This community-based study compares the relative accuracy of US Preventive Services Task Force and American College of Cardiology/American Heart Association recommendations in identifying African American individuals with subclinical and clinical atherosclerotic cardiovascular disease.
Key Points
Question
How accurate are statin therapy guidelines from the US Preventive Services Task Force (USPSTF) and American College of Cardiology/American Heart Association (ACC/AHA) for African American individuals?
Findings
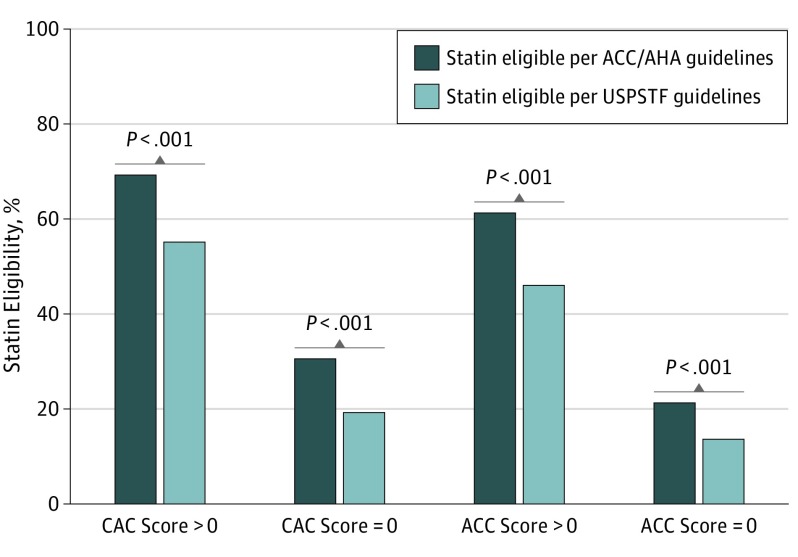
In this community-based study of 2182 participants, recommendation for statin therapy was associated with a 5-fold increased odds of vascular calcification for both guidelines, but USPSTF guidelines only identified 55% of African American individuals with a coronary artery calcium score greater than 0 compared with 69% identified by ACC/AHA guidelines. African American individuals indicated for statins only by ACC/AHA guidelines and not USPSTF guidelines also experienced a low to intermediate cardiovascular event rate (4.1 events per 1000 patient-years).
Meaning
Compared with ACC/AHA guidelines, USPSTF guidelines focus therapy recommendations on a smaller subset of African American individuals but also do not recommend therapy for many African American individuals with vascular calcification and at risk of atherosclerotic cardiovascular disease.
Abstract
Importance
Modern prevention guidelines substantially increase the number of individuals who are eligible for treatment with statins. Efforts to refine statin eligibility via coronary calcification have been studied in white populations but not, to our knowledge, in large African American populations.
Objective
To compare the relative accuracy of US Preventive Services Task Force (USPSTF) and American College of Cardiology/American Heart Association (ACC/AHA) recommendations in identifying African American individuals with subclinical and clinical atherosclerotic cardiovascular disease (ASCVD).
Design, Setting, and Participants
In this prospective, community-based study, 2812 African American individuals aged 40 to 75 years without prevalent ASCVD underwent assessment of ASCVD risk. Of these, 1743 participants completed computed tomography.
Main Outcomes and Measures
Nonzero coronary artery calcium (CAC) score, abdominal aortic calcium score, and incident ASCVD (ie, myocardial infarction, ischemic stroke, or fatal coronary heart disease).
Results
Of the 2812 included participants, the mean (SD) age at baseline was 55.4 (9.4) years, and 1837 (65.3%) were female. The USPSTF guidelines captured 404 of 732 African American individuals (55.2%) with a CAC score greater than 0; the ACC/AHA guidelines identified 507 individuals (69.3%) (risk difference, 14.1%; 95% CI, 11.2-17.0; P < .001). Statin recommendation under both guidelines was associated with a CAC score greater than 0 (odds ratio, 5.1; 95% CI, 4.1-6.3; P < .001). While individuals indicated for statins under both guidelines experienced 9.6 cardiovascular events per 1000 patient-years, those indicated under only ACC/AHA guidelines were at low to intermediate risk (4.1 events per 1000 patient-years). Among individuals who were statin eligible by ACC/AHA guidelines, the 10-year ASCVD incidence per 1000 person-years was 8.1 (95% CI, 5.9-11.1) in the presence of CAC and 3.1 (95% CI, 1.6-5.9) without CAC (P = .02). While statin-eligible individuals by USPSTF guidelines did not have a significantly higher 10-year ASCVD event rate in the presence of CAC, African American individuals not eligible for statins by USPSTF guidelines had a higher ASCVD event rate in the presence of CAC (2.8 per 1000 person-years; 95% CI, 1.5-5.4) relative to without CAC (0.8 per 1000 person-years; 95%, CI 0.3-1.7) (P = .03).
Conclusions and Relevance
The USPSTF guidelines focus treatment recommendations on 38% of high-risk African American individuals at the expense of not recommending treatment in nearly 25% of African American individuals eligible for statins by ACC/AHA guidelines with vascular calcification and at low to intermediate ASCVD risk.
Introduction
African American individuals are at disproportionately high risk for atherosclerotic cardiovascular disease (ASCVD)—defined as a history of myocardial infarction by self-report or 12-lead electrocardiogram, self-reported stroke, carotid angioplasty, coronary artery bypass, carotid endarterectomy, arterial revascularization, coronary angiogram, or cardiac catheterization—with a more adverse response to cardiovascular risk and subclinical ASCVD compared with those of other racial backgrounds. Several reports suggest that while 2013 American College of Cardiology/American Heart Association (ACC/AHA) guidelines using the race-specific Pooled Cohort Equations (PCEs) risk scores discriminate ASCVD risk well in African American individuals, the guidelines also call for a marked increase in statin eligibility (relative to older 2004 Adult Treatment Panel ATP-III guidelines). The increase in statin eligibility in adults with a low expected cardiovascular event rate (with potential for increased cost and adverse effects) has prompted search for biomarkers to prioritize statin therapy. Furthermore, the US Preventive Services Task Force (USPSTF) recently developed new statin guidelines for primary ASCVD prevention that address these issues, emphasizing clinical risk factors and incorporating risk assessment via the PCE risk score estimator. Nevertheless, to our knowledge, it remains unknown whether newer USPSTF clinical guidelines or ACC/AHA guidelines accurately identify African American individuals with vascular calcification and high ASCVD risk, specifically whether statin eligibility and vascular calcification provide complementary information in this population.
To address this, we examined whether statin eligibility by USPSTF guidelines compared with ACC/AHA guidelines identifies African American individuals with higher ASCVD risk and vascular calcification in the Jackson Heart Study (JHS), a large, established cohort of African American individuals with coronary and aortic calcium quantification. Our goals were to understand whether statin eligibility under USPSTF recommendations better identifies African American individuals with (1) higher ASCVD risk and (2) higher coronary and abdominal aortic calcium scores than ACC/AHA guidelines and (3) whether the presence of coronary calcification provides incremental value to USPSTF or ACC/AHA guidelines in determining ASCVD risk.
Methods
Study Population
The JHS is a population-based prospective study of 5306 African American individuals 21 years or older from the Jackson, Mississippi, tricounty area (ie, Hinds, Madison, and Rankin). The study was designed to identify causes of ASCVD among African American individuals. Study participants were examined at a baseline clinic visit between 2000 and 2004 (visit 1) and during 2 additional visits between 2005 and 2008 (visit 2) and between 2009 and 2013 (visit 3). We included participants aged 40 to 75 years without prevalent ASCVD, not receiving statin treatment, and with complete data on variables used to calculate 10-year risk scores by PCEs (eTable 1 in the Supplement). Of 2812 participants, 2716 (96.6%) had complete data on incident ASCVD and 1743 (62.0%) had available computed tomography (CT) at visit 2. The JHS was approved by the institutional review boards of Jackson State University, University of Mississippi Medical Center, and Tougaloo College. All participants provided written informed consent.
Risk Factor Measurement
Prevalent diabetes was defined according to the American Diabetes Association criteria of a fasting glucose level of 126 mg/dL (to convert to millimoles per liter, multiply by 0.0555) or greater, a hemoglobin A1c level of 6.5% or greater (to convert to the proportion of total hemoglobin, multiply by 0.01), or the use of medications for diabetes. Current cigarette smoking was assessed at baseline. Blood pressure was calculated in the seated position as the average of 2 resting blood pressure recordings. Hypertension was defined as a systolic blood pressure of 140 mm Hg or greater, a diastolic blood pressure of 90 mm Hg or greater, or the use of antihypertensive medications. Lipid profile was measured as previously described.
Statin Eligibility
Statin eligibility by 2013 ACC/AHA guidelines was defined according to published guidelines. Participants were eligible for statins if they (1) had a low-density lipoprotein cholesterol (LDL-C) level of 190 mg/dL (to convert to millimoles per liter, multiply by 0.0259) or greater; (2) had diabetes, were aged 40 to 75 years, and had an LDL-C level between 70 and 189 mg/dL; or (3) had no diabetes, were aged 40 to 75 years, had an LDL-C level between 70 and 189 mg/dL, and had an estimated 10-year ASCVD risk score of 7.5% or greater, as determined by the PCEs.
Statin eligibility by USPSTF guidelines (grade B recommendation) was defined using risk factors and the PCEs, as published. Participants were elgible for statins if they were aged 40 to 75 years, had 1 or more ASCVD risk factors, and had a calculated 10-year ASCVD risk (by PCE risk score estimator) of 10% or greater. Atherosclerotic cardiovascular disease risk factors include dyslipidemia, diabetes, hypertension, or smoking. Dyslipidemia was defined as an LDL-C level greater than 130 mg/dL or a high-density lipoprotein cholesterol level less than 40 mg/dL. Of note, while USPSTF guidelines did not make specific recommendations for statin use in individuals with an LDL-C level greater than 190 mg/dL, they acknowledge that these individuals may require statin use. Therefore, we considered participants with an LDL-C level greater than 190 mg/dL as meeting criteria for statin use by both guidelines.
Coronary and Aortic Vascular Calcification
By JHS study design, vascular calcium was quantified at visit 2 and not at visit 1 (median interval between visit 1 and 2, 4.5 years). Heart and abdominal imaging were obtained with a 16-channel multidetector CT using a prospective electrocardiogram-triggered protocol (Lightspeed 16 Pro; GE Healthcare), as published. Coronary artery calcium (CAC) score and abdominal aortic calcium (AAC) score were quantified using the Agatston score (TeraRecon Aquarius Workstation).
Incident Atherosclerotic Cardiovascular Disease
Incident ASCVD was defined as the occurrence of the first myocardial infarction, ischemic stroke, or fatal coronary heart disease event. Incident myocardial infarction, ischemic stroke, and fatal coronary heart disease were determined through adjudication of relevant medical records, as previously described. The final date of follow-up was December 31, 2012.
Statistical Analysis
A central component of our analysis is the selection of exposure (statin eligibility) and outcomes (ASCVD events; vascular calcification). Given the low overall event rate in this primary prevention population, for our prognostic aim, we chose to maximize power (with greatest events and follow-up in Cox regression) by examining the association between statin eligibility at visit 1 (exposure) with long-term ASCVD events (outcome). For our vascular calcification aim (assessed at visit 2 only in the JHS), we performed analyses based on statin eligibility at visit 1. The study flow is shown in eFigure 1 in the Supplement.
We first used logistic regression models to estimate the probability of the presence of CAC or AAC (zero vs nonzero) based on statin eligibility by 2016 USPSTF guidelines and 2013 ACC/AHA guidelines. “Not statin eligible” was treated as the referent category. We assessed model discrimination (C statistic) for vascular calcification. Differences in C statistics between statin eligibility by USPSTF and ACC/AHA guidelines and reclassification for CAC or AAC were calculated as described by Pencina and others.
To address our prognostic aim, we examined the effect of statin eligibility by USPSTF vs ACC/AHA guidelines on clinical outcomes, independent of CAC score. First, we constructed Cox proportional hazards regression models and estimated annualized event rates for incident ASCVD as a function of statin eligibility by USPSTF guidelines vs ACC/AHA guidelines. Event rates were calculated per 1000 patient-years of follow-up, analogous to a previously published study, with comparison by Poisson regression. In the subgroup of 1743 individuals with CT imaging, we examined whether the presence of CAC by CT imaging was associated with ASCVD risk independent of statin eligibility by either guideline. The assumption of proportional hazards was confirmed via Kolmogorov supremum test. Kaplan-Meier survival curves were used to visualize cumulative incidence over time. Statistical analyses were performed using SAS version 9.4 (SAS Institute). A 2-tailed P value < .05 was considered significant.
Results
Baseline Characteristics
A diagram summarizing analytic sample construction is shown in eFigure 1 in the Supplement. We evaluated statin eligibility at visit 1 in all 2812 participants for our prognostic aim and evaluated statin eligibility at visit 1 in 1743 participants with CT imaging for our calcification aim. Demographic, clinical, and biochemical characteristics and imaging characteristics stratified by statin eligibility are shown in Table 1. The mean (SD) age was 55.4 (9.4) years, 1837 (65.3%) were female, and the mean (SD) body mass index (calculated as weight in kilograms divided by height in meters squared) was 31.6 (7.0), which indicated obesity. The median (interquartile range) 10-year PCE risk score was 6.9% (3.1%-13.1%). Of the 1743 participants with CT imaging who were eligible for statins, 732 (42.0%) had detectable coronary calcification and 1110 (63.7%) had detectable abdominal aortic calcification. As expected, the participants excluded from analysis had an overall higher prevalence of ASCVD risk factors and greater statin use (eTable 1 in the Supplement).
Table 1. Baseline Characteristics of Jackson Heart Study Participants Stratified by Statin Eligibility by ACC/AHA and USPSTF Guidelines.
| Characteristic | USPSTF Guidelines | P Value | ACC/AHA Guidelines | P Value | ||
|---|---|---|---|---|---|---|
| Statin Eligible (n = 1072) | Statin Ineligible (n = 1740) | Statin Eligible (n = 1404) | Statin Ineligible (n = 1408) | |||
| Age, mean (SD), y | 62.4 (7.6) | 51.0 (7.6) | <.001 | 60.9 (8.3) | 49.9 (6.9) | <.001 |
| Female, No. (%) | 612 (57.1) | 1225 (70.4) | <.001 | 812 (57.8) | 1025 (72.8) | <.001 |
| Male, No. (%) | 460 (42.9) | 515 (29.6) | <.001 | 592 (42.2) | 383 (27.2) | <.001 |
| BMI, mean (SD) | 31.7 (6.7) | 31.6 (7.3) | .80 | 31.7 (6.8) | 31.5 (7.3) | .59 |
| Current smoking, No. (%) | 182 (17.0) | 182 (10.5) | <.001 | 222 (15.8) | 142 (10.1) | <.001 |
| Hypertension, No. (%) | 839 (78.3) | 647 (37.2) | <.001 | 1002 (71.4) | 484 (34.4) | <.001 |
| Diabetes, No. (%) | 348 (32.5) | 86 (4.9) | <.001 | 416 (29.6) | 18 (1.3) | <.001 |
| Antihypertensive therapy, No. (%) | 723 (67.4) | 579 (33.3) | <.001 | 879 (62.6) | 423 (30.0) | <.001 |
| Total cholesterol, mean (SD), mg/dL | 215.8 (45.3) | 194.1 (32.8) | <.001 | 213.4 (41.8) | 191.4 (33.6) | <.001 |
| LDL-C | 141.8 (42.1) | 122.1 (30.5) | <.001 | 139.9 (38.3) | 119.4 (31.8) | <.001 |
| HDL-C | 50.4 (14.5) | 53.4 (14.5) | <.001 | 50.8 (14.1) | 53.7 (14.8) | <.001 |
| PCE risk score, median (IQR), % | 15.5 (11.9-21.7) | 4.0 (1.7-6.5) | <.001 | 12.9 (9.3-19.1) | 3.3 (1.3-5.2) | <.001 |
| Coronary artery calcium score, No. | 600 | 1143 | 817 | 926 | ||
| Mean (SD) | 220.3 (466.4) | 37.0 (140.5) | NA | 178.7 (413.2) | 30.8 (136.4) | NA |
| Median (IQR) | 37.6 (0-194.3) | 0 (0-4.7) | <.001 | 23.8 (0-138.2) | 0 (0-0) | <.001 |
| Score >0, No. (%) | 404 (67.3) | 328 (28.7) | <.001 | 507 (62.1) | 225 (24.3) | <.001 |
| Score >100, No. (%) | 213 (35.5) | 97 (8.5) | <.001 | 248 (30.4) | 62 (6.7) | <.001 |
| Abdominal aortic calcium score, No. | 599 | 1143 | 816 | 926 | ||
| Mean (SD) | 1218.8 (1621.4) | 332.2 (904.3) | NA | 1090.6 (1559.9) | 237.3 (746.8) | NA |
| Median (IQR) | 532.3 (66.6-1866.1) | 5.5 (0-173.7) | <.001 | 418.4 (40.9-1538.0) | 0 (0-108.7) | <.001 |
| Score >0, No. (%) | 512 (85.5) | 598 (52.3) | <.001 | 681 (83.5) | 429 (46.3) | <.001 |
Abbreviations: ACC/AHA, American College of Cardiology/American Heart Association; BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); HDL-C, high-density lipoprotein cholesterol; IQR, interquartile range; LDL-C, low-density lipoprotein cholesterol; NA, not applicable; PCE, Pooled Cohort Equation; USPSTF, US Preventive Services Task Force.
Distribution of Statin Eligibility in African American Individuals
Of 2812 participants not receiving statin therapy at baseline, 1072 (38.1%) were statin eligible by USPSTF grade B guideline recommendations compared with 1404 (49.9%) by ACC/AHA guidelines (risk difference, 11.8%; 95% CI, 10.5-13.1; P < .001). Overall, among individuals not receiving statins at the baseline study visit, statin recommendations were concordant for both guidelines in 2422 participants (86.1%). While 361 (12.8%) were statin eligible based on ACC/AHA guidelines alone, only 29 (1.0%) were eligible by USPSTF alone, and 361 of 1404 African American individuals (25.7%) recommended for statin therapy under ACC/AHA guidelines were not recommended for statin therapy under USPSTF guidelines.
Statin Eligibility and Clinical Risk in Statin-Naive African American Individuals
Over a median 10-year follow-up (interquartile range, 9.1-10.7 years), we observed 123 (4.5%) incident ASCVD events (60 with coronary heart disease events and 63 with ischemic stroke; eTable 1 in the Supplement). We observed a 5.0-fold increased hazard of incident ASCVD (hazard ratio, 5.0; 95% CI, 3.3-7.4; P < .001) among statin-eligible participants by USPSTF guidelines vs noneligible participants and a 5.5-fold increased hazard of incident ASCVD (hazard ratio, 5.5; 95% CI, 3.4-8.8; P < .001) among statin-eligible participants by ACC/AHA guidelines (eFigure 2 in the Supplement). Importantly, those indicated for statins under both guidelines had a higher event rate than those indicated only under ACC/AHA guidelines (9.6 events per 1000 patient-years; 95% CI, 7.8-11.8; vs 4.1 events per 1000 patient-years; 95% CI, 2.4-6.9; P = .003).
Statin Eligibility and Subclinical Vascular Calcification
Of our overall cohort, 1743 (62.0%) underwent cardiac and abdominal CT for CAC and AAC scoring at visit 2. Participants in the CT subgroup were at lower ASCVD risk (eTable 2 in the Supplement). Nevertheless, coronary calcification was identified in 507 of 732 African American individuals (69.3%) by ACC/AHA guidelines compared with 404 (55.2%) by USPSTF guidelines (risk difference, 14.1%; 95% CI, 11.2-17.0; P < .001) and aortic calcification was identified in 681 of 1110 (61.4%) by ACC/AHA guidelines compared with 512 (46.1%) by USPSTF guidelines (risk difference, 15.2%; 95% CI, 12.9-17.5; P < .001) (Figure 1). We observed a 5-fold greater odds of detectable CAC (odds ratio, 5.1; 95% CI, 4.1-6.3; P < .001) and AAC (odds ratio, 5.4; 95% CI, 4.2-6.9; P < .001) among participants eligible for statins by USPSTF grade B guideline recommendations vs noneligible participants (Table 2). We observed a 5-fold greater odds of detectable CAC (odds ratio, 5.1; 95% CI, 4.1-6.3; P < .001) and a nearly 6-fold greater odds of detectable AAC (odds ratio, 5.8; 95% CI, 4.7-7.3; P < .001) among participants eligible for statins by ACC/AHA guidelines vs noneligible participants (Table 2).
Figure 1. Prevalence of Coronary and Aortic Vascular Calcification in African American Individuals.
AAC indicates abdominal aortic calcium; ACC/AHA, American College of Cardiology/American Heart Association; CAC, coronary artery calcium; USPSTF, US Preventive Services Task Force.
Table 2. Identification of Vascular Calcification by Statin Eligibility.
| Eligibility | CAC Score >0 (n = 732/1743) | C Statistic (95% CI) | CAC Score ≥100 (n = 310/1743) | C Statistic (95% CI) | AAC Score >0 (n = 1110/1742) | C Statistic (95% CI) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No./Total No. (%) | Statistic (95% CI) | P Value | No./Total No. (%) | Statistic (95% CI) | P Value | No./Total No. (%) | Statistic (95% CI) | P Value | ||||
| 2016 USPSTF Grade B Recommendation | 0.68 (0.66 to 0.70) | 0.71 (0.68 to 0.74) | 0.66 (0.64 to 0.68) | |||||||||
| Statin eligible | 404/600 (67.3) | 5.1 (4.1 to 6.3) | <.001 | 213/600 (35.5) | 5.9 (4.5 to 7.8) | <.001 | 512/599 (85.5) | 5.4 (4.2 to 6.9) | <.001 | |||
| Not statin eligible | 328/1143 (28.7) | 1 [Reference] | NA | 97/1143 (8.5) | 1 [Reference] | NA | 598/1143 (52.3) | 1 [Reference] | NA | |||
| 2013 ACC/AHA Guidelines | 0.69 (0.67 to 0.71) | 0.70 (0.68 to 0.73) | 0.70 (0.68 to 0.72) | |||||||||
| Statin eligible | 507/817 (62.1) | 5.1 (4.1 to 6.3) | <.001 | 248/817 (30.4) | 6.1 (4.5 to 8.2) | <.001 | 681/816 (83.5) | 5.8 (4.7 to 7.3) | <.001 | |||
| Not statin eligible | 225/926 (24.3) | 1 [Reference] | NA | 62/926 (6.7) | 1 [Reference] | NA | 429/926 (46.3) | 1 [Reference] | NA | |||
Abbreviations: AAC, abdominal aortic calcium; ACC/AHA, American College of Cardiology/American Heart Association; CAC, coronary artery calcium; USPSTF, US Preventive Services Task Force.
Although USPSTF guidelines did not provide overall better risk discrimination and net reclassification for the presence and extent of coronary calcification relative to ACC/AHA guidelines, USPSTF guidelines were significantly less sensitive (net reclassification index [for CAC], −14%; P < .001) and more specific (net reclassification index [for no CAC], 11%; P < .001) (Table 3). Statin eligibility by ACC/AHA guidelines provided better risk discrimination and net reclassification for the presence of aortic calcification (Table 3) (eTable 3 in the Supplement). The effect of statin eligibility by ACC/AHA guidelines vs USPSTF guidelines on risk of aortic calcification was primarily in correctly reclassifying individuals who had detectable AAC. Individuals with AAC were more often incorrectly reclassified by USPSTF statin eligibility guidelines.
Table 3. Statin Eligibility Comparison: 2016 USPSTF Grade B Recommendation vs 2013 ACC/AHA Recommendationa.
| Statistic | CAC Score >0 | P Value | CAC Score ≥100 | P Value | AAC Score >0 | P Value |
|---|---|---|---|---|---|---|
| Difference in C statistic | −0.01 (−0.03 to 0.004) | .12 | 0.007 (−0.02 to 0.03) | .58 | −0.04 (−0.05 to −0.02) | <.001 |
| NRI (CAC) | −0.03 (−0.06 to 0.007) | .14 | 0.01 (−0.04 to 0.06) | .59 | −0.08 (−0.11 to −0.04) | <.001 |
| Net % of individuals with CAC correctly reclassified by USPSTF (NRI CAC) | −14 | <.001 | −11 | <.001 | −15 | <.001 |
| Net % of individuals without CAC correctly reclassified by USPSTF (NRI No CAC) | 11 | <.001 | 13 | <.001 | 8 | <.001 |
Abbreviations: AAC, abdominal aortic calcium; ACC/AHA, American College of Cardiology/American Heart Association; CAC, coronary artery calcium score; NRI, net reclassification index; USPSTF, US Preventive Services Task Force.
Comparison of eligibility status was performed such that reclassification metrics and C statistics represent the improvement of 2016 USPSTF guidelines over 2013 ACC/AHA guidelines.
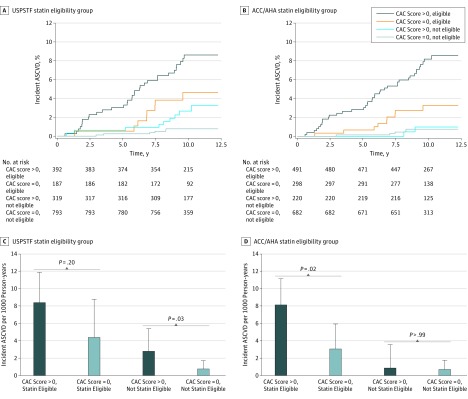
Calcium and Incident ASCVD
To understand whether the presence of CAC might influence contemporary clinical recommendations for statin use, we investigated the effect of adding calcification to statin eligibility on incident ASCVD. In the subgroup of 1743 participants with CT imaging (including those receiving statins at visit 2 but not receiving statins at visit 1), we observed 55 events (30 with coronary heart disease events and 25 with ischemic stroke) over a median 10-year follow-up. Participants in this subgroup who were statin eligible by USPSTF guidelines had a numerically higher but not statistically significant 10-year ASCVD event rate in the presence of CAC vs without CAC (8.4 per 1000 person-years; 95% CI, 5.9-11.9; vs 4.4 per 1000 person-years; 95% CI, 2.2-8.8; P = .20) (Figure 2). Participants not statin eligible by USPSTF guidelines had a higher ASCVD event rate in the presence of CAC vs without CAC (2.8 per 1000 person-years; 95% CI, 1.5-5.4; vs 0.8 per 1000 person-years; 95% CI, 0.3-1.7; P = .03) (Figure 2). Participants who were statin eligible by ACC/AHA guidelines experienced a higher 10-year ASCVD event rate in the presence of CAC vs without CAC (8.1 per 1000 person-years; 95% CI, 5.9-11.1; vs 3.1 per 1000 person-years; 95% CI, 1.6-5.9; P = .02) (Figure 2). Participants not statin eligible by ACC/AHA guidelines had a low 10-year ASCVD event rate regardless of CAC score (Figure 2).
Figure 2. Incident Atherosclerotic Cardiovascular Disease (ASCVD) Stratified by Calcification Status and Statin Eligibility.
A, Kaplan-Meier survival curves for incident ASCVD stratified by the presence of coronary artery calcification by US Preventive Services Task Force (USPSTF) statin eligibility groups. B, Kaplan-Meier survival curves for incident ASCVD stratified by presence of coronary artery calcification by American College of Cardiology/American Heart Association (ACC/AHA) statin eligibility groups. C, Incident ASCVD rate stratified by the presence of coronary artery calcium by USPSTF statin eligibility groups. D, Incident ASCVD rate stratified by the presence of coronary artery calcium by ACC/AHA statin eligibility groups. Comparison of event rates was performed using Poisson regression. Error bars indicate 95% CIs. CAC indicates coronary artery calcium.
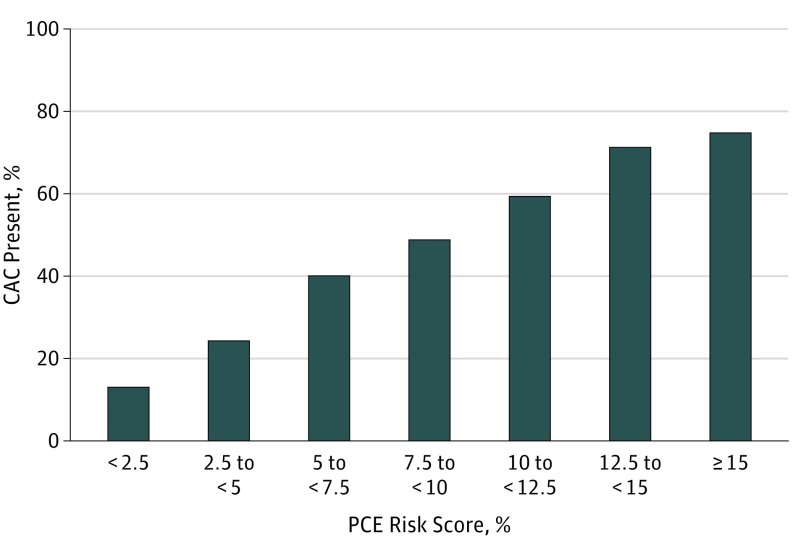
Distribution of CAC in Individuals Across PCE Risk Score
Given the proposed role for CAC to improve on PCE-directed statin recommendations, an important question is whether specific thresholds of 10-year risk score by PCE might influence decisions to perform CAC screening in African American individuals. To provide the broadest cohort for addressing this question, we included all 1417 JHS participants in our cohort who underwent CT imaging and had a measurable 10-year PCE risk score but did not qualify for statins by diabetes or by LDL-C level. Figure 3 shows the distribution of prevalent (nonzero) CAC scores across 10-year PCE risk scores. We observed a continuous increase in CAC prevalence across PCE risk scores. In gray-zone risk (5%-7.5% 10-year risk), only 86 of 214 African American individuals (40.2%) had CAC, whereas 162 of 220 (73.6%) harbored CAC in the group with more than 12.5% 10-year ASCVD risk.
Figure 3. Prevalence of Coronary Artery Calcification by Estimated Pooled Cohort Risk Equation (PCE) Risk Scores.
The frequency of nonzero coronary artery calcium (CAC) by PCE risk score was measured in 1417 statin-naive participants with available calcium scores, without diabetes, and with low-density lipoprotein cholesterol levels less than 190 mg/dL (to convert to millimoles per liter, multiply by 0.0259).
Discussion
In this large community-based cohort of African American adults, we identified 3 major findings central to prevention efforts. First, approximately 1 in 4 African American individuals recommended for statin therapy under ACC/AHA guidelines are no longer recommended for statin therapy under USPSTF guidelines. Individuals only eligible for statins under ACC/AHA guidelines experienced a low to intermediate event rate (equivalent to 4.1% per 10 years of patient follow-up), suggesting decreased sensitivity of the USPSTF recommendations in identifying participants at risk of ASCVD. Consequently, USPSTF guidelines focus treatment on a smaller high-risk cohort at the expense of missing significant numbers of African American individuals with vascular calcification (ie, increased specificity relative to ACC/AHA guidelines). Second, while those who were eligible for statins by both USPSTF and ACC/AHA guidelines had a similar hazard ratio of incident ASCVD compared with noneligible participants, the addition of CAC scoring improved risk stratification above guideline recommendations. Specifically, participants eligible for statin therapy under ACC/AHA guidelines with CAC were at higher risk than those without CAC. Conversely, participants not recommended for statins under USPSTF guidelines who had CAC experienced higher event rates than those without CAC. This suggests that CAC has the potential to personalize recommendation for statin therapy by both guideline recommendations. Finally, we detected CAC in 40.2% of individuals in the gray zone of PCE risk score (5%-7.5%) and in more than 70% of those with PCE risk scores greater than 12.5%. This observation supports guideline recommendations for subclinical ASCVD testing in individuals at intermediate risk while suggesting that there is a threshold of PCE risk score above which most African American individuals have CAC wherein testing may not be clinically expedient or cost efficient.
Alignment of contemporary statin prescription guidelines with noninvasive measures of ASCVD has been investigated in several cohorts worldwide. Work by Nasir et al in 2015 in the Multi-Ethnic Study of Atherosclerosis (MESA) demonstrated that more than 40% of statin-eligible individuals under ACC/AHA guidelines have a calcium score of 0, with a 5.2% 10-year ASCVD event rate (near the 5% 10-year event rate floor where ancillary testing is suggested by guidelines). In addition, investigators from the Heinz Nixdorf Recall study demonstrated in 2017 that CAC score may identify individuals at both higher and lower risk regardless of statin indication, suggesting that ancillary calcification testing may be clinically useful. Similarly, in 5805 participants in the BioImage study (mean age, 69 years), Mortensen et al reported that a CAC score of 0 was present in nearly 1 in 3 participants and forecasted a low incident ASCVD rate. We extend these results to newer USPSTF guidelines in African American individuals. In 1743 participants with calcium scoring in JHS, we found that while statin eligibility by either ACC/AHA (69%) or USPSTF (55%) guidelines captured a large fraction of individuals with coronary calcification, there remained a significant proportion of African American individuals with coronary calcification who were not identified by either guideline. In turn, among the participants not eligible for statins by USPSTF guidelines, the presence of CAC was associated with a greater risk of ASCVD; this was not the case for the ACC/AHA guidelines. Of note, while event rates in MESA (5.2%) and JHS (4.5%) were comparably low, there was potential value of CAC in improving risk stratification in both studies.
Strengths and Limitations
The strengths of our study are a large cohort of African American individuals with measurement of coronary and aortic calcification, detailed cardiovascular phenotyping, long follow-up, and careful event adjudication. While our event rates appeared low overall, they were consistent with prior work from several other multiracial epidemiologic studies with long-term follow-up. In an era of widespread use of statins in high-risk individuals, the PCEs may overestimate risk in the remaining pool of lower-risk individuals. Furthermore, an inherent limitation of the JHS study design is that CT imaging was performed in a (healthier) subgroup, introducing the possibility of referral bias, and that the timing of CT imaging was separated from the determination of statin eligibility. Nevertheless, we chose to use a “zero” vs “nonzero” CAC threshold, noting that individuals without CAC at visit 2 would necessarily be without CAC at visit 1. We recognize that this may exclude some individuals with interval development of calcification (itself a higher-risk scenario) or may focus on individuals who do not develop CAC over time (itself a lower-risk scenario). We excluded individuals with statin use at study baseline to target the population in whom statin therapy should be considered based on atherosclerotic disease risk. While therapeutic use is carefully classified in JHS (only 7% with incomplete recording of medications), the prevalence of statin therapy at baseline was low (11.3%), raising concern regarding possible confounding by participants who should have been prescribed statins but were not. However, the prevalence is similar to the 13% statin use observed in a large African American cohort of the Southern Community Cohort study, suggesting our estimates may resemble those of the general African American population prior to the release of 2013 guideline recommendations.
Conclusions
In conclusion, in a large cohort of African American individuals, we found that the clinical application of the USPSTF guidelines to determine statin eligibility focuses treatment on a smaller pool of high-risk individuals at the expense of missing many with vascular calcification and at low to intermediate risk compared with ACC/AHA guidelines and is associated with a similar increased hazard of incident ASCVD compared with ACC/AHA guidelines. Subclinical atherosclerosis remains associated with ASCVD events in statin-eligible African American individuals under ACC/AHA guidelines and in statin-ineligible African American individuals under USPSTF guidelines, suggesting that imaging may improve precision of modern guidelines. Finally, because presence of CAC increases across PCE-determined risk scores, bedside application of PCE risk score estimates may effectively identify intermediate-risk African American individuals in whom the addition of CAC scoring may have most value. Despite debate over the potential cost, risk calibration, and metabolic health implications of increasing statin use, these results support a guideline-based approach to statin recommendation, leveraging targeted imaging (or other surrogate atherosclerotic measures) in African American individuals to further personalize statin-based prevention programs.
eTable 1. Baseline characteristics of JHS participants stratified by inclusion vs exclusion from the study cohort.
eTable 2. Comparison of baseline characteristics by participation in CT scans.
eTable 3. Reclassification tables for coronary and abdominal aortic vascular calcification as a function of 2016 USPSTF vs 2013 ACC/AHA statin eligibility.
eFigure 1. Construction of JHS analytic cohorts used in the study.
eFigure 2. Kaplan-Meier survival analysis for combined incident ASCVD.
References
- 1.Mozaffarian D, Benjamin EJ, Go AS, et al. ; American Heart Association Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics–2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29-e322. [DOI] [PubMed] [Google Scholar]
- 2.Safford MM, Brown TM, Muntner PM, et al. ; REGARDS Investigators . Association of race and sex with risk of incident acute coronary heart disease events. JAMA. 2012;308(17):1768-1774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stone NJ, Robinson JG, Lichtenstein AH, et al. ; American College of Cardiology/American Heart Association Task Force on Practice Guidelines . 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25, suppl 2):S1-S45. [DOI] [PubMed] [Google Scholar]
- 4.Grundy SM, Cleeman JI, Merz CN, et al. ; Coordinating Committee of the National Cholesterol Education Program . Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III Guidelines. J Am Coll Cardiol. 2004;44(3):720-732. [DOI] [PubMed] [Google Scholar]
- 5.Pencina MJ, Navar-Boggan AM, D’Agostino RB Sr, et al. . Application of new cholesterol guidelines to a population-based sample. N Engl J Med. 2014;370(15):1422-1431. [DOI] [PubMed] [Google Scholar]
- 6.Pursnani A, Massaro JM, D’Agostino RB Sr, O’Donnell CJ, Hoffmann U. Guideline-based statin eligibility, coronary artery calcification, and cardiovascular events. JAMA. 2015;314(2):134-141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nasir K, Bittencourt MS, Blaha MJ, et al. . Implications of coronary artery calcium testing among statin candidates according to American College of Cardiology/American Heart Association cholesterol management guidelines: MESA (Multi-Ethnic Study of Atherosclerosis) [published correction appears in J Am Coll Cardiol. 2015;66(23):2686]. J Am Coll Cardiol. 2015;66(15):1657-1668. [DOI] [PubMed] [Google Scholar]
- 8.Bibbins-Domingo K, Grossman DC, Curry SJ, et al. ; US Preventive Services Task Force . Statin use for the primary prevention of cardiovascular disease in adults: US Preventive Services Task Force recommendation statement. JAMA. 2016;316(19):1997-2007. [DOI] [PubMed] [Google Scholar]
- 9.Taylor HA Jr, Wilson JG, Jones DW, et al. . Toward resolution of cardiovascular health disparities in African Americans: design and methods of the Jackson Heart Study. Ethn Dis. 2005;15(4, suppl 6):S6-S4, 17. [PubMed] [Google Scholar]
- 10.Fuqua SR, Wyatt SB, Andrew ME, et al. . Recruiting African-American research participation in the Jackson Heart Study: methods, response rates, and sample description. Ethn Dis. 2005;15(4, suppl 6):S6-S18, 29. [PubMed] [Google Scholar]
- 11.American Diabetes Association Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33(suppl 1):S62-S69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Carpenter MA, Crow R, Steffes M, et al. . Laboratory, reading center, and coordinating center data management methods in the Jackson Heart Study. Am J Med Sci. 2004;328(3):131-144. [DOI] [PubMed] [Google Scholar]
- 13.Goff DC Jr, Lloyd-Jones DM, Bennett G, et al. ; American College of Cardiology/American Heart Association Task Force on Practice Guidelines . 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25, suppl 2):S49-S73. [DOI] [PubMed] [Google Scholar]
- 14.Sung JH, Yeboah J, Lee JE, et al. . Diagnostic value of coronary artery calcium score for cardiovascular disease in African Americans: the Jackson Heart Study. Br J Med Med Res. 2016;11(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Carr JJ, Nelson JC, Wong ND, et al. . Calcified coronary artery plaque measurement with cardiac CT in population-based studies: standardized protocol of Multi-Ethnic Study of Atherosclerosis (MESA) and Coronary Artery Risk Development in Young Adults (CARDIA) study. Radiology. 2005;234(1):35-43. [DOI] [PubMed] [Google Scholar]
- 16.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15(4):827-832. [DOI] [PubMed] [Google Scholar]
- 17.Keku E, Rosamond W, Taylor HA Jr, et al. . Cardiovascular disease event classification in the Jackson Heart Study: methods and procedures. Ethn Dis. 2005;15(4, suppl 6):S6-S62, 70. [PubMed] [Google Scholar]
- 18.Pencina MJ, D’Agostino RB. Overall C as a measure of discrimination in survival analysis: model specific population value and confidence interval estimation. Stat Med. 2004;23(13):2109-2123. [DOI] [PubMed] [Google Scholar]
- 19.Pencina MJ, D’Agostino RB Sr, D’Agostino RB Jr, Vasan RS. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med. 2008;27(2):157-172, 207-212. [DOI] [PubMed] [Google Scholar]
- 20.Fox ER, Samdarshi TE, Musani SK, et al. . Development and validation of risk prediction models for cardiovascular events in black adults: the Jackson Heart Study Cohort. JAMA Cardiol. 2016;1(1):15-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mahabadi AA, Möhlenkamp S, Lehmann N, et al. ; Heinz Nixdorf Recall Study Investigators . CAC score improves coronary and CV risk assessment above statin indication by ESC and AHA/ACC primary prevention guidelines. JACC Cardiovasc Imaging. 2017;10(2):143-153. [DOI] [PubMed] [Google Scholar]
- 22.Mortensen MB, Fuster V, Muntendam P, et al. . A simple disease-guided approach to personalize ACC/AHA-recommended statin allocation in elderly people: the BioImage Study. J Am Coll Cardiol. 2016;68(9):881-891. [DOI] [PubMed] [Google Scholar]
- 23.Lipworth L, Fazio S, Kabagambe EK, et al. . A prospective study of statin use and mortality among 67,385 blacks and whites in the Southeastern United States. Clin Epidemiol. 2013;6:15-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pandya A, Sy S, Cho S, Weinstein MC, Gaziano TA. Cost-effectiveness of 10-year risk thresholds for initiation of statin therapy for primary prevention of cardiovascular disease. JAMA. 2015;314(2):142-150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.DeFilippis AP, Blaha MJ. Predicted vs observed clinical event risk for cardiovascular disease. JAMA. 2015;314(19):2082. [DOI] [PubMed] [Google Scholar]
- 26.Preiss D, Seshasai SR, Welsh P, et al. . Risk of incident diabetes with intensive-dose compared with moderate-dose statin therapy: a meta-analysis. JAMA. 2011;305(24):2556-2564. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Baseline characteristics of JHS participants stratified by inclusion vs exclusion from the study cohort.
eTable 2. Comparison of baseline characteristics by participation in CT scans.
eTable 3. Reclassification tables for coronary and abdominal aortic vascular calcification as a function of 2016 USPSTF vs 2013 ACC/AHA statin eligibility.
eFigure 1. Construction of JHS analytic cohorts used in the study.
eFigure 2. Kaplan-Meier survival analysis for combined incident ASCVD.