Abstract
Purpose.
Food and eating convey memories and feelings and serve important functions in creating and maintaining relationships. Given the increasing rate of diabetes in the United States, research understanding the meaning of food may shed light on how patients negotiate everyday food choices while managing type 2 diabetes. The purpose of this qualitative study was to explore the meaning of food among adults with type 2 diabetes living in Northern Appalachia.
Methods.
In-depth, face-to-face interviews were conducted with type 2 diabetes patients. Interviews were coded and analyzed via thematic analysis.
Results.
Nineteen adults with type 2 diabetes (mean age 68.7 ± 10.6 years, mean A1C 7.4 ± 1.4%, mean diabetes duration 10.9 ± 11.9 years, 52.6% female, 100% white) participated in the study. Qualitative analysis revealed three themes: 1) “Sustaining Life:” Food and the Demands of Diabetes Management, in which participants described the role of food as operational and said that eating was dictated by time rather than hunger or pleasure; 2) “Diabetes Feels Like a Yield Sign:” Diabetes Changes Perceptions of Food, Enjoyment, and Social Relationships, in which most participants described a negative or ambivalent relationship with food after their diabetes diagnosis; and 3) “Food is Everywhere; It’s Seducing:” Struggling With Diabetes Management in a Fast-Food Culture, in which participants discussed how the American fast-food culture was in direct conflict with the demands of diabetes and described how they struggled to follow a healthful diet in a culture that advertised the opposite in many venues.
Conclusion.
Adults with diabetes may benefit from education that addresses both the personal and sociocultural factors that guide food choices.
Diabetes is one of the most significant and growing chronic health problems in the United States. Nearly 30 million people, or 9.3% of the population (1), have diabetes, with the vast majority (90–95%) diagnosed with type 2 diabetes (1–3). Managing type 2 diabetes requires patients to follow specific self-care recommendations, including following a healthful diet (4), engaging in regular physical activity (5,6), monitoring blood glucose levels (7), taking medications, and attending regular clinical appointments (8–10). These behaviors are critically linked to maintaining optimal glycemia; however, integrating them into daily life can be challenging (11–13).
Many patients perceive following a healthful diet to be the most challenging diabetes self-care behavior (4,14–18). Research has identified numerous barriers to dietary management, including a lack of family and friend support, the costs of healthful eating, difficulty in determining appropriate portion sizes, lack of knowledge about diet plans, negative emotions (e.g., depression and distress), age-related changes (e.g., altered taste and smell perception and dentation problems), time constraints, feelings of deprivation, and competing priorities (19–24). Compounding these barriers is the meaning food plays in peoples’ lives. For example, Liburd (25) explored the social and cultural meanings of food for African-American women with type 2 diabetes and found that food conveyed history, memory, feelings, and social status. Food and eating also serve important functions in creating and maintaining relationships (26–34) by providing a means to communicate and reflect emotions (35).
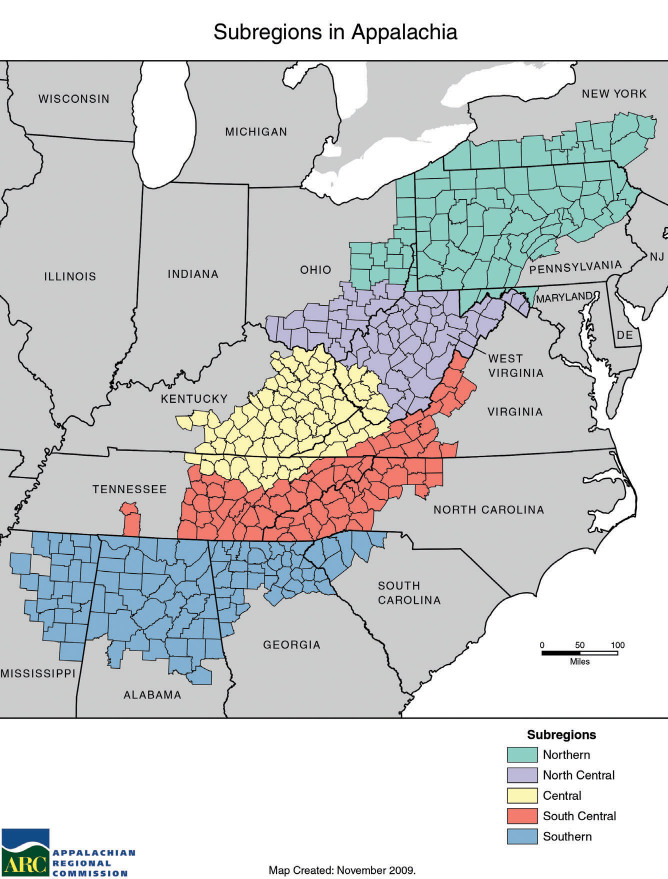
In rural Appalachia, healthful eating is influenced by family, church, the economy, the media, and social policies (36). Appalachia is a 205,000-square-mile region that encompasses 420 counties in 13 states from New York to Mississippi (Figure 1) (37). Forty-two percent of the region is rural compared to 20% nationally, and 95% of the population is white (37). Furthermore, people in Appalachia battle a poverty rate 1.5 times greater than the national average and suffer from higher unemployment, lower educational achievement, poorer health, and lower access to health care (37,38). Appalachia has its own cultural identity, which is defined by a strong sense of community, family, religion, and work ethic (39–41), as well as fatalistic attitudes, distrust of outsiders, and distrust of medical providers (41–45). Understanding the influences of Appalachian culture on the meaning of food for residents of the region is especially important given that diabetes rates in the region are 30–40% higher than the national average (46–48).
FIGURE 1.
Map of the subregions of Appalachia. Reprinted from ref. 37.
The purpose of this qualitative study was to explore the meaning of food among adults with type 2 diabetes living in Northern Appalachia. Given the integral role food plays in diabetes self-management, this research aimed at understanding the meaning of food among the region’s patients with type 2 diabetes may shed light on how patients negotiate everyday food choices while managing this chronic condition in Northern Appalachia.
Methodology
Research Design
Focused ethnographic methods were used in this study to describe the meaning of food in adults with type 2 diabetes living in Northern Appalachia. Focused ethnography is a means to accessing beliefs and practices in the context in which they occur, thereby improving our understanding of factors surrounding health and disease (49). As in other forms of qualitative research, the data collected are rich in their descriptions of beliefs, experiences, and behaviors of a population. In focused ethnography, informants, or participants, may not be connected by the same culture in the broadest sense; however, they typically share behavioral norms, local knowledge, and a common language from living through a common experience (e.g., living with type 2 diabetes). For the purposes of this study, Northern Appalachia, and specifically Central Pennsylvania, was the sociocultural context of the informants. The diagnosis of type 2 diabetes was an additional sociocultural context such that participants shared the diagnosis of type 2 diabetes, diabetes education practices, diabetes beliefs (e.g., high blood glucose is damaging), diabetes language (e.g., diabetes terminology such as A1C, insulin, and hypoglycemia), and recommended diabetes management behaviors (e.g., following a healthful diet, getting regular physical activity, checking blood glucose levels, and practicing preventive foot care).
Sample
To maximize the phenomenon of interest, we employed judgmental sampling, a form of purposive sampling (50), to recruit community-dwelling adults who were English-speaking and mentally alert and had been diagnosed with type 2 diabetes for at least 1 year. Consistent with the philosophical underpinnings of qualitative research, we used judgmental sampling to identify participants who were able to richly describe the experience of living with type 2 diabetes. Judgmental sampling techniques are useful in learning more about how a group (i.e., people with type 2 diabetes living in Northern Appalachia) thinks and experiences a given sociocultural phenomenon.
We screened potential participants for eligibility and collected sociodemographic information by telephone. Participants were excluded if they reported being diagnosed with Alzheimer’s disease, other dementia, stroke, or cancer in the past year; having severe psychopathology (i.e., schizophrenia or bipolar disorder); alcohol or drug abuse; or impaired activities of daily living (e.g., difficulties with bathing, dressing, personal hygiene, or walking). We recruited participants via the university diabetes database and through direct mailings and flyers in the communities surrounding Pennsylvania State University in University Park. The university’s institutional review board approved the study. All participants provided written informed consent before participating and received compensation for their time.
Data Collection
A multidisciplinary research team developed a semi-structured interview guide and field-tested it with two people. An experienced qualitative researcher conducted all interviews, asking participants broad, open-ended questions about the role of food in type 2 diabetes self-management and the personal, social, and cultural meanings of food in their lives. Participants were also asked how the diagnosis of diabetes has changed the meaning of food in their lives. The interviewer used directive probes to elicit additional information and clarify questions. Interviews were conducted at community sites (recreation centers and churches) and university conference rooms and lasted 30–120 minutes each. All interviews were digitally audio-recorded and transcribed verbatim. The researchers performed quality checks of the transcribed files while listening to the interview recordings to validate the transcriptions. Participants’ names and identifiers were removed to ensure confidentiality.
Additionally, a reflexive journal (written by the interviewer) was maintained during data collection. The purpose of the reflexive journal was to record the interviewer’s thoughts, beliefs, and experiences during the research process. The personal notes were used to evaluate the investigator’s response to specific interviews. The value of the reflexive journal was to reduce personal bias and maintain objectivity (51). In addition, memoing was incorporated to record ideas and insights regarding the data. Memoing is a form of data coding completed during data collection. Memos were written to connect notations with shared meaning. Such reflections helped the investigator recognize the need for additional interviewing of the informants (52). Salient information from the reflexive journal and memos was integrated into the data analysis.
Data Analysis
To analyze the qualitative data, we employed Spradley’s Developmental Research Sequence (DRS) of domain analysis, taxonomic analysis, componential analysis, and cultural themes (53). Spradley defines ethnographic analysis as a systematic examination of something to determine its parts, the relationships between the parts, and the relationships of the parts to the whole. The DRS method is an iterative process through which cultural ideas that arise in the field are transformed, translated, and represented during data analysis. This process involves sifting and sorting through pieces of data to detect and interpret thematic categorizations, searching for inconsistencies, and generating conclusions about what is happening and why. All levels of data analysis occur concurrently, informing each level throughout the analysis process. This process continues until data saturation is reached (i.e., until no new codes emerge).
For domain analysis, we identified categories evident in the transcripts with the intention of revealing participants’ role and personal, social, and cultural meanings of food. This analysis grouped words, phrases, and experiences into a collection of categories labeled by cover terms. For taxonomic analysis, we categorized the items in each domain to identify subsets of cultural knowledge. For semantic relationships, we noted links between the generic and specified concepts within and between categories. With componential analysis, we searched for attributes or components of meaning associated with the cultural categories. The objective of the componential analysis was to specify and understand the conditions under which the participants assigned something a specific name. Finally, we conducted thematic analysis to thread cultural themes via the domain, taxonomic, and componential analyses. The cultural themes represented propositions that guided the meaning of food and diet-related decision-making and, in turn, the optimal management of diabetes. Specifically, the research team selected themes that characterized the participants’ perceptions and experiences from data that occurred multiple times, both within and across transcripts. Each theme included words expressed by the participants to demonstrate that the concepts were grounded in the data. We used NVivo 10 software (QSR International, Victoria, Australia) to organize, sort, and structure the large amounts of text generated from the in-depth interviews.
Rigor
To support credibility (i.e., validity), we triangulated the investigators with experts from different disciplines (i.e., behavioral medicine, clinical psychology, and gerontology); this analyst triangulation provided a check on selective perceptions, as well as a means of identifying blind spots in the analysis (54). Furthermore, three participants reviewed the findings to achieve participant corroboration (55). Transferability (i.e., external validity) was supported via rich descriptions and verbatim quotations included in the data. To support dependability (i.e., reliability) of the data, a researcher not involved with the study conducted an external audit both to examine the process of the research study and to evaluate whether the findings, interpretations, and conclusions were supported by the data (56). Confirmability (i.e., objectivity) of the data was supported by tracking the decision-making process with an audit trail, which is a detailed description of the research steps conducted from the development of the project to the presentation of its findings (54,57).
Results
Nineteen adults with type 2 diabetes (mean age 68.7 ± 10.6 years, mean A1C 7.4 ± 1.4%, mean diabetes duration 10.9 ± 11.9 years, mean BMI 28.6 ± 5.2 kg/m2, mean education level 15.7 ± 2.6 years, 78.9% prescribed oral hypoglycemic agents, 31.6% prescribed insulin injections, 52.6% female, 100% white, 84.2% married, and 68.4% retired) participated in in-depth, face-to-face interviews lasting between 30 and 120 minutes (Table 1). All but one participant were born and raised in Northern Appalachia; the one participant not born in the region had lived there for >10 years.
TABLE 1.
Demographic and Health Characteristics of Participants
| Mean ± SD (n = 19) | Range | |
|---|---|---|
| A1C (%) | 7.4 ± 1.4 | 5.4–9.8 |
| BMI (kg/m2) | 28.6 ± 5.2 | 22.1–39.9 |
| Age (years) | 68.7 ± 0.6 | 50–83 |
| Diabetes duration (years) | 10.9 ± 11.9 | 3–47 |
| Education (years) | 15.7 ± 2.6 | 12–20 |
| Percentage | ||
| Prescribed oral hypoglycemic agent(s) | 78.9 | |
| Prescribed insulin injection(s) | 31.6 | |
| Female | 52.6 | |
| White | 100.0 | |
| Married | 84.2 | |
| Retired | 68.4 | |
A1C, BMI, and prescribed medications data are based on participant self-reports.
Below are descriptions of the themes that emerged from the data analysis. Transcript identifiers are used with quotations to indicate participant number, age, and sex.
“Sustaining Life:” Food and the Demands of Diabetes Management
All of the participants agreed that food was an important component of diabetes management. Participants described the role of food in self-management as operational:
“Sustaining life is what it means. My heritage is such that it is always a part of sustaining life. I was born as an Amish, and I grew up on a farm. The Amish heritage has always had a very strong influence in terms of how I think of food.” (ID 5, male, age 60 years)
“I know that I need food to be able to sustain my body. I’m a little furnace; it’s what I am.” (ID 2, male, age 76 years)
“Food is something that you operate with. So, has the role changed? No. It still helps me operate.” (ID 4, male, age 68 years)
Although most participants noted that the role of food was necessary to sustain life, many said diabetes changed how they approached food. Participants described making food-related decisions based on carbohydrate content and nutrition quality. The most commonly discussed barrier to following a healthful diet was difficulty with counting carbohydrates or following a low-carbohydrate meal plan:
“I do try to follow low carb, but it’s hard. For instance, this morning, when I dashed out the door, I grabbed a banana thinking, ‘I need to cut this in half.’ So, I put the rest in a Ziploc bag. I was hungry, and I really wanted to eat the whole banana, but I knew that I only wanted to have half now and half at lunch. It’s a give and take. I think now when I look at food, I look at fat, calories, and carbs, so food does look different to me. I look at a white baked potato and a baked sweet potato, and I just know that I’m going to go for half of a sweet potato.” (ID 3, female, age 58 years)
Participants who were prescribed insulin reported challenges in the timing of meals and carbohydrate counting. As described by this participant, insulin demanded that her eating be dictated by time rather than by hunger or pleasure:
“I guess before I became diabetic . . . we enjoyed eating. But now, I eat because I have to eat. I guess I don’t think about it. I just know, come lunch time, I have to eat; come 1:30, I have my snack; come dinner time, I have to eat; come bedtime, I have my snack. I eat because I look at the clock, and I see it’s time to eat. It’s a thing I have to do. I know, since I’m on insulin, I shouldn’t miss any meals, so I watch the clock.” (ID 1, female, age 77 years)
Others noted the challenge of insulin administration and how it requires a balance between what one eats and one’s subsequent self-care behaviors:
“An analogy is between a pail with a little hole in the bottom and a scale. . . . I have to be able to adjust how much water I put in the pail by how much leaks out. What a balancing trick that is! You have this continually changing dynamic of how much energy you need and how much [insulin] you need to put in the system.” (ID 2, male, age 76 years)
Interestingly, participants did not discuss many of the common barriers to healthful eating cited in the literature. For example, participants did not mention a lack of knowledge about dietary plans, meal planning and preparation, food shopping, cost, or age-related physical changes (e.g., dentation or altered taste or smell perception) affecting their ability to follow a healthful diet.
“Diabetes Feels Like a Yield Sign:” Diabetes Changes Perceptions of Food, Enjoyment, and Social Relationships
When asked to reflect on the personal and social meaning of food before they were diagnosed with diabetes, participants described it as communal and celebratory. To these participants, food was associated with family, religion, happiness, comfort, fond memories, and togetherness. Participants expressed joy with smiles, widened eyes, and looks upward while describing their reflections on food:
“Food is a gathering place. When family comes together, you sit around a table. When I’m with clients and they ask me to sit down and have something to eat or break bread or even have a drink with them, I very seldom refuse because that’s sort of a bonding thing. Bonding is important.” (ID 18, male, age 60 years)
“Food is very crucial to life to me in a social way. I’m Italian, and our social life was— I come from a very large family—life was always Sunday dinner and groups of people. And food always defined holidays. Christmas Eve, we were having fish, and Christmas Day, that was usually pasta and ravioli. Food has always been a big part of defining me and the rest of my family.” (ID 17, female, age 53 years)
“Food is comfort; that’s basically what it is. It’s something I do well: eat. No, I don’t do it well [laughing]. Or, I shouldn’t do it as well as I do it [laughing]. We use food socially. . . . It’s interesting, when you think about it. So many happy times, whether they are memories or what’s going on now, food is always there. It’s very hard to separate fun from food. The two f’s.” (ID 19, male, age 68 years)
Participants expressed that they gained more awareness about their food choices after their diabetes diagnosis. Participants said they had to think more about portion sizes and carbohydrate content, which often increased their caution and restraint when eating:
“We do eat differently. For instance, on Saturday night, we were out of town, and we were eating with friends. A lot of times, eating out is a lot more difficult because you don’t always know the portion sizes, and it’s hard to count your carbs. I knew I would have a larger meal, and I knew we were going to an Italian restaurant, so I was thinking pasta, bread, carbs. So, throughout the day Saturday, I made sure what I ate was low carb. . . . Sometimes, I sort of feel like, when you’re selecting food, diabetes almost feels like a yield sign or a stop sign to me because it’s always there, and it does make me stop for a bit.” (ID 3, female, age 58 years)
Because they needed to pay more attention to nutritional content, participants said they no longer associated food with celebration or pleasure. In fact, most participants described a negative or ambivalent relationship with food, with many likening it to an enemy or poison. This negative relationship may have contributed to participants’ expressed sense of guilt or personal failure when they indulged in “bad” foods:
“To be honest, I just tell myself that food is a poison for my system. Because it is! It’s just as bad for me as a poison. So, I just say, okay, taste it, maybe, because a little bit of poison won’t kill you [laughing]. But more than that, I just shouldn’t have it.” (ID 16, female, age 66 years)
“It’s made me appreciate that some foods are enemies. . . . I continually have feelings of guilt. The guilt is because I know it’s doing some bad stuff to me. . . . A lot of us know what we ought to be doing, but not so many of us do it. So, there’s a love/hate, or maybe that’s too strong a term, but it’s in that direction. Food is the enemy, but I really like it. There’s a tension there because you know that stuff [bad food] is really dangerous. Literally, it’s dangerous.” (ID 14, male, age 69 years)
Increased awareness, consciousness, and concern about food may have influenced participants’ views of food as less enjoyable. One participant conveyed visible frustration, with restless hands and a raised voice while saying:
“To me, sometimes, if I’m running high blood sugars and I’m feeling discouraged, I find myself getting annoyed that I’m dining with people who can just wolf it down. And to me, I look at it, and I’m thinking numbers, numbers, numbers! What’s my blood sugar? How much did I weigh today? How many carbs are in this? And if I eat this and avoid a piece of bread today, maybe I can have a little dessert today. I don’t enjoy food as much. [It is] too much to think and worry about.” (ID 3, female, age 58 years)
Another participant echoed this sentiment:
“It [food] was used as an enjoyment or a pleasure kind of a thing. I don’t quite see it that way now.” (ID 7, female, age 64 years)
Pressure to eat at social events was prominent and may have contributed to participants’ difficulty following a healthful diet. Some individuals chose to avoid social events and holiday get-togethers so as to not be tempted by food or offend family members and friends who prepared meals. Participants also expressed being annoyed and discouraged, with their hands balled into fists, because they had to think about blood glucose levels and complications, whereas other family members and friends did not:
“Last week, the Jewish community had a Hanukkah party. You could go there and have a meal and buy some stuff to take home. I had originally put it on my calendar because I didn’t visit my family for the holidays. But that night, I decided not to go, and it was mainly because I just got my A1C, and it was 9.7. A year ago, I probably wouldn’t have let it affect me. But I did not go to that event because I did not want to be tempted to have the food that was going to be there or to bring any of it home.” (ID 15, male, age 68 years)
“The only problem is, when you go out to eat or someone invites you over to eat, then [diabetes is] a big problem. I know every time I go to my in-laws, everything on the table is carbs, and you can’t just say, ‘I can’t eat that.’” (ID 19, male, age 58 years)
“Food Is Everywhere; It’s Seducing:” Struggling With Diabetes Management in a Fast-Food Culture
All 19 participants referenced fast food when describing the cultural meaning of food in the United States. Participants described how abundant and readily available food is in American culture. This abundance and availability was widespread in Northern Appalachia:
“[The cultural meaning of food] is big. [It is] every celebration, every excuse to eat. Our friends said that, every month, they come up with some reason to get the whole family together as an excuse to eat. I think the majority of people, even our friends, celebrate with food. . . . Everything revolves around food. That’s American culture.” (ID 1, female, age 77 years)
“Every celebration makes you go out and eat. At work, we eat every day. There are always brownies, fudge, and doughnuts. What do you do when you have a birthday or a holiday or a celebration? You go out and eat. And I don’t have the self-control to just go and have soup or salad.” (ID 9, female, age 50 years)
“It’s fast and very readily available, but it’s not as good for you. I think everyone is in too much of a hurry. Not only the fast-food restaurants, but the supermarkets, too—just grab it and run. (ID 17, female, age 53 years)
Participants felt that the social and celebratory aspect of food, coupled with the perceived fast-food American culture, was in direct conflict with the demands of diabetes. All participants referred to this socio-cultural-personal conflict and the challenge of following a healthful diet in a culture that advertises the opposite in many venues:
“I’m kind of offended by all this advertising that’s continually attacking you, saying, ‘It’s good; it’s convenient; it’s so neat to have it; just have a snack, and it’ll make you feel good.’ I’ve had to change my approach because I’m diabetic. I can’t be seduced by that. I have to be willing to temper my own attraction to food knowing that there are certain consequences that come from that. So how does a diabetic fight all this and try to manage their diabetes? We sit on a teeter-totter. When you look around, you can see that a lot of people are seduced by it because so many people are overweight and obese. . . . There’s stuff that seduces me, and I fall off the wagon. And I eat things I shouldn’t, probably because it tastes so good.” (ID 2, male, age 76 years)
As people living with diabetes, participants noted that they had to exert more willpower toward food compared to the average American:
“As a diabetic, you have to have more willpower and exercise more willpower when it comes to food and other things, too. It doesn’t bother me to look at a tray of desserts, but I know there are a lot of people who can’t do what I do. . . . A lot of people are heavily influenced by advertising. Fast food is a tremendous challenge for people who tend to lean that way anyway.” (ID 4, male, age 68 years)
Several participants felt they were losing this battle to the media and society. These participants did not believe that a change in eating habits was possible for them; however, they wished for change in the younger generations and in people with prediabetes:
“Even with diabetes getting out of control and more people having it, I still don’t think things will change. . . . People are in such a hurry, and people are making tons of money on fast food. That’s just the way culture is now.” (ID 18, male, age 60 years)
“If you can intervene for any group, it should be children. Next, the prediabetic group, who still have a hope of avoiding this. But it’s hard because there are too many contradictory messages coming out in society.” (ID 14, male, age 69 years)
Discussion
This qualitative study explored the meaning of food among adults with type 2 diabetes living in Northern Appalachia. All participants recognized the importance of following a healthful diet in diabetes self-care. They knew that healthful eating was essential for effective management. However, the diagnosis of diabetes changed not only how they approached food, but also what food meant to them. For many of the participants, eating was dictated by time rather than by hunger and pleasure. Furthermore, participants described feeling more aware of food choices, carbohydrate content, and portion sizes after their diabetes diagnosis. Participants also noted that, before their diagnosis of diabetes, the meaning of food was social and celebratory. After their diagnosis, participants felt that food was associated with negative emotions and, for some, a sense of personal failure. Several participants chose to avoid social events and holiday get-togethers so as to not be tempted by food. Finally, they viewed the perceived fast-food American culture as being in direct conflict with the demands of diabetes management. Participants reported struggling to follow a healthful diet in a culture that often advertised the opposite.
For these reasons, patients may benefit from having their health care providers (HCPs) identify and help to shift the existing cultural norms toward health promotion and disease prevention. Liburd (25) notes how this must occur in African-American culture, in which certain social settings contribute to unhealthful food choices for women, and the rituals of eating need to be recreated to emphasize health. HCPs must begin to address both the personal and sociocultural factors that guide the food choices and behaviors of patients with type 2 diabetes.
Our research builds on earlier work exploring perspectives of healthful eating among people in Appalachia (36). Consistent with this previous work, we found that church, family, and the media influenced participants’ meaning of food and perspectives of healthful eating. However, our sample did not discuss economic constraints or social policies (e.g., welfare), as was found in the study by Schoenberg et al. (36). Volunteer bias may partially explain why these factors were not discussed during the interviews; adults with major financial barriers may not have been able to participate because of transportation costs or reluctance to disclose their financial constraints.
Participants in this study reported changes in how and what they are eating; however, these changes were perceived as losses to their social environment. Participants described a sense of deprivation and unfairness, especially as they described not enjoying food as much and having lost a sense of celebration during events where food is served. HCPs are well positioned to give patients the message that having diabetes offers them an opportunity to consider whether they want to start eating more healthfully. This message may provide a teachable moment to educate patients that the average person in the United States is eating unhealthfully and that unhealthful eating patterns are contributing to obesity, heart disease, diabetes, some types of cancer, and other illnesses. Thus, the patient-provider discussion of diabetes can be the impetus for patients to move toward a more healthful eating style and more healthful behaviors.
Patient-provider discussions about behavior change can be reinforced through diabetes education. Diabetes education is an important component of diabetes care for all people with diabetes (58), and ongoing and repeated education is necessary to help people maintain what they learn during initial education (59). The American Diabetes Association (ADA) recommends individualized medical nutrition therapy (MNT) to help patients with diabetes to achieve treatment goals (60). The goals of diabetes nutrition education are to promote healthful eating and achieve glycemic, lipid, and blood pressure targets (60–63). For people with type 2 diabetes, nutrition therapy focuses on reduced caloric intake (63). Unfortunately, only half of diabetes patients receive diabetes education, and even fewer receive education from a dietitian or nutritionist (64).
In this study, none of the participants reported participating in formal diabetes self-management education (DSME) or MNT delivered by a registered dietitian; however, we did not review medical chart data to confirm the reported lack of DSME or MNT.
Previous research shows that diabetes nutrition education interventions result in average A1C reductions of 1–2% (range –0.23 to –2.6%, with reductions dependent on type and duration of diabetes) (60–63). A variety of dietary patterns, including low-carbohydrate, low–glycemic index, Mediterranean, and high-protein diets, have been shown to improve glycemia and reduce cardiovascular risk factors (e.g., lipid profiles, blood pressure, and weight) (65). Thus, diabetes patients can choose from various effective options to take their differing personal, social, and cultural food preferences into account (66).
Although having a variety of dietary options allows for consideration of patients’ food preferences, it also may create a mismatch between nutrition goals and the sociocultural environment (27,67). In the United States, the food industry has created a surplus of accessible, inexpensive, and calorie-dense foods. Peer group pressure and fast-food consumption further compound the dietary challenges faced by diabetes patients (68–70).
For this reason, diabetes patients may require education focusing on problem-solving skills, coping, and risk prevention (71). The ADA Standards of Medical Care in Diabetes recommend culturally relevant content and delivery of DSME (72,73). Current evidence-based MNT recommendations include cultural assessment for an individualized approach to eating patterns (61). Findings from our study may assist DSME and MNT providers in tailoring meal plans for adults with type 2 diabetes living in Northern Appalachia.
When education is provided in a culturally relevant context, the information about diabetes and self-care behaviors becomes more meaningful to individuals (74–77). In addition, education that incorporates scaffolding techniques and brief cognitive behavioral strategies may help participants identify and develop solutions to personal and sociocultural barriers to following a healthful diet (78). Strategies for scaffolding include 1) incorporating participants’ existing knowledge about diabetes and nutrition, 2) offering a motivational context to pique participants’ interest, 3) breaking complex behaviors/tasks into easier and more attainable steps, 4) modeling a behavior/task to participants before asking them to complete the same behavior/task on their own, 5) facilitating active engagement and participation, 6) using graphic organizers to provide a visual framework for assimilating new information, and 7) providing hints or partial solutions to problems or barriers. Finally, numerous psychosocial factors affect how well diabetes patients are able to follow a healthful diet (79–82). Thus, education that acknowledges and addresses the impact of social relationships, as well as depression, distress, and anxiety, on eating may assist patients in integrating effective self-care behaviors.
Limitations
Limitations of this study include homogeneity of the study sample from one city in the Northern Appalachian region of the United States with regard to race/ethnicity, small sample size, participant self-selection, and the use of self-reported data. The all-white study sample is reflective of the racial and ethnic distribution in Northern Appalachia; however, our participants were more educated than the general Northern Appalachia population. The cross-sectional study design limited our ability to detect any causal associations between diabetes diagnosis, changes in the meaning of food, or changes in dietary self-care behaviors. The small sample size and participant self-selection also limited the generalizability of the findings. Self-reported data are vulnerable to social desirability bias. To minimize bias, the researchers informed participants that their responses were confidential and could not be linked back to their personal identity. The researchers also emphasized the voluntary nature of participation and explicitly informed the participants that their responses had no bearing on their diabetes care.
Future research with a larger, more heterogeneous sample should involve the collection of mixed-method data from adults with type 2 diabetes to assess objective measures of diabetes self-care behaviors, glycemic control, and physical and psychosocial changes. Additionally, research is needed to assess how the meaning of food changes over time and at different stages in the life span as well as its impact on self-care, glycemia, and well-being. Finally, the relative importance of these findings depends on a variety of factors including how recently individuals immigrated to the United States, their generational cohort, their degree of acculturation in the United States, and their self-identification as American or as a member of another culture.
Conclusion
For people with type 2 diabetes, healthful food choices and dietary modifications are of great importance to self-management. However, many patients struggle to manage food choices and to change the amount and type of carbohydrates they consume. The demands of diabetes may counter the social and celebratory aspects of eating and contribute to social isolation or promote a kind of anhedonia (reduced ability to experience pleasure) (83). The findings reported here expand the understanding of the meaning of food among adults with type 2 diabetes living in Northern Appalachia. Exploring the meaning of food among type 2 diabetes patients prompts HCPs to consider how patients’ personal and sociocultural beliefs toward food need to be embraced in diabetes education. Diabetes patients need strategies to help balance the demands of diabetes with eating and interpersonal relationships for the rest of their lives.
Acknowledgments
The authors thank the participants who shared their experiences and perceptions for this project.
Funding
This work was supported by the Heritage College of Osteopathic Medicine, National Institutes of Health training grant T32 DK007260, and a Pennsylvania State University College of Health & Human Development Alumni Association research grant.
Duality of Interest
No potential conflicts of interest relevant to this article were reported.
Author Contributions
E.A.B. and M.D.R. researched data, contributed to the discussion, and wrote, reviewed, and edited the manuscript. L.A.W. and C-J.C. contributed to the discussion and reviewed and edited the manuscript. E.S. reviewed and edited the manuscript. E.A.B. is the guarantor of this work and, as such, had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Centers for Disease Control and Prevention. National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States, 2011. Atlanta, Ga., U.S: Department of Health and Human Services, Centers for Disease Control and Prevention, 2014 [Google Scholar]
- 2.Engelgau MM, Geiss LS, Saaddine JB, et al. The evolving diabetes burden in the United States. Ann Intern Med 2004;140:945–950 [DOI] [PubMed] [Google Scholar]
- 3.Caspersen CJ, Thomas GD, Boseman LA, Beckles GL, Albright AL. Aging, diabetes, and the public health system in the United States. Am J Public Health 2012;102:1482–1497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pi-Sunyer FX, Maggio CA, McCarron DA, et al. Multicenter randomized trial of a comprehensive prepared meal program in type 2 diabetes. Diabetes Care 1999;22:191–197 [DOI] [PubMed] [Google Scholar]
- 5.Conn VS, Hafdahl AR, Mehr DR, Lemaster JW, Brown SA, Nielsen PJ. Metabolic effects of interventions to increase exercise in adults with type 2 diabetes. Diabetologia 2007;50:913–921 [DOI] [PubMed] [Google Scholar]
- 6.Maiorana A, O'Driscoll G, Goodman C, Taylor R, Green D. Combined aerobic and resistance exercise improves glycemic control and fitness in type 2 diabetes. Diabetes Res Clin Pract 2002;56:115–123 [DOI] [PubMed] [Google Scholar]
- 7.Karter AJ, Ackerson LM, Darbinian JA, et al. Self-monitoring of blood glucose levels and glycemic control: the Northern California Kaiser Permanente diabetes registry. Am J Med 2001;111:1–9 [DOI] [PubMed] [Google Scholar]
- 8.Jacobson AM, Adler AG, Derby L, Anderson BJ, Wolfsdorf JI. Clinic attendance and glycemic control: study of contrasting groups of patients with IDDM. Diabetes Care 1991;14:599–601 [DOI] [PubMed] [Google Scholar]
- 9.Dyer PH, Lloyd CE, Lancashire RJ, Bain SC, Barnett AH. Factors associated with clinic non-attendance in adults with type 1 diabetes mellitus. Diabet Med 1998;15:339–343 [DOI] [PubMed] [Google Scholar]
- 10.Khan H, Lasker SS, Chowdhury TA. Exploring reasons for very poor glycaemic control in patients with type 2 diabetes. Prim Care Diabetes 2011;5:251–255 [DOI] [PubMed] [Google Scholar]
- 11.Gafarian CT, Heiby EM, Blair P, Singer F. The Diabetes Time Management Questionnaire. Diabetes Educ 1999;25:585–592 [DOI] [PubMed] [Google Scholar]
- 12.Wdowik MJ, Kendall PA, Harris MA. College students with diabetes: using focus groups and interviews to determine psychosocial issues and barriers to control. Diabetes Educ 1997;23:558–562 [DOI] [PubMed] [Google Scholar]
- 13.Rubin RR, Peyrot M. Psychological issues and treatment for people with diabetes. J Clin Psychol 2001;57:457–478 [DOI] [PubMed] [Google Scholar]
- 14.Nelson KM, Reiber G, Boyko EJ. Diet and exercise among adults with type 2 diabetes: findings from the Third National Health and Nutrition Examination Survey (NHANES III). Diabetes Care 2002;25:1722–1728 [DOI] [PubMed] [Google Scholar]
- 15.Neuhouser ML, Miller DL, Kristal AR, Barnett MJ, Cheskin LJ. Diet and exercise habits of patients with diabetes, dyslipidemia, cardiovascular disease or hypertension. J Am Coll Nutr 2002;21:394–401 [DOI] [PubMed] [Google Scholar]
- 16.Oza-Frank R, Cheng YJ, Narayan KM, Gregg EW. Trends in nutrient intake among adults with diabetes in the United States: 1988–2004. J Am Diet Assoc 2009;109:1173–1178 [DOI] [PubMed] [Google Scholar]
- 17.Vitolins MZ, Anderson AM, Delahanty L, et al. Action for Health in Diabetes (Look AHEAD) trial: baseline evaluation of selected nutrients and food group intake. J Am Diet Assoc 2009;109:1367–1375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Delahanty LM, Halford BN. The role of diet behaviors in achieving improved glycemic control in intensively treated patients in the Diabetes Control and Complications Trial. Diabetes Care 1993;16:1453–1458 [DOI] [PubMed] [Google Scholar]
- 19.Vijan S, Stuart NS, Fitzgerald JT, et al. Barriers to following dietary recommendations in type 2 diabetes. Diabet Med 2005;22:32–38 [DOI] [PubMed] [Google Scholar]
- 20.Nagelkerk J, Reick K, Meengs L. Perceived barriers and effective strategies to diabetes self-management. J Adv Nurs 2006;54:151–158 [DOI] [PubMed] [Google Scholar]
- 21.Schlundt DG, Hargreaves MK, Buchowski MS. The Eating Behavior Patterns Questionnaire predicts dietary fat intake in African American women. J Am Diet Assoc 2003;103:338–345 [DOI] [PubMed] [Google Scholar]
- 22.Marcy TR, Britton ML, Harrison D. Identification of barriers to appropriate dietary behavior in low-income patients with type 2 diabetes mellitus. Diabetes Ther 2011;2:9–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Massachusetts Department of Education. Special nutrition needs of older adults. In Nutrition Resource Manual for Adult Day Health Programs. Boston, Mass., Massachusetts Department of Education, 2006, p. 35–60 [Google Scholar]
- 24.Kirkman MS, Briscoe VJ, Clark N, et al. Diabetes in older adults. Diabetes Care 2012;35:2650–2664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liburd LC. Food, identity, and African-American women with type 2 diabetes: an anthropological perspective. Diabetes Spectr 2003;16:160–165 [Google Scholar]
- 26.Wong OL. Meaning of food in childhood obesity: an exploratory study in a Chinese family context. Soc Work Health Care 2010;49:362–377 [DOI] [PubMed] [Google Scholar]
- 27.Rozin P. The meaning of food in our lives: a cross-cultural perspective on eating and well-being. J Nutr Educ Behav 2005;37(Suppl. 2):S107–S112 [DOI] [PubMed] [Google Scholar]
- 28.Falk LW, Bisogni CA, Sobal J. Food choice processes of older adults: a qualitative investigation. J Nutr Educ 1996;28:257–265 [Google Scholar]
- 29.Bisogni CA, Falk LW, Madore E, et al. Dimensions of everyday eating and drinking episodes. Appetite 2007;48:218–231 [DOI] [PubMed] [Google Scholar]
- 30.Bisogni CA, Jastran M, Shen L, Devine CM. A biographical study of food choice capacity: standards, circumstances, and food management skills. J Nutr Educ Behav 2005;37:284–291 [DOI] [PubMed] [Google Scholar]
- 31.Furst T, Connors M, Bisogni CA, Sobal J, Falk LW. Food choice: a conceptual model of the process. Appetite 1996;26:247–265 [DOI] [PubMed] [Google Scholar]
- 32.Rozin P, Fischler C, Imada S, Sarubin A, Wrzesniewski A. Attitudes to food and the role of food in life in the USA, Japan, Flemish Belgium and France: possible implications for the diet-health debate. Appetite 1999;33:163–180 [DOI] [PubMed] [Google Scholar]
- 33.Sobal J, Bisogni CA. Constructing food choice decisions. Ann Behav Med 2009;38(Suppl. 1):S37–S46 [DOI] [PubMed] [Google Scholar]
- 34.Jastran MM, Bisogni CA, Sobal J, Blake C, Devine CM. Eating routines: embedded, value based, modifiable, and reflective. Appetite 2009;52:127–136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jacobsson A, Pihl E, Martensson J, Fridlund B. Emotions, the meaning of food and heart failure: a grounded theory study. J Adv Nurs 2004;46:514–522 [DOI] [PubMed] [Google Scholar]
- 36.Schoenberg NE, Howell BM, Swanson M, Grosh C, Bardach S. Perspectives on healthy eating among Appalachian residents. J Rural Health 2013;29(Suppl. 1)S25–S34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Appalachian Regional Commission The Appalachian region [Internet]. Available from http://www.arc.gov/appalachian_region/TheAppalachianRegion.asp. Accessed 3 August 2016
- 38.Ohio University Voinovich Center for Leaders h: ip and Public Affairs , Appalachian Rural Health Institute: Chronic Conditions Prevalence and Risk Needs Assessment: Study Area II. Athens, Ohio, Ohio University, 2006 [Google Scholar]
- 39.Coyne CA, Demian-Popescu C, Friend D. Social and cultural factors influencing health in southern West Virginia: a qualitative study. Prev Chronic Dis 2006;3:A124 [PMC free article] [PubMed] [Google Scholar]
- 40.Jesse DE, Reed PG. Effects of spirituality and psychosocial well-being on health risk behaviors in Appalachian pregnant women. J Obstet Gynecol Neonatal Nurs 2004;33:739–747 [DOI] [PubMed] [Google Scholar]
- 41.McGarvey EL, Leon-Verdin M, Killos LF, Guterbock T, Cohn WF. Health disparities between Appalachian and non-Appalachian counties in Virginia USA. J Community Health 2011;36:348–356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Deskins S, Harris CV, Bradlyn AS, et al. Preventive care in Appalachia: use of the theory of planned behavior to identify barriers to participation in cholesterol screenings among West Virginians. J Rural Health 2006;22:367–374 [DOI] [PubMed] [Google Scholar]
- 43.Lohri-Posey B. Middle-aged Appalachians living with diabetes mellitus: a family affair. Fam Community Health 2006;29:214–220 [DOI] [PubMed] [Google Scholar]
- 44.McMillan SJ, Haley E, Zollman-Huggler P, Johnson Avery E, Winchenbach MG, Bell JL. Breast health education for working women in Appalachia: insights from focus group research. Cancer Control 2007;14:265–276 [DOI] [PubMed] [Google Scholar]
- 45.Denham SA. Part I: The definition and practice of family health. J Fam Nurs 1999;5:133–159 [Google Scholar]
- 46.Schwartz F, Ruhil AV, Denham S, Shubrook J, Simpson C, Boyd SL. High self-reported prevalence of diabetes mellitus, heart disease, and stroke in 11 counties of rural Appalachian Ohio. J Rural Health 2009;25:226–230 [DOI] [PubMed] [Google Scholar]
- 47.Centers for Disease Control and Prevention Diagnosed diabetes [Internet]. Available from http://gis.cdc.gov/grasp/diabetes/DiabetesAtlas.html. Accessed 3 August 2016
- 48.Centers for Disease Control and Prevention Diabetes: county data indicators. Available from http://www.cdc.gov/diabetes/data/countydata/countydataindicators.html. Accessed 3 August 2016
- 49.Morse J, Field P. Nursing Research: The Application of Qualitative Approaches. 2nd ed. London, England, Chapman and Hall, 1996 [Google Scholar]
- 50.Morse JM, Field PA. Qualitative Research Methods for Health Professionals. 2nd ed. Thousand Oaks, Calif., Sage Publications, 1995 [Google Scholar]
- 51.Speziale HJ, Carpenter DR. Qualitative Research in Nursing: Advancing the Humanistic Imperative. Philadelphia, Pa., Lippincott, Williams, & Wilkins, 2003 [Google Scholar]
- 52.Roper JM, Shapira J. Ethnography in Nursing Research. Thousand Oaks, Calif., Sage Publications, 2000 [Google Scholar]
- 53.Spradley JP. The Ethnographic Interview. New York, N.Y., Holt, Rinehart, & Winston, 1979 [Google Scholar]
- 54.Miles MB, Huberman AM. Qualitative Data Analysis: An Expanded Sourcebook. 2nd ed. Thousand Oaks, Calif, Sage Publications, 1994 [Google Scholar]
- 55.Denzin N. The Research Act: A Theoretical Introduction to Sociological Methods. 2nd ed. New York, N.Y., McGraw-Hill, 1978 [Google Scholar]
- 56.Lincoln Y, Guba E. Naturalistic Inquiry. Newbury Park, Calif, Sage Publications, 1985 [Google Scholar]
- 57.Russell CK, Gregory DM. Evaluation of qualitative research studies. Evid Based Nurs 2003;6:36–40 [DOI] [PubMed] [Google Scholar]
- 58.Ismail K, Winkley K, Rabe-Hesketh S. Systematic review and meta-analysis of randomised controlled trials of psychological interventions to improve glycaemic control in patients with type 2 diabetes. Lancet 2004;363:1589–1597 [DOI] [PubMed] [Google Scholar]
- 59.Beverly EA, Fitzgerald SM, Brooks KM, et al. Impact of reinforcement of diabetes self-care on poorly controlled diabetes: a randomized controlled trial. Diabetes Educ 2013;39:504–514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Evert AB, Boucher JL, Cypress M, et al. Nutrition therapy recommendations for the management of adults with diabetes. Diabetes Care 2013;36:3821–3842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Franz MJ, Boucher JL, Evert AB. Evidence-based diabetes nutrition therapy recommendations are effective: the key is individualization. Diabetes Metab Syndr Obes 2014;7:65–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Franz MJ, Boucher JL, Green-Pastors J, Powers MA. Evidence-based nutrition practice guidelines for diabetes and scope and standards of practice. J Am Diet Assoc 2008;108(Suppl. 1):S52–S58 [DOI] [PubMed] [Google Scholar]
- 63.Franz MJ, Powers MA, Leontos C, et al. The evidence for medical nutrition therapy for type 1 and type 2 diabetes in adults. J Am Diet Assoc 2010;110:1852–1889 [DOI] [PubMed] [Google Scholar]
- 64.Ali MK, Bullard KM, Gregg EW. Achievement of goals in U.S. diabetes care, 1999–2010. N Engl J Med 2013;369:287–288 [DOI] [PubMed] [Google Scholar]
- 65.Ajala O, English P, Pinkney J. Systematic review and meta-analysis of different dietary approaches to the management of type 2 diabetes. Am J Clin Nutr 2013;97:505–516 [DOI] [PubMed] [Google Scholar]
- 66.Ley SH, Hamdy O, Mohan V, Hu FB. Prevention and management of type 2 diabetes: dietary components and nutritional strategies. Lancet 2014;383:1999–2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Basu S, Stuckler D, McKee M, Galea G. Nutritional determinants of worldwide diabetes: an econometric study of food markets and diabetes prevalence in 173 countries. Public Health Nutr 2013;16:179–186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med 2007;357:370–379 [DOI] [PubMed] [Google Scholar]
- 69.Trogdon JG, Nonnemaker J, Pais J. Peer effects in adolescent overweight. J Health Econ 2008;27:1388–1399 [DOI] [PubMed] [Google Scholar]
- 70.Fortin B, Yazbeck M. Peer effects, fast food consumption and adolescent weight gain. J Health Econ 2015;42:125–138 [DOI] [PubMed] [Google Scholar]
- 71.Weinger K, Beverly EA, Smaldone A. Diabetes self-care and the older adult. West J Nurs Res 2014;36:1272–1298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.American Diabetes Association Standards of medical care in diabetes—2015: summary of revisions. Diabetes Care 2015;38(Suppl. 1):S4 [Google Scholar]
- 73.American Diabetes Association Standards of Medical Care in Diabetes— 2015: abridged for primary care providers. Clin Diabetes 2015;33:97–111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kreuter MW, Lukwago SN, Bucholtz RD, Clark EM, Sanders-Thompson V. Achieving cultural appropriateness in health promotion programs: targeted and tailored approaches. Health Educ Behav 2003;30:133–146 [DOI] [PubMed] [Google Scholar]
- 75.Kumanyika SK. Cultural appropriateness: working our way toward a practicable framework. Health Educ Behav 2003;30:147–150 [DOI] [PubMed] [Google Scholar]
- 76.Sowattanangoon N, Kotchabhakdi N, Petrie KJ. The influence of Thai culture on diabetes perceptions and management. Diabetes Res Clin Pract 2009;84:245–251 [DOI] [PubMed] [Google Scholar]
- 77.Finucane ML, McMullen CK. Making diabetes self-management education culturally relevant for Filipino Americans in Hawaii. Diabetes Educ 2008;34:841–853 [DOI] [PubMed] [Google Scholar]
- 78.Weinger K, Beverly EA, Lee Y, Sitnokov L, Ganda OP, Caballero AE. The effect of a structured behavioral intervention on poorly controlled diabetes: a randomized controlled trial. Arch Intern Med 2011;171:1990–1999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Lai JS, Hiles S, Bisquera A, Hure AJ, McEvoy M, Attia J. A systematic review and meta-analysis of dietary patterns and depression in community-dwelling adults. Am J Clin Nutr 2014;99:181–197 [DOI] [PubMed] [Google Scholar]
- 80.Dipnall JF, Pasco JA, Meyer D, et al. The association between dietary patterns, diabetes and depression. J Affect Disord 2015;174:215–224 [DOI] [PubMed] [Google Scholar]
- 81.Silverman J, Krieger J, Kiefer M, Hebert P, Robinson J, Nelson K. The relationship between food insecurity and depression, diabetes distress and medication adherence among low-income patients with poorly-controlled diabetes. J Gen Intern Med 2015;30:1476–1480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Raymond KL, Lovell GP. Food addiction symptomology, impulsivity, mood, and body mass index in people with type two diabetes. Appetite 2015;95:383–389 [DOI] [PubMed] [Google Scholar]
- 83.Ribot T. The Psychology of Emotions. London, England, W. Scott, 1897 [Google Scholar]