Abstract
Background and Objectives
Up to one-half of children may use complementary health approaches (CHA). However, current prevalence in North America, variables associated with CHA use and caregiver perceptions of effectiveness are unclear. We aimed to determine the self-reported use of CHA during the previous 12 months in paediatric patients, demographic variables associated with CHA use and perceptions around effectiveness of CHA.
Methods
A cross-sectional survey study of patients aged between 28 days and 18 years who presented to a large paediatric emergency department was conducted between December 2014 and July 2015. Univariate analysis and multivariate logistic regression were used to examine variables associated with CHA use.
Results
Of 475 potential participants, 412 (86.7%) responded to the questionnaire, of whom 369 (89.5%) had completed the entire survey. Of these, 61.7% (95% confidence interval [CI] 56.7% to 66.6%) reported using CHA for their child. The most used CHA products were vitamins and minerals (59.2%, 95% CI 52.4% to 65.7%). Among CHA practices, massage (50.0%, 95% CI 15.5% to 30.1%) was most common. Most CHA users perceived effectiveness of the therapy used. Parental education remained statistically significant (P=0.03) in multivariate logistic regression; the odds of CHA use among caregivers with university-level education were 1.65 times higher when compared with those without (95% CI 1.04% to 2.61%).
Conclusions
CHA use is higher than previously reported in children. Given the high self-reported perceived effectiveness, paediatricians and family physicians should review CHA use with their patients in an open, non-judgmental manner, exploring both perceptions of safety and efficacy.
Keywords: Alternative medicine, Caregiver perceptions, Complementary health approaches, Complementary medicine
‘Complementary health approaches’ (CHA), a new term by the National Center for Complementary and Integrative Health (NCCIH) (1) may be thought of as ‘a group of diverse medical and health care systems, practices, and products not presently considered to be part of conventional Western medicine’ (2).
A recent Cochrane review remarked on the high number of inconclusive primary research reviews around the evidence for various CHA therapies (3). Further, CHA use may be associated with adverse events (4–7) and in rare cases, may be responsible for emergency department (ED) visits (8). Despite all of this, many caregivers view CHA favourably: usually reporting effectiveness and a preference over conventional medical treatments (9).
Estimates of CHA use in children in Western countries place the prevalence anywhere from just over half of children (10,11) to as low as 2% to 15% (12,13), with less than half of CHA users reporting this use to their physician (10,11). CHA prevalence and type of CHA used may vary widely even within a country (14,15). Canadian attitudes and perceptions regarding CHA may differ from the USA given the differences in health care insurance systems, access and/or regulations. Further, countries such as Switzerland and Germany may cover CHA during medical school training (e.g., Switzerland and Germany) (16).
Despite a number of studies evaluating the use of CHA in various settings, to our knowledge, there have been no large studies examining the perception of effectiveness of specific types of CHA used among self-reported CHA users in a primary care context. Further, we have very limited recent estimates on CHA use among generally healthy children in Canada. We aimed to ensure an appropriate sample size for our study, to evaluate perceptions of effectiveness among CHA users, and to assess demographic associations with CHA use.
METHODS
Study design
We conducted a cross-sectional survey study of paediatric patients presenting with an acute, non-life-threatening complaint between December 2014 and July 2015 in the ED at the Children’s Hospital of Eastern Ontario (CHEO), one of the busiest paediatric EDs in Canada. Our survey was developed after reviewing similar robust surveys (17) and included questions around the child’s age, sex, parental education, access to private insurance, access to a primary care provider and patient or caregiver-reported health status of the child.
Data around CHA use over the previous 12 months and perceptions around effectiveness were also obtained. CHA users were defined as ‘any CHA use over the previous 12 months’. The first part of the question asked about the use of a particular CHA practice/product; if it was used, the question would branch to ask about effectiveness. For instance, if the respondent indicated that they had used acupuncture in the past 12 months for their child, the question would branch to a statement and a Likert scale response. One example is: ‘In the past, the use of acupuncture was helpful to my child’. The respondent would then indicate any one of the following responses: ‘strongly agree’, ‘somewhat agree’, ‘somewhat disagree’ and ‘strongly disagree’. We classified those responses in the ‘agree’ columns as ‘perceived effective’.
The paper survey was piloted, edited and transferred into an electronic version through RedCap that was piloted for clarity and appropriateness, with the final survey (with informed consent) being offered on an iPAD by CHEO-ED ‘SUPPORT’ research volunteers in the ED waiting room. Data were collected from the questionnaires on a rolling basis, managed by the principal investigator through RedCap and was exported and analyzed in SPSS (version 20) in the CHEO RI Clinical Research Unit. The study was approved by the CHEO Research Ethics Board (Ottawa, Canada).
Study population
Inclusion criteria
All patients attending the ambulatory care zone of the ED, who were between 28 days and 18 years of age. Age cut-offs were established to ensure generalizability to the paediatric population (0 to 18) while excluding participants in an ongoing neonatal (0 to 28 days) study in the same ED (to avoid responder fatigue or related bias) during the same study period.
Exclusion criteria
Patients over 18 or under 28 days of age, and patients presenting with Clinical Triage Assessment Score (CTAS) 1 ‘Resuscitation’ or CTAS 2 ‘Emergent’, for which a survey was not a reasonable expectation for the patient or parent/guardian.
Caregivers responded to the survey, and patients over the age of 16 were permitted to complete the survey themselves if they presented without a parent/guardian.
Outcome measures
Our survey instrument examined the main outcome measure of CHA use over the past 12 months, with secondary measures that included perceptions around effectiveness of the CHA therapy used. Questionnaire items included: patient age, gender, health-status, availability of private health insurance, highest level of parental education, CHA use and perceptions of effectiveness of CHA.
Sample size
Previous estimates in North America have reported a prevalence of between 42% and 71% in paediatric patients (10,15). Based on a conservative estimate of 50% prevalence, we required a sample size of 380 to achieve a margin of error of ±5%. We obtained a final sample size of 412 respondents before halting the study.
Statistical analysis
Analyses of the questionnaire data were performed using SPSS version 22 (IBM Corp., Released 2013, IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY). Descriptive statistics were used to examine the characteristics of the parents/guardians and patients who use CHA, as well as the frequency and perceptions around CHA use. The χ2 and Fisher’s exact tests were used to compare demographic information between CHA users and non-users. Multivariate logistic regression was used to examine the association between CHA use and various demographic variables that included gender, age, parental education, self-reported health status and availability of private insurance.
RESULTS
Study population
During the study period, a total of 475 participants were offered the survey, and 412 agreed to participate. Reasons for decline included language barrier, discharge prior to completion, parents not with child or technical difficulties. A final study sample of 369 caregivers and patients were enrolled, as 43 had missing data or did not complete the entire survey. The majority of participants were aged between 3 and 9 years (43%, 95% confidence interval [CI] 37.9% to 47.9%) and most participants were female (54.2%, 95% CI 49.1% to 59.2%). The historical and clinical characteristics of the study population are described in Table 1.
Table 1.
Demographic characteristics of the study population
| Variable | Value in % (95% CI) |
|---|---|
| Gender | |
| Male | 45.8 (40.8–50.9) |
| Female | 54.2 (49.1–59.2) |
| Age | |
| <28 days | 0.5 (0.1–2.0) |
| 29 days to 6 months | 5.7 (3.8–8.5) |
| 6 months 1 year | 5.7 (3.8–8.5) |
| 1–2 years | 20.1 (16.3–24.4) |
| 3–5 years | 21.7 (17.8–26.2) |
| 6–9 years | 21.1 (17.3–25.6) |
| 10–13 years | 14.1 (10.9–18.0) |
| 14–18 years | 11.1 (8.3–14.7) |
| Self-reported overall health status | |
| Excellent | 41.2 (36.3–46.3) |
| Very good | 37.4 (32.6–42.4) |
| Good | 16.0 (12.6–20.1) |
| Fair | 4.6 (2.8–7.2) |
| Poor | 0.8 (0.2–2.3) |
| Have primary care provider | |
| No | 7.9 (5.5–11.1) |
| Yes | 92.1 (88.9–94.4) |
| Private insurance | |
| No | 27.9 (23.6–32.7) |
| Yes | 72.1 (67.3–76.4) |
| Private insurance coverage of CHA | |
| No | 8.3 (5.5–12.2) |
| Yes | 52.3 (46.3–58.2) |
| Not sure | 39.4 (33.8–45.5) |
| Language of respondent | |
| English | 84.8 (80.8–88.1) |
| French | 15.2 (11.9–19.2) |
| Education level | |
| No certificate, diploma or degree | 1.9 (0.9–3.9) |
| High school certificate or equivalent | 11.1 (8.3–14.7) |
| Apprenticeship certificate | 2.2 (1.1–4.2) |
| College, CEGEP or other non-university diploma | 25.5 (21.3–30.2) |
| University certificate or diploma | 34.7 (30.0–39.7) |
| Postgraduate degree | 24.4 (20.3–29.0) |
| Other | 0.3 (0.04–1.5) |
CHA Complementary health approaches; CI Confidence interval.
Use of CHA
Of the 369 respondents surveyed, 228 (61.7%, 95% CI 56.7% to 66.6%) reported using any CHA products or practices for their child. When vitamins/minerals were excluded, the overall prevalence dropped slightly to 52.0% (95% CI 46.9% to 57.1%)—therefore, the use of vitamins/minerals only accounts for 10% of the prevalence. Overall, 55.8% (95% CI 50.7% to 60.8%) reported using CHA products, and 33.3% (95% CI 28.7% to 38.3%) reported using CHA practices. The use of CHA products and practices was not mutually exclusive—a number of respondents reported using both.
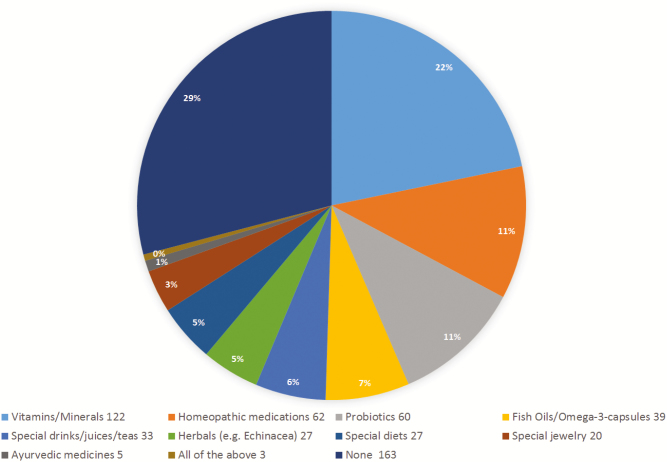
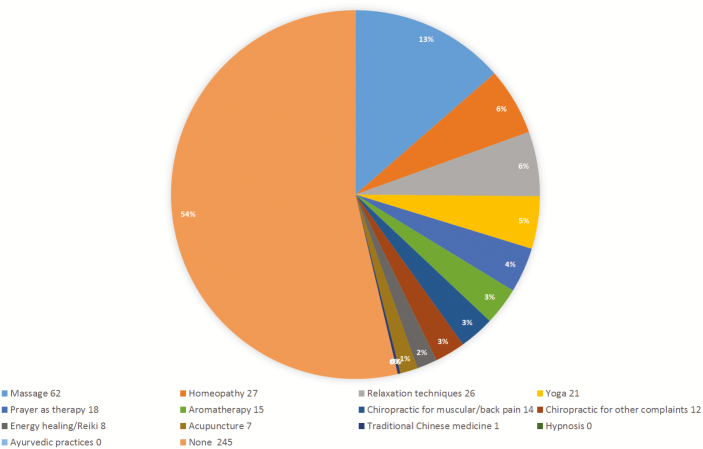
As shown in Figure 1, among users of CHA products, the most common CHA products used were vitamins and minerals (59.2%, 95% CI 52.4% to 65.7%), followed by homeopathic remedies (30%, 95% CI 24.2% to 36.7%) and probiotics (29.1%, 95% CI 23.3% to 35.7%). Figure 2 illustrates that, among users of CHA practices, the commonly used CHA practices included massage (50%, 95% CI 41.7% to 59.1%), homeopathy (21.8%, 95% CI 15.5% to 30.1%) and relaxation techniques (21%, 95% CI 14.9% to 29.2%).
Figure 1.
Most common CHA products administered within previous 12 months (N=369). CHA Complementary health approaches
Figure 2.
Most common CHA practices administered within previous 12 months. CHA Complementary health approaches
Association between CHA use and demographic variables
Among males, 62.7% (95% CI 55.2% to 69.7%) used CHA, and among females, 61.0% (95% CI 54.1% to 67.5%) used CHA. The differences were not statistically significant (P=0.734). CHA use was distributed evenly among age groups, between a 54.2% use in children under 2 to 65.6% use for children between 10 and 18 years of age (P=0.123).
There were no statistically significant associations between CHA use and language of respondent (English or French), private insurance or availability of a primary care provider. CHA use was statistically significantly higher among children who had at least one University-educated caregiver (66.1%, 95% CI 59.5% to 72.0%) compared with those who did not (55.6%, 95% CI 47.4% to 63.3%) (P=0.043).
This association remained even while controlling for other demographic variables in the multivariate model, with the odds of CHA use in children with a University-educated caregiver being 65% higher than in children without a University-educated caregiver (OR=1.65; 95% CI 1.04% to 2.61%) (P=0.03).
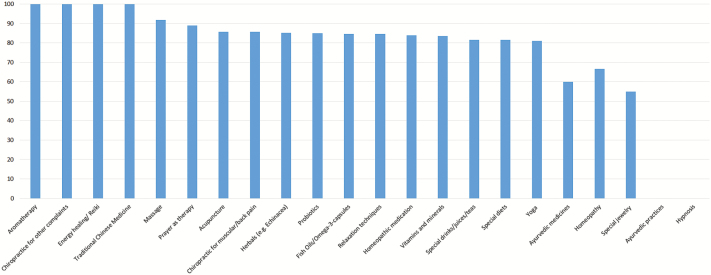
Perceptions of effectiveness of CHA use
Among those using CHA practices, as Figure 3 shows, high perceived effectiveness was noted for aromatherapy (15/15; 95% CI 79.6% to 100%), energy healing (8/8; 95% CI 67.6% to 100%), traditional Chinese medicine (1/1; 95% CI 20.7% to 100%), chiropractic for non-MSK complaints (12/12; 95% CI 75.8% to 100%), massage (57/62; 95% CI 82.5% to 96.5%), prayer (16/19; 95% CI 82.5% to 96.5%) and acupuncture (6/7; 95% CI 48.7% to 97.4%). In terms of CHA products, effectiveness was perceived to be high for probiotics (51/60; 95% CI 73.9% to 91.9%), homeopathic remedies (52/62; 95% CI 72.8% to 91.0%), vitamins/minerals (102/117; 95% CI 79.9% to 92.1%) and herbals (23/27; 95% CI 67.5% to 94.1%). Fewer found homeopathy as a practice (18/26; 95% CI 50.0% to 83.5%) or special jewellery (11/20; 95% CI 34.2% to 74.2%) helpful.
Figure 3.
Perceived effectiveness of CHA product/practice used. CHA Complementary health approaches
DISCUSSION
In this survey of 369 patients visiting a paediatric ED, we provide additional evidence of the high use of CHA in children and youth, in addition to generally high perceived effectiveness of CHA. While previous studies have assessed perceived effectiveness, limitations included subspecialty clinics (15,18). Goldman et al. examined vitamin use in paediatric ED attendees, but did not report about other CHA (5). Previous studies have examined perceived effectiveness of CHA in a general paediatric context outside of Canada (19,20). Therefore, our participants represent a population that is likely more generalizable to emergency physicians, family physicians, general paediatricians and nurse practitioners in Canada.
Overall, we found a 61.7% prevalence of CHA use in our study population, with a prevalence of 52% when vitamins and minerals were excluded. This is slightly higher than quoted previously (9,10,11,15,20,21), and much higher than other Canadian studies (13,22). These findings may suggest a general trend toward higher use of CHA in children and youth. Explanations include differences in acceptance rates by geographical location or heterogeneity in how CHA is classified—for instance, the exclusion of prayer, nutritional supplements or relaxation techniques in one study (22) or limiting the number of CHA therapies in the survey (19)—all which may lead to differences in reported prevalence.
Similar to existing literature, we found a high utilization of vitamins/minerals (13,15,21,23,24), probiotics (16,20) and homeopathic remedies (15) in addition to massage (13,15,23).
Our findings are in contrast to previous Canadian studies which found a high prevalence of reported chiropractic use as well (15,22). We postulate that oral natural health products, homeopathic remedies and massage may be used most frequently given the safety profile, accessibility and possibly the affordability of these options. Further, products such as vitamins/minerals and probiotics, in addition to massage, may be recommended in the conventional medical system; however, this does not explain why homeopathic remedies are used so frequently. It is possible that the latter are used as they are perceived as safe by the caregiver.
In terms of socioeconomic factors associated with increased use of CHA, we only found a statistically significant association between parental education—specifically that CHA use was higher among caregivers who had a University-level education compared with those that did not. Most studies examining CHA use have noted a correlation between higher parental education and CHA, and this association has been previously reported in Western Europe and North American countries (13,25–29); our results further corroborate this relationship in the Canadian context. Interestingly, this relationship is not necessarily consistent with lower-income countries such as Turkey or Iran, or in studies focused primarily in African-American populations (29–31). Thus, this association may only be generalized to higher-income countries.
Unlike previous work outside of Canada, we did not find an association with the availability of private insurance (12,20,24,32,33). It is possible that there may be two influencing factors, which makes such any possible associations difficult to predict in countries that do not have universal health care like Canada. For example, a lack of public health insurance might encourage a parent to seek alternative health care methods that may be more accessible and/or more affordable. Conversely, having extended health insurance (which we have dubbed ‘private health insurance’) may include options that cover CHA—for instance massage, acupuncture, chiropractic for dependents (i.e., children) and as such could be a factor influencing CHA use in Canada or elsewhere.
Further, we could not corroborate previous associations made between CHA use and gender (12), or self-reported health status of the child (12,33). We surmise that given how popular CHA use has become today, along with accessibility and acceptability for the general population, we may see a blurring of demographic associations such as age, gender and health status.
The general trend from our data is that users of CHA are likely to view their CHA product or practice as helpful, which has been found in studies looking at CHA use in chronic disease (7,33–35). Further research is needed to identify what therapies are most useful to whom, and why. Our findings, which reflect the Canadian context, echo previous findings in the USA (19).
The two notable modalities that did not follow the trend of upwards of over 80% perceived effectiveness were special jewellery (e.g., teething necklaces), in which just over half perceived benefit, and homeopathy with two-thirds perceiving benefit. While this may be explained by the lack of a clear biomedical model of effectiveness, it is not reflected in other techniques such as energy healing or prayer. Of interest, Ayurvedic medicines, of which some, such as curcumin (the active component of turmeric) have built a strong evidence base (36), only 60% of users perceived benefit. This echoes findings from Zuzak et al. (37) who found that parents were concerned about side effects of conventional medicine but often stated CHA therapies were effective; hence effectiveness may not always be correlated to current available evidence.
Limitations and strengths
As an exploratory study, there are several limitations. First, while our sample size was robust to examine the primary research question, it is still much smaller than other studies, which sacrifices power and external validity. Second, given that this study was done within a conventional medical system (an ED), and required the respondent to review behaviour over the past 12 months, both selection bias and recall bias are possible. This could underestimate or overestimate the actual use of CHA, as we do not account for those that may be heavily reliant on alternative practices, and may be dissuaded from visiting a conventional ED. This can also affect external validity, which is compounded by the fact that our study was a single-centre project. Third, while other have found associations between socioeconomic status and CHA use (13,29,38,39), we did not evaluate socioeconomic status or income in this study, choosing instead the proxies of parental education and private insurance. Further work may want to directly examine these variables. Future studies should consider these limitations.
Strengths of the study include a high number of respondents, provision of a secure and private electronic method to complete the survey, limited issues related to data entry (given that the responses were automatically entered into the database), multiple options of different CHA modalities and the availability of a SUPPORT research volunteer should the respondent require clarification for any particular question.
CONCLUSIONS
Despite these limitations, this study has clear clinical implications. These results corroborate previous studies finding prevalence of CHA use among over half of children, and, given a large increase in prevalence from previous estimates, may suggest a general trend in Canada toward increased prevalence of CHA use in children. We also call into question the association between demographic variables (notably availability of private insurance, age, health status and gender) while reaffirming other demographic factors (i.e., parental education) and the decision to use CHA in children. Moreover, we add novel information around perceptions of effectiveness of CHA use in Canadian children, generally showing that most caregivers perceive their chosen CHA modality as effective.
Future work should focus on using a survey instrument that has both content and construct validity in paediatrics, aim for an even larger sample size to have greater power to further examine socioeconomic factors (for instance income and cultural background), evaluate perceived side effects of CHA and choose respondents who actively use the conventional medical system (e.g., in hospitals and clinics) in addition to those that may not (e.g., alternative provider clinics, schools surveys) to improve external validity. Above all we hope that this study helps encourage paediatric providers to probe more deeply into the products and practices used by their patients, become more familiar with the theory and evidence around CHA and provide care in an open and non-judgmental way for all paediatric patients, regardless of the provider’s own use or preference for CHA.
Conflict of Interest
The authors have no conflicts of interest relevant to this article to disclose.
Acknowledgements
The authors would like to acknowledge the literature search guidance provided by Dr Margaret Sampson, translation services provided by Melissa Jean-Baptiste and survey distribution coordination by Jessica Paul. All study authors had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. A.K. conceptualized and designed the study, designed the data collection instruments, drafted the initial manuscript and approved the version of the manuscript that was submitted. R.Z. reviewed the study design, coordinated and supervised data collection, reviewed the analysis plan, critically reviewed the manuscript and approved the final manuscript as submitted. J.C. carried out the initial analyses, reviewed the manuscript and approved the final manuscript as submitted. N.B. designed the initial analysis plan, supervised the initial analysis, critically reviewed the manuscript and approved the manuscript as submitted. S.V. reviewed the study design, shared relevant instruments from other studies, reviewed the survey instrument, critically reviewed the manuscript and approved the final manuscript as submitted. K.T.-A. reviewed the survey instrument, critically reviewed the manuscript and approved the final manuscript as submitted. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work. This study was supported by a resident research grant from the Children’s Hospital of Eastern Ontario Research Institute. The authors have no financial relationships relevant to this article to disclose.
References
- 1. National Center for Complementary and Integrative Health. Complementary, Alternative, or Integrative Health: What’s in a Name? <https://nccih.nih.gov/health/integrative-health> (Accessed August 9, 2017).
- 2. Kemper KJ, Vohra S, Walls R. American Academy of Pediatrics: The use of complementary therapies in pediatrics. Pediatrics 2008;122(6):1374–86. [DOI] [PubMed] [Google Scholar]
- 3. Meyer S, Gortner K, Karsen A, Kutschke G, Gottschling S, Graber S. Complementary therapies in paediatrics: A systematic overview/synthesis of Cochrane Collaboration reviews. Swiss Med Weekly 2013;143:w13794. [DOI] [PubMed] [Google Scholar]
- 4. Canadian Paediatric Surveillance Program. Complementary therapies in paediatrics: Looking at the safety profile. Paediatr Child Health 2008;13(6):492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Goldman RD, Rogovik AL, Lai D, Vohra S. Potential interactions of drug-natural health products and natural health products-natural health products among children. J Pediatr 2008;152(4):521–6, 526.e1–4. [DOI] [PubMed] [Google Scholar]
- 6. Vohra S, Brulotte J, Le C, Charrois T, Laeeque H. Adverse events associated with paediatric use of complementary and alternative medicine: Results of a Canadian Paediatric Surveillance Program Survey. Paediatr Child Health 2009;14(6):385–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Beringer A, Vaillancourt R, Villarreal G, Vadeboncoeur C. The use of natural health products by paediatric patients in respite care. Paediatr Child Health 2015;20(1):23–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Geller AI, Shehab N, Weidle NJ et al. Emergency department visits for adverse events related to dietary supplements. N Engl J Med 2015;373(16):1531–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Zuzak TG, Zuzak-Siegrist I, Simoes-Wust AP, Rist L. Use of complementary therapies by patients presenting to a pediatric emergency department. Eur J Pediatrics 2009;168(4):431–7. [DOI] [PubMed] [Google Scholar]
- 10. Jean D, Cyr C. Use of complementary therapies in general pediatric clinic. Pediatrics 2007;120(1):e138–41. [DOI] [PubMed] [Google Scholar]
- 11. Madsen H, Andersen S, Nielsen RG, Dolmer BS, Høst A, Damkier A. Use of complementary/alternative medicine among paediatric patients. Eur J Pediatr 2003;162(5):334–41. [DOI] [PubMed] [Google Scholar]
- 12. Yussman SM, Ryan SA, Auinger P, Weitzman M. Visits to complementary therapies providers by children and adolescents in the United States. Ambul Pediatr 2004;4(5):429–35. [DOI] [PubMed] [Google Scholar]
- 13. Losier A, Taylor B, Fernandez CV. Use of alternative therapies by patients presenting to a pediatric emergency department. J Emerg Med 2005;28(3):267–71. [DOI] [PubMed] [Google Scholar]
- 14. Cincotta DR, Crawford NW, Lim A et al. Comparison of complementary therapies use: Reasons and motivations between two tertiary childrens hospitals. Arc Dis Child 2006;91(2):153–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Adams D, Dagenais S, Clifford T et al. Complementary therapies use by pediatric specialty outpatients. Pediatrics 2013;131(2):225–32. [DOI] [PubMed] [Google Scholar]
- 16. Brinkhaus B, Witt CM, Jena S, Bockelbrink A, Ortiz M, Willich SN. Integration of complementary and alternative medicine into medical schools in Austria, Germany and Switzerland—results of a cross-sectional study. Wien Med Wochenschr 2011;161(1–2):32–43. [DOI] [PubMed] [Google Scholar]
- 17. Adams D, Schiffgen M, Kundu A et al. Patterns of utilization of complementary therapies in 2 pediatric gastroenterology clinics. J Pediatr Gastroenterol Nutr 2014;59(3):334–9. [DOI] [PubMed] [Google Scholar]
- 18. Richmond E, Adams D, Dagenais S, et al. Complementary therapies: A survey of its use in children with chronic respiratory illness. Can J Respir Ther 2014;50(1):27–32. [PMC free article] [PubMed] [Google Scholar]
- 19. Pitetti R, Singh S, Hornyak D, Garcia SE, Herr S. Complementary therapies use in Children. Pediatr Emerg Care 2001;17(3):165–9. [DOI] [PubMed] [Google Scholar]
- 20. Taylor DM, Dhir R, Craig SS et al. Complementary therapies use among paediatric emergency department patients. J Paediatr Child Health 2015;51(9):895–900. [DOI] [PubMed] [Google Scholar]
- 21. Lim A, Cranswick N, Skull S, South M. Survey of complementary therapies use at a tertiary children’s hospital. J Paediatr Child Health 2005;41(8):424–7. [DOI] [PubMed] [Google Scholar]
- 22. Spiegelblatt L, Laine-Ammara G, Pless IB, Guyver A. The use of alternative medicine by children. Pediatrics 1994;94:811–4. [PubMed] [Google Scholar]
- 23. Galicia-Connolly E, Adams D, Bateman J et al. CT use in pediatric neurology: An exploration of concurrent use with conventional medicine. PLoS ONE 2014;9(4):e94078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Loman DG. The use of complementary and alternative health care practices among children. J Pediatr Health Care 2003;17(2):58–63. [DOI] [PubMed] [Google Scholar]
- 25. Kemper KJ, Gardiner P, Birdee GS. Use of complementary and alternative medical therapies among youth with mental health concerns. Acad Pediatr 2013;13(6):540–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Akins RS, Krakowiak P, Angkustsiri K, Hertz-Picciotto I, Hansen RL. Utilization patterns of conventional and complementary/alternative treatments in children with autism spectrum disorders and developmental disabilities in a population-based study. J Dev Behav Pediatr 2014;35(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Italia S, Brand H, Heinrich J, Berdel D, von Berg A, Wolfenstetter SB. Utilization of complementary therapies (CT) among children from a German birth cohort (GINIPlus): Patterns, costs and trends of use. BMC Complement Altern Med 2015;15:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Vinson R, Yeh G, Davis RB, Logan D. Correlates of complementary therapies use in a pediatric tertiary pain center. Acad Pediatr 2014;14(5):491–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Zuzak TJ, Zuzak-Siegrist I, Rist L, Staubli G, Simoes-Wust AP. Attitudes towards vaccination: Users of complementary therapies versus non-users. Swiss Med Wkly 2008;138(47–48):713–8. [DOI] [PubMed] [Google Scholar]
- 30. Fesharakinia A, Abedini M. Prevalence of using complementary therapies in children and its related factors in East Iran. Iran J Pediatr 2014;24(1):111–4. [PMC free article] [PubMed] [Google Scholar]
- 31. Tuncel T, Sen V, Kelekci S et al. Use of complementary therapies in children who have no chronic disease. Turk Pediar Ars 2014;49(2):148–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Sawni A, Ragothaman R, Thomas RL, Mahajan P. The use of complementary/alternative therapies among children attending an urban pediatric emergency department. Clin Pediatr (Phila) 2007;46(1):36–41. [DOI] [PubMed] [Google Scholar]
- 33. Adams D, Whidden A, Honkanen M et al. Complementary therapies: A survey of its use in pediatric cardiology. CMAJ Open 2014;2(4):E217–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Vlieger AM, Blink M, Tromp E, Benninga MA. Use of complementary and alternative medicine by pediatric patients with functional and organic gastrointestinal diseases: Results from a multicenter survey. Pediatrics 2008;122(2):e446–51. [DOI] [PubMed] [Google Scholar]
- 35. Sanchez HC, Karlson CW, Hsu JH, Ostrenga A, Gordon C. Complementary therapies use in pediatric hematology/oncology patients at the University of Mississippi Medical Center. J Altern Complement Med 2015;21(11):660–6. [DOI] [PubMed] [Google Scholar]
- 36. Kumar S, Ahuja V, Sankar MJ, Kumar A, Moss AC. Curcumin for maintenance of remission in ulcerative colitis. Cochrane Database Syst Rev 2012;10:CD008424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Zuzak TJ, Zuzak-Siegrist I, Rist L, Staubli G, Simoes-Wust AP. Medicinal systems of complementary therapies: A cross-sectional survey at a pediatric emergency department. J Alternat Complement Med 2010;16(4):473–9. [DOI] [PubMed] [Google Scholar]
- 38. Ganasegeran K, Rajendran AK, Al-Dubai SA. Psycho-socioeconomic factors affecting complementary therapies use among selected rural communities in Malaysia: A cross-sectional study. PLoS ONE 2014;9(11):e112124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Burke A, Nahin RL, Stussman BJ. Limited health knowledge as a reason for non-use of four common complementary health practices. PLoS ONE 2015;10(6):e0129336. [DOI] [PMC free article] [PubMed] [Google Scholar]