Introduction
Ecosystem Goods and Services (EGS) are the outputs of ecological processes that directly or indirectly contribute to social welfare (Munns et al 2015). One of the key uncertainties limiting the protection of EGS is the limited knowledge of how they may relate to human health (Corvalan et al. 2005). Since the Millennium Ecosystem Assessment (MEA 2005), there has been increasing interest in addressing this information gap, and an upsurge in the number of studies on the subject (Hartig et al 2014).
The emerging body of literature relating EGS to human health has been compiled in over fifty review articles (Hartig et al 2014), and captured in interactive tools, such as the US-EPA’s Eco-Health Relationship Browser (Jackson et al. 2013). Although these compilations highlight empirical evidence, the references to date do not necessarily support causality, but rather focus on establishing plausible associations (Jackson et al 2013). Moreover, the field is dominated by observational research and there is a dearth of primary studies to establish causal associations between EGS and health in a consistent and rigorous manner (Hartig et al 2014).
Notably, there are few studies directly linking the presence of ecosystems to physical health and disease by means of buffering EGS. Buffering EGS refers to the ecosystem’s capacity to “buffer” against health impacts by, for example, removing pollutants from air and water, and mitigating heat and water hazards (Jackson et al 2013). Most existing research links disease to intermediate processes (e.g. air pollution, floods), which may be attributed to anthropogenic impacts and not necessarily to buffering EGS by ecosystems. Given that the ecosystem is the operable management unit in the conservation of buffering EGS for human health, a lack of empirical evidence supporting a direct association could undermine the effectiveness (and public support) of conservation plans. There are few papers tracing the full pathways from ecosystem, to EGS processes, to health outcomes, which further limits our ability to demonstrate causality (Hartig et al. 2014).
One solution to these limitations is the collective analysis of existing Eco-Health literature using Causal Criteria Analysis (CSA). CSA emerged in the field of epidemiology due to the need for decision making based on relatively weak independent pieces of evidence (Weed 1997). Bradford Hill’s criteria represent the most widely used guide for assessing causality, and consist of standards, summarized by Russo and Williamson (2007), into two categories: 1) Probabilistic evidence, or consistent cause-effect association; and 2) Mechanistic evidence, or a logical explanation of how the causal association occurs. Norris et al. (2011) subsequently applied causality criteria to develop a framework for assessing cause-effect relationships in environmental research. The premise is that isolated studies may not offer a strong case for causality, but they may do so if considered collectively.
We focus our CSA on the context of Green Spaces, its effects on buffering EGS, and the impact of these on human diseases. We address the following questions: i) which linkages are theoretically plausible but need further research, ii) which diseases have been associated directly with presence/absence of Green Spaces, and iii) which Eco-Health linkages are best supported and should be considered for management. Addressing these questions will better characterize the current state of knowledge, define management priorities, and identify pending Eco-Health research topics.
Methods
To conduct our CSA, we applied a numerical technique that combines individual studies, weighted by research design, into a single score for or against a given hypothesis (Norris et al. 2011, Table 1). This method helps determine whether the composite of existing research supports the cause and effect relationship, or suggests inconsistent evidence, or support for an alternative hypothesis. This approach differs from meta-analysis as it is not meant to measure effect sizes. Instead it helps determine the evidence for a given causal linkage. It also allows consideration of studies that do not report summary statistics, which are needed for quantitative reviews (Norris et al 2011). This method represents an alternative to narrative reviews as it allows for succinct literature synthesis and a systematic assessment of relative weight of evidence (Norris et al 2011). This approach has been incorporated into an online tool called Eco-Evidence, summarized here in four sections: context definition; cause and effect mechanism; literature review; and weighting the evidence (Webb et al 2015).
Table 1.
Factors considered and weight of evidence scores for causal criteria analysis (modified from Norris et al. 2011)
| Factors Considered | Weight Applied |
|---|---|
| Study design type | |
| BACI or BARI MBACI* | 4 |
| Gradient response model | 3 |
| Before v. after (no reference/control) | 2 |
| Reference v. control (no before) | 2 |
| After impact only | 1 |
| Number of independent control locations | |
| 0 | 0 |
| 1 | 2 |
| 1+ | 3 |
| Number of independent impact locations | |
| 1 | 0 |
| 2 | 2 |
| 2+ | 3 |
| Locations for gradient response model | |
| 3 | 0 |
| 4 | 2 |
| 5 | 4 |
| 5+ | 6 |
BACI: Before-After-Control-Impact; BARI: Before-After-Reference-Impact; MBACI: Multiple Before-After-Control (or Reference)-Impact
Context definition
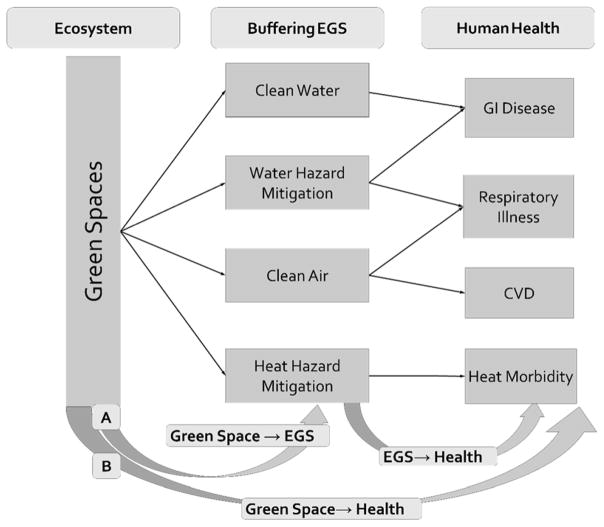
Our analysis focuses on diseases linked to buffering EGS provided by Green Spaces (Figure 1). Here the term Green Space refers to any vegetation within a human dominated environment (Kabisch and Haase 2013). This includes urban trees, green roofs, and wetlands.
Figure 1.
Selected Eco-Health linkages for causal criteria analysis. We followed two approaches for our analysis: A) Evaluating the intermediate steps linking green spaces to human health; B) Evaluating the evidence linking green spaces directly to human health. EGS refers to Ecosystem Goods and Services; GI disease refers to gastro intestinal disease; CVD refers to cardio vascular disease.
We did not consider health promoting services (physical activity, engagement with nature), or mental health outcomes. Recent reviews describe the state of knowledge regarding these topics (Lee and Maheswaran 2011, Shanahan et al. 2015), while there is relatively less information on the weight of evidence linking acute morbidities such as gastrointestinal disease, respiratory illness, cardio-vascular disease, and heat morbidities to green-space-EGS (Hartig et al. 2014). We selected these four health endpoints for our assessment which followed two approaches:
-
Evaluating intermediate linkages:
Green Space →EGS (i.e. Green Spaces providing buffering EGS)
EGS→ Health (i.e. exposure to environmental hazards leading to disease.)
-
Evaluating direct linkages:
Green Space →Health (i.e. health benefits associated to presence/extent of the ecosystem).
This approach allowed us to fully characterize the cause-effect model (Figure 1), and identify the greatest data gaps and the strongest support.
Cause and effect mechanisms
Green Spaces mitigate water hazards (e.g. floods, storm surge) by increasing rainfall interception and infiltration and by acting as a physical barrier to waves and storm surges (Broody and Highfield 2013, Costanza et al. 2008). Water hazard mitigation lowers exposure to polluted flood waters that cause GI disease, and prevents flood prone homes from harboring conditions that lead to mold growth and asthma (Wade et al. 2004, Chew et al. 2006). Green Spaces remove infectious and toxic pollutants (Silva et al. 1990, Karim et al 2004), helping to prevent GI disease from drinking and recreational water (Araya et al. 2004, Katukiza et al 2014). They trap air contaminants (Räsänen et al. 2013), which may otherwise lead to respiratory illness and cardiovascular disease (Peters et al. 1997, Brook et al. 2004). Green Spaces mitigate extreme temperatures through shade and evapotranspiration, lowering heat morbidities during heat waves (Bouchama and Knochel 2002). Table 2, summarizes these cause-effect mechanisms.
Table 2.
Cause and effect mechanisms for the intermediate steps of the selected Eco-Health linkages
| Eco-Health Linkages | Cause-Effect Mechanism | Mechanistic References | # Studies |
|---|---|---|---|
| Green Spaces and EGS* | |||
| Green Spaces-Clean Water | Green spaces provide physical barriers to the movement of pollutants in water, change the soil’s condition to promote pollutant immobilization, or capture pollutants in plant biomass. | Silva et al. 1990, Karim et al 2004 | 44 |
| Green Spaces-Water Hazard Mitigation | Green Spaces reduce surface runoff by increasing rainfall interception and infiltration. They also act as physical barriers to waves and storm surges. | Broody and Highfield 2013, Costanza et al. 2008 | 19 |
| Green Spaces-Clean Air | Green spaces provide physical barriers to the movement of pollutants in air and absorb pollutants. | Räsänen et al. 2013 | 22 |
| Green Spaces-Heat Hazard Mitigation | Green spaces provide cooling through shade and evapotranspiration. | Pokorny et al. 2010, Kong et al. 2014 | 19 |
| EGS* and Health | |||
| Clean Water-GI Disease* | Pathogenic microbes cause toxicity and infection, heavy metals like copper cause vagal nerve stimulations which triggers GI symptoms. | Araya et al. 2004, Katukiza et al 2014 | 6 |
| Water Hazard Mitigation-GI Disease* | Flood water mixes with waste water discharged into rivers, or other polluted sources. Individuals in flood prone areas come in contact with contaminated flood waters. | Wade et al 2004 | 7 |
| Water Hazard Mitigation-Respiratory Illness | The humidity and dampness in flood prone households lead to indoor mold growth. Mold endotoxins cause respiratory conditions like asthma. | Chew et al. 2006 | 4 |
| Clean Air-Respiratory Illness | Outdoor air pollutants (i.e. PM, O3, SO2 and NO2) cause oxidative stress and airway inflammation. Other mechanisms causing respiratory illness include increased susceptibility to infections and disruptions in oxygen transport. | Kagawa 1985, Nel et al. 2006, Reno et al. 2015, | 28 |
| Clean Air-Cardiovascular Disease (CVD) | Airway inflammation and obstruction in oxygen transport caused by PM2.5 and PM10), O3, SO2 and NO2 leads to plaque formation and atherosclerosis. Pollutants may also affect blood coagulation. | Peters et al. 1997, Brook et al. 2004 | 23 |
| Heat Hazard Mitigation-Heat Morbidities | Heated blood is transferred towards the surface of the body, increasing blood output and activating sweating. This leads to dehydration, increases in heart rate, and affects kidneys, liver and digestive systems as blood circulation is transferred away from the organs and towards the skin. | Bouchama and Knochel 2002 | 18 |
EGS= Ecosystem Goods and Services; GI disease=gastrointestinal disease
Literature Review
We examined 2,756 publications regarding Eco-Health linkages ( (ESM 1) from years 2000 to 2016. First, we searched within an existing Eco-Health database (Jackson et al. 2013, N=1434) and selected papers relevant to our focal Eco-Health relationships (N=112). We expanded this database with a targeted keyword search (ESM 2). We examined the titles and abstracts of all articles from the first 50 non-duplicative results per key-word combination (N = 950), and eliminated non-relevant results (e.g. review articles) for a total of 208 papers. We then evaluated study methodology for all papers selected (N=320 (112+208)) and excluded papers that were not primary research papers. For example, we excluded papers that used modelling techniques such as i-Tree (Nowak et al 2008) as these tend to infer provision of EGS from estimates made by previous studies, and thus may not add new evidence. When available we assessed articles that helped informed model development (e.g., Pope et al. 2002). We also excluded articles that looked at the Green Space-Human Health link through the lens of physical activity or restorative theories, as our focus was buffering EGS. Our final selection (N=212, ESM 4) was evaluated using CSA.
Weighting the Evidence
Selected articles were classified using the weights described in Table 1. We summed these weights to calculate an evidence score for each cause and effect linkage. A score of 20 was the threshold for rejecting or supporting the causal linkage. This threshold implies that at least three high quality studies are needed to provide evidence for causality, whereas in the case of lower quality research studies, more articles may be needed to obtain the same level of support (Norris et al. 2011). A score of 20 or more for articles contradicting the hypothesis serves as basis for rejecting the cause-effect relationship. Norris et al. 2011 chose this threshold after expert consultation and multiple trials, however, Eco-Evidence allows modifying these values if necessary. For our study, we applied the suggested score of 20, with the following possible scenarios:
In Favor ≥ 20 + Not in Favor ≤ 20 = Support for Hypothesis
In Favor < 20 + Not in Favor ≥ 20= Support for Alternate Hypothesis
In Favor < 20 + Not in Favor < 20 = Insufficient Evidence
In Favor ≥ 20 + Not in Favor ≥ 20 = Inconsistent Evidence.
To determine the sensitivity of our conclusions to the chosen threshold, we examined results at 5,10,15 and 20% of the base value (e.g., when using a 20% variation in threshold, scores of 16 and 24 were applied instead of 20.)
Results
Weighting the Evidence: Intermediate Linkages
Green Spaces and Buffering EGS
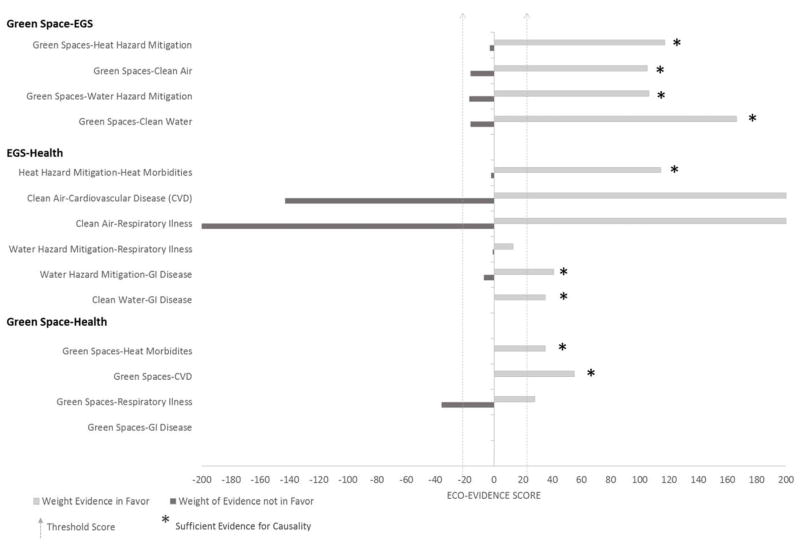
We reviewed 105 articles linking Green Spaces to clean water, water hazard mitigation, clean air, and heat hazard mitigation (Figure 2, ESM 3).
Figure 2.
Results from Causal Criteria Analysis. Interpreting possible outcomes: a) In Favor ≥ 20 + Not in Favor ≤ 20 = Support for Hypothesis; b) In Favor < 20 + Not in Favor ≥ 20 = Support for alternate Hypothesis; c) In Favor < 20 + Not in Favor < 20 = Insufficient Evidence; d) In Favor ≥ 20 + Not in Favor ≥ 20 = Inconsistent Evidence. Negative values here represent evidence not in favor, while positive values represent evidence in favor. EGS=Ecosystem Goods and Services; GI Disease=Gastro Intestinal Disease; CVD=Cardiovascular Disease
We found 44 papers supporting the Green Spaces-Clean Water linkage. Most of the studies assessed the role of wetlands in removing copper and fecal coliform; we found fewer studies assessing the capacity of other types of Green Spaces (riparian vegetation, green roofs, urban trees) for removing pollutants (ESM 3). We found 20 papers supporting the role of Green Spaces in mitigating water hazards. Studies linked this EGS to several types of Green Spaces, including green roofs, wetlands and open spaces. Indicators used to assess Water Hazard Mitigation included wave energy, surface runoff, and flood related property damages, in the presence and absence of Green Spaces (ESM 3).
Our assessment supports the linkage between Green Spaces and Clean Air. We reviewed 22 articles, where urban trees (canopy cover, tree cover) were consistently shown to remove air pollutants, most frequently Particulate Matter (PM 10 and PM 2.5). We also found support for the role of Green Spaces in Heat Hazard mitigation in19 studies on the subject. The indicators to assess Heat Hazard were mostly temperature change and heat waves, while NDVI (Normalized Difference Vegetation Index) and tree cover were commonly used to measure Green Spaces.
EGS and Health
GI disease
We reviewed 6 papers providing sufficient support for Clean Water-GI disease linkage. Swimming and consumption were the two mechanisms of exposure in the papers assessed, while surveys were used to characterize GI disease occurrences.
For the Water Hazard Mitigation-GI disease linkage, we found 7 papers providing sufficient evidence in favor (Figure 2). Most studies correlated flood events to GI disease, except for one which focused on rainfall. In this case, GI disease occurrences were assessed using hospital admissions or surveys.
Respiratory illness
We found only 4 studies evaluating the linkage between Water Hazard Mitigation and Respiratory Illness (ESM 3). Three of the papers assessed asthma as a response, and the fourth assessed bronchitis and cough. To measure Water Hazards, authors looked at flood and severe rainfall events, while health impacts were assessed using surveys or insurance claims. These papers provided insufficient evidence of a causal relationship (Figure 2).
The linkage between Respiratory Illness and Clean Air has been studied extensively (N = 27 papers reviewed). Of the respiratory conditions assessed (bronchitis, cough, wheezing, asthma) we found more evidence against the correlation between air pollutants and asthma (not in favor= 93) than the evidence in favor (in favor = 79; ESM 3). In terms of indicators, most of the studies measured air pollutants using data from monitoring stations, while hospital admissions and surveys were commonly used to assess health outcomes.
Cardiovascular disease (CVD)
The link between Clean Air and CVD had inconsistent evidence (Figure 2). The studies reviewed (N = 22) used a variety of indicators to assess CVD, from blood pressure, to hospital admissions, to indicators of inflammation. This variability in methods may explain our inconsistent results. In terms of the air pollution variables, studies mostly used data from monitoring stations, and indicators like PM10, PM2.5, and NO2.
Heat morbidities
We reviewed 18 papers linking Heat Hazards to health, which provided strong support for causality. To measure Heat Hazards the authors used either temperature fluctuations or specific Heat Wave events. The health indicators used were hospital admissions and Emergency Room visits, particularly those related to heat (e.g., heat stroke), the renal system, or the circulatory system.
Weighing the Evidence: Direct Eco-Health Linkages
The evidence directly linking Green Spaces to health included 5 papers on Respiratory Conditions, 3 papers on Heat Morbidities, and 2 papers on CVD (Figure 2). We found sufficient support for the role of Green Spaces in reducing Heat Morbidities and CVD, with most papers reporting correlations between green space cover and hospital admissions or mortality related to these conditions. The evidence linking Green Spaces to Respiratory Illness was inconsistent; most of the inconsistencies were associated with the response of asthma and/or allergies to green space cover (ESM 3). We did not find papers associating Green Spaces with GI disease, so our results indicate insufficient evidence to support this direct linkage (Figure 2).
Sensitivity Analysis
Most relationships remained unchanged when varying the threshold value by 5–20%, with a few exceptions. Varying the threshold by 15% (i.e. a threshold of 17, or 23, instead of 20) would have changed the conclusion regarding the Green Spaces-Water Hazard Mitigation and Clean Water linkage, from “sufficient” evidence, to “inconsistent” evidence as we found a few studies that found no support for the relationship. Varying the threshold by 20% (i.e. threshold of 16, or 24) would have changed the evidence supporting the Green Space linkage to Clean Air from “sufficient” to “inconsistent” with two well-designed studies falsifying the hypothesis. A 20% threshold decrease would have altered the conclusions regarding the Water Hazard Mitigation-Respiratory Illness relationship, going from “insufficient evidence” to “sufficient evidence” as we found two well-designed studies and a relatively poor study in support of the linkage. See ESM3 for details of the studies reviewed.
Discussion
Evidence for Causality: Eco-Health linkages
GI Disease
Green Spaces are causally linked to clean water and water hazard mitigation. Wetlands have been particularly well studied for their role in providing clean water. Factors determining their effectiveness include wetland type (De lacerda et al. 1984), the species involved (Yang et al. 2008), hydrological residence time, and season (Reinelt and Horner 1995). For Water Hazard Mitigation, several types of urban vegetation, including open spaces and green roofs, help reduce surface runoff and flooding (Bliss et al. 2008, Broody and Highfield 2013). Marshes and mangroves have been linked mainly to storm surge reduction and wave attenuation (Granek and Ruttenberg 2007, Moller et al. 2014); we found no papers assessing their role in mitigating urban floods. Our results correspond to findings by Shepard et al. (2011), and suggest this is an area that remains unexplored.
Our review found sufficient evidence linking Clean Water and Water Hazard Mitigation to GI disease. The impacts of water pollutants depend on exposure time, concentration of pollutants, extent of exposure, and sensitivity of exposed individuals (Araya et al. 2004, Wade et al. 2004, Collier et al. 2015). Most of the papers assessing these linkages used self-reporting to characterize health response. More objective indicators, such as medical records, or hospital visitations, are less common and could provide further support for this linkage.
We did not find studies addressing direct linkage between Green-Space and GI Disease, even though there is sufficient evidence supporting intermediate processes leading to this association, as detailed above. Future research should focus on determining the effectiveness of Green Spaces to mitigate environmental exposure to toxic and pathogenic water pollutants in diverse contexts, such as recreation, consumption and hazard events.
Respiratory Illness
We found support for the role of Green Spaces in Water Hazard Mitigation (see GI Disease section) and Clean Air, both of which protect from Respiratory Illness. Urban trees have been the focus of most studies assessing Clean Air EGS (e.g., Cavanagh et al. 2009, Grundström and Pleijel 2014), with evergreens showing greater effectiveness because of year-long foliage retention and more complex leaf structures (Beckett et al. 2000, Nguyen et al. 2015). Hairiness, stomatal density and leaf wettability are also factors that seem to increase pollutant capture by trees and that should be maximized for Clean Air EGS (Räsänen et al. 2013, Weber et al. 2014).
The evidence linking Water Hazards to Respiratory Illness was less clear. We found few papers linking floods to asthma. Only three of the four papers reviewed supported the linkage, while the fourth paper found a negative association (Park et al. 2013). Of the supporting papers, one found that response was partially mediated by psychological distress, and that asthma negatively correlated to flooding depth, which contradicts their findings (Reacher et al. 2004). The other two studies convincingly connected flood, mold and asthma, but only one followed an experimental approach (Dales et al. 1991), while the other consisted of a single case study (Makaryus et al. 2015). Therefore, the hypothesized linkage between flooding and asthma, mediated by mold growth, remains to be explored.
From the studies assessing linkage between clean air and respiratory illness, those using asthma as a response showed inconsistent evidence for causality (ESM 3). The inconsistencies are likely due to the types of indicators used to measure cause and effect. For example, a widely used Clean Air indicator is PM2.5 mass (e.g. μg/m3), while the mechanism that links air pollutants to asthma is in part mediated by oxidative stress and inflammation (Li et al. 2008). Certain particles have greater oxidative capacity than others, and their relative concentration may be a better indicator to assess respiratory impact than mass alone. Only one paper assessed oxidative potential in the air as an explanatory variable (Delfino et al. 2013); it found this was a better predictor of asthma than PM2.5 mass. Other inconsistencies were related to season, with more respiratory susceptibility in the winter months. This trend may be related to more indoor pollutant exposure during winter (Walters et al. 1994), differences in pollution sources due to heating, or meteorological patterns in winter (e.g., less rainfall) that affect diffusion of pollutants (Zhen et al. 2013).
Accordingly, we found inconsistent evidence linking Green Spaces to asthma and allergies. Some studies report positive association between Green Space and asthma, pointing toward the negative influence of pollen and other allergens (Lovasi et al. 2013). Previous studies have found that while trees help remove pollutants, sometimes these pollutants get recirculated depending on location of buildings, wind direction and flow dynamics (Wania et al, 2012). Therefore, careful selection of tree species, and the use of flow dynamics modelling, are important considerations for designing green space configurations as part of restoration initiatives.
Cardio vascular disease (CVD)
We found inconsistent evidence for the link between Clean Air-CVD. We can hypothesize potential reasons, such as the use of various indicators in different studies and the presence of confounding natural and demographic factors. For example, in an experimental study by Hajat et al. (2012), different pollutants were tested against indicators of inflammation and blood clot formation with inconsistent results among the combinations tested (ESM 3). This signals a need for better characterizing the physiological mechanisms linking Clean Air to CVD to determine the best indicators to detect this connection. Another study found that age is an important factor, with the elderly showing greater CVD response to pollution (Prescott et al. 1999). Season may also play a role; in some instances, correlations were observed in cold but not warm months (Chang et al. 2015). Moreover, when looking at relationships that have many associated studies (e.g., CVD-Clean Air), the likelihood of finding inconsistencies increases (Norris et al 2011). This does not imply that “inconsistent” connections are not real; rather, the inconsistencies help refine hypotheses and future research questions (Norris et al 2011).
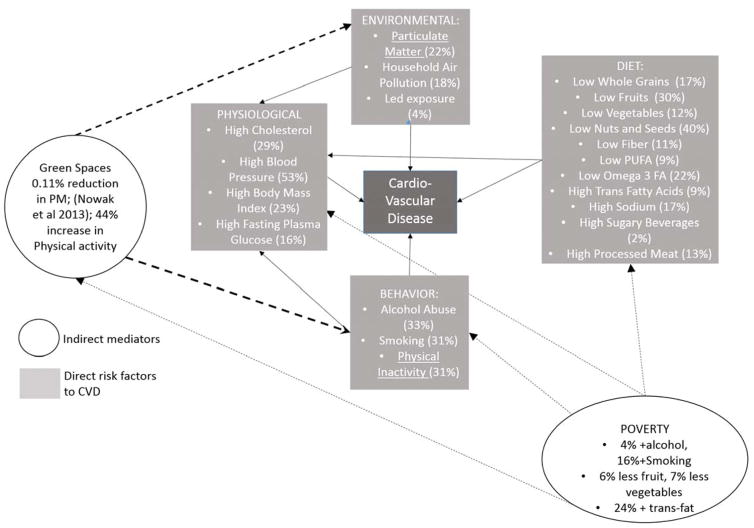
We found support for a direct link between Green Space and CVD. Although we tried to avoid papers focusing on the health promoting benefits of Green Spaces, the studies we used were correlative, without explicit assessments of the mechanisms involved. The findings may in part be related to promotion of physical activity, engagement with nature, and the stress reducing potential of Green Spaces. In one of the papers, Perreira et al. (2012) found that neighborhood variability of greenness had a stronger association to CVD than absolute greenness, a finding that points toward physical activity as a mediating factor, since non-green areas (e.g., sidewalks, parking lots) were also important. Donovan et al. 2015 found that correlations between green space loss and CVD were significant after controlling for exercise, indicating that factors other than physical activity were important. Nevertheless, these other factors could include stress reduction from promotion of social engagement (EGS that also reduce CVD risk) and not necessarily air quality. Based on our review, we hypothesize that the benefits of trees to CVD could be attributed to mechanisms other than supporting air quality. In Figure 3, we present this hypothesis by illustrating risk factors for CVD, and the role of Green Spaces using previous studies. Green Spaces have been shown to promote a 44% increase in physical activity, but provide on average 0.11% air quality improvement via reduction of PM (Richardson et al. 2013, Nowak et al. 2013). Although these values come from studies with different methodologies, and quantitative comparisons are not justified, the differences in magnitude illustrate the relative influence of Green Spaces via these two EGS. Moreover, a study by Lim et al. (2013) showed that PM corresponds to 22% of the risk for CVD, while physical activity accounts for 31% and influences other important CVD drivers like stress and body mass index. Considering the relative importance of Green Spaces for physical activity versus clean air, and the relative importance of physical activity vs clean air in CVD, we propose that Green Spaces mainly influence CVD by promoting physical activity. This is not suggesting that clean air is unimportant for CVD, rather that Green Spaces likely play a modest pollutant buffering role, and that emphasis should be placed primarily on reducing pollution. In turn, management of Green Spaces for health promoting services should align with aspects of the built environment, such as access and safety features. This is especially important for low income communities, which face higher CVD risks (Figure 3).
Figure 3.
Direct risk factors for cardiovascular disease (CVD, grey boxes) and indirect mediators (white circles, Green Spaces and Poverty). The percentages represent the proportion of the effect attributed to the cause. The causes for CVD or risk factors (environmental, diet, behavior and physiological) were adapted from Lim et al. (2013), who looked at Ischemic Heart Disease, a common type of CVD. The % of air quality improvement from trees was adapted from Nowak et al. 2013, by averaging the estimates for the ten US cities they assessed in their study. The percent in promotion of physical activity comes from Richardson et al. (2013); Poverty percentages come from Hulshof et al. (1991), and Galobardes et al. (2001)
Heat Morbidities
The link between Green Spaces and Heat Hazard Mitigation is unequivocal, both for direct health outcomes and for the intermediate steps. Heat mitigation by trees has been reported for cities with different types of green space and ecosystems, and at multiple scales (Hou et al 2013, Valishery et al 2013). Likewise, the protective value of green cover on heat morbidities has been well documented in relation to heat waves and within arid environments at risk of heat extremes (Vandertorren et al 2006, Harlan et al 2013). Consistently, studies confirm increased risk from heat for vulnerable populations, such as elderly individuals and those with impaired mobility (Vandertorren et al 2006, Burkart et al 2016). Although correlations have been observed when documenting green cover at lower resolutions (e.g. 30m resolution, using indicators such as NDVI), vegetation is most likely to be protective when it i strategically placed near exposed households within the urban context (Li et al 2013).
In terms of management for Heat Hazard Mitigation, the amount of green space is the most important factor, but there are other design considerations. Mixing tree species along street corridors to avoid continuous canopies that trap heat, and designing green roofs to have high leaf area index and adequate irrigation, are strategies to enhance the cooling effect (Norton et al. 2015). Urban greening not only buffers against heat islands and heat waves, but may also provide economic services to sectors that cannot rely on air conditioning, while supporting efficient energy use.
Limitations and Recommendations
Limitations of the Eco-Evidence tool are discussed in detail in Norris et al (2011). The authors address criticisms regarding the threshold value of 20, and advise that expert judgement should always be included. From our sensitivity analysis, we found that we would need to change the threshold by 15–20% to alter our conclusions. Because Norris et al. (2011) used trials and expert advice to develop the threshold of 20, we feel compelled to adhere to this value to maintain consistency, but we encourage readers to consider these alternative results when interpreting our findings. Another limitation is that the approach does not differentiate studies by their attention to confounding factors, which in the case of Eco-Health studies could be influential. Weighting studies by environmental or socio-economic confounders would be a much-needed revision to the method (Norris et al 2011). Lastly, while Eco-Evidence is not a substitute for strictly quantitative approaches such as meta-analyses, it allows weighting evidence from a variety of studies, including those that do not report summary statistics or cannot be combined due to fundamental differences in datasets. The contribution of Eco-Evidence is to help evaluate the knowledge base in support of a given relationship, not the effect size of that relationship, as in meta-analyses.
Our results are partly determined by the keywords used to identify relevant scientific studies (ESM2). We invite readers to evaluate our selected search items and account for potentially missing terms when interpreting our conclusions. In addition, to maintain consistency in the quality of material included, we only considered peer-reviewed publications, and excluded book chapters and grey literature. Despite these limitations, our review allowed us to make consistent comparisons, determine their relative state of knowledge, refine hypotheses and define areas of research need. Our findings support a proposed research agenda (Table 3) to advance the management of EGS for human health benefits.
Table 3.
Summary of causality assessment and priority questions for an Eco-Health research agenda
| Eco-Health linkages | Evidence for causality | Priority questions | |
|---|---|---|---|
|
| |||
| Intermediate linkages | Direct linkages | ||
| Green Spaces-Clean Water/Polluted Water-GI Disease | Support for Hypothesis | Insufficient | Is GI disease prevalence related to green space measures (presence, % cover, etc.) in areas exposed to water pollution? |
| Green Spaces-Water Hazard Mitigation/Water Hazards-GI Disease* | Support for Hypothesis | Insufficient | Is GI disease prevalence related to green space measures (presence, % cover, etc.) in flood prone areas? |
| Green Spaces-Water Hazard Mitigation/Water Hazards-Respiratory Illness | Insufficient for EGS*-Health linkage | Insufficient | Is mold more common in houses prone to natural flooding flood prone houses? Does household mold correlate to asthma? |
| Green Spaces-Clean Air /Polluted Air Respiratory Illness | Inconsistent for EGS*-Health linkage | Inconsistent | What are the best indicators to detect the impact of air quality on respiratory illnesses (e.g. oxidative potential vs pollutant mass)? Are there consistent confounding factors (demographics, seasonality) determining the impact of air pollutants? Could we define transferable green space restoration guidelines to enhance pollution removal and reduce allergen potential? How can we incorporate flow dynamic principles into the design of green space restoration? |
| Green Spaces-Clean Air/Polluted Air-CVD* | Inconsistent for Eco-Health linkage | Support for Hypothesis | What are the best indicators to detect the impact of air quality on CVD (e.g. inflammatory response, coagulation, CVD prevalence)? Are there consistent confounding factors (demographics, seasonality) determining the impact of air pollutants on CVD? What is the main mediator between Green Spaces and CVD--physical activity or clean air? |
| Green Spaces-Heat Hazard Mitigation/Heat Hazard-Heat Morbidities | Support for Hypothesis | Support for Hypothesis | What are the barriers to establishing green space policy for heat morbidity prevention in cities? |
GI Disease=Gastrointestinal disease; CVD=Cardiovascular disease; EGS=Ecosystem Goods and Services
Conclusions
We conducted a CSA to characterize Eco-Health literature. Our study fills a void that previous reviews had identified as crucial for valuing Eco-Health evidence: namely reviewing the evidence for the full pathways between ecosystem, ecosystem processes (e.g. EGS) and health outcomes (Hartig et al 2014).
Our work confirms that most current Eco-Health literature supports the intermediate steps of these pathways (e.g. Ecosystem-EGS, EGS-Health), but few studies trace linkages from ecosystem to disease. Of these, few simultaneously address the pathways by which these direct connections occur. Research that fully determines if/how greening strategies deliver health benefits through buffering EGS is generally lacking, and in need of attention.
Despite identifying research needs, our review found consistent evidence of a connection between Green Spaces and buffering EGS, and between Green Spaces and certain health outcomes such as cardiovascular disease and heat morbidities. The role of Green Spaces in providing health benefits is enhanced in cities if considered alongside design aspects such as selection of tree species, attention to placement and configuration of trees, and aspects of the built environment that encourage use of Green Spaces. This evidence should encourage green space planning within cities by showing human health is an achievable objective of restoration investments.
Footnotes
Ethical Statement
There is no conflict of interest to declare. Our work did not involve human subjects or third party funding sources.
References
- 1.Araya M, Olivares M, Pizarro F, Llanos A, Figueroa G, Uauy R. Community-based randomized double-blind study of gastrointestinal effects and copper exposure in drinking water. Environmental Health Perspectives. 2004;112(10):1068–1073. doi: 10.1289/ehp.6913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beckett KP, Freer-Smith PH, Taylor G. Particulate pollution capture by urban trees: effect of species and windspeed. Global change biology. 2000;6(8):995–1003. doi: 10.1046/j.1365-2486.2000.00376.x. [DOI] [Google Scholar]
- 3.Bliss DJ, Neufeld RD, Ries RJ. Storm water runoff mitigation using a green roof. Environmental Engineering Science. 2009;26(2):407–18. doi: 10.1089/ees.2007.0186. [DOI] [Google Scholar]
- 4.Bouchama A, Knochel JP. Heat stroke. New England Journal of Medicine. 2002;346(25):1978–1988. doi: 10.1056/NEJMra011089. [DOI] [PubMed] [Google Scholar]
- 5.Brody SD, Highfield WE. Open space protection and flood mitigation: A national study. Land Use Policy. 2013;32:89–95. doi: 10.1016/j.landusepol.2012.10.017. [DOI] [Google Scholar]
- 6.Brook RD, Franklin B, Cascio W, Hong Y, Howard G, Lipsett M, Luepker R, Mittleman M, Samet J, Smith SC, Tager I. Air pollution and cardiovascular disease. Circulation. 2004;109(21):2655–71. doi: 10.1161/01.CIR.0000128587.30041.C8. [DOI] [PubMed] [Google Scholar]
- 7.Burkart K, Meier F, Schneider A, Breitner S, Canário P, Alcoforado MJ, Scherer D, Endlicher W. Modification of heat-related mortality in an elderly urban population by vegetation (urban green) and proximity to water (urban blue): evidence from Lisbon, Portugal. Environmental Health Perspectives. 2016;124(7):927. doi: 10.1289/ehp.1409529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chang CC, Chen PS, Yang CY. Short-term effects of fine particulate air pollution on hospital admissions for cardiovascular diseases: A case-crossover study in a tropical city. Journal of Toxicology and Environmental Health, Part A. 2015;78(4):267–77. doi: 10.1080/15287394.2014.960044. [DOI] [PubMed] [Google Scholar]
- 9.Chew GL, Wilson J, Rabito FA, Grimsley F, Iqbal S, Reponen T, Muilenberg ML, Thorne PS, Dearborn DG, Morley RL. Mold and endotoxin levels in the aftermath of Hurricane Katrina: a pilot project of homes in New Orleans undergoing renovation. Environmental Health Perspectives. 2006;114(12):1883–1889. doi: 10.1289/ehp.9258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Collier SA, Wade TJ, Sams EA, Hlavsa MC, Dufour AP, Beach MJ. Swimming in the USA: beachgoer characteristics and health outcomes at US marine and freshwater beaches. Journal of Water and Health. 2015;13(2):531–543. doi: 10.2166/wh.2014.095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Corvalan C, Hales S, McMichael AJ. Ecosystems and human well-being: health synthesis. World Health Organization; 2005. [Google Scholar]
- 12.Costanza R, Pérez-Maqueo O, Martinez ML, Sutton P, Anderson SJ, Mulder K. The value of coastal wetlands for hurricane protection. AMBIO: A Journal of the Human Environment. 2008;37(4):241–8. doi: 10.1579/0044-7447(2008)37[241:TVOCWF]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 13.Dales RE, Zwanenburg H, Burnett R, Franklin CA. Respiratory health effects of home dampness and molds among Canadian children. American Journal of Epidemiology. 1991;134(2):196–203. doi: 10.1093/oxfordjournals.aje.a116072. [DOI] [PubMed] [Google Scholar]
- 14.De Lacerda LD, Abrao JJ. Heavy metal accumulation by mangrove and saltmarsh intertidal sediments. Rvta Brasil Bot. 1984;7:49–52. [Google Scholar]
- 15.Delfino RJ, Staimer N, Tjoa T, Gillen DL, Schauer JJ, Shafer MM. Airway inflammation and oxidative potential of air pollutant particles in a pediatric asthma panel. Journal of Exposure Science and Environmental Epidemiology. 2013;23(5):466–73. doi: 10.1038/jes.2013.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Donovan GH, Michael YL, Gatziolis D, Prestemon JP, Whitsel EA. Is tree loss associated with cardiovascular-disease risk in the Women’s Health Initiative? A natural experiment. Health & Place. 2015;36:1–7. doi: 10.1016/j.healthplace.2015.08.007. [DOI] [PubMed] [Google Scholar]
- 17.Galobardes B, Morabia A, Bernstein MS. Diet and socioeconomic position: does the use of different indicators matter? International journal of Epidemiology. 2001;30(2):334–340. doi: 10.1093/ije/30.2.334. [DOI] [PubMed] [Google Scholar]
- 18.Granek EF, Ruttenberg BI. Protective capacity of mangroves during tropical storms: a case study from ‘Wilma’ and ‘Gamma’ in Belize. Marine Ecology Progress Series. 2007;343:101–5. doi: 10.3354/meps07141. [DOI] [Google Scholar]
- 19.Gronlund CJ, Zanobetti A, Schwartz JD, Wellenius GA, O’Neill MS. Heat, heat waves, and hospital admissions among the elderly in the United States, 1992–2006. Environmental Health Perspectives. 2014;122(11):1187–1192. doi: 10.1289/ehp.1206132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Grundström M, Pleijel H. Limited effect of urban tree vegetation on NO 2 and O 3 concentrations near a traffic route. Environmental Pollution. 2014;189:73–6. doi: 10.1016/j.envpol.2014.02.026. [DOI] [PubMed] [Google Scholar]
- 21.Hajat A, Allison M, Diez-Roux AV, Jenny NS, Jorgensen NW, Szpiro AA, Vedal S, Kaufman JD. Long-term exposure to air pollution and markers of inflammation, coagulation, and endothelial activation: a repeat-measures analysis in the Multi-Ethnic Study of Atherosclerosis (MESA) Epidemiology. 2015;26(3):310–320. doi: 10.1097/EDE.0000000000000267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Harlan SL, Declet-Barreto JH, Stefanov WL, Petitti DB. Neighborhood effects on heat deaths: social and environmental predictors of vulnerability in Maricopa County, Arizona. Environmental Health Perspectives. 2013;121(2):197. doi: 10.1289/ehp.1104625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hartig T, Mitchell R, De Vries S, Frumkin H. Nature and health. Annual Review of Public Health. 2014;18(35):207–28. doi: 10.1146/annurev-publhealth-032013-182443. [DOI] [PubMed] [Google Scholar]
- 24.Hou P, Chen Y, Qiao W, Cao G, Jiang W, Li J. Near-surface air temperature retrieval from satellite images and influence by wetlands in urban region. Theoretical and applied climatology. 2013;111(1–2):109–18. doi: 10.1007/s00704-012-0629-7. [DOI] [Google Scholar]
- 25.Hulshof KF, Löwik MR, Kok FJ, Wedel M, Brants HA, Hermus RJ, Ten Hoor F. Diet and other life-style factors in high and low socio-economic groups (Dutch Nutrition Surveillance System) European journal of clinical nutrition. 1991;45(9):441–50. [PubMed] [Google Scholar]
- 26.Jackson LE, Daniel J, McCorkle B, Sears A, Bush KF. Linking ecosystem services and human health: the Eco-Health Relationship Browser. International journal of public health. 2013;58(5):747–55. doi: 10.1007/s00038-013-0482-1. [DOI] [PubMed] [Google Scholar]
- 27.Kabisch N, Haase D. Green spaces of European cities revisited for 1990–2006. Landscape and Urban Planning. 2013;110:113–122. doi: 10.1016/j.landurbplan.2012.10.017. [DOI] [Google Scholar]
- 28.Karim MR, Manshadi FD, Karpiscak MM, Gerba CP. The persistence and removal of enteric pathogens in constructed wetlands. Water Research. 2004;38(7):1831–7. doi: 10.1016/j.watres.2003.12.029. [DOI] [PubMed] [Google Scholar]
- 29.Katukiza AY, Ronteltap M, Steen P, Foppen JW, Lens PN. Quantification of microbial risks to human health caused by waterborne viruses and bacteria in an urban slum. Journal of applied microbiology. 2014;116(2):447–63. doi: 10.1111/jam.12368. [DOI] [PubMed] [Google Scholar]
- 30.Lee AC, Maheswaran R. The health benefits of urban green spaces: a review of the evidence. Journal of Public Health. 2011;33(2):212–22. doi: 10.1093/pubmed/fdq068. [DOI] [PubMed] [Google Scholar]
- 31.Li N, Xia T, Nel AE. The role of oxidative stress in ambient particulate matter-induced lung diseases and its implications in the toxicity of engineered nanoparticles. Free Radical Biology and Medicine. 2008;44(9):1689–99. doi: 10.1016/j.freeradbiomed.2008.01.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Li X, Zhou W, Ouyang Z. Relationship between land surface temperature and spatial pattern of greenspace: What are the effects of spatial resolution? Landscape and Urban Planning. 2013;114:1–8. doi: 10.1016/j.freeradbiomed.2008.01.028. [DOI] [Google Scholar]
- 33.Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, AlMazroa MA, Amann M, Anderson HR, Andrews KG, Aryee M. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. The lancet. 2013;380(9859):2224–60. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lovasi GS, O’Neil-Dunne JP, Lu JW, Sheehan D, Perzanowski MS, MacFaden SW, King KL, Matte T, Miller RL, Hoepner LA, Perera FP. Urban tree canopy and asthma, wheeze, rhinitis, and allergic sensitization to tree pollen in a New York City birth cohort. Environmental health perspectives. 2013;121(4):494. doi: 10.1289/ehp.1205513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Makaryus M, Iakovou A, Lisker G. Interesting cases in allergy and immunology. American Thoracic Society; 2015. A case of severe asthma with fungal sensitization (safs) due to Aureobasidium Pullulans following Hurricane Sandy; pp. A5644–A5644. [Google Scholar]
- 36.Millennium Ecosystem Assessment (MEA) Ecosystems and human well-being: synthesis. Washington, DC: Island Press; 2005. [Google Scholar]
- 37.Möller I, Kudella M, Rupprecht F, Spencer T, Paul M, Van Wesenbeeck BK, Wolters G, Jensen K, Bouma TJ, Miranda-Lange M, Schimmels S. Wave attenuation over coastal salt marshes under storm surge conditions. Nature Geoscience. 2014;7(10):727–31. doi: 10.1038/ngeo2251. [DOI] [Google Scholar]
- 38.Munns WR, Rea AW, Mazzotta MJ, Wainger LA, Saterson K. Toward a standard lexicon for ecosystem services. Integrated environmental assessment and management. 2015;11(4):666–73. doi: 10.1002/ieam.1631. [DOI] [PubMed] [Google Scholar]
- 39.Nguyen T, Yu X, Zhang Z, Liu M, Liu X. Relationship between types of urban forest and PM 2.5 capture at three growth stages of leaves. Journal of Environmental Sciences. 2015;27:33–41. doi: 10.1016/j.jes.2014.04.019. [DOI] [PubMed] [Google Scholar]
- 40.Norris RH, Webb JA, Nichols SJ, Stewardson MJ, Harrison ET. Analyzing cause and effect in environmental assessments: using weighted evidence from the literature. Freshwater Science. 2011;31(1):5–21. doi: 10.1899/11-027.1. [DOI] [Google Scholar]
- 41.Norton BA, Coutts AM, Livesley SJ, Harris RJ, Hunter AM, Williams NS. Planning for cooler cities: A framework to prioritise green infrastructure to mitigate high temperatures in urban landscapes. Landscape and Urban Planning. 2015;134:127–38. doi: 10.1016/j.landurbplan.2014.10.018. [DOI] [Google Scholar]
- 42.Nowak DJ, Crane DE, Stevens JC, Hoehn RE, Walton JT, Bond J. A ground-based method of assessing urban forest structure and ecosystem services. Arboriculture and Urban Forestry. 2008;34(6):347–358. [Google Scholar]
- 43.Nowak DJ, Hirabayashi S, Bodine A, Hoehn R. Modeled PM 2.5 removal by trees in ten US cities and associated health effects. Environmental Pollution. 2013;178:395–402. doi: 10.1016/j.envpol.2013.03.050. [DOI] [PubMed] [Google Scholar]
- 44.Park KJ, Moon JY, Ha JS, Kim SD, Pyun BY, Min TK, Park YH. Impacts of heavy rain and typhoon on allergic disease. Osong public health and research perspectives. 2013;4(3):140–5. doi: 10.1016/j.phrp.2013.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pereira G, Christian H, Foster S, Boruff BJ, Bull F, Knuiman M, Giles-Corti B. The association between neighborhood greenness and weight status: an observational study in Perth Western Australia. Environmental Health. 2013;12(1):49. doi: 10.1186/1476-069X-12-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Peters A, Döring A, Wichmann HE, Koenig W. Increased plasma viscosity during an air pollution episode: a link to mortality? The Lancet. 1997;349(9065):1582–7. doi: 10.1016/S0140-6736(97)01211-7. [DOI] [PubMed] [Google Scholar]
- 47.Pope CA, III, Burnett RT, Thun MJ, Calle EE, Krewski D, Ito K, Thurston GD. Lung cancer, cardiopulmonary mortality, and long-term exposure to fine particulate air pollution. Jama. 2002;287(9):1132–41. doi: 10.1001/jama.287.9.1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Prescott GJ, Lee RJ, Cohen GR, Elton RA, Lee AJ, Fowkes FG, Agius RM. Investigation of factors which might indicate susceptibility to particulate air pollution. Occupational and environmental medicine. 2000;57(1):53–7. doi: 10.1136/oem.57.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Räsänen JV, Holopainen T, Joutsensaari J, Ndam C, Pasanen P, Rinnan Å, Kivimäenpää M. Effects of species-specific leaf characteristics and reduced water availability on fine particle capture efficiency of trees. Environmental pollution. 2013;183:64–70. doi: 10.1016/j.envpol.2013.05.015. [DOI] [PubMed] [Google Scholar]
- 50.Reacher M, McKenzie K, Lane C, Nichols T, Kedge I, Iversen A, Hepple P, Walter T, Laxton C, Simpson J. Health impacts of flooding in Lewes: a comparison of reported gastrointestinal and other illness and mental health in flooded and non-flooded households. Communicable Disease and Public Health. 2004;7(1):39–46. [PubMed] [Google Scholar]
- 51.Reinelt LE, Horner RR. Pollutant removal from stormwater runoff by palustrine wetlands based on comprehensive budgets. Ecological Engineering. 1995;4(2):77–97. doi: 10.1016/0925-8574(94)00002-M. [DOI] [Google Scholar]
- 52.Richardson EA, Pearce J, Mitchell R, Kingham S. Role of physical activity in the relationship between urban green space and health. Public health. 2013;127(4):318–24. doi: 10.1016/j.puhe.2013.01.004. [DOI] [PubMed] [Google Scholar]
- 53.Russo F, Williamson J. Interpreting causality in the health sciences. International studies in the philosophy of science. 2007;21(2):157–70. doi: 10.1080/02698590701498084. [DOI] [Google Scholar]
- 54.Semenza JC, McCullough JE, Flanders WD, McGeehin MA, Lumpkin JR. Excess hospital admissions during the July 1995 heat wave in Chicago. American journal of preventive medicine. 1999;16(4):269–77. doi: 10.1016/S0749-3797(99)00025-2. [DOI] [PubMed] [Google Scholar]
- 55.Shanahan DF, Lin BB, Bush R, Gaston KJ, Dean JH, Barber E, Fuller RA. Toward improved public health outcomes from urban nature. American Journal of Public Health. 2015;105(3):470–477. doi: 10.2105/AJPH.2014.302324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Shepard CC, Crain CM, Beck MW. The protective role of coastal marshes: a systematic review and meta-analysis. PloS one. 2011;6(11):1–11. doi: 10.1371/journal.pone.0027374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Silva CA, Lacerda LD, Rezende CE. Metals reservoir in a red mangrove forest. Biotropica. 1990;22(4):339–45. doi: 10.2307/2388551. [DOI] [Google Scholar]
- 58.Suter GW, Cormier SM. Why and how to combine evidence in environmental assessments: weighing evidence and building cases. Science of the Total Environment. 2011;409(8):1406–17. doi: 10.1016/j.scitotenv.2010.12.029. [DOI] [PubMed] [Google Scholar]
- 59.Vailshery LS, Jaganmohan M, Nagendra H. Effect of street trees on microclimate and air pollution in a tropical city. Urban forestry & urban greening. 2013;12(3):408–15. doi: 10.1016/j.ufug.2013.03.002. [DOI] [Google Scholar]
- 60.Vandentorren S, Bretin P, Zeghnoun A, Mandereau-Bruno L, Croisier A, Cochet C, Ribéron J, Siberan I, Declercq B, Ledrans M. August 2003 heat wave in France: risk factors for death of elderly people living at home. The European Journal of Public Health. 2006;16(6):583–91. doi: 10.1093/eurpub/ckl063. [DOI] [PubMed] [Google Scholar]
- 61.Wade TJ, Sandhu SK, Levy D, Lee S, LeChevallier MW, Katz L, Colford JM., Jr Did a severe flood in the Midwest cause an increase in the incidence of gastrointestinal symptoms? American Journal of Epidemiology. 2004;159(4):398–405. doi: 10.1093/aje/kwh050. [DOI] [PubMed] [Google Scholar]
- 62.Walters S, Griffiths RK, Ayres JG. Temporal association between hospital admissions for asthma in Birmingham and ambient levels of sulphur dioxide and smoke. Thorax. 1994;49(2):133–40. doi: 10.1136/thx.49.10.1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wania A, Bruse M, Blond N, Weber C. Analysing the influence of different street vegetation on traffic-induced particle dispersion using microscale simulations. Journal of environmental management. 2012;94(1):91–101. doi: 10.1016/j.jenvman.2011.06.036. [DOI] [PubMed] [Google Scholar]
- 64.Webb JA, Miller KA, Stewardson MJ, de Little SC, Nichols SJ, Wealands SR. An online database and desktop assessment software to simplify systematic reviews in environmental science. Environmental Modelling & Software. 2015;64:72–9. doi: 10.1016/j.envsoft.2014.11.011. [DOI] [Google Scholar]
- 65.Weber F, Kowarik I, Säumel I. Herbaceous plants as filters: Immobilization of particulates along urban street corridors. Environmental Pollution. 2014;186:234–240. doi: 10.1016/j.envpol.2013.12.011. [DOI] [PubMed] [Google Scholar]
- 66.Weed DL. On the use of causal criteria. International Journal of Epidemiology. 1997;26(6):1137–1141. doi: 10.1093/ije/26.6.1137. [DOI] [PubMed] [Google Scholar]
- 67.Yang Q, Tam NF, Wong YS, Luan TG, Su WS, Lan CY, Shin PK, Cheung SG. Potential use of mangroves as constructed wetland for municipal sewage treatment in Futian, Shenzhen, China. Marine Pollution Bulletin. 2008;57(6):735–743. doi: 10.1016/j.marpolbul.2008.01.037. [DOI] [PubMed] [Google Scholar]
- 68.Zhen WM, Shan ZH, Gong WS, Yan TA, Zheng SK. The weather temperature and air pollution interaction and its effect on hospital admissions due to respiratory system diseases in western China. Biomedical and Environmental Sciences. 2013;26:403–407. doi: 10.3967/0895-3988.2013.05.011. [DOI] [PubMed] [Google Scholar]