Highlights
-
•
Aneurysms of the proximal occipital artery may cause symptoms by compressing adjacent structures.
-
•
Resection may require intubation by the nose.
-
•
Resection if usually followed by regeression of symptoms.
Keywords: Arterial aneurysm, Occipital artery, Case report
Abstract
Introduction
True aneurysms of the proximal occipital artery are rare, may cause neurological symptoms due to compression of the hypoglossal nerve and their resection may be technically demanding.
Presentation of case
The case of an aneurysm of the proximal occipital artery causing discomfort and tongue deviation by compression on the hypoglossal nerve is reported. Postoperative course after resection was followed by complete regression of symptoms.
Conclusion
Surgical resection, as standard treatment of aneurysms of the occipital artery, with the eventual technical adjunct of intubation by the nose is effective in durably relieving symptoms and preventing aneurysm-related complication.
1. Introduction
Spontaneous, true aneurysms of the occipital artery are extremely rare [[1], [2], [3], [4], [5], [6], [7], [8], [9]]. They may be associated with neurofibromatosis or diseases of connective tissue [2] and occipital bone defects [3,7]. Pseudo-aneurysms may develop after traumas or surgical operations [[4], [5], [6],9]. We now report the case of a true aneurysm of the proximal occipital artery causing discomfort and mild tongue deviation, due to compression over the ipsilateral hypoglossal nerve. This case is reported in line with the SCARE criteria [10].
2. Case presentation
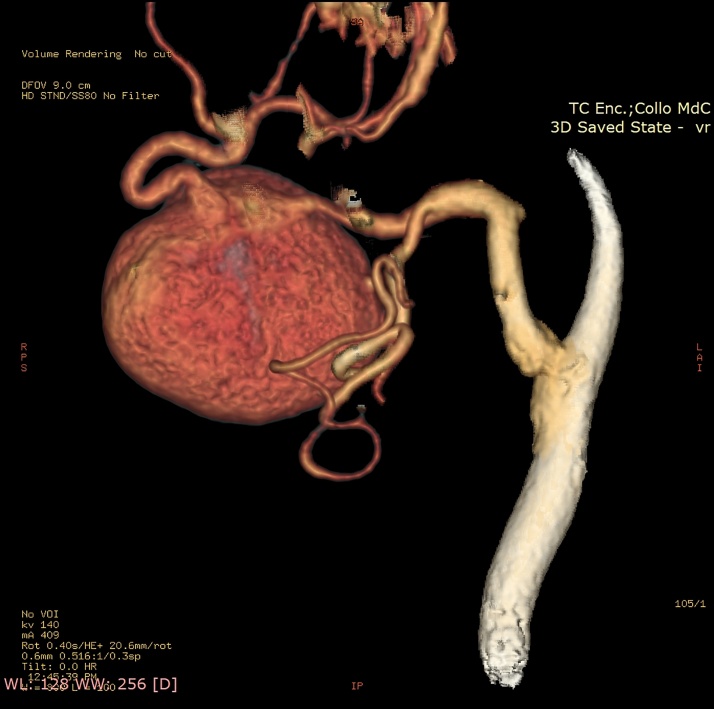
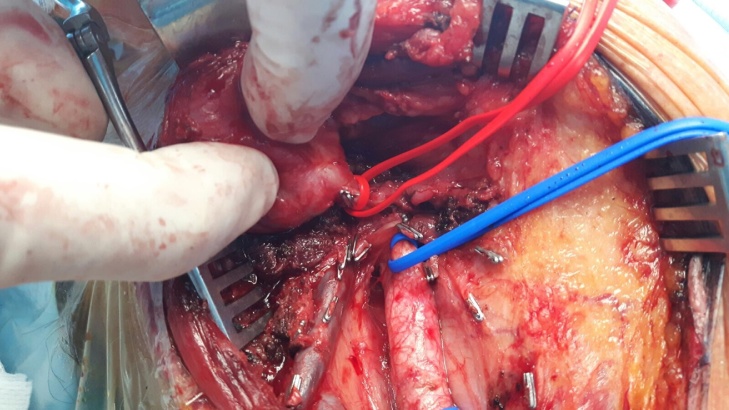
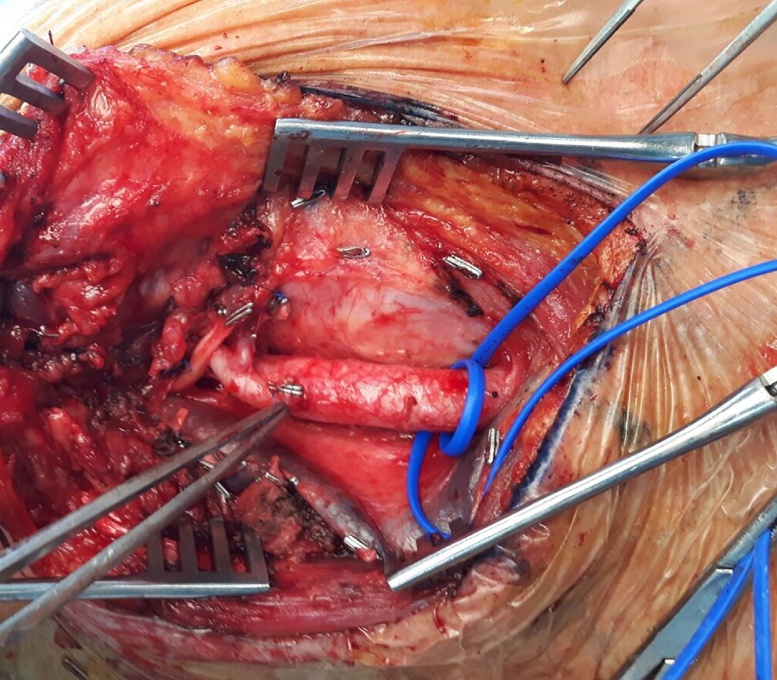
An 83-year-old woman was admitted for the treatment of an pulsating, right retromandibular-infraauricular mass. She had no history of trauma, surgery, autoimmune disease, or infection. She reported first noticing the mass, as a friend pointed out a weaving of her earring on the right side. She also complained the recent onset of a mild deviation of the tongue on the right side. Computed tomography angiography revealed a 4 cm diameter aneurysm of the right occipital artery, located on its proximal, retro-mandibular course with scarce thrombus lining (Fig. 1) and excluded associated intracranial aneurysms. Given the setting of the aneurysm and the risk of potential dislodgement of embolizing material into the internal carotid artery, surgical resection was preferred to trans-catheter embolization. Under general anesthesia with intubation by the nose, the carotid bifurcation was exposed thorough a standard, pre-sternocleidomastoid incision, prolonged toward the mastoid process. The digastric muscle was sectioned. The hypoglossal nerve was identified, exposed on its crossing over the carotid bifurcation and gently mobilized by sectioning its descending branch, without surrounding it with a loop. After systemic heparinization, the external carotid artery was clamped on a vessel-loop and the aneurysm was gently detached from the hypoglossal nerve (Fig. 2). The occipital artery was ligated and the aneurysm was resected (Fig. 3, Fig. 4). Subluxation of the mandible was not necessary. Histology was consistent with the diagnosis of a degenerative aneurysm. Postoperative course was uneventful and the right deviation of the tongue fully regressed within three weeks.
Fig. 1.
CT-scan imaging showing a saccular aneurysm of the proximal occipital artery.
Fig. 2.
Intraoperative picture. After controlling the common and external carotid arteries together with the proximal occipital artery, the aneurysm is gently mobilized and detached from the hypoglossal nerve.
Fig. 3.
Intraoperative picture. The surgical field after resection of the aneurysm.
Fig. 4.
The resected aneurysm, measuring 4 cm in its larger diameter.
3. Discussion
True degenerative aneurysms of the occipital aneurysm can be asymptomatic and appear as a pulsating mass or cause symptoms related to compression of the surrounding structures, usually with associated nevralgic. When dealing with aneurysm of the proximal occipital artery, compression or inflammatory adhesion to the hypoglossal nerve may cause tongue as in the reported case. Surgical resection is always indicated in order to prevent symptoms and complications related to aneurysmal growth. Timely surgical resection prevents rupture, allows durable cure and regression of neurologic symptoms. Depending to their location along the course of the artery, these aneurysm may pose different technical problems. Aneurysms involving the distal artery do not pose special technical problems of proximal and distal control of the artery. On the other hand, aneurysms of the proximal occipital artery are technically more demanding due to the neuro-vascular structures of the retromandibular space and require control of the carotid bifurcation. Although mandibular subluxation may not be necessary, intubation by the nose alone facilitates exposure and is advisable, especially when dealing with large aneurysms.
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request”.
4. Conclusion
Aneurysms of the proximal occipital artery are rare and may cause tongue deviation due to compression of the hypoglossal nerve. Surgical resection is best accomplished through pre-sternocleidomastoid incision, is facilitated by nasal intubation and is usually followed by complete regression of symptoms.
Conflicts of interest
The authors do not have conflicts of interest to disclose.
Funding
None.
Ethical approval
Ethical approval has been exempted by institutional committee as publication deals with a single treated case and not a randomized trial or a case series, provided that the patient gave her written consent both for operation and publication of the case.
Consent
The patient gave her written consent for operation and publication of the case. Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request”.
Author contribution
Giulio Illuminati: Study design, data analysis, critical revision, writing the paper.
Marco Cannistrà: data collection, data analysis, critical revision.
Giulia Pizzardi: data collection, data analysis, critical revision.
Rocco Pasqua: data collection, data analysis.
Francesca Frezzotti: data collection, data analysis.
Francesco G Calio’: study design, data analysis, critical revision.
Guarantor
Giulio Illuminati.
References
- 1.Chaudhry N.S., Gaynor B.G., Hussain S., Dernbach P.D., Aziz-Sultan M.A. Etiology and treatment modalities of occipital artery aneurysms. World Neurosurg. 2017;102:697. doi: 10.1016/j.wneu.2017.02.121. (e1–697.e4) [DOI] [PubMed] [Google Scholar]
- 2.Bissacco D., Domanin M., Romagnoli S., Martelli E., Civelli V., Gabrielli L. Spontaneous rupture of multiple occipital artery aneurysms in a patient with neurofibromatosis type 1. Vasc. Endovascular Surg. 2018;52:86–88. doi: 10.1177/1538574417742285. [DOI] [PubMed] [Google Scholar]
- 3.Kawasaki T., Yoshida K., Kikuchi T., Ishii A., Takagi Y., Miyamoto S. Ruptured aneurysms of the occipital artery associated with congenital occipital bone defect. World Neurosurg. 2017;97:759. doi: 10.1016/j.wneu.2016.09.116. (e13−759. e15) [DOI] [PubMed] [Google Scholar]
- 4.John N., Leach J.L., Rachana T., Mangano F.T. Traumatic aneurysm of the occipital artery secondary to paintball injury. Clin. Neurol. Neurosurg. 2009;111:105–108. doi: 10.1016/j.clineuro.2008.08.006. [DOI] [PubMed] [Google Scholar]
- 5.Skandalakis G.P., Korfias S., Kalyvas A.V., Anagnostopoulos C., Sakas D.E. A giant pseudoaneurysm of the occipital artery. Surg. Neurol. Int. 2017;8:281. doi: 10.4103/sni.sni_214_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Srinivasan V.M., Karas P.J., Sen A.N., Fridley J.S., Chen S.R., Gopinath S.P. Occipital artery pseudoaneurysm after posterior fossa craniotomy. World Neurosurg. 2017;98:868. doi: 10.1016/j.wneu.2016.12.050. (e 1- 868. e4) [DOI] [PubMed] [Google Scholar]
- 7.Kawasaki T., Yoshida K., Kikuchi T., Ishii A., Takagi Y., Miyamoto S. Ruptured aneurysms of the occipital artery associated with congenital occipital bone defect. World Neurosurg. 2017;97:759. doi: 10.1016/j.wneu.2016.09.116. e13–759. e15. [DOI] [PubMed] [Google Scholar]
- 8.Kim H.S., Son B.C., Lee S.W., Kim I.S. A rare case of spontaneous true aneurysm of the occipital artery. J. Korean Neurosurg. Soc. 2010;47:310–312. doi: 10.3340/jkns.2010.47.4.310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Patel M., Tchelepi H., Rice D.H. Traumatic pseudoaneurysm of the occipital artery: case report and review of the literature. Ear Nose Throat J. 2008;87:E7–E12. [PubMed] [Google Scholar]
- 10.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S., Orgill D.P., for the SCARE Group A protocol for the development of reporting criteria for surgical case reports: The SCARE statement. Int. J. Surg. 2016;27:187–189. doi: 10.1016/j.ijsu.2016.01.094. [DOI] [PubMed] [Google Scholar]