Abstract
Background
The increased prevalence of temporomandibular disorders (TMDs) requires searching for new, easily accessible diagnostic methods. In addition to routine clinical examination, various methods of imaging temporomandibular joints are available, such as magnetic resonance imaging, computed tomography scans, or scintigraphy. Ultrasound imaging, due to short examination time, low cost, and non-invasiveness, should be recommended as a routine diagnostic procedure. The aim of the study was to investigate whether ultrasound imaging can be used in the diagnosis of temporomandibular joint disorders.
Material/Methods
Publications during the period 2006 to March 2017 from the US National Library of Medicine database were selected for analysis by entering the terms “ultrasonography”, “ultrasound”, “USG”, “temporomandibular joint”, “TMJ”, “temporomandibular disorders”, and “TMD”. Papers were chosen if they met the required criteria relating to the sensitivity, specificity, accuracy, positive predictive value, and negative predictive value of this diagnostic technique with regard to imaging articular disc displacement, joint effusion, and condylar abnormalities.
Results
The search yielded 1883 publications, of which 8 were selected that met the criteria for inclusion in the analysis. For articular disc displacement examinations, the following results were obtained: sensitivity 75.6%; specificity 69.1%; accuracy 76.1%; positive predictive value 72.2%; negative predictive value 65.6%. When the examinations of joint effusion and condylar abnormalities were included, the results were respectively 66.9%; 70.8%; 69.9%; 75.8%; and 62.4%.
Conclusions
The use of ultrasonography in the diagnosis of temporomandibular disorders requires standardizing the method as well as further research to confirm its effectiveness.
MeSH Keywords: Temporomandibular Joint, Temporomandibular Joint Disorders, Ultrasonography
Background
Nowadays, a significant increase in the prevalence of temporomandibular disorders (TMDs) can be observed. Among the general population, it varies between 10% and 70% [1]. In children and adolescents, it ranges between 16% and 68% [2]. The increasing number of TMD cases may be related to the impact of the growing psychological pressure on today’s society [3]. There may be a number of different causes for these disorders as well as a number of different specific conditions. The similarity of the symptoms for the different disorders causes difficulties in clinical diagnosis. In addition to the basic clinical examination, there are a variety of methods and techniques for TMD diagnosis. Magnetic resonance imaging (MRI) is regarded as the gold standard in the evaluation of soft tissues as well as the articular disc. Computed tomography (CT) is used to diagnose bone lesions such as bone erosion, fractures, postoperative deformities, and deformities of the adjacent temporal bone. Bone scintigraphy is useful for the evaluation of osteoarthritis and joint inflammation [4,5]. All of these methods have certain limitations, which will be discussed later in the article. Ultrasound imaging of the joint and surrounding tissues seems to be a reasonable direction in which TMD diagnostics should proceed. It is a cheap, non-invasive, and quick examination technique, widely available in most healthcare institutions. The aim of this paper was to discuss the possibility of using ultrasonography for TMD diagnosis, show the advancements in imaging technology, as well as present the rationale for further research into the use of ultrasound waves in the diagnosis of temporomandibular disorders.
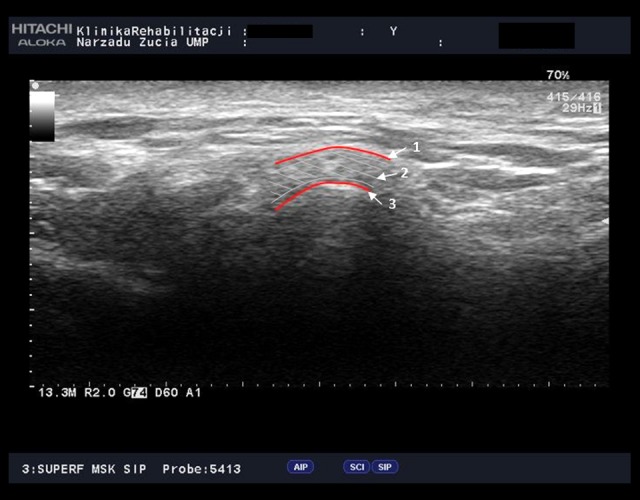
During an ultrasound of the temporomandibular joint, a linear probe is used, which is positioned transversely or longitudinally relative to the zygomatic arch, and then tilted to obtain the best view [6–10]. During the examination, the patient remains in a prone position with their mouth either closed or maximally open. To better understand this issue under discussion, the authors performed their own examinations of the temporomandibular joint by means of an ultrasound machine. The ultrasound scans were of a healthy patient. In the first and second imaged (Figures 1, 2), the probe was positioned perpendicular to the zygomatic arch with the mouth open and closed respectively. In images 3 and 4 (Figures 3, 4), the probe was positioned parallel to the zygomatic arch with the mouth open and closed respectively. The arrows indicating the structures of the temporomandibular joint showed the following: arrow 1, TMJ capsule; arrow 2, articular disk; and arrow 3, condyle. Dynamic ultrasound examinations were also carried out with the patient continuously opening and closing their mouth, because according to Emshoff et al., this is a very good method for excluding disc displacement [6]. In later research, however, this method was discontinued due to the difficulty in tracking the image of the disc while the mandible was moving. It is, thus, recommended that a probe with a frequency equal to or higher than 8 MHz should be used [4]. When analyzing the use of probes over time, one can observe an increase in probe frequency up to even 17 MHz used in more recent studies [6,7,10]. There are 2 methods for analyzing the images obtained. The first is the direct method, involving an assessment of the relationships between the anatomical structures visible on the ultrasound scans, and on this basis making a diagnosis [7–10]. The other is an indirect method based on measuring the size of the joint space, which then becomes the basis for a diagnosis [11]. The aim of this study was to investigate whether ultrasound imaging can be used in the diagnosis of temporomandibular joint disorders based on research findings available in international literature.
Figure 1.
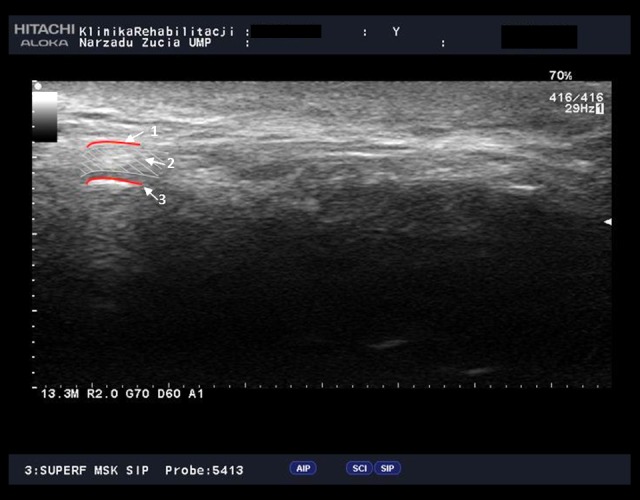
Temporomandibular joint (TMJ), coronal view, open mouth (arrow 1, TMJ capsule; arrow 2, articular disk; arrow 3, condyle).
Figure 2.

Temporomandibular joint (TMJ), coronal view, closed mouth (arrow 1, TMJ capsule; arrow 2, articular disk; arrow 3, condyle).
Figure 3.

Temporomandibular joint (TMJ), axial view, open mouth (arrow 1, TMJ capsule; arrow 2, articular disk; arrow 3, condyle).
Figure 4.
Temporomandibular joint (TMJ), axial view, closed mouth (arrow 1, TMJ capsule; arrow 2, articular disk; arrow 3, condyle).
Material and Methods
In order search for relevant articles in the US National Library of Medicine database, combinations of the words “ultrasonography”, “ultrasound”, “USG” or “US” with “temporomandibular joint”, “TMJ”, “temporomandibular disorders”, and “TMD”, “disk displacement”, “temporomandibular joint effusion”, or “condyle” were entered. The results are presented in Table 1, with a total of 1883 papers published in 2006 to March 2017. Papers published before 2006 (862) were excluded from the analysis due to a meta-analysis performed by Manfredini et al. on the same topic [12]. The following publications were also rejected: 174 articles concerning animal research, 89 literature reviews, 743 papers unrelated to the topic, 3 papers where the full versions were unavailable, and 4 papers containing incomplete data. Articles regarded as containing complete information were those which described the sensitivity, specificity, accuracy, as well as the positive and negative predictive value of ultrasound imaging of the temporomandibular joint. Two papers had to be translated due to the lack of an English-language versions [13,14]. In the end, a total of 8 publications were included.
Table 1.
Database search results.
| Combinations of the terms Ultrasonography, Ultrasound, USG or US along with | Number of studies |
|---|---|
| Temporomandibular joint | 445 |
| Temporomandibular disorder | 316 |
| TMJ | 453 |
| TMD | 188 |
| Disk Displacement | 91 |
| Temporomandibular joint effusion | 18 |
| Condyle | 372 |
Results
The data obtained in the analyses from all the publications are presented in Table 2. In the case of studies where statistical data were calculated separately for an open and closed mouth, it was decided to calculate the arithmetic mean to be included in further analysis [8]. The largest number of ultrasound examinations were performed to detect a displacement of the articular disc. The analysis considered their sensitivity, specificity, accuracy, as well as positive predictive value and negative predictive value. After calculating weighted averages, that considered the size of the test group determining the validity of the study, the following results were obtained for publications related to disc displacement: sensitivity 75.6%; specificity 69.1%; accuracy 76.1%; positive predictive value 77.2%; negative predictive value 65.6%. As regards temporomandibular joint effusion and condylar abnormalities, in each case only one publication was found containing the aforementioned statistical data. After calculating the average values for all the possibilities for use ultrasound in temporomandibular joint examination, the following results were obtained: sensitivity 66.9%; specificity 70.8%; accuracy 69.9%; positive predictive value 75.8%; negative predictive value 62.4%.
Table 2.
Summary of results obtained for the studies analysed.
| Author | Year of publication | Number of joints | Comparison examination | Probe frequency | Probe position | Sensitivity | Specificity | Accuracy | Positive predictive value | Negative predictive value |
|---|---|---|---|---|---|---|---|---|---|---|
| Disc displacement | ||||||||||
| Kaya et al. | 2009 | 52 | MR | 7.5 MHz D, O, C | Longitudinal, transverse | 91% | 16% | 82% | 89% | 20% |
| Nilufer et al. | 2010 | 56 | MR | 12 MHz O, C | Transverse | 66.05% | 68.75% | 67.43% | 68.48% | 67% |
| Dupuy-Bonafe et al. | 2012 | 120 | MR | 5–12 MHz O, C, D | Longitudinal, transverse | 71.5% | 74.3% | 72.5% | 66% | 78.8% |
| Yang et al. | 2012 | 40 | MR | 82.6% | 94.1% | 92.5% | 95% | 80% | ||
| Razek et al. | 2014 | 40 | MR | 77.15% | 68.15% | 72.1% | 65.65% | 72.3% | ||
| Habashi et al. | 2015 | 78 | MR | 5–17 MHz O, C, D | Longitudinal, transverse | 74.3% | 84.2% | 77.7% | 89.7% | 64.0% |
| Joint effusion | ||||||||||
| Kaya et al. | 2009 | 52 | MR | 7.5 MHz D, O, C | Longitudinal, transverse | 53% | 63% | 57% | 72% | 50% |
| Condylar abnormalities | ||||||||||
| Muller et al. | 2009 | 60 | MR | 12 MHz O, C | Longitudinal, transverse | 23% | 89% | 41% | 70% | 52% |
Discussion
The number of publications related to ultrasound imaging of the temporomandibular joint has been relatively small over the years. Comparing the results obtained in the present study to those obtained by Manfredini at al. [12], who analyzed works published up to 2006, it can be observed that the discrepancies in the results have stabilized considerably. In the case of articular disc displacement, Manfredini et al. obtained sensitivity in the range of 31% to 100%, while in our study the results for sensitivity were 66% to 91%. Similarly, specificity was 30% to 100% compared to 16% to 94% in our study; accuracy was 62% to 100% vs. 72% to 92%; positive predictive value was 41% to 100% vs. 65% to 95%; negative predictive value was 51% to 100% vs. 20% to 80%.
The principal expectation connected with the use of ultrasound devices in the diagnosis of TMD is the use of this method as a screening test. Magnetic resonance imaging, which is associated with exposure to magnetic fields, is too expensive, not available in most medical facilities, and impossible in patients with claustrophobia. Computed tomography (CT) does not show soft tissues such as the articular disc [12]. CT scans, due to exposure to x-rays, cannot be done more often than once or twice a year [15]. Traditional pantomographic images, available in many dental offices, show only very advanced changes in the temporomandibular joint [12]. Importantly, the correct diagnosis of temporomandibular disorders cannot be based solely on clinical examination [16]. Clinical symptoms commonly manifest very late in patients with TMD, while imaging diagnostic techniques such as MRI and ultrasonography can detect degenerative changes and disc dislocations at earlier stages of the condition [15]. In addition, noises in the joint, for example clicking, which are used in clinical assessments, may be simply a physiological symptom [17]. The temporomandibular joint may be the first, and sometimes even the only joint involved in juvenile idiopathic arthritis (JIA) [18,19]. The issue can be complicated by the fact that this joint is often affected without any detectable clinical symptoms, which may additionally delay the diagnosis [20,21]. TMD can also be masked by anti-rheumatic therapy, used in the treatment of polyarthritis [15].
The use of ultrasound examinations as a screening test requires obtaining the greatest possible sensitivity. The low sensitivity of ultrasound examinations recorded in Müller’s research precludes, according to the authors, the use of ultrasound as an early diagnostic method [22]. However, the opinions of the authors of various publications on this subject vary significantly. A study published in 2006 by Jank et al., which was conducted on 100 patients and which compared the techniques of ultrasound and MRI in terms of detecting degenerative changes, joint effusion, and disc displacement obtained very good results. For degenerative changes, the sensitivity was 94%, specificity was 100%, and accuracy was 94%; and for joint effusion the sensitivity was 81%, specificity was 100%, and accuracy was 95%. For disc displacement, a comparison of ultrasound and MRI resulted in sensitivity, specificity, and accuracy at a level of 92% each. Thus, this publication appears to open up the possibility of using ultrasound examination as a diagnostic method for TMD, however, it seems that ultrasound still cannot replace MRI [23]. Dupuy-Bonafé et al. do not recommend the use of ultrasound in the diagnosis of TMD as in their research they obtained low sensitivity but high specificity in the diagnosis of disc displacement [9]. Kaya et al., on the other hand, obtained high sensitivity and accuracy, but low specificity. They concluded that ultrasound is useful for the diagnosis of disc displacement but unfortunately not very effective in excluding disorders in a healthy temporomandibular joint. Although ultrasound can detect disc displacement, it cannot determine the type of displacement and, according to the authors, it is not suitable for assessing the presence of joint effusion [7]. Siegfried et al. used high frequency ultrasound to examine patients with JIA for degenerative changes in the temporomandibular joint and articular disc displacement. A 12 MHz transducer was used, which was positioned parallel to the mandibular ramus with the patient’s mouth fully open. The study was conducted on 48 people. A significant relationship was found between the results obtained by ultrasonography and the number of joints involved in JIA. The authors proposed a high frequency ultrasound scan as an interesting diagnostic technique for screening tests [15].
Ultrasonographic examination is a procedure which greatly depends on the operator’s skill and experience [10]. Differences of opinion among researchers may result from the lack of standardization in the procedures related to conducting the examination: starting from the selection of the transducer, its settings, and the mouth opening position; and ending with interpreting the results using either the direct or indirect method. A probe with a higher frequency enables a better visualization of the tissues, with high frequency ultrasound using a probe with a frequency equal to or higher than 12 MHz [10]. Attempts have been made to standardize the position of the transducer relative to Camper’s line [9], and the vast majority of practitioners conduct the examination with the patient in a supine position, but variations in the administration of ultrasound also concern mouth positions. When measuring the distances in the joint, some authors noticed that examination with the mouth open was more reliable for assessing disc displacement, while examination with the mouth closed was more useful for determining the normal position of the disc [8]. Others encountered difficulties in locating the disc during an open-mouth examination due to the fact that the bony structures obscure the deeper structures [9] and found that the sensitivity of ultrasound examination was a higher with the mouth closed than with the mouth open [10]. It should also be remembered that only the lateral part of the temporomandibular joint can be adequately shown in ultrasound images. The medial part is obscured by bony structures; consequently, lateral or medial displacement, as well as disc rotation, can be difficult to assess in an ultrasound image, which may negatively influence examination results [9]. This should encourage the use of the indirect imaging technique, which is based on measuring the distances between the joint capsule and the condylar head. Nilüfer et al. found the greatest accuracy in the assessment of joint space distances for the anterior distance with the mouth closed, and argued that measuring the anterior distance was more appropriate for assessing disc displacement. They stated that the results of their study were influenced by the fact that the majority of the patients had medial disc displacement, making the diagnosis more difficult and paradoxically reducing the anterior distance between the joint capsule and the condyle [8]. Burcu et al. describe 2 possible methods of ultrasound diagnosis for the presence of effusion in the temporomandibular joint. One is by direct visualization of a hypoechoic area within the joint space; and the other is by an indirect measurement of capsular distension. This measurement is made between the condylar latero-superior surface and the articular capsule with the patient in the closed-mouth position [11].
It was evident that there was no uniform methodology for performing ultrasound imaging of the temporomandibular joint. This supports the need for further research that would include a larger number of people and therefore help in standardizing the procedure as well as improving the assessment of the results. Nilüfer et al. mentioned the need for a more precise determination of the threshold values for joint space distance measurements [8]. The vast majority of publications were concerned with the issue of disc displacement. However, it should be remembered that ultrasonographic temporomandibular joint examinations should not be limited to disc displacement but should also assess degenerative changes regarding joint surfaces, joint effusion and synovitis [15]. JIA is the most common pediatric rheumatic disease [24]. The condition affects synovial joints and can often involve the temporomandibular joint [25–27]. When mandibular asymmetry or progressive retrognathias become evident, irreversible changes in the condyles are already present [28]. Muller et al. compared the possibilities of a JIA diagnosis by means of ultrasound along with clinical rheumatological and orthodontic examination, to that of using MRI and concluded that ultrasound is the more specific diagnostic method [22]. Melchiorre et al. considered ultrasound to also be useful in diagnosing pathological changes in the temporomandibular joint in adult patients with rheumatoid arthritis [29]. Burcu et al. obtained a high consistency in their research between MRI and an indirect examination of intra-articular effusion [11]. Ultrasound examination can also be used as a cheaper option in assessing the impact of conservative treatment on alleviating lockjaw [9].
Conclusions
Temporomandibular joint examination using high-frequency ultrasound is a diagnostic method of unconfirmed effectiveness. Most of the studies conducted to date concerned the assessment of pathological conditions rather than that of healthy joints in order to determine the correct ultrasound image. Nevertheless, there is a need for a cheap, non-invasive and simple diagnostic technique for imaging the temporomandibular joint. High-frequency ultrasound seems promising, both due to technological advances that provide increasingly more powerful transducers as well as some of the findings of research conducted so far. However, all the knowledge acquired to date needs to be unified and standardized, and further research is required that should involve both normal and abnormal joints.
Acknowledgements
The authors would like to thank the medical staff of the Wiktor Dega Orthopedic and Rehabilitation Hospital in Poznań for their assistance in interpreting ultrasound images.
Footnotes
Source of support: Department of Oral Rehabilitation’s own resources
References
- 1.Kundu H, Basavaraj P, Kote S, Singla A, Singh S. Assessment of TMJ disorders using ultrasonography as a diagnostic tool: A review. J Clin Diagn Res. 2013;7:3116–20. doi: 10.7860/JCDR/2013/6678.3874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sena MF, Mesquita KS, Santos FR, et al. Prevalence of temporomandibular dysfunction in children and adolescents. Rev Paul Pediatr. 2013;31:538–45. doi: 10.1590/S0103-05822013000400018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tomas X, Pomes J, Berenguer J, et al. MR imaging of temporomandibular joint dysfunction: a pictorial review. Radiographics. 2006;26:765–81. doi: 10.1148/rg.263055091. [DOI] [PubMed] [Google Scholar]
- 4.Bag AK, Gaddikeri S, Singhal A, et al. Imaging of the temporomandibular joint: An update. World J Radiol. 2014;28:567–82. doi: 10.4329/wjr.v6.i8.567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Petscavage-Thomas JM, Walker EA. Unlocking the jaw: Advanced imaging of the temporomandibular joint. Am J Roentgenol. 2014;203:1047–58. doi: 10.2214/AJR.13.12177. [DOI] [PubMed] [Google Scholar]
- 6.Emshoff R, Bertram S, Rudisch A, Gassner R. The diagnosticvalue of ultrasonography to determine the temporomandibular joint disk position. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;84:688–96. doi: 10.1016/s1079-2104(97)90374-7. [DOI] [PubMed] [Google Scholar]
- 7.Kaya K, Dulgeroglu D, Unsal-Delialioglu S, et al. Diagnostic value of ultrasonography in the evaluation of the temporomandibular joint anterior disc displacement. J Craniomaxillofac Surg. 2010;38:391–95. doi: 10.1016/j.jcms.2009.10.017. [DOI] [PubMed] [Google Scholar]
- 8.Cakir-Ozkan N, Sarikaya B, Erkorkmaz U, Aktürk Y. Ultrasonographic evaluation of disc displacement of the temporomandibular joint compared with magnetic resonance imaging. J Oral Maxillofac Surg. 2010;68:1075–80. doi: 10.1016/j.joms.2009.08.010. [DOI] [PubMed] [Google Scholar]
- 9.Dupuy-Bonafé I, Picot MC, Maldonado IL, et al. Internal derangement of the temporomandibular joint: Is here still a place for ultrasound? Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113:832–40. doi: 10.1016/j.oooo.2011.11.017. [DOI] [PubMed] [Google Scholar]
- 10.Habashi H, Eran A, Blumenfeld I, Gaitini D. Dynamic high-resolution sonography compared to magnetic resonance imaging for diagnosis of temporomandibular joint disk displacement. J Ultrasound Med. 2015;34:75–82. doi: 10.7863/ultra.34.1.75. [DOI] [PubMed] [Google Scholar]
- 11.Bas B, Yılmaz N, Gökce E, Akan H. Ultrasound assessment of increased capsular width in temporomandibular joint internal derangements: Relationship with joint pain and magnetic resonance grading of joint effusion. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:112–17. doi: 10.1016/j.tripleo.2011.02.020. [DOI] [PubMed] [Google Scholar]
- 12.Manfredini D, Guarda-Nardini L. Ultrasonography of the temporomandibular joint: A literature review. Int J Oral Maxillofac Surg. 2009;38:1229–36. doi: 10.1016/j.ijom.2009.07.014. [DOI] [PubMed] [Google Scholar]
- 13.Razek AA, Al Mahdy Al Belasy F, et al. Assessment of articular disc displacement of temporomandibular joint with ultrasound. J Ultrasound. 2014;7:159–63. doi: 10.1007/s40477-014-0133-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yang J, Liu W, Zhong Y, Zhao H. [The diagnosticvalue of high-resolution ultrasonography for detecting anterior disc displacement without reduction of temporomandibular joint]. Hua Xi Kou Qiang Yi Xue Za Zhi. 2012;30:632–34. [in Chinese] [PubMed] [Google Scholar]
- 15.Jank S, Haase S, Strobl H, et al. Sonographic investigation of the temporomandibular joint in patients with juvenile idiopathic arthritis: A pilot study. Arthritis Rheum. 2007;57:213–18. doi: 10.1002/art.22533. [DOI] [PubMed] [Google Scholar]
- 16.Tvrdy P. Methods of imaging in the diagnosis of temporomandibular joint disorders. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2007;151:133–36. doi: 10.5507/bp.2007.026. [DOI] [PubMed] [Google Scholar]
- 17.Scrivani SJ, Keith DA, Kaban LB. Temporomandibulardisorders. N Engl J Med. 2008;18:2693–705. doi: 10.1056/NEJMra0802472. [DOI] [PubMed] [Google Scholar]
- 18.Martini G, Bacciliero U, Tregnaghi A, et al. Isolated temporomandibular synovitis as unique presentation of juvenile idiopathic arthritis. J Rheumatol. 2001;28:1689–92. [PubMed] [Google Scholar]
- 19.Scolozzi P, Bosson G, Jaques B. Severe isolated temporomandibular joint involvement in juvenile idiopathic arthritis. J Oral Maxillofac Surg. 2005;63:1368–71. doi: 10.1016/j.joms.2005.05.300. [DOI] [PubMed] [Google Scholar]
- 20.Hu YS, Schneiderman ED, Harper RP. The temporomandibular joint in juvenile rheumatoid arthritis: Part II. Relationship between computed tomographic and clinical findings. Pediatr Dent. 1996;18:312–19. [PubMed] [Google Scholar]
- 21.Svensson B, Adell R, Kopp S. Temporomandibular disorders in juvenile chronic arthritis patients. A clinical study. Swed Dent J. 2000;24:83–92. [PubMed] [Google Scholar]
- 22.Liljeström MR, Jämsä A, Le Bell Y, et al. Signs and symptoms of temporomandibular disorders in children with different types of headache. Acta Odontol Scand. 2001;59:413–17. doi: 10.1080/000163501317153284. [DOI] [PubMed] [Google Scholar]
- 23.Jank S, Emshoff R, Norer B, et al. Diagnostic quality of dynamic high-resolution ultrasonography of the TMJ – a pilot study. Int J Oral Maxillofac Surg. 2005;34:132–37. doi: 10.1016/j.ijom.2004.03.014. [DOI] [PubMed] [Google Scholar]
- 24.Gare BA. Epidemiology of rheumaticdisease in children. Curr Opin Rheumatol. 1996;8:449–54. [PubMed] [Google Scholar]
- 25.Pedersen TK, Jensen JJ, Melsen B, Herlin T. Resorption of the temporomandibular condylar bone according to subtypes of juvenile chronic arthritis. J Rheumatol. 2001;28:2109–15. [PubMed] [Google Scholar]
- 26.Ronning O, Valiaho ML, Laaksonen AL. The involvement of the temporomandibular joint in juvenile rheumatoid arthritis. Scand J Rheumatol. 1974;3:89–96. doi: 10.3109/03009747409115807. [DOI] [PubMed] [Google Scholar]
- 27.Twilt M, Mobers SM, Arends LR, et al. Temporomandibular involvement in juvenile idiopathic arthritis. J Rheumatol. 2004;31:1418–22. [PubMed] [Google Scholar]
- 28.Twilt M, van der Giesen E, Mobers SM, et al. Abrupt condylar destruction of the mandibula in juvenile idiopathic arthritis. Ann Rheum Dis. 2003;62:366–67. doi: 10.1136/ard.62.4.366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Melchiorre D, Calderazzi A, MaddaliBongi S, et al. A comparison of ultrasonography and magnetic resonance imaging in the evaluation of temporomandibular joint involvement in rheumatoid arthritis and psoriatic arthritis. Rheumatology. 2003;42:673–76. doi: 10.1093/rheumatology/keg181. [DOI] [PubMed] [Google Scholar]


