This nationwide cohort study examined changes in bystander defibrillation and subsequent survival among patients with out-of-hospital cardiac arrest according to public or residential location.
Key Points
Question
Were nationwide initiatives to facilitate public-access defibrillation associated with an increase in bystander defibrillation in residential and public locations of out-of-hospital cardiac arrests?
Findings
This nationwide cohort study of 18 688 patients showed a large increase in bystander defibrillation in public locations from 1.2% in 2001 to 15.3% in 2012, whereas bystander defibrillation in residential locations remained unchanged from 1.3% in 2001 to 1.3% in 2012. During this period, several initiatives were undertaken to facilitate bystander defibrillation.
Meaning
Nationwide initiatives to facilitate bystander defibrillation were associated with a marked increase in bystander defibrillation in public but not residential locations.
Abstract
Importance
Bystander-delivered defibrillation (hereinafter referred to as bystander defibrillation) of patients with out-of-hospital cardiac arrests (OHCAs) remains limited despite the widespread dissemination of automated external defibrillators (AEDs).
Objective
To examine calendar changes in bystander defibrillation and subsequent survival according to a public or a residential location of the cardiac arrest after nationwide initiatives in Denmark to facilitate bystander-mediated resuscitative efforts, including bystander defibrillation.
Design, Setting, and Participants
This nationwide study identified 18 688 patients in Denmark with first-time OHCA from June 1, 2001, to December 31, 2012, using the Danish Cardiac Arrest Registry. Patients had a presumed cardiac cause of arrest that was not witnessed by emergency medical services personnel. Data were analyzed from April 1, 2015, to December 10, 2016.
Exposures
Nationwide initiatives to facilitate bystander resuscitative efforts, including bystander defibrillation, consisted of resuscitation training of Danish citizens, dissemination of on-site AEDs, foundation of an AED registry linked to emergency medical dispatch centers, and dispatcher-assisted guidance of bystander resuscitation efforts.
Main Outcomes and Measures
The proportion of patients who received bystander defibrillation according to the location of the cardiac arrest and their subsequent 30-day survival.
Results
Of the 18 688 patients with OHCAs (67.8% men and 32.2% women; median [interquartile range] age, 72 [62-80] years), 4783 (25.6%) had a cardiac arrest in a public location and 13 905 (74.4%) in a residential location. The number of registered AEDs increased from 141 in 2007 to 7800 in 2012. The distribution of AED location was consistently skewed in favor of public locations. Bystander defibrillation increased in public locations from 3 of 245 (1.2%; 95% CI, 0.4%-3.5%) in 2001 to 78 of 510 (15.3%; 95% CI, 12.4%-18.7%) in 2012 (P < .001) but remained unchanged in residential locations from 7 of 542 (1.3%; 95% CI, 0.6%-2.6%) in 2001 to 21 of 1669 (1.3%; 95% CI, 0.8%-1.9%) in 2012 (P = .17). Thirty-day survival after bystander defibrillation increased in public locations from 8.3% (95% CI, 1.5%-35.4%) in 2001/2002 to 57.5% (95% CI, 48.6%-66.0%) in 2011/2012 (P < .001) in residential locations, from 0.0% (95% CI, 0.0%-19.4%) in 2001/2002 to 25.6% (95% CI, 14.6%-41.1%) in 2011/2012 (P < .001).
Conclusions and Relevance
Initiatives to facilitate bystander defibrillation were associated with a marked increase in bystander defibrillation in public locations, whereas bystander defibrillation remained limited in residential locations. Concomitantly, survival increased after bystander defibrillation in residential and public locations.
Introduction
The placement of automated external defibrillators (AEDs) in public places, such as airports, sport facilities, offices, casinos, and aircrafts, is associated with survival rates of out-of-hospital cardiac arrest (OHCA) as high as 74%. Consequently, based on recommendations from the American Heart Association and the European Resuscitation Council, AEDs have been broadly distributed in many countries.
Although cardiopulmonary resuscitation (CPR) performed by bystanders has increased in many countries, defibrillation performed by bystanders (hereinafter referred to as bystander defibrillation) remains limited in broader populations, and strategies for increasing bystander defibrillation are warranted. The limited rates of bystander defibrillation have been associated with logistical barriers to AED use, such as the placement of AEDs in areas with low incidences of cardiac arrests, limited accessibility to AEDs, and difficulties with finding or remembering to use AEDs at the time of the cardiac arrest. Thus, increasing bystander defibrillation rates depends on improving the strategic placement and accessibility of AEDs and on enhancing the ability of bystanders to locate and use a nearby AED. Furthermore, the location of the cardiac arrest must be considered when designing strategies to promote bystander defibrillation. In general, the conditions for early bystander defibrillation are less favorable in residential than in public locations because factors associated with a nonshockable heart rhythm are more frequent in residential locations, such as a greater number of unwitnessed arrests, less performance of bystander CPR, and older patients with more comorbidities. Consequently, the effect of strategies aimed to improve early defibrillation are likely to differ according to the location of arrest, and different approaches might be needed.
In Denmark, initiatives to facilitate bystander defibrillation have been undertaken, including dissemination of on-site AEDs, registration of the AEDs with location information linked to emergency dispatch centers, dispatcher-assisted guidance to their use, and increased education of the lay public in performing resuscitation. We aimed to examine (1) temporal changes in bystander defibrillation according to the location of cardiac arrest and (2) temporal changes in survival according to bystander defibrillation and location of arrest.
Methods
Setting
This nationwide cohort study included data collected from June 1, 2001, to December 31, 2012, in Denmark. Denmark has approximately 5.6 million inhabitants and covers 42 900 km2 (approximately 16 565 square miles). This study was approved by the Danish Data Protection Agency. Ethical approval is not required for retrospective registry-based studies in Denmark (https://www.retsinformation.dk/Forms/R0710.aspx?id=137674).
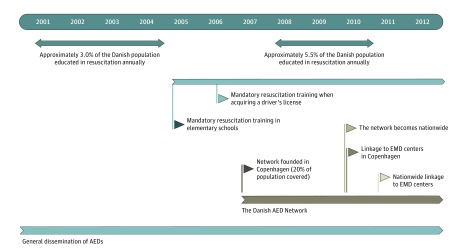
Initiatives to Increase AED Availability, Awareness, and Use
Several initiatives have been undertaken to strengthen bystander resuscitative efforts and AED use in Denmark. In 2007, the Danish AED Network was established in Copenhagen and became nationwide in 2010. In February of 2010, AED location information was integrated with emergency medical dispatch centers in Copenhagen and instituted nationwide in 2011. In addition, the locations of registered AEDs have been publicly available on the AED Network homepage since 2007 and via a smartphone app since 2012, allowing citizens to locate nearby AEDs. The Danish Health and Medicines Authority issued official recommendations for the dissemination, strategic placement, and accessibility of AEDs in 2011. Efforts were taken to strengthen bystander resuscitation attempts, including mandatory resuscitation training in elementary schools (2005) and when acquiring a driver’s license (2006). The number of annually distributed first aid certificates increased from about 175 000 in 2001 to 2004 to about 300 000 in 2008 to 2011. Since 2011, emergency medical dispatch centers have been staffed nationwide with health care professionals, and dispatchers have followed a standardized nationwide protocol to provide guidance to bystanders to perform CPR and retrieve a nearby registered AED when a cardiac arrest is suspected. The accumulated number of AEDs sold in Denmark was estimated at 3000 in 2006 and 15 000 in 2011. Finally, public campaigns were launched to increase AED knowledge and awareness. Figure 1 provides an overview of the most important initiatives during the study period.
Figure 1. Overview of Initiatives Undertaken in Denmark to Facilitate Bystander Resuscitative Efforts, Including Bystander Defibrillation.
AED indicates automated external defibrillator; EMD, emergency medical dispatch.
OHCA, Study Variables, and Study Population
Emergency medical services personnel are activated for all suspected OHCAs, and in case of a cardiac arrest, they are subsequently required to complete a short case report for the Danish Cardiac Arrest Registry based on the Utstein template. An OHCA is included in the registry when a clinical condition of cardiac arrest has resulted in resuscitative efforts by emergency medical service personnel or bystanders. This definition excludes cases with obvious late signs of death for which resuscitation is not initiated. The Danish Cardiac Arrest Registry has been described in detail.
In Denmark, each citizen is assigned a unique civil registration number, allowing individual-level linkage of information between nationwide registries. We retrieved the following data from the Danish Cardiac Arrest Registry: the date of arrest; whether the arrest was bystander witnessed, nonwitnessed, or witnessed by emergency medical services personnel; public or residential location; whether bystander CPR or bystander defibrillation was performed; the estimated interval from the recognition of the arrest to the first rhythm analysis by the emergency medical service personnel; the first recognized rhythm (shockable or nonshockable); and the patient’s status on hospital arrival. Using the civil registration number of each person in the study population, we obtained data regarding age, sex, and survival status from the Danish National Population Registry. Admission dates, discharge dates, and discharge diagnoses from hospitals were retrieved from the Danish National Patient Registry. We retrieved the causes of death from the Danish Registry of Causes of Death. Discharge diagnoses and causes of death were available according to the World Health Organization International Classification of Diseases and Related Health Problems, Tenth Revision.
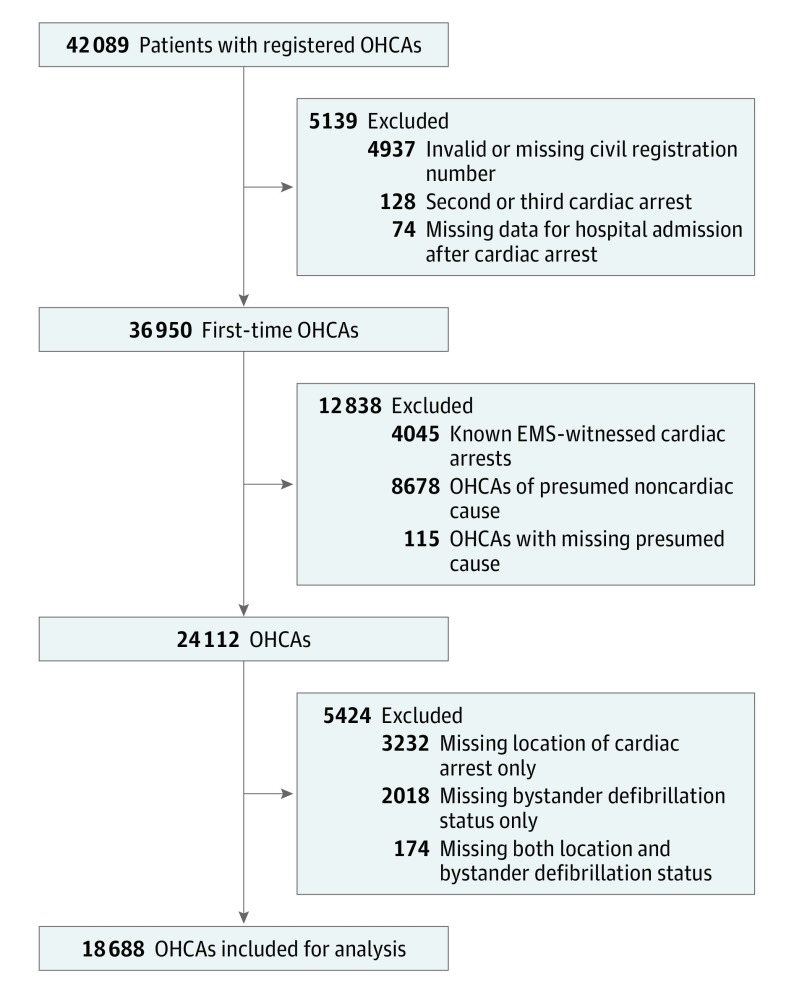
Death certificates or discharge diagnosis codes were used to define the presumed cause of cardiac arrest. Death certificates and discharge diagnoses of cardiac disease, unknown disease, or unexpected collapse were defined as presumed cardiac cause of arrest. Death certificates and discharge diagnoses without the above-mentioned diagnoses but showing other medical disorders were defined as noncardiac causes. Trauma, drug overdose, attempted suicide, and violent assault were considered to be noncardiac causes regardless of other diagnoses. For this study, we excluded patients with OHCA and (1) an invalid civil registration number (including foreigners without permanent residence in Denmark), (2) a second or third cardiac arrest, (3) cardiac arrests without registered hospital admission, (4) cardiac arrests that were witnessed by emergency medical services, (5) cardiac arrests with missing information about location and/or bystander defibrillation, and (6) arrests due to a presumed noncardiac cause (Figure 2).
Figure 2. Flowchart Showing the Study Population With Out-of-Hospital Cardiac Arrest (OHCA).
EMS indicates emergency medical service.
Registered AEDs
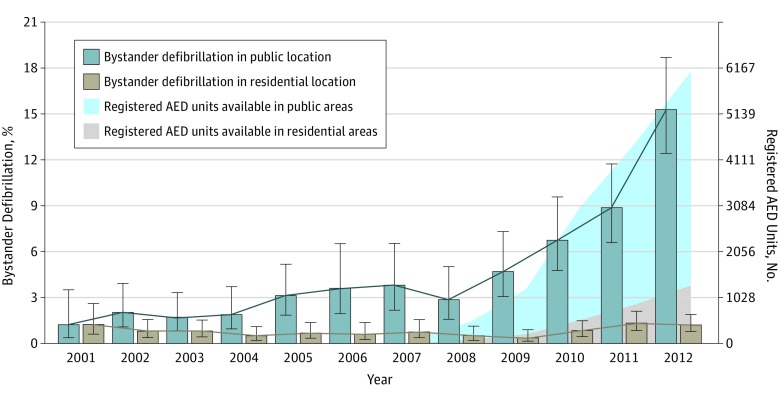
To determine the location of each registered AED, we used the geocoded location of the AED according to publicly available municipal land-use plans. A detailed description is available in eMethods in the Supplement. Locations of AEDs were classified into the following 3 groups: (1) residential areas (private homes cover >80% of the parcels), (2) mixed residential and public areas (20%-80% of the parcels consist of private homes mixed with buildings used for business), and (3) public areas (eg, educational buildings, health care institutions, shopping areas, business areas, and recreational areas). In Figure 3, residential areas were defined as residential and mixed residential and public areas.
Figure 3. Bystander Defibrillation According to the Location of the Out-of-Hospital Cardiac Arrest (OHCA) and Registered Automated External Defibrillator (AED) Units.
The proportion of patients with OHCAs who underwent defibrillation by bystanders according to the calendar year (2001-2012) in residential and public locations. Shaded areas indicate the number of registered AED units over time. Error bars indicate 95% CIs.
Study Outcomes
The primary outcome measure was the rate of bystander defibrillation according to the location of the cardiac arrest from 2001 to 2012. This outcome only included patients who had a shock delivered and not those who had AED pads applied but no shock delivered. The secondary outcome measure was 30-day survival according to the location of the arrest and bystander defibrillation status.
Statistical Analysis
Data were analyzed from April 1, 2015, to December 10, 2016. Calendar trends in bystander defibrillation for cardiac arrests in public and residential locations were analyzed separately using univariate logistic regression. The calendar changes in 30-day survival, with or without bystander defibrillation for each location, were modeled using logistic regression and restricted cubic splines (with prespecified knots at 2004, 2007, and 2011).
We analyzed whether missing data on bystander defibrillation and/or the location of the arrest (excluded patients) could have introduced bias by comparing the results from complete case analyses with the results based on multiple imputation. Specifically, we imputed 100 data sets using the calendar year and the information in the Table and compared the mean bystander defibrillation probability with the complete case results according to the calendar year and the location of the arrest. Data management and analyses were performed using SAS (version 9.4; SAS Institute Inc) and R software. A 2-sided P < .05 was considered statistically significant. For trend tests, we used the univariate logistic regression.
Table. Baseline Characteristics and Survival Among Patients With OHCAs in Denmark According to Location and Whether Bystander Defibrillation Was Performeda.
| Variable | Location of OHCA | All (n = 18 688) |
Missing Data | |||
|---|---|---|---|---|---|---|
| Residential | Public | |||||
| Bystander Defibrillation (n = 117) |
No Bystander Defibrillation (n = 13 788) |
Bystander Defibrillation (n = 243) |
No Bystander Defibrillation (n = 4540) |
|||
| Age, median (IQR), y | 68 (58-77) | 73 (63-81) | 64 (53-73) | 68 (58-78) | 72 (62-80) | 0 |
| Males | 84 (71.8) | 8913 (64.6) | 220 (90.5) | 3459 (76.2) | 12 676 (67.8) | 0 |
| OHCA characteristics | ||||||
| Bystander CPR | 99 (84.6) | 4377 (31.8) | 229 (94.2) | 2428 (53.6) | 7133 (38.2) | 47 |
| Bystander-witnessed arrest | 82 (70.1) | 6475 (47.2) | 203 (83.5) | 2999 (66.5) | 9759 (52.2) | 103 |
| Shockable heart rhythm | 117 (100) | 2859 (21.6) | 243 (100) | 1976 (45.0) | 5195 (27.8) | 722 |
| Time interval, median (IQR), minb | 15.0 (10.0-21.0) | 12.0 (7.0-20.0) | 13.0 (8.0-17.0) | 10.0 (6.0-15.0) | 11.0 (7.0-19.0) | 1771 |
| Comorbidity | ||||||
| Ischemic heart disease (MI not included) | 36 (30.8) | 3597 (26.1) | 59 (24.3) | 1111 (24.5) | 4803 (25.7) | 0 |
| Previous MI | 16 (13.7) | 1747 (12.7) | 36 (14.8) | 531 (11.7) | 2330 (12.5) | 0 |
| Heart failure | 29 (24.8) | 2987 (21.7) | 42 (17.3) | 823 (18.1) | 3881 (20.8) | 0 |
| COPD | 14 (12.0) | 2239 (16.2) | 6 (2.5) | 422 (9.3) | 2681 (14.3) | 0 |
| Malignant disease | 13 (11.1) | 1698 (12.3) | 15 (6.2) | 406 (8.9) | 2132 (11.4) | 0 |
| Renal disease | 2 (1.7) | 715 (5.2) | 6 (2.5) | 153 (3.4) | 876 (4.7) | 0 |
| Survival | ||||||
| ROSC at hospital arrival | 42 (37.2) | 1702 (12.6) | 133 (56.4) | 1121 (25.1) | 2998 (16.0) | 347 |
| 30-d Survival | 23 (19.7) | 660 (4.8) | 114 (46.9) | 676 (14.9) | 1473 (7.9) | 0 |
Abbreviations: COPD, chronic obstructive pulmonary disease; CPR, cardiopulmonary resuscitation; IQR, interquartile range; MI, myocardial infarction; OHCA, out-of-hospital cardiac arrest; ROSC, return of spontaneous circulation.
Data are presented as number (percentage) of patients unless otherwise indicated. Data were collected from June 1, 2001, to December 31, 2012.
Indicates estimated time from recognition of the arrest to the first rhythm analysis by the emergency medical services personnel.
Results
A total of 18 688 patients with OHCAs (67.8% men and 32.2% women; median [interquartile range] age, 72 [62-80] years) were included in the study (Figure 2). The patient characteristics according to the location of arrest and bystander defibrillation are shown in the Table. A total of 4783 (25.6%) OHCAs occurred in public locations, and 13 905 (74.4%) occurred in residential locations. The patients who underwent bystander defibrillation in public locations (243 [5.1%]) were younger and more frequently male, had fewer chronic diseases, had more witnessed arrests, and received bystander CPR more often compared with patients undergoing defibrillation in residential locations (117 [0.8%]). For both locations, the patients who underwent defibrillation were younger and more frequently male, had fewer chronic diseases, had more witnessed arrests, and received bystander CPR more often compared with patients who did not undergo defibrillation.
Bystander defibrillation increased markedly in public locations from 3 of 245 (1.2%; 95% CI, 0.4%-3.5%) in 2001 to 78 of 510 (15.3%; 95% CI, 12.4%-18.7%) in 2012 (P < .001); in residential locations, bystander defibrillation remained unchanged and limited from 7 of 542 (1.3%; 95% CI, 0.6%-2.6%) in 2001 to 21 of 1669 (1.3%; 95% CI, 0.8%-1.9%) in 2012 (P = .17) (Figure 3). eTable 1 in the Supplement shows the absolute numbers of patients who underwent defibrillation each year according to location. Registered AED units in the Danish AED Network increased from 141 in 2007 to 7800 in 2012. Over time, the distribution of AED location was consistently skewed in favor of public locations. eTable 2 in the Supplement shows the registered AED units and estimated AED units sold.
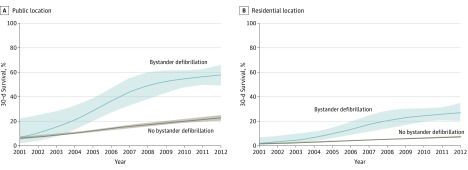
Thirty-day survival increased among patients undergoing defibrillation in public locations from 8.3% (95% CI, 1.5%-35.4%) in 2001/2002 to 57.5% (95% CI, 48.6%-66.0%) in 2011/2012 (P < .001); for patients undergoing defibrillation in residential locations, 30-day survival increased from 0.0% (95% CI, 0.0%-19.4%) in 2001/2002 to 25.6% (95% CI, 14.6%-41.1%) in 2011/2012 (P < .001). In both locations, survival increased more over time for patients undergoing defibrillation by bystanders than for patients who did not (Figure 4). For patients undergoing defibrillation by bystanders, an increase in bystander CPR was observed over time from 72.6% in 2001 to 92.0% in 2007 and 98.4% in 2012 in public locations and from 58.4% in 2001 to 85.9% in 2007 and 97.1% in 2012 in residential locations (eFigure 1 in the Supplement).
Figure 4. 30-Day Survival According to the Location of the Out-of-Hospital Cardiac Arrest (OHCA) and Performance of Bystander Defibrillation.
The 30-day survival among patients with OHCAs in public vs residential locations according to whether the patients underwent defibrillation by bystanders. The results from logistic regression were not adjusted for patient characteristics, and restricted cubic splines were used to model changes in calendar time. Shaded areas indicate 95% CIs.
Additional Analyses
When our study population was restricted to patients with a witnessed arrest of presumed cardiac cause and a first shockable rhythm, bystander defibrillation increased in public locations from 1 of 95 (1.1%; 95% CI, 0.2%-5.7%) in 2001 to 66 of 210 (31.4%; 95% CI, 25.5%-38.0%) in 2012 (P < .001) and in residential locations from 2 of 87 (2.3%; 95% CI, 0.6%-8.0%) in 2001 to 18 of 251 (7.2%; 95% CI, 4.6%-11.0%) in 2012 (P = .06) (eFigure 2 in the Supplement). When all OHCAs were considered irrespective of presumed cause, bystander defibrillation increased in public locations from 5 of 350 (1.4%; 95% CI, 0.6%-3.3%) in 2001 to 84 of 707 (11.9%; 95% CI, 9.7%-14.5%) in 2012 (P < .001) and in residential locations from 12 of 770 (1.6%; 95% CI, 0.9%-2.7%) in 2001 to 23 of 2368 (1.0%; 95% CI, 0.6%-1.5%) in 2012 (P = .72) (eFigure 3 in the Supplement). Multiple imputation analysis indicated that the exclusion of the patients with missing data did not affect the observed changes in bystander defibrillation (eFigure 4 in the Supplement). eTable 3 in the Supplement shows the patient characteristics of excluded patients (n = 5424) compared with included patients (n = 18 688).
Discussion
This nationwide study showed that national initiatives to facilitate bystander defibrillation using on-site AEDs were associated with an increase in bystander defibrillation of patients with OHCAs from 1.2% in 2001 to 15.3% in 2012 in public locations, whereas bystander defibrillation remained limited in residential locations during the entire study period. In addition, bystander defibrillation was associated with an increase in survival over time for both locations. Furthermore, survival after bystander defibrillation increased over time irrespective of location.
Few studies have assessed the association between bystander defibrillation and publicly available AEDs, likely owing to uncertainties about the quantity or the location of AEDs. Kitamura et al reported an association between a large increase in AED wholesale purchases and an increase in bystander defibrillation from 1.1% to 16.5% during a 9-year period. However, only patients with a witnessed arrest of presumed cardiac cause and a shockable rhythm were considered in the analysis. Such restrictions, with the exclusion of most patients who might benefit from a public AED, seem problematic and could distance the results from real-life settings. Thus, patients with a nonshockable rhythm at the arrival of emergency medical services might have had a shockable rhythm if an AED had been applied earlier, and patients with an unwitnessed arrest are clearly still eligible for bystander resuscitative efforts, including potential defibrillation from an AED before the arrival of emergency medical services. In addition, unlike the present study, details concerning the location of the cardiac arrest and bystander defibrillation were not available, with a risk for overlooking important details; that is, different public access defibrillation strategies are probably needed in residential locations, where conditions for bystander defibrillation in general are less favorable. Furthermore, during our study period, several initiatives were taken to facilitate bystander defibrillation in addition to general AED dissemination. These initiatives could be considered when organizing public-access defibrillation strategies.
The present study showed that, although most OHCAs occurred in residential locations (74.4%), no increase in bystander defibrillation occurred in residential areas. One possible explanation is that only 17.4% of the registered AEDs were located in residential areas; furthermore, some AEDs might have been inaccessible to bystanders at a nearby cardiac arrest. In addition, patients with OHCAs in residential locations were older, had more chronic diseases, had fewer bystander-witnessed arrests, and underwent bystander CPR less often than patients with OHCAs in public locations. These factors are thought to reduce the chance of a shockable heart rhythm and therefore limit the potential benefit of early defibrillation in residential areas. A previous study reported that, although 41% of all bystander-applied AEDs were in private locations, only 24% of all delivered shocks occurred in private locations, supporting the notion that a lack of shockable heart rhythm is an important limiting factor. A lack of a shockable rhythm is also likely to have contributed to the low defibrillation rate in residential locations in our study, although our study was limited in that it had no data about applied AEDs when no shock was delivered. Our findings support previous observations that the use of on-site AEDs in residential areas seems very limited, even when AED location information is available to emergency medical dispatch centers. To increase bystander defibrillation, recent studies have described strategies in which first responders trained in resuscitation are equipped with AEDs with the chance of providing early defibrillation irrespective of residential or public cardiac arrest location. In addition, training of citizens in performing resuscitation could increase bystander resuscitative efforts further, including those in residential locations. Our study supports the idea that in residential areas, new initiatives, such as first-responder programs, should be considered to increase early interventions that allow a shock to be delivered before the heart rhythm degrades to a nonshockable rhythm.
We found that 30-day survival after bystander defibrillation increased in public and residential locations over time, and at the end of our study period, the survival rate in a public, nonselected national environment was as high as that reported in highly selected environments, such as casinos and airports. Survival in both locations increased during the study period. Of note, patient survival without bystander defibrillation also increased during the study period. This indicates that factors other than early defibrillation are important for increasing survival, such as an increase in bystander CPR, which was observed among the patients who underwent bystander defibrillation and improved advanced postresuscitation care. Such improvements have previously been associated with an increase in survival after OHCA in general and in patients undergoing bystander defibrillation in particular. Furthermore, in our study, patients in public and residential locations who underwent bystander defibrillation had additional characteristics that favored higher survival rates compared with patients who did not undergo defibrillation. When we examined the increase in bystander defibrillation and survival after bystander defibrillation, the incidence of OHCAs in Denmark did not change during the study period, reducing the possibility that changes in reporting over time affected our results (eFigure 5 in the Supplement).
Limitations
First, because of its observational design, the study could not interpret the effect of each individual initiative on the increase in bystander defibrillation. In addition, the design precludes assurance that the higher survival rate in patients undergoing bystander defibrillation was due to the increased AED use alone because we cannot exclude the possibility that bystander defibrillation was associated with unmeasured factors that favored high survival, such as higher-quality CPR and more aggressive post–cardiac arrest care. Furthermore, we did not have reliable data on time to bystander defibrillation, which might have decreased during the study period.
Second, only data from registered AEDs in the AED Network were available. As such, the exact number and the actual distribution of all AEDs in public and residential locations are unknown. However, the reported number of registered AEDs can only be an underestimation of the actual number of AEDs in residential locations. Consequently, this limitation does not change our conclusion that, despite several initiatives, including placement of AEDs in residential areas, no increase occurred in bystander defibrillation in residential locations.
Third, data on the exact geographic locations of the cardiac arrests were not available, and we cannot analyze the distance to the nearest registered AED for each cardiac arrest. Fourth, patients with missing data on bystander defibrillation and/or on the location of the arrest were excluded. However, a sensitivity analysis that included these patients did not change our conclusions.
Conclusions
Dissemination and registration of on-site public AEDs with dispatcher-assisted guidance to use them and education of laypersons in performing resuscitation were associated with a marked increase in bystander defibrillation in public locations. However, bystander defibrillation remained limited in residential locations. Concomitantly, survival increased after bystander defibrillation in residential and public locations.
eMethods. Location of Automated External Defibrillators
eTable 1. Defibrillation of Cardiac Arrest Patients in Denmark According to Location, 2001-2012
eTable 2. Cumulative Number of Registered AEDs According to Location and the Estimated Total Number of AED Units Sold in Denmark, 2007-2012
eTable 3. Baseline Characteristics and Survival of the Patients With Out-of-Hospital Cardiac Arrest Included for Analysis (n = 18 688) and of Patients Excluded Due to Missing Data on the Location of Arrest and/or Bystander Defibrillation (n = 5424)
eFigure 1. Bystander CPR Performed During the Study Period 2001-2012 for Patients Receiving Bystander Defibrillation
eFigure 2. Bystander Defibrillation for Public and Residential Locations From 2001-2012 for Patients With a Bystander-Witnessed OHCA of Presumed Cardiac Cause and a Shockable Rhythm (n = 3972)
eFigure 3. Bystander Defibrilltion for Public and Residential Locations From 2001-2012 for Patients With a Non–EMS-Witnessed OHCA, Irrespective of Presumed Cause
eFigure 4. Multiple Imputation vs Complete Case Analysis of Bystander Defibrillation Probability According to the Location of Out-of-Hospital Cardiac Arrest in Denmark
eFigure 5. Incidence of OHCAs per 100 000 Danish Citizens From 2001-2012 for All Non–EMS-Witnessed OHCAs and Non–EMS-Witnessed OHCAs of Presumed Cardiac Cause
References
- 1.Caffrey SL, Willoughby PJ, Pepe PE, Becker LB. Public use of automated external defibrillators. N Engl J Med. 2002;347(16):1242-1247. [DOI] [PubMed] [Google Scholar]
- 2.Valenzuela TD, Roe DJ, Nichol G, Clark LL, Spaite DW, Hardman RG. Outcomes of rapid defibrillation by security officers after cardiac arrest in casinos. N Engl J Med. 2000;343(17):1206-1209. [DOI] [PubMed] [Google Scholar]
- 3.Page RL, Joglar JA, Kowal RC, et al. . Use of automated external defibrillators by a US airline. N Engl J Med. 2000;343(17):1210-1216. [DOI] [PubMed] [Google Scholar]
- 4.Kitamura T, Kiyohara K, Sakai T, et al. . Public-access defibrillation and out-of-hospital cardiac arrest in Japan. N Engl J Med. 2016;375(17):1649-1659. [DOI] [PubMed] [Google Scholar]
- 5.Link MS, Atkins DL, Passman RS, et al. . 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care: part 6: electrical therapies: automated external defibrillators, defibrillation, cardioversion, and pacing. Circulation. 2010;122(18)(suppl 3):S706-S719. [DOI] [PubMed] [Google Scholar]
- 6.Perkins GD, Handley AJ, Koster RW, et al. ; Adult basic life support and automated external defibrillation section Collaborators . European Resuscitation Council Guidelines for Resuscitation 2015, section 2: adult basic life support and automated external defibrillation. Resuscitation. 2015;95:81-99. [DOI] [PubMed] [Google Scholar]
- 7.Chan PS, McNally B, Tang F, Kellermann A; CARES Surveillance Group . Recent trends in survival from out-of-hospital cardiac arrest in the United States. Circulation. 2014;130(21):1876-1882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wissenberg M, Lippert FK, Folke F, et al. . Association of national initiatives to improve cardiac arrest management with rates of bystander intervention and patient survival after out-of-hospital cardiac arrest. JAMA. 2013;310(13):1377-1384. [DOI] [PubMed] [Google Scholar]
- 9.Daya MR, Schmicker RH, Zive DM, et al. ; Resuscitation Outcomes Consortium Investigators . Out-of-hospital cardiac arrest survival improving over time: results from the Resuscitation Outcomes Consortium (ROC). Resuscitation. 2015;91:108-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Deakin CD, Shewry E, Gray HH. Public access defibrillation remains out of reach for most victims of out-of-hospital sudden cardiac arrest. Heart. 2014;100(8):619-623. [DOI] [PubMed] [Google Scholar]
- 11.Graham R, Mccoy MA, Schultz AM Strategies to improve cardiac arrest survival: a time to act. http://iom.nationalacademies.org/Reports/2015/Strategies-to-Improve-Cardiac-Arrest-Survival.aspx. Released June 30, 2015. Accessed December 11, 2016. [PubMed]
- 12.Folke F, Lippert FK, Nielsen SL, et al. . Location of cardiac arrest in a city center: strategic placement of automated external defibrillators in public locations. Circulation. 2009;120(6):510-517. [DOI] [PubMed] [Google Scholar]
- 13.Hansen CM, Wissenberg M, Weeke P, et al. . Automated external defibrillators inaccessible to more than half of nearby cardiac arrests in public locations during evening, nighttime, and weekends. Circulation. 2013;128(20):2224-2231. [DOI] [PubMed] [Google Scholar]
- 14.Brooks B, Chan S, Lander P, Adamson R, Hodgetts GA, Deakin CD. Public knowledge and confidence in the use of public access defibrillation. Heart. 2015;101(12):967-971. [DOI] [PubMed] [Google Scholar]
- 15.Folke F, Gislason GH, Lippert FK, et al. . Differences between out-of-hospital cardiac arrest in residential and public locations and implications for public-access defibrillation. Circulation. 2010;122(6):623-630. [DOI] [PubMed] [Google Scholar]
- 16.Zijlstra JA, Stieglis R, Riedijk F, Smeekes M, van der Worp WE, Koster RW. Local lay rescuers with AEDs, alerted by text messages, contribute to early defibrillation in a Dutch out-of-hospital cardiac arrest dispatch system. Resuscitation. 2014;85(11):1444-1449. [DOI] [PubMed] [Google Scholar]
- 17.Ringh M, Jonsson M, Nordberg P, et al. . Survival after public access defibrillation in Stockholm, Sweden—a striking success. Resuscitation. 2015;91:1-7. [DOI] [PubMed] [Google Scholar]
- 18.Danish Foundation TrygFonden Hjertestarter.dk. https://www.hjertestarter.dk/english. Accessed December 11, 2016.
- 19.Hansen CM, Lippert FK, Wissenberg M, et al. . Temporal trends in coverage of historical cardiac arrests using a volunteer-based network of automated external defibrillators accessible to laypersons and emergency dispatch centers. Circulation. 2014;130(21):1859-1867. [DOI] [PubMed] [Google Scholar]
- 20.Jacobs I, Nadkarni V, Bahr J, et al. ; International Liaison Committee on Resuscitation; American Heart Association; European Resuscitation Council; Australian Resuscitation Council; New Zealand Resuscitation Council; Heart and Stroke Foundation of Canada; InterAmerican Heart Foundation; Resuscitation Councils of Southern Africa; ILCOR Task Force on Cardiac Arrest and Cardiopulmonary Resuscitation Outcomes . Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation. Circulation. 2004;110(21):3385-3397. [DOI] [PubMed] [Google Scholar]
- 21.van Buuren S, Groothuis-Oudshoorn K. mice: Multivariate imputation by chained equations in R. J Stat Softw. 2011;45(3):67. [Google Scholar]
- 22.R Core Team R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2015. [Google Scholar]
- 23.Weisfeldt ML, Everson-Stewart S, Sitlani C, et al. ; Resuscitation Outcomes Consortium Investigators . Ventricular tachyarrhythmias after cardiac arrest in public versus at home. N Engl J Med. 2011;364(4):313-321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Weisfeldt ML, Sitlani CM, Ornato JP, et al. ; ROC Investigators . Survival after application of automatic external defibrillators before arrival of the emergency medical system: evaluation in the Resuscitation Outcomes Consortium population of 21 million. J Am Coll Cardiol. 2010;55(16):1713-1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bardy GH, Lee KL, Mark DB, et al. ; HAT Investigators . Home use of automated external defibrillators for sudden cardiac arrest. N Engl J Med. 2008;358(17):1793-1804. [DOI] [PubMed] [Google Scholar]
- 26.Blom MT, Beesems SG, Homma PCM, et al. . Improved survival after out-of-hospital cardiac arrest and use of automated external defibrillators. Circulation. 2014;130(21):1868-1875. [DOI] [PubMed] [Google Scholar]
- 27.Hasselqvist-Ax I, Riva G, Herlitz J, et al. . Early cardiopulmonary resuscitation in out-of-hospital cardiac arrest. N Engl J Med. 2015;372(24):2307-2315. [DOI] [PubMed] [Google Scholar]
- 28.Hallstrom AP, Ornato JP, Weisfeldt M, et al. ; Public Access Defibrillation Trial Investigators . Public-access defibrillation and survival after out-of-hospital cardiac arrest. N Engl J Med. 2004;351(7):637-646. [DOI] [PubMed] [Google Scholar]
- 29.Sunde K, Pytte M, Jacobsen D, et al. . Implementation of a standardised treatment protocol for post resuscitation care after out-of-hospital cardiac arrest. Resuscitation. 2007;73(1):29-39. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods. Location of Automated External Defibrillators
eTable 1. Defibrillation of Cardiac Arrest Patients in Denmark According to Location, 2001-2012
eTable 2. Cumulative Number of Registered AEDs According to Location and the Estimated Total Number of AED Units Sold in Denmark, 2007-2012
eTable 3. Baseline Characteristics and Survival of the Patients With Out-of-Hospital Cardiac Arrest Included for Analysis (n = 18 688) and of Patients Excluded Due to Missing Data on the Location of Arrest and/or Bystander Defibrillation (n = 5424)
eFigure 1. Bystander CPR Performed During the Study Period 2001-2012 for Patients Receiving Bystander Defibrillation
eFigure 2. Bystander Defibrillation for Public and Residential Locations From 2001-2012 for Patients With a Bystander-Witnessed OHCA of Presumed Cardiac Cause and a Shockable Rhythm (n = 3972)
eFigure 3. Bystander Defibrilltion for Public and Residential Locations From 2001-2012 for Patients With a Non–EMS-Witnessed OHCA, Irrespective of Presumed Cause
eFigure 4. Multiple Imputation vs Complete Case Analysis of Bystander Defibrillation Probability According to the Location of Out-of-Hospital Cardiac Arrest in Denmark
eFigure 5. Incidence of OHCAs per 100 000 Danish Citizens From 2001-2012 for All Non–EMS-Witnessed OHCAs and Non–EMS-Witnessed OHCAs of Presumed Cardiac Cause