This study of all delivery admissions in the California State Inpatient Database compares maternal and fetal risks and outcomes between women with and without congenital heart disease.
Key Points
Question
How do the risks and outcomes for labor and delivery compare in women with and without congenital heart disease?
Findings
In this study capturing nearly every delivery admission in California during a 7-year period, congenital heart disease was associated with incident heart failure, atrial arrhythmias, fetal growth restriction, and readmission; complex congenital heart disease was also associated with ventricular arrhythmias and maternal in-hospital mortality, although these outcomes were rare, even in women with congenital heart disease.
Meaning
This study highlights some of the peripartum and postpartum risks for women with CHD, findings that may guide monitoring decisions and risk assessment for pregnant women with CHD at the time of delivery.
Abstract
Background
Women with congenital heart disease (CHD) may be at increased risk for adverse events during pregnancy and delivery.
Objective
To compare delivery outcomes between women with and without CHD.
Design, Setting, and Participants
This retrospective study of inpatient delivery admissions in the Healthcare Cost and Utilization Project’s California State Inpatient Database compared maternal and fetal outcomes between women with and without CHD by using multivariate logistic regression. Female patients with codes for delivery from the International Classification of Diseases, Ninth Revision, from January 1, 2005, through December 31, 2011, were included. The association of CHD with readmission was assessed to 7 years after delivery. Cardiovascular morbidity and mortality were hypothesized to be higher among women with CHD. Data were analyzed from April 4, 2014, through January 23, 2017.
Exposures
Noncomplex and complex CHD.
Main Outcomes and Measures
Maternal outcomes included in-hospital arrhythmias, eclampsia or preeclampsia, congestive heart failure (CHF), length of stay, preterm labor, anemia complicating pregnancy, placental abnormalities, infection during labor, maternal readmission at 1 year, and in-hospital mortality. Fetal outcomes included growth restriction, distress, and death.
Results
Among 3 642 041 identified delivery admissions, 3189 women had noncomplex CHD (mean [SD] age, 28.6 [7.6] years) and 262 had complex CHD (mean [SD] age, 26.5 [6.8] years). Women with CHD were more likely to undergo cesarean delivery (1357 [39.3%] vs 1 164 509 women without CHD [32.0%]; P < .001). Incident CHF, atrial arrhythmias, ventricular arrhythmias, and maternal mortality were uncommon during hospitalization, with each occurring in fewer than 10 women with noncomplex or complex CHD (<0.5% each). After multivariate adjustment, noncomplex CHD (odds ratio [OR], 9.7; 95% CI, 4.7-20.0) and complex CHD (OR, 56.6; 95% CI, 17.6-182.5) were associated with greater odds of incident CHF. Similar odds were found for atrial arrhythmias in noncomplex (OR, 8.2; 95% CI, 3.0-22.7) and complex (OR, 31.8; 95% CI, 4.3-236.3) CHD, for fetal growth restriction in noncomplex (OR, 1.6; 95% CI, 1.3-2.0) and complex (OR, 3.5; 95% CI, 2.1-6.1) CHD, and for hospital readmission in both CHD groups combined (OR, 3.6; 95% CI, 3.3-4.0). Complex CHD was associated with greater adjusted odds of serious ventricular arrhythmias (OR, 31.8; 95% CI, 4.3-236.3) and maternal in-hospital mortality (OR, 79.1; 95% CI, 23.9-261.8).
Conclusions and Relevance
In this study of hospital admissions for delivery in California, CHD was associated with incident CHF, atrial arrhythmias, and fetal growth restriction and complex CHD was associated with ventricular arrhythmias and maternal in-hospital mortality, although these outcomes were rare, even in women with complex CHD. These findings may guide monitoring decisions and risk assessment for pregnant women with CHD at the time of delivery.
Introduction
Labor, delivery, and the postpartum period are a time of increased arrhythmia and heart failure incidences, even in patients without cardiovascular disease. Possible explanations include altered hemodynamics with myocardial irritability owing to increases in intravascular volume, hypokalemia, autonomic changes, and hormonal influences on adrenergic receptor number and behavior. Maternal arrhythmias increase during labor and delivery, possibly owing to volume shifts and hypertension. In women with arrhythmias before pregnancy, recurrence during pregnancy is common and is associated with an increased risk for fetal complications. Despite these risks, a small series including women with implantable cardioverter defibrillators followed up during subsequent pregnancies has revealed no increase in implantable cardioverter defibrillator shocks. Likewise, congestive heart failure (CHF) is more common during and after pregnancy in women without a history of cardiovascular disease.
Owing to improvements in the treatment of congenital heart disease (CHD), most patients with CHD now survive to adulthood, and more than 1 million adults are living with CHD in the United States. As patients with CHD live longer, arrhythmias are an increasing cause of morbidity and mortality. In addition, more women with CHD are becoming pregnant, and these patients are at increased risk for arrhythmias and CHF.
We sought to evaluate contemporary maternal and fetal outcomes in women with and without CHD during admissions for delivery in California. We used the Health Care Cost and Utilization Project (HCUP), a group of databases that have already been used to study CHD hospitalizations and procedures, to evaluate cardiac and other complications of labor and delivery for women with and without CHD from 2005 through 2011.
Methods
Admissions for female patients with a diagnosis code from the International Classification of Diseases, Ninth Revision (ICD-9), a procedure code from the International Classification of Diseases, Ninth Revision, Clinical Modification, or a diagnosis related group code for delivery from January 1, 2005, through December 31, 2011, were identified from HCUP’s California State Inpatient Database. If an ICD-9 code for cesarean delivery was not present and the delivery type was not specified, delivery was categorized as vaginal. The details of the ICD-9 codes used are listed in eTable 1 in the Supplement. Identifying patient information was anonymized before analysis, and certification to use these deidentified HCUP data was obtained from the Committee on Human Research at the University of California, San Francisco.
Diagnoses of CHD were determined by ICD-9 or Current Procedural Terminology codes used by others previously (eTable 2 in the Supplement). If a CHD diagnosis code was present for any encounter during the study period, the patient was assigned that diagnosis for all visits. Complex CHD included endocardial cushion defects, hypoplastic left heart syndrome, tetralogy of Fallot, transposition of the great arteries, truncus arteriousus, and univentricular heart defects. All other CHD defects were classified as noncomplex. Patients with complex and noncomplex CHD diagnoses were assigned to the complex CHD group.
Maternal cardiovascular outcomes included in-hospital atrial arrhythmias (including atrial fibrillation, atrial flutter, or paroxysmal supraventricular tachycardia), serious ventricular arrhythmias (including paroxysmal ventricular tachycardia, ventricular fibrillation, ventricular flutter, cardiac arrest, and sudden death due to an unknown cause during the puerperium), eclampsia or preeclampsia, and CHF (eTable 3 in the Supplement). Other maternal outcomes included length of stay and in-hospital mortality. Maternal and fetal outcomes, defined by others previously, included preterm labor, anemia complicating pregnancy, placental abnormalities (previa, abruptio, or accreta), infection during labor, fetal growth restriction, fetal distress, and fetal death.
Outcomes after discharge included readmission to the hospital (after excluding admissions for subsequent delivery) for CHF, atrial arrhythmias, and serious ventricular arrhythmias at 1 year. Women with a primary residence outside California were excluded from this analysis. Because these outcomes were uncommon and because we found no significant differences between the complex and noncomplex CHD groups, both were analyzed as a single group for the 1-year follow-up.
Medical comorbidities were classified based on ICD-9 diagnosis codes for coronary artery disease, CHF, cerebrovascular disease, chronic kidney disease, hypertension, diabetes, and depression (eTable 4 in the Supplement). Patients were identified as having the comorbidity of interest if the diagnosis code was recorded for any health care encounter from January 1, 2005, to the admission date for delivery. Thus, these comorbidities included comorbidities diagnosed before pregnancy and those diagnosed during pregnancy but before the admission for delivery.
Statistical Analysis
Data were analyzed from April 4, 2014, through January 23, 2017. Continuous variables are presented as mean (SD); categorical variables, as percentages. Continuous variables that were not normally distributed are presented as median (interquartile range [IQR]). We compared outcomes using multivariate logistic regression with the following covariates: age, race, cesarean delivery, multiple birth, maternal history of CHF, hypertension, coronary artery disease, chronic kidney disease, diabetes, and cerebrovascular disease. We assessed the association of CHD with readmission to the hospital for reasons other than subsequent delivery by using survival analysis, with failure defined as readmission to the hospital to 7 years after delivery. Women without a readmission were administratively censored on December 31, 2011. The association of CHD with the hazard of readmission was evaluated with Cox proportional hazards modeling. Beginning with an a priori set of predictors, backward selection was used to remove covariates with P < .1 in adjusted analyses. Two-tailed P < .05 was considered to be statistically significant. Owing to HCUP publication requirements, cell sizes of less than 10 are not reported, although the exact number is used in the analyses. Statistical analyses were performed using STATA/SE software (version 13.1; StataCorp).
Results
Of a total of 27 907 535 inpatient hospitalizations in California from January 1, 2005, through December 31, 2011, we identified 3 642 041 admissions for women with a delivery diagnosis. After including codes for multiple births, we identified 3 702 838 live births accounting for 98.4% of all live births in California during the 7-year period.
Among these admissions for delivery, we identified 3189 women with noncomplex CHD (mean [SD] age, 28.6 [7.6] years) and 262 women with complex CHD (mean [SD] age, 26.5 [6.8] years) (Table 1) with a variety of congenital defects (eTable 5 in the Supplement). The remaining 3 638 590 women without CHD (mean [SD] age, 28.3 [6.6] years) comprised the comparison group. A history of CHF was more common in women with CHD (19 [7.3%] with complex CHD, 111 [3.5%] with noncomplex CHD, and 4517 [0.1%] without CHD; P < .001). A history of arrhythmias was rare in all groups but somewhat more common in women with CHD.
Table 1. Baseline Characteristics of Women Admitted for Deliveriesa.
| Characteristic | Patient Group, No. (%) | P Valueb | ||
|---|---|---|---|---|
| No CHD (n = 3 638 590) |
Noncomplex CHD (n = 3189) |
Complex CHD (n = 262) |
||
| Age, mean (SD), y | 28.3 (6.6) | 28.6 (7.6) | 26.5 (6.8) | <.001 |
| Race or ethnicity | ||||
| Asian or Pacific Islander | 380 592 (10.8) | 293 (9.3) | 25 (9.6) | <.001 |
| Black | 187 794 (5.4) | 218 (6.9) | 13 (5.0) | |
| Hispanic | 1 765 517 (50.3) | 1314 (41.7) | 100 (38.5) | |
| Native American | 5428 (0.2) | 13 (0.4) | 0 | |
| White | 1 058 119 (30.1) | 1173 (37.2) | 107 (41.2) | |
| Other | 114 822 (3.3) | 140 (4.4) | 15 (5.8) | |
| Cesarean delivery | 1 164 509 (32.0) | 1236 (38.8) | 121 (46.2) | <.001 |
| Multiple birth | 55 745 (1.5) | 63 (1.9) | <10c | .20 |
| CHF | 4517 (0.1) | 111 (3.5) | 19 (7.3) | <.001 |
| Hypertension | 37 930 (1.0) | 202 (6.3) | 14 (5.3) | <.001 |
| Diabetes | 37 270 (1.0) | 118 (3.7) | 16 (6.1) | <.001 |
| Depression | 35 728 (1.0) | 82 (2.6) | <10c | <.001 |
| History of AF, AFL, or SVT | 1796 (0.05) | 41 (1.3) | <10c | <.001 |
| History of VT, VF, or SCA | 744 (0.02) | <10c | <10c | <.001 |
| Hospital delivery volume quartile | ||||
| Lowest | 1323 (0.04) | 10 (0.3) | 0 | <.001 |
| Second | 242 539 (6.7) | 182 (5.7) | 13 (5.0) | |
| Third | 1 003 283 (27.6) | 874 (27.4) | 81 (30.9) | |
| Highest | 2 391 445 (65.7) | 2123 (66.6) | 168 (64.1) | |
Abbreviations: AF, atrial fibrillation; AFL, atrial flutter; CHD, congenital heart disease; CHF, congestive heart failure; SCA, sudden cardiac arrest; SVT, supraventricular tachycardia; VF, ventricular fibrillation; VT, ventricular tachycardia.
Owing to missing data, totals may not equal column heads.
Calculated using Pearson χ2 test.
Health Care Cost and Utilization Project policy prohibits reporting cell frequencies of less than 10, but each frequency was more common than for women without CHD.
In-Hospital Maternal and Fetal Outcomes
Women with CHD were more likely to undergo cesarean delivery (121 [46.2%] with complex CHD, 1236 [38.8%] with noncomplex CHD, and 1 164 509 [32.0%] without CHD; P < .001). For tetralogy of Fallot, 56 of 102 women with CHD (54.9%) underwent cesarean delivery (eTable 5 in the Supplement).
Median length of stay was longer for women with CHD compared with women without CHD (3 [IQR, 2-4] vs 2 [IQR, 2-3] days; P < .001). In addition, 29 women with complex CHD (11.1%) and 191 women with noncomplex CHD (6.0%) were admitted for longer than 7 days, compared with only 49 089 women without CHD (1.3%). After multivariate adjustment, CHD was associated with greater odds of admissions longer than 1 week (Table 2). Preeclampsia or eclampsia was observed in 19 women with complex CHD (7.3%), 182 women with noncomplex CHD (5.7%), and 122 539 women without CHD (3.4%). After multivariate adjustment, noncomplex CHD was significantly associated with increased odds of preeclampsia or eclampsia (OR, 1.3; 95% CI, 1.1-1.5; P = .003); the association for complex CHD was not significant (OR, 1.5; 95% CI, 0.9-2.4; P = .12).
Table 2. Maternal and Fetal In-Hospital Outcomes.
| Outcome | Patient Group, No. (%) | Noncomplex vs No CHD | Complex vs No CHD | ||||
|---|---|---|---|---|---|---|---|
| No CHD (n = 3 638 583) |
Noncomplex CHD (n = 3189) |
Complex CHD (n = 262) |
AOR (95% CI) | P Valuea | AOR (95% CI) | P Valuea | |
| Maternal | |||||||
| LOS, median (IQR), d | 2 (2-3) | 3 (2-4) | 3 (2-4) | ||||
| LOS>7 d | 49 089 (1.3) | 191 (6.0) | 29 (11.1) | 2.8 (2.3-3.3) | <.001 | 6.7 (4.4-10.1) | <.001 |
| Preeclampsia or eclampsia | 122 539 (3.4) | 182 (5.7) | 19 (7.3) | 1.3 (1.1-1.5) | .003 | 1.5 (0.9-2.4) | .12 |
| Preterm labor | 235 834 (6.5) | 356 (11.2) | 49 (18.7) | 1.6 (1.4-1.8) | <.001 | 3.0 (2.2-4.1) | <.001 |
| Anemia complicating pregnancy | 296 207 (8.1) | 446 (14.0) | 39 (14.9) | 1.5 (1.4-1.7) | <.001 | 1.6 (1.1-2.3) | .007 |
| Placental abnormalities | 75 043 (2.1) | 85 (2.7) | <10b | 1.2 (0.95-1.5) | .14 | 1.6 (0.8-3.0) | .20 |
| Infection during labor | 143 333 (3.9) | 151 (4.7) | 16 (6.1) | 1.2 (1.01-1.4) | .04 | 1.5 (0.9-2.5) | .13 |
| Incident CHF | 508 (0.01) | <10b | <10b | 9.7 (4.7-20.0) | <.001 | 56.6 (17.6-182.5) | <.001 |
| Incident AF, AFL, or SVT | 253 (0.01) | <10b | <10b | 8.2 (3.0-22.7) | <.001 | 31.8 (4.3-236.3) | .001 |
| Incident VT, VF, or SCA | 744 (0.02) | <10b | <10b | 1.9 (0.7-5.1) | .23 | 35.3 (13.4-93.5) | <.001 |
| In-hospital mortality | 1143 (0.03) | <10b (0.2) | <10b | 1.7 (0.8-4.0) | .19 | 79.1 (23.9-261.8) | <.001 |
| Fetal/neonatal | |||||||
| Growth restriction | 48 765 (1.3) | 76 (2.4) | 14 (5.3) | 1.6 (1.3-2.0) | <.001 | 3.5 (2.1-6.1) | <.001 |
| Distress | 526 343 (14.5) | 490 (15.4) | 49 (18.7) | 1.1 (1.0-1.2) | .34 | 1.3 (0.9-1.7) | .15 |
| Death | 13 017 (0.36) | 22 (0.69) | 0 | 1.7 (1.09-2.64) | .02 | ||
Abbreviations: AF, atrial fibrillation; AFL, atrial flutter; AOR, adjusted odds ratio; CHD, congenital heart disease; CHF, congestive heart failure; IQR, interquartile range; LOS, length of stay; SCA, sudden cardiac arrest; SVT, supraventricular tachycardia; VF, ventricular fibrillation; VT, ventricular tachycardia.
Calculated using multivariate logistic regression.
Although Health Care Cost and Utilization Project policy prohibits reporting cell frequencies less than 10, actual numbers were known to investigators and used for analyses.
Incident CHF, atrial arrhythmias, serious ventricular arrhythmias, and maternal mortality were uncommon during hospitalization, each occurring in fewer than 0.5% of women with CHD (Table 2). After multivariate adjustment, noncomplex CHD (OR, 9.7; 95% CI, 4.7-20.0; P < .001) and complex CHD (OR, 56.6; 95% CI, 17.6-182.5; P < .001) were associated with greater odds of CHF. Similar associations for noncomplex CHD (OR, 8.2; 95% CI, 3.0-22.7; P < .001) and complex CHD (OR, 31.8; 95% CI, 4.3-236.3; P = .001) were found for atrial arrhythmias. After multivariate adjustment, only complex CHD was associated with greater odds of serious ventricular arrhythmias (OR, 35.3; 95% CI, 13.4-93.5; P < .001) or maternal in-hospital mortality (OR, 79.1; 95% CI, 23.9-261.8; P < .001) (Table 2).
Fetal growth restriction was reported in 14 women with complex CHD (5.3%), 76 women with noncomplex CHD (2.4%), and 48 765 women without CHD (1.3%). After multivariate adjustment, noncomplex CHD (OR, 1.6; 95% CI, 1.3-2.0; P < .001) and complex CHD (OR, 3.5; 95% CI, 2.1-6.1; P < .001) were associated with greater odds of fetal growth restriction. Fetal death occurred in no deliveries for women with complex CHD, 22 deliveries for women with noncomplex CHD (0.7%), and 13 017 deliveries for women without CHD (0.4%). After multivariate adjustment, noncomplex CHD was associated with greater odds of fetal death compared with women without CHD (OR, 1.7; 95% CI, 1.1-2.6; P = .02).
Maternal Outcomes After Hospital Discharge
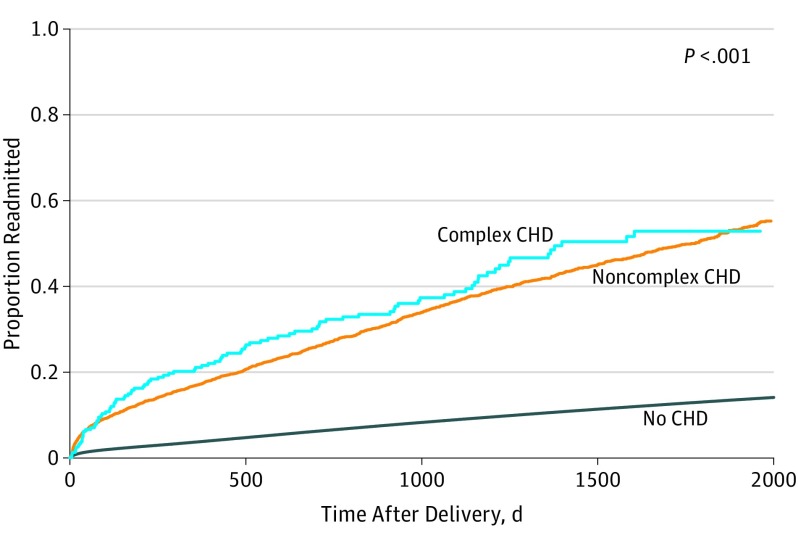
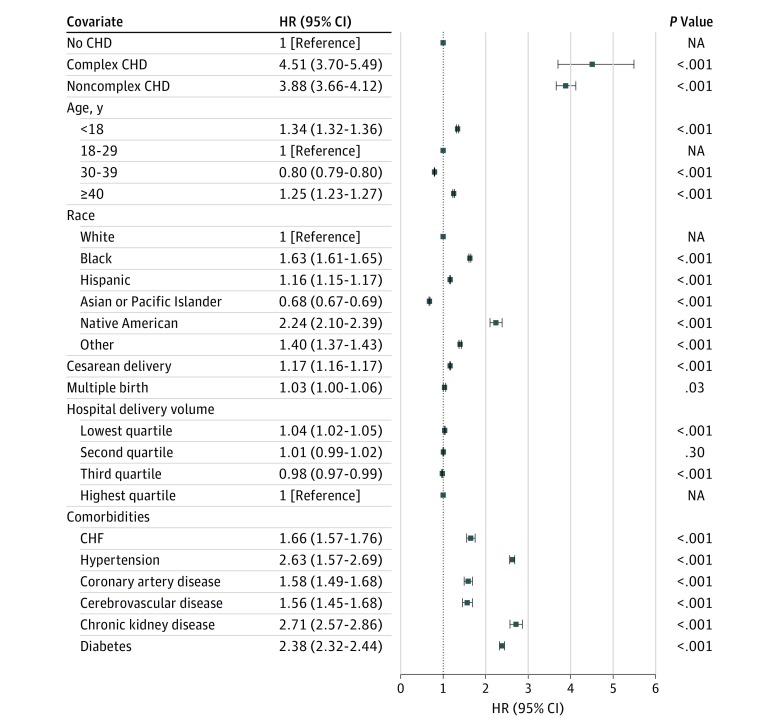
When women were followed up after discharge, 30 155 women without CHD (1.1%) and 166 women with CHD (5.6%) were readmitted to the hospital within 30 days (P < .001); the readmission rate exclusive of subsequent deliveries remained higher for women with CHD at 1 year (OR, 3.6; 95% CI, 3.3-4.0; P < .001) (Table 3) and to 7 years after discharge (χ2 = 3941, P < .001, log-rank test for comparing complex CHD, noncomplex CHD, and no CHD) (Figure 1). At 1 year, readmissions for CHF (OR, 6.7; 95% CI, 4.0-11.1; P < .001), atrial arrhythmias (OR, 10.9; 95% CI, 7.0-17.1; P < .001), and serious ventricular arrhythmias (OR, 6.2; 95% CI, 3.5-11.2; P < .001) were more common for women with CHD than for those without (Table 3). For readmissions within 1 year of delivery, the 10 most common diagnoses were noncardiac for women without CHD, whereas for women with CHD, 3 of the top 10 were cardiac (CHF, ostium secundum, atrial septal defect, and chest pain). After multivariate analysis, noncomplex CHD (hazard ratio, 3.88; 95% CI, 3.66-4.12) and complex CHD (hazard ratio, 4.51; 95% CI, 3.70-5.49) had the largest association with increasing the hazard of readmission (Figure 2).
Table 3. Maternal Outcomes at 1 Yeara.
| Outcome | No CHD (n = 2 807 672) |
CHD (n = 3106)b |
CHD vs No CHD, AOR (95% CI) |
|---|---|---|---|
| Any readmission | 119 441 (4.3) | 544 (17.5) | 3.6 (3.3-4.0) |
| Readmission for CHF | 689 (0.02) | 19 (0.6) | 6.7 (4.0-11.1) |
| Readmission for atrial arrhythmiasc | 736 (0.03) | 32 (1.0) | 10.9 (7.0-17.1) |
| Readmission for serious ventricular arrhythmias | 543 (0.02) | 15 (0.5) | 6.2 (3.5-11.2) |
Abbreviations: AOR, adjusted odds ratio; CHD, congenital heart disease; CHF, congestive heart failure.
Excludes admissions for subsequent delivery and women with a primary residence outside California.
Noncomplex CHD and complex CHD were pooled owing to small numbers of outcomes and the fact that the 2 groups were not significantly different. Groups were compared with χ2 tests, and all differences were statistically significant (P < .001).
Includes atrial fibrillation, atrial flutter, or paroxysmal supraventricular tachycardia.
Figure 1. Cumulative Proportion of Women Readmitted After Delivery.
Includes admissions other than for subsequent delivery. P values comparing equality of survivor functions for complex, noncomplex, and no congenital heart disease (CHD) were calculated using log-rank test (χ2 = 3941; P < .01).
Figure 2. Multivariate Analysis for Hospital Readmission.
Includes admissions other than for subsequent delivery. CHD indicates congenital heart disease; CHF, congestive heart failure; HR, hazard ratio; and NA, not applicable.
Discussion
In this study of more than 3.6 million admissions for delivery in California during a 7-year period that accounted for more than 98% of all live births, women with CHD were more likely to have a history of CHF, undergo cesarean delivery, and have longer lengths of stay. Incident maternal CHF, arrhythmias, and mortality were uncommon for all groups of women, but the odds of these outcomes were substantially greater for women with complex CHD. The adjusted odds of CHF, atrial arrhythmias, and maternal death were also increased for women with noncomplex CHD. At 1 year, readmissions for CHF, atrial arrhythmias, and serious ventricular arrhythmias were more common for women with CHD. After multivariate analysis, CHD had a greater associaton with increasing the hazard of readmission than did diabetes, chronic kidney disease, or hypertension. Despite these associations, the absolute risks for adverse cardiovascular outcomes among women with CHD were still low. The risks for incident CHF, supraventricular arrhythmias, serious ventricular arrhythmias, and maternal in-hospital mortality were less than 0.5% among women with CHD. The magnitude of the increases in relative risk among women with CHD appears to be high in part owing to comparisons against the rare levels of these complications in the general population.
Women with CHD more often underwent cesarean delivery, but the underlying reasons for this difference are unclear. Cesarean delivery is more commonly used in mothers who have delivered by cesarean delivery previously and in cases of breech presentation, dystocia, and fetal distress. Women with CHD were not more likely to have codes for fetal distress; therefore, increased use of cesarean delivery does not seem to be attributable to fetal instability. Cesarean deliveries may have been more likely to be planned owing to physician and/or patient preference because of the belief that the procedure has less effect on maternal physiology, although at present no definitive data on this issue exist. We found a higher rate of cesarean delivery among women with CHD (46.2% for complex CHD and 38.8% for noncomplex CHD) than did other studies. In a multicenter cohort of mothers with CHD from more than a decade ago, Siu and colleagues found that 27% of births were by cesarean delivery and 96% of these were for obstetric indications (compared with maternal cardiac status indication in only 4%).
We also found significantly greater odds of preeclampsia or eclampsia in women with noncomplex CHD and increased odds in women with complex CHD. Reduced placental perfusion may cause preeclampsia, which could be more common in women with CHD. Studies have shown that compared with the general population and women with repaired defects, women with an unrepaired atrial septal defect or ventricular septal defect have an increased risk for preeclampsia. In addition, even in women with CHD, preeclampsia or eclampsia is uncommon and only occurred in 7.3% of women in our complex CHD group.
Compared with the studies by Karamlou and colleagues and Thompson and colleagues, our study captured nearly every birth in California, as opposed to a representative sample of the United States obtained from the HCUP Nationwide Inpatient Sample. All 3 studies found higher rates of cesarean delivery and cardiac complications among women with CHD. Because of differences between the databases, the present study was also able to ascertain serious complications requiring readmission after discharge.
Cardiac complications were less commonly observed in this study than in the study by Siu and colleagues, who reported a primary cardiac event in 13% of completed pregnancies. However, more than half of these events occurred in the prepartum period, which was not evaluated in the present study. One review found cardiac events in 1.9%, CHF in 4.8%, and arrhythmias in 4.5% of deliveries in women with CHD. A Dutch national study of CHD identified cardiovascular events at 1 year in 6.4% of pregnancies, and 9 of 11 events were new-onset arrhythmias. In our contemporary statewide study of nearly every delivery to mothers with CHD, arrhythmias occurred in approximately 1% of women.
Prior studies of women with CHD have found that their offspring are at increased risk for premature birth, being small for gestational age, and neonatal mortality. We found greater odds of fetal growth restriction for women with CHD and greater odds of fetal death for women with noncomplex CHD. Patients with complex disease are at particular risk for intrauterine growth restriction, and monitoring for such complications requires vigilance by obstetricians. Owing to coding restrictions, we could not examine prematurity as an end point or as a mediator of the association between maternal CHD and neonatal mortality. Prior studies have also shown that miscarriages and terminations for medical reasons are more common in women with CHD, but this study did not capture any outcomes before the time of delivery.
This study also found a higher risk for maternal readmission among mothers with CHD at 30 days and 1 and 7 years. Although we examined the cause of readmission at 1 year, we did not do so at 7 years, and the higher readmission rates across long-term follow-up may be attributable to the natural history of CHD and not to complications of pregnancy.
Limitations
Despite the large number of women with CHD captured in the study, this study has several limitations. First, ICD-9 codes have imperfect sensitivity and specificity, and CHD may have been undercoded. However, undercoding is unlikely to bias the results, because even a small number of women with CHD misclassified as not having CHD would not have a sizable effect on summary estimates of more than 3.6 million women. Second, the administrative nature of the database does not allow the medical records of mothers and neonates to be linked to determine the long-term health outcomes of these infants. Third, this analysis captured only women who chose to become pregnant and carried pregnancies to term. We did not evaluate women who chose not to become pregnant or who did not carry pregnancies to term, which may account for approximately 20% of pregnancies among women with CHD. Fourth, the number of women with CHD who delivered at low-volume centers was small, and multivariate analysis did not demonstrate an association of hospital delivery volume with outcomes for women with CHD. Fifth, the inpatient nature of this database did not allow us to capture intensity or quality of care before and after delivery. In a recent study of cardiovascular deaths related to pregnancy in California, health care professional factors were found to play a role in most cardiovascular deaths. Finally, for the follow-up analysis, only women who were readmitted to a California hospital were captured; therefore, women who moved or died outside the hospital were not captured.
Conclusions
In this study of nearly all women admitted to California hospitals for delivery during a 7-year period, women with CHD were more likely to undergo cesarean delivery and have a longer length of stay. Incident maternal CHF, arrhythmias, and mortality were uncommon in all groups of women, but CHD was significantly associated with incident CHF, atrial arrhythmias, fetal growth restriction, and hospital readmission. Complex CHD was a significant predictor of ventricular arrhythmias and maternal in-hospital mortality. These results may guide monitoring decisions and risk assessment for pregnant women with CHD at the time of delivery. Given the higher rate of cardiac and obstetrical complications, pregnant women with CHD should be treated in a center with expertise in adult CHD.
eTable 1. Inclusion and Exclusion Criteria
eTable 2. CHD Diagnoses With Corresponding ICD-9 Codes
eTable 3. Outcomes
eTable 4. Medical Comorbidities
eTable 5. Type of CHD
References
- 1.Gowda RM, Khan IA, Mehta NJ, Vasavada BC, Sacchi TJ. Cardiac arrhythmias in pregnancy: clinical and therapeutic considerations. Int J Cardiol. 2003;88(2-3):129-133. [DOI] [PubMed] [Google Scholar]
- 2.Roberts JM, Insel PA, Goldfien A. Regulation of myometrial adrenoreceptors and adrenergic response by sex steroids. Mol Pharmacol. 1981;20(1):52-58. [PubMed] [Google Scholar]
- 3.Widerhorn J, Widerhorn AL, Rahimtoola SH, Elkayam U. WPW syndrome during pregnancy: increased incidence of supraventricular arrhythmias. Am Heart J. 1992;123(3):796-798. [DOI] [PubMed] [Google Scholar]
- 4.Lee JCR, Wetzel G, Shannon K. Maternal arrhythmia management during pregnancy in patients with structural heart disease. Prog Pediatr Cardiol. 2004;19(1):71-82. [Google Scholar]
- 5.Silversides CK, Harris L, Haberer K, Sermer M, Colman JM, Siu SC. Recurrence rates of arrhythmias during pregnancy in women with previous tachyarrhythmia and impact on fetal and neonatal outcomes. Am J Cardiol. 2006;97(8):1206-1212. [DOI] [PubMed] [Google Scholar]
- 6.Miyoshi T, Kamiya CA, Katsuragi S, et al. . Safety and efficacy of implantable cardioverter-defibrillator during pregnancy and after delivery. Circ J. 2013;77(5):1166-1170. [DOI] [PubMed] [Google Scholar]
- 7.Natale A, Davidson T, Geiger MJ, Newby K. Implantable cardioverter-defibrillators and pregnancy: a safe combination? Circulation. 1997;96(9):2808-2812. [DOI] [PubMed] [Google Scholar]
- 8.Ntusi NB, Badri M, Gumedze F, Sliwa K, Mayosi BM. Pregnancy-associated heart failure: a comparison of clinical presentation and outcome between hypertensive heart failure of pregnancy and idiopathic peripartum cardiomyopathy. PLoS One. 2015;10(8):e0133466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hoffman JI, Kaplan S, Liberthson RR. Prevalence of congenital heart disease. Am Heart J. 2004;147(3):425-439. [DOI] [PubMed] [Google Scholar]
- 10.Warnes CA, Liberthson R, Danielson GK, et al. . Task Force 1: the changing profile of congenital heart disease in adult life. J Am Coll Cardiol. 2001;37(5):1170-1175. [DOI] [PubMed] [Google Scholar]
- 11.Oechslin EN, Harrison DA, Connelly MS, Webb GD, Siu SC. Mode of death in adults with congenital heart disease. Am J Cardiol. 2000;86(10):1111-1116. [DOI] [PubMed] [Google Scholar]
- 12.Pillutla P, Shetty KD, Foster E. Mortality associated with adult congenital heart disease: trends in the US population from 1979 to 2005. Am Heart J. 2009;158(5):874-879. [DOI] [PubMed] [Google Scholar]
- 13.Drenthen W, Pieper PG, Roos-Hesselink JW, et al. ; ZAHARA Investigators . Outcome of pregnancy in women with congenital heart disease: a literature review. J Am Coll Cardiol. 2007;49(24):2303-2311. [DOI] [PubMed] [Google Scholar]
- 14.Drenthen W, Boersma E, Balci A, et al. ; ZAHARA Investigators . Predictors of pregnancy complications in women with congenital heart disease. Eur Heart J. 2010;31(17):2124-2132. [DOI] [PubMed] [Google Scholar]
- 15.Gurvitz MZ, Inkelas M, Lee M, Stout K, Escarce J, Chang RK. Changes in hospitalization patterns among patients with congenital heart disease during the transition from adolescence to adulthood. J Am Coll Cardiol. 2007;49(8):875-882. [DOI] [PubMed] [Google Scholar]
- 16.Opotowsky AR, Siddiqi OK, Webb GD. Trends in hospitalizations for adults with congenital heart disease in the U.S. J Am Coll Cardiol. 2009;54(5):460-467. [DOI] [PubMed] [Google Scholar]
- 17.Hayward RM, Dewland TA, Moyers B, et al. . Device complications in adult congenital heart disease. Heart Rhythm. 2015;12(2):338-344. [DOI] [PubMed] [Google Scholar]
- 18.Zhan C, Baine WB, Sedrakyan A, Steiner C. Cardiac device implantation in the United States from 1997 through 2004: a population-based analysis. J Gen Intern Med. 2008;23(suppl 1):13-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shah RU, Freeman JV, Shilane D, Wang PJ, Go AS, Hlatky MA. Procedural complications, rehospitalizations, and repeat procedures after catheter ablation for atrial fibrillation. J Am Coll Cardiol. 2012;59(2):143-149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.James AH, Jamison MG, Brancazio LR, Myers ER. Venous thromboembolism during pregnancy and the postpartum period: incidence, risk factors, and mortality. Am J Obstet Gynecol. 2006;194(5):1311-1315. [DOI] [PubMed] [Google Scholar]
- 21.Kuklina EV, Whiteman MK, Hillis SD, et al. . An enhanced method for identifying obstetric deliveries: implications for estimating maternal morbidity. Matern Child Health J. 2008;12(4):469-477. [DOI] [PubMed] [Google Scholar]
- 22.Mackie AS, Ionescu-Ittu R, Pilote L, Rahme E, Marelli AJ. Hospital readmissions in children with congenital heart disease: a population-based study. Am Heart J. 2008;155(3):577-584. [DOI] [PubMed] [Google Scholar]
- 23.Marelli AJ, Mackie AS, Ionescu-Ittu R, Rahme E, Pilote L. Congenital heart disease in the general population: changing prevalence and age distribution. Circulation. 2007;115(2):163-172. [DOI] [PubMed] [Google Scholar]
- 24.Mackie AS, Pilote L, Ionescu-Ittu R, Rahme E, Marelli AJ. Health care resource utilization in adults with congenital heart disease. Am J Cardiol. 2007;99(6):839-843. [DOI] [PubMed] [Google Scholar]
- 25.Bansil P, Kuklina EV, Meikle SF, et al. . Maternal and fetal outcomes among women with depression. J Womens Health (Larchmt). 2010;19(2):329-334. [DOI] [PubMed] [Google Scholar]
- 26.Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project (HCUP). Nationwide HCUP databases. 2005-2011. https://www.hcup-us.ahrq.gov/databases.jsp. Modified November 11, 2016. Accessed August 26, 2015.
- 27.State of California, Department of Public Health. Live Births, California Counties, 2002-2011. http://www.cdph.ca.gov/data/statistics/Documents/VSC-2011-0218.pdf. Accessed July 31, 2015.
- 28.Zhang J, Troendle J, Reddy UM, et al. . Contemporary cesarean delivery practice in the United States. Am J Obstet Gynecol. 2010;203(4):326.e-326.e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Taffel SM, Placek PJ, Liss T. Trends in the United States cesarean section rate and reasons for the 1980-85 rise. Am J Public Health. 1987;77(8):955-959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gregory KD, Curtin SC, Taffel SM, Notzon FC. Changes in indications for cesarean delivery: United States, 1985 and 1994. Am J Public Health. 1998;88(9):1384-1387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Siu SC, Sermer M, Colman JM, et al. ; Cardiac Disease in Pregnancy (CARPREG) Investigators . Prospective multicenter study of pregnancy outcomes in women with heart disease. Circulation. 2001;104(5):515-521. [DOI] [PubMed] [Google Scholar]
- 32.Roberts JM, Gammill HS. Preeclampsia: recent insights. Hypertension. 2005;46(6):1243-1249. [DOI] [PubMed] [Google Scholar]
- 33.Yap SC, Drenthen W, Meijboom FJ, et al. ; ZAHARA investigators . Comparison of pregnancy outcomes in women with repaired versus unrepaired atrial septal defect. BJOG. 2009;116(12):1593-1601. [DOI] [PubMed] [Google Scholar]
- 34.Yap SC, Drenthen W, Pieper PG, et al. ; ZAHARA investigators . Pregnancy outcome in women with repaired versus unrepaired isolated ventricular septal defect. BJOG. 2010;117(6):683-689. [DOI] [PubMed] [Google Scholar]
- 35.Karamlou T, Diggs BS, McCrindle BW, Welke KF. A growing problem: maternal death and peripartum complications are higher in women with grown-up congenital heart disease. Ann Thorac Surg. 2011;92(6):2193-2198. [DOI] [PubMed] [Google Scholar]
- 36.Thompson JL, Kuklina EV, Bateman BT, Callaghan WM, James AH, Grotegut CA. Medical and obstetric outcomes among pregnant women with congenital heart disease. Obstet Gynecol. 2015;126(2):346-354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kampman MA, Balci A, Groen H, et al. ; ZAHARA II investigators . Cardiac function and cardiac events 1-year postpartum in women with congenital heart disease. Am Heart J. 2015;169(2):298-304. [DOI] [PubMed] [Google Scholar]
- 38.Siu SC, Colman JM, Sorensen S, et al. . Adverse neonatal and cardiac outcomes are more common in pregnant women with cardiac disease. Circulation. 2002;105(18):2179-2184. [DOI] [PubMed] [Google Scholar]
- 39.Balci A, Sollie-Szarynska KM, van der Bijl AG, et al. ; ZAHARA-II investigators . Prospective validation and assessment of cardiovascular and offspring risk models for pregnant women with congenital heart disease. Heart. 2014;100(17):1373-1381. [DOI] [PubMed] [Google Scholar]
- 40.Humphries KH, Rankin JM, Carere RG, Buller CE, Kiely FM, Spinelli JJ. Co-morbidity data in outcomes research: are clinical data derived from administrative databases a reliable alternative to chart review? J Clin Epidemiol. 2000;53(4):343-349. [DOI] [PubMed] [Google Scholar]
- 41.Hameed AB, Lawton ES, McCain CL, et al. . Pregnancy-related cardiovascular deaths in California: beyond peripartum cardiomyopathy. Am J Obstet Gynecol. 2015;213(3):379.e1-379.e10. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Inclusion and Exclusion Criteria
eTable 2. CHD Diagnoses With Corresponding ICD-9 Codes
eTable 3. Outcomes
eTable 4. Medical Comorbidities
eTable 5. Type of CHD