Key Points
Question
What is the association between the trans-fatty acid restrictions in New York State and hospital admissions for myocardial infarction and stroke?
Findings
In this study using data from the New York State Department of Public Health (2002-2013), there was an additional 6.2% decline in hospital admissions for myocardial infarction and stroke among populations living in counties with vs without trans-fatty acid restrictions. The decline in events reached statistical significance 3 or more years after restrictions were implemented.
Meaning
Restrictions on trans-fatty acid consumption are associated with a decrease in hospitalization for cardiovascular events.
Abstract
Importance
Trans-fatty acids (TFAs) have deleterious cardiovascular effects. Restrictions on their use were initiated in 11 New York State (NYS) counties between 2007 and 2011. The US Food and Drug Administration plans a nationwide restriction in 2018. Public health implications of TFA restrictions are not well understood.
Objective
To determine whether TFA restrictions in NYS counties were associated with fewer hospital admissions for myocardial infarction (MI) and stroke compared with NYS counties without restrictions.
Design, Setting, and Participants
We conducted a retrospective observational pre-post study of residents in counties with TFA restrictions vs counties without restrictions from 2002 to 2013 using NYS Department of Health’s Statewide Planning and Research Cooperative System and census population estimates. In this natural experiment, we included those residents who were hospitalized for MI or stroke. The data analysis was conducted from December 2014 through July 2016.
Exposure
Residing in a county where TFAs were restricted.
Main Outcomes and Measures
The primary outcome was a composite of MI and stroke events based on primary discharge diagnostic codes from hospital admissions in NYS. Admission rates were calculated by year, age, sex, and county of residence. A difference-in-differences regression design was used to compare admission rates in populations with and without TFA restrictions. Restrictions were only implemented in highly urban counties, based on US Department of Agriculture Economic Research Service Urban Influence Codes. Nonrestriction counties of similar urbanicity were chosen to make a comparison population. Temporal trends and county characteristics were accounted for using fixed effects by county and year, as well as linear time trends by county. We adjusted for age, sex, and commuting between restriction and nonrestriction counties.
Results
In 2006, the year before the first restrictions were implemented, there were 8.4 million adults (53.6% female) in highly urban counties with TFA restrictions and 3.3 million adults (52.3% female) in highly urban counties without restrictions. Twenty-five counties were included in the nonrestriction population and 11 in the restriction population. Three or more years after restriction implementation, the population with TFA restrictions experienced significant additional decline beyond temporal trends in MI and stroke events combined (−6.2%; 95% CI, −9.2% to −3.2%; P < .001) and MI (−7.8%; 95% CI, −12.7% to −2.8%; P = .002) and a nonsignificant decline in stroke (−3.6%; 95% CI, −7.6% to 0.4%; P = .08) compared with the nonrestriction populations.
Conclusions and Relevance
The NYS populations with TFA restrictions experienced fewer cardiovascular events, beyond temporal trends, compared with those without restrictions.
This study determines whether trans-fatty acid restrictions in New York State counties were associated with fewer hospital admissions for myocardial infarction and stroke compared with counties without restrictions.
Introduction
Industrial trans-fatty acids (TFAs) remain a significant part of American diets. Consumption of TFAs is associated with an elevated risk for cardiovascular disease (CVD). Trans-fatty acids are modified unsaturated fats with a trans- double bond in place of a cis- double bond. Trans-fatty acids primarily enter the diet via partially hydrogenated oils (PHOs) used in baked goods, yeast breads, fried foods, chips, crackers, and margarine. Consumption of TFAs is associated with unfavorable physiologic changes, including reduced high-density lipoprotein cholesterol and increased low-density lipoprotein cholesterol levels, triglycerides, markers of systemic inflammation (C-reactive protein, interleukin 6, and tumor necrosis factor α), and endothelial cell dysfunction. Observational studies have shown that higher TFA consumption is associated with elevated risk for stroke, coronary heart disease, and sudden cardiac death.
Given the deleterious effects of TFAs, many have advocated minimizing or eliminating their use. On June 16, 2015, the US Food and Drug Administration (FDA) revoked the “Generally Recognized As Safe” status of PHOs. The FDA’s measure takes effect in 2018 and prohibits unrestricted use of PHOs in all food without prior approval, therefore nearly eliminating industrial TFAs from American diets. Pending a final amendment to revoke the “Generally Recognized as Safe” status of 2 PHOs that are not commonly used in food products, menhaden and low erucic acid rapeseed oil, this restriction will be comprehensive to all PHOs.
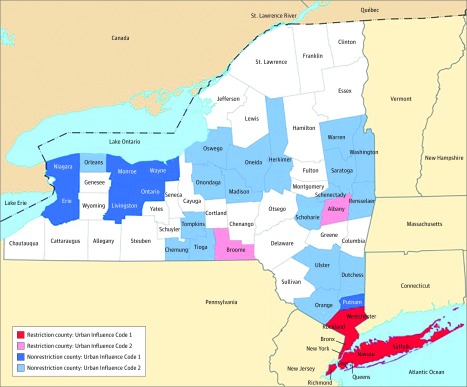
Many years prior to the FDA decision to restrict PHOs, local authorities took action to reduce exposure. New York City (NYC) was the first large metropolitan area in the United States to restrict TFAs in eateries, starting July 1, 2007. Eateries included restaurants, bakeries, caterers, cafeterias, senior-meal programs, mobile food-vending units, soup kitchens, park concessions, street-fair food booths, and others. Similar TFA restrictions were subsequently enacted in additional New York State (NYS) counties, including Westchester (January 15, 2008), Nassau (April 1, 2008), Albany (January 1, 2009), Suffolk (October 28, 2010), Rockland (January 1, 2011), and Broome (December 1, 2011) (Figure 1). While restricting TFAs in eateries substantially reduced exposure to TFAs, they could still be found in packaged foods.
Figure 1. Highly Urban New York State Counties With and Without Trans-Fatty Acid Restrictions.
Modified New York State county map courtesy of the US Geological Survey (modified by the author).Urban Influence Codes were obtained from the US Department of Agriculture Economic Research Service 2003 data collections for Urban Influence Code. Urban Influence Code 1 represents large metropolitan areas with at least 1 million residents. Urban Influence Code 2 represents small metropolitan areas with fewer than 1 million residents. Counties with restrictions include Bronx, Kings, New York, Queens, and Richmond starting on July 1, 2007; Westchester on January 15, 2008; Nassau on April 1, 2008; Albany on January 1, 2009; Suffolk on October 28, 2010; Rockland on January 1, 2011; and Broome on December 1, 2011.
Reduction in TFA consumption is associated with meaningful clinical outcomes. Restrepo and Rieger reported a 4.5% reduction in CVD mortality in counties with TFA restrictions within 1 year after restrictions. The decline in CVD mortality rates translated to 13 fewer CVD deaths per 100 000 persons per year after the restrictions were enacted. However, nonfatal events were not reported. Therefore, we sought to determine the association of TFA restrictions with MI and stroke events. We hypothesized that NYS populations with TFA restrictions experienced a reduction in both MI and stroke events compared with populations without TFA restrictions.
Methods
Included Data
Annual hospital admissions for MI and stroke in all 62 NYS counties were tracked from January 1, 2002, to December 31, 2013, using data from the NYS Department of Health’s Statewide Planning and Research Cooperative System (SPARCS) limited inpatient data set. Nonfederal public and private hospitals certified for inpatient care in NYS are required to submit data for all inpatient admissions. The International Classification of Diseases, Ninth Revision, Clinical Modification diagnostic codes 410.00 through 410.99 and 430.00 through 438.99 were used to identify principal admission diagnoses of MI or stroke, respectively, which were established at discharge. The SPARCS data do not specify whether events were incident or recurrent. Annual MI and stroke hospitalization rates were calculated by decade of age (starting at 25 years), sex, and county using yearly census population estimates as the denominator. Patients’ primary zip code of residence, not hospital zip code, determined county of residence to ensure that patients were correctly classified as living in TFA restriction vs nonrestriction counties. Adults whose zip code of residence was outside of NYS were excluded.
The study was approved by the University of Chicago institutional review board. This analysis used deidentified clinical data from SPARCS data of the NYS Department of Health, so participant consent was not required. Data analysis was conducted from December 2014 through July 2016.
Comparison Groups
We sought to determine whether changes in MI and stroke events after TFA restrictions extended beyond temporal trends. To construct populations for comparison, we used 2003 and 2013 US Department of Agriculture Economic Research Service Urban Influence Codes (UICs) to determine county urbanicity. All counties with TFA restrictions had the highest urbanicity classifications as UIC-1 (large metropolitan area of >1 million residents) or UIC-2 (small metropolitan area of <1 million residents) in both 2003 and 2013. Thus, we only included hospital admission data from counties without TFA restrictions that were classified as UIC-1 or UIC-2 in both 2003 and 2013. In 2 sensitivity analyses, we restricted the analysis to counties with UIC-1 in both 2003 and 2013 and then excluded NYC from this analysis.
We measured multiple factors to compare populations living in counties with and without TFA restrictions. We used estimates from the US Census and Centers for Disease Control and Prevention in 2006—the year before the first TFA restriction—to calculate the proportion of women, black individuals, Hispanic individuals, and adults aged 45 to 65 and older than 65 years. We also calculated the median income for counties (reported as range of median incomes), as well as age-adjusted rates of total mortality, MI, and stroke events, standardized to the national 2010 population. Standard differences (Cohen term d, calculated as the difference in means divided by the pooled SD) were reported to compare the restriction and nonrestriction populations, wherein absolute values can be interpreted as small (0.2), medium (0.5), or large (≥0.8).
Statistical Analysis
To distinguish between changes related to TFA restrictions and temporal trends, we used a difference-in-differences negative binomial regression strategy. The difference-in-differences approach compares trends in admission rates before and after TFA restrictions in counties with and without restrictions. The approach is designed to study 2 populations that may not have the same absolute event rates but do have parallel trends in event rates before 1 population experiences an intervention. The key assumption is that if 2 populations had parallel trends in the past, these parallel trends would have continued in the absence of an intervention. Therefore, if one population undergoes an intervention, data from the other population can be used to predict what would have occurred in that population without the intervention. One can then measure the difference between the observed and expected differences between groups. The difference-in-differences approach represents the change attributable to the intervention (eFigure 1 in Supplement). We tested for parallel trends in admission rates prior to 2007, the year the first TFA restriction was enacted, using negative binomial regression models.
The assumption of parallel trends before the policy change is necessary but not sufficient to ascertain the internal validity of the method. Additional potential confounding due to differences in counties with and without TFA restrictions was addressed in several ways. First, by adding county fixed effects, we controlled for unobserved county characteristics that remained unbalanced (but remained fixed over time) across the study period. As such, we used within-county variation to compare hospital admissions before vs after each TFA restriction occurred, which allowed us to account for different periods of TFA restriction implementation. Second, we accounted for prerestriction MI and stroke event rates by adding linear trends at the county level. Third, year fixed effects were incorporated to control for year-specific shifts, such as economic changes, which could affect restaurant use. We clustered SEs to account for the repeated observations at the county level.
We also accounted for commuting between counties with and without TFA restrictions because commuters from nonrestriction counties into a restriction county would be exposed to a TFA restriction if they ate restaurant meals near their workplace. To account for commuting in the model, we added 2 variables as controls in the regression, capturing the proportion of the adult population commuting from counties with TFA restrictions to counties without TFA restrictions and vice versa. The proportion of adults that commutes between counties with and without TFA restrictions was determined using data from the American Community Survey’s Commuting Worker Flows. The American Community Survey tracks a population’s county of residence and county of work. Estimates from 2006-2010 and 2009-2013 were used. In overlapping years, we used an average of the 2 estimates.
Our primary outcome was a composite of MI and stroke event rates. Secondary outcomes were MI and stroke individually. Negative binomial regression models were used in which events were modeled as rates per population, adjusting for decade of age, sex, county, year, and commuting between counties; linear time trends (estimated separately for each county); and exposure to TFA restrictions. Events and population counts were tabulated by age, sex, year, and county for inclusion in the model. Given that there may be a delay between change in TFA consumption and its association with cardiovascular events, we report results at 1 year, 2 years, and 3 or more years after restrictions were implemented.
In some counties, the TFA restrictions were implemented in 2 phases. For example, on July 1, 2007, phase 1 of the NYC restriction eliminated using PHOs for frying, pan-frying, grilling, or as a spread. Partially hydrogenated oils used for deep-frying, cake batter, and yeast dough were permitted until phase 2, which began July 1, 2008. When applicable, phase 1 implementation dates were used because this was the earliest date of reduced TFA exposure. Restriction start dates for all counties were assumed to start at the nearest half-year to the effective restriction date.
We performed sensitivity analyses to ensure NYC did not drive the results. Because all NYC counties are UIC-1, we first restricted the analyses to UIC-1 counties. We then repeated the analysis after excluding NYC. We examined the effect of data specifically after excluding NYC for 2 reasons. First, NYC had the longest exposure to a TFA restriction. Second, NYC also implemented other public health measures during our period of observation, such as smoking and food menu regulations, which could have affected rates of MI and stroke.
The analyses were performed using Stata version 14 (StataCorp). For all analyses, a 2-tailed P < .05 was considered statistically significant.
Results
Population Characteristics
In the UIC-1 populations, there were 9 counties with TFA restrictions and 8 counties without restrictions. In the UIC-2 populations, there were 2 counties with TFA restrictions and 17 counties without restrictions, giving a total study sample of 11 counties with restrictions and 25 without restrictions. Figure 1 provides a map of counties included in the analyses.
Characteristics of the study populations are shown in Table 1. When comparing TFA restriction and nonrestriction populations (UIC-1 or UIC-2), they were most similar on age-adjusted MI and stroke rates. There were large differences between the TFA restriction and nonrestriction populations in the proportion of black and Hispanic adults (Table 1). The results were similar when we compared only UIC-1 populations (eTable 1 in the Supplement). When excluding NYC from UIC-1 populations, the population characteristics were similar, although the difference in the proportion of black adults between populations with and without TFA restrictions was smaller (eTable 1 in the Supplement).
Table 1. 2006 Characteristics of Populations in UIC-1 or -2 New York State Populations With vs Without Subsequent TFA Restrictionsa.
| Characteristic | Population | Standard Differenceb | |
|---|---|---|---|
| Nonrestriction (n = 3 317 642) |
Restriction (n = 8 419 441) |
||
| Age-adjusted rate (per 100 000) | |||
| Mortality | 1199 | 1085 | −0.10 |
| MI and stroke combined | 753 | 726 | −0.04 |
| MI | 316 | 293 | −0.08 |
| Stroke | 437 | 433 | −0.01 |
| Proportion of population age | |||
| >65 y | 0.21 | 0.15 | −0.41 |
| 45-65 y | 0.40 | 0.29 | −0.50 |
| Proportion of demographic group | |||
| Male | 0.52 | 0.49 | −0.12 |
| Hispanic | 0.04 | 0.25 | 1.30 |
| Black | 0.09 | 0.29 | 1.10 |
| Median county income, US $ | |||
| Minimum | 38 601 | 31 498 | NA |
| Maximum | 82 058 | 85 537 | NA |
| Cases, No. (%) | |||
| MIs | 9300 (0.3) | 19 076 (0.2) | NA |
| Strokes | 14 512 (0.4) | 31 203 (0.4) | NA |
Abbreviations: MI, myocardial infarction; NA, not applicable; TFA, trans-fatty acid; UIC, Urban Influence Code.
Data sources include the US Centers for Disease Control and Prevention (2006), Census (2006), and Department of Agriculture Economic Research Service (2003 and 2013) UIC. UIC-1 represents large metropolitan areas with at least 1 million residents. UIC-2 represents small metropolitan areas with fewer than 1 million residents.
Standard differences are calculated from the difference in means divided by the pooled SD. Therefore, standard differences are reported as positive values when proportions or rates are higher in restriction populations vs nonrestriction populations and negative when proportions or rates are higher in nonrestriction populations vs restriction populations.
Baseline Trends in Cardiovascular Events
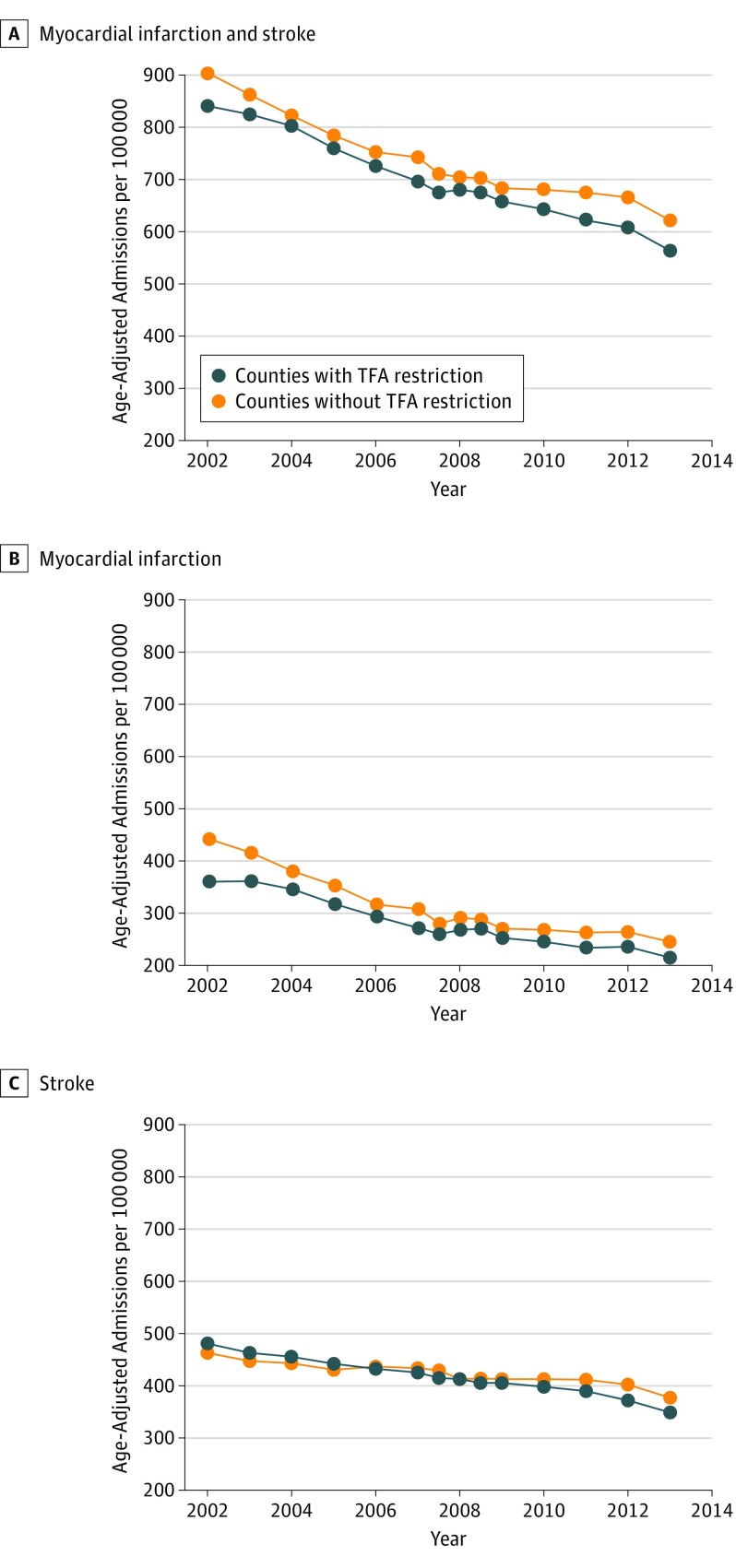
Before TFA restrictions, annual admission rates were already declining across the state (Figure 2). Trends in admissions for MI and stroke event rates combined, MI, and stroke before implementation of TFA restrictions were comparable between the populations with and without TFA restrictions in all analyses (Figure 2; Table 2; eFigure 2 in the Supplement).
Figure 2. Temporal Trends in Myocardial Infarction and Stroke Event Rates in Urban Influence Codes 1 or 2 New York State Populations With and Without Subsequent Trans-Fatty Acid (TFA) Restrictions.
Each point corresponds to an annual admission rate. Years 2007 and 2008 have points corresponding to each half year during the period of multiple restriction implementations. Data are age-adjusted to the national population in 2010.
Table 2. Slopes of Hospital Admission Rates Before Implementation of TFA Restrictions (2002-2006) Between Populations With vs Without Subsequent TFA Restrictions.
| Group | Population Change in Events/100 000/y (SE)a | P Value for Difference Between Slopes | |
|---|---|---|---|
| Nonrestriction | Restriction | ||
| UIC-1 or -2 Populationsb | |||
| Myocardial infarction and stroke | −38.0 (6.6) | −28.9 (8.0) | .93 |
| Myocardial infarction | −31.4 (4.5) | −16.8 (5.4) | .70 |
| Stroke | −6.6 (2.9) | −12.1 (3.4) | .66 |
| UIC-1 Populationsb | |||
| Myocardial infarction and stroke | −42.2 (12.1) | −29.2 (8.1) | .95 |
| Myocardial infarction | −35.7 (8.0) | −16.9 (5.5) | .64 |
| Stroke | −6.5 (5.2) | −12.3 (3.4) | .74 |
| UIC-1 Populations, Excluding NYCb | |||
| Myocardial infarction and stroke | −42.2 (12.6) | −37.9 (13.4) | .92 |
| Myocardial infarction | −35.7 (8.4) | −24.2 (9.6) | .84 |
| Stroke | −6.5 (5.4) | −13.7 (4.8) | .73 |
Abbreviations: NYC, New York City; TFA, trans-fatty acids; UIC, Urban Influence Code.
Data are age adjusted. SEs for age-adjusted slopes are calculated using 1000 bootstrap samples.
Population urban status is defined by US Department of Agriculture Economic Research Service (2003 and 2013) UICs. UIC-1 represents large metropolitan areas with at least 1 million residents. UIC-2 represents small metropolitan areas with fewer than 1 million residents.
Cardiovascular Events After Trans-Fatty Acid Restrictions
By 3 or more years after TFA restrictions were enacted, there was a significant additional decline in admissions for the primary end point of MI and stroke combined (−6.2%; 95% CI, −9.2% to −3.2%; P < .001) beyond temporal trends in UIC-1 or UIC-2 populations with vs without TFA restrictions. The decline in events equates to 43 events averted per 100 000. For secondary end points, there was a significant decline in MI (−7.8%; 95% CI, −12.7% to −2.8%; P = .002) and a nonsignificant decline in stroke (−3.6%; 95% CI, −7.6% to 0.4%; P = .08) (Table 3). Results were similar for both men and women (Table 3).
Table 3. Additional Change in Hospital Admission for Myocardial Infarction and Stroke in New York State Populations With vs Without Subsequent TFA Restrictions.
| Group | Postrestriction, % (95% CI) | |||||
|---|---|---|---|---|---|---|
| 1 y | P Value | 2 y | P Value | ≥3 y | P Value | |
| Myocardial Infarction and Stroke Combineda | ||||||
| UIC-1 or UIC-2 | −0.6 (−5.6 to 4.5) | .83 | 6.0 (−13.6 to 1.7) | .13 | −6.2 (−9.2 to −3.2) | <.001b |
| Men | −1.1 (−7.1 to 4.8) | .71 | −6.4 (−15.0 to 2.3) | .14 | −5.8 (−8.9 to −2.7) | <.001b |
| Women | 0.0 (−5.2 to 5.2) | .99 | −5.5 (−13.9 to 2.9) | .20 | −6.7 (−9.9 to −3.5) | <.001b |
| Sensitivity analyses | ||||||
| UIC-1 only | −0.9 (−7.3 to 5.5) | .78 | −7.8 (−18.2 to 2.5) | .13 | −6.6 (−10.2 to −3.0) | <.001b |
| UIC-1 only, excluding NYC | −8.2 (−16.6 to 0.2) | .05 | −9.0 (−17.3 to −0.7) | .03b | −7.0 (−12.5 to −1.6) | .01b |
| Myocardial Infarctiona | ||||||
| UIC-1 or UIC-2 | 3.1 (−3.2 to 9.4) | .34 | −7.6 (−14.0 to −1.1) | .02b | −7.8 (−12.7 to −2.8) | .002b |
| Men | 0.7 (−6.4 to 7.7) | .85 | −7.6 (−16.6 to 1.4) | .09 | −7.6 (−12.2 to −3.0) | .001b |
| Women | 5.8 (−2.4 to 13.9) | .16 | −7.8 (−15.8 to 0.3) | .05 | −8.0 (−14.1 to −1.9) | .01b |
| Sensitivity analyses | ||||||
| UIC-1 only | 2.5 (−4.8 to 9.8) | .50 | −8.7 (−17.7 to 0.4) | .06 | −8.7 (−15.7 to −1.6) | .01b |
| UIC-1 only, excluding NYC | −4.5 (−11.0 to 2.0) | .17 | −7.3 (−14.0 to −0.8) | .03b | −6.4 (−12.7 to −0.1) | .04b |
| Strokea | ||||||
| UIC-1 or UIC-2 | −2.5 (−8.5 to 3.5) | .41 | −4.7 (−14.3 to 4.8) | .32 | −3.6 (−7.6 to 0.4) | .08 |
| Men | −2.9 (−9.9 to 4.1) | .42 | −6.1 (−15.6 to 3.4) | .20 | −2.7 (−7.2 to 1.9) | .24 |
| Women | −2.1 (−8.1 to 3.9) | .49 | −3.4 (−14.4 to 7.5) | .53 | −4.5 (−8.4 to −0.6) | .02b |
| Sensitivity analyses | ||||||
| UIC-1 only | −2.7 (−10.2 to 4.7) | .47 | −6.6 (−18.3 to 5.1) | .26 | −3.7 (−7.9 to 0.5) | .08 |
| UIC-1 only, excluding NYC | −9.7 (−22.0 to 2.5) | .11 | −9.0 (−19.8 to 1.7) | .10 | −6.3 (−12.9 to 0.4) | .06 |
Abbreviations: NYC, New York City; TFA, trans-fatty acid; UIC, Urban Influence Code.
Data are adjusted for county-level trends, county and year fixed effects, age, sex, and commuting into or out of counties with TFA restrictions.
Significant value (P < .05).
In the sensitivity analyses, when we restricted the sample to UIC-1 populations and also excluded NYC from UIC-1 populations, the results were unchanged (Table 3). For sensitivity analyses results stratified by sex, see eTable 2 in the Supplement.
Discussion
Myocardial infarction and stroke rates were already declining across NYS prior to the first TFA restrictions. After 2006, populations in NYS with TFA restrictions experienced a significant additional decline in rates of hospital admissions for MI and stroke rates combined compared with populations without TFA restrictions, beyond what would have been expected based on temporal trends. The significant decline in events became apparent 3 or more years after the restrictions were implemented. Both men and women experienced a significant decline in events. To our knowledge, this is the first study examining the association between TFA restrictions in NYS with MI and stroke.
Consumption of TFAs has been shown to increase the risk for coronary heart disease and stroke over 6 or more years of follow-up. Just 2 g of daily TFA consumption portends significant risk for CVD; complete avoidance may be necessary to avert risk. However, it is possible to reach significant TFA intake with just 1 food item. For example, a large order of Popeye’s Louisiana Kitchen cajun fries contains 3.5 g of TFAs per serving, Taco Bell’s Cinnabon Delights (12-pack) contain 2.0 g of TFAs per serving, and multiple varieties of Pillsbury Shape sugar cookies contain 2.5 g of TFAs per serving. Studies after the NYS restrictions found a clinically meaningful reduction in TFA exposure. For example, a random sample of fast-food purchases in NYC suggested that TFA consumption decreased by an average of 2.4 g per meal between 2007 and 2009. Additionally, 16 months after implementation of phase 1 of the NYC TFA restriction, use of TFAs had decreased from 50% of restaurants to less than 2%. In Nassau County, 81% of randomly inspected food service establishments were compliant within 3 to 5 months after TFA restriction implementation.
Our results complement those of previous analyses. For example, Restrepo and Rieger used US Centers for Disease Control and Prevention mortality data to demonstrate that TFA restrictions in NYS were associated with a reduction in CVD mortality. Also similar to our study, the authors found that the reduction in heart disease mortality (11 per 100 000 persons/year) was larger than the reduction in stroke mortality (2 per 100 000 persons/year). Furthermore, the reduction in MI that we observed falls within the predicted bounds by Mozaffarian et al, who estimated that near elimination of TFAs from diets would prevent 6% to 19% of coronary heart disease events.
It is important to consider other public health measures that coincided with the TFA restrictions and could have affected rates of MI and stroke. To our knowledge, there were 2 relevant measures in NYC: the 2011 extension of the Smoke-Free Air Act, which extended smoking bans to parks, beaches, and pedestrian plazas, and the 2008 measure to post caloric content on food menus. However, our results remained significant for UIC-1 populations when excluding NYC from the analyses. As a result, it is unlikely that our results were confounded by the public health measures.
It is possible that our results are related to unmeasured differences between the 2 groups. For example, using data from the Behavioral Risk Factor Surveillance System, Restrepo and Rieger showed that while rates of obesity, smoking, and alcohol use were lower in restriction vs nonrestriction counties, physical activity was also lower in restriction vs nonrestriction counties. However, adjusting for the differences in lifestyle factors between restriction and nonrestriction counties did not alter the authors’ results. In addition, both Restrepo and Rieger’s analysis and ours included county-level fixed effects and county-specific linear time trends to adjust for differences between counties. Nevertheless, there could still be residual confounding.
It is notable that the reduction in MI and stroke rates occurred after TFA restrictions that only included limiting of TFA consumption from eateries. Consumers could be exposed to TFA from other products not included in the restriction. For example, in grocery stores, foods labeled as 0 g of TFAs per serving may contain up to 0.49 g of TFAs based on current labeling guidelines. Our results show the potential benefit of the FDA’s comprehensive restriction on PHOs, which is the source of TFAs in most packaged food.
Strengths
Our study has a number of strengths. Our analyses are comprehensive, as SPARCS data include admissions from all nonfederal hospitals in NYS. Events were classified according to each adult’s county of residence rather than the hospital location, allowing tracking of events based on restriction exposure. The benefit of the difference-in-differences approach is that population-level factors that differ between comparison groups do not bias the results as long as trends between the comparison groups would have remained parallel in the absence of an intervention. Prerestriction trends were similar across populations with vs without TFA restrictions. Furthermore, we accounted for additional exposure to TFA restrictions by adjusting for commuting between restriction and nonrestriction counties. Last, the effect of the restriction exhibited a dose-response by time, wherein there was typically greater degree of decline and significance of decline in events with the passage of time, which is the biologically expected response to cardiovascular risk factor modification.
Limitations
Our study has limitations. First, we were not able to assess population-level changes in TFA consumption. Second, race/ethnicity was poorly reported in SPARCS and so we did not adjust for it or stratify results by race/ethnicity. However, county-level indicators and time trends helped to adjust for differences across populations with vs without TFA restrictions, such as differences in racial/ethnic composition of the population. Also, despite differences in race/ethnicity, slopes were not different between populations with and without TFA restrictions. Third, MI and stroke events that did not result in hospital admission within NYS were not captured. Fourth, although we control for linear trends over time on the county level, additional differences between comparison counties could have developed over time that were not accounted for in our analysis.
Conclusions
Our results suggest that the NYS restrictions on TFAs in eateries were associated with an accelerated decline in hospital admissions for MI and stroke. The difference between TFA restriction and nonrestriction populations was significant 3 or more years after restriction implementation.
eTable 1. 2006 Characteristics of Urban Influence Code-1 New York State Counties With and Without Trans-Fatty Acid Restrictions.
eTable 2. Additional Change in Hospital Admission for MI and Stroke, in Populations With vs Without Subsequent TFA Restrictions Stratified by Sex.
eFigure 1. Theoretical Example of the Difference-in-Difference Analysis.
eFigure 2. Temporal Trends in Incident MI and Stroke in Urban Influence Code-1 New York State Populations With and Without Subsequent TFA Restrictions.
References
- 1.Doell D, Folmer D, Lee H, Honigfort M, Carberry S. Updated estimate of trans fat intake by the US population. Food Addit Contam Part A Chem Anal Control Expo Risk Assess. 2012;29(6):861-874. [DOI] [PubMed] [Google Scholar]
- 2.Mozaffarian D, Katan MB, Ascherio A, Stampfer MJ, Willett WC. Trans fatty acids and cardiovascular disease. N Engl J Med. 2006;354(15):1601-1613. [DOI] [PubMed] [Google Scholar]
- 3.Kiage JN, Merrill PD, Judd SE, et al. . Intake of trans fat and incidence of stroke in the Reasons for Geographic and Racial Differences in Stroke (REGARDS) cohort. Am J Clin Nutr. 2014;99(5):1071-1076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yaemsiri S, Sen S, Tinker L, Rosamond W, Wassertheil-Smoller S, He K. Trans fat, aspirin, and ischemic stroke in postmenopausal women. Ann Neurol. 2012;72(5):704-715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Imamura F, Lemaitre RN, King IB, et al. . Novel circulating fatty acid patterns and risk of cardiovascular disease: the Cardiovascular Health Study. Am J Clin Nutr. 2012;96(6):1252-1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yaemsiri S, Sen S, Tinker LF, et al. . Serum fatty acids and incidence of ischemic stroke among postmenopausal women. Stroke. 2013;44(10):2710-2717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kris-Etherton PM, Lefevre M, Mensink RP, Petersen B, Fleming J, Flickinger BD. Trans fatty acid intakes and food sources in the US population: NHANES 1999-2002. Lipids. 2012;47(10):931-940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mozaffarian D, Aro A, Willett WC. Health effects of trans-fatty acids: experimental and observational evidence. Eur J Clin Nutr. 2009;63(suppl 2):S5-S21. [DOI] [PubMed] [Google Scholar]
- 9.Panel of Macronutrients; Panel on the Definition of Dietary Fiber; Subcommittee on Upper Reference Levels of Nutrients; Subcommittee on Interpretation and Uses of Dietary Reference Intakes; Standing Committee on the Scientific Evaluation of Dietary Reference Intakes . Dietary fats: total fat and fatty acids In: Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids. Washington, DC: National Academies Press; 2005:423-424. [Google Scholar]
- 10.Brownell KD, Pomeranz JL. The trans-fat ban: food regulation and long-term health. N Engl J Med. 2014;370(19):1773-1775. [DOI] [PubMed] [Google Scholar]
- 11.US Food and Drug Administration FDA cuts trans fat in processed foods. http://www.fda.gov/forconsumers/consumerupdates/ucm372915.htm. Updated June 16, 2015. Accessed September 11, 2015.
- 12.US Food and Drug Administration Final Determination Regarding Partially Hydrogenated Oils (Removing Trans Fat). Vol FDA-2013-N-13172015 Silver Spring, MD: US Food and Drug Administration; 2016:21. [Google Scholar]
- 13.US Food and Drug Administration, Office of Information and Regulatory Affairs Direct Food Substances Affirmed as Generally Recognized as Safe. Silver Spring, MD: US Food and Drug Administration; 2016. [Google Scholar]
- 14.Office of Information and Regulatory Affairs, Office of Management and Budget Direct food substances affirmed as generally recognized as safe; partially hydrogenated menhaden oil and rapeseed oil. https://www.reginfo.gov/public/do/eAgendaViewRule?pubId=201610&RIN=0910-AH28. Accessed March 6, 2017.
- 15.City of New York Article 81: food preparation and food establishments: §81.08: foods containing artificial trans fat. https://www1.nyc.gov/assets/doh/downloads/pdf/about/healthcode/health-code-article81.pdf Published 2006. Accessed March 8, 2016.
- 16.US Geological Survey New York: counties. https://nationalmap.gov/small_scale/printable/images/pdf/counties/pagecnty_ny2.pdf. Accessed October 25, 2015.
- 17.US Geological Survey Reference and outline maps of the United States. https://nationalmap.gov/small_scale/printable/reference.html#New_York. Accessed October 25, 2015.
- 18.Restrepo BJ, Rieger M. Trans fat and cardiovascular disease mortality: evidence from bans in restaurants in New York. J Health Econ. 2016;45:176-196. [DOI] [PubMed] [Google Scholar]
- 19.US Census Bureau Intercensal estimates of the resident population by five-year age groups, sex, race, and Hispanic origin for counties: April 1, 2000, to July 1, 2010. https://www2.census.gov/programs-surveys/popest/datasets/2000-2010/intercensal/county/co-est00int-alldata-36.csvhttp://www.census.gov/popest/data/intercensal/county/CO-EST00INT-alldata.html. Accessed July 22, 2016.
- 20.US Department of Agriculture Economic Research Service 2003 Urban Influence Codes. https://www.ers.usda.gov/webdocs/DataFiles/Urban_Influence_Codes__18018/UrbanInfluenceCodes.xls?v=39559. Published 2003. Accessed March 8, 2017.
- 21.US Department of Agriculture Economic Research Service 2013 Urban Influence Codes. https://www.ers.usda.gov/webdocs/DataFiles/Urban_Influence_Codes__18018/UrbanInfluenceCodes2013.xls?v=41404. Published 2013. Accessed March 8, 2017.
- 22.US Census Bureau Small area income and poverty estimates: state and county estimates for 2006. http://www.census.gov/did/www/saipe/data/statecounty/data/2006.html. Accessed July 30, 2016.
- 23.US Centers for Disease Control and Prevention CDC WONDER: about compressed mortality, 1999-2015. http://wonder.cdc.gov/cmf-icd10.html. Accessed December 30, 2014.
- 24.Sullivan GM, Feinn R. Using effect size: or why the P value is not enough. J Grad Med Educ. 2012;4(3):279-282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dimick JB, Ryan AM. Methods for evaluating changes in health care policy: the difference-in-differences approach. JAMA. 2014;312(22):2401-2402. [DOI] [PubMed] [Google Scholar]
- 26.US Census Bureau 2006-2010 5-Year American Community Survey Commuting Flows. Washington, DC: US Census Bureau; 2010. [Google Scholar]
- 27.US Census Bureau 2009-2013 5-year American Community Survey Commuting Flows. Washington, DC: US Census Bureau; 2013. [Google Scholar]
- 28.Brandt EJ. Deception of trans fats on Food and Drug Administration food labels: a proposed revision to the presentation of trans fats on food labels. Am J Health Promot. 2011;25(3):157-158. [DOI] [PubMed] [Google Scholar]
- 29.Popeyes Louisiana Kitchen Inc Nutrition. http://popeyes.com/menu/nutrition. Accessed July 14, 2016.
- 30.Taco Bell Corp Full nutrition info. https://www.tacobell.com/food/nutrition/info. Accessed July 20, 2016.
- 31.General Mills Inc Pillsbury Shape ghost sugar cookies. https://www.pillsbury.com/products/cookies/holiday-shape-cookies/ghosts. Accessed March 10, 2017.
- 32.Angell SY, Cobb LK, Curtis CJ, Konty KJ, Silver LD. Change in trans fatty acid content of fast-food purchases associated with New York City’s restaurant regulation: a pre-post study. Ann Intern Med. 2012;157(2):81-86. [DOI] [PubMed] [Google Scholar]
- 33.Angell SY, Silver LD, Goldstein GP, et al. . Cholesterol control beyond the clinic: New York City’s trans fat restriction. Ann Intern Med. 2009;151(2):129-134. [DOI] [PubMed] [Google Scholar]
- 34.Sood RK, Torroella Carney M, Buchman T, et al. . First time compliance inspections to evaluate an artificial trans fat ban in Nassau County. Clin Ther. 2014;36(3):333-337.e1. [DOI] [PubMed] [Google Scholar]
- 35.Brewer G, Quinn C, Arroyo M, et al. . Smoke Free Air Act Addendum: Prohibiting Smoking in Pedestrian Plazas and Public Parks: Int 0332-2010. Vol 2011/0112011 New York: The New York City Council Committee on Health; 2011. [Google Scholar]
- 36.New York City Department of Health and Mental Hygiene Posting of calorie information In: New York City Department of Health and Mental Hygiene. New York: New York City Department of Health and Mental Hygiene; 2008:2. [Google Scholar]
- 37.Code of Federal Regulations Title 21, Food Labeling Part 101.9(c)(2). 2008; http://edocket.access.gpo.gov/cfr_2008/aprqtr/pdf/21cfr101.9.pdf. Accessed March 29, 2015.
- 38.Mozaffarian D, Benjamin EJ, Go AS, et al. ; American Heart Association Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics: 2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29-e322. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. 2006 Characteristics of Urban Influence Code-1 New York State Counties With and Without Trans-Fatty Acid Restrictions.
eTable 2. Additional Change in Hospital Admission for MI and Stroke, in Populations With vs Without Subsequent TFA Restrictions Stratified by Sex.
eFigure 1. Theoretical Example of the Difference-in-Difference Analysis.
eFigure 2. Temporal Trends in Incident MI and Stroke in Urban Influence Code-1 New York State Populations With and Without Subsequent TFA Restrictions.