Abstract
Background:
Use of enhanced recovery pathways (ERPs) can improve patient outcomes, yet national implementation of these pathways remains low. The Agency for Healthcare Research and Quality (AHRQ; funder), the American College of Surgeons, and the Johns Hopkins Medicine Armstrong Institute for Patent Safety and Quality have developed the Safety Program for Improving Surgical Care and Recovery—a national effort to catalyze implementation of practices to improve perioperative care and enhance recovery of surgical patients. This review synthesizes evidence that can be used to develop a protocol for elective total knee arthroplasty (TKA) and total hip arthroplasty (THA).
Study Design:
This review focuses on potential components of the protocol relevant to surgeons; anesthesia components are reported separately. Components were identified through review of existing pathways and from consultation with technical experts. For each, a structured review of MEDLINE identified systematic reviews, randomized trials, and observational studies that reported on these components in patients undergoing elective TKA/THA. This primary evidence review was combined with existing clinical guidelines in a narrative format.
Results:
Sixteen components were reviewed. Of the 10 preoperative components, most were focused on risk factor assessment including anemia, diabetes mellitus, tobacco use, obesity, nutrition, immune-modulating therapy, and opiates. Preoperative education, venous thromboembolism (VTE) prophylaxis, and bathing/Staphylococcus aureus decolonization were also included. The routine use of drains was the only intraoperative component evaluated. The 5 postoperative components included early mobilization, continuous passive motion, extended duration VTE prophylaxis, early oral alimentation, and discharge planning.
Conclusion:
This review synthesizes the evidence supporting potential surgical components of an ERP for elective TKA/THA. The AHRQ Safety Program for Improving Surgical Care and Recovery aims to guide hospitals and surgeons in identifying the best practices to implement in the surgical care of TKA and THA patients.
Keywords: enhanced recovery, total knee replacement, total hip replacement, total joint replacement, patient safety, quality improvement
Introduction
A multistakeholder partnership between the Agency for Healthcare Research and Quality (AHRQ; funder), the American College of Surgeons (ACS), and the Johns Hopkins Medicine Armstrong Institute for Patient Safety and Quality has developed the Safety Program for Improving Surgical Care and Recovery. This 5-year national effort aims to assist over 750 hospitals in implementing pathways for surgical patients using evidence-based practices. This program will cover 5 surgical areas including colorectal, orthopedics, gynecology, bariatrics, and emergency general surgery. The cornerstone of this project is evidence-based enhanced recovery pathways (ERPs).
ERPs have previously been shown to reduce complications, shorten length of stay (LOS), improve patient satisfaction, and reduce costs for a variety of operations across specialties, including orthopedics.1–4 The effectiveness of these programs is directly related to a hospitals’ ability to promote high compliance with each pathway process. Adherence to these pathways appears to have a dose–response effect on clinical outcomes.5 Successful and sustainable implementation goes beyond protocol development, requiring integration across patient units, timely feedback of performance data sharing, senior executive support, and ongoing educational sessions.6 As such, the Safety Program for Improving Surgical Care and Recovery will provide extensive resources beyond the ERP including access to outcome registries, performance benchmarking, educational materials, leadership training, and contemporary implementation science tools.
The foundation on which all of this lies, however, is an evidence-based protocol including best practices for preventing harm and the principles of enhanced recovery. Recognizing that successful and sustainable pathways require transdisciplinary collaboration among surgeons, anesthesia providers, nurses, and other health-care providers, we have split this review into “surgery” and “anesthesia” components. The objective of this article is to review the evidence supporting proposed ERP components relevant primarily to surgeons. This includes a structured review of the literature and existing clinical guidelines. The anesthesia review is being conducted by anesthesiologists and will be published separately (Appendix A). The ultimate goal of these combined reviews is to provide an evidence base that can be used for the development of a total joint (total knee arthroplasty [TKA]/total hip arthroplasty [THA]) ERP.
Methods
The detailed protocol guiding this review has been previously published.7 Potential components (“bins”) of the ERP were identified through review of existing protocols from community hospitals, academic medical centers, integrated health-care delivery systems, and the expert opinion of technical advisors (Table 1). The focus was on identification of pre- and postoperative practices that can enhance recovery. While a number of operative decisions likely influence patient outcomes, such as approach and technique, these areas fall into the realm of “appropriateness” and were considered beyond the scope of this project. Well-accepted components of ERP pathways, such as the early removal of Foley catheters and adequate skin preparation, were not targeted as the evidence supporting these practices are robust and reported elsewhere.7,8 We instead focused on procedure-specific and potentially uncertain components. For each bin, we conducted a structured review of the literature. Searches of MEDLINE were conducted between January and August 2017. Search criteria (Appendix B) were generated with the assistance of a research librarian (E.W.). Additional citations were identified through reference mining and from recommendations of our technical experts. Across all bins, articles were included if they utilized a systematic review (SR) with or without meta-analysis (MA), randomized controlled trial (RCT), or observational design and focused on TKA or THA. We focused only on articles that reported outcomes for a specific protocol component, excluding those that studied multiple components simultaneously or those that evaluated entire pathways. Common exclusion criteria were non-SRs, editorials, case reports, articles where the full text was not available, and articles reporting interventions not relevant to US hospitals. The focus of this review was on primary elective TKA/THA for patients with osteoarthritis (OA) or rheumatoid arthritis (RA). Therefore, hip fractures and TKAs/THAs after trauma indications were excluded. A technical review for hip fracture surgery was performed concurrently (separate publication).
Table 1.
Improving Surgical Care and Recovery: TKA/THA Protocol Components—Surgery.
| Preoperative management |
| Risk factor assessment |
| Anemia |
| Diabetes mellitus |
| Tobacco use/smoking |
| Obesity |
| Malnutrition |
| Immune modulators |
| Opiates/drug abuse |
| Preoperative education |
| Preoperative bathing/decolonization |
| Preoperative VTE prophylaxis |
| Intraoperative management |
| Drains |
| Postoperative management |
| Early mobilization |
| Continuous passive motion |
| Extended duration VTE prophylaxis |
| Early oral alimentation and enhanced nutrition |
| Discharge planning/discharge criteria |
Abbreviations: THA, total hip arthroplasty; TKA, total knee arthroplasty; VTE, venous thromboembolism.
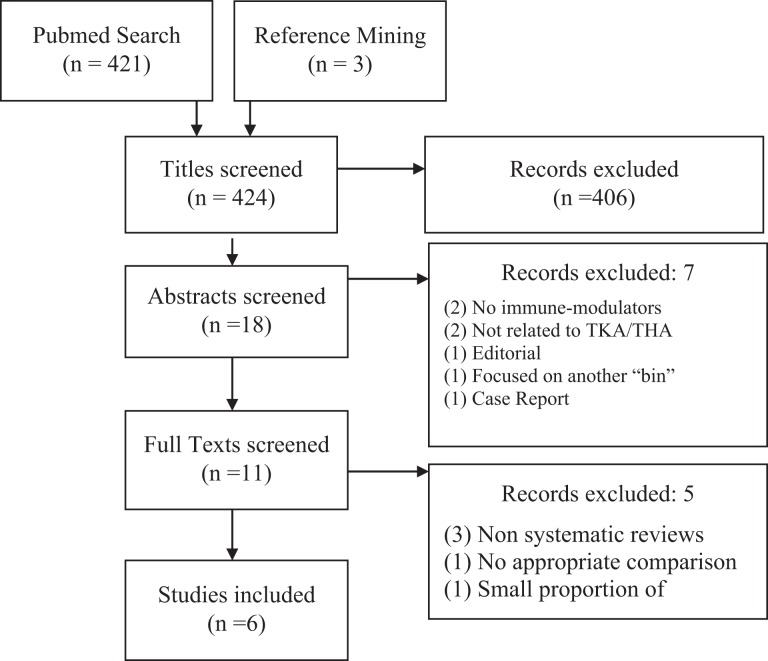
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagrams were recorded for each bin (example reported in Appendix C). After title and abstract screen, full texts were retrieved and assessed according to predefined inclusion/exclusion criteria. Included studies were evaluated in a hierarchical fashion. For example, if a contemporary well-conducted SR/MA was available, this would serve as the foundation for the evidence synthesis. This SR/MA was updated with more recent RCTs or observational studies. If an SR/MA did not exist, the evidence synthesis was focused on available RCTs and/or observational studies. Given the rapid evolution of ERPs, we favored newer studies, with most included studies published after the year 2000. Finally, clinical guidelines from national and international organizations were incorporated into the review, when available. Results are presented in a narrative format.
Results
For each component, we provide the rationale, a review of the primary evidence, a summary of available guidelines (when available), and our overall conclusion as it relates to the development of an ERP. Table 1 lists the 16 protocol components evaluated in this review. Table 2 summarizes the evidence reviewed for each component, the strength and consistency of the evidence, and its concordance with guidelines. Table 3 provides details regarding the guideline recommendations for each component.
Table 2.
Summary of Reviewed TKA/THA Protocol Components, Outcomes, and Literature/Guideline Support.a
| Component “Bin” | Outcome(s) | Studies | Population Studied | Evidence | Guideline Support |
|---|---|---|---|---|---|
| Preoperative management | |||||
| Risk factor assessment | |||||
| Anemia | ↑ Postop transfusion, +/− LOS, infection, mortality; iron, Epo, preop donation → ↓ postop transfusion, +/− LOS, readmission | 2 SR, 2 RCT, 9 Obs | TKA/THA | + | NA |
| Diabetes | ↑ Infections (wound, UTI, and respiratory), ↑ pain, ↓ functional improvement | 1 SR, 13 Obs | TKA/THA | +++ | √√√ |
| Smoking | Cessation → ↓ Complications (wound, CV, and reoperation), ↓ pain | 2 RCT, 5 Obs | TKA/THA, spine, other surgical procedures | +++ | √ |
| Obesity | ↑ Implant failure/reoperation, superficial and deep SSI, DVT, reduced functional scores | 5 SR, 23 Obs | TKA/THA | +++ | √√√ |
| Malnutrition | ↑ LOS, wound complications | 9 Obs | TKA/THA | + | NA |
| Immune modulators | No consistent findings | 1 RCT, 5 Obs | TKA/THA | +/− | √ |
| Opiates/drug abuse | ↑ Opioid dependence postoperatively | 6 Obs | TKA/THA | + | √ |
| Preoperative education | ↓ LOS for TKA | 4 SR, 6 Obs | TKA/THA | +/− | NA |
| Preoperative bathing/ decolonization | ↓ SSI | 1 RCT, 3 Obs | TKA/THA | +++ | √√√ |
| Preoperative VTE prophylaxis | No difference in VTE vs postoperative initiation | 2 SR, 5 RCT | TKA/THA | +/− | √ |
| Intraoperative management | |||||
| Drains | No benefit; may ↑ complications/costs | 2 SR, 3 RCT, 7 Obs | TKA/THA | − | √√√ |
| Postoperative management | |||||
| Early mobilization | ↓ LOS | 1 SR, 1 RCT | TKA/THA | +++ | √√√ |
| Continuous passive motion | No effect | 1 SR, 2 RCT | TKA | − | √√√ |
| Extended duration VTE prophylaxis | ↓ Overall VTE rate, ↓DVT | 5 SR, 1 RCT | TKA/THA | + | √ |
| Early oral alimentation and enhanced nutrition | No effect | 1 SR | HFS | +/− | NA |
| Discharge planning/ discharge criteria | No consistent findings | 1 SR, 1 RCT, 7 Obs | TKA/THA | +/− | NA |
Abbreviations: CV, cardiovascular; DVT, deep vein thrombosis; EPO, erythropoietin; HFS, hip fracture surgery; LOS, length of stay; Obs, observational study; RCT, randomized clinical trial; SR, systematic review; SSI, surgical site infection; THA, total hip arthroplasty; TKA, total knee arthroplasty; UTI, urinary tract infection; VTE, venous thromboembolism.
aEvidence grading: +++, consistent evidence across studies showed benefit (interventions) or impact (risk assessment); +, evidence was either mixed with the majority favoring benefit/impact or little evidence existed in only one direction; +/−, evidence either did not exist or existed in both directions without one direction being favored; −, evidence showed no effect of a given practice or the intervention’s harms outweighed its benefits. Consistency with clinical guidelines: √√√, all guidelines supported a given practice or the guidelines cited strong evidence of support; √, some, but not all, guidelines supported a given practice or guidelines cited weak evidence or expert opinion.
Table 3.
Summary of Guidelines Supporting the Reviewed Components.a
| Component “Bin” | Procedure | Society | Yearb | Recommendation/Statement |
|---|---|---|---|---|
| Preoperative management | ||||
| Risk factor assessment | ||||
| Anemia | Not available | |||
| Diabetes | TKA | AAOS | 2015 | Patients with diabetes mellitus are at increased risk of complications (moderate evidence) |
| Smoking | THA | AAOS | 2017 | Tobacco users are at increased risk of complications (limited evidence) |
| Surgery | ACS SSI | 2016 | Cessation 4-6 weeks before surgery reduces risk of SSI and is recommended for all current smokers | |
| Obesity | THA | AAOS | 2017 | Obese patients may achieve lower clinical scores but a similar level of patient satisfaction and relative improvement in pain and function after surgery (moderate evidence) |
| THA | AAOS | 2017 | Obese patients are at increased risk of dislocation, superficial wound infection, and blood loss (limited evidence) | |
| TKA | AAOS | 2015 | Obese patients have less improvement in outcomes (strong evidence) | |
| Malnutrition | Not available | |||
| Opiates/drug abuse | TKA | AAOS | 2015 | Patients with select chronic pain conditions (eg, low-back pain) have less improvement in patient-reported outcomes (moderate evidence) |
| Immune modulators | TKA/THA | ACR/AAHKS | 2017 | For patients with rheumatoid arthritis, continue conventional agents (eg, methotrexate) and hold biologic agents (eg, TNF-α inhibitors) |
| Preoperative education | Not available | |||
| Preoperative bathing/ decolonization | Ortho | WHO | 2016 | Nasal carriers of Staphylococcus aureus should receive intranasal mupirocin +/− chlorhexidine body wash (strong recommendation) |
| Surgery | WHO | 2016 | Patients should bathe prior to surgery with plain or antimicrobial soap; inadequate evidence to assess chlorhexidine (conditional recommendation) | |
| Surgery | CDC SSI | 2017 | Patients should bathe prior to surgery with plain or antimicrobial soap at least the night before the operation (strong recommendation); optimal timing/number of applications/use of chlorhexidine unclear | |
| Ortho | ACS SSI | 2017 | Nasal carriers of Staphylococcus aureus should receive intranasal mupirocin +/− chlorhexidine body wash | |
| Preoperative VTE prophylaxis | Ortho | CHEST | 2012 | No preference preoperative versus postoperative initiation; however, if using LMWH, therapy should be initiated >12 hours before or after surgery compared to <4 hours before or after surgery |
| Intraoperative management | ||||
| Drains | TKA | AAOS | 2015 | There is no benefit to the use of drains with respect to complications or patient outcomes (strong evidence) |
| Postoperative management | ||||
| Early mobilization | THA | AAOS | 2017 | Postoperative physical therapy can improve early function (moderate evidence) |
| TKA | AAOS | 2015 | Rehabilitation started on the day of TKA reduces length of stay (strong evidence) and improves pain and function (moderate evidence) | |
| Continuous passive motion | TKA | AAOS | 2015 | Continuous passive motion after TKA does not improve outcomes (strong evidence) |
| Extended duration VTE prophylaxis | TKA/THA | AAOS | 2011 | Recommend use of pharmacologic agents and/or mechanical compressive devices for VTE prophylaxis, but they make no recommendation regarding which strategy or the duration of therapy |
| TKA/THA | CHEST | 2012 | Recommend therapy over no therapy; dual (pharmacologic and mechanical) over single; LMWH over fondaparinux, DOAC (apixaban, dabigatran, and rivaroxaban), UFH, VKA, or ASA; and therapy should be continued for up to 35 days | |
| THA | NICE | 2016 | Combined mechanical and pharmacologic prophylaxis; any of the following are acceptable with start times in parenthesis: dabigatran (1-4 hours), fondaparinux (6 hours), LMWH (6-12 hours), rivaroxaban (6-10 hours), UFH if renal impairment (6-12 hours) and continue for 28-35 days; timing based on manufacturer recommendations | |
| TKA | NICE | 2016 | Same as above but continue for 10-14 days | |
| Early oral alimentation and enhanced nutrition | Not available | |||
| Discharge planning/discharge criteria | Not available | |||
Abbreviations: AAHKS, Association of Hip and Knee Surgeons; AAOS, American Academy of Orthopedic Surgeons; ACR, American College of Rheumatology; ASA, aspirin; CDC, Centers for Disease Control; CHEST, The American College of Chest Physicians; DOAC, direct oral anticoagulant (eg, apixaban, dabigatran, and rivaroxaban); LMWH, low-molecular-weight heparin (eg, enoxaparin); NICE, National Institute for Health and Care Excellence; Ortho, orthopedic operations; SSI, surgical site infection; THA, total hip arthroplasty; TKA, total knee arthroplasty; TNF, tumor necrosis factor; UFH, unfractionated heparin; VKA, vitamin K antagonist (eg, warfarin); WHO, World Health Organization; VTE, venous thromboembolism.
aAdapted from American Academy of Orthopedic Surgeons,9 American College of Rheumatology/American Association of Hip and Knee Surgeons,10 American College of Surgeons and Surgical Infection Society,8 Centers for Disease Control and Prevention surgical site infection,11 CHEST,12 and National Institute for Health and Care Excellence.13
bYear includes published date or date guidelines were last updated, whichever is later.
Preoperative Management
Risk factor assessment: Preoperative anemia
Rationale
Anemia is common14 and may predispose patients to postoperative transfusion resulting in adverse clinical outcomes. Correction of anemia may prove beneficial prior to TKA/THA by reducing risk of transfusion.
Evidence
The literature search identified 170 articles, of which 13 met the inclusion criteria and were specific to total joint replacement: 2 SRs, 2 RCTs, and 9 observational studies. One SR14 and 4 observational studies15–18 show that preoperative anemia is associated with increased postoperative transfusion rate. However, the relationship with postoperative clinical outcomes (ie, LOS, mortality) is less clear. For example, 1 National Surgical Quality Improvement Program study16 found higher odds of 30-day mortality after TKA in patients with preoperative anemia but not in THA, while another study found no difference in mortality for either operation up to 1 year postoperatively.15 The most frequently used definition of anemia is the World Health Organization (WHO)19 classification using a hemoglobin <13 g/dL (men) and <12 g/dL (women). Two SRs,14,20 1 RCT,21 and several observational studies22–26 have shown iron (oral and intravenous) supplementation, erythropoietin, and preoperative autologous donation are effective in reducing postoperative allogenic transfusion; however, the benefit on clinical outcomes (ie, LOS and mortality) is unclear. Routine use of these strategies does not appear to benefit nonanemic patients.22,23
Summary and recommendations
All patients undergoing elective joint replacement should be screened for anemia, and if identified, appropriate evaluation and treatment prior to surgery should be coordinated with the patients’ care team, including their primary care provider.
Risk factor assessment: Diabetes mellitus
Rationale
Diabetes mellitus (DM) is prevalent in those undergoing elective joint replacement27,28 and may adversely affect outcomes. Preoperative optimization of diabetes may prove beneficial prior to TKA/THA for improving clinical outcomes.
Evidence
The literature search identified 126 articles, of which 14 met the inclusion criteria and were specific to total joint replacement: 1 SR and 13 observational studies. For TKA, 10 observational studies addressed preoperative DM and its relationship with outcomes,29–38 with 2 large studies (>10 000 patients) showing increased risk of mortality (odds ratio [OR]: 2.9930 and hazard ratio: 1.4931). These studies also found increased risk of postoperative pain,33,35,36 functional limitations,37 and periprosthetic infections.31,34,38 For THA, 1 SR/MA28 found an increased risk of surgical site infection (SSI; OR: 2.04), urinary tract infection (UTI; OR: 1.43), and respiratory tract infection (OR: 1.95). Three observational studies corroborated these findings.31,36,39 In both TKA and THA, studies demonstrated a dose–response curve between severity of DM (variably defined, eg, insulin dependent, with complications, hemoglobin [HbA1c] level) and probability of adverse outcomes.
There is some evidence to support increased risk of complications (primarily SSI) with HbA1c > 740 (within 1 year prior to surgery), HbA1c >841 (within 4 weeks prior to surgery), and fasting blood sugar >200 mg/dL (within 4 weeks prior to surgery).41 We identified no studies that addressed the impact of preoperative optimization of DM prior to undergoing elective TKA/THA on clinical outcomes. The American Academy of Orthopedic Surgery (AAOS) found moderate evidence that patients with DM are at an increased risk of complications.9
Summary and recommendations
Preoperative DM is associated with worse postoperative outcomes including wound complications, postoperative infections (UTI, respiratory), pain, functional impairment, and possibly mortality. Diabetes mellitus should be screened for and identified prior to undergoing joint replacement surgery and should be optimized through consultation with primary care or endocrinology. No clear cutoff value (or method) has been established, and for now, decisions about surgical management in diabetic patients should be individualized.
Risk factor assessment: Smoking/tobacco use
Rationale
Smoking and other tobacco use may increase the risk of adverse postoperative events, including wound healing complications, pulmonary complications, and other infections.
Evidence
The literature search identified 11 articles, of which 5 met the inclusion criteria and were specific to total joint replacement; 2 additional studies were retrieved via recommendation of the technical experts for a total of 7 included studies42–48: 2 RCTs and 5 observational studies.
One trial randomized patients scheduled for TKA/THA to weekly meetings and nicotine replacement.45 Sixty percent of intervention recipients stopped smoking compared to 7% of controls. Those who decreased smoking >50% had lower rates of postoperative complications (18% vs 52%, P < .01). A second RCT in a mixed surgical population also found reduced complications (21% vs 41%, P = .03) among those who partially or completely stopped smoking perioperatively.46 Additional observational evidence found increased complications among smokers43,47 and that smokers who quit for surgery may benefit from greater reductions in pain and improved wound healing.42,44
The AAOS guidelines found limited evidence that smokers are at an increased risk of complications.41 The ACS SSI guidelines recommend cessation of smoking 4 to 6 weeks prior to surgery to reduce the risk of SSI.8
Summary and recommendations
Smoking is associated with increased risk of postoperative complications. Preoperative interventions can help patients with cessation and can improve postoperative outcomes. Patients should abstain for at least 4 to 6 weeks preoperatively and postoperatively; this can be facilitated through counseling and nicotine replacement therapy.
Risk factor assessment: Obesity
Rationale
Obese patients may be at increased risk of adverse events and longer recovery following TKA/THA. Strategies to promote weight loss may prove beneficial.
Evidence
The literature search identified 372 articles, of which 28 met the inclusion criteria and were specific to total joint replacement: 5 SRs and 23 observational studies. For TKA, 3 SRs/MAs49–51 found higher rates of implant failure, 3 SRs/MAs49,51,52 found higher rates of SSI, and 1 SR/MA found higher rates of deep infection.49 Further, 1 SR/MA found lower functional scores postoperatively,49,50 and 1 SR/MA found higher rates of deep vein thrombosis (DVT). Additional observational studies corroborated these findings53–60 and suggested obese patients may be at increased risk of acute kidney injury (AKI) perioperatively.55,61 Similar findings were identified for THA including several observational studies showing increased rates of implant failure,53,57,62 SSI,53,55,59,60,62,63 AKI, and DVT. There appears to be a dose–response relationship with significant increases in adverse events among the morbidly obese (body mass index [BMI] >40).
One SR evaluated nonsurgical weight loss prior to joint replacement and actually found higher rates of complications and readmissions in the cohort that lost ≥5%.64 One observational study of patients undergoing TKA/THA following bariatric surgery found no difference in rates of complications between those who had undergone bariatric surgery and matched patients who had not.65
For THA, the AAOS guidelines found that obese patients have worse absolute outcome scores (moderate evidence) and increased risk of dislocation and wound infection (limited evidence).9 For TKA, the AAOS guidelines found strong evidence that obese patients have less outcome improvement than nonobese patients.9
Summary and recommendations
Obese patients, especially those with a BMI >40, are at increased risk of adverse outcomes and often experience delayed and dampened functional recovery. These risks should be discussed with patients and incorporated into individualized decision-making. There is insufficient data to support specific use of surgical or nonsurgical weight loss prior to undergoing joint replacement.
Risk factor assessment: Malnutrition
Rationale
Malnourished patients may be at increased risk of complications. Optimization of nutrition prior to elective TKA/THA may reduce adverse events.
Evidence
The literature search identified 179 articles, of which 9 met the inclusion criteria and were specific to total joint replacement (all observational).66–74 The included studies associated preoperative nutritional status with postoperative outcomes. Nutritional parameters varied and included serum markers (eg, albumin, lymphocyte count), nutrition surveys, and anthropomorphic (ie, body measurement) data. Outcome measures were heterogeneous and included SSI, wound complications, and LOS. Results were mixed with 1 negative study,66 3 with increased LOS,67,69,73 and 4 with increased rates of wound complications.68,71,72,74 However, individual markers of malnutrition were not consistently tied to outcomes; for example, 1 study found transferrin levels associated with wound complications but not lymphocyte count or albumin,71 while another study found anthropomorphic data associated with wound complications but not biochemical markers.72 No studies were identified that evaluated an intervention to optimize preoperative nutrition prior to TKA/THA.
Summary and recommendations
There is no consistent evidence regarding who should be screened for malnutrition or what measure should be used to assess malnutrition prior to TKA/THA. Malnourished patients may be at increased risk of complications including increased LOS and wound complications, but no studies have addressed nutrition optimization prior to surgery.
Risk factor assessment: Immune-modulating therapy
Rationale
Patients undergoing joint replacement for RA are often on immune-modulating drugs including steroids, conventional agents (eg, methotrexate [MTX]), and newer biologic/synthetic agents (eg, tumor necrosis factor α inhibitors). There is concern that these patients are at increased risk of complications.
Evidence
The literature search identified 424 articles, of which 6 met the inclusion criteria: 1 RCT and 5 observational studies. One RCT randomized elective orthopedic patients (including 121 TKA/THA) to continue MTX through the perioperative period.75 In adjusted analysis, there was no independent effect of MTX on postoperative outcomes. However, patients in this trial were on a variety of medications, and multivariate analysis did find strong associations between steroids, penicillamine, cyclosporine, and hydroxychloroquine and adverse outcomes. Five observational studies76–80 found no independent effect of immune-modulating therapy on wound or medical complications; however, these studies have methodologic limitations. None of these studies addressed the timing of discontinuation of agents nor did they address the ramifications of discontinuing therapy on rheumatoid symptoms. A collaboration between the American College of Rheumatology (ACR) and the Association of Hip and Knee Surgeons (AAHKS) recently released guidelines on this topic, including a comprehensive assessment of the literature—the majority of which was not specific to orthopedic operations.10 In brief, for patients with RA, they recommend perioperative continuation of conventional agents and holding biologic agents.
Summary and recommendations
There is limited evidence to guide clinicians on the perioperative management of immune-modulating drugs for TKA/THA. Recent guidelines from the ACR/AAHKS recommend continuing conventional agents and holding biologic agents in the perioperative period.
Risk factor assessment: Opiate use
Rationale
Pain is a dominant manifestation of OA and may increase the risk of developing opiate dependence. In all, 7% to 23% of THA patients and 10% to 34% of TKA patients have persistent pain following surgery.81 Understanding the relationship between preoperative opioid dependence and postoperative outcomes may assist with setting patient expectations.
Evidence
The literature search identified 9 articles, of which 3 met the inclusion criteria; 3 additional studies were retrieved via recommendation of the technical expert for a total of 6 included studies (all observational). Multiple observational studies have associated preoperative opioid use with negative postoperative outcomes.81–85 Large studies in patients undergoing TKA and THA have found that patients on preoperative opioids will often remain opioid dependent postoperatively and may be less satisfied with their clinical outcomes.82,85 For example, a cohort study of over 6000 patients found that 14% of patients prescribed preoperative narcotics remained on narcotics postoperatively, compared to 3% of patients not prescribed opiates preoperatively.82 The risk factors for persistent use included younger age, concomitant back pain, diabetes, use of hypnotics, and longer/higher use of opioids preoperatively.85 A small pilot study of 41 patients found that those who could successfully wean themselves of opioids prior to TKA/THA had greater improvements in patient-reported outcomes than those who did not wean (Western Ontario and McMaster Universities Arthritis Index 43.7 vs 17.8, P < .01).86
The AAOS guidelines found moderate evidence that patients with select chronic pain conditions (eg, low-back pain) may have less improvement in patient-reported outcomes following TKA.9
Summary and recommendations
The current evidence suggests that a fraction of patients on opioids preoperatively will be able to completely stop postoperatively, and of those who do, the time to cessation will be prolonged. Early evidence suggests that patients who can successfully wean themselves from opioids before surgery may have better outcomes than those who cannot. Information about long-term opioid use should be incorporated into discussions with patients before surgery.
Education/bootcamps
Rationale
Preoperative education may improve patient outcomes through improved informed consent and adherence to postoperative protocols.
Evidence
The literature search identified 248 articles, of which 10 met the inclusion criteria and were specific to total joint replacement: 4 SRs and 6 observational studies. Four SRs addressed preoperative education prior to joint replacement including a recent Cochrane SR/MA.87–90 Educational interventions were heterogeneous and included written and in-person materials, presented either inpatient or prior to admission. Pedagogies included audiovisual, written, and plastic models. Sessions were typically run by physiotherapists or nurses. Across multiple analyses, the only positive finding of the Cochrane review was a reduction in LOS for TKA (2 studies, 1.86 days). They found no benefit in pain, function, adverse events, and quality of life (QOL).
Summary and recommendations
While there is minimal objective evidence that preoperative education has a significant impact on measured postoperative outcomes, their inclusion is important for informed consent and shared decision-making, and educational efforts convey minimal risk. They are recommended to be incorporated into the ERP.
Bathing/Staphylococcus aureus decolonization
Rationale
Preoperative bathing and Staphylococcus aureus decolonization may reduce the risk of postoperative SSI.
Evidence
The literature search identified 37 articles, of which 3 met the inclusion criteria; 1 additional observational study was provided to us from a technical expert for a total of 4 studies (1 RCT and 3 observational). One RCT focused on preoperative bathing and 3 observational studies addressed Staphylococcus aureus decolonization.91–94 The RCT compared chlorhexidine cloths to soap and water in patients undergoing TKA/THA and found lower rates of periprosthetic infection in the chlorhexidine cohort (OR: 8.15 for control vs chlorhexidine); however, the statistical significance was borderline (P = .049, 95% confidence interval: 1.01-65.6), and the authors calculated a treatment effect as opposed to traditional intent-to-treat effect, reducing external validity. The observational pre–post studies, including a large multicenter study, found reduced SSI rates following the implementation of a screening/treatment program for S aureus colonization. An additional large observational study found reduced SSI rates following implementation of a universal decolonization procedure (without screening).94
Multiple organizations have issued guidelines related to preoperative bathing and decolonization including the ACS, Centers for Disease Control and Prevention, and the WHO.8,11,95 The consensus is that preoperative bathing with either plain or antimicrobial soap the night before surgery is beneficial. Further, especially in orthopedic patients, decolonization of nasal carriers of Stapholococus aureus (whether methicillin resistant or not) is recommended. These guidelines have not identified compelling evidence for the use of preoperative chlorhexidine cloths over soap and water.
Summary and recommendation
Patients undergoing elective joint replacement should bathe the night before surgery with soap and water. The evidence supporting the use of chlorhexidine wipes over soap and water is limited. The carriers of Staphylococcus aureus should be identified and a decolonizing regimen should be prescribed prior to undergoing surgery. Universal decolonization regimens have some observational support.
Preoperative VTE prophylaxis
Rationale
Chemical venous thromboembolism (VTE) prophylaxis is recommended for all patients undergoing elective total joint replacement. Questions remain however about whether VTE prophylaxis should be initiated preoperatively (focus of this section) and for how long prophylaxis should be continued postoperatively (focus of upcoming section titled extended duration VTE prophylaxis). Intraoperative stasis may contribute to the development of VTE; therefore, preoperative prophylaxis may reduce this risk, but potentially at the expense of increased bleeding.
Evidence
The literature search identified 235 articles, of which 7 met the inclusion criteria and were specific to total joint replacement: 2 SRs and 5 RCTs. A 2002 SR showed no difference in major bleeding and VTE rates comparing preoperative and postoperative low-molecular-weight heparin (LMWH) strategies in patients undergoing THA. Further, while they found that patients started on therapy perioperatively (ie, within 2-4 hours before or after surgery) did have slightly lower VTE rates (10.0% vs 15.3%), they also experienced much higher rates of major bleeding (3.5% vs 0.9%).96 Subsequent RCTs have randomized patients to preoperative versus postoperative regimens but using different agents, rendering direct comparisons difficult.97,98 Finally, a recent large registry study found no difference in bleeding, thromboembolic events, or complications when comparing preoperative and postoperative LMWH regimens.99
The American College of Chest Physicians (CHEST) guidelines for orthopedic VTE management do not favor preoperative or postoperative initiation but do recommend that therapy be started at least 12 hours before or after surgery as opposed to <4 hours before or after surgery.12
Summary and recommendations
While chemical VTE prophylaxis is recommended for all patients undergoing elective joint replacement, there is no convincing evidence favoring preoperative or postoperative initiation. There is evidence that immediate perioperative administration (within 2-4 hours before or after surgery) may increase bleeding disproportionately to the VTE risk reduction. Upcoming section titled extended duration will address extended duration of VTE prophylaxis.
Intraoperative Management
Drains
Rationale
Prophylactic drain placement may reduce hematoma formation and prevent wound infection.
Evidence
The literature search identified 212 articles, of which 12 met the inclusion criteria and were specific to total joint replacement: 2 SRs, 3 RCTs, and 7 observational studies. A Cochrane SR in 2007 for patients undergoing major orthopedic operations, including TKA/THA, found no difference in wound infections, hematoma, dehiscence, or reoperations with the routine placement of closed suction drains.100 A recent SR in patients undergoing TKA found no difference in LOS, postoperative function, or postoperative hemoglobin levels.101 These findings have been corroborated in additional RCTs102,103 and observational studies.104–106 The AAOS guidelines found strong evidence against the routine use of drains.9
Summary and recommendations
There is no evidence supporting the routine use of drains in patients undergoing elective joint replacement.
Postoperative Management
Early mobilization/ambulation
Rationale
Early mobilization may improve postoperative outcomes but potentially at the expense of wound disruption.
Evidence
The literature search identified 283 articles, of which 2 met the inclusion criteria and were specific to total joint replacement: 1 SR and 1 RCT. One SR/MA107 compared patients undergoing TKA/THA mobilized on postoperative day 0 (4 of 5 studies) or day 1 compared to controls (day 2 or later). Early mobilization reduced LOS by 1.8 days, with secondary outcomes (function, QOL, adverse events, patient satisfaction) no different or favoring early mobilization. One additional RCT108 randomized 119 THA patients to day of surgery mobilization versus day after surgery. This study was limited to nonobese, limited complexity (ASA score 2 or less) patients under the care of a single surgeon. They found an increased proportion of intervention patients were discharged at 48 or 72 hours, but no difference in mean LOS. Neither the SR nor the RCT explicitly describes the effect of early mobilization on rates of wound disruption. The AAOS guidelines found moderate (THA) and strong (TKA) evidence in favor of early mobilization for improving LOS and function.9
Summary and recommendations
Mobilization of patients on postoperative day 0 appears to be effective and safe. For the majority of patients, mobilization should begin within 24 hours of surgery unless a significant contraindication exists.
Continuous passive motion
Rationale
Passive mobilization of the knee following surgery may improve functional outcomes following TKA.
Evidence
The literature search identified 125 articles, of which 3 met the inclusion criteria and were specific to TKA: 1 SR and 2 RCTs. One SR/MA109 identified 24 RCTs that compared continuous passive motion (CPM) to standard postoperative care. Usage varied between studies ranging from 1.5 to 24 hours per day for 1 to 17 days, with treatment initiation between the first and fourth postoperative day. They found a small improvement in short-term range of motion (2 degrees) and decreased rate of subsequent surgical manipulations, but no difference in pain, medium/long-term function, QOL, adverse events, or LOS. Two RCTs have been published since this review,110,111 neither of which found benefit with respect to range of motion or QOL. The AAOS guidelines found strong evidence against the routine use of CPM in TKA.9
Summary and recommendations
Continuous passive motion has been studied extensively. There is no evidence of consistent benefit for range of motion, function, QOL, or LOS. Continuous passive motion is likely not as beneficial as alternative modalities such as early mobilization and physiotherapy.
Extended duration VTE thromboprophylaxis
Rationale
Chemical VTE prophylaxis is recommended for all patients undergoing elective total joint replacement. Questions remain however about whether VTE prophylaxis should be initiated preoperatively or postoperatively (focus of previous section titled preoperative VTE prophylaxis) and for how long prophylaxis should be continued postoperatively (focus of this section). In 2012, CHEST guidelines recommended extended duration prophylaxis for patients undergoing major orthopedic operations.12
Evidence
The literature search identified 1942 articles, of which 6 met the inclusion criteria and were specific to total joint replacement: 5 SRs and 1 RCT. A 2016 Cochrane review112 synthesized a large number of contemporary RCTs (referred to as “trials” below); to this, we added 4 additional SRs113–116 and 1 additional RCT117 that have been published since the Cochrane literature search concluded.
Heparins
Within the Cochrane review, 6 trials compared LMWH to placebo (ie, no extended prophylaxis), with evidence of reduced composite VTE (combining DVT and pulmonary embolus, symptomatic and asymptomatic) and asymptomatic DVT.
Vitamin K antagonists
Within the Cochrane review, 1 trial compared warfarin to placebo and showed reduced composite VTE. An additional trial in the Cochrane review compared LMWH to a warfarin derivative and found no difference in total VTE.
Two additional studies addressed vitamin K antagonists (VKAs). A 2015 RCT117 compared fixed low-dose warfarin to variable warfarin (ie, targeting an International Normalized Ratio [INR]) and fondaparinux and found no difference in VTE. A network SR/MA of 94 RCTs114 assessed 12 different prophylaxis strategies and concluded that variable warfarin conveyed the highest risk of DVT.
Direct oral anticoagulants (eg, rivaroxaban, apixaban)
Within the Cochrane review, 2 trials evaluated rivaroxaban versus placebo, both showing reduced symptomatic DVT and one showing reduced composite VTE. Five of the included trials compared direct oral anticoagulants (DOACs) to heparins (predominantly LMWH) demonstrating reduced composite VTE.
Two additional studies addressed DOACs. An SR/MA115 of 18 RCTs found reduced composite VTE for DOACs compared to LMWH. The network SR/MA of 94 RCTs114 also concluded that DOACs had the lowest risk of asymptomatic and symptomatic DVT compared to other prophylaxis strategies. Limited evidence exists comparing DOACs to one another.
Aspirin
A recent SR/MA focused exclusively on ASA.116 The quality of included studies limited conclusions, but they did not find any evidence to support the use of aspirin over other agents.
Timing and duration
No studies evaluated the optimal first dose timing. The RCTs typically follow manufacturer’s guidelines, although lessons from various studies indicate that the safety of DOACs may be improved by delaying the first postoperative dose for at least 6 hours after surgery. Eligibility for inclusion in the Cochrane review required a minimum duration of therapy of 35 days. Contemporary RCTs differ with respect to therapy duration, but most are between 4 and 5 weeks.
Bleeding
The Cochrane review did not find increased rates of major or clinically relevant bleeding when comparing heparin to placebo, warfarin to placebo, DOAC to placebo, or DOAC to heparin; 1 trial within the review did find higher rates of major bleeding in warfarin compared to heparin (in THA only).
The network SR/MA similarly found no statistical difference in major hemorrhage comparing LMWH to VKA, ASA, or DOACs.114 One SR did find statistically different rates of bleeding between different DOACs.115
Guidelines
The AAOS guidelines recommend the use of chemical and/or mechanical prophylaxis but do not recommend one chemical strategy over another nor do they make specific reference to duration of therapy.9 CHEST guidelines recommend chemical prophylaxis, ideally combined with mechanical prophylaxis, with LMWH preferred over fondaparinux/DOACs/unfractionated heparin (UFH)/VKA/ASA.12 CHEST guidelines further recommend continuing therapy for up to 35 days (TKA or THA). Finally, National Institute for Health and Care Excellence guidelines recommend dual (chemical and mechanical) prophylaxis with no preference between DOACs, LMWH, fondaparinux, and UFH for 28 to 35 days (THA) or 10 to 14 days (TKA).1
Summary and recommendations
Extended duration of pharmacologic prophylaxis appears to be safe and effective at reducing total VTE. While heparins (namely, LMWH), warfarin, aspirin, and DOACs are all effective in preventing VTE, there is some comparative evidence that DOACs may be the most efficacious. Little comparative data directly compare DOACs to one another. No consensus exists regarding optimal duration of therapy, although 4 to 5 weeks is a common target.
Early oral alimentation and enhanced nutrition
Rationale
Prolonged fasting can harm patients recovering from major surgery; early enteral nutrition may improve patient outcomes.
Evidence
The literature search identified 52 articles, of which none met the inclusion criteria. One SR in hip fracture surgery is summarized below.
No studies addressed early alimentation or enhanced postoperative nutrition in patients undergoing elective joint replacement. One SR in patients undergoing hip fracture surgery118 found that oral multinutrient feeds (eg, Boost, Ensure, Sustagen) may reduce complications (eg, pressure sores). They found no support for nasogastric feeds, vitamin/mineral supplementation, or high protein intake. One study included in the SR showed that dietetic assistants may reduce mortality but had no effect on complications. Patients undergoing elective surgery are likely at reduced risk of complications or nutrition-mediated mortality, so these benefits may not apply.
Summary and recommendations
No evidence exists to guide postoperative nutrition in patients undergoing elective joint replacement. In hip fracture surgery, there is no benefit of nasogastric feeds, high protein intake, or vitamin/mineral supplementation. Patients should be fed a regular (or comorbidity appropriate) diet as soon as they are able to tolerate following surgery.
Discharge planning/discharge criteria
Rationale
Early identification of patients at risk of nonhome discharge may allow swifter placement and improve patient outcomes.
Evidence
The literature search identified 529 articles, of which 9 met the inclusion criteria: 1 SR, 1 RCT, and 7 observational studies. Two studies have developed indices to predict discharge based on preoperative variables (eg, age, QOL) with reasonable sensitivity/specificity.119,120 One study found functional assessments completed after admission could predict timing of discharge.121 The literature associating discharge location with patient outcomes has significant limitations due to the number of settings (eg, home health, acute and subacute rehab, skilled nursing) and lack of standardized outcome measurement. For example, discharge to inpatient rehabilitation may reduce risk of readmission122 but may also result in smaller gains in physical QOL measures.123,124 Patients receiving home health may reach goals more quickly than patients receiving subacute rehabilitation,125 while discharge to a skilled nursing facility (SNF) may be associated with higher readmission rates.126 Finally, one RCT randomized THA patients to an enhanced discharge intervention including education and home visits for wound care and medical therapy.127 While small (n = 50), this study found significant cost savings as well as possible improvements in objective funtional measures.
Summary and reccomendations
Discharge planning is an important component of any ERP. Discharge planning should begin well before surgery and involve a multidisciplinary approach including physical therapists, case managers, and social workers. There is insufficient evidence to guide identification strategies or to conclude which settings are best suited to optimize patient outcomes.
Discussion
A vast and growing body of literature exists to help guide clinicians as they implement ERPs in elective joint replacement. Institutions that have introduced ERPs have been able to improve patient outcomes including reduced complications and shorter LOS.1–4 This ultimately translates to lower costs128,129—a factor especially relevant to orthopedic surgeons in the era of episode-based payments. This review includes 16 surgical components potentially relevant to developing a total joint ERP, supported through primary literature, clinical practice guidelines, and/or expert consensus. While the level of support varies in its strength from one bin to the next, there is clear evidence that a number of interventions can improve patient outcomes.
Many of the interventions outlined in this review should be a part of a comprehensive evaluation and discussion with patients before surgery. While the ultimate goal should be reducing adverse events and enhancing recovery, setting appropriate expectations for patients and their families is critical. Screening for anemia, DM, obesity, tobacco use, and opiate dependence can identify cohorts who may have increased risk of transfusion, postoperative infections, wound complications, reoperations, chronic opioid use, and possibly, higher mortality. The literature supporting and optimizing these criteria is, unfortunately, limited, but there is some evidence that correcting preoperative anemia, encouraging smoking cessation through education and nicotine replacement, and opiate weaning prior to surgery can mitigate risk. These assessments should be considered a part of comprehensive preoperative evaluation and included as a part of the ERP.
Key ERP components beyond the preoperative risk assessment include those related to SSI prevention, VTE reduction, and enhancing mobility. Preoperative bathing with soap and water should be routine, and protocols should be developed to screen/decolonize those individuals colonized with Staphylococcus aureus. Routine use of drains should be discouraged. Mobilizing patients as soon as possible appears to decrease LOS and should be incorporated into an ERP in lieu of CPM. Chemical VTE prophylaxis should begin either 12 hours prior to or 12 hours following surgery and should be continued for 4 to 5 weeks postoperatively. Finally, it should be acknowledged that practices beyond those discussed here are also likely beneficial to perioperative care. Examples of these practices include guideline-based administration of prophylactic antibiotics (with discontinuation at the end of the procedure), intraoperative skin prep with an alcohol-based solution, and early discontinuation of Foley catheters.7,8,130
In summary, this study provides a review for 16 possible components of an ERP for total joint replacement. Importantly, 7 of these components fall under the category of preoperative evaluation and optimization. The other 8 components represent multidisciplinary processes of care that are evidence-based best practices. Combined with the anesthesia components (reported separately, Appendix A), consistent delivery of the complete ERP will provide patients with the best opportunity for a swift and complete recovery.
Conclusions
This review of 16 surgical bins for enhanced recovery in total joint replacement represents one component of AHRQ Safety Program for Improving Surgical Care and Recovery. Participating hospitals will also be provided state-of-the-art guidance in translating these evidence-based practices into their own clinical settings, with the ultimate goal of improving perioperative care at the national level.
Acknowledgments
The authors would like to thank Evans Whitaker, MD, MLIS, for assistance with search term generation.
Appendix A
Table A1.
Reviewed TKA/THA Protocol Components, Including Anesthesia.
| Preoperative management |
| Risk factor assessment |
| Anemia |
| Diabetes mellitus |
| Tobacco use/smoking |
| Obesity |
| Nutrition |
| Immune modulators |
| Opiates/drug abuse |
| Preoperative education |
| Preoperative bathing/decolonization |
| Preoperative VTE prophylaxis |
| Immediate preoperative management |
| Carbohydrate loading and reduced fastinga |
| Multimodal preanesthesia medicationsa |
| Multimodal postoperative nausea and vomiting prophylaxisa |
| Intraoperative management |
| Drains |
| Antibiotic prophylaxisa |
| Standard intraoperative anesthesia pathwaya |
| Tranexamic acida |
| Fluids/goal-directed fluid therapya |
| Glycemic controla |
| Multimodal postoperative nausea and vomiting prophylaxisa |
| Standard intraoperative analgesic pathway |
| Postoperative management |
| Standard postoperative multimodal analgesic regimena |
| Glycemic controla |
| Early mobilization |
| Continuous passive motion |
| Extended duration VTE prophylaxis |
| Early oral alimentation and enhanced nutrition |
| Discharge planning / discharge criteria |
Abbreviations: THA, total hip arthroplasty; TKA, total knee arthroplasty; VTE, venous thromboembolism.
aProtocol component is reported in separate, anesthesia-focused, article.
Appendix B
Table B1.
MEDLINE Search Terms.
| Component “Bin” | Search Terms | ||
|---|---|---|---|
| Operation | Bin | Qualifiers | |
| Preoperative management | |||
| Anemia | ((“Hip Fractures”[Mesh] OR “Intertrochanteric Fractures”[tiab] OR “Subtrochanteric Fractures”[tiab] OR “Intertrochanteric Fracture”[tiab] OR “Subtrochanteric Fracture”[tiab] OR “hip fracture”[tiab] OR “hip fractures”[tiab])) OR ((Arthroplasty, Replacement, Knee[Mesh]) OR “knee replacement”[tiab]) OR “knee arthroplasty”[tiab]) OR “knee replacements”[tiab]) OR “knee arthroplasties”[tiab]) OR “total knee”[tiab]) OR Arthroplasty, Replacement, Hip [Mesh]) OR “hip replacement”[tiab]) OR “hip arthroplasty”[tiab]) OR “hip replacements”[tiab]) OR “hip arthroplasties”[tiab]) OR “total hip”[tiab]) OR “hip prosthesis implantation”[tiab]) OR “hip prosthesis implantations”[tiab]) | anemia[tw] | (preop*[tw] OR pre-op*[tw]) AND English[lang] |
| Diabetes | (“Arthroplasty, Replacement, Hip”[Mesh] OR “Arthroplasty, Replacement, Knee”[Mesh] OR “Hip Fractures”[Mesh] OR “Arthroplasty, Replacement, Hip”[all fields] OR “Arthroplasty, Replacement, Knee”[all fields] OR “Hip Fractures”[all fields] OR “prosthetic joint”[all fields]) | (“Diabetes Mellitus”[Mesh] OR “Diabetes Mellitus, Type 2”[Mesh] OR “Hemoglobin A, Glycosylated”[Mesh] OR “Hemoglobin A, Glycosylated/analysis”[Mesh] OR “Hyperglycemia”[Mesh] OR “hyperglycemia/complications”[mesh terms] OR “blood glucose”[mesh terms] OR “Diabetes complications/blood”[mesh terms] OR “diabetes mellitus/blood”[mesh terms] OR “Diabetes Mellitus”[all fields] OR “Diabetes Mellitus, Type 2”[all fields] OR “Hemoglobin A, Glycosylated”[all fields] OR “Hyperglycemia”[all fields] OR “glycemic markers”[all fields] OR “blood glucose”[all fields]) | (“Preoperative Period”[Mesh] OR “Preoperative Care”[Mesh] OR “Preoperative Period”[all fields] OR “Preoperative Care”[all fields] OR “outcome”[all fields]) AND English[lang] |
| Smoking | (“Smoking”[Mesh] OR “Smoking Cessation”[Mesh] OR “Tobacco Smoke Pollution”[Mesh] OR “Smoking”[all fields] OR “Smoking Cessation”[all fields] OR “Tobacco Smoke Pollution”[all fields]) | ||
| Obesity | (“Arthroplasty, Replacement, Knee”[Mesh] OR “knee replacement”[tiab] OR “knee replacements”[tiab] OR “knee arthroplasty”[tiab] OR “knee arthroplasties”[tiab] or “total knee”[tiab] OR “Arthroplasty, Replacement, Hip”[Mesh] OR “hip replacement”[tiab] OR “hip replacements”[tiab] OR “hip arthroplasty”[tiab] OR “hip arthroplasties”[tiab] OR “total hip”[tiab] OR “hip prosthesis implantation”[tiab] or “hip prosthesis implantations”[tiab] OR “Arthroplasty, Replacement”[Mesh] OR “total joint arthroplasty”[tiab] OR “total joint”[tiab]”) | (“Body Mass Index”[mesh] OR “body mass index”[tiab] OR “overweight”[mesh] OR “overweight”[tiab] OR “obesity”[mesh] OR “obesity”[tiab] OR “obesity, morbid”[mesh] or “morbid obesity”[tiab]) | |
| Nutrition | (Arthroplasty, Replacement, Knee[Mesh]) OR “knee replacement”[tiab]) OR “knee arthroplasty”[tiab]) OR “knee replacements”[tiab]) OR “knee arthroplasties”[tiab]) OR “total knee”[tiab]) OR Arthroplasty, Replacement, Hip [Mesh]) OR “hip replacement”[tiab]) OR “hip arthroplasty”[tiab]) OR “hip replacements”[tiab]) OR “hip arthroplasties”[tiab]) OR “total hip”[tiab]) OR “hip prosthesis implantation”[tiab]) OR “hip prosthesis implantations”[tiab] | (“nutrition”[tiab]) OR “Nutritional Status”[Mesh] | NA |
| Immune modulators | ((“Antirheumatic Agents”[Mesh]) OR (“Tumor Necrosis Factor-alpha/antagonists and inhibitors”[Mesh])) OR “Immunosuppressive Agents”[Mesh] | NA | |
| Opiates/Drug Abuse | (“opiate dependent”[tiab]) OR “opioid dependent”[tiab]) OR “opiate dependence”[tiab]) OR “Opioid-Related Disorders”[Mesh] | NA | |
| Education | Patient Education as Topic[mesh] OR “pre-operative education”[tiab] OR “preoperative education”[tiab] | NA | |
| Bathing/decolonization | bath*[tw] OR clean*[tw] OR clorhex*[tw] | preop*[tw] | |
| VTE prophylaxis | “Thromboembolism”[Mesh] OR “thromboembolism”[tw] OR “thromboprophylaxis”[tw] | “Preoperative”[tw] OR “intraoperative”[tw] | |
| Intraoperative | |||
| Drains | Arthroplasty, Replacement, Hip”[All Fields] OR “Arthroplasty, Replacement, Knee”[All Fields] OR “Hip Fractures”[All Fields] OR “Arthroplasty, Replacement, Hip”[All Fields] OR “Arthroplasty, Replacement, Knee”[All Fields] OR “Hip Fractures”[All Fields] OR “prosthetic joint”[All Fields] | “drain”[All Fields] | English [lang] |
| Postoperative | |||
| Early mobilization | Arthroplasty, Replacement, Knee[Mesh]) OR “knee replacement”[tiab]) OR “knee arthroplasty”[tiab]) OR “knee replacements”[tiab]) OR “knee arthroplasties”[tiab]) OR “total knee”[tiab]) OR Arthroplasty, Replacement, Hip [Mesh]) OR “hip replacement”[tiab]) OR “hip arthroplasty”[tiab]) OR “hip replacements”[tiab]) OR “hip arthroplasties”[tiab]) OR “total hip”[tiab]) OR “hip prosthesis implantation”[tiab]) OR “hip prosthesis implantations”[tiab] | (“early ambulation”[tw]) OR “early mobilization”[tw] | NA |
| Continuous passive motion | “Motion Therapy, Continuous Passive”[Mesh] OR “continuous passive motion”[tiab] OR “CPM therapy”[tiab] OR “CPM therapies”[tiab] | NA | |
| VTE thromboprophylaxis | “Thromboembolism”[Mesh] OR “thromboembolism”[tw] OR “thromboprophylaxis”[tw] | NA | |
| Early oral alimentation and enhanced nutrition | ((“Hip Fractures”[Mesh] OR “Intertrochanteric Fractures”[tiab] OR “Subtrochanteric Fractures”[tiab] OR “Intertrochanteric Fracture”[tiab] OR “Subtrochanteric Fracture”[tiab] OR “hip fracture”[tiab] OR “hip fractures”[tiab])) OR (Arthroplasty, Replacement, Knee[Mesh]) OR “knee replacement”[tiab]) OR “knee arthroplasty”[tiab]) OR “knee replacements”[tiab]) OR “knee arthroplasties”[tiab]) OR “total knee”[tiab]) OR Arthroplasty, Replacement, Hip [Mesh]) OR “hip replacement”[tiab]) OR “hip arthroplasty”[tiab]) OR “hip replacements”[tiab]) OR “hip arthroplasties”[tiab]) OR “total hip”[tiab]) OR “hip prosthesis implantation”[tiab]) OR “hip prosthesis implantations”[tiab]) | nutrition”[tiab] OR “feeding”[tiab] OR “alimentation”[tiab] or “enteral”[tiab] | (“Postoperative Period”[Mesh]) OR (“postoperative”[tiab] OR “postop”[tiab] OR “post-operative”[tiab] OR “post-op”[tiab]) |
| Discharge planning/ discharge criteria | (“Arthroplasty, Replacement, Hip”[Mesh] OR “Arthroplasty, Replacement, Knee”[Mesh] OR “Hip Fractures”[Mesh] OR “Arthroplasty, Replacement, Hip”[all fields] OR “Arthroplasty, Replacement, Knee”[all fields] OR “Hip Fractures”[all fields] OR “prosthetic joint”[all fields]) | (“Patient discharge”[Mesh] OR “Patient discharge”[all fields]) | English[lang] |
Appendix C
Example PRISMA Flow Diagram and Inclusion/Exclusion Criteria for Each Reviewed Component
Operation: Joints (total hip arthroplasty [THA]; total knee arthroplasty [TKA]) Bin: Pre/perioperative management of immune-modulating drugs (biologics, disease-modifying drugs, etc) Inclusion Criteria:
Patients: Adult patients undergoing elective TKA or THA for rheumatoid arthritis
Intervention: Patients on immune-modulating drugs
Comparisons: Patients on alternative therapies or not on immune-modulating drugs
Outcome(s): Postoperative outcomes
Study Design(s): Systematic reviews, randomized controlled trials, observational studies Exclusion Criteria: Non-English, nonsystematic reviews, editorials, case reports, articles focused only on NSAIDs/COX2 inhibitors or corticosteroids.
Authors’ Note: The opinions expressed in this document are those of the authors and do not reflect the official position of Agency for Healthcare Research and Quality or the US Department of Health and Human Services. Elizabeth C. Wick is currently affiliated to Department of Surgery, University of California San Francisco, San Francisco, CA, USA.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Dr. Christopher Childers receives salary support through the AHRQ (F32HS025079). Dr Anaar Siletz receives salary support through NHLBI (F32HL134269). Drs Clifford Ko and Elizabeth Wick receive salary support through the AHRQ contract (HHSP233201500020I). Dr. Melinda Gibbons receives a consultant fee through the AHRQ contract (HHSP233201500020I). Dr. Gregory Golladay receives consultant, royalties, stock, paid presentations, and research support from OrthoSensor, Inc.; he is the publications committee chair for AAHKS; board member for the Virgina Orthopaedic Society; and on the editorial board of Journal of Arthroplasty. Dr. Stephen Kates is the editor-in-chief for Geriatric Orthopaedic Surgery & Rehabilitation.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This project was funded under contract number HHSP233201500020I from the Agency for Healthcare Research and Quality, US Department of Health and Human Services.
ORCID iD: Christopher P. Childers, MD http://orcid.org/0000-0002-6489-8222
References
- 1. Ni TG, Yang HT, Zhang H, Meng HP, Li B. Enhanced recovery after surgery programs in patients undergoing hepatectomy: a meta-analysis. World J Gastroenterol. 2015;21(30):9209–9216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Greco M, Capretti G, Beretta L, Gemma M, Pecorelli N, Braga M. Enhanced recovery program in colorectal surgery: a meta-analysis of randomized controlled trials. World J Surg. 2014;38(6):1531–1541. [DOI] [PubMed] [Google Scholar]
- 3. Ibrahim MS, Twaij H, Giebaly DE, Nizam I, Haddad FS. Enhanced recovery in total hip replacement: a clinical review. Bone Joint J. 2013;95-B(12):1587–1594. [DOI] [PubMed] [Google Scholar]
- 4. Ibrahim MS, Alazzawi S, Nizam I, Haddad FS. An evidence-based review of enhanced recovery interventions in knee replacement surgery. Ann R Coll Surg Engl. 2013;95(6):386–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. ERAS Compliance Group. The impact of enhanced recovery protocol compliance on elective colorectal cancer resection: results from an international registry. Ann Surg. 2015;261(6):1153–1159. [DOI] [PubMed] [Google Scholar]
- 6. Abeles A, Kwasnicki RM, Darzi A. Enhanced recovery after surgery: current research insights and future direction. World J Gastrointest Surg. 2017;9(2):37–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ban KA, Gibbons MM, Ko CY, Wick EC. Surgical technical evidence review for colorectal surgery conducted for the ahrq safety program for improving surgical care and recovery. J Am Coll Surg. 2017;225(4):548–557.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ban KA, Minei JP, Laronga C, et al. American College of Surgeons and Surgical Infection Society: surgical site infection guidelines, 2016 update. J Am Coll Surg. 2017;224(1):59–74. [DOI] [PubMed] [Google Scholar]
- 9. American Academy of Orthopedic Surgeons. Clinical Practice Guidelines. https://www.aaos.org/guidelines/?ssopc=1. Accessed September 25th, 2017.
- 10. Goodman SM, Springer B, Guyatt G, et al. 2017 American College of Rheumatology/American Association of Hip and Knee Surgeons guideline for the perioperative management of antirheumatic medication in patients with rheumatic diseases undergoing elective total hip or total knee arthroplasty. J Arthroplasty. 2017;32(9):2628–2638. [DOI] [PubMed] [Google Scholar]
- 11. Segreti J, Parvizi J, Berbari E, Ricks P, Berrios-Torres SI. Introduction to the Centers for Disease Control and Prevention and healthcare infection control practices advisory committee guideline for prevention of surgical site infection: prosthetic joint arthroplasty section. Surg Infect (Larchmt). 2017;18(4):394–400. [DOI] [PubMed] [Google Scholar]
- 12. Falck-Ytter Y, Francis CW, Johanson NA, et al. Prevention of VTE in orthopedic surgery patients: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012;141(suppl 2):e278S–e325S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. National Institute for Health and Care Excellence. Venous thromboembolism: reducing the risk for patients in hospital. https://www.nice.org.uk/guidance/cg92. Updated June 2015. Accessed September 25th, 2017.
- 14. Spahn DR. Anemia and patient blood management in hip and knee surgery: a systematic review of the literature. Anesthesiology. 2010;113(2):482–495. [DOI] [PubMed] [Google Scholar]
- 15. Greenky M, Gandhi K, Pulido L, Restrepo C, Parvizi J. Preoperative anemia in total joint arthroplasty: is it associated with periprosthetic joint infection? Clin Orthop Relat Res. 2012;470(10):2695–2701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hart A, Khalil JA, Carli A, Huk O, Zukor D, Antoniou J. Blood transfusion in primary total hip and knee arthroplasty. Incidence, risk factors, and thirty-day complication rates. J Bone Joint Surg Am. 2014;96(23):1945–1951. [DOI] [PubMed] [Google Scholar]
- 17. Jans O, Jorgensen C, Kehlet H, Johansson PI. Role of preoperative anemia for risk of transfusion and postoperative morbidity in fast-track hip and knee arthroplasty. Transfusion. 2014;54(3):717–726. [DOI] [PubMed] [Google Scholar]
- 18. To J, Sinha R, Kim SW, et al. Predicting perioperative transfusion in elective hip and knee arthroplasty: a validated predictive model. Anesthesiology. 2017;127(2):317–325. [DOI] [PubMed] [Google Scholar]
- 19. Freischlag JA. The operating room dance. BMJ Qual Saf. 2012;21(1):1. [DOI] [PubMed] [Google Scholar]
- 20. Alsaleh K, Alotaibi GS, Almodaimegh HS, Aleem AA, Kouroukis CT. The use of preoperative erythropoiesis-stimulating agents (ESAs) in patients who underwent knee or hip arthroplasty: a meta-analysis of randomized clinical trials. J Arthroplasty. 2013;28(9):1463–1472. [DOI] [PubMed] [Google Scholar]
- 21. Bernabeu-Wittel M, Romero M, Ollero-Baturone M, et al. Ferric carboxymaltose with or without erythropoietin in anemic patients with hip fracture: a randomized clinical trial. Transfusion. 2016;56(9):2199–2211. [DOI] [PubMed] [Google Scholar]
- 22. Bou Monsef J, Buckup J, Mayman D, Marx R, Ranawat A, Boettner F. Targeted preoperative autologous blood donation in total knee arthroplasty reduces the need for postoperative transfusion. HSS J. 2013;9(3):214–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Bou Monsef J, Figgie MP, Mayman D, Boettner F. Targeted pre-operative autologous blood donation: a prospective study of two thousand and three hundred and fifty total hip arthroplasties. Int Orthop. 2014;38(8):1591–1595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Enko D, Wallner F, von-Goedecke A, Hirschmugl C, Auersperg V, Halwachs-Baumann G. The impact of an algorithm-guided management of preoperative anemia in perioperative hemoglobin level and transfusion of major orthopedic surgery patients. Anemia. 2013;2013:641876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kotze A, Carter LA, Scally AJ. Effect of a patient blood management programme on preoperative anaemia, transfusion rate, and outcome after primary hip or knee arthroplasty: a quality improvement cycle. British J Anaesth. 2012;108(6):943–952. [DOI] [PubMed] [Google Scholar]
- 26. Rashiq S, Jamieson-Lega K, Komarinski C, Nahirniak S, Zinyk L, Finegan B. Allogeneic blood transfusion reduction by risk-based protocol in total joint arthroplasty. Can J Anaesth. 2010;57(4):343–349. [DOI] [PubMed] [Google Scholar]
- 27. Hu F, Jiang C, Shen J, Tang P, Wang Y. Preoperative predictors for mortality following hip fracture surgery: a systematic review and meta-analysis. Injury. 2012;43(6):676–685. [DOI] [PubMed] [Google Scholar]
- 28. Tsang ST, Gaston P. Adverse peri-operative outcomes following elective total hip replacement in diabetes mellitus: a systematic review and meta-analysis of cohort studies. Bone Joint J. 2013;95-B(11):1474–1479. [DOI] [PubMed] [Google Scholar]
- 29. Adams AL, Paxton EW, Wang JQ, et al. Surgical outcomes of total knee replacement according to diabetes status and glycemic control, 2001 to 2009. J Bone Joint Surg Am. 2013;95(6):481–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Belmont PJ, Jr, Goodman GP, Waterman BR, Bader JO, Schoenfeld AJ. Thirty-day postoperative complications and mortality following total knee arthroplasty: incidence and risk factors among a national sample of 15,321 patients. J Bone Joint Surg Am. 2014;96(1):20–26. [DOI] [PubMed] [Google Scholar]
- 31. Chrastil J, Anderson MB, Stevens V, Anand R, Peters CL, Pelt CE. Is hemoglobin a1c or perioperative hyperglycemia predictive of periprosthetic joint infection or death following primary total joint arthroplasty? J Arthroplasty. 2015;30(7):1197–1202. [DOI] [PubMed] [Google Scholar]
- 32. Clement ND, MacDonald D, Burnett R, Breusch SJ. Diabetes does not influence the early outcome of total knee replacement: a prospective study assessing the Oxford knee score, short form 12, and patient satisfaction. Knee. 2013;20(6):437–441. [DOI] [PubMed] [Google Scholar]
- 33. Fisher DA, Dierckman B, Watts MR, Davis K. Looks good but feels bad: factors that contribute to poor results after total knee arthroplasty. J Arthroplasty. 2007;22(6 suppl 2):39–42. [DOI] [PubMed] [Google Scholar]
- 34. Jamsen E, Nevalainen P, Kalliovalkama J, Moilanen T. Preoperative hyperglycemia predicts infected total knee replacement. Eur J Intern Med. 2010;21(3):196–201. [DOI] [PubMed] [Google Scholar]
- 35. Meding JB, Reddleman K, Keating ME, et al. Total knee replacement in patients with diabetes mellitus. Clin Orthop Relat Res. 2003(416):208–216. [DOI] [PubMed] [Google Scholar]
- 36. Rajamaki TJ, Jamsen E, Puolakka PA, Nevalainen PI, Moilanen T. Diabetes is associated with persistent pain after hip and knee replacement. Acta Orthop. 2015;86(5):586–593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Singh JA, Lewallen DG. Diabetes: a risk factor for poor functional outcome after total knee arthroplasty. PLoS One. 2013;8(11):e78991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Watts CD, Houdek MT, Wagner ER, Abdel MP, Taunton MJ. Insulin dependence increases the risk of failure after total knee arthroplasty in morbidly obese patients. J Arthroplasty. 2016;31(1):256–259. [DOI] [PubMed] [Google Scholar]
- 39. Jenny JY, Adamczewski B, De Thomasson E, et al. Can the presence of an infection be predicted before a revision total hip arthroplasty? Preliminary study to establish an infection score. Orthop Traumatol Surg Res. 2016;102(2):161–165. [DOI] [PubMed] [Google Scholar]
- 40. Harris AH, Bowe TR, Gupta S, Ellerbe LS, Giori NJ. Hemoglobin A1C as a marker for surgical risk in diabetic patients undergoing total joint arthroplasty. J Arthroplasty. 2013;28(suppl 8):25–29. [DOI] [PubMed] [Google Scholar]
- 41. Hwang JS, Kim SJ, Bamne AB, Na YG, Kim TK. Do glycemic markers predict occurrence of complications after total knee arthroplasty in patients with diabetes? Clin Orthop Relat Res. 2015;473(5):1726–1731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Behrend C, Schonbach E, Coombs A, Coyne E, Prasarn M, Rechtine G. Smoking cessation related to improved patient-reported pain scores following spinal care in geriatric patients. Geriatr Orthop Surg Rehabil. 2014;5(4):191–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Fisher L, Fisher A, Pavli P, Davis M. Perioperative acute upper gastrointestinal haemorrhage in older patients with hip fracture: incidence, risk factors and prevention. Aliment Pharmacol Ther. 2007;25(3):297–308. [DOI] [PubMed] [Google Scholar]
- 44. Glassman SD, Anagnost SC, Parker A, Burke D, Johnson JR, Dimar JR. The effect of cigarette smoking and smoking cessation on spinal fusion. Spine (Phila Pa 1976). 2000;25(20):2608–2615. [DOI] [PubMed] [Google Scholar]
- 45. Lindstrom D, Sadr Azodi O, Wladis A, et al. Effects of a perioperative smoking cessation intervention on postoperative complications: a randomized trial. Ann Surg. 2008;248(5):739–745. [DOI] [PubMed] [Google Scholar]
- 46. Moller AM, Villebro N, Pedersen T, Tonnesen H. Effect of preoperative smoking intervention on postoperative complications: a randomised clinical trial. Lancet. 2002;359(9301):114–117. [DOI] [PubMed] [Google Scholar]
- 47. Tokarski AT, Patel RG, Parvizi J, Deirmengian GK. Dental clearance prior to elective arthroplasty may not be needed for everyone. J Arthroplasty. 2014;29(9):1729–1732. [DOI] [PubMed] [Google Scholar]
- 48. Winemaker M, Petruccelli D, Kabali C, de Beer J. Not all total joint replacement patients are created equal: preoperative factors and length of stay in hospital. Can J Surg. 2015;58(3):160–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Kerkhoffs GM, Servien E, Dunn W, Dahm D, Bramer JA, Haverkamp D. The influence of obesity on the complication rate and outcome of total knee arthroplasty: a meta-analysis and systematic literature review. J Bone Joint Surg Am. 2012;94(20):1839–1844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. McElroy MJ, Pivec R, Issa K, Harwin SF, Mont MA. The effects of obesity and morbid obesity on outcomes in TKA. J Knee Surg. 2013;26(2):83–88. [DOI] [PubMed] [Google Scholar]
- 51. Si HB, Zeng Y, Shen B, et al. The influence of body mass index on the outcomes of primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2015;23(6):1824–1832. [DOI] [PubMed] [Google Scholar]
- 52. Vaishya R, Vijay V, Wamae D, Agarwal AK. Is total knee replacement justified in the morbidly obese? A systematic review. Cureus. 2016;8(9):e804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Alvi HM, Mednick RE, Krishnan V, Kwasny MJ, Beal MD, Manning DW. The Effect of BMI on 30 day outcomes following total joint arthroplasty. J Arthroplasty. 2015;30(7):1113–1117. [DOI] [PubMed] [Google Scholar]
- 54. Mulhall KJ, Ghomrawi HM, Mihalko W, Cui Q, Saleh KJ. Adverse effects of increased body mass index and weight on survivorship of total knee arthroplasty and subsequent outcomes of revision TKA. J Knee Surg. 2007;20(3):199–204. [DOI] [PubMed] [Google Scholar]
- 55. Ward DT, Metz LN, Horst PK, Kim HT, Kuo AC. Complications of morbid obesity in total joint arthroplasty: risk stratification based on BMI. J Arthroplasty. 2015;30(suppl 9):42–46. [DOI] [PubMed] [Google Scholar]
- 56. Jamsen E, Nevalainen P, Eskelinen A, Huotari K, Kalliovalkama J, Moilanen T. Obesity, diabetes, and preoperative hyperglycemia as predictors of periprosthetic joint infection: a single-center analysis of 7181 primary hip and knee replacements for osteoarthritis. J Bone Joint Surg Am. 2012;94(14):e101. [DOI] [PubMed] [Google Scholar]
- 57. Watts CD, Wagner ER, Houdek MT, Lewallen DG, Mabry TM. Morbid obesity: increased risk of failure after aseptic revision TKA. Clin Orthop Relat Res. 2015;473(8):2621–2627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Lubbeke A, Zingg M, Vu D, et al. Body mass and weight thresholds for increased prosthetic joint infection rates after primary total joint arthroplasty. Acta Orthop. 2016;87(2):132–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Namba RS, Inacio MC, Paxton EW. Risk factors associated with deep surgical site infections after primary total knee arthroplasty: an analysis of 56,216 knees. J Bone Joint Surg Am. 2013;95(9):775–782. [DOI] [PubMed] [Google Scholar]
- 60. Pugely AJ, Martin CT, Gao Y, Schweizer ML, Callaghan JJ. The incidence of and risk factors for 30-day surgical site infections following primary and revision total joint arthroplasty. J Arthroplasty. 2015;30(suppl 9):47–50. [DOI] [PubMed] [Google Scholar]
- 61. Kelz RR, Reinke CE, Zubizarreta JR, et al. Acute kidney injury, renal function, and the elderly obese surgical patient: a matched case-control study. Ann Surg. 2013;258(2):359–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Houdek MT, Wagner ER, Watts CD, et al. Morbid obesity: a significant risk factor for failure of two-stage revision total hip arthroplasty for infection. J Bone Joint Surg Am. 2015;97(4):326–332. [DOI] [PubMed] [Google Scholar]
- 63. Frisch N, Wessell NM, Charters M, et al. Effect of body mass index on blood transfusion in total hip and knee arthroplasty. Orthopedics. 2016;39(5):e844–e849. [DOI] [PubMed] [Google Scholar]
- 64. Lui M, Jones CA, Westby MD. Effect of non-surgical, non-pharmacological weight loss interventions in patients who are obese prior to hip and knee arthroplasty surgery: a rapid review. Syst Rev. 2015;4:121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Inacio MC, Paxton EW, Fisher D, Li RA, Barber TC, Singh JA. Bariatric surgery prior to total joint arthroplasty may not provide dramatic improvements in post-arthroplasty surgical outcomes. J Arthroplasty. 2014;29(7):1359–1364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Schwarzkopf R, Russell TA, Shea M, Slover JD. Correlation between nutritional status and staphylococcus colonization in hip and knee replacement patients. Bull NYU Hosp Jt Dis. 2011;69(4):308–311. [PubMed] [Google Scholar]
- 67. Nicholson JA, Dowrick AS, Liew SM. Nutritional status and short-term outcome of hip arthroplasty. J Orthop Surg (Hong Kong). 2012;20(3):331–335. [DOI] [PubMed] [Google Scholar]
- 68. Marin LA, Salido JA, Lopez A, Silva A. Preoperative nutritional evaluation as a prognostic tool for wound healing. Acta Ortho Scand. 2002;73(1):2–5. [DOI] [PubMed] [Google Scholar]
- 69. Lavernia CJ, Sierra RJ, Baerga L. Nutritional parameters and short term outcome in arthroplasty. J Am Coll Nutr. 1999;18(3):274–278. [DOI] [PubMed] [Google Scholar]
- 70. Greene KA, Wilde AH, Stulberg BN. Preoperative nutritional status of total joint patients. relationship to postoperative wound complications. J Arthroplasty. 1991;6(4):321–325. [DOI] [PubMed] [Google Scholar]
- 71. Gherini S, Vaughn BK, Lombardi AV, Jr, Mallory TH. Delayed wound healing and nutritional deficiencies after total hip arthroplasty. Clinical Orthop Relat Res. 1993(293):188–195. [PubMed] [Google Scholar]
- 72. Font-Vizcarra L, Lozano L, Rios J, Forga MT, Soriano A. Preoperative nutritional status and post-operative infection in total knee replacements: a prospective study of 213 patients. Int J Artif Organs. 2011;34(9):876–881. [DOI] [PubMed] [Google Scholar]
- 73. Del Savio GC, Zelicof SB, Wexler LM, et al. Preoperative nutritional status and outcome of elective total hip replacement. Clinical Orthop Relat Res. 1996(326):153–161. [DOI] [PubMed] [Google Scholar]
- 74. Alfargieny R, Bodalal Z, Bendardaf R, El-Fadli M, Langhi S. Nutritional status as a predictive marker for surgical site infection in total joint arthroplasty. Avicenna J Med. 2015;5(4):117–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Grennan DM, Gray J, Loudon J, Fear S. Methotrexate and early postoperative complications in patients with rheumatoid arthritis undergoing elective orthopaedic surgery. Ann Rheum Dis. 2001;60(3):214–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. LoVerde ZJ, Mandl LA, Johnson BK, et al. Rheumatoid arthritis does not increase risk of short-term adverse events after total knee arthroplasty: a retrospective case-control study. J Rheumatol. 2015;42(7):1123–1130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Kubota A, Nakamura T, Miyazaki Y, Sekiguchi M, Suguro T. Perioperative complications in elective surgery in patients with rheumatoid arthritis treated with biologics. Mod Rheumatol. 2012;22(6):844–848. [DOI] [PubMed] [Google Scholar]
- 78. Kadota Y, Nishida K, Hashizume K, et al. Risk factors for surgical site infection and delayed wound healing after orthopedic surgery in rheumatoid arthritis patients. Mod Rheumatol. 2016;26(1):68–74. [DOI] [PubMed] [Google Scholar]
- 79. Johnson BK, Goodman SM, Alexiades MM, Figgie MP, Demmer RT, Mandl LA. Patterns and associated risk of perioperative use of anti-tumor necrosis factor in patients with rheumatoid arthritis undergoing total knee replacement. J Rheumatol. 2013;40(5):617–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Bongartz T, Halligan CS, Osmon DR, et al. Incidence and risk factors of prosthetic joint infection after total hip or knee replacement in patients with rheumatoid arthritis. Arthritis Rheum. 2008;59(12):1713–1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Beswick AD, Wylde V, Gooberman-Hill R, Blom A, Dieppe P. What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis? A systematic review of prospective studies in unselected patients. BMJ Open. 2012;2(1):e000435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Franklin PD, Karbassi JA, Li W, Yang W, Ayers DC. Reduction in narcotic use after primary total knee arthroplasty and association with patient pain relief and satisfaction. J Arthroplasty. 2010;25(suppl 6):12–16. [DOI] [PubMed] [Google Scholar]
- 83. Smith SR, Bido J, Collins JE, Yang H, Katz JN, Losina E. Impact of preoperative opioid use on total knee arthroplasty outcomes. J Bone Joint Surg Am. 2017;99(10):803–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Carroll I, Barelka P, Wang CK, et al. A pilot cohort study of the determinants of longitudinal opioid use after surgery. Anesth Analg. 2012;115(3):694–702. [DOI] [PubMed] [Google Scholar]
- 85. Inacio MC, Hansen C, Pratt NL, Graves SE, Roughead EE. Risk factors for persistent and new chronic opioid use in patients undergoing total hip arthroplasty: a retrospective cohort study. BMJ Open. 2016;6(4):e010664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Nguyen LC, Sing DC, Bozic KJ. Preoperative reduction of opioid use before total joint arthroplasty. J Arthroplasty. 2016;31(suppl 9):282–287. [DOI] [PubMed] [Google Scholar]
- 87. McDonald S, Page MJ, Beringer K, Wasiak J, Sprowson A. Preoperative education for hip or knee replacement. Cochrane Database Syst Rev. 2014;(5):Cd003526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Louw A, Diener I, Butler DS, Puentedura EJ. Preoperative education addressing postoperative pain in total joint arthroplasty: review of content and educational delivery methods. Physiother Theory Pract. 2013;29(3):175–194. [DOI] [PubMed] [Google Scholar]
- 89. Jordan RW, Smith NA, Chahal GS, Casson C, Reed MR, Sprowson AP. Enhanced education and physiotherapy before knee replacement; is it worth it? A systematic review. Physiother. 2014;100(4):305–312. [DOI] [PubMed] [Google Scholar]
- 90. Aydin D, Klit J, Jacobsen S, Troelsen A, Husted H. No major effects of preoperative education in patients undergoing hip or knee replacement—a systematic review. Dan Med J. 2015;62(7). pii: A5106. [PubMed] [Google Scholar]
- 91. Kapadia BH, Elmallah RK, Mont MA. A randomized, clinical trial of preadmission chlorhexidine skin preparation for lower extremity total joint arthroplasty. J Arthroplasty. 2016;31(12):2856–2861. [DOI] [PubMed] [Google Scholar]
- 92. Rao N, Cannella BA, Crossett LS, et al. Preoperative screening/decolonization for Staphylococcus aureus to prevent orthopedic surgical site infection: prospective cohort study with 2-year follow-up. J Arthroplasty. 2011;26(8):1501–1507. [DOI] [PubMed] [Google Scholar]
- 93. Schweizer ML, Chiang HY, Septimus E, et al. Association of a bundled intervention with surgical site infections among patients undergoing cardiac, hip, or knee surgery. JAMA. 2015;313(21):2162–2171. [DOI] [PubMed] [Google Scholar]
- 94. Stambough JB, Nam D, Warren DK, et al. Decreased hospital costs and surgical site infection incidence with a universal decolonization protocol in primary total joint arthroplasty. J Arthroplasty. 2017;32(3):728–734.e1. [DOI] [PubMed] [Google Scholar]
- 95. Leaper DJ, Edmiston CE. World Health Organization: global guidelines for the prevention of surgical site infection. J Hosp Infect. 2017;95(2):135–136. [DOI] [PubMed] [Google Scholar]
- 96. Strebel N, Prins M, Agnelli G, Buller HR. Preoperative or postoperative start of prophylaxis for venous thromboembolism with low-molecular-weight heparin in elective hip surgery? Arch Intern Med. 2002;162(13):1451–1456. [DOI] [PubMed] [Google Scholar]
- 97. Lassen MR, Bauer KA, Eriksson BI, Turpie AG; European Pentasaccharide Elective Surgery Study Steering Commitee. Postoperative fondaparinux versus preoperative enoxaparin for prevention of venous thromboembolism in elective hip-replacement surgery: a randomised double-blind comparison. Lancet. 2002;359(9319):1715–1720. [DOI] [PubMed] [Google Scholar]
- 98. Navarro-Quilis A, Castellet E, Rocha E, Paz-Jimenez J, Planes A; Bemiparin Study Group in Knee Arthroplasty. Efficacy and safety of bemiparin compared with enoxaparin in the prevention of venous thromboembolism after total knee arthroplasty: a randomized, double-blind clinical trial. J Thromb Haemost. 2003;1(3):425–432. [DOI] [PubMed] [Google Scholar]
- 99. Borgen PO, Pripp AH, Dybvik E, Leistad L, Dahl OE, Reikeras O. Similar clinical outcomes with preoperative and postoperative start of thromboprophylaxis in tha: a register-based study. Clin Orthop Relat Res. 2017;475(9):2245–2252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Parker MJ, Livingstone V, Clifton R, McKee A. Closed suction surgical wound drainage after orthopaedic surgery. Cochrane Database Syst Rev. 2007;(3):CD001825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Quinn M, Bowe A, Galvin R, Dawson P, O’Byrne J. The use of postoperative suction drainage in total knee arthroplasty: a systematic review. Int Orthop. 2015;39(4):653–658. [DOI] [PubMed] [Google Scholar]
- 102. Wang D, Xu J, Zeng WN, et al. Closed suction drainage is not associated with faster recovery after total knee arthroplasty: a prospective randomized controlled study of 80 patients. Orthop Surg. 2016;8(2):226–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Dora C, von Campe A, Mengiardi B, Koch P, Vienne P. Simplified wound care and earlier wound recovery without closed suction drainage in elective total hip arthroplasty. A prospective randomized trial in 100 operations. Arch Orthop Trauma Surg. 2007;127(10):919–923. [DOI] [PubMed] [Google Scholar]
- 104. Kumar S, Penematsa S, Parekh S. Are drains required following a routine primary total joint arthroplasty? Int Orthop. 2007;31(5):593–596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Watanabe T, Muneta T, Yagishita K, Hara K, Koga H, Sekiya I. Closed suction drainage is not necessary for total knee arthroplasty: a prospective study on simultaneous bilateral surgeries of a mean follow-up of 5.5 years. J Arthroplasty. 2016;31(3):641–645. [DOI] [PubMed] [Google Scholar]
- 106. Mardian S, Matziolis G, Schwabe P. Influence of wound drainage in primary total knee arthroplasty without tourniquet. Int Orthop. 2015;39(3):435–440. [DOI] [PubMed] [Google Scholar]
- 107. Guerra ML, Singh PJ, Taylor NF. Early mobilization of patients who have had a hip or knee joint replacement reduces length of stay in hospital: a systematic review. Clin Rehabil. 2015;29(9):844–854. [DOI] [PubMed] [Google Scholar]
- 108. Okamoto T, Ridley RJ, Edmondston SJ, Visser M, Headford J, Yates PJ. Day-of-surgery mobilization reduces the length of stay after elective hip arthroplasty. J Arthroplasty. 2016;31(10):2227–2230. [DOI] [PubMed] [Google Scholar]
- 109. Harvey LA, Brosseau L, Herbert RD. Continuous passive motion following total knee arthroplasty in people with arthritis. Cochrane Database Syst Rev. 2014;(2):Cd004260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Joshi RN, White PB, Murray-Weir M, Alexiades MM, Sculco TP, Ranawat AS. Prospective randomized trial of the efficacy of continuous passive motion post total knee arthroplasty: experience of the hospital for special surgery. J Arthroplasty. 2015;30(12):2364–2369. [DOI] [PubMed] [Google Scholar]
- 111. Boese CK, Weis M, Phillips T, Lawton-Peters S, Gallo T, Centeno L. The efficacy of continuous passive motion after total knee arthroplasty: a comparison of three protocols. J Arthroplasty. 2014;29(6):1158–1162. [DOI] [PubMed] [Google Scholar]
- 112. Forster R, Stewart M. Anticoagulants (extended duration) for prevention of venous thromboembolism following total hip or knee replacement or hip fracture repair. Cochrane Database Syst Rev. 2016;3:CD004179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Eikelboom JW, Quinlan DJ, Douketis JD. Extended-duration prophylaxis against venous thromboembolism after total hip or knee replacement: a meta-analysis of the randomised trials. Lancet. 2001;358(9275):9–15. [DOI] [PubMed] [Google Scholar]
- 114. Kapoor A, Ellis A, Shaffer N, et al. Comparative effectiveness of venous thromboembolism prophylaxis options for the patient undergoing total hip and knee replacement: a network meta-analysis. J Thromb Haemost. 2017;15(2):284–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Venker BT, Ganti BR, Lin H, Lee ED, Nunley RM, Gage BF. Safety and efficacy of new anticoagulants for the prevention of venous thromboembolism after hip and knee arthroplasty: a meta-analysis. J Arthroplasty. 2017;32(2):645–652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Wilson DG, Poole WE, Chauhan SK, Rogers BA. Systematic review of aspirin for thromboprophylaxis in modern elective total hip and knee arthroplasty. Bone Joint J. 2016;98-B(8):1056–1061. [DOI] [PubMed] [Google Scholar]
- 117. Bern MM, Hazel D, Deeran E, et al. Low dose compared to variable dose warfarin and to fondaparinux as prophylaxis for thromboembolism after elective hip or knee replacement surgery; a randomized, prospective study. Thromb J. 2015;13:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Avenell A, Smith TO, Curtain JP, Mak JC, Myint PK. Nutritional supplementation for hip fracture aftercare in older people. Cochrane Database Syst Rev. 2016;11:Cd001880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Barsoum WK, Murray TG, Klika AK, et al. Predicting patient discharge disposition after total joint arthroplasty in the United States. J Arthroplasty. 2010;25(6):885–892. [DOI] [PubMed] [Google Scholar]
- 120. Bindelglass DF, Garrison S, Essig K, Leopold T. A tool to measure the need for subacute care on discharge from the hospital after total knee arthroplasty. J Arthroplasty. 1999;14(6):761–763. [DOI] [PubMed] [Google Scholar]
- 121. Wang T, Ackland T, Hall S, Gilbey H, Parsons R. Functional recovery and timing of hospital discharge after primary total hip arthroplasty. Aust N Z J Surg. 1998;68(8):580–583. [DOI] [PubMed] [Google Scholar]
- 122. Riggs RV, Roberts PS, Aronow H, Younan T. Joint replacement and hip fracture readmission rates: impact of discharge destination. PM R. 2010;2(9):806–810. [DOI] [PubMed] [Google Scholar]
- 123. Stolee P, Lim SN, Wilson L, Glenny C. Inpatient versus home-based rehabilitation for older adults with musculoskeletal disorders: a systematic review. Clin Rehabil. 2012;26(5):387–402. [DOI] [PubMed] [Google Scholar]
- 124. Rissman CM, Keeney BJ, Ercolano EM, Koenig KM. Predictors of facility discharge, range of motion, and patient-reported physical function improvement after primary total knee arthroplasty: a prospective cohort analysis. J Arthroplasty. 2016;31(1):36–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Chimenti CE, Ingersoll G. Comparison of home health care physical therapy outcomes following total knee replacement with and without subacute rehabilitation. J Geriatr Phys Ther. 2007;30(3):102–108. [DOI] [PubMed] [Google Scholar]
- 126. Bini SA, Fithian DC, Paxton LW, Khatod MX, Inacio MC, Namba RS. Does discharge disposition after primary total joint arthroplasty affect readmission rates? J Arthroplasty. 2010;25(1):114–117. [DOI] [PubMed] [Google Scholar]
- 127. Sigurdsson E, Siggeirsdottir K, Jonsson H, Jr, Gudnason V, Matthiasson T, Jonsson BY. Early discharge and home intervention reduces unit costs after total hip replacement: results of a cost analysis in a randomized study. Int J Health Care Finance Econ. 2008;8(3):181–92. [DOI] [PubMed] [Google Scholar]
- 128. Stowers MD, Manuopangai L, Hill AG, Gray JR, Coleman B, Munro JT. Enhanced recovery after surgery in elective hip and knee arthroplasty reduces length of hospital stay. ANZ J Surg. 2016;86(6):475–479. [DOI] [PubMed] [Google Scholar]
- 129. Stowers MD, Lemanu DP, Hill AG. Health economics in enhanced recovery after surgery programs. Can J Anaesth. 2015;62(2):219–230. [DOI] [PubMed] [Google Scholar]
- 130. Berrios-Torres SI, Umscheid CA, Bratzler DW, et al. Centers for disease control and prevention guideline for the prevention of surgical site infection, 2017. JAMA Surg. 2017;152(8):784–791. [DOI] [PubMed] [Google Scholar]