
Figure 2.
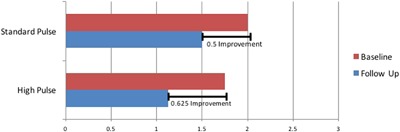
Average Fitzpatrick Wrinkle Scale score at baseline and final follow‐up for standard pulse and high pulse treatment areas from a 3‐point grading scale (1—fine wrinkles, 2—fine to moderate depth wrinkles, moderate number of lines, 3—fine to deep wrinkles, numerous lines with, or without redundant skin folds.
Comparison of the baseline to final follow‐up photographs of each subject gave an average GAIS score of 2.0 +/− 0.7 for the standard pulse sides of the subjects faces and 1.8 +/− 0.6 for the high pulse treatment side equating to an assessment between Much Improved and Very Much Improved for both treatment sides. There was no statistically significant difference between the standard and high pulse treatment sides (P = 0.788) (See Fig. 3).
Figure 3.
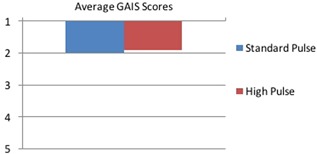
Average Global Aesthetic Improvement Scale Assessment (GAIS) from baseline to final follow‐up for the standard pulse and high pulse treatment areas (1—very much improved, 2—much improved, 3—improved, 4—no change, 5—worse.
Four of the seven subjects rated their improvement after treatment as Good, with a score of 4 out of 5 while three subjects sored themselves 3 out of 5 with Reasonable improvement. One subject scored themselves 2 out of 5 with a Slight improvement. In answer to the question if the subjects could see any difference in the treatment outcome on their left or right sides of the face, six of the seven subjects (86%) said that they could not see a difference, while the final subject reported they had slightly more improvement on the Standard treatment side. When asked if the treatment was comfortable and easy to tolerate, all seven subjects either Agreed or Strongly Agreed.
There was no increased incidence of side effects other than the mild occurrences typically observed with this type of treatment during this study, even on areas treated with “high pulse” coverage. These include erythema and edema lasting for several hours. None of the subjects experienced any petechiae post‐treatment using the diffractive array in conjunction with the 755 nm Alexandrite hand‐piece. Treatments were performed in the lead up to and during summertime and one subject with phototype IV experienced mild transient post‐inflammatory hyperpigmentation, which resolved spontaneously within 2 months.
DISCUSSION
For both the acne scarring and wrinkle subjects, the visible clinical outcomes from treatment with both standard numbers of pulses and elevated number of pulses are assessed by blinded observers with similar good improvements from baseline to final follow up (see Fig. 4a–d and Fig. 5a–d).
Figure 4.

Acne scarring subject. (a) left side of face at baseline before treatment, (b) left side of face 12 months post 4 treatments with standard number of pulses, (c) right side of face at baseline before treatment, and (d) right side of face 12 months post 4 treatments with high number of pulses.
Figure 5.

Wrinkle subject. (a) Left side of face at baseline before treatment, (b) left side of face 6 months post 5 treatments with high number of pulses, (c) right side of face at baseline before treatment, and (d) right side of face 6 months post 5 treatments with standard number of pulses.
This improvement at the final follow‐up does not appear any further enhanced using a higher pulse treatment protocol over the standard number of pulses. Similarly, clinical improvement did not appear adversely effected by the higher pulse protocol nor did the post treatment experiences of the subjects with adverse effects.
The 755 nm picosecond alexandrite laser with the incorporation of the diffractive lens array has been well documented as safe and effective for treatment of signs of photo‐aging including wrinkles, pigmentation and scarring. The diffractive lens comprises of a close packed array of over 120 hexagonal lenses, 500μm center to center, which changes the energy profile of the laser pulse, focusing 70% of the total pulse energy into micro‐spots of high fluence surrounded by an even background distribution of low energy comprising of the remaining 30% of the pulse total. Less than 10% of the tissue is exposed to this ultra‐high energy, with the corresponding point in the epidermis beneath the micro‐spot experiencing a controlled injury which results in a Laser Induced Optical Breakdown (LIOB). These discrete micro‐injuries have been identified as pockets of intra‐epidermal necrosis, created without damage to the junctional melanocytes or the dermis below or ablative wound to the tissue surface 6. Their formation is described as a laser‐matter interaction mechanism involving limited thermal residue around the micro‐damaged areas. This process results in cavitation bubbles in the skin which, when they expand, may generate shock waves to disrupt the tissue and generate a repair response 13. In addition to studies with the picosecond device used in this study, similar micro‐damage vacuoles have been observed with a prototype fractionated Nd:YAG 1064 nm device with sub‐nanosecond pulses 14 and very recently visualized in‐vivo with multiphoton‐microscopy (MPM) using a dual wavelength 532 nm and 1064 nm picosecond device with holographic diffractive beam splitter 15. This study by Balu and colleagues confirmed the study findings of Tanghetti et al with the 755 nm picosecond laser for location of the LIOB's in the epidermis and for melanin being the main target. MPM could clearly pinpoint the damage to the pigmented cells as ruptured cells with enlarged and irregularly shaped nuclei compared to normal cells in the vicinity, noting that areas of microscopic epidermal necrotic debris were smaller when the 1064 nm wavelength was used compare to when the 532 nm wavelength was used. This was concluded to be likely due to the higher melanin absorption at 532 nm as compared to 1064 nm 16.
The MPM study also identified clusters of small inflammatory cells in the proximity of the damaged cells and separate histological investigations have confirmed the increased production of collagen and density of elastin fibers in the weeks and months post treatment 2.
Clinical investigations have demonstrated that pulse counts of 5000–6000 pulses (3–4 passes) for full face coverage have demonstrated clinically consistent results and that has been adopted as the standard suggested treatment protocol for this diffractive lens hand‐piece. The results from this study would suggest that there is little observable benefit to be gained from using higher than standard number of pulses to cover a treatment area and that in effect, the use of the standard number of pulses is already reaching the saturation point of possible clinical influence in the epidermis and dermis at that time, which may be dictated by the level of endogenous melanin target in the tissue.
CONCLUSION
The use of the diffractive lens array with a 755 nm picosecond laser and with the current recommended treatment protocol for parameters and number of pulses for coverage of an area gives the clinician opportunity to obtain good clinical benefit for the patient. The results from this small population pilot investigation suggest that the addition of significantly more pulses to cover a treatment area does not appear to add to this clinical benefit, however the number of subjects in this study was small and further subject data would be needed to confirm if this is a trend that extrapolates to the wider population or if there are other influences.
The use of increased treatment pulses and repeated laser passes to the area of tissue in this study did not increase incidence of side effects other than the mild occurrences usually associated with this type of treatment. None of these typical post treatment effects last more than several hours which makes this treatment commercially, a very acceptable treatment option for a laser clinician. In addition to consideration for side effects in daily practice, patient satisfaction and cost effectiveness is also an important factor. An interesting point to reflect on would be that if there is enhancement because of increased pulses noted in a larger population study, would this additional benefit be cost effective for the patient?
ACKNOWLEDGMENTS
I would like to acknowledge the support of Donna Freeman (Cynosure, Inc.) and Alexander Denis (Cynosure, Inc.) for their help with the data analysis and production of this manuscript.
Conflict of Interest Disclosures: Dr. Dierickx reports non‐financial support from Cynosure, Inc. during the conduct of the study; personal fees from Cynosure, Inc. outside of the submitted work.
REFERENCES
- 1. Brauer JA, Reddy KK, Anolik R, et al. Successful and rapid treatment of blue and green tattoo pigment with a novel picosecond laser. Arch Dermatol 2012; 148(7):820–823. [DOI] [PubMed] [Google Scholar]
- 2. Brauer JA, Kazlouskaya V, Alabdulrazzaq H, et al. Use of a picosecond pulse duration laser with specialized optic for treatment of facial acne scarring. JAMA Dermatol 2015; 151(3):278–284. [DOI] [PubMed] [Google Scholar]
- 3. Chan JC, Shek SY, Kono T, Yeung CK, Chan HH. A retrospective analysis on the management of pigmented lesions using a picosecond 755‐nm alexandrite laser in Asians. Lasers Surg Med 2016; 48(1):23–29. [DOI] [PubMed] [Google Scholar]
- 4. Weiss RA, McDaniel DH, Weiss MA, Mahoney AM, Beasley KL, Halvorson CR. Safety and efficacy of a novel diffractive lens array using a picosecond 755nm alexandrite laser for treatment of wrinkles. Lasers Surg Med 2017; 49(1):40–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Saedi N, Metelitsa A, Petrell K, Arndt KA, Dover JS. Treatment of tattoos with a picosecond alexandrite laser: a prospective trial. Arch Dermatol 2012; 148(12):1360–1363. [DOI] [PubMed] [Google Scholar]
- 6. Tanghetti EA. The histology of skin treated with a picosecond alexandrite laser and a fractional lens array. Lasers Surg Med 2016; 48(7):646–652. [DOI] [PubMed] [Google Scholar]
- 7. Wu DC, Fletcher L, Guiha I, Goldman MP. Evaluation of the safety and efficacy of the picosecond alexandrite laser with specialized lens array for treatment of the photoaging décolletage. Lasers Surg Med 2016; 48(2):188–192. [DOI] [PubMed] [Google Scholar]
- 8. Saluja R. Evaluation of the safety and efficacy of a low fluence, picopulsed, alexandrite laser in a pico‐toning technique with a diffractive lens optic for the treatment of photodamaged and textural improvement in “off the face” applications. J Drugs Dermatol 2016; 15(11):1398–1401. [PubMed] [Google Scholar]
- 9. Haimovic A. Brauer JA, Cindy Bae YS, Geronemus RG. Safety of a picosecond laser with diffractive lens array (DLA) in the treatment of Fitzpatrick skin types IV to VI: A retrospective review. J Am Acad Dermatol 2016; 74(5):931–936. [DOI] [PubMed] [Google Scholar]
- 10. Levin MK, Ng E, Bae YS, Brauer JA, Geronemus RG. Treatment of pigmentary disorders in patients with skin of color with a novel 755‐nm picosecond, Q‐switched ruby, and Q‐switched Nd:YAG nanosecond lasers: a retrospective photographic review. Lasers Surg Med 2016; 48(2):181–187. [DOI] [PubMed] [Google Scholar]
- 11. Khetarpal S, Desai S, Kruter L, et al. Picosecond laser with specialized optic for facial rejuvenation using a compressed treatment interval. Lasers Surg Med 2016; 48(8):723–726. [DOI] [PubMed] [Google Scholar]
- 12. Polla L.L. (2015, September) Picoseconds laser facial rejuvenation. Paper presented at 24th European Academy of Dermatology and Venereology, Copenhagen, Denmark.
- 13. Habbema L, Verhagen R, Van Hal R, Liu Y, Varghese B. Efficacy of minimally invasive nonthermal laser‐induced optical breakdown technology for skin rejuvenation. Lasers Med Sci 2013; 28(3):935–940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Habbema L, Verhagen R, Van Hal R, Liu Y, Varghese B. Minimally invasive non‐thermal laser‐induced optical breakdown for skin rejuvenation. J Biophotonics 2012; 5(2):194–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Balu M, Lentsch G, Korta DZ, Konig K, Kelly KM, Tromberg BJ, Zachary CB. In vivo multiphoton‐microscopy of picosecond‐laser‐induced optical breakdown in human skin. Lasers Surg Med 2017; 49(6):555–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Zonios G, Bykowski J, Kollias N. Skin melanin, hemoglobin and light scattering properties can be quantitatively assed in vivo using diffuse reflectance spectroscopy. J Invest Dermatol 2001; 117(6):1452–1457. [DOI] [PubMed] [Google Scholar]


