Summary
It is commonly assumed that a person identifying that they are ‘overweight’ is an important prerequisite to successful weight management. However, there has been no systematic evaluation of evidence supporting this proposition. The aim of the present research was to systematically review evidence on the relationship between perceived overweight and (i) weight loss attempts, (ii) weight control strategies (healthy and unhealthy), (iii) weight‐related behaviours (physical activity and eating habits), (iv) disordered eating and (v) weight change. We synthesized evidence from 78 eligible studies and evaluated evidence linking perceived overweight with outcome variables separately according to the gender, age and objective weight status of study participants. Results indicated that perceived overweight was associated with an increased likelihood of attempting weight loss and with healthy and unhealthy weight control strategies in some participant groups. However, perceived overweight was not reliably associated with physical activity or healthy eating and was associated with greater disordered eating in some groups. Rather than being associated with improved weight management, there was consistent evidence that perceived overweight was predictive of increased weight gain over time. Individuals who perceive their weight status as overweight are more likely to report attempting weight loss but over time gain more weight.
Keywords: Perceived overweight, weight gain, weight management, weight misperception
There is often a mismatch between the weight status a person believes they have and their objective weight status 1. Some people with a ‘normal’ or healthy weight misperceive their weight status as ‘overweight’. More prevalent, however, is the tendency for individuals with overweight or obesity to underestimate their weight status and fail to identify their weight as being ‘overweight’ 2. A recent analysis of data from a nationally representative survey of UK adults revealed that approximately one‐third of women and one half of men with overweight failed to identify themselves as such 3, and similar rates have been reported in adolescents 4. The prevailing attitude underlying a number of public health approaches is that individuals with overweight and obesity must be made aware of their weight status to be better able to manage their weight. For example, physicians in the UK and USA are encouraged to monitor and provide information to patients about their weight status 5, 6. In the UK, the national child measurement programme is in place to monitor and notify parents of their child's weight 7, and similar school health screening programmes have been launched in many US states 8.
In support of the traditional view that ‘ignorance is damaging’ in relation to self‐perception of being overweight, a considerable body of research has shown that both adults and children who perceive themselves as overweight are more likely to attempt to lose weight than those who do not 9, 10. However, the evidence for how perceived overweight relates to weight‐related lifestyle behaviours is mixed. While some studies have shown that individuals who perceive their weight status as overweight are more likely to report using exercise as a weight control strategy than those who do not perceive themselves as overweight 11, others have shown that perceived overweight is associated with lower physical activity 12, and some find no relation 13. Likewise, perceived overweight has been associated with self‐reported ‘eating healthily’ to lose weight 11, but in terms of actual behaviour, some studies show that individuals who perceive their weight status as overweight are more likely to have poor eating habits such as failing to consume adequate fruits and vegetables 14, 15, whereas other research has shown that unhealthy eating habits like fast food consumption and inadequate fruit and vegetable intake are unrelated to whether or not someone perceives themselves to be overweight 12.
Conversely, it is also possible that ‘knowing hurts’ in relation to perceiving oneself as overweight 16. Overweight and obesity are widely stigmatized, and perceiving oneself as belonging to a stigmatized group could bring psychological distress and associated negative health consequences. Individuals who identify as overweight, for example, experience higher levels of body dissatisfaction 17 and may thus have a more extreme desire to lose weight than individuals who do not identify as overweight. Consistent with this argument, perceived overweight has been associated with extreme weight management strategies such as vomiting and laxative use 18. Such behaviours can compromise health and lead to disordered eating 19, which may or may not be associated with perceived overweight. In addition, weight stigma can undermine self‐regulation in people who identify as overweight, which can impair the healthy behaviours that facilitate effective weight management 20. The distress associated with perceiving oneself as belonging to a stigmatized group may encourage the adoption of maladaptive coping strategies such as stress‐induced eating 21. Finally, longitudinal studies of adolescents and adults have demonstrated that perceived overweight is associated with greater weight gain in individuals with objective normal weight and with overweight 22, 23. This evidence suggests that perceived overweight may not be associated with better weight management in the long term.
Given the mixed evidence regarding the relationship between perceived overweight and weight management, a comprehensive review of the evidence is warranted. The purpose of the present research was to systematically review the evidence for the association between perceived overweight and weight‐related behaviours and outcomes including (i) weight loss attempts, (ii) healthy and unhealthy weight control strategies, (iii) weight‐related behaviours (including healthy eating habits and physical activity), (iv) disordered eating and (v) weight gain. Because perceived overweight could be more strongly associated with weight‐related behaviours in some population groups than others, we examined the overall evidence and evidence within participant subgroups according to gender, age and objective weight status.
Methods
This review was guided by the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses 24.
Eligibility criteria
Studies eligible for inclusion were those which (a) reported a quantitative analysis of the association between participants' perceived weight status (enabling a comparison between perceived overweight and perceived normal/healthy weight or ‘not overweight’) and at least one of the following variables: (i) intention or attempt to control or lose weight, (ii) weight control strategies used: ‘healthy’ (including eating less or different foods, or increasing physical activity to lose weight) or ‘unhealthy’ (including use of diet medication without medical advice, purging or fasting to lose weight), (iii) weight‐related behaviours: healthy physical activity or healthy eating habits (including intake of fruits and vegetables, snack or fast foods and energy intake), (iv) disordered eating (including bulimic symptoms, disordered eating attitudes or binge eating), or (v) weight change; (b) were published in peer‐reviewed articles from 1991 onwards, as we believed results prior to the last 25 years may not be representative, and the majority of the research we were aware of was conducted during this period; and (c) were available in English. Studies were excluded if they sampled a clinical (e.g. patients with cystic fibrosis) or non‐general population (e.g. pregnant women only), if they assessed perceptions of weight status in a way that made it unclear whether participants identified as being overweight (e.g. pictorial scales without weight status labels), if perceived overweight was an outcome variable, or if analyses of interest did not control or stratify by objective body mass index (BMI) or weight status (to minimize the potential confounding effect of objective weight). For further information on search strategy and eligibility, see Appendix A (supporting information).
Healthy weight control strategies (including using diet or exercise to lose weight) were distinguished from weight‐related behaviours (including healthy eating habits and physical activity). Specifically, the former typically refers to whether or not a given strategy was used in order to achieve weight loss, whereas the latter refers to the participant's enactment of behaviours (e.g. frequency of fruit and vegetable consumption and hours of physical activity per week) known to be related to body weight but which may/may not be completed for the purpose of weight loss. Unhealthy weight control strategies (e.g. use of diet medication, purging or fasting to lose weight) were distinguished from disordered eating in that the unhealthy weight control strategies were assessed by asking participants to report the methods they used to try to lose weight without reference to problematic patterns of excessive eating behaviour (e.g. binge eating and loss of control over eating) or weight‐related attitudes (e.g. preoccupation with weight). Disordered eating, on the other hand, was usually assessed with validated questionnaires designed to assess clinical diagnostic criteria for disordered eating habits.
Information sources and search strategy
Electronic searches were conducted using PubMed, PsycInfo and Cumulative Index to Nursing and Allied Health Literature databases in June 2016. A set of search terms was devised to identify articles concerning perceived weight status and outcome variables (Table S1). Initial sensitivity of the search terms was assessed by confirming that they successfully retrieved a set of core references identified by the authors prior to beginning the review 10, 25, 26, 27, 28, 29, 30. Additionally, the reference lists of eligible articles were manually searched for relevant articles, and each author was responsible for suggesting additional articles not identified by the electronic and reference list searches. To ensure adequate coverage of recent studies, supplementary database searches were conducted in July 2017 (Appendix A, supporting information).
Study selection
The titles and abstracts of electronic search results were independently screened by two researchers (A. H. and C. T.) for eligibility for full‐text screening, and discrepancies were resolved by discussion. The two researchers then independently screened the full text of those articles for inclusion. Initial discrepancies in eligibility decisions at the full‐text screening phase were resolved by the two researchers and confirmed by a third researcher (E. R.) when a decision could not be reached. Initially, the coders agreed on selection decisions for 97.5% of title and abstracts (indicating a high level of agreement, κ = .95) and 87.8% of full‐text articles (indicating substantial agreement, κ = 0.76).
Data extraction
Data extraction included information about (i) publication features (title, authors, year of publication and journal), (ii) study methods (design, country of origin, sampling method and measurement of perceived weight status and correlates), (iii) sample characteristics (sample size and age, gender and weight status distributions) and (iv) findings (relation between perceived overweight and relevant outcome).
The outcome category ‘weight‐related behaviours: healthy eating habits’ included findings on consumption of both healthy (e.g. fruit and vegetable) and unhealthy foods (e.g. fast foods and sugar sweetened beverages). The outcome category ‘weight‐related behaviours: healthy physical activity’ included findings on both physical activity (e.g. hours of physical activity) and sedentary behaviour (e.g. hours of screen time). Weight‐related behaviour findings were coded as positive when they demonstrated an association between perceived overweight and healthier consumption (e.g. greater consumption of fruits and vegetables or lower consumption of fast food) or healthier activity levels (e.g. more frequent physical activity or lower sedentariness). In the outcome category ‘weight change’, a positive relationship was indicative of a finding of a longitudinal association between perceived overweight and weight gain or onset of overweight or obesity.
For studies that compared ‘perceived overweight’ with ‘perceived normal weight’ and with ‘perceived underweight’ in separate analyses, only findings for the comparison between perceived overweight and normal weight were extracted; and for studies that collapsed ‘perceived underweight’ and ‘perceived normal weight’ categories into ‘not perceived overweight’ for analysis, findings comparing ‘perceived overweight’ and ‘not perceived overweight’ were extracted. For studies using perceived weight as a continuous predictor, findings were treated as indicating an association between ‘perceived overweight’ and the outcome variable. If an article included multiple studies, findings from each study were extracted separately. If a study reported multiple findings for the same outcome in different subsamples (e.g. stratified by gender or objective weight status), those findings were extracted separately. For each study, results from the most appropriately adjusted statistical model (i.e. adjusted for variables known to be associated with weight perception such as gender and socioeconomic status) were extracted. Data were extracted from each eligible study by one of two authors (A. H. and I. K.), and each author's extraction was then cross‐checked by the other author.
Quality assessment
The methodological quality of the selected studies was assessed against a list of established criteria adapted from checklists for cross‐sectional 31 and longitudinal 32 observational studies (Table 1). For each item, each study was assigned a score of ‘yes’ (indicating the study meets the quality criterion), ‘no’ (potential bias indicated) or ‘not applicable’. A total quality score was calculated for each study by dividing the number of positively scored criteria by the total number of applicable criteria. Two authors (A. H. and I. K.) independently scored a subset of 20 studies to pilot the quality assessment tool. Inter‐rater reliability for each criterion was acceptable to high (κ = 0.69–1.00). The methodological quality of the remaining studies was coded by one of two authors (A. H. and I. K.).
Table 1.
Criteria for assessment of the methodological quality of included studies
| Criteria | Percentage of studies meeting criterion† |
|---|---|
| Study population and participation | |
| 1. Adequate description of study population recruitment methods, period of recruitment and place of recruitment | 95 |
| 2. Sample representative of population of interest | 51 |
| 3. Participation/response rate reported | 81 |
| 4. Study attrition: reported whether loss to follow‐up associated with key characteristics ‡ | 18 |
| 5. Provision of the exact number of participants at each follow‐up measurement ‡ | 71 |
| 6. Provision of exact information on follow‐up duration ‡ | 94 |
| Data collection | |
| 7. Adequate description of methods of data collection (i.e. tools, processes and setting and/or geographic location) | 97 |
| 8. Adequate measurement of height and weight (anthropomorphic measurements by trained personnel, not self‐report) | 45 |
| 9. Sample size based on a priori power calculation (or authors report a priori consideration of sample size), if N < 1,000 | 13 |
| Data analysis | |
| 10. Adequate description of inclusion and exclusion criteria for analysed sample, and reporting of number of people meeting inclusion and exclusion for analysis | 81 |
| 11. Adequate description of analysed sample (number of participants, age, gender and BMI) (positively scored if adequate information provided for all items) | 78 |
| 12. Analysed sample adequate (n > 100 per weight perception group) in size? | 79 |
| 13. Adjusts for BMI (continuous) in analysis | 36 |
| 14. Adjusts or stratifies analyses by demographic characteristics potentially correlated with weight perception (gender, socioeconomic status indicator and ethnicity) (positively scored if controlled for each characteristic) | 40 |
Percentage of studies scored as meeting each quality criterion, excluding studies for which item was not applicable.
Applicable to longitudinal studies only.
BMI, body mass index.
Evidence synthesis
Because of heterogeneity in analytical designs (e.g. reporting odds ratios vs. regression coefficients) and assessment of outcomes (e.g. sedentary vs. physical activity, weight gain vs. onset of obesity and unhealthy snack vs. fruit and vegetable intake), a quantitative meta‐analysis was not undertaken. Instead, we conducted a qualitative evidence synthesis as in previous reviews of observational studies of health and weight‐related behaviours 33, 34. The evidence synthesis accounted for the number of studies, the methodological quality of included studies and the consistency of findings. Cross‐sectional and longitudinal evidence was summarized for each outcome category separately. Because of stratification by participant characteristics being common in studies and the potential for study findings to be dependent on sampled population, we deemed it most appropriate to evaluate evidence separately by gender, age group (‘children, adolescents, young adults’ and ‘adults’) and objective weight status (‘normal weight’, ‘overweight, obese’ and ‘no weight status criteria’), as well as making an overall evaluation of evidence for each outcome. Where a study reported a non‐significant interaction between perceived overweight and gender (or objective weight) alongside a significant relation between perceived overweight and an outcome variable, the finding was replicated in the evidence table for both male and female participants (or both participants with overweight and normal weight), as this was deemed as providing evidence that the association observed was not dependent on participant gender (or weight status). Where a study reported multiple relations in different subsamples for the same outcome, those associations were coded separately in the evidence table but contributed only one ‘piece’ of evidence towards overall grading (e.g. where a study contributed evidence for one outcome in male and female adolescent subgroups separately, the two findings only counted once towards overall evidence grading). Similarly, when multiple studies analysed data from the same data source, those studies contributed only one ‘piece’ of evidence towards the overall evidence grading. We used the following a priori criteria based on those used in previous systematic reviews 33, 34, 35 to grade level of evidence both overall and within participant subgroups:
Strong evidence: consistent findings in multiple (≥2) high‐quality studies (if low‐quality studies are available, results from high‐quality and low‐quality studies must be consistent to provide ‘strong’ evidence; otherwise, evidence is downgraded to ‘moderate’).
Moderate evidence: consistent findings in one high‐quality study and at least one low‐quality study; consistent findings in multiple (≥2) low‐quality studies; or consistent findings in multiple (>2) high‐quality studies, but inconsistent findings when high‐quality and low‐quality studies pooled.
Insufficient evidence: only one study available or inconsistent findings in multiple (≥2) studies.
Evidence of no association: consistent findings for no relation in at least one high‐quality study and at least one low‐quality study; consistent findings for no relation in multiple (≥2) low‐quality studies; or consistent findings for no relation in multiple (>2) high‐quality studies, but inconsistent findings when high‐quality and low‐quality studies pooled.
Findings were considered consistent if at least 75% of results were in the same direction and statistically significant.
Results
Initial database searches identified 10,398 unique records, and an additional 41 articles were identified by authors, from the reference lists of eligible articles or from supplementary searches. Full‐text review of 366 articles was completed, and 74 articles 9, 10, 11, 12, 13, 14, 15, 18, 21, 22, 23, 30, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72, 73, 74, 75, 76, 77, 78, 79, 80, 81, 82, 83, 84, 85, 86, 87, 88, 89, 90, 91, 92, 93, 94, 95, 96, 97 (indicated with asterisks in reference list) that described 78 studies were included in the review (Fig. 1).
Figure 1.
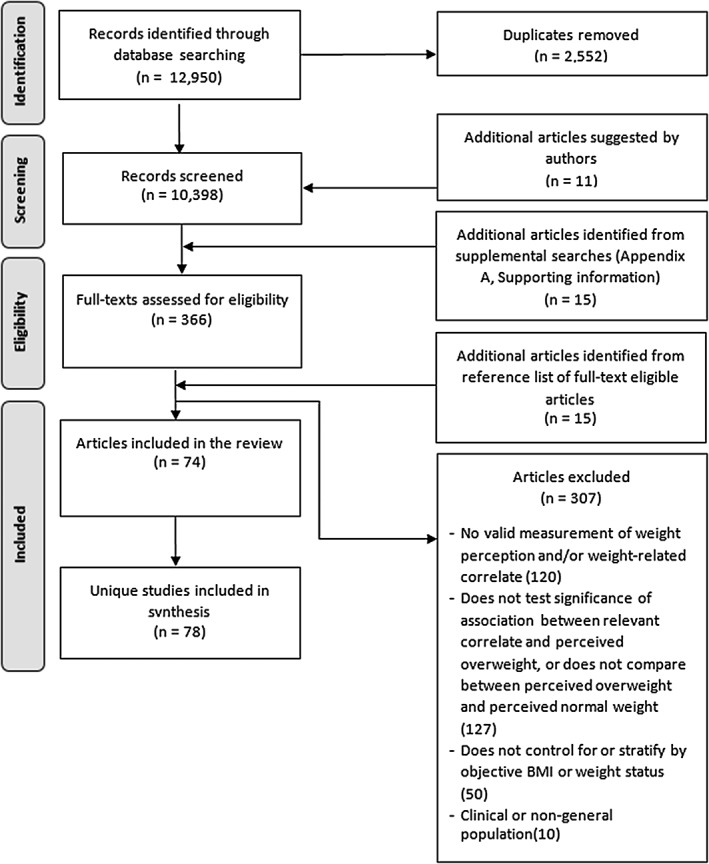
Preferred Reporting Items for Systematic Reviews and Meta‐Analyses flow diagram of study selection, inclusion and exclusion of studies. BMI, body mass index.
Study and sample characteristics
Table S2a describes the characteristics of each of the 78 included studies. The majority of the studies were cross‐sectional 62, and the remaining 16 reported longitudinal analyses (follow‐up periods ranging from 66 days to 22 years). The number of published studies on weight perception and weight management increased in recent years, with the majority of studies included in the review being published between 2011 and 2017 (62%), the remainder being published between 2004 and 2010 27, and a small number before 2003 3. There was a trend towards an increasing proportion of longitudinal studies over time: 27% of studies published between 2011 and 2017 included a longitudinal analysis of the relation between perceived overweight and weight management, compared with 11.1% of studies published between 2004 and 2010. Most studies (57.7%) were conducted in the USA 45, with the remainder of studies conducted in Asia 12, Europe 9 and Australia or New Zealand 4. Sample sizes ranged from 106 to 104,199. The majority (83.3%) of studies included both male and female participants. Most study samples did not include participants of a specific weight status (79.5%), but a small number of findings were reported from participants with overweight or obesity 11 or normal weight 5. Half of included studies were conducted on adolescent samples or a combination of children and adolescents, with the remainder on adults or a combination of adults and other ages 30, or only young adults (aged 18–25) 9.
Measurement characteristics
All of the studies included in the review measured perceived weight by asking participants to describe their current weight on a rating scale. In most studies (76.9%, Table S2b), the response format consisted of the options: ‘very underweight’, ‘slightly underweight’, ‘about right’ (or variants ‘acceptable’, ‘normal’ and ‘average’), ‘slightly overweight’ (or ‘somewhat overweight’) and ‘very overweight’ (or ‘obese’). The responses ‘slightly’ or ‘very overweight’ were categorized as ‘perceived overweight’ in most studies.
The most frequently examined outcome variable analysed in the included studies was weight loss intention or attempt. In the 24 studies that analysed this variable, most administered a single self‐report item (e.g. ‘what are you currently trying to do about your weight?’). Twenty‐eight studies examined weight control strategies: 19 studies examined the use of ‘healthy’ weight control strategies (i.e. health‐promoting weight loss strategies recommended by national public health bodies, such as eating less or different foods [also called ‘moderate dieting’] or increasing physical activity to lose weight), and 20 studies examined the use of ‘unhealthy’ weight control strategies (i.e. also called ‘extreme’ weight control behaviours: potentially harmful strategies such as using diet pills without medical advice or vomiting to lose weight). These outcomes were assessed with self‐report measures that asked participants to indicate the strategies they had recently used (i.e. in the past 30 days or 12 months) or were currently using, to try to lose or maintain weight, or the frequency with which they used these strategies. Evidence on weight‐related behaviours was provided by 14 studies. Specifically, 13 studies examined physical activity, and 11 studies examined healthy eating habits. In some studies, physical activity was assessed using validated self‐report scales (e.g. Physical Activity Questionnaire for Children), and others assessed physical activity and sedentariness using single self‐report items (e.g. ‘In the past week, on how many days were you physically active for at least 60 minutes?’). One study objectively assessed physical activity using accelerometers. Outcomes were either analysed continuously (e.g. number of physically active days in past week) or dichotomized into meeting or not meeting recommended activity levels, but the cut‐off points for determining ‘recommended’ activity levels varied. The majority of the studies on healthy eating habits assessed participants' self‐reported consumption frequency of various foods (e.g. fruits and vegetables, fast food, etc.), and one study assessed energy intake from 24‐h intake recall. Outcomes were either analysed as continuous variables or dichotomized into meeting or not meeting daily recommended intake (e.g. of fruits and vegetables), but cut‐off points for determining ‘recommended’ intake varied. Twelve studies examined disordered eating behaviour or attitudes, which were assessed using single self‐report items or validated clinical scales (e.g. Eating Disorders Inventory). Fourteen prospective longitudinal studies provided evidence on weight change. In all studies, weight change was based on anthropomorphic measurements by a researcher or health professional or self‐reported height and weight and was either analysed as a change in weight (either absolute or as a percentage of baseline weight), change in BMI or the onset of overweight or obesity.
Methodological quality
We deemed the methodological quality of the individual studies included in the review to be moderate on average (Table S3). The majority of included studies (52.6%) did not meet the criteria for high‐quality methodology, and on average, the studies were assigned a quality score of 66%. The most commonly met indicators of quality (Table 1) were the provision of an adequate description of recruitment (95%) and data collection methods (97%), and for longitudinal studies, a description of the follow‐up duration (94%). The most prevalent potential sources of bias were a lack of evidence concerning appropriateness of sample size (e.g. power calculation) in studies with N < 1,000 (only 13% of applicable studies met this criterion), and for longitudinal studies, the lack of demonstration that loss to follow‐up was not associated with key characteristics (only 18% of applicable studies met this criterion). Sixty per cent of studies did not adjust for variables (e.g.,socioeconomic status) known to be associated with weight perception 98, and over half of studies assessed BMI using self‐report rather than anthropomorphic measurements of height and weight (55%).
Relation between perceived overweight and weight‐related correlates
A summary of the evidence for the association between perceived overweight and weight‐related correlates is presented in Tables 2a (cross‐sectional) and 2b (longitudinal). Evidence is stratified by outcome category and subsample (gender and age group), and weight status of samples are indicated. Tables S4a and S4b present the evidence synthesis with references.
Table 2a.
Evidence synthesis by outcome category and subsample (cross‐sectional studies)
| Male only sample | Female only sample | Genders combined sample | ||
|---|---|---|---|---|
| (a) Weight loss attempt or intention | ||||
| Children/adolescents/young adults only |
3 hi qual. studies (NW) ae: ↑ 4 hi qual. studies (OW/OB)abe:↑ 2 lo qual. studies (OW/OB)cd:↑ 2 lo qual. studies ef: ↑ |
1 hi qual. study: ↑ 3 hi qual. studies (NW) ae: ↑ 4 hi qual. studies (OW/OB)aeg:↑ 2 lo qual. studies (OW/OB)cd:↑ 3 lo qual. studies ef: ↑ |
1 hi qual. study (NW)a: ↑ 2 hi qual. studies (OW/OB)ab:↑ 2 hi qual. studies: ↑ 1 lo qual. study (NW): ↑ 1 lo qual. study (non‐OW): ↑ 1 lo qual. study: ↑ |
Overall: strong evidence of ↑ association
NW: strong evidence of ↑ association OW/OB: strong evidence of ↑ association No weight status criteria: strong evidence of ↑ association |
| Strong evidence of ↑ association | Strong evidence of ↑ association | Strong evidence of ↑ association | ||
| Adults |
2 hi qual. studies (OW/OB)gh:↑ 2 hi qual. studies hi: ↑ |
2 hi qual. studies (OW/OB)gh:↑ 2 hi qual. studies hi: ↑ |
1 hi qual. study (non‐OB): ↑ 1 hi qual. study (OW/OB): ↑ 2 lo qual. studies (OW/OB):↑ 1 lo qual. study: ↑ |
|
| Strong evidence of ↑ association | Strong evidence of ↑ association | Strong evidence of ↑ association | ||
| (b) Weight control strategies: healthy | ||||
| Children/adolescents/young adults only |
1 hi qual. study (non‐OW)a: ↑ 2 hi qual. studies (OW)ae: ↑ 1 hi qual. study (NW)e: ↑ 1 hi qual. study b: ↔ 1 lo qual. study (OW) c: ↑ 1 lo qual. study (OB) d: ↑↔ 2 lo qual. studies ef: ↑ |
1 hi qual. study (non‐OW)a: ↑ 2 hi qual. studies (OW)ae: ↑ 1 hi qual. study (NW)e: ↑ 2 hi qual. studies b: ↔ 1 lo qual. study (OW)c: ↑ 1 lo qual. study (OB)d: ↑↔ 4 lo qual. studies ef: ↑ 1 lo qual. study: ↑↔ |
2 hi qual. studies (NW)e: ↑ 1 hi qual. study (OW): ↑ 1 lo qual. study (NW): ↑ 1 lo qual. study: ↓ |
Overall: moderate evidence of ↑ association due to mixed findings
NW: strong evidence of ↑ association OW/OB: moderate evidence of ↑ association due to mixed findings No weight status criteria: evidence of no association |
| Insufficient evidence due to mixed findings | Insufficient evidence due to mixed findings | Strong evidence of ↑ association | ||
| Adults | 1 hi qual. study (OW/OB)g: ↑ | 1 hi qual. study (OW/OB)g: ↑ | 1 lo qual. study (OB): ↔ | |
| Insufficient evidence | Insufficient evidence | Insufficient evidence | ||
| (c) Weight control strategies: unhealthy | ||||
| Children/adolescents/young adults only |
2 hi qual. studies (NW)af: ↑ 1 hi qual. study (OW)afg: ↔ 1 hi qual. study (OW/OB)a: ↔ 1 hi qual. study (OW/OB)agl:↑↔↔ 1 hi qual. study (OW/OB)b: ↑ 1 hi qual. study: ↑ 1 hi qual. study c: ↑↔ 1 lo qual. study (UW/NW)d: ↑ 2 lo qual. studies (OW)ef: ↑ 1 lo qual. study (OW/OB)g: ↔ 1 lo qual. study (OB)h: ↓ 2 lo qual. studies ij: ↔ 1 lo qual. study (NW)f: ↑ 2 lo qual. studies kl: ↑ |
2 hi qual. studies (NW)af: ↑ 3 hi qual. studies (OW/OB)abgl:↑ 1 hi qual. study (OW)afg: ↑↔ 1 hi qual. study c: ↑ 1 lo qual. study (UW/NW)d: ↑ 1 lo qual. study (OW)e: ↑ 1 lo qual. study (OW)f: ↔ 1 lo qual. study (OB)h: ↓ 1 lo qual. study (OW/OB)g: ↔ 4 lo qual. studies kjl: ↑ 1 lo qual. study i: ↔ 1 lo qual. study: ↓↔ 1 lo qual. study (NW)f: ↑ |
1 hi qual. study (NW): ↑ 1 hi qual. study (OW/OB)agl:↑↑↔ 1 hi qual. study b: ↑ 2 lo qual. studies (NW)f: ↑ 1 lo qual. study (OW): ↔ 1 lo qual. study (OB): ↔ 1 lo qual. study l: ↑ |
Overall: moderate evidence of ↑ association due to mixed findings
NW: strong evidence of ↑ association OW/OB: insufficient evidence due to mixed findings No weight status criteria: strong evidence of ↑ association |
| Moderate evidence of ↑ association due to mixed findings | Moderate evidence of ↑ association due to mixed findings | Moderate evidence of ↑ association due to mixed findings | ||
| Adults | 1 hi qual. study: ↑ | |||
| None | Insufficient evidence | None | ||
| (d) Weight‐related behaviour: healthy physical activity | ||||
| Children/adolescents/young adults only |
2 hi qual. studies (NW) ac: ↓ 1 hi qual. study (OW)c: ↓ 2 hi qual. studies (OW/OB)ab:↓ 1 lo qual. study (OW/OB)c: ↓ 1 lo qual. study (OB): ↔↓d |
1 hi qual. study (NW): ↓↔a
1 hi qual. study (NW)c: ↔ 1 hi qual. study (OW)c: ↔ 1 hi qual. study (OW/OB)a:↓↔ 1 hi qual. study (OW/OB)b: ↓ 1 hi qual. study: ↔ 1 lo qual. study (OW/OB)c:↔ 1 lo qual. study (OB)d: ↓ |
1 hi qual. study (OW/OB):↓b
1 hi qual. study (OW): ↔↓ 1 hi qual. study (NW): ↔↑ 1 lo qual. study (NW): ↓ 1 lo qual. study (OB): ↓ 2 lo qual. studies: ↓ |
Overall: insufficient evidence due to mixed findings
NW: insufficient evidence due to mixed findings OW/OB: insufficient evidence due to mixed findings No weight status criteria: insufficient evidence due to mixed findings |
| Strong evidence of ↓ association | Insufficient evidence due to mixed findings | Moderate evidence of ↓ association due to mixed findings | ||
| Adults |
1 hi qual. study (OW/OB)e:↔ 1 lo qual. study (NW)f: ↓ 1 lo qual. study (OW/ OB)f: ↓ |
1 hi qual. study (OW/OB)e: ↓ 1 lo qual. study (NW)f: ↔ 1 lo qual. study (OW/OB)f:↔ |
||
| Insufficient evidence due to mixed findings | Insufficient evidence due to mixed findings | None | ||
| (e) Weight‐related behaviour: healthy eating habits | ||||
| Children/adolescents/young adults only |
1 hi qual. study (OW/OB)a:↔ 1 hi qual. study (OW)b: ↔↓↓ 1 hi qual. study (NW)b: ↔ 2 lo qual. studies (OW/OB)bc:↔ 1 lo qual. study (NW)c: ↔ 1 lo qual. study d: ↔ |
1 hi qual. studyb: ↑↓↔ 1 hi qual. study (NW)b: ↔ 1 hi qual. study (OW)b: ↔ 1 hi qual. study(OW/OB)a:↔ 1 lo qual. study (NW)c: ↔ 2 lo qual. studies (OW/OB)bc:↔ 1 lo qual. study: ↔ |
1 hi qual. study (OW/OB)a:↔ 1 hi qual. study (OW): ↔ 1 hi qual. study (NW): ↔ 1 lo qual. study (NW): ↓ 1 lo qual. study (OB): ↓ |
Overall: evidence of no association
NW: evidence of no association OW/OB: evidence of no association No weight status criteria: insufficient evidence due to mixed findings |
| Evidence of no association | Evidence of no association | Evidence of no association | ||
| Adults | 1 hi qual. study (OW/OB)e:↔ | 1 hi qual. study (OW/OB)e:↔ | ||
| Insufficient evidence | Insufficient evidence | None | ||
| (f) Disordered eating | ||||
| Children/ adolescents/young adults only | 1 hi qual. study (OW/OB)a: ↔ |
1 hi qual. study (OW/OB)a: ↑ 3 lo qual. studies: ↑ 1 lo qual. study: ↔ |
1 hi qual. study (NW): ↑b
1 hi qual. study (OW): ↑b 2 lo qual. studies c: ↑ 1 lo qual. study (OW)c: ↑ 1 lo qual. study (NW)c: ↑ 1 lo qual. study: ↑↔ |
Overall: strong evidence of ↑ association
NW: moderate evidence of ↑ association OW/OB: strong evidence of ↑ association No weight status criteria: moderate evidence of ↑ association |
| Insufficient evidence | Moderate evidence of ↑ association | Strong evidence of ↑ association | ||
| Adults | 1 lo qual. study d: ↔ | 1 lo qual. study d: ↑ | 1 lo qual. study (OB): ↑ | |
| Insufficient evidence | Insufficient evidence | Insufficient evidence | ||
↑ indicates a significant positive association, ↓ indicates a significant negative association, and ↔ indicates no significant association between perceived overweight and outcome. Results with common superscript within evidence categories are from overlapping samples. For longitudinal studies, samples are classified into subgroups by baseline age and weight characteristics. Objective weight status categories: NW, normal weight; OB, obese; OW, overweight; UW, underweight. For individual study references, see Tables S4a and S4b.
hi qual., high‐quality; lo qual., low‐quality; POW, perceived overweight.
Table 2b.
Evidence synthesis by outcome category and subsample (longitudinal studies)
| Male only sample | Female only sample | Genders combined sample | ||
|---|---|---|---|---|
| (a) Weight control strategies: unhealthy | ||||
| Children/adolescents/young adults only | 1 lo qual. study: ↔ |
Overall: insufficient evidence
NW: none OW/OB: none No weight status criteria: insufficient evidence |
||
| None | Insufficient evidence | None | ||
| Adults | None | None | None | |
| (b) Disordered eating | ||||
| Children/adolescents/young adults only | 1 lo qual. study: ↔ |
Overall: insufficient evidence
NW: none OW/OB: none. No weight status criteria: insufficient evidence |
||
| None | Insufficient evidence | None | ||
| Adults | ||||
| None | None | None | ||
| (c) Weight change (↑ indicates weight gain or onset of overweight or obesity) | ||||
| Children/adolescents/young adults only |
2 hi qual. studies (NW)ab: ↑ 1 hi qual. study (OW)a: ↑ 1 hi qual. study (OW/OB)b:↑ 1 lo qual. study (NW)a: ↔ 1 lo qual. study (UW/NW)b:↑ 1 lo qual. study (OW)b: ↑ 1 lo qual. study (NW)d: ↑ |
2 hi qual. studies (NW)ab: ↑ 1 hi qual. study (OW)a: ↑ 1 hi qual. study (OW/OB)b: ↑ 2 lo qual. studies (NW)ad: ↑ 1 lo qual. study (UW/NW)b: ↑ 1 lo qual. study (OW)b: ↑ |
1 hi qual. study (NW)b: ↑ 1 lo qual. study (NW)d: ↑ |
Overall: strong evidence of ↑ association
NW: strong evidence of ↑ association OW/OB: strong evidence of ↑ association No weight status criteria: moderate evidence of ↑ association due to mixed findings |
| Strong evidence of ↑ association | Strong evidence of ↑ association | Moderate evidence of ↑ association | ||
| Adults |
3 hi qual. studies bef: ↑ 1 hi qual. study g: ↔ |
4 hi qual. studies befg: ↑ 1 lo qual. study (OW/OB): ↓ |
4 hi qual. studies bbef: ↑ 3 hi qual. studies (NW)bef: ↑ 3 hi qual. studies (OW)bef: ↑ 1 hi qual. study h: ↔ 1 hi qual. study (NW)h: ↔ 1 hi qual. study (OW/OB)h:↔ 1 lo qual. study: ↔ |
|
| Strong evidence of ↑ association | Strong evidence of ↑ association | Strong evidence of ↑ association | ||
↑ indicates a significant positive association, ↓ indicates a significant negative association, and ↔ indicates no significant association between perceived overweight and outcome. Results with common superscript within evidence categories are from overlapping samples. For longitudinal studies, samples are classified into subgroups by baseline age and weight characteristics. Objective weight status categories: UW, underweight; NW, normal weight; OW, overweight; OB, obese. For individual study references, see Tables S4a and S4b.
hi qual., high‐quality; lo qual., low‐quality; POW, perceived overweight.
Cross‐sectional evidence.
Weight loss attempt or intention
We found strong evidence for an association between perceived overweight and weight loss attempts from cross‐sectional studies. All included studies provided consistent evidence to suggest that individuals who perceived themselves as overweight had a higher likelihood of intending or attempting to lose weight than those who perceived themselves as normal weight (32 findings from high‐quality studies 9, 10, 12, 30, 42, 43, 51, 56, 80, 87, 93, 95 and 15 from low‐quality studies 11, 14, 42, 63, 65, 68, 69, 71, 75, 85, 88). Overall, there was strong evidence to suggest that perceived overweight was associated with higher likelihood of trying to lose weight across all participant subgroups.
Weight control strategies: healthy
There was moderate cross‐sectional evidence for a relation between perceived overweight and use of healthy weight control strategies (e.g. eating less or different foods, or exercising to lose weight). A majority of findings suggested that individuals who perceived themselves as overweight were more likely to use healthy weight control strategies than those who did not (13 positive findings from high‐quality studies 45, 64, 72, 81, 93 and 9 from low‐quality studies 11, 30, 50, 55, 83, 89), but inconsistencies downgraded the evidence to moderate (three null findings from high‐quality studies 36, 87 and one from low‐quality studies 60, one negative from low‐quality study 82 and three mixed findings from low‐quality studies 65, 75). Within subgroups, there was moderate to strong evidence for a positive relation between perceived overweight and use of healthy weight control strategies for individuals with overweight/obesity and normal weight, and combined gender adolescent groups. For other participant subgroups, there was insufficient evidence because of inconsistent findings for male and female adolescent groups and evidence of no relation in subsamples with no weight status criteria. For each of these subgroups, some findings indicated a null relation, and some indicated a positive relation (i.e. perceived overweight was associated with greater use of healthy weight control strategies). In adult subgroups, the evidence was insufficient because of scarce evidence (only two findings from a high‐quality study 64 suggested a positive relationship, and one low‐quality study 60 provided null results). Perceived overweight was therefore associated with greater use of healthy weight control strategies overall and in certain participant groups (e.g. individuals with normal weight and overweight/obesity, and combined gender subgroups), but because of small study numbers and inconsistent findings, there was insufficient evidence to conclude that perceived overweight was associated with healthy weight control strategies in other subgroups.
Weight control strategies: unhealthy
There was moderate evidence for a relation between perceived overweight and unhealthy weight control strategies. The majority of cross‐sectional evidence suggested that perceived overweight was associated with higher likelihood of using unhealthy weight control strategies (12 findings from high‐quality studies 18, 36, 57, 62, 67, 78, 81, 94 and 13 from low‐quality studies 37, 48, 50, 53, 55, 61, 83, 89), but the strength of the evidence was downgraded to ‘moderate’ as an additional 10 findings were null 11, 41, 48, 54, 57, 89, and 7 were mixed findings or suggested a negative relation (such that perceived overweight was associated with lower likelihood of using unhealthy weight control strategies) 36, 65, 93, 94. There was strong evidence to suggest that perceived overweight was associated with greater use of unhealthy weight control strategies in the normal weight and no weight status criteria subgroups. For all adolescent subgroups, the evidence was moderate because of inconsistent findings: a majority of findings from high‐quality studies within these subgroups suggested a positive relation between perceived overweight and greater use of unhealthy weight control strategies, but there was a high number of null, negative or mixed findings. In the overweight and obese subgroup, there was insufficient evidence because of mixed findings. There was insufficient evidence to draw conclusions in adult subgroups because of a scarcity of studies, with only one high‐quality study 62 suggesting a positive relation between perceived overweight and use of unhealthy weight control strategies in female adults. Overall, there was moderate evidence to indicate that perceived overweight was associated with greater use of unhealthy weight control strategies, and there was moderate to strong evidence to support this conclusion within several participant subgroups, but because of a high level of inconsistency and a scarcity of evidence, the evidence was insufficient in adult and overweight/obese samples.
Weight‐related behaviour: healthy physical activity
There was insufficient cross‐sectional evidence for a relation between perceived overweight and healthy physical activity due to inconsistent findings. Eight findings from high‐quality studies 12, 30, 70, 93 and eight from low‐quality studies 11, 14, 15, 38, 65, 74, 86, 93 showed a negative relation, such that participants who perceived themselves as overweight were less physically active than those who perceived themselves as normal weight. However, other evidence included a combination of null (4 high‐quality studies 13, 30, 93 and 3 low‐quality studies 11, 86) and mixed (4 high‐quality studies 70, 91 and 1 low‐quality study 65) results. For male adolescents, there was strong evidence for an association between perceived overweight and lower physical activity, and there was moderate evidence because of mixed findings for this association in the combined gender adolescent subgroup. The evidence was also insufficient within each other participant subgroup because of inconsistent null and negative findings or because of a scarcity of evidence. Overall, while a majority of findings suggested that perceived overweight was associated with lower physical activity, a number of studies provided null results, meaning there was insufficient evidence to confirm a reliable association between perceived overweight and physical activity.
Weight‐related behaviour: healthy eating habits
Evidence from cross‐sectional studies suggested no association between perceived overweight and healthy eating habits. The majority of included studies found no relation between perceived overweight and healthy eating behaviours (9 high‐quality 12, 30, 91, 93 and 7 low‐quality studies11, 70, 90), but others produced negative (2 findings from low‐quality studies 14, 15 suggested perceived overweight was associated with less healthy eating) or mixed findings (2 high‐quality studies found a combination of negative, positive and null relations between perceived overweight and different indices of healthy eating 13, 93). In the overweight/obese, normal weight and each adolescent subgroup, perceived overweight was unrelated to healthy eating habits. Evidence within each adult participant subgroup was insufficient because of a lack of studies (1 high‐quality study 30 contributed evidence for a null relation between perceived overweight and healthy eating in male and female adults), and there was insufficient evidence because of mixed findings in the subgroup with no weight status criteria. Overall, perceived overweight was shown to be unrelated to healthy eating habits, although there was insufficient evidence and a high degree of inconsistency within some populations. Results of supplementary analyses of the relations between perceived overweight and fruit and vegetable consumption and between perceived overweight and unhealthy snack, beverage or fast food consumption (Table S4a) were consistent with the main evidence synthesis. Namely, there was evidence of no association between perceived overweight and fruit and vegetable consumption 11, 12, 13, 14, 70, 91, 93 or unhealthy food consumption 11, 12, 13, 14, 70, 91, 93.
Disordered eating
There was strong cross‐sectional evidence suggesting that perceived overweight was associated with higher levels of disordered eating. Three findings from high‐quality 45, 78 and nine from low‐quality studies 40, 49, 50, 52, 59, 60, 76 suggested a positive relation, such that perceived overweight was associated with disordered eating, and only a small number of studies produced null or mixed findings (1 high‐quality study 78 and 3 low‐quality studies 73, 75, 76). Within subgroups, there was strong evidence for a relation between perceived overweight and greater disordered eating in the combined gender adolescent and overweight/obese subgroups. In the female adolescent 78 and normal weight 45 subgroups, there was only moderate evidence for an association between perceived overweight and higher levels of disordered eating due to only one high‐quality study contributing evidence to each subgroup, and there was moderate evidence in the no weight status criteria subgroup due to there being no high‐quality studies. The evidence within other subgroups was classified as insufficient because of a scarcity of studies: one low‐quality study each within male adolescents 78 and adults 76 produced null results, and one low‐quality study suggested a positive relation between perceived overweight and disordered eating in female 76 and gender combined 60 adults. Overall, a majority of findings indicated that individuals who perceived themselves as overweight reported higher levels of disordered eating than those who perceived themselves as normal weight, contributing to strong evidence for this relation overall. However, because of a scarcity of high‐quality studies, the strength of evidence was downgraded to moderate or insufficient in various participant subgroups.
Longitudinal evidence
There were no longitudinal studies that examined the relation between perceived overweight and weight loss attempt or intentions, weight‐related behaviours (healthy physical activity or healthy eating habits) or healthy weight control strategies.
Weight control strategies: unhealthy
One low‐quality longitudinal study 79 found that perceived overweight was not significantly associated with future use of unhealthy weight control strategies in female adolescents. Thus, because of a lack of studies, there was insufficient evidence to make a conclusion about the longitudinal evidence for a relation between perceived overweight and unhealthy weight control strategies.
Disordered eating
One low‐quality longitudinal study 84 found that perceived overweight was not significantly associated with future disordered eating in female adolescents. As such, there was insufficient longitudinal evidence to make a conclusion about the association between perceived overweight and disordered eating because of a lack of studies.
Weight change
There was strong longitudinal evidence for an association between perceived overweight and weight change, such that perceived overweight was associated with greater weight gain or increased likelihood of overweight/obesity onset over time. Twenty‐six findings from high‐quality studies 21, 22, 47, 58, 92, 96 and eight findings from low‐quality studies 23, 44, 66 suggested that perceived overweight was associated with weight gain, while only a small number of null findings were included (2 from low‐quality studies23, 77 and 4 from high‐quality studies 58, 97), and one low‐quality study 39 suggested a negative relation (such that perceived overweight was associated with greater weight loss). Within most participant subgroups split by gender, objective weight status and age group, there was strong evidence for an association between perceived overweight and weight gain, except for the participant subgroup with no weight status criteria (where the evidence for a positive relationship was downgraded to moderate because of mixed findings), and in the combined adolescent subgroup (where there was moderate evidence for a positive association due to there being only one high‐quality study). Overall, there was strong evidence to suggest that individuals who perceived themselves as overweight were more likely to gain weight over time than those who perceived themselves as normal weight across most participant subgroups. Results of a supplementary analysis of a subset of nine studies 21, 44, 47, 58, 62, 92, 96, 97 that assessed weight change using objectively measured BMI only (i.e. those that met quality criterion 8; Table S4a) were consistent with the main evidence synthesis: there was strong evidence to indicate that overall, perceived overweight was associated with weight gain over time.
Discussion
The aim of this systematic review was to evaluate evidence for the relation between self‐perceived overweight and weight management. We examined peer‐reviewed literature published between 1991 and 2017 and found strong evidence to suggest perceived overweight was associated with a higher likelihood of trying to lose weight and moderate evidence to suggest perceived overweight was associated with greater use of both healthy and unhealthy weight control strategies. However, those weight loss attempts and strategies did not appear to be translated into healthy weight‐related behaviours. While there was no association between perceived overweight and healthier eating habits, there was moderate to strong evidence in some participant groups that perceived overweight was associated with reduced physical activity levels. However, overall, there was insufficient evidence because of inconsistent findings to evaluate the association between perceived overweight and physical activity. There was, however, strong evidence that perceived overweight was associated with disordered eating. Finally, strong longitudinal evidence indicated that perceived overweight was associated with increased future weight gain.
The most consistent evidence to emerge from this review was that perceived overweight was associated with attempting to lose weight. This was the case regardless of participant weight status, age group and gender. There was also moderate evidence for the relation between perceived overweight and the types of strategies adopted to lose weight; however, this relation varied by participant characteristics. In combined gender adolescent and normal weight samples, individuals who perceived themselves as overweight were more likely than those who did not, to engage in both healthy and unhealthy weight control strategies. There was also evidence from samples with no specific weight status criteria and of individuals with normal weight, and from separate male and female adolescent samples, that perceived overweight was associated with greater use of unhealthy weight control strategies. However, the evidence for a relationship between perceived overweight and use of healthy or unhealthy weight control strategies was inconclusive in other subgroups, because of scarce and inconsistent findings, and for samples with no weight status criteria, there was evidence to suggest no association between perceived overweight and use of healthy weight control strategies. Only one study provided longitudinal evidence to suggest that perceived overweight was unrelated to later use of unhealthy weight control strategies; therefore, it is unclear whether perceived overweight precedes the development of healthy or unhealthy weight control strategies, or vice versa.
Despite finding that perceived overweight was associated with use of healthy weight control strategies in some participant subgroups, the review did not provide evidence to suggest that perceived overweight was associated with the enactment of actual weight‐related behaviours such as healthy dietary intake and physical activity. In other words, while individuals who perceived their weight status as overweight were more likely to report trying to consume a healthy diet and increasing physical activity to lose weight, there was no evidence to suggest that these individuals were actually more likely to enact these behaviours than those who did not identify as overweight. All included studies (except one with mixed findings) on the relation between perceived overweight and physical activity suggested a negative (i.e. perceived overweight associated with lower physical activity levels) or null relationship. In adolescent male (where there was strong evidence) and combined gender (where there was moderate evidence) subgroups, perceived overweight was associated with lower levels of physical activity. However, a lack of longitudinal studies in weight‐related behaviour outcome categories means that it is unclear whether perceived overweight precedes lower physical activity or vice versa. In contrast to physical activity, there was evidence of no relationship between perceived overweight and healthy eating habits. The tendency for individuals to intend to engage in weight control behaviours but not execute these behaviours may be explained by the stigma attached to being overweight. For example, a fear of negative evaluation because of one's weight may make exercising in public unappealing 99, 100, and the stress of identifying as part of a stigmatized social group may promote poor dietary habits 101, 102.
Overall, the present review provided strong evidence to suggest that perceived overweight is associated with disordered eating. While there was inconclusive evidence on the relation between perceived overweight and disordered eating in male adolescent and all adult samples, there was moderate to strong evidence to suggest perceived overweight was associated with disordered eating in all other participant subgroups (female and combined gender adolescents, normal weight, overweight/obese and no specific weight status criteria subgroups). However, as only one study provided longitudinal evidence, it is unclear whether perceived overweight precedes or develops in conjunction with disordered eating. It is also possible that an unmeasured third factor predisposes an individual to both develop disordered eating and perceive their weight status as overweight.
Finally, there was strong longitudinal evidence to suggest that perceived overweight predicts weight gain over time, and this was the case across the majority of participant subgroups. This finding challenges the common assumption that identifying oneself as overweight will be associated with better weight management 2, 30.
The finding that identifying as overweight is associated with attempts to lose weight, but at the same time greater weight gain, appears counterintuitive. Attempts to lose weight by individuals who perceive themselves as overweight may not necessarily translate into the adoption or appropriate implementation of effective weight control strategies. Perceived overweight was associated with unhealthy weight control strategies and disordered eating. These findings could be attributable, at least in part, to the stigma attached to psychologically identifying as being overweight 101. Perceiving oneself as part of a stigmatized group could motivate individuals to adopt more extreme efforts to lose weight in an attempt to escape stigma, which could lead to later weight gain 12, 19. Second, despite being associated with greater self‐reported use of healthy weight control strategies, perceived overweight was not associated with healthier eating habits and, in some samples, was associated with lower physical activity. Thus, despite greater self‐reported attempts to lose weight, individuals who perceive their weight status as overweight may not effectively translate their weight loss intentions into effective weight loss behaviours. This intention–behaviour gap is well‐recognized in health psychology 103, and for individuals who perceive themselves as overweight, the experience of perceiving oneself as part of a stigmatized group could be responsible. Experiencing stigma can deplete self‐regulatory resources 104, which could inhibit the initiation and maintenance of complex patterns of behaviours required for healthy weight loss such as eating healthily and maintaining adequate levels of physical activity 20. Weight stigma has also been shown to encourage binge eating and overconsumption of unhealthy snack foods, which can undermine weight loss efforts 101. There appeared to be little evidence in the studies reviewed here that the relationship between perceived overweight and the outcome measures varied systematically between samples of individuals who were objectively overweight or obese and those of a normal weight. These findings suggest that the accuracy of weight perception may be less important than perceiving oneself as part of a stigmatized group.
The findings of this review have implications for public health approaches to tackle obesity. Some public health approaches are based on the assumption that notifying individuals that they are overweight is necessary to motivate them to adopt healthy behaviours and lose weight, but the evidence reviewed here does not support this proposition. The evidence reviewed here suggests that although perceiving one's weight status as overweight may motivate an individual to try to lose weight, it may not result in the implementation of effective weight loss behaviours and could even lead to greater weight gain. Further, notifying individuals of their weight status may also have other unintended negative consequences such as increasing the risk of poor mental health 25, 105 and encouraging disordered eating 2, 78, 105, although this review highlights the need for further longitudinal evidence to inform whether identifying as overweight is a precursor of disordered eating, or merely a correlate. Eating disorders and obesity share common precursors such as body dissatisfaction and excessive dieting 106, 107. As a result, they are increasingly being jointly targeted in prevention efforts which, for example, promote the adoption of healthy lifestyle behaviours and simultaneously reduce excessive weight concern and obesity stigma 108, 109. Such approaches may temper the association between perceived overweight and both disordered eating and weight gain and could offer a better alternative to obesity prevention efforts which focus on notifying individuals of their weight status. However, controlled experimental studies of the effect of manipulating perceived weight status are now needed to better address the question of whether it is mostly helpful or harmful to notify individuals of their weight status.
A strength of the present review is that it included a large number of studies and only included those that controlled or stratified by objective weight status. This allowed closer isolation of the association between perceived overweight and weight management intentions and behaviours, both of which are associated with objective weight status. Nonetheless, the present review is also subject to several limitations. First, publication bias may have influenced the findings. Given the wide date range, it was not practical to perform searches for unpublished studies, meaning that the association between perceived overweight and certain outcomes may be overstated. Second, despite the large number of included studies, the evidence was graded as insufficient for several outcome categories in some participant subgroups. Third, it is important to note that weight‐related behaviours were commonly assessed with short self‐report scales or single items that are subject to reporting bias and demand characteristics. Future research would be well‐placed to obtain more robust estimates of the association between perceived overweight and weight‐related behaviour by using more objective assessment methods. Fourth, the majority of studies included in the review were conducted in the USA or Europe (69%), highlighting a need for further research on the relation between perceived overweight and weight management in other cultural contexts. Previous research has demonstrated ethnic differences in body weight preferences, body dissatisfaction and weight stigma 110, 111, 112. Therefore, it is plausible that the impact of perceived overweight on weight‐related intentions, behaviours and outcomes could differ by ethnic group, which is an important direction for future research. Finally, the type of studies included in the review limits the strength of the conclusions that can be drawn. For all outcome categories except weight gain, insufficient longitudinal studies were included to determine whether perceived overweight precedes the onset of the weight‐related correlate, or vice versa. For example, it is conceivable that the negative relation between perceived overweight and physical activity evidenced in some participant groups could reflect that individuals who are less active are more likely to perceive themselves as overweight than individuals of the same objective weight status but who engage in sufficient physical activity. Furthermore, the review only included observational studies, precluding causal conclusions. It is possible that some third variable is attributable for the relation between perceived overweight and the weight management outcome variables. Longitudinal studies that track weight management behaviours over time and experiments in which participants are randomly assigned to interventions where they are notified of their overweight status would help to elucidate whether becoming aware of one's overweight status is beneficial or harmful to weight management.
Conflict of interest statement
No conflict of interest was declared.
Supporting information
Table S1. Search Strategy
Table S2a. Characteristics of included studies.
Table S2b. Weight perception measurement and outcome categories.
Table S3. Methodological quality of included studies
Table S4a. Evidence synthesis by outcome category and subsample with references (cross‐sectional studies).
Table S4b. Evidence synthesis by outcome category and subsample with references (longitudinal studies).
Acknowledgements
We are grateful to Chloe Thompson, Rebecca Bianchi and Emily Crowne for research assistance. E. R.'s salary was supported by the Medical Research Council and Economic Social Research Council. E. R. has previously received research funding from Unilever and the American Beverage Association. A. R. S. was supported by a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (1R15HD083947).
Haynes, A. , Kersbergen, I. , Sutin, A. , Daly, M. , and Robinson, E. (2018) A systematic review of the relationship between weight status perceptions and weight loss attempts, strategies, behaviours and outcomes. Obesity Reviews, 19: 347–363. doi: 10.1111/obr.12634.
References
- 1. Robinson E. Overweight but unseen: a review of the underestimation of weight status and a visual normalization theory. Obes Rev 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Johnson F, Cooke L, Croker H, Wardle J. Changing perceptions of weight in Great Britain: comparison of two population surveys. BMJ 2008; 337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Robinson E, Oldham M. Weight status misperceptions among UK adults: the use of self‐reported vs. measured BMI. BMC Obesity 2016; 3(1): 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Foti K, Lowry R. Trends in perceived overweight status among overweight and nonoverweight adolescents. Arch Pediatr Adolesc Med 2010; 164(7): 636–642. [DOI] [PubMed] [Google Scholar]
- 5. NICE . Obesity: identification, assessment, and management. Clinical Guideline [CG189]. National Institute for Health and Care Excellence. London; 2014. [PubMed]
- 6. Moyer VA, on behalf of the USPSTF . Screening for and management of obesity in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 2012;157(5):373–8. [DOI] [PubMed] [Google Scholar]
- 7. NHS . National Child Measurement Programme [Internet, cited 23/05/2017]. Available from: http://www.content.digital.nhs.uk/ncmp (accessed 23/05/2017).
- 8. Ruggieri DG, Bass SB. A comprehensive review of school‐based body mass index screening programs and their implications for school health: do the controversies accurately reflect the research? J Sch Health 2015; 85(1): 61–72. [DOI] [PubMed] [Google Scholar]
- 9. Chen HY, Lemon SC, Pagoto SL, Barton BA et al Personal and parental weight misperception and self‐reported attempted weight loss in US children and adolescents, National Health and Nutrition Examination Survey, 2007–2008 and 2009–2010. Prev Chronic Dis 2014; 11: E132.* [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Yaemsiri S, Slining MM, Agarwal SK. Perceived weight status, overweight diagnosis, and weight control among US adults: the NHANES 2003–2008 Study. Int J Obes 2011; 35(8): 1063–1070.* [DOI] [PubMed] [Google Scholar]
- 11. Edwards NM, Pettingell S, Borowsky IW. Where perception meets reality: self‐perception of weight in overweight adolescents. Pediatrics 2010; 125(3): e452–e458.* [DOI] [PubMed] [Google Scholar]
- 12. Fredrickson J, Kremer P, Swinburn B, de Silva A et al Weight perception in overweight adolescents: associations with body change intentions, diet and physical activity. J Health Psychol 2015; 20(6): 774–784.* [DOI] [PubMed] [Google Scholar]
- 13. Xie B, Chou C‐P, Spruijt‐Metz D, Reynolds K et al Weight perception and weight‐related sociocultural and behavioral factors in Chinese adolescents. Prev Med 2006; 42(3): 229–234.* [DOI] [PubMed] [Google Scholar]
- 14. Southerland J, Wang L, Richards K, Pack R et al Misperceptions of overweight: associations of weight misperception with health‐related quality of life among normal‐weight college students. Public Health Rep 2013; 128(6): 562–568.* [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Thunfors P, Hanlon AL, Collins BN. Weight status misperception and the health behaviors of obese adolescents. Internet J Pediatr Neonatol 2011; 13(1).* [Google Scholar]
- 16. Robinson E, Haynes A, Sutin A, Daly M. Telling people they are overweight: helpful, harmful or beside the point? Int J Obes 2017; 41: 1160–1161. [DOI] [PubMed] [Google Scholar]
- 17. Wilson JMB, Tripp DA, Boland FJ. The relative contributions of subjective and objective measures of body shape and size to body image and disordered eating in women. Body Image 2005; 2(3): 233–247 15p. [DOI] [PubMed] [Google Scholar]
- 18. Stephen EM, Rose J, Kenney L, Rosselli‐Navarra F et al Prevalence and correlates of unhealthy weight control behaviors: findings from the national longitudinal study of adolescent health. J Eat Disord 2014; 2(1): 16.* [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Neumark‐Sztainer D, Wall M, Guo J, Story M et al Obesity, disordered eating, and eating disorders in a longitudinal study of adolescents: how do dieters fare 5 years later? J Am Diet Assoc 2006; 106(4): 559–568. [DOI] [PubMed] [Google Scholar]
- 20. Hunger JM, Major B, Blodorn A, Miller CT. Weighed down by stigma: how weight‐based social identity threat contributes to weight gain and poor health. Soc Personal Psychol Compass 2015; 9(6): 255–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Robinson E, Hunger JM, Daly M. Perceived weight status and risk of weight gain across life in US and UK adults. Int J Obes 2015; 39(12): 1721–1726.* [DOI] [PubMed] [Google Scholar]
- 22. Sutin AR, Terracciano A. Body weight misperception in adolescence and incident obesity in young adulthood. Psychol Sci 2015; 26(4): 507–511.* [DOI] [PubMed] [Google Scholar]
- 23. Klein EG, Lytle LA, Chen V. Social ecological predictors of the transition to overweight in youth: results from the Teens Eating for Energy and Nutrition at Schools (TEENS) study. J Am Diet Assoc 2008; 108(7): 1163–1169.* [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Moher D, Liberati A, Tetzlaff J, Altman DG et al Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. Ann Intern Med 2009; 151(4): 264–269. [DOI] [PubMed] [Google Scholar]
- 25. Atlantis E, Ball K. Association between weight perception and psychological distress. Int J Obes 2008; 32. [DOI] [PubMed] [Google Scholar]
- 26. Eaton DK, Lowry R, Brener ND, Galuska DA et al Associations of body mass index and perceived weight with suicide ideation and suicide attempts among US high school students. Arch Pediatr Adolesc Med 2005; 159(6) 513‐9 7p. [DOI] [PubMed] [Google Scholar]
- 27. Farhat T, Iannotti RJ, Summersett‐Ringgold F. Weight, weight perceptions, and health‐related quality of life among a national sample of US girls. J Dev Behav Pediatr 2015; 36(5): 313–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Hayward J, Millar L, Petersen S, Swinburn B et al When ignorance is bliss: weight perception, body mass index and quality of life in adolescents. Int J Obes 2014; 38(10): 1328 34 7p. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Tang J, Yu Y, Du Y, Ma Y et al Association between actual weight status, perceived weight and depressive, anxious symptoms in Chinese adolescents: a cross‐sectional study. BMC Public Health 2010; 10(1): 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Duncan DT, Wolin KY, Scharoun‐Lee M, Ding EL et al Does perception equal reality? Weight misperception in relation to weight‐related attitudes and behaviors among overweight and obese US adults. Int J Behav Nutr Phys Act 2011: 8.* [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Joanna Briggs Institute . Critical appraisal checklist for analytical cross sectional studies In: Joanna Briggs Institute Reviewer's Manual: Australia, 2014. [Google Scholar]
- 32. Tooth L, Ware R, Bain C, Purdie DM et al Quality of reporting of observational longitudinal research. Am J Epidemiol 2005; 161(3): 280–288. [DOI] [PubMed] [Google Scholar]
- 33. van Ekris E, Altenburg TM, Singh AS, Proper KI et al An evidence‐update on the prospective relationship between childhood sedentary behaviour and biomedical health indicators: a systematic review and meta‐analysis. Obes Rev 2016; 17(9): 833–849. [DOI] [PubMed] [Google Scholar]
- 34. Chinapaw MJM, Proper KI, Brug J, van Mechelen W et al Relationship between young peoples' sedentary behaviour and biomedical health indicators: a systematic review of prospective studies. Obes Rev 2011; 12(7): e621–ee32. [DOI] [PubMed] [Google Scholar]
- 35. Singh AS, Mulder C, Twisk JW, Van Mechelen W et al Tracking of childhood overweight into adulthood: a systematic review of the literature. Obes Rev 2008; 9(5): 474–488. [DOI] [PubMed] [Google Scholar]
- 36. Al Sabbah H, Vereecken C, Abdeen Z, Kelly C et al Weight control behaviors among overweight, normal weight and underweight adolescents in Palestine: findings from the national study of Palestinian schoolchildren (HBSC‐WBG2004). Int J Eat Disord 2010; 43(4): 326–336.* [DOI] [PubMed] [Google Scholar]
- 37. Armstrong B, Westen SC, Janicke DM. The role of overweight perception and depressive symptoms in child and adolescent unhealthy weight control behaviors: a mediation model. J Pediatr Psychol 2014; 39(3): 340–348.* [DOI] [PubMed] [Google Scholar]
- 38. Baharudin A, Zainuddin AA, Manickam MA, Ambak R et al Factors associated with physical inactivity among school‐going adolescents: data from the Malaysian School‐Based Nutrition Survey 2012. Asia Pac J Public Health 2014; 26(5 Suppl): 27s–35s.* [DOI] [PubMed] [Google Scholar]
- 39. Bak‐Sosnowska M, Zahorska‐Markiewicz B. The image of one's own body and the effectiveness of weight loss therapy. Wiad Lek 2009; 62(2): 104–110.* [PubMed] [Google Scholar]
- 40. Bilali A, Galanis P, Velonakis E, Katostaras T. Factors associated with abnormal eating attitudes among Greek adolescents. J Nutr Educ Behav 2010; 42(5): 292–298.* [DOI] [PubMed] [Google Scholar]
- 41. Bittner Fagan H, Diamond J, Myers R, Gill JM. Perception, intention, and action in adolescent obesity. J Am Board Fam Med 2008; 21(6): 555–561.* [DOI] [PubMed] [Google Scholar]
- 42. Brug J, Wammes B, Kremers S, Giskes K et al Underestimation and overestimation of personal weight status: associations with socio‐demographic characteristics and weight maintenance intentions. J Hum Nutr Diet 2006; 19(4): 253–262.* [DOI] [PubMed] [Google Scholar]
- 43. Cai L, Han X, Qi Z, Li Z et al Prevalence of overweight and obesity and weight loss practice among Beijing adults, 2011. PLoS One 2014; 9(9) e98744.* [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Cuypers K, Kvaløy K, Bratberg G, Midthjell K et al Being normal weight but feeling overweight in adolescence may affect weight development into young adulthood—an 11‐year followup: the HUNT study, Norway. J Obes 2012: 2012.* [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Deschamps V, Salanave B, Chan‐Chee C, Vernay M et al Body‐weight perception and related preoccupations in a large national sample of adolescents. Pediatr Obes 2015; 10(1): 15–22.* [DOI] [PubMed] [Google Scholar]
- 46. Duncan JS, Duncan EK, Schofield G. Associations between weight perceptions, weight control and body fatness in a multiethnic sample of adolescent girls. Public Health Nutr 2011; 14(1): 93–100.* [DOI] [PubMed] [Google Scholar]
- 47. Duong HT, Roberts RE. Perceived weight in youths and risk of overweight or obesity six years later. J Psychosom Res 2014; 76(1): 23–27.* [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Eichen DM, Conner BT, Daly BP, Fauber RL. Weight perception, substance use, and disordered eating behaviors: comparing normal weight and overweight high‐school students. J Youth Adolesc 2012; 41(1): 1–13.* [DOI] [PubMed] [Google Scholar]
- 49. Fay K, Economos C, Lerner RM, Becker AE et al The association between sports participation and athletic identity with eating pathology among college‐aged males and females. Eat Weight Disord 2011; 16(2): e102–ee12*. [DOI] [PubMed] [Google Scholar]
- 50. French SA, Story M, Neumark‐Sztainer D, Downes B et al Ethnic differences in psychosocial and health behavior correlates of dieting, purging, and binge eating in a population‐based sample of adolescent females. Int J Eat Disord 1997; 22(3): 315–322.* [DOI] [PubMed] [Google Scholar]
- 51. Getaneh A, Giardina EG, Findley SE. Factors related to weight loss attempt among Dominican immigrants. J Immigr Minor Health 2013; 15(3): 591–597.* [DOI] [PubMed] [Google Scholar]
- 52. Haase AM. Weight perception in female athletes: associations with disordered eating correlates and behavior. Eat Behav 2011; 12(1): 64–67.* [DOI] [PubMed] [Google Scholar]
- 53. Hadland SE, Austin SB, Goodenow CS, Calzo JP. Weight misperception and unhealthy weight control behaviors among sexual minorities in the general adolescent population. J Adolesc Health 2014; 54(3): 296–303.* [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Haley CC, Hedberg K, Leman RF. Disordered eating and unhealthy weight loss practices: which adolescents are at highest risk? J Adolesc Health 2010; 47(1): 102–105.* [DOI] [PubMed] [Google Scholar]
- 55. Harring HA, Montgomery K, Hardin J. Perceptions of body weight, weight management strategies, and depressive symptoms among US college students. J Am Coll Health 2010; 59(1): 43–50.* [DOI] [PubMed] [Google Scholar]
- 56. Hwang JH, Ryu DH, Park SW. Interaction effect between weight perception and comorbidities on weight control behavior in overweight and obese adults: is there a sex difference? J Korean Med Sci 2015; 30(8): 1017–1024.* [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Ibrahim C, El‐Kamary SS, Bailey J, St George DM. Inaccurate weight perception is associated with extreme weight‐management practices in U.S. high school students. J Pediatr Gastroenterol Nutr 2014; 58(3): 368–375.* [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Inoue M, Toyokawa S, Inoue K, Suyama Y et al Lifestyle, weight perception and change in body mass index of Japanese workers: MY Health Up Study. Public Health 2010; 124(9): 530–537.* [DOI] [PubMed] [Google Scholar]
- 59. Joiner TEJ, Heatherton TF, Rudd MD, Schmidt NB. Perfectionism, perceived weight status, and bulimic symptoms: two studies testing a diathesis‐stress model. J Abnorm Psychol 1997; 106(1): 145.* [DOI] [PubMed] [Google Scholar]
- 60. Jones M, Grilo CM, Masheb RM, White MA. Psychological and behavioral correlates of excess weight: misperception of obese status among persons with class II obesity. Int J Eat Disord 2010; 43(7): 628–632.* [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Kim DS, Cho Y, Cho SI, Lim IS. Body weight perception, unhealthy weight control behaviors, and suicidal ideation among Korean adolescents. J Sch Health 2009; 79(12): 585–592.* [DOI] [PubMed] [Google Scholar]
- 62. Kim DS, Kim HS, Cho Y, Cho SI. The effects of actual and perceived body weight on unhealthy weight control behaviors and depressed mood among adult women in Seoul, Korea. J Prev Med Public Health 2008; 41(5): 323–330.* [DOI] [PubMed] [Google Scholar]
- 63. Lebrun LA, Chowdhury J, Sripipatana A, Nair S et al Overweight/obesity and weight‐related treatment among patients in U.S. federally supported health centers. Obes Res Clin Pract 2013; 7(5): e377–e390.* [DOI] [PubMed] [Google Scholar]
- 64. Lemon SC, Rosal MC, Zapka J, Borg A et al Contributions of weight perceptions to weight loss attempts: differences by body mass index and gender. Body Image 2009; 6(2): 90–96.* [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Lenhart CM, Daly BP, Eichen DM. Is accuracy of weight perception associated with health risk behaviors in a diverse sample of obese adolescents? J Sch Nurs 2011; 27(6): 416–423.* [DOI] [PubMed] [Google Scholar]
- 66. Liechty JM, Lee MJ. Body size estimation and other psychosocial risk factors for obesity onset among US adolescents: findings from a longitudinal population level study. Int J Obes (Lond) 2015; 39(4): 601–607.* [DOI] [PubMed] [Google Scholar]
- 67. McGee RE, Thompson NJ. Disordered eating and forced sex among adolescent males. J Mens Health 2013; 10(3): 104–111.* [Google Scholar]
- 68. Mehio‐Sibai A, Kanaan N, Chaaya M, Rahal B et al Ethnic differences in weight loss behavior among secondary school students in Beirut: the role of weight perception. Soz Praventivmed 2003; 48(4): 234–241.* [DOI] [PubMed] [Google Scholar]
- 69. Ojala K, Tynjälä J, Välimaa R, Villberg J et al Overweight adolescents' self‐perceived weight and weight control behaviour: HBSC study in Finland 1994–2010. J Obes 2012: 1–9.* [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Patte KA, Laxer RE, Qian W, Leatherdale ST. An analysis of weight perception and physical activity and dietary behaviours among youth in the COMPASS study. Soc Sci Med Popul Health 2016; 2: 841–849.* [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Peltzer K, Pengpid S. Trying to lose weight among non‐overweight university students from 22 low, middle and emerging economy countries. Asia Pac J Clin Nutr 2015; 24(1): 177–183.* [DOI] [PubMed] [Google Scholar]
- 72. Quick V, Nansel TR, Liu D, Lipsky LM et al Body size perception and weight control in youth: 9‐year international trends from 24 countries. Int J Obes (Lond) 2014; 38(7): 988–994.* [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Saules KK, Collings AS, Hoodin F, Angelella NE et al The contributions of weight problem perception, BMI, gender, mood, and smoking status to binge eating among college students. Eat Behav 2009; 10(1): 1–9.* [DOI] [PubMed] [Google Scholar]
- 74. Seo D‐C, Nehl E, Agley J, Ma S‐M. Relations between physical activity and behavioral and perceptual correlates among Midwestern college students. J Am Coll Health 2007; 56(2): 187–197.* [DOI] [PubMed] [Google Scholar]
- 75. Shamaley‐Kornatz A, Smith B, Tomaka J. Weight goals, perceptions, and practices among Hispanic and Anglo college females. Hispanic J Behav Sci 2007; 29(4): 535–553.* [Google Scholar]
- 76. Siqueira KS, Appolinario JC, Sichieri R. Relationship between binge‐eating episodes and self‐perception of body weight in a nonclinical sample of five Brazilian cities. Rev Bras Psiquiatr 2005; 27(4): 290–294.* [DOI] [PubMed] [Google Scholar]
- 77. Siu J, Giskes K, Shaw J, Turrell G. Perceived weight status may contribute to education inequalities in five‐year weight change among mid‐aged women. Aust N Z J Public Health 2011; 35(3): 284–291.* [DOI] [PubMed] [Google Scholar]
- 78. Sonneville KR, Thurston IB, Milliren CE, Gooding HC et al Weight misperception among young adults with overweight/obesity associated with disordered eating behaviors. Int J Eat Disord 2016; 49(10): 937–946.* [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Stephen EM, Rose J, Kenney L, Rosselli‐Navarra F et al Adolescent risk factors for purging in young women: findings from the national longitudinal study of adolescent health. J Eat Disord 2014; 2(1): 1.* [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Swaminathan S, Selvam S, Pauline M, Vaz M. Associations between body weight perception and weight control behaviour in South Indian children: a cross‐sectional study. BMJ Open 2013; 3(3) e002239.* [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Talamayan KS, Springer AE, Kelder SH, Gorospe EC et al Prevalence of overweight misperception and weight control behaviors among normal weight adolescents in the United States. Scientific World J 2006; 6: 365–373.* [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Ting WH, Huang CY, Tu YK, Chien KL. Association between weight status and depressive symptoms in adolescents: role of weight perception, weight concern, and dietary restraint. Eur J Pediatr 2012; 171(8): 1247–1255.* [DOI] [PubMed] [Google Scholar]
- 83. Ursoniu S, Putnoky S, Vlaicu B. Body weight perception among high school students and its influence on weight management behaviors in normal weight students: a cross‐sectional study. Wien Klin Wochenschr 2011; 123(11–12): 327–333.* [DOI] [PubMed] [Google Scholar]
- 84. Vohs KD, Bardone AM, Joiner TE Jr, Abramson LY et al Perfectionism, perceived weight status, and self‐esteem interact to predict bulimic symptoms: a model of bulimic symptom development. J Abnorm Psychol 1999; 108(4): 695–700.* [DOI] [PubMed] [Google Scholar]
- 85. Wang Y, Liang H, Chen X. Measured body mass index, body weight perception, dissatisfaction and control practices in urban, low‐income African American adolescents. BMC Public Health 2009; 9: 183.* [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Yancey AK, Simon PA, McCarthy WJ, Lightstone AS et al Ethnic and sex variations in overweight self‐perception: relationship to sedentariness. Obesity (Silver Spring) 2006; 14(6): 980–988.* [DOI] [PubMed] [Google Scholar]
- 87. Yost J, Krainovich‐Miller B, Budin W, Norman R. Assessing weight perception accuracy to promote weight loss among U.S. female adolescents: a secondary analysis. BMC Public Health 2010; 10: 465.* [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Zapka J, Lemon SC, Estabrook B, Rosal MC. Factors related to weight loss behavior in a multiracial/ethnic workforce. Ethn Dis 2009; 19(2): 154–160.* [PMC free article] [PubMed] [Google Scholar]
- 89. Zhang J, Seo DC, Kolbe L, Lee A et al Comparison of overweight, weight perception, and weight‐related practices among high school students in three large Chinese cities and two large U.S. cities. J Adolesc Health 2011; 48(4): 366–372.* [DOI] [PubMed] [Google Scholar]
- 90. Zhao M, Zhang M, Zhou X, Yang H et al Weight misperception and its barriers to keep health weight in Chinese children. Acta Paediatr 2012; 101(12): 550–556.* [DOI] [PubMed] [Google Scholar]
- 91. Cai L, Zhang T, Ma J, Ma L et al Self‐perception of weight status and its association with weight‐related knowledge, attitudes, and behaviors among Chinese children in Guangzhou. J Epidemiol 2017; 27(7): 338–345.* [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Daly M, Robinson E, Sutin AR. Does knowing hurt? Perceiving oneself as overweight predicts future physical health and well‐being. Psychol Sci 2017; 28(7): 872–881.* [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Fan M, Jin Y. The effects of weight perception on adolescents' weight‐loss intentions and behaviors: evidence from the Youth Risk Behavior Surveillance Survey. Int J Environ Res Public Health 2015; 12(11) 14640.* [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Hazzard VM, Hahn SL, Sonneville KR. Weight misperception and disordered weight control behaviors among U.S. high school students with overweight and obesity: associations and trends, 1999–2013. Eat Behav 2017; 26: 189–195.* [DOI] [PubMed] [Google Scholar]
- 95. Patte KA, Laxer R, Qian W, Leatherdale ST. Weight perception and weight‐control intention among youth in the COMPASS study. Am J Health Behav 2016; 40(5): 614–623.* [DOI] [PubMed] [Google Scholar]
- 96. Sonneville KR, Thurston IB, Milliren CE, Kamody RC et al Helpful or harmful? Prospective association between weight misperception and weight gain among overweight and obese adolescents and young adults. Int J Obes (Lond) 2016; 40(2): 328–332.* [DOI] [PubMed] [Google Scholar]
- 97. Wang ML, Haughton CF, Frisard C, Pbert L et al Perceived weight status and weight change among a U.S. adult sample. Obesity (Silver Spring) 2017; 25(1): 223–228.* [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Paeratakul S, White MA, Williamson DA, Ryan DH et al Sex, race/ethnicity, socioeconomic status, and BMI in relation to self‐perception of overweight. Obes Res 2002; 10(5): 345–350. [DOI] [PubMed] [Google Scholar]
- 99. Vartanian LR, Shaprow JG. Effects of weight stigma on exercise motivation and behavior. J Health Psychol 2008; 13(1): 131–138. [DOI] [PubMed] [Google Scholar]
- 100. Ball K, Crawford D, Owen N. Obesity as a barrier to physical activity. A N Z J Public Health 2000; 24(3): 331–333. [DOI] [PubMed] [Google Scholar]
- 101. Vartanian LR, Porter AM. Weight stigma and eating behavior: a review of the literature. Appetite 2016; 102: 3–14. [DOI] [PubMed] [Google Scholar]
- 102. Major B, Hunger JM, Bunyan DP, Miller CT. The ironic effects of weight stigma. J Exp Soc Psychol 2014; 51: 74–80. [Google Scholar]
- 103. Sheeran P. Intention—behavior relations: a conceptual and empirical review. Eur Rev Soc Psychol 2002; 12(1): 1–36. [Google Scholar]
- 104. Inzlicht M, McKay L, Aronson J. Stigma as ego depletion. Psychol Sci 2006; 17(3): 262–269. [DOI] [PubMed] [Google Scholar]
- 105. Roberts RE, Duong HT. Perceived weight, not obesity, increases risk for major depression among adolescents. J Psychiatr Res 2013; 47(8): 1110–1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Haines J, Neumark‐Sztainer D. Prevention of obesity and eating disorders: a consideration of shared risk factors. Health Educ Res 2006; 21(6): 770–782. [DOI] [PubMed] [Google Scholar]
- 107. Neumark‐Sztainer DR, Wall MM, Haines JI, Story MT et al Shared risk and protective factors for overweight and disordered eating in adolescents. Am J Prev Med 2007; 33(5): 359–369. [DOI] [PubMed] [Google Scholar]
- 108. Sánchez‐Carracedo D, Neumark‐Sztainer D, López‐Guimerà G. Integrated prevention of obesity and eating disorders: barriers, developments and opportunities. Public Health Nutr 2012; 15(12): 2295–2309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Austin SB. The blind spot in the drive for childhood obesity prevention: bringing eating disorders prevention into focus as a public health priority. Am J Public Health 2011; 101(6): e1–e4. [DOI] [PubMed] [Google Scholar]
- 110. Latner JD, Stunkard AJ, Wilson GT. Stigmatized students: age, sex, and ethnicity effects in the stigmatization of obesity. Obesity (Silver Spring) 2005; 13(7): 1226–1231. [DOI] [PubMed] [Google Scholar]
- 111. Fitzgibbon ML, Blackman LR, Avellone ME. The relationship between body image discrepancy and body mass index across ethnic groups. Obes Res 2000; 8(8): 582–589. [DOI] [PubMed] [Google Scholar]
- 112. Wildes JE, Emery RE, Simons AD. The roles of ethnicity and culture in the development of eating disturbance and body dissatisfaction: a meta‐analytic review. Clin Psychol Rev 2001; 21(4): 521–551. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Search Strategy
Table S2a. Characteristics of included studies.
Table S2b. Weight perception measurement and outcome categories.
Table S3. Methodological quality of included studies
Table S4a. Evidence synthesis by outcome category and subsample with references (cross‐sectional studies).
Table S4b. Evidence synthesis by outcome category and subsample with references (longitudinal studies).


