Abstract
Social disability is a defining characteristic of schizophrenia and a substantial public health problem. It has several components that are difficult to disentangle. One component, social disconnection, occurs extensively in the general community among nonhelp-seeking individuals. Social disconnection is an objective, long-standing lack of social/family relationships and minimal participation in social activities. It is associated with negative health effects, including early mortality, and is distinct from subjective loneliness. These 2 topics, social disability in schizophrenia and social disconnection in the general community, have generated entirely distinct research literatures that differ in their respective knowledge gaps and emphases. Specifically, the consequences of social disability in schizophrenia are unknown but its determinants (ie, nonsocial cognition, social cognition, and social motivation) have been well-examined. Conversely, the health consequences of social disconnection in the general community are well-established, but the determinants are largely unknown. Social disconnection is a condition that presents substantial public health concerns, exists within and outside of current psychiatric diagnostic boundaries, and may be related to the schizophrenia spectrum. A comparison of these 2 literatures is mutually informative and it generates intriguing research questions that can be critically evaluated.
Keywords: schizophrenia, cognition, functioning, social connections, social integration
The boundaries that separate psychopathology from health are indistinct. Social disability is a feature of schizophrenia1 that occurs with surprising frequency, and in a revealing manner, outside the illness in the general community. Social disability is pervasive, stable, and long-standing throughout the course of illness in schizophrenia, and it is present at intermediate levels in other severe mental illnesses, such as bipolar disorder.2–4 Social disability is a complex and difficult phenomenon to study because it is a multidimensional, multiply determined feature of schizophrenia that includes reduction in 3 major functional spheres: independent living, work and school, and interpersonal contacts with friends and family.5,6 Although it is commonly studied as a single entity, its inherent complexity means that a better understanding of social disability in schizophrenia requires us to disentangle its constituent components. The determinants and consequences for one aspect of social disability are unlikely to be the same as the others. Hence, insights can be obtained by careful consideration of each functional sphere. Here, we focus on one component: reduced contact with friends and family, ie, social disconnection. In this At Issue, we summarize 2 distinct literatures: one on social disability in schizophrenia and one on social disconnection in the general community. The goal is to hold these 2 literatures side-by-side to see how they complement and mutually inform each other, as well as to identify innovative research directions.
Social Disability in Schizophrenia
Schizophrenia is among the top 10 causes of disability for both adult men and women in developed countries,4 and the degree of social disability in schizophrenia remains high throughout the world despite the common use of antipsychotic medications.4,7 The progress in management of psychotic symptoms contrasts with the lack of progress for functional improvements in schizophrenia and underscores that these are relatively separate forms of outcome. This realization led to a focus on unmet therapeutic needs that might be required for improved functioning; ie, a focus on recovery-oriented interventions.8,9 Overall, the determinants of social disability can be divided into 2 general categories: ability and motivation.
Ability variables include social and nonsocial cognition which represent the skills needed to interact with one’s world.10,11 Nonsocial cognition, including memory, attention, reasoning and problem solving, and speed of processing are consistent determinants of social disability in schizophrenia.12,13 Abilities linked to social processes, referred to as social cognition, include such processes as perceiving social cues, sharing other peoples’ experiences, and inferring other peoples’ thoughts and emotions.14
Of the 2 types of abilities, social cognition tends to have stronger associations with social disability than nonsocial cognition,15 suggesting that social cognitive abilities are building blocks for interpersonal interactions and productive activities.16,17 It appears that some social processing systems are intact or largely intact (eg, experience sharing, emotional experience) in schizophrenia, whereas others are clearly impaired.14 For example, social cue recognition, the ability to process a diverse array of social cues from faces, voices and body movements, is impaired in schizophrenia.14 Several meta-analyses of functional neuroimaging studies indicate that people with schizophrenia show aberrant neural activity for face emotion identification in the amygdala and fusiform regions.18,19 Mentalizing, the ability to infer the mental states of other people,20,21 is also impaired in schizophrenia.22
Aside from social processing abilities, motivation to engage with the social world is needed to achieve successful interactions. Motivation refers to what people are willing to do, and includes the direction, intensity, and persistence of goal-directed behavior.23 Motivation is most often assessed in schizophrenia through clinically rated negative symptom interviews.24 However, these scales are not designed to distinguish between different types of motivation; eg, differences between social approach and social avoidance motivation. These aspects of social motivation are not simply 2 sides of the same coin; they involve distinct neural systems.25,26 The problems of social motivation in schizophrenia can stem from disturbances in either type of motivational drive. For example, those with prominent clinically rated asociality show diminished social approach motivation and a lack of motivation to seek out social interactions.27–29 However, others show elevated social avoidance motivation in that they are interested in social connections but do not attempt to engage in them due to fear of rejection.30,31
Social Disconnection in the General Community
Social disconnection is a major public health problem that is associated with a wide range of negative effects, including early mortality.32–35 Social disconnection refers to an objective, long-standing lack of social/family relationships and minimal participation in social/family activities.36 Although social disconnection is prevalent in the general community,32,34 these individuals fall beneath the mental health radar because they typically do not seek treatment and, thus, do not come to the attention of clinicians. The term general community in this context includes people with and without diagnoses of mental illness. Most of the research in the general community have used surveys of large samples and have not conducted assessments for psychiatric diagnoses.
Although social disconnection has received considerably less attention than other known risk factors, evidence is overwhelming that it plays a role in early mortality.33–35 Associations have been reported between social disconnection and blood pressure, lipids, inflammatory response, immune function, and white matter integrity.37–40 A recent meta-analysis found that social disconnection was linked with a 29% increased risk for development of coronary heart disease and a 32% increased risk for stroke.41 The risk for dementia is also heightened,42 as well as memory decline in older adults.43,44
Social disconnection is consistently associated with all-cause early mortality.32–35 A meta-analysis examined prospective all-cause mortality data across 148 studies (over 300000 participants) with an average follow-up of 7.5 years.32 Sixty-three studies examined social disconnection and the odds ratio for survival was 1.57; ie, people with more social relationships had 50% higher odds of survival compared to those with fewer relationships. Fewer social relationships carry a risk that is comparable to that of smoking, and exceeds other factors such as obesity and alcohol abuse.32 Another recent, very large meta-analysis (>3 million participants) controlled for numerous potentially confounding variables (eg, age, health status at baseline, socioeconomic status) and reported an increased mortality risk of 29%–32% in socially disconnected adults.35
It is important to distinguish social disconnection from loneliness. Loneliness is based on the subjective evaluation of social interactions, while social disconnection is based on the objective quantity of the interactions. Thus, people may feel lonely even when surrounded by friends and family. Loneliness is closely related to depressed mood.45,46 Notably, social disconnection and loneliness are only weakly correlated (about r = .25).47,48
Social Disconnection and Society
Social disconnection is relatively common in the United States, and might be on the rise.49 Across studies and surveys an estimated 5%–10% of respondents report that they have no confidants in their social network.50,51 In addition, data from the General Social Survey and other large representative studies indicate that the mean overall social network size (ie, number of people who are considered to be confidants or with whom the respondent could discuss important matters) has decreased in recent decades. For example, the mean number of confidants in this survey decreased from approximately 3 people in 1985 to approximately 2 people in 2004.49 This finding has been replicated in other recent studies50,51 suggesting that modern social networks are diminishing in size.
Technology, particularly email, texting, internet use, and social media, is changing the nature of social connection, and it is cutting in both directions. On the one hand, technological advances have dramatically expanded the means by which people can establish and maintain connections to others. Several studies have reported beneficial effects of increased social media use, such as greater self-esteem, greater sense of belonging, and enhancement of users’ existing relations.52,53 However, while the technology has enhanced the opportunity for social connectivity, there may be a corresponding cost in the “depth” of such connections, which may be less supportive, rich, and meaningful. Consistent with this perspective, some studies report links between increased internet/social media use and depression, loneliness, and reduced self-esteem and life satisfaction, although others fail to find such relations.54–56
Recruiting People With Social Disconnection in the General Community
To better understand the clinical features of individuals with social disconnection in the community, we placed an ad online (Craigslist) that solicited “healthy individuals … who have few friends, or have little need of friends, or typically prefer to do activities alone.” We assessed 30 individuals with scales for psychiatric diagnosis, degree of social connections to family and friends, autism, and loneliness. The Box includes 3 case vignettes to illustrate the types of individuals who responded to the notice.
All participants self-reported being socially disconnected, but they were not entirely removed from the community (see Table 1 and case vignettes). They averaged over 15 years of education, 50% were currently or formerly married, and most worked full-time (30%) or part-time (60%). Two participants had psychotic symptoms, 3 had a history of recurrent depression, and 3 had a history of anxiety disorder. Notably, 10 met criteria for a personality disorder that can be considered within the schizophrenia spectrum. Fifteen participants received no psychiatric diagnosis. About one-third of our sample (n = 11) were considered lonely based on our assessment of loneliness57 and no participant had elevated scores on a measure of the autistic spectrum.58
Table 1.
Demographic and Clinical Information on the Community Sample Recruited for Social Disconnection (n = 30)
| Age (SD) | 45.2 (9.2) |
| Gender (F/M) | 11/19 |
| Education (SD) | 15.3 (2.5) |
| Marital status (single/married/divorced) | 15/10/5 |
| Work (full/part/none) | 9/18/3 |
| Psychiatric diagnosesa | |
| Psychotic symptoms | 2 |
| History of bipolar disorder | 1 |
| History of recurrent depression | 3 |
| History of anxiety disorder | 3 |
| Personality disorder | 10 |
| Paranoid (3) | |
| Schizotypal (1) | |
| Avoidant (2) | |
| Schizoid (3) | |
| Not otherwise specified (1) | |
| No diagnosis (among the mood, psychotic, and personality disorders probed) | 15 |
aSome participants received more than one diagnosis.
Regarding social networks, the sample scored very low, indicating that the recruitment method indeed yielded a disconnected group. We administered the Role Functioning Scale59 which we have used in previous studies with healthy controls and people with schizophrenia.60 The measure includes a subscale for connections to friends and one for connections to family (both rated on a 7-point Likert scale). The scores for this community sample were essentially the same as those with chronic schizophrenia for friends (both groups had a mean of 4.3) and family (means of 5.0 and 5.1 for chronic schizophrenia and disconnected individuals, respectively), and both were well below the levels seen in healthy controls (means of 6.2 and 6.5 for friends and family, respectively). Notably, the degree of social disconnection was comparable for those with a psychiatric diagnosis (excluding the 2 with psychosis) versus those with no diagnosis (means of 4.3 vs 4.5 for friends; 4.9 vs 5.1 for family, for those with and without a diagnosis, respectively).
Implications of These Separate Literatures for a Research Agenda
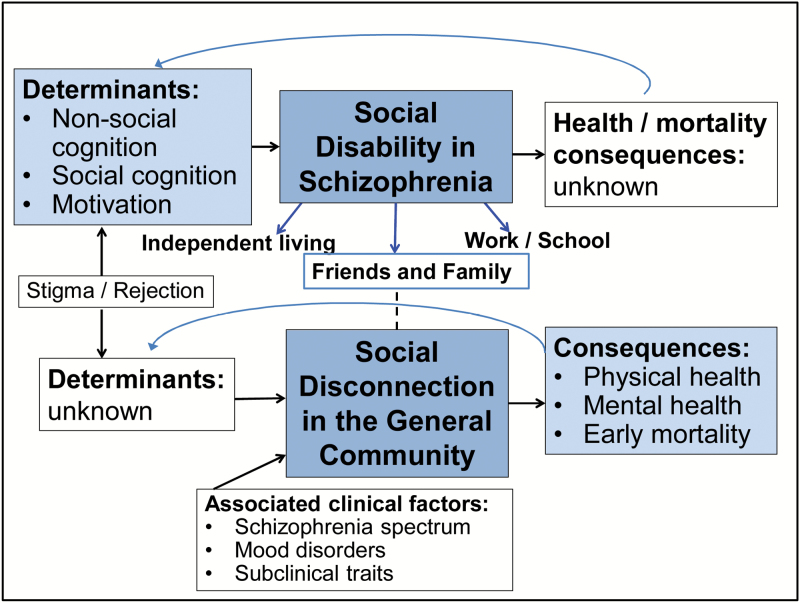
These 2 literatures each have impressive accomplishments, clear findings, and notable knowledge gaps (Figure 1). These gaps lead to intriguing, and testable, research questions.
Fig. 1.
Social disability and social disconnection. This figure shows the known determinants and consequences of social disability in schizophrenia (top part) and social disconnection in the general community (bottom part), as well as the remaining gaps in knowledge. It also depicts some of the clinical and associated features that might be associated with social disconnection in the community.
What Are the Health and Mortality Consequences of Social Disconnection in Schizophrenia?
The literature on social disconnection in the community might provide clues regarding reasons for reduced life expectancy in schizophrenia. Schizophrenia is associated with a life expectancy about 20 years shorter than that of the general population.61,62 Many factors have been identified that contribute to this risk for early mortality, including heart disease, life style factors (eg, smoking, lack of physical exercise), and suicide. Perhaps social disconnection is a contributor as well. In support of this notion, a recent 13-year follow up study of people with psychotic disorders in Finland found that living alone at baseline was a strong and significant predictor of mortality, with a larger effect size than even smoking status or metabolic syndrome.63
What Are the Determinants of Social Connection in the Community?
Most of what we know about determinants of social disconnection in the community comes from large surveys and health outcome data, but examination of determinants requires more intensive examination of smaller samples and longitudinal designs. The literature on schizophrenia suggests that social processing abilities and social motivation might be relevant for disconnection in the community. However, a systematic examination of these factors requires more costly and time-consuming assessments, including specialized self-report measures, and neuroscientific approaches such as electroencephalography and functional magnetic resonance imaging.
The study of determinants of social disconnection in the general community will naturally lead to interventions that target those determinants. In schizophrenia, this approach has taken the form of recovery-oriented interventions that target potential ability and motivational determinants of social disability. Nonpharmacological interventions include social cognitive skills training,64,65 cognitive behavioral therapy,66,67 and cognitive remediation.68 There is interest in combining innovative pharmacological (eg, oxytocin) or neurostimulation (eg, transcranial direct current stimulation) approaches with traditional approaches to enhance the effects of training interventions.69–71 Much of the efforts to improve determinants of functional outcome in schizophrenia have focused on novel drugs to enhance cognition, social cognition, and negative symptoms/motivation.72–74 These efforts to develop interventions to treat personal determinants of social disability may prove useful for social disconnection in the general community.
Is Social Disconnection Associated With Risk for Subsequent Psychopathology?
Another question that arises from schizophrenia research is whether social disconnection in the general community is associated with risk for subsequent psychopathology. For example, schizoid traits, such as social anhedonia, are elevated among individuals at heightened risk for schizophrenia (eg, first degree relatives) and predict later onset of psychosis.28,75–76 Individuals with elevated social anhedonia often report a preference for solitude that is not accompanied by loneliness and, by their own choice, have diminished social/family connections.77 Further investigation of links between social disconnection and schizotypy in the general community could help identify the determinants of social disconnection and, possibly, new opportunities for early intervention. Social disconnection may be predictive for other (nonschizophrenia-spectrum) types of psychopathology. For example, a large prospective study found that reduced social networks increased the rate of depression in men over 2 years.78
What Is the Role of Stigma and Rejection for Social Disconnection?
It is possible that odd or eccentric behaviors among disconnected individuals in the general community that are perceived as rare may lead to gradual social distancing. For example, an online study of attitudes toward mental illness found that one-third of the sample would distance themselves from someone with schizophrenia and a full 20% would “flee” if in contact with a person with schizophrenia.79 These responses were attributed to fear of unpredictability and perceived dangerousness. Importantly, little is known about the temporal relation between behaviors associated with the illness, social distancing and rejection, and social disability. Further, it is possible that any odd or eccentric behaviors among disconnected individuals in the general community may lead to gradual social distancing. However, longitudinal data will be needed to ascertain whether these attributes precede or follow social disconnection.
Independent and Interactive Effects of Loneliness Vs Social Disconnection
As mentioned above, loneliness and social disconnection are only weakly correlated and they are seldom examined in the same study. Social disconnection and loneliness have comparable effects on early mortality (increases of 29% and 26%, respectively, in a recent meta-analysis) but these estimates come from different sets of studies.35 One large study that examined both constructs prospectively found that both social disconnection and loneliness predicted all-cause mortality.33 The higher mortality rates for social disconnection remained significant when controlling for baseline health factors, but this was not true for loneliness. These findings suggest that social disconnection in particular is an independent, and likely causal, factor for all-cause mortality. Overall, there is a notable paucity of studies that examine both factors and thereby can evaluate the unique contributions of each.
How Does Social Disconnection Develop Over the Life Span?
In schizophrenia, it is well-established that problems in social interactions exist well before onset of psychotic symptoms, including in the prodromal period and even in early childhood.80–82 However, it is not known how early problems in interactions harden into stable patterns of social disconnection. The developmental course of social disconnection in the general community is clearly diverse. For many people, social disconnection represents a long-standing pattern of diminished interpersonal interactions. Longitudinal studies have shown that toddlers with high levels of behavioral restraint and sensitivity to novel stimuli are significantly more quiet and socially avoidant at age 783 and more impaired by social anxiety in adolescence.84 However, we also know that social disconnection can change over time and can be influenced by major life events. For example, marriage, retirement, and loss of a spouse all can strongly alter one’s social networks. A developmental perspective on social disconnection would be highly valuable, but is currently missing.
Conclusion
We focused on one functional sphere of social disability in schizophrenia, namely social disconnection. The 2 research literatures (social disability in schizophrenia and social disconnection in the general community) have proceeded in parallel with little scientific interaction. Yet, we see promising opportunities for these areas to be mutually informative. It is possible that social disconnection in the general community and the schizophrenia spectrum may have shared risk factors and determinants, or social disconnection may be a risk factor for development of schizophrenia. Overall, social disconnection is a common condition that presents substantial public health concerns and exists both within and outside of current psychiatric diagnostic boundaries.
Box: Participant vignettes
TL
TL is a 49-year-old single female. At the time of the interview she was living alone in an apartment, employed sporadically as a TV extra and intermittently collecting unemployment disability. She completed college with a degree in French language and culture. She reported she “loves” being an actress and feels like “dressing up and playing all day” is her way of “participating in society.” She spent her time exercising, watching cooking and travel shows, baking, and running errands. When asked why she responded to the study ad, she stated, “I have few friends and prefer to be alone.” Further, she reported she had never been in a close romantic relationship but would like a significant other. On measures of social disconnection, she endorsed low levels of social approach motivation and moderate levels of loneliness. She endorsed some personality disorder traits, including preferring to do things alone because it makes her more efficient, and expressing ambivalence about physical intimacy, but she did not meet criteria for a personality disorder.
MJ
MJ is a 32-year-old, married female who was employed as a postdoctoral fellow in the business school of a large, university at the time of her interview. When asked why she responded to our ad, she replied that she “in fact does not like people,” “feels antisocial,” and “having no friends doesn’t bother her.” She described herself as someone who “is not receptive to socializing.” If at a work-related conference she “buys lunch at the hotel and eats alone instead of eating at the conference lunch” with others. She reported that, other than her husband, she does not talk with family and her only social contact with others consists of interacting with co-workers. She spends her time working, reading, watching TV, and hanging out with her husband. (Incidentally, her husband also reported being socially disconnected. He reported high levels of social anxiety and avoidance. Although he spends time with his wife and has casual acquaintances at work, he reported that he prefers solitary activities such as video games). On measures of social disconnection, MJ scored extremely low on social approach motivation and extremely high on social avoidance, and low on role functioning scores for family and social networks. She met diagnostic criteria for schizoid personality disorder.
SK
SK is a 46-year-old, single male with no children who was working part time as a background actor in the film and television industry at the time of the interview. During the interview he said that “I have no friends right now,” “when I’m around people who don’t have positive energy I feel uncomfortable and have to leave,” and “loneliness is my best friend.” He said that he had recently severed all relationships and moved to a different city. SK reported he wished he were more open and outgoing. He indicated that he spent his free time in bed the whole day, browsed the internet, occasionally exercised, and visited stores. He scored moderately low on measures of social approach and high on social avoidance. His ratings for social networks were very low. During the diagnostic interview he endorsed the need for few close friends, ideas of reference, and demonstrated odd thinking and speech. He met diagnostic criteria for schizotypal personality disorder.
Funding
This work was supported by National Institute of Mental Health (MH110470 to Dr Green).
Acknowledgments
Dr Green has been a consultant for AbbVie, ACADIA, DSP, and Takeda, a member of the Scientific Board of Luc, and has received research funds from Forum. The other authors report no disclosures.
References
- 1. APA. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, (DC): American Psychiatric Association; 2013. [Google Scholar]
- 2. Juckel G, Morosini PL. The new approach: psychosocial functioning as a necessary outcome criterion for therapeutic success in schizophrenia. Curr Opin Psychiatry. 2008;21:630–639. [DOI] [PubMed] [Google Scholar]
- 3. Burns T, Patrick D. Social functioning as an outcome measure in schizophrenia studies. Acta Psychiatr Scand. 2007;116:403–418. [DOI] [PubMed] [Google Scholar]
- 4. Organization WH. The Global Burden of Disease: 2004 Update. Geneva, Switzerland: WHO Press; 2008. [Google Scholar]
- 5. Brekke JS, Long JD. Community-based psychosocial rehabilitation and prospective change in functional, clinical, and subjective experience variables in schizophrenia. Schizophr Bull. 2000;26:667–680. [DOI] [PubMed] [Google Scholar]
- 6. Brekke J, Kay DD, Lee KS, Green MF. Biosocial pathways to functional outcome in schizophrenia. Schizophr Res. 2005;80:213–225. [DOI] [PubMed] [Google Scholar]
- 7. Hegarty JD, Baldessarini RJ, Tohen M, Waternaux C, Oepen G. One hundred years of schizophrenia: a meta-analysis of the outcome literature. Am J Psychiatry. 1994;151:1409–1416. [DOI] [PubMed] [Google Scholar]
- 8. Hyman SE, Fenton WS. Medicine. What are the right targets for psychopharmacology?Science. 2003;299:350–351. [DOI] [PubMed] [Google Scholar]
- 9. Green MF, Nuechterlein KH, Gold JM et al. Approaching a consensus cognitive battery for clinical trials in schizophrenia: The NIMH-MATRICS conference to select cognitive domains and test criteria. Biol Psychiatry. 2004;56:301–307. [DOI] [PubMed] [Google Scholar]
- 10. Green MF, Hellemann G, Horan WP, Lee J, Wynn JK. From perception to functional outcome in schizophrenia: modeling the role of ability and motivation. Arch Gen Psychiatry. 2012;69:1216–1224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Harvey PD, Raykov T, Twamley EW, Vella L, Heaton RK, Patterson TL. Validating the measurement of real-world functional outcomes: phase I results of the VALERO study. Am J Psychiatry. 2011;168:1195–1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Green MF. What are the functional consequences of neurocognitive deficits in schizophrenia?Am J Psychiatry. 1996;153:321–330. [DOI] [PubMed] [Google Scholar]
- 13. Green MF, Kern RS, Heaton RK. Longitudinal studies of cognition and functional outcome in schizophrenia: implications for MATRICS. Schizophr Res. 2004;72:41–51. [DOI] [PubMed] [Google Scholar]
- 14. Green MF, Horan WP, Lee J. Social cognition in schizophrenia. Nat Rev Neurosci. 2015;16:620–631. [DOI] [PubMed] [Google Scholar]
- 15. Fett AK, Viechtbauer W, Dominguez MD, Penn DL, van Os J, Krabbendam L. The relationship between neurocognition and social cognition with functional outcomes in schizophrenia: a meta-analysis. Neurosci Biobehav Rev. 2011;35:573–588. [DOI] [PubMed] [Google Scholar]
- 16. Kunda Z. Social Cognition: Making Sense of People. Cambridge, MA: MIT Press; 1999. [Google Scholar]
- 17. Fiske ST, Taylor SE.. Social cognition. 2nd ed New York, NY: McGraw-Hill Book Company; 1991. [Google Scholar]
- 18. Delvecchio G, Sugranyes G, Frangou S. Evidence of diagnostic specificity in the neural correlates of facial affect processing in bipolar disorder and schizophrenia: a meta-analysis of functional imaging studies. Psychol Med. 2013;43:553–569. [DOI] [PubMed] [Google Scholar]
- 19. Taylor SF, Kang J, Brege IS, Tso IF, Hosanagar A, Johnson TD. Meta-analysis of functional neuroimaging studies of emotion perception and experience in schizophrenia. Biol Psychiatry. 2012;71:136–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Baron-Cohen S, Wheelwright S, Hill J, Raste Y, Plumb I. The “Reading the Mind in the Eyes” Test revised version: a study with normal adults, and adults with Asperger syndrome or high-functioning autism. J Child Psychol Psychiatry. 2001;42:241–251. [PubMed] [Google Scholar]
- 21. Frith CD. The Cognitive Neuropsychology of Schizophrenia. Hove, UK: Lawrence Erlbaum Associates; 1992. [Google Scholar]
- 22. Bora E, Yucel M, Pantelis C. Theory of mind impairment in schizophrenia: meta-analysis. Schizophr Res. 2009;109:1–9. [DOI] [PubMed] [Google Scholar]
- 23. Marin RS. Apathy: a neuropsychiatric syndrome. J Neuropsychiatry Clin Neurosci. 1991;3:243–254. [DOI] [PubMed] [Google Scholar]
- 24. Blanchard JJ, Kring AM, Horan WP, Gur R. Toward the next generation of negative symptom assessments: the collaboration to advance negative symptom assessment in schizophrenia. Schizophr Bull. 2011;37:291–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Insel TR. The challenge of translation in social neuroscience: a review of oxytocin, vasopressin, and affiliative behavior. Neuron. 2010;65:768–779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. MacDonald K, MacDonald TM. The peptide that binds: a systematic review of oxytocin and its prosocial effects in humans. Harv Rev Psychiatry. 2011;18:1–21. [DOI] [PubMed] [Google Scholar]
- 27. Blanchard JJ, Horan WP, Brown SA. Diagnostic differences in social anhedonia: a longitudinal study of schizophrenia and major depressive disorder. J Abnorm Psychol. 2001;110:363–371. [DOI] [PubMed] [Google Scholar]
- 28. Horan WP, Kring AM, Blanchard JJ. Anhedonia in schizophrenia: a review of assessment strategies. Schizophr Bull. 2006;32:259–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Horan WP, Blanchard JJ. Neurocognitive, social, and emotional dysfunction in deficit syndrome schizophrenia. Schizophr Res. 2003;65:125–137. [DOI] [PubMed] [Google Scholar]
- 30. Grant PM, Beck AT. Evaluation sensitivity as a moderator of communication disorder in schizophrenia. Psychol Med. 2009;39:1211–1219. [DOI] [PubMed] [Google Scholar]
- 31. Achim AM, Ouellet R, Lavoie MA, Vallières C, Jackson PL, Roy MA. Impact of social anxiety on social cognition and functioning in patients with recent-onset schizophrenia spectrum disorders. Schizophr Res. 2013;145:75–81. [DOI] [PubMed] [Google Scholar]
- 32. Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med. 2010;7:e1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Steptoe A, Shankar A, Demakakos P, Wardle J. Social isolation, loneliness, and all-cause mortality in older men and women. Proc Natl Acad Sci U S A. 2013;110:5797–5801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Pantell M, Rehkopf D, Jutte D, Syme SL, Balmes J, Adler N. Social isolation: a predictor of mortality comparable to traditional clinical risk factors. Am J Public Health. 2013;103:2056–2062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Holt-Lunstad J, Smith TB, Baker M, Harris T, Stephenson D. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect Psychol Sci. 2015;10:227–237. [DOI] [PubMed] [Google Scholar]
- 36. Cornwell EY, Waite LJ. Social disconnectedness, perceived isolation, and health among older adults. J Health Soc Behav. 2009;50:31–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Uchino BN. Social support and health: a review of physiological processes potentially underlying links to disease outcomes. J Behav Med. 2006;29:377–387. [DOI] [PubMed] [Google Scholar]
- 38. Yang YC, McClintock MK, Kozloski M, Li T. Social isolation and adult mortality: the role of chronic inflammation and sex differences. J Health Soc Behav. 2013;54:183–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Shankar A, McMunn A, Banks J, Steptoe A. Loneliness, social isolation, and behavioral and biological health indicators in older adults. Health Psychol. 2011;30:377–385. [DOI] [PubMed] [Google Scholar]
- 40. Molesworth T, Sheu LK, Cohen S, Gianaros PJ, Verstynen TD. Social network diversity and white matter microstructural integrity in humans. Soc Cogn Affect Neurosci. 2015;10:1169–1176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Valtorta NK, Kanaan M, Gilbody S, Ronzi S, Hanratty B. Loneliness and social isolation as risk factors for coronary heart disease and stroke: systematic review and meta-analysis of longitudinal observational studies. Heart. 2016;102:1009–1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Fratiglioni L, Wang HX, Ericsson K, Maytan M, Winblad B. Influence of social network on occurrence of dementia: a community-based longitudinal study. Lancet. 2000;355:1315–1319. [DOI] [PubMed] [Google Scholar]
- 43. Ertel KA, Glymour MM, Berkman LF. Effects of social integration on preserving memory function in a nationally representative US elderly population. Am J Public Health. 2008;98:1215–1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Shankar A, Hamer M, McMunn A, Steptoe A. Social isolation and loneliness: relationships with cognitive function during 4 years of follow-up in the English Longitudinal Study of Ageing. Psychosom Med. 2013;75:161–170. [DOI] [PubMed] [Google Scholar]
- 45. Weeks DG, Michela JL, Peplau LA, Bragg ME. Relation between loneliness and depression: a structural equation analysis. J Pers Soc Psychol. 1980;39:1238–1244. [DOI] [PubMed] [Google Scholar]
- 46. Cacioppo JT, Hughes ME, Waite LJ, Hawkley LC, Thisted RA. Loneliness as a specific risk factor for depressive symptoms: cross-sectional and longitudinal analyses. Psychol Aging. 2006;21:140–151. [DOI] [PubMed] [Google Scholar]
- 47. Reinhardt JP, Boerner K, Horowitz A. Good to have but not to use: differential impact of perceived and received support on well-being. J Soc Pers Relat. 2006;23:117–129. [Google Scholar]
- 48. Cornwell EY, Walte LJ. Measuring social isolation among older adults using multiple indicators from the NSHAP Study. J Gerontol B Psychol Sci Soc Sci. 2009;64:138–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. McPherson M, Smith-Lovin L, Brashears ME. Social isolation in America: changes in core discussion networks over two decades. Am Sociol Rev. 2006;71:353–375. [Google Scholar]
- 50. Brashears ME. Small networks and high isolation? A reexamination of American discussion networks. Soc Netw. 2011;33:331–341. [Google Scholar]
- 51. Hampton KN, Sessions LF, Her EJ. Core networks, social isolation, and new media: how Internet and mobile phone use is related to network size and diversity. Inf Commun Soc. 2011;14:130–155. [Google Scholar]
- 52. Best P, Manktelow R, Taylor B. Online communication, social media, and adolescent well-being: a systematic narrative review. Child Youth Serv Rev. 2014;41:27–36. [Google Scholar]
- 53. Valkenberg PM, Peter J. Social consequences of the internet for adolscents: a decade of research. Curr Dir Psychol Sci. 2009;18:1–5. [Google Scholar]
- 54. Huang C. Internet use and psychological well-being: a meta-analysis. Cyberpsychol Behav Soc Netw. 2010;13:241–249. [DOI] [PubMed] [Google Scholar]
- 55. Kross E, Verduyn P, Demiralp E et al. Facebook use predicts declines in subjective well-being in young adults. PLoS One 2013;8:e69841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Lin LY, Sidani JE, Shensa A et al. Association between social media use and depression among U.S. young adults. Depress Anxiety. 2016;33:323–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Russell DW. UCLA Loneliness Scale (Version 3): reliability, validity, and factor structure. J Pers Assess. 1996;66:20–40. [DOI] [PubMed] [Google Scholar]
- 58. Allison C, Auyeung B, Baron-Cohen S. Toward brief “Red Flags” for autism screening: The Short Autism Spectrum Quotient and the Short Quantitative Checklist for Autism in toddlers in 1,000 cases and 3,000 controls. J Am Acad Child Adolesc Psychiatry. 2012;51:202.e207–212.e207. [DOI] [PubMed] [Google Scholar]
- 59. Kern RS, Penn DL, Lee J et al. Adapting social neuroscience measures for schizophrenia clinical trials, Part 2: trolling the depths of psychometric properties. Schizophr Bull. 2013;39:1201–1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Reavis EA, Lee J, Wynn JK, Engel SA, Jimenez AM, Green MF. Cortical thickness of functionally defined visual areas in schizophrenia and bipolar disorder. Cereb Cortex. 2017;27:2984–2993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Laursen TM, Nordentoft M, Mortensen PB. Excess early mortality in schizophrenia. Annu Rev Clin Psychol. 2014;10:425–448. [DOI] [PubMed] [Google Scholar]
- 62. Crump C, Winkleby MA, Sundquist K, Sundquist J. Comorbidities and mortality in persons with schizophrenia: a Swedish national cohort study. Am J Psychiatry. 2013;170:324–333. [DOI] [PubMed] [Google Scholar]
- 63. Keinanen J, Mantere O, Markkula N et al. Mortality in people with psychotic disorders in Finland: a population-based 13-year follow-up study. Schizophr Res. 2017. doi: 10.1016/j.schres.2017.04.048 [DOI] [PubMed] [Google Scholar]
- 64. Horan WP, Kern RS, Tripp C et al. Efficacy and specificity of social cognitive skills training for outpatients with psychotic disorders. J Psychiatr Res. 2011;45:1113–1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Penn DL, Roberts DL, Combs D, Sterne A. Best practices: the development of the Social Cognition and Interaction Training program for schizophrenia spectrum disorders. Psychiatr Serv. 2007;58:449–451. [DOI] [PubMed] [Google Scholar]
- 66. Turkington D, Munetz M, Pelton J et al. High-yield cognitive behavioral techniques for psychosis delivered by case managers to their clients with persistent psychotic symptoms: an exploratory trial. J Nerv Ment Dis. 2014;202:30–34. [DOI] [PubMed] [Google Scholar]
- 67. Granholm E, Holden J, Link PC, McQuaid JR, Jeste DV. Randomized controlled trial of cognitive behavioral social skills training for older consumers with schizophrenia: defeatist performance attitudes and functional outcome. Am J Geriatr Psychiatry. 2013;21:251–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Wykes T, Huddy V, Cellard C, McGurk SR, Czobor P. A meta-analysis of cognitive remediation for schizophrenia: methodology and effect sizes. Am J Psychiatry. 2011;168:472–485. [DOI] [PubMed] [Google Scholar]
- 69. Radke S, Roelofs K, de Bruijn ER. Acting on anger: social anxiety modulates approach-avoidance tendencies after oxytocin administration. Psychol Sci. 2013;24:1573–1578. [DOI] [PubMed] [Google Scholar]
- 70. Davis MC, Green MF, Lee J et al. Oxytocin-augmented social cognitive skills training in schizophrenia. Neuropsychopharmacology. 2014;39:2070–2077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Rassovsky Y, Dunn W, Wynn J et al. The effect of transcranial direct current stimulation on social cognition in schizophrenia: a preliminary study. Schizophr Res. 2015;165:171–174. [DOI] [PubMed] [Google Scholar]
- 72. Marder SR, Alphs L, Anghelescu IG et al. Issues and perspectives in designing clinical trials for negative symptoms in schizophrenia. Schizophr Res. 2013;150:328–333. [DOI] [PubMed] [Google Scholar]
- 73. Davis MC, Lee J, Horan WP et al. Effects of single dose intranasal oxytocin on social cognition in schizophrenia. Schizophr Res. 2013;147:393–397. [DOI] [PubMed] [Google Scholar]
- 74. Buchanan RW, Davis M, Goff D et al. A summary of the FDA-NIMH-MATRICS workshop on clinical trial design for neurocognitive drugs for schizophrenia. Schizophr Bull. 2005;31:5–19. [DOI] [PubMed] [Google Scholar]
- 75. Barrantes-Vidal N, Grant P, Kwapil TR. The role of schizotypy in the study of the etiology of schizophrenia spectrum disorders. Schizophr Bull. 2015;41(suppl 2):S408–S416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Kwapil TR. Social anhedonia as a predictor of the development of schizophrenia-spectrum disorders. J Abnorm Psychol. 1998;107:558–565. [DOI] [PubMed] [Google Scholar]
- 77. Llerena K, Park SG, Couture SM, Blanchard JJ. Social anhedonia and affiliation: examining behavior and subjective reactions within a social interaction. Psychiatry Res. 2012;200:679–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Santini ZI, Fiori KL, Feeney J, Tyrovolas S, Haro JM, Koyanagi A. Social relationships, loneliness, and mental health among older men and women in Ireland: a prospective community-based study. J Affect Disord. 2016;204:59–69. [DOI] [PubMed] [Google Scholar]
- 79. Thonon B, Laroi F. What predicts stigmatization about schizophrenia? Results from a general population survey examining its underlying cognitive, affective, and behavioral factors. Psychosis. 2017;9:99–109. [Google Scholar]
- 80. Walker E, Lewine RJ. Prediction of adult-onset schizophrenia from childhood home movies of the patients. Am J Psychiatry. 1990;147:1052–1056. [DOI] [PubMed] [Google Scholar]
- 81. Walker EF, Grimes KE, Davis DM, Smith AJ. Childhood precursors of schizophrenia: facial expressions of emotion. Am J Psychiatry .1993;150:1654–1660. [DOI] [PubMed] [Google Scholar]
- 82. Cornblatt BA, Carrión RE, Addington J et al. Risk factors for psychosis: impaired social and role functioning. Schizophr Bull. 2012;38:1247–1257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Kagan J, Reznick JS, Snidman N. Biological bases of childhood shyness. Science. 1988;240:167–171. [DOI] [PubMed] [Google Scholar]
- 84. Schwartz CE, Snidman N, Kagan J. Adolescent social anxiety as an outcome of inhibited temperament in childhood. J Am Acad Child Adolesc Psychiatry. 1999;38:1008–1015. [DOI] [PubMed] [Google Scholar]