Abstract
Purpose.
The purpose of this study was to compare achievement of glycemic control on insulin drips before and after the implementation of EndoTool, a glucose management software system used in a community hospital setting.
Methods.
A retrospective chart review was performed of patients on an insulin drip who were managed before and after implementation of the EndoTool software. Fifty patients were selected for each group. Statistical analyses were run to compare metrics gathered between groups.
Results.
Patients in the standard care group were on an insulin drip for an average of 23.9 hours compared to 20.9 hours in the EndoTool group (P = 0.38). Hypoglycemia occurred at an average rate of 0.036 events per patient in the standard group and 0.007 events per patient in the EndoTool group (P = 0.17). The average rate of hyperglycemia was 0.358 events per patient in the standard group and 0.283 events per patient in the EndoTool group (P = 0.25). The average time to achieve the blood glucose target was 2.78 and 3.67 hours in the standard and EndoTool groups, respectively (P = 0.27). Total patient values were within target range 45.2% of the time in the standard care group and 47.3% of the time in the EndoTool group (P = 0.71).
Conclusion.
Analysis of the implementation of EndoTool in the community hospital setting found no statistically significant differences between groups, although rates of hypo- and hyperglycemia showed a trend toward improved safety in the EndoTool group. These results could be attributed to the conservative parameters the hospital set in the initial phase of EndoTool implementation.
Hospitalized patients with persistent, worsening, and highly variable hyperglycemia experience significantly increased intensive care unit (ICU) stays, more days on a ventilator, increased rates of infection, and increased mortality rates compared to patients with controlled glucose levels (1–3). The Centers for Medicare & Medicaid Services considers “manifestations of poor management of blood glucose levels” to be a hospital-acquired condition and will not pay for complications that arise from blood glucose fluctuations (4).
The EndoTool software system (Monarch Medical Technologies, Charlotte, N.C.) has been found to reduce hyperglycemia episodes by 45–57% (P <0.0001) (5). EndoTool is a computer software system that replaces standard paper protocols for dosing and titrating insulin drips for patients with hyperglycemia, diabetic ketoacidosis (DKA), and hyperosmolar hyperglycemic state (HHS). Instead of simply adjusting insulin rates based on blood glucose levels, the system takes into account a variety of factors, including a patient’s diabetes status, weight, steroid dosing, renal function, indication for insulin, response to insulin, and estimated residual extracellular insulin (an unpublished algorithm developed by EndoTool that predicts the amount of residual extracellular insulin circulating in a patient’s bloodstream). The software allows an insulin drip to be adjusted to prevent hypoglycemia before a paper chart might show that a patient’s glucose level is trending toward hypoglycemia. Studies have shown that, compared to patients with standard paper protocols, those managed with EndoTool have had a 95% reduction in serious hypoglycemic episodes (defined as blood glucose <40 mg/dL) (5,6).
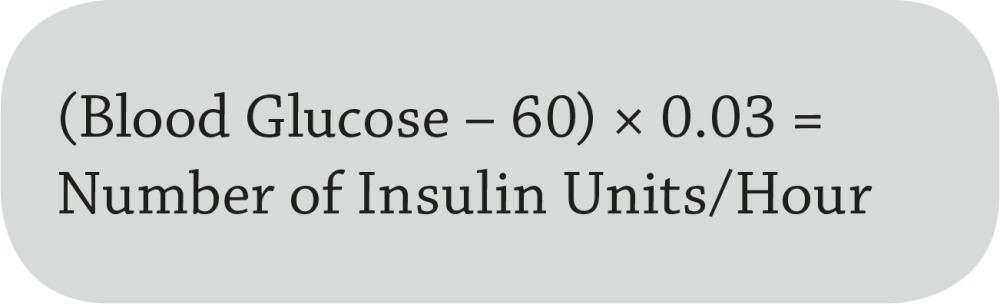
Based on blood glucose alone, our institution previously used a paper protocol and Eq. 1 to determine patients’ initial insulin rate. Blood glucose values were obtained by manual fingerstick tests performed by a nurse at bedside. The nurse checked a patient’s blood glucose every hour initially and then calculated insulin drip rates by hand at bedside, which left room for calculation errors. The multiplier was increased or decreased every hour depending on whether the patient’s blood glucose was above or below the target range. Blood glucose monitoring could only be decreased to every 2 hours after blood glucose was within the target range for three consecutive readings. A physician then had to write orders to discontinue the insulin drip.
 |
As an alternative to such paper protocols, computer-guided glucose management systems are now starting to be used to improve glucose management by reducing insulin infusion calculation errors and standardizing therapy (7). EndoTool is one such system. EndoTool is advertised to help patients reach target glucose ranges faster and to reduce episodes of hypo- and hyperglycemia by determining an optimal initial insulin dose based on patients’ known characteristics and condition. However, specific details about how this software works have not been published.
An additional advertised benefit of EndoTool is its ease of use. When a user (e.g., a nurse, pharmacist, or physician) logs on, the system automatically displays the patients on that user’s unit who are on an insulin drip. The system also alerts the nurse when each patient’s next blood glucose check is due. When a patient’s blood glucose is checked and entered into the software, the system then performs a calculation based on its proprietary algorithm and notifies the nurse if an adjustment in the patient’s insulin rate is needed. In an efficacy study, use of EndoTool resulted in a 46% decrease in the total number of blood glucose measurements taken each month and an overall reduction in the total number of minutes spent by nurses dealing with glucose control issues (6).
The cycle of monitoring blood glucose and adjusting insulin rates via EndoTool continues until a patient is deemed stable based on parameters set by a panel of the hospital’s clinicians. Once a patient has maintained consistent glucose levels around a set average for the requisite time period, the software displays a stable message. At this point, the system can be configured to provide transition orders for subcutaneous insulin dosing. The nurse is prompted to give a dose of long-acting insulin 2 hours before discontinuing the drip. The insulin infusion can then be discontinued safely without waiting for orders from a physician.
Studies comparing EndoTool to standard paper protocols showed that patients reached blood glucose targets faster with the software than with a paper protocol and that blood glucose remained within the target range as much as 97.25% of the time after control was achieved via the software (8). These results allow patients to come off of an insulin drip sooner and thereby decreases lengths of stay and rates of infection and mortality.
The purpose of this preliminary study was to analyze the effects of implementing this computer-guided glucose management system and to evaluate its effect on patient outcomes at our institution.
Design and Methods
Site and Background
The study site was a 553-bed, not-for-profit health care network providing a wide array of services, including a cardiovascular intensive care unit, a progressive care unit, a traditional intensive care unit, and a level II trauma center emergency department. A study evaluating the software with postoperative cardiovascular patients had been published in 2009 (9). Therefore, our health system implemented the software system in August 2015, starting with the cardiovascular intensive care unit and expanding to the intensive care unit, progressive care unit, and finally the emergency department.
In our hospital system, physicians order insulin drips from protocols for DKA, HHS, hyperglycemia, or as needed for post-operative cardiovascular patients. A nurse then initiates the EndoTool software and inputs the patient’s characteristics. Patients on insulin drips are usually on NPO (nothing by mouth) status because they are either ICU patients with hyperglycemia (on total parenteral nutrition or tube feedings), postoperative cardiovascular surgery patients, or patients with DKA or HHS. A carbohydrate-controlled or “diabetic clear liquid” diet can be ordered, but this is usually after their hyperglycemia has resolved and they are about to come off of the insulin drip. Mealtime insulin is calculated along with bolus doses once patients are ready for transition off of the insulin drip. The software system makes recommendations for this based on patients’ total daily insulin needs. These data were not collected in our study.
Primary Outcome
Because EndoTool is advertised to reduce patients’ time on insulin drips, our primary outcome was total patient days on an insulin drip using the software versus our standard paper protocol. With the paper protocol, insulin drips were discontinued by an order from the physician when a patient was deemed stable. With the software, insulin drips were discontinued by a nurse when the software displayed the “Stable” message based on the software algorithm.
The software system provides recommended settings based on what many other hospitals use. However, each hospital can choose its own settings based on its previous protocols. For this study, the software settings were as follows:
For HHS or hyperglycemia, the stable message appears for the nurse to transition the patient from the insulin drip when average blood glucose has been ≤160 mg/dL for the past 2.5 hours with no more than a 25 mg/dL fluctuation in the readings.
For DKA, the stable message first appears when a patient’s blood glucose is ≤250 mg/dL, at which point the software automatically transitions into “standard mode.” The nurse then ensures that the anion gap is ≤12 mEq/L, after which intravenous fluids are changed from NaCl 0.9% or NaCl 0.45% to a dextrose-containing solution. A second stable message appears when the patient’s average blood glucose has been ≤160 mg/dL with the same parameters as with HHS or hyperglycemia.
Secondary Outcomes
To evaluate safety, our secondary outcomes included rates of hypo- and hyperglycemia, time to achievement of target blood glucose, and rates of patients remaining within their target range once it was reached. Target ranges were the same for the standard paper protocol and software groups and were individualized based on patients’ indication for insulin drip (Table 1).
TABLE 1.
Blood Glucose Target Ranges
| Blood Glucose Range (mg/dL) | |
|---|---|
| Cardiovascular surgery | 100–150 |
| DKA or HHS | 100–150 |
| Critical care/sepsis (not in DKA) | 120–180 |
| Women’s Pavilion patients | 70–100 |
| Hyperglycemia, DKA, or HHS treated in the emergency department | 100–150 |
Data Collection
This was a single-center, retrospective chart review study that was approved by the hospital’s institutional review board. All patients who were placed on an insulin drip during the 10-month timeframe were eligible for inclusion. Patients who were transferred to another facility or who were on an insulin drip without following either the paper or the EndoTool protocol were excluded.
We collected data on randomly selected patients for the standard group from 1 March 2015 (5 months before implementation of the software system) to 31 July 2015. We collected data on randomly selected patients for the EndoTool group from 1 August 2015 to 31 December 2015 (5 months after the implementation of the software system).
Patients were randomized using block randomization. To account for the change in time as the protocol was rolled out, we randomly selected 10 patients each month. A random number generator was used to select a sample of patients. This resulted in 100 patients for purposes of analysis. Also, for the purpose of this study, we used our hospital’s definitions of hypoglycemia (any blood glucose <70 mg/dL) and hyperglycemia (any blood glucose >180 mg/dL).
Statistical Analysis
To analyze baseline characteristics between the two groups, we used a Student’s t test for ordinal data and a χ2 test for nominal data. Student’s t tests were also used to analyze primary and secondary endpoints. Statistical analyses were performed using SAS University Edition (SAS Institute, Cary, N.C.).
Results
Baseline Characteristics
There were no statistically significant differences in the baseline characteristics of the two groups, as summarized in Table 2.
TABLE 2.
Baseline Characteristics
| Standard Group | EndoTool Group | P | |
|---|---|---|---|
| Age (years; mean [SD]) | 57 (21–83) | 56 (18–103) | 0.88 |
| Sex (n [%]) | Female 23 (46) | Female 27 (54) | 0.55 |
| Male 27 (54) | Male 23 (46) | ||
| Weight (kg) | 86.58 | 78.14 | 0.06 |
| Height (inches) | 67.6 | 67.1 | 0.52 |
| Mean BMI (kg/m2) | 29.02 | 26.89 | * |
| Mean A1C (%) | 9.74 | 9.99 | 0.86 |
| Hospital units (n [%]) | 0.94 | ||
| Emergency department | 6 (12) | 5 (10) | |
| ICU | 10 (20) | 12 (24) | |
| Cardiovascular ICU | 24 (48) | 20 (40) | |
| Progressive care unit | 10 (20) | 13 (26) | |
| Diabetes status (n [%]) | * | ||
| Type 1 | 8 (16) | 8 (16) | |
| Type 2 | 25 (50) | 23 (48) | |
| Prediabetes | 10 (20) | 17 (34) | |
| No diabetes | 7 (14) | 2 (4) | |
| Indication for insulin (n [%]) | * | ||
| DKA | 18 (36) | 21 (42) | |
| HHS | 3 (6) | 4 (8) | |
| Cardiovascular surgery | 24 (48) | 23 (46) | |
| Hyperglycemia | 5 (10) | 2 (4) |
Statistical analysis of P values was not performed.
Time on Insulin Drip
Findings for the primary outcome are shown in Table 3. The average time on an insulin drip for patients whose insulin rates were titrated using the standard paper protocol was 23.9 hours, compared to 20.9 hours in the EndoTool group. The average blood glucose value for patients in the standard group while on the drip was 193.34 mg/dL, compared to 186.49 mg/dL in the EndoTool group. These differences were not statistically significant.
TABLE 3.
Primary Outcome
| Standard Group | EndoTool Group | P | |
|---|---|---|---|
| Time on insulin drip (hours; mean [SD]) | 23.9 (2.0–109.5) | 20.9 (4.8-87.5) | 0.38 |
Safety Outcomes
Findings for the secondary outcomes are summarized in Table 4. In the standard protocol group, the hypoglycemia rate for all blood glucose readings taken while on an insulin drip was 0.036 events per patient, compared to 0.007 events per patient in the EndoTool group. This 80.6% relative risk (RR) reduction was not statistically significant.
TABLE 4.
Secondary Outcomes
| Standard Group | EndoTool Group | RR (%) | P | |
|---|---|---|---|---|
| Rate of hypoglycemia while on insulin drip (mean [range]) | 0.036 (0–1) | 0.007 (0–0.2) | –80.6 | 0.17 |
| Rate of hyperglycemia while on insulin drip (mean [range]) | 0.358 (0–1) | 0.283 (0–1) | –20.9 | 0.25 |
| Time to achieve target blood glucose (hours; mean [range]) | 2.78 (0–16) | 3.67 (0–16) | +32.0 | 0.27 |
| Values within target blood glucose range (mean [range]) | 0.452 (0–1) | 0.473 (0–1) | +4.6 | 0.71 |
| Rate of blood glucose monitoring/hour (mean [range]) | 1.45 (0.60–1.95) | 1.18 (0.91–2.00) | –18.6 | * |
Statistical analysis of P value not performed.
Two patients in the standard protocol group and no patients in the EndoTool group experienced severe hypoglycemia (blood glucose <40 mg/dL).
In the standard group, the average rate of hyperglycemia of all blood glucose readings taken of patients while on an insulin drip was 0.358 events per patient, compared to 0.283 events per patient in the EndoTool group. This 20.9% reduction in RR was not statistically significant.
The average time to achieve target blood glucose was 2.78 hours in the standard group and 3.67 hours in the EndoTool group. This time difference was not statistically significant.
Blood glucose values were in the physician’s set target range during insulin drip 45.2% of the time for patients in the standard group, compared to 47.3% of the time for those in the EndoTool group. This difference also was not statistically significant.
Discussion
We found that the EndoTool did reduce time on insulin drip by 3 hours, but this reduction was not statistically significant. Although this reduction may not seem clinically significant, it can be expected to reduce both costs for pharmacy services and time from a nursing perspective. We attribute the nonsignificance of this finding to parameters being set too conservatively by the study site’s EndoTool panel of clinicians when the software was first being rolled out. Although these parameters were not adjusted during the study period, there are plans to adjust them moving forward.
With regard to secondary outcomes, although none were statistically significant, we found a trend toward reduction in the rates of both hypo- and hyperglycemia in the EndoTool group, suggesting improvement in safety from implementation of the software. There was also an increase in the rate of blood glucose values within the target range for patients in the EndoTool group. Finally, we saw an increase in the time needed to achieve glucose levels in the target range. We believe this was also the result of conservative parameters initially set for EndoTool at this hospital.
Limitations of our study include its small sample study and retrospective chart review design. We also did not calculate power for these data because this was a preliminary study. A possibly confounding factor is that certain units in the hospital began using EndoTool at different times, and subgroups based on this timing difference were not analyzed. It is also possible that physicians in some cases discontinued insulin drips before a stable message was received from the software, which could have resulted in skewed results. Another limitation was that data collected from electronic health records in each group may have shown insulin drips being discontinued before or after they were actually discontinued.
Conclusion
Based on this study, EndoTool is being used appropriately to promote a culture of safety at our institution. We expect that, with time and adjustment of conservative to more stringent parameters, we will see patients on insulin drips for shorter periods of time and with higher rates of blood glucose within designated target ranges.
Duality of Interest
No potential conflicts of interest relevant to this article were reported.
Author Contributions
S.M.J. researched data, contributed to discussion, and wrote, reviewed, and edited the manuscript. K.L.W. and K.J. researched data, contributed to the discussion, and reviewed and edited the manuscript. S.M.J. is the guarantor of this work and, as such, had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.van den Berghe G, Woouters P, Weekers F, et al. . Intensive insulin therapy in critically ill patients. N Engl J Med 2001;345:1359–1367 [DOI] [PubMed] [Google Scholar]
- 2.Umpierrez GE, Isaacs SD, Bazargan N, You X, Thaler LM, Kitabchi AE. Hyperglycemia: an independent marker of in-hospital mortality in patients with undiagnosed diabetes. J Clin Endocrinol Metab 2002;87:978–982 [DOI] [PubMed] [Google Scholar]
- 3.Bochicchio GV, Sung J, Joshi M, et al. . Persistent hyperglycemia is predictive of outcome in critically ill trauma patients. J Trauma 2005;58:921–924 [DOI] [PubMed] [Google Scholar]
- 4.Centers for Medicare & Medicaid Services Hospital-acquired conditions (HAC) and present on admission indicator reporting provision [Internet]. Available from https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/wPOA-Fact-Sheet.pdf. Accessed 10 October 2017
- 5.Fogel SL, Baker CC. Effects of computerized decision support systems on blood glucose regulation in critically ill surgical patients. J Am Coll Surg 2013;216:828–833 [DOI] [PubMed] [Google Scholar]
- 6.Juneja R, Roudebush CP, Nasraway SA, et al. . Computerized intensive insulin dosing can mitigate hypoglycemia and achieve tight glycemic control when glucose measurement is performed frequently and on time. Crit Care 2009;13:R163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Crockett SE. Glucose control in the critically ill patient utilizing computerized intravenous insulin dosing. US Endocrinol 2009;5:45–48 [Google Scholar]
- 8.Monarch Medical Technologies Private investment firm Eigen Capital unveils Monarch Medical Technologies, new corporate entity behind market-leading EndoTool™ solution [Internet]. Available from https://monarchmedtech.com/blog/privateinvestment-firmeigencapitalunveilsmonarchmedicaltechnologies-newcorporateentitybehindmarket-leadingendotool-solution. Accessed 19 December 2016
- 9.Harris C, Green D. Guardian of glucose: consider using an electronic algorithm to achieve postcardiac surgery glycemic control. Nurs Manage 2009;40:18–20, 22 [DOI] [PubMed] [Google Scholar]


