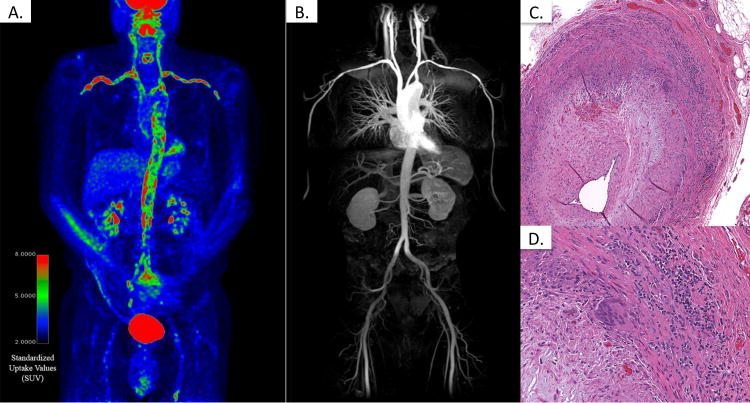
A 71 year-old previously healthy male presented with a pathologic fracture of the left humerus. Biopsy revealed diffuse large B-cell lymphoma. He was treated with 6 cycles of etoposide, prednisone, vincristine, cyclophosphamide, and rituximab (EPOCH-R) without radiation therapy. Surveillance 18F-Fluorodeoxyglucose (FDG) positron emission tomography (PET) imaging, performed 4 months after completion of chemotherapy, showed complete resolution of lymphoma with new intense FDG uptake throughout the aorta and its primary branches, suspicious for an inflammatory process and not seen on prior studies (A). He was asymptomatic and denied headaches, jaw or limb claudication, scalp tenderness, constitutional symptoms, vision loss, and shoulder/hip discomfort. He was not taking immunosuppressant medications. Blood pressure and pulses were normal and symmetric in all extremities. There were no bruits or temporal artery abnormalities. A complete blood count, erythrocyte sedimentation rate, and C-reactive protein were all within normal limits. In contrast to the markedly abnormal PET scan, magnetic resonance angiography revealed subtle stenoses of the distal subclavian arteries with no other vascular abnormalities (B). Biopsy of a 2.5cm segment of the left temporal artery demonstrated transmural mononuclear cell infiltrate with disruption of the internal elastic membrane (C) and giant cells (D), consistent with a diagnosis of giant cell arteritis (GCA). In addition to cranial arteritis, GCA can affect the aorta and branch vessels[1]. Angiography and FDG-PET are complimentary imaging modalities to assess large vessel vasculitis[2, 3]. Angiography can detail arterial damage from vasculitis (e.g. aneurysm, stenosis) while FDG-PET can detect vascular inflammation, potentially at earlier stages in the disease process. FDG-PET can help diagnose atypical cases of large vessel vasculitis, including cases of GCA without cranial symptoms. This unique case of GCA found incidentally in an asymptomatic patient illustrates that temporal artery biopsy can confirm GCA with large vessel involvement even in absence of cranial features of disease.
Figures 1.
Acknowledgments
This research was supported through the Intramural Research Program at the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS).
Footnotes
Financial supports of conflicts disclosure:
The authors declare no conflicts of interest relevant to this work.
References
- 1.Grayson PC, Maksimowicz-McKinnon K, Clark TM, Tomasson G, Cuthbertson D, Carette S, et al. Distribution of arterial lesions in Takayasu’s arteritis and giant cell arteritis. Annals of the rheumatic diseases. 2012;71(8):1329–34. doi: 10.1136/annrheumdis-2011-200795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Soussan M, Nicolas P, Schramm C, Katsahian S, Pop G, Fain O, et al. Management of large-vessel vasculitis with FDG-PET: a systematic literature review and meta-analysis. Medicine. 2015;94(14):e622. doi: 10.1097/MD.0000000000000622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Einspieler I, Thurmel K, Pyka T, Eiber M, Wolfram S, Moog P, et al. Imaging large vessel vasculitis with fully integrated PET/MRI: a pilot study. European journal of nuclear medicine and molecular imaging. 2015;42(7):1012–24. doi: 10.1007/s00259-015-3007-8. [DOI] [PubMed] [Google Scholar]


